Abstract
Background:
COVID-19 was first reported on 31 December 2019 and has so far claimed over 2,000 lives in Nigeria. Through global and national efforts, about 4 million doses of the AstraZeneca vaccine was distributed and used in Nigeria from March 2021. Vaccine hesitancy could pose a serious problem for COVID-19 prevention and control.
Objectives:
To estimate the proportion of the Nnamdi Azikiwe University community that is willing to be vaccinated against COVID-19; level of hesitancy and its associated factors.
Methods:
A cross-sectional survey was conducted using online Google form distributed to staff and students of the university via different WhatsApp groups. The outcome measures were the proportion of persons willing to be vaccinated, vaccine hesitancy rates and reasons for this hesitancy. Data were analyzed using SPSS version 23 and Minitab version 19. Bivariate analysis was performed by the chi-square test, Odds Ratios (ORs) and statistical significance was accepted when p-value is < 0.05.
Results:
Only 349 of the survey responses were analyzed in the survey. Results show that 34.70 ± 5.00% of the university community were willing to receive the COVID-19 vaccine when it is offered to them. The COVID-19 hesitancy rate among staff and students was 65.04 ± 5.00%. It was discovered that marital status (OR = 2.06), age (OR = 0.802) and christian denominational affiliation (OR = 0.366) influenced respondents’ perception of COVID-19 vaccination. Gender, occupation, previous vaccination experience, awareness of COVID-19 and previous symptoms of COVID-19 did not significantly (p = 0.05) influence respondents’ willingness to be vaccinated.
Conclusion:
COVID-19 vaccine hesitancy is high among staff and students in a Nigerian university and is significantly influenced by marital status, respondents’ age and christian denominational affiliation.
Keywords: AstraZeneca, COVID-19, Nigeria, Nnamdi Azikiwe University, vaccine hesitancy
Introduction
Vaccines are well-known for their effectiveness in controlling and, in some instances, eradicating some diseases of humanity such as smallpox. 1 Smallpox was eradicated in May 1980 following vaccination 2 while wild-type poliomyelitis was recently defeated in Nigeria in August 2020. 3 Vaccines reduce the risk of getting a disease by working with the body’s natural defenses to build protection. When an individual is vaccinated, the person’s immune system is stimulated to form defenses against the disease. 2
An outbreak of COVID-19 in Wuhan, China, caused by a novel Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) was reported on 31 December 2019. COVID-19 subsequently spread to many countries of the world, necessitating the World Health Organization 4 to declare it a public health emergency of international concern on 30 January 2020. By 23 June 2021, the world had witnessed 178, 837,204 confirmed cases of COVID-19, including 3, 880, 450 deaths. 5 COVID-19 has caused disruptions in international travels, global trade and the lockdown of many countries of the world. Within the first 30 days of COVID-19 in Nigeria, the Nigerian Center for Disease Control (NCDC) observed that 70.0% of the individuals who tested positive for COVID-19 were male, and 30.0% were female and their ages ranged between 30 and 60 years. People aged 31–50 years were the most affected (39.0%) and about 44.0% of the cases were imported, while 41.0% had incomplete epidemiological information as the sources of their infections were unknown. Up to 15.0% patients were known contacts of positive cases, suggesting community transmission or cross-infection. 6
The global community was therefore thrown into a race of vaccine design and discovery for COVID-19 pandemic. Scientists around the world worked faster than ever to develop and produce vaccines that could stop the spread of the pandemic. This yielded spectacular results in less than one year and thus offered humanity hope that COVID-19 pandemic will be under control in the coming years. Twenty-two COVID-19 vaccines were within the World Health Organization 7 Emergency Use Listing/Pre-Qualification (WHO EUL/PQ) evaluation process as at June 2021. Assessment of eight out of these vaccines has been finalized. 7 Whereas Pfizer and Moderna vaccines are mRNA-based vaccines, the AstraZeneca, Janssen and Serum Institute vaccines are recombinant adenoviral-vectored vaccines; and Sinopharm and Sinovac vaccines are inactivated viruses produced in Vero cells. 7
Vaccines are perhaps the best hope for ending the pandemic to prevent COVID-19. 8 To bring a vaccine-preventable disease under control, herd immunity is usually pursued. Herd immunity refers to enough people having immunity to an infectious disease — whether through previous infection or vaccination. 9 Herd immunity is the goal of vaccinations and the more contagious the disease, the higher the threshold required for herd immunity. For example, the herd immunity required for control of measles in a population is 95%. 9 Scientists have estimated that 70–90% immunity will be required to provide herd immunity for COVID-19. 9
Vaccine hesitancy refers to delay in acceptance or refusal of vaccination despite availability of vaccination services. 10 The “3 Cs” model of vaccine hesitancy, namely Complacency, Convenience, and Confidence, was first proposed to the WHO EURO Vaccine Communications Working Group in 2011. 11 Vaccine hesitancy especially in Nigeria, may be driven by fear of the unknown. In a very recent review by Sallam on vaccine acceptance rates worldwide, it was concluded that more studies are recommended to address the scope of COVID-19 vaccine hesitancy. 12 The study further concluded that addressing the scope of COVID-19 vaccine hesitancy in various countries is recommended as an initial step for building trust in COVID-19 vaccination efforts. 12
The pandemic has brought about huge negative consequences on business, education, health, and tourism globally. During the first wave, the primary, secondary and tertiary institutions in Nigeria were closed and these seriously affected millions of students in tertiary institutions who have their semesters canceled or suspended due to the pandemic. While many other countries switched to virtual learning, many tertiary institutions within Nigeria lack the various online educational platforms or facilities for such method of teaching, which have worsened the situation for students in the country. 13
Nnamdi Azikiwe University is a close-knit community with a large staff and student population, in addition to children from the University Demonstration Primary and University High School. The university is located in Awka, the State capital of Anambra State, South-East, Nigeria. Given the growing visibility and popularity of the university, there is a large population of stakeholders who come into the university frequently. Consequently, any vaccine hesitancy in this community may be devastating and will put the university population at high risk of COVID-19 infection. Moreso, the university is located in a State where the COVID-19 protocols appear to be largely ignored by residents as can be seen in marketplaces, churches and funeral ceremonies. The University Medical Services obtained the AstraZeneca vaccine and administered same to members of the university community.
Based on the foregoing, there was an urgent need to interrogate the perception of COVID-19 vaccination exercise among staff and students of Nnamdi Azikiwe University. This might help determine the level of COVID-19 vaccine acceptance and hesitancy in the university amid the vaccine roll-out. The study was also expected to reveal the reasons for hesitancy and make recommendations for enhancing the vaccine acceptance in the university.
The objectives of the study were to establish the proportion of the Nnamdi Azikiwe University community that is willing to be vaccinated against COVID-19; level of hesitancy and its associated factors.
Methods
Study design
A cross-sectional study.
Study population
Staff and students of Nnamdi Azikiwe University, staff of University Demonstration Primary School as well as staff and students of the University High School. The study population has Internet access in their homes via cellular reception, although signal strength may fluctuate.
Study site
Nnamdi Azikiwe University, Awka, South-East Nigeria. It is a tertiary institution responsible for undergraduate and postgraduate training. It is the only federal university in Anambra State, Nigeria. Internet access (Wi-Fi) on campus is free but may be weak at periods of peak use by the community.
Inclusion criteria
These included all staff and students in any department or unit of the university aged between 16 and 80 years who received the online questionnaire and submitted the electronic form voluntarily. Respondents’ informed consent for the study was required and implied by voluntary completion and submission of survey.
Exclusion criteria
Persons within the university community who were not students or staff were excluded.
Data collection
Data were collected using a self-administered electronic questionnaire. Both qualitative and quantitative data were collected. Effectively, a Google form—containing the study questions and response facilities—was developed. The link to the form was then copied and sent to all faculties, departments, units and institutes in Nnamdi Azikiwe University. The link to the survey form was also sent to relevant staff and student WhatsApp groups. Through this process, the link was well-distributed across the university, reaching a good number of staff and students, thus allowing interested members of the university community to respond. Data were collected for 38 days, from 21 January, 2021 to 28 February, 2021.
Data collection technique
A questionnaire was used to collect the data from which key percentage frequencies needed to address some of the study’s objectives were calculated. The following steps were involved in the questionnaire development and validation. First, the questionnaire’s face validity was established by having it reviewed by two different experts (expert in infectious disease management and measurement and evaluation expert in test construction). The expert in infectious disease ensured that the questions successfully captured the topics on vaccine hesitancy. The measurement and evaluation expert ensured that our questionnaire did not contain common errors such as confusing, leading, or double-barreled questions. We revised the questionnaire based on the feedback obtained.
Open-ended questions in the questionnaire were used to collect the qualitative data with which the perceptions of the university community on COVID-19 vaccination were uncovered. This method was chosen because it is adequate for the collection of the type of qualitative data needed (given that it allowed respondents to freely input their responses into text boxes, thereby making it possible for their deep perceptions to be captured just as qualitative research requires. 14
The questionnaire was administered electronically. While this approach generally had the potential to limit responses (given that strong Internet access at periods of peak use is usually an out-of-pocket expense in the university and because people are relatively less enthusiastic when it comes to filling online questionnaires), the online format was nevertheless chosen. This was because the COVID-19 pandemic and the movement restrictions associated with it made it inappropriate for the type of physical movement needed to effectively distribute hardcopy questionnaires across the university.
Survey questions
The participants were asked to provide their age, marital status, level of education and occupation. They were then asked whether they have used medication for COVID-19 and whether they had prior symptoms of COVID-19, heard of COVID-19, willing or not willing to receive COVID-19 vaccine as well as whether they were undecided to receive COVID-19 vaccine. They were also asked whether their unwillingness to accept COVID-19 vaccine was due to safety concern, or lack of trust in the vaccine source, lack of trust in the vaccine developers, conspiracy theory or disbelief over existence of COVID-19.
Outcome measures
The outcome measures were the proportion of persons who were willing to be vaccinated, vaccine hesitancy rate and reasons for vaccine hesitancy.
Sample size calculation for cross sectional study
Using the COVID-19 vaccine acceptance rate in a Congo study 15 of 27.7%, 10% attrition and using the sample size formular of 16
a total of 339 subjects were needed as the minimum sample size for the study.
Data analysis
Quantitative data were analyzed using SPSS version 23 and Minitab version 19. Relevant percentage frequencies, standard error, chi-square, odds ratio, and confidence interval estimations were obtained. Odds ratio was calculated by casting the responses into a 2x2 contingency table. Qualitative data were analyzed thematically and the perceptions of respondents on COVID-19 vaccination were then organized into key themes. To stay true to the participants’ words and experiences, two independent coders read each filled questionnaires and used grounded theory coding techniques to gather all emerging categories from the text. The grounded theory coding started with a line-by-line review of the text, creating open codes that captured pieces of text relevant to the research questions. The open codes were then gathered into focused codes to capture major coding themes emerging from the participants. Finally, these categories were reorganized and revised to reach a broader understanding. The researchers translated the focused codes into broader themes and subthemes to best represent study participants’ perceptions of COVID-19 vaccine and capture any phenomenon. Additional analysis was conducted to see how participant’s experiences varied by gender, age, marital status, and religious denomination.
Ethical approval
Ethical approval was obtained from the Health Research Ethics Committee of Chukwuemeka Odumegwu Ojukwu University Teaching Hospital, Awka, Nigeria (Assigned number: COOUTH/CMAC/ETH.C/Vol1/FN:04/103).
Results
Demographic characteristics of respondents
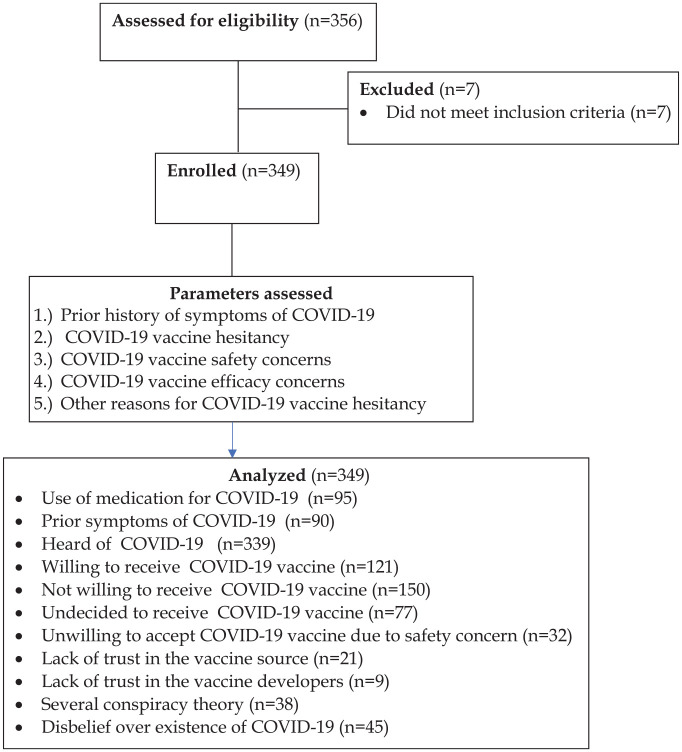
The survey received a total of 356 responses from different age groups ranging from 10 to over 80 years but 349 responses were analyzed after we excluded those younger than 16 years (Figure 1). Most, 28.94% (101/349) of the respondents were between 31 and 40 years old. Nearly all respondents are Nigerians (99.14%, 346/349) and 66.19% (231/349) of respondents are from Anambra State. Respondents are from different faculties, departments, units in the university as well as from the University Demonstration Primary School and University High School. The faculty of Engineering had the highest number of respondents (14.04%, 49/349). Most of the respondents were teaching staff (43.27%, 151/349), males (59.31%, 207/349), married (52.15%, 182/349), and Christians (99.14%, 346/349).
Figure 1.
Flow pattern of respondents who participated in the survey.
Approach to prevention, history of symptoms and tests
Some of the respondents (27.22%, 95/349) were using medications to prevent COVID-19 infection. Out of this percentage, 26.32% (25/95) and 23.16% (22/95) of respondents were using orthodox and herbal medicines respectively. Other approaches employed by the respondents include use of hand sanitizers (5.3%), facemasks (4.2%), steam inhalation (2.1%), exercise (2.1%), social and physical distancing (4.2%) etc. Although as many as 25.79% (90/349) of respondents might have had symptoms of COVID-19, none of the respondents ever tested for the virus.
COVID-19 vaccination
While 97.13% (339/349) of respondents have heard about the COVID-19 vaccine at the time of this study, only 34.67% (121/349) were willing to receive the vaccine when it is offered to them. As many as 42.98% (150/349) of the respondents were not willing to receive the COVID-19 vaccine while 22.06% (77/349) were undecided, thus yielding a hesitancy rate of 65.04%. This high hesitancy exists even though most of the respondents (78.51%, 274/349) had been vaccinated against one disease or the other in the past and 85.30% (238/279) of those have never had allergic reaction to any vaccine or injectable medication.
Reasons for COVID-19 vaccine hesitancy
The respondents stated several reasons why they were unwilling to receive the COVID-19 vaccine when it is offered to them. These included:
Efficacy concern
Uncertainty about the vaccine’s efficacy was the most important concern (34.34%, 37/108) expressed by respondents. According to some of the respondents, this concern arises due to the alleged inability of the vaccine to provide protection against all known strains of COVID-19(18.52%, 20/108), as well as the cold chain storage challenges (24.07%, 26/108) usually encountered in Nigeria.
Safety concern
Safety concern was a major reason (9.17%, 32/349) respondents were skeptical about receiving the COVID-19 vaccine. Safety concern revolved around lack of trust in the vaccine sources (6.0%), vaccine developers (2.6%), donors and the Nigerian government (4.6%); vaccine development within 1 year (1.7%); lack of rigorous safety testing (1.7%); several conspiracy theories (10.8%); possibility of receiving a fake vaccine (6.2%); fears of adverse effects and events (11.2%), among others.
Other reasons for COVID-19 vaccine hesitancy
The other reasons for the unwillingness of some respondents to be vaccinated, beyond safety and effectiveness concerns, included disbelief over the existence of COVID-19 in Nigeria(12.89%, 45/349); poor knowledge of COVID-19 vaccine(7.45%, 26/349); belief that other preventive measures are enough protection(2.58%, 9/349); belief that the body’s immunity is strong enough against the virus(0.86%, 3/349); the vaccine not needed if one is not infected with the virus(3.72%, 13/349); and COVID-19 can be easily treated with medicines such as chloroquine(1.43%, 5/349). Some respondents also cited unpredictable consequences of messenger RNA (mRNA) COVID-19 vaccine (1.15%, 4/349) as well as religious beliefs (1.43%, 5/349).
Factors influencing willingness to receive COVID-19 vaccine
Age and attitude to vaccination
Association between age and attitude was investigated using the chi-square test for association. Table 1 below shows the pooled two-way classification for the test. Expected frequencies are in parentheses. Hesitancy was derived from the summation of “Maybe” and “No” responses while non-hesitancy was obtained from number of “Yes” responses.
Table 1.
Relationship between age and responses to the question, “Will you be willing to be vaccinated against COVID-19 disease?”
| Age range (years) | Responses | Hesitancy (%) | Non-hesitancy (%) | |||
|---|---|---|---|---|---|---|
| Maybe | No | Yes | Total | |||
| 16–20 | 2 (4.19) | 9 (8.17) | 8 (6.64) | 19 | 51.9 | 42.1 |
| 21–25 | 19 (16.33) | 23 (31.81) | 32 (25.87) | 74 | 56.8 | 43.2 |
| 26–30 | 13 (10.37) | 16 (20.20) | 18 (16.43) | 47 | 61.7 | 38.3 |
| 31–40 | 27 (22.28) | 38 (43.41) | 36 (35.31) | 101 | 64.4 | 35.6 |
| 41–50 | 12 (13.68) | 36 (26.65) | 14 (21.67) | 62 | 77.4 | 22.6 |
| 51–60 | 3 (7.50) | 23 (14.61) | 8 (11.89) | 34 | 76.5 | 23.5 |
| 61–80 | 1 (2.65) | 5 (5.16) | 6 (4.19) | 12 | 50.0 | 50.0 |
| Total | 77 | 150 | 122 | 349 | 65.04 | 34.96 |
Chi-square value = 26.012 (p-value = 0.011, level of significance < 0.05, odds ratio = 0.802).
Marital status and attitude to vaccination
Association between marital status and attitude was investigated using the chi-square test for association. Table 2 below shows the pooled two-way classification for the test. Expected frequencies are in parentheses. Hesitancy was derived from the summation of “Maybe” and “No” responses while non-hesitancy was obtained from number of “Yes” responses.
Table 2.
Relationship between marital status and responses to the question, “Will you be willing to be vaccinated against COVID-19 disease?”
| Marital status | Responses | Hesitancy (%) | Non-hesitancy (%) | |||
|---|---|---|---|---|---|---|
| Maybe | No | Yes | Total | |||
| Ever married | 37 (41.48) | 96 (80.80) | 55 (65.72) | 188 | 70.70 | 29.30 |
| Never married and others | 40 (35.52) | 54 (69.20) | 67 (56.28) | 161 | 58.40 | 41.60 |
| Total | 77 | 150 | 122 | 349 | 65.04 | 34.96 |
Chi-square value = 11.034 (p-value = 0.004, level of significance < 0.05, odds ratio = 2.06).
Church denomination and attitude to vaccination
Association between church denomination and attitude was investigated using the chi-square test for association. Table 3 below shows the pooled two-way classification for the test. Expected frequencies are in parentheses. Hesitancy was derived from the summation of “Maybe” and “No” responses while non-hesitancy was obtained from number of “Yes” responses.
Table 3.
Relationship between church denomination and responses to the question, “Will you be willing to be vaccinated against COVID-19 disease?”
| Christian denomination | Responses | Hesitancy (%) | Non-hesitancy (%) | |||
|---|---|---|---|---|---|---|
| Maybe | No | Yes | Total | |||
| Pentecostal/ Sabbatherian | 11 (19.28) | 84 (59.50) | 21 (37.23) | 116 | 81.9 | 18.1 |
| Protestant | 10 (11.80) | 34 (36.42) | 27 (22.79) | 71 | 62.0 | 38.0 |
| Roman Catholic | 37 (26.92) | 61 (83.09) | 64 (51.99) | 162 | 60.5 | 39.5 |
| Total | 58 | 179 | 112 | 349 | 67.9 | 32.1 |
Chi-square value = 34.345 (p-value = 0.001, level of significance < 0.05, odds ratio = 0.366).
Relationship between willingness to be vaccinated and other variables
There was no significant relationship (p = 0.05) between willingness to be vaccinated on the one hand and each of gender, occupation, previous vaccination experience, awareness of COVID-19 and previous symptoms of COVID-19 on the other hand.
Discussion
The motivation for this study was that the University Medical Services received and administered the AstraZeneca COVID-19 vaccine that was donated in large quantities to Nigeria through the global COVAX scheme. 8 Because a university community (staff and students) can be a reliable source of health information, their willingness or unwillingness to receive COVID-19 vaccine can influence the general population’s uptake of the vaccine.
From the findings of the study, 34.70 ± 5.00% of the university community are willing to be vaccinated against COVID-19. This is lower than the national average of 50% (as reported by the Honorable Minister of Health on national television in March 2021) and 55.5% reported among some Nigerian health workers in a study. 17 Willingness to receive the COVID-19 vaccine was 27.7% among healthcare workers in Democratic Republic of Congo. 15 As many as 65.7% and 83.8% of Japanese and Chinese adults respectively were willing to receive COVID-19 vaccine.18,19 Up to 86.1% of Italian university students were willing to be vaccinated. 20 It is evident that the willingness to receive COVID-19 vaccine by members of Nnamdi Azikiwe University community is poor in comparison with the university students in Italy and adults in high-income countries such as Japan and China. This low level has implications for the larger Nigerian society, who will obviously look up to the enlightened university community for direction. In a recent systematic review by Wake, 21 the overall rate of participants’ willingness to receive the COVID-19 vaccine was ranged from 27.7% to 91.3%, which was from Congo and China respectively. Factors such as age, educational status, gender, income, residency, occupation, marital status, race/ethnicity, perceived risk of COVID-19, trust in healthcare system, health insurance, norms, attitude toward vaccine, perceived benefit of vaccine, perceived vaccine barriers, self-efficacy, up-to-date on vaccinations, tested for COVID-19 in the past, perceived efficacy of the COVID-19 vaccination, recommended for vaccination and political leaning were associated with the willingness of receive COVID-19 vaccine. Other factors include perceived severity of COVID-19, perceived effectiveness of COVID-19 vaccine, belief that vaccination makes them feel less worried about COVID-19, believing in mandatory COVID-19 vaccination, perceived potential vaccine harms, presence of chronic disease, confidence, COVID-19 vaccine safety concern, working in healthcare field, believing vaccines can stop the pandemic, fear about COVID-19, cues to action, COVID-19 vaccine hesitancy, complacency, and receiving any vaccine in the past 5 years. 21
In this study, the COVID-19 hesitancy rate was found to be 65.04 ± 5.00% in the Nnamdi Azikiwe University community. This is higher than the hesitancy rate of 22.0% obtained in a community-based study of American adult population and 43.5% obtained among students at health schools in Jordan, 12 but similar to 65% found in Portugal.22,23 The high COVID-19 hesitancy among Nnamdi Azikiwe University community is attributed largely to safety and efficacy concerns, despite the approval of the COVID-19 vaccine by the WHO and the Nigerian drug regulatory agency, National Agency for Food and Drug Administration and Control. 7 Also, the clinical trials that generated the COVID-19 vaccine safety and effectiveness data were conducted using samples that are very representative of the black. 24 These suggest that the vaccine is safe and effective in blacks and can be used in Africa, even where resources do not permit additional local clinical trials, as was the case in Nigeria.
Another interesting aspect of the findings were the COVID-19 prevention strategies adopted by the participants. Some participants used approved strategies such as hand sanitizers (5.3%), facemasks (4.2%), as well as social and physical distancing (4.2%) as preventive strategies. Many of the participants, however, reported using orthodox medicines (27.22%) or herbal medicines (26.32%), steam inhalation (2.1%), exercise (2.1%) as preventive strategies. Family and friends freely recommended on social media the use of orthodox medicines (especially chloroquine and ivermectin), herbal remedies made from local food spices and citrus, steam inhalations of leaves of lemon grass, guava etc. These unordinary preventive strategies adopted by the participants, though unsubstantiated, may explain the high vaccine hesitancy rate reported in the study. Although the first published study on COVID-19 vaccine hesitancy in Nigeria reported a 25.5% hesitancy among respondents by August 2020 when the vaccine was not yet available, 25 the worsened COVID-19 vaccine hesitancy (65.04%) by March 2021 may have been largely fueled by social media conspiracy theories, efficacy and safety concerns.
Three factors, namely: age, marital status and christian denominational affiliation were significantly associated with COVID-19 vaccine hesitancy in our study community. There is a significant association between age and attitude toward COVID-19 vaccination. The odds ratio value of 0.802 obtained implies that younger members of the university community are more likely to take the vaccine than older members. Interestingly, respondents aged 61 to 80 were the least hesitant (50%) about the COVID-19 vaccine. Perceived higher vulnerability of this age group may account for their willingness to accept the vaccine. This is in tandem with published research results by Davies et al., 26 and Soares et al. 23 Davies attributed this to the fact that COVID-19 infection is more fatal in older population than in younger population.
There is a significant association between marital status and attitude toward COVID-19 vaccination. The odds ratio value of 2.06 obtained implies that “Ever Married” members of Nnamdi Azikiwe University are more hesitant than the “Never Married” members of the community.
There is a significant association between church denomination and attitude toward COVID-19 vaccination. The odds ratio value of 0.366 obtained showed that Roman Catholics and Protestants are more likely to accept the COVID-19 vaccine than the Pentecostals and Sabbaterians. The association of COVID-19 vaccination and the end of the world (conspiracy theory) by some popular Pentecostal evangelists on social media may be responsible for the higher hesitancy among the Pentecostals and Sabbaterians.
The study did not find significant relationships (p = 0.05) between willingness to be vaccinated and each of the following variables: gender, occupation, previous vaccination experience, awareness of COVID-19 and previous symptoms of COVID-19.
Safety and efficacy concerns were the major reasons why respondents were skeptical about receiving the COVID-19 vaccine. Lack of trust in the vaccine sources, vaccine developers, donors and the Nigerian government; vaccine development within one year; lack of rigorous safety testing; several conspiracy theories; possibility of receiving a fake vaccine; fears of adverse effects and events were the major drivers of the concerns. A similar study in India among medical students cited lack of trust in government agencies as a predictor of their high COVID-19 vaccine hesitancy. 27
High vaccine hesitancy rate observed in our study was corroborated by a study in France which predicted high vaccine hesitancy rates for vaccines manufactured in China (with 50% efficacy and a 1 in 10 000 risk of serious side-effects) as against vaccines manufactured in the European Union (with 90% efficacy and a 1 in 100 000 risk of serious side-effects). 28 AstraZeneca COVID-19 deployed in Nigeria was manufactured in India, a country with similar drug regulatory standards like China. There were also doubts about the vaccine’s efficacy and hence protection against emerging strains of COVID-19. Efficacy of the vaccines down to the last mile was also in doubt among the respondents because of the well-known cold chain storage challenges usually encountered in Nigeria.
Other reasons for the unwillingness of some respondents to be vaccinated included disbelief over the existence of COVID-19 in Nigeria; poor knowledge of the new technology platforms used in the design and development of COVID-19 vaccine; belief that other preventive measures are enough protection; belief that the body’s immunity is strong enough against the virus; the vaccine not needed if one is not infected with the virus; COVID-19 can be easily treated with medicines such as chloroquine. In a similar study among medical students in Egypt, the most significant barriers of COVID-19 vaccination were deficient data regarding the vaccine’s adverse effects and insufficient information regarding the vaccine itself. 29
In this study, some respondents cited unpredictable consequences of mRNA COVID-19 vaccine as their reason for COVID-19 vaccine hesitancy. This is consistent with report on hesitation against mRNA vaccines in the global community occasioned by the rapid pace of vaccine development and the uncertainty of its potential long-term adverse effects. 30 The mRNA is one of the new technology platforms used in the design and development of vaccines for about two decades with instability as its major challenge. The solution to mRNA instability challenge appears to have been figured out by scientists. 31
Although the other preventive approaches to COVID-19 infection such as social and physical distancing, use of facemasks in public places, frequent hand washing and use of hand sanitizers are somewhat effective, vaccination would offer the maximum possible protection against COVID-19 to both an individual recipient and the university community. 32 Self-help and nature-based remedies circulated freely on social media and were patronized by some respondents.
Many respondents believed that COVID-19 can be easily treated with medicines such as chloroquine. Though approved drugs for COVID-19 such as remdesivir and dexamethasone provide some benefits to patients, they are not a sufficient treatment for the disease.32,33 Not minding that the COVID-19 vaccine can be received free of charge in designated healthcare facilities in Nigeria, many eligible persons were unwilling to receive the jab. In addition, financial benefits, however, could help to focus vaccine decisions on medical factors by offsetting other costs, such as the need to take time off work because of vaccine adverse effects.
Trust in the body’s immune system and disbelief that COVID-19 exists in Nigeria also explain the huge disinterest in COVID-19 vaccination. However, till date, there is no scientific evidence that anyone is immune to COVID-19 infection. Instead, published figures from the Nigeria Centers for Disease Control (NCDC) show that Nigeria has had a total of 167,375 confirmed cases of COVID-19 as at 24 June 2021, and a total of 2,118 deaths have resulted from these cases. 34
Religious inclinations were also implicated in the high COVID-19 vaccine hesitancy. This corroborates findings from studies in England and Wales which showed that religion was a significant factor in matters relating to risks of deaths due COVID-19. 35
Some respondents also opined that the virus cannot thrive in countries with tropical weather conditions and as such, conceptualized COVID-19 reports in Nigeria as a myth and mere avenue for corrupt government officials to siphon public funds. Other respondents believed that being the black race and having been availed several vaccines at the early stages of their lives, Nigerians are more immune to the virus than non-Africans. 36 In summary, the large volumes of misinformation on COVID-19 vaccines that circulate freely in the social media may have undermined COVID-19 vaccine acceptance in Nigeria.
Limitations and strength of study
This study is limited to Nnamdi Azikiwe University community and the findings are therefore limited to this population. There could also be the bias due to the qualitative nature of the analysis employed in this study as well as the potential selection bias as some participants who had no or weak Internet access at the time of the survey may have been eschewed. However, this limitation is also a strength because the study was conducted in an academic community, whose members are expected to be better informed on the subject-matter of this study than the general populace. To our knowledge, this is one of the first studies in Nigeria on COVID-19 vaccine hesitancy in a university community.
Conclusion and recommendations
COVID-19 vaccine hesitancy is high among staff and students of Nnamdi Azikiwe University and is significantly influenced by marital status, respondents’ age and christian denominational affiliation.
It is therefore recommended that appropriately designed advocacy and behavior-change communication messages that target the respective segments of university community members should be deployed to minimize vaccine hesitancy in the community. The high hesitancy rate is alarming for an academic institution and this should stir further studies on the root causes of COVID-19 vaccine hesitancy in Nigeria.
Acknowledgments
The current work had taken great efforts from all colleagues that work in the Nnamdi Azikiwe University who kindly participated in the online survey. Great thanks to all who shared and helped to put this work in its final form.
Footnotes
Author contributions: IC Uzochukwu, GU Eleje and GO Chukwuma were involved in the overall conceptual design. IC Uzochukwu, GU Eleje, GO Chukwuma, BA Mathias, CE Uzochukwu, CA Uzuke, CS Okunna, CH Nwankwo, LA Asomugha and CO Esimone were involved in the implementation of the project and writing of this manuscript and overall revision of the manuscript. The authors read, approved the final manuscript, and agreed to be accountable for all aspects of the work.
Conflict of interest statement: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Disclosure statement for publication: All authors have made substantial contributions to: conception and design of the study, or acquisition of data, or analysis and interpretation of data; drafting the article or revising it critically for important intellectual content; and final approval of the version submitted. This manuscript has not been submitted for publication in any other journal.
ORCID iDs: Ikemefuna Chijioke Uzochukwu  https://orcid.org/0000-0002-5139-1537
https://orcid.org/0000-0002-5139-1537
George Uchenna Eleje  https://orcid.org/0000-0002-0390-2152
https://orcid.org/0000-0002-0390-2152
George Okechukwu Chukwuma  https://orcid.org/0000-0002-7397-2391
https://orcid.org/0000-0002-7397-2391
Data availability: The data used to support the findings of this study are publicly available from the site.
Contributor Information
Ikemefuna Chijioke Uzochukwu, Department of Pharmaceutical & Medicinal Chemistry, Faculty of Pharmaceutical Sciences, Nnamdi Azikiwe University, Awka 420281, Nigeria.
George Uchenna Eleje, Department of Obstetrics and Gynecology, Faculty of Medicine, Nnamdi Azikiwe University, Awka, Nigeria.
Chike Henry Nwankwo, Department of Statistics, Faculty of Physical Sciences, Nnamdi Azikiwe University, Awka, Nigeria.
George Okechukwu Chukwuma, Department of Medical Laboratory Science, Faculty of Health Sciences and Technology, Nnamdi Azikiwe University, Awka, Nigeria.
Chinwendu Alice Uzuke, Department of Statistics, Faculty of Physical Sciences, Nnamdi Azikiwe University, Awka, Nigeria.
Chinwe Elizabeth Uzochukwu, Department of Mass Communication, Faculty of Social Sciences, Nnamdi Azikiwe University, Awka, Nigeria.
Bentina Alawari Mathias, Department of Sociology and Anthropology, Faculty of Social Sciences, Nnamdi Azikiwe University, Awka, Nigeria.
Chinyere Stella Okunna, Department of Mass Communication, Faculty of Social Sciences, Nnamdi Azikiwe University, Awka, Nigeria.
Lasbrey Azuoma Asomugha, Department of Anatomy, Faculty of Basic Medical Sciences/University Medical Services, Nnamdi Azikiwe University, Awka, Nigeria.
Charles Okechukwu Esimone, Department of Pharmaceutical Microbiology & Biotechnology, Faculty of Pharmaceutical Sciences, Nnamdi Azikiwe University, Awka, Nigeria.
References
- 1. Horton R. The lessons of smallpox eradication for COVID-19. Lancet (London, England) 2021; 396: 1951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Strassburg MA. The global eradication of smallpox. Am J Infect Control 1982; 10: 53–59. [DOI] [PubMed] [Google Scholar]
- 3. Adebisi YA, Eliseo-Lucero Prisno D, Nuga BB. Last fight of wild polio in Africa: Nigeria’s battle. Public Health Pract 2020; 1: 100043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Health Organization. Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV), https://www.who.int/news/item/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) (2020, accessed 24 June 2021).
- 5. World Health Organization. WHO health emergency dashboard, https://who.sprinklr.com/ (2021, accessed 24 June 2021).
- 6. Amzat J, Aminu K, Kolo VI, et al. Coronavirus outbreak in Nigeria: burden and socio-medical response during the first 100 days. Int J Infect Dis 2020; 98: 218–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. World Health Organization. Status of COVID-19 vaccines with WHO-EUL/PQ evaluation process, https://extranet.who.int/pqweb/sites/default/files/documents/Status_of_COVID-19_Vaccines_within_WHO_EUL-PQ_evaluation_process-16June2021_Final.pdf (2021, accessed 24 June 2021).
- 8. World Health Organization. COVID-19 vaccines shipped by COVAX arrive in Nigeria, https://www.afro.who.int/news/covid-19-vaccines-shipped-covax-arrive-nigeria (2021, accessed 18 March 2021).
- 9. Hicks L. Herd immunity and COVID-19: 5 things to know. Medscape, 12 April, https://www.medscape.com/viewarticle/949145 (2021, accessed 25 June 2021).
- 10. MacDonald NE and SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: definition, scope and determinants. Vaccine 2015; 33: 4161–4164. [DOI] [PubMed] [Google Scholar]
- 11. World Health Organization. Appendices to the report of the SAGE working group on vaccine hesitancy, https://www.who.int/immunization/sage/meetings/2014/october/2_SAGE_Appendicies_Background_final.pdf (2014, accessed 24 June 2021).
- 12. Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines (Basel) 2021; 9: 160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Adebowale OO, Adenubi OT, Adesokan HK, et al. SARS-CoV-2 (COVID-19 pandemic) in Nigeria: multi-institutional survey of knowledge, practices and perception amongst undergraduate veterinary medical students. PLoS ONE 2021; 16: e0248189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. SAGE Publications. Methods of data collection in quantitative, qualitative, and mixed research, https://us.sagepub.com/sites/default/files/upm-assets/106363_book_item_106363.pdf (2020, accessed 16 March 2021).
- 15. Kabamba NM, Kabamba NL, Ngoie MG, et al. Acceptability of vaccination against COVID-19 among healthcare workers in the Democratic Republic of the Congo. Pragmat Obs Res 2020; 11: 103–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Noordzij M, Tripepi G, Dekker FW, et al. Sample size calculations: basic principles and common pitfalls. Nephrol Dial Transplant 2010; 25: 1388–1393. [DOI] [PubMed] [Google Scholar]
- 17. Tobin EA, Okonofua M, Adeke A, et al. Willingness to accept a COVID-19 vaccine in Nigeria: a population-based cross-sectional study. Cent Afr J Public Health 2021; 7: 53–60. [Google Scholar]
- 18. Chen M, Li Y, Chen J, et al. An online survey of the attitude and willingness of Chinese adults to receive COVID-19 vaccination. Hum Vaccin Immunother 2021; 17: 2279–2288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Yoda T, Katsuyama H. Willingness to receive COVID-19 vaccination in Japan. Vaccines 2021; 9: 48, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7828811/ (accessed 20 April 2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Barello S, Nania T, Dellafiore F, et al. Vaccine hesitancy among university students in Italy during the COVID-19 pandemic. Eur J Epidemiol 2020; 35: 781–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wake AD. The willingness to receive COVID-19 vaccine and its associated factors: “vaccination refusal could prolong the war of this pandemic”—a systematic review. Risk Manag Health Policy 2021; 14: 2609–2623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Khubchandani J, Sharma S, Price JH, et al. Covid-19 vaccination hesitancy in the United States: a rapid national Assessment. J Community Health 2021; 46: 270–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Soares P, Rocha JV, Moniz M, et al. Factors associated with COVID-19 vaccine hesitancy. Vaccines (Basel) 2021; 9: 300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Artiga S, Kates J, Michaud J, et al. Racial diversity within COVID-19 vaccine clinical trials: key questions and answers, https://www.kff.org/racial-equity-and-health-policy/issue-brief/racial-diversity-within-covid-19-vaccine-clinical-trials-key-questions-and-answers/ (2021, accessed 18 March 2021).
- 25. Adebisi YA, Alaran AJ, Bolarinwa OA, et al. When it is available, will we take it? Social media users’ perception of hypothetical COVID-19 vaccine in Nigeria. Pan Afr Med J 2021; 38: 230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Davies NG, Klepac P, Liu Y, et al. Age dependent effects in the transmission and control of COVID-19 epidemic. Nat Med 2020; 26: 1205–1211. [DOI] [PubMed] [Google Scholar]
- 27. Jain J, Saurabh S, Kumar P, et al. COVID-19 vaccine hesitancy among medical students in India. Epidemiol Infect 2021; 149: e132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Schwarzinger M, Watson V, Arwidson P, et al. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health 2021; 6: e210–e221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Saied SM, Saied EM, Kabbash IA, et al. Vaccine hesitancy: beliefs and barriers associated with COVID-19 vaccination among Egyptian medical students. J Med Virol 2021; 93: 4280–4291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Anand P, Stahel VP. The safety of Covid-19 mRNA vaccines: a review. Patient Saf Surg 2021; 15: 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zhang C, Maruggi G, Shan H, et al. Advances in mRNA vaccines for infectious diseases. Fronti Immunol 2019; 10: 594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Centers for Disease Control and Prevention. Benefits of getting vaccinated, https://www.cdc.gov/coronavirus/2019-ncov/vaccines/vaccine-benefits.html (2021, accessed 18 March 2021).
- 33. National Institutes of Health. Final report confirms remdesivir benefits for COVID-19, https://www.nih.gov/news-events/nih-research-matters/final-report-confirms-remdesivir-benefits-covid-19 (2020, accessed 18 March 2021).
- 34. Nigeria Centre for Disease Control. COVID-19 NIGERIA, https://covid19.ncdc.gov.ng/ (2021, accessed 24 June 2021).
- 35. Gaughan CH, Ayoubkhani D, Nafilyan V, et al. Religious affiliation and the risk of COVID 19 related mortality; a retrospective analysis of variation in pre and post lockdown risk by religious group in England and Wales. MedRxiv, 2020. DOI: 10.1101/2020.10.01.20204495. [DOI] [Google Scholar]
- 36. Akeredolu OA, Azeez AA, Adetunji AS, et al. Perception and awareness of people towards covid-19 and the various methods of treatment in Nigeria. World J Adv Res Rev 2020; 6: 78–85. [Google Scholar]