Abstract
OBJECTIVE:
This study aims to facilitate a surgeon's preoperative assessment by detecting the prevalence, location, and course of the mandibular incisive canal (MIC) in our population.
METHODOLOGY:
A retrospective study was conducted at King Saud University, Riyadh, Saudi Arabia. A total of 93 cone-beam computed tomography (CBCT) scans of patients aged 18–50 years were taken. The images were reformatted from the sagittal sections to para-sagittal sections at premolars, canines, lateral incisors, and central incisors measured to the distance of MIC to the tooth apex, to the inferior border of the mandible, to the buccal cortex, and to the lingual cortex.
RESULTS:
MIC among the patients was found to be present in 96.8% of the total subjects. Prevalence between genders showed that it was present in 97.9% of the male patients and 95.5% of the female patients. The average distance from the buccal cortex is 4.88, the lingual cortex is 5.54, inferior border is 9.94, and root apices is 7.67. The age-wise and gender-wise comparison of a mean distance of MIC to the different surfaces in the different cross-sections showed that there is no correlation, and there is a significant correlation, respectively.
CONCLUSION:
The detection of the MIC presence and location using CBCT should be earnestly considered for surgical procedures that are intended to be done in the interforaminal region.
Keywords: Cone-beam computed tomography, interforaminal region, mandibular incisive nerve, safe margins
Introduction
The mandibular incisive canal (MIC) is the intra-bony terminal branch of the inferior alveolar nerve (IAN).[1] According to some researchers, the incisive nerve does not run through a canal but through the medullary spaces, hence, it cannot be detected using conventional radiography.[1,2] But clear evidence is found on the existence of the MIC by anatomical studies that used advanced imaging tools.[2,3] It is located mesially to the mental foramen, smaller in diameter, and less corticated than the mandibular canal containing the neurovascular bundle.[4,5,6] The MIC was scrutinized as early as 1928.[7] Since then, studies have shown the MIC to be a consistent finding in cadavers.[8] Furthermore, recent use of advanced imaging showed that it runs in a canal like the IAN canal but in smaller dimensions and is less corticated.[2,3]
The avoidance of surgical complications remains a challenging aspect in the field of surgery. With the increase in the number of operations in an area, the possibility of surgical complications increases. Therefore, the interforaminal region is one of the most vulnerable areas of surgeries in the oral cavity as it is considered a safe zone, and the bone quality and quantity are good.[9] Surgeries frequently done in this region are implant placement, osteotomy, bone graft, mini-screws, and mini plates.[10] However, there is a greater risk as the anterior mandible contains intra-bony vascular canals[11] as well as the MIC; the intra-bony extension of the inferior alveolar nerve mesial to the mental foramen.[6] This indistinct anatomic structure carries a major neurovascular bundle, the mandibular incisive nerve, and surrounding vessels, for innervation and vascular supply of the lower anterior dentition, i.e., incisors, canines, and first premolars.[12] Despite being considered an area of a superior risk-benefit ratio, the mandibular symphysis is prone to post-surgery complications, including unsuccessful osteointegration of implants, edema, and hematoma hemorrhage, sensory disturbance such as hypoesthesia and paresthesia.[9] Therefore, the position of the MIC must be kept in mind during the procedures. Several methods are used to detect the incisive nerve's presence and course, which includes following average measurements of the nerve course or tracing it radiographically.[9] Our aim in this study is to facilitate the surgeon's preoperative assessment by detecting the prevalence, location, and course of the MIC in patients attending King Saud University Dental Hospital.
Methodology
A retrospective study was conducted of 93 cone-beam computed tomography (CBCT) scans of patients aging from 18 to 50 years, which were taken from the archives of 2017 and 2018. The study subjects included 47 males and 43 females. Assessment of MIC was done in dentate mandibles in relation to root apex, inferior border of the mandible, buccal and lingual cortices. Our exclusion criteria include syndromic patients, mandibles with trauma, pathology, history of surgery in the area, edentulous, impacted canine or premolar, and blurred scans. Inclusion criteria are patients attending King Saud University Dental Hospital within the age of 18–50. All the CBCT scans were acquired with a Planmeca ProMax 3D Plus [Planmeca Co., Helsinki, Finland). The CBCT data were reconstructed using the Planmeca Romexis software. Ethical approval for this study was provided by the Ethical Committee of the Institutional Review Board (IRB) King Saud University College of Medicine, King Saud University Medical City, Riyadh, Saudi Arabia, on December 8, 2019 [Research project no. E-19-3704).
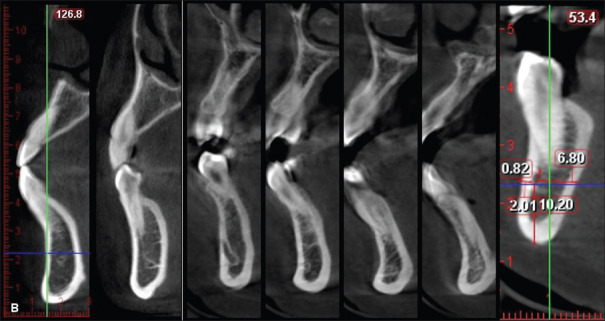
Images were reformatted from the sagittal sections to para-sagittal (modified sagittal view) sections at premolars, canines, lateral incisors, and central incisors [Figure 1]. In these para-sagittal sections, the MIC was located and measured to the distance of MIC to the tooth apex, to the inferior border of the mandible, to the buccal cortex, and to the lingual cortex.
Figure 1.
Para-sagittal sections of CBCT to detect MIC
Descriptive statistics (mean, standard deviation, and standard error) were used to express variables. Different statistical tests were conducted to assess the relation of the variables such as t-test and Chi-square. The sample size calculation was based on the previous studies like ours. The reliability of the measurements will be ensured by taking two different measures by two examiners and performing intraclass and interclass correlation coefficient tests. Significant differences will be identified at P < 0.05.
Results
The prevalence of MIC among the patients was found to be present in 90 patients (96.8%) of the total subjects and absent in three (3.2%) patients, showing an increased prevalence of MIC among the population [Figure 2 and Table 1].
Figure 2.
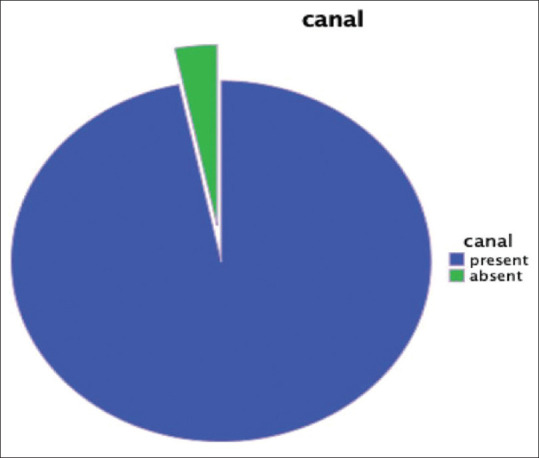
Prevalence of MIC
Table 1.
MIC prevalence
| MIC | n (%) |
|---|---|
| Present | 90 (96.8) |
| Absent | 3 (3.2) |
| Total | 93 |
Prevalence of MIC on the right and left side
When compared based on laterality, there was a slightly increased prevalence on the left side than the right side [Table 2].
Table 2.
MIC laterality prevalence
| MIC | Category | n (%) |
|---|---|---|
| Right | Present | 86 (92.47) |
| Absent | 7 (7.52) | |
| Left | Present | 89 (95.69) |
| Absent | 4(4.30) |
Prevalence of MIC among different genders
The gender-wise comparison of the MIC among the patients showed that the MIC was present in 47 male patients (97.9%) and 43 female patients (95.5%). The data concludes that there is a slightly increased prevalence of MIC among males compared to females [Table 3].
Table 3.
MIC gender prevalence
| MIC | Total | χ 2 | P | ||
|---|---|---|---|---|---|
|
| |||||
| Present | Absent | ||||
| Gender | |||||
| Male | 47 | 1 | 48 | 0.609 | 0.476 |
| Female | 43 | 2 | 45 | ||
| Total | 90 | 3 | 93 | ||
Using Chi-square test
The proximity of MIC to adjacent structures and the course of the canal
The average distance from the buccal cortex is 4.88 mm [Table 4], and the average distance from the lingual cortex is 5.54 mm [Table 5], which concludes that the neurovascular bundle is closer to the buccal cortex. The average distance from the mandible's inferior border is 9.94 mm [Table 6] and the average distance from the root apices in the different cross-sections is 7.67 mm [Table 7], which concludes that the MIC is closer to the root apices.
Table 4.
Distance of MIC to the buccal cortical plate
| Mean±SD | Minimum | Maximum | |
|---|---|---|---|
| Premolar | 4.23±3.10 | 1 | 9.5 |
| Canine | 4.76±3.7 | 1 | 9.5 |
| Lateral incisor | 5.14±3.84 | 2 | 10 |
| Central incisor | 5.41±4.11 | 2 | 10 |
Average: 4.88 mm
Table 5.
Distance of MIC to the lingual cortical plate
| Mean±SD | Minimum | Maximum | |
|---|---|---|---|
| Premolar | 5.18±3.39 | 2 | 10.5 |
| Canine | 5.08±3.76 | 1.5 | 10.5 |
| Lateral incisor | 5.84±3.62 | 2 | 10.5 |
| Central incisor | 6.09±3.70 | 2.5 | 10 |
Average: 5.54 mm
Table 6.
Distance of MIC to the inferior border of the mandible
| Mean±SD | Minimum | Maximum | |
|---|---|---|---|
| Premolar | 9.84±4.11 | 4 | 14.5 |
| Canine | 9.71±4.48 | 4.5 | 15.5 |
| Lateral incisor | 10.12±5.19 | 5 | 20.5 |
| Central incisor | 10.09±5.81 | 3 | 20 |
Average: 9.94 mm
Table 7.
Distance of MIC to the root apex
| Mean±SD | Minimum | Maximum | |
|---|---|---|---|
| Premolar | 6.55±5.77 | 0.5 | 15 |
| Canine | 5.85±6.24 | 0.5 | 16 |
| Lateral incisor | 8.48±6.80 | 2 | 18 |
| Central incisor | 9.82±7.43 | 3.5 | 20 |
Average: 7.67 mm
The age-wise comparison
The age-wise comparison of a mean distance of MIC to different surfaces in the different cross-sections showed that there is no correlation between the age and the course of the nerve except three weak relations. All showed no significant P value except three significant P values but with weak correlation below 40% which are the following:
Right central incisor apex: P value 0.016, Pearson's correlation 0.260 (<40%, weak relation)
Left lateral incisor apex: P value 0.008, Pearson's correlation 0.287 (<40%, weak positive relation)
Left central incisor apex: P value 0.016, Pearson's correlation 0.265 (<40%, weak positive relation).
Gender-wise comparison of MIC course
Independent t-test shows that 10 of the 32 variables have significant P values which are the following:
PM_R_Buccal: male is significantly higher than female by P values of 0.001
PM_R_Inferior: male is significantly higher than female by P values of 0.003
PM_R_Apex: male is significantly higher than female by P values of 0.003
Canine_R_inferior: male is significantly higher than female by P values of 0.013
Latrel_R_Buccal: male is significantly higher than female by P values of 0.009
Centeral_R_Buccal: male is significantly higher than female by P values of 0.030
PM_L_Buccal: male is significantly higher than female by P values of 0.008
PM_L_Infeior: male is significantly higher than female by P values of 0.000
Canine_L_Buccal: male is significantly higher than female by P values of 0.022
Latrel_L_Infeior: male is significantly higher than female by P values of 0.039.
Concluding, there is a difference between males and females in the anatomic course of the nerve since 31% of the variables were significantly different in measurements [Table 8].
Table 8.
Gender-wise comparison of MIC course
| Tooth | Tooth, side, surface | Gender | n | Mean | Sth. Deviation | P |
|---|---|---|---|---|---|---|
| Right premolar | PM_R_Buccal | Male | 44 | 4.5452 | 1.50894 | 0.001 |
| Female | 40 | 3.4725 | 1.39456 | |||
| PM_R_Lingual | Male | 43 | 5.1505 | 1.74951 | 0.621 | |
| Female | 39 | 5.3495 | 1.78377 | |||
| PM_R_Infeior | Male | 44 | 10.6211 | 1.83485 | 0.003 | |
| Female | 40 | 9.3948 | 1.86880 | |||
| PM_R_Apex | Male | 44 | 7.4293 | 2.96206 | 0.003 | |
| Female | 40 | 5.5828 | 2.46078 | |||
| Right canine | Canine_R_Buccal | Male | 44 | 5.2868 | 1.78548 | 0.004 |
| Female | 42 | 4.1607 | 1.73814 | |||
| Canine_R_Lingual | Male | 44 | 4.8925 | 1.74059 | 0.563 | |
| Female | 41 | 5.1205 | 1.87997 | |||
| Canine_R_Infeior | Male | 45 | 10.3231 | 2.75747 | 0.013 | |
| Female | 42 | 8.9821 | 2.10999 | |||
| Canine_R_Apex | Male | 45 | 6.1204 | 3.21478 | 0.789 | |
| Female | 42 | 5.9357 | 3.19990 | |||
| Right lateral incisor | Latrel_R_Buccal | Male | 44 | 5.7734 | 1.93036 | 0.009 |
| Female | 42 | 4.7250 | 1.67796 | |||
| Latrel_R_Lingual | Male | 43 | 5.3900 | 1.58028 | 0.450 | |
| Female | 41 | 5.6622 | 1.70814 | |||
| Latrel_R_Infeior | Male | 44 | 10.9198 | 3.00570 | 0.055 | |
| Female | 42 | 9.8207 | 2.12939 | |||
| Latrel_R_Apex | Male | 44 | 8.6793 | 3.39158 | 0.305 | |
| Female | 42 | 7.9021 | 3.59585 | |||
| Right central incisor | Centeral_R_Buccal | Male | 44 | 6.2798 | 2.10232 | 0.030 |
| Female | 42 | 5.2881 | 2.06196 | |||
| Centeral_R_Lingual | Male | 43 | 5.5377 | 1.54513 | 0.644 | |
| Female | 41 | 5.7032 | 1.72597 | |||
| Centeral_R_Infeior | Male | 43 | 10.8828 | 3.41918 | 0.155 | |
| Female | 42 | 9.9014 | 2.84546 | |||
| Centeral_R_Apex | Male | 44 | 9.8964 | 3.59683 | 0.183 | |
| Female | 42 | 8.8245 | 3.81374 | |||
| Left premolar | PM_L_Buccal | Male | 46 | 4.8498 | 1.58108 | 0.008 |
| Female | 37 | 3.9395 | 1.40349 | |||
| PM_L_Lingual | Male | 46 | 5.1215 | 1.54800 | 0.978 | |
| Female | 37 | 5.1316 | 1.76013 | |||
| PM_L_Infeior | Male | 46 | 10.3898 | 1.92001 | 0.000 | |
| Female | 37 | 8.7184 | 2.14554 | |||
| PM_L_Apex | Male | 46 | 6.9663 | 2.96790 | 0.154 | |
| Female | 37 | 6.0500 | 2.78068 | |||
| Left canine | Canine_L_Buccal | Male | 43 | 5.2460 | 1.96431 | 0.022 |
| Female | 40 | 4.3093 | 1.65518 | |||
| Canine_L_Lingual | Male | 42 | 5.2671 | 1.77317 | 0.639 | |
| Female | 40 | 5.0623 | 2.16187 | |||
| Canine_L_Infeior | Male | 43 | 10.0874 | 1.99554 | 0.101 | |
| Female | 40 | 9.3888 | 1.83474 | |||
| Canine_L_Apex | Male | 43 | 5.8942 | 3.33463 | 0.524 | |
| Female | 40 | 5.4633 | 2.74389 | |||
| Left lateral incisor | Latrel_L_Buccal | Male | 44 | 5.4250 | 2.13050 | 0.053 |
| Female | 40 | 4.5965 | 1.69437 | |||
| Latrel_L_Lingual | Male | 43 | 6.4830 | 1.82989 | 0.130 | |
| Female | 40 | 5.8228 | 2.10142 | |||
| Latrel_L_Infeior | Male | 44 | 10.4066 | 2.84084 | 0.039 | |
| Female | 40 | 9.2655 | 2.03413 | |||
| Latrel_L_Apex | Male | 44 | 8.9786 | 3.33324 | 0.370 | |
| Female | 40 | 8.3263 | 3.29035 | |||
| Left central incisor | Centeral_L_Buccal | Male | 42 | 5.2336 | 2.12708 | 0.373 |
| Female | 40 | 4.8390 | 1.83827 | |||
| Centeral_L_Lingual | Male | 41 | 6.8666 | 1.88930 | 0.200 | |
| Female | 40 | 6.2730 | 2.23100 | |||
| Centeral_L_Infeior | Male | 42 | 9.9505 | 2.83755 | 0.572 | |
| Female | 40 | 9.6173 | 2.45929 | |||
| Centeral_L_Apex | Male | 42 | 10.9579 | 4.08012 | 0.085 | |
| Female | 40 | 9.5460 | 3.18098 |
Discussion
The interforaminal region is a vulnerable area of surgeries in the oral cavity either for bone grafting surgeries or for implant placements or other indications. A detailed anatomical study of the region is significant to avoid complications. Many authors have studied the anatomy of MIC and the anterior mandibular region in either CBCT or panoramic radiographs. In the current study, MIC was examined in CBCT, which is the recommended way as attributed in the study of Pires CA et al.,[13] since the panoramic radiograph will have superimpositions of other structures that will obstruct proper visibility and examination.
The prevalence of MIC in this study was 96.8% of the population. This percentage is similar to the findings of different studies considering the results of Işık BK et al.[14] and Arzouman et al.[15] on CBCT scans, Pires et al.[13] on CBCT scans, and Jacobs et al.[16] on CT scans that were 97.5, 97, 83, and 93%, respectively. The prevalence was 100% in a study performed on cadavers by Mardinger O,[17] but the canal might be too small to detect on a CBCT.
In this study, the canal's average distance to the buccal cortex lingual cortex, inferior border of the mandible, and the tooth apex are 4.88, 5.54, 9.94, and 7.67 mm, respectively. Regarding the distance of the canal to the tooth apex, we can notice that there is a drop in the measurement in the cross-section taken at the position of the canine. This drop does not mean that the nerve there deviates more toward the inferior mandible, but it is associated with root length, which is the highest in the canine.
When analyzing the gender correlation with variables, measurements taken in all four cross-sections were higher in males. It can be justified by the mandibular anatomy difference between the males and females, where the mandibular linear length measurements were higher in the males.[18]
The age-wise comparison in this study showed no significant difference between the age group included in our study. On the other hand, a study by Ayesha et al.[19] showed that there is a difference between the age groups to buccal and lingual measurement. Therefore, the literature does not give us a conclusion regarding the age-nerve location correlation because of a lack of studies that examined this correlation.
Conclusion
It can be concluded that the detection of MIC presence and location using CBCT should be earnestly considered for surgical procedures that are intended to be done in the interforaminal region. By strictly adhering to the surgical protocol, the risk of transient or persistent tooth sensitivity loss can be minimized.[10] Therefore, these recent measurements will create safe margins for surgeons. In conclusion, a more significant number of studies on MIC are needed, specifically the correlation of its location and age, which can help to elucidate the boundaries for more precise and shielded perimeters.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Polland K, Munro S, Reford G, Lockhart A, Logan G, Brocklebank L, et al. The mandibular canal of the edentulous jaw. Clin Anat. 2001;14:445–52. doi: 10.1002/ca.1080. [DOI] [PubMed] [Google Scholar]
- 2.Uchida Y, Noguchi N, Goto M, Yamashita Y, Hanihara T, Takamori H, et al. Measurement of anterior loop length for the mandibular canal and diameter of the mandibular incisive canal to avoid nerve damage when installing endosseous implants in the interforaminal region: A second attempt introducing cone beam computed tomography. J Oral Maxillofac Surg. 2009;67:744–50. doi: 10.1016/j.joms.2008.05.352. [DOI] [PubMed] [Google Scholar]
- 3.Rosa M, Sotto-Maior B, De Carvalho Machado V, Francischone C. Retrospective study of the anterior loop of the inferior alveolar nerve and the incisive canal using cone beam computed tomography. Int J Oral Maxillofac Implants. 2013;28:388–92. doi: 10.11607/jomi.2648. [DOI] [PubMed] [Google Scholar]
- 4.Kilic E, Doganay S, Ulu M, Çelebi N, Yikilmaz A, Alkan A. Determination of lingual vascular canals in the interforaminal region before implant surgery to prevent life-threatening bleeding complications? Clin Oral Implants Res. 2012;25:e90–3. doi: 10.1111/clr.12065. doi: 10.1111/ clr. 12065. [DOI] [PubMed] [Google Scholar]
- 5.Makris N, Stamatakis H, Syriopoulos K, Tsiklakis K, Van Der Stelt P. Evaluation of the visibility and the course of the mandibular incisive canal and the lingual foramen using cone-beam computed tomography. Clin Oral Implants Res. 2010;21:766–71. doi: 10.1111/j.1600-0501.2009.01903.x. [DOI] [PubMed] [Google Scholar]
- 6.Mardinger O, Chaushu G, Arensburg B, Taicher S, Kaffe I. Anatomic and radiologic course of the mandibular incisive canal. Surg Radiol Anat. 2000;22:157–61. doi: 10.1007/s00276-000-0157-5. [DOI] [PubMed] [Google Scholar]
- 7.Purnell A. Eosinophilic granuloma presenting as inferior alveolar nerve anaesthesia. Br Dent J. 1988;164:355–6. doi: 10.1038/sj.bdj.4806454. [DOI] [PubMed] [Google Scholar]
- 8.Mraiwa N, Jacobs R, Moerman P, Lambrichts I, Van Steenberghe D, Quirynen M. Presence and course of the incisive canal in the human mandibular interforaminal region: Two-dimensional imaging versus anatomical observations. Surg Radiol Anat. 2003;25:416–23. doi: 10.1007/s00276-003-0152-8. [DOI] [PubMed] [Google Scholar]
- 9.Ramesh AS, Rijesh K, Sharma A, Prakash R, Kumar A, Karthik The prevalence of mandibular incisive nerve canal and to evaluate its average location and dimension in Indian population. J Pharm Bioallied Sci. 2015;7(Suppl 2):S594–S596. doi: 10.4103/0975-7406.163559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pommer B, Tepper G, Gahleitner A, Zechner W, Watzek G. New safety margins for chin bone harvesting based on the course of the mandibular incisive canal in CT. Clin Oral Implants Res. 2008;19:1312–6. doi: 10.1111/j.1600-0501.2008.01590.x. [DOI] [PubMed] [Google Scholar]
- 11.Gahleitner A, Hofschneider U, Tepper G, Pretterklieber M, Schick S, Zauza K, et al. Lingual vascular canals of the mandible: evaluation with dental CT. Radiology. 2001;220:186–9. doi: 10.1148/radiology.220.1.r01jl05186. [DOI] [PubMed] [Google Scholar]
- 12.Strong S. Success of unsplinted implant-retained removable mandibular and maxillary overdentures: A retrospective study of consecutive cases. Int J Periodontics Restorative Dent. 2015;35:533–9. doi: 10.11607/prd.2233. [DOI] [PubMed] [Google Scholar]
- 13.Pires C, Bissada N, Becker J, Kanawati A, Landers M. Mandibular incisive canal: Cone beam computed tomography. Clin Implant Dent Relat Res. 2009;14:67–73. doi: 10.1111/j.1708-8208.2009.00228.x. [DOI] [PubMed] [Google Scholar]
- 14.Işık BK, Taşsöker M, Menziletoğlu D, Şener S, Esen A. Assessment of the mandibular incisive canal by panoramic radiograph and cone-beam computed tomography. Selcuk Dent J. 2017;4:17–22. [Google Scholar]
- 15.Arzouman MJ, Otis L, Kipnis V, Levine D. Observations of the anterior loop of the inferior alveolar canal. Int J Oral Maxillofac Implants. 1993;8:295–300. [PubMed] [Google Scholar]
- 16.Jacobs R, Mraiwa N, Vansteenberghe D, Gijbels F, Quirynen M. Appearance, location, course, and morphology of the mandibular incisive canal: An assessment on spiral CT scan. Dentomaxillofac Radiol. 2002;31:322–7. doi: 10.1038/sj.dmfr.4600719. [DOI] [PubMed] [Google Scholar]
- 17.Mardinger O, Chaushu G, Arensburg B, Taicher S, Kaffe I. Anterior loop of the mental canal. Implant Dent. 2000;9:120–5. doi: 10.1097/00008505-200009020-00003. [DOI] [PubMed] [Google Scholar]
- 18.Direk F, Uysal I, Kivrak A, Unver Dogan N, Fazliogullari Z, Karabulut A. Reevaluation of mandibular morphometry according to age, gender, and side. J Craniofac Surg. 2018;29:1054–9. doi: 10.1097/SCS.0000000000004293. [DOI] [PubMed] [Google Scholar]
- 19.Ayesha R, Pachipulusu B, Govindaraju P. Assessment of prevalence and position of mandibular incisive canal: A cone beam computed tomography study. Tzu Chi Med J. 2020;32:205–10. doi: 10.4103/tcmj.tcmj_76_19. [DOI] [PMC free article] [PubMed] [Google Scholar]