Sirs:
According to the recent analysis of the US Center for Disease Control (CDC), a number of 56–69 cases of myocarditis per 1 million mRNA-vaccine doses have to be expected in the age group of 12–17 years in males and of only 3–4 cases in the age group 30 years [1], the latter number also corresponding to the latest report from August 2021 of the responsible German authority (Federal Institute for Vaccines and Biomedicines, Paul-Ehrlich-Institut) [2]. The estimated number of deaths prevented by COVID-19 vaccine in the age group 30 years is 700, thus proving the overwhelming net benefit of the vaccination. The US vaccine safety passive monitoring system reported as to July 22, 2021 n = 497 patients meeting the CDC’s case definition of myocarditis, but the median age was 19 years only [3].
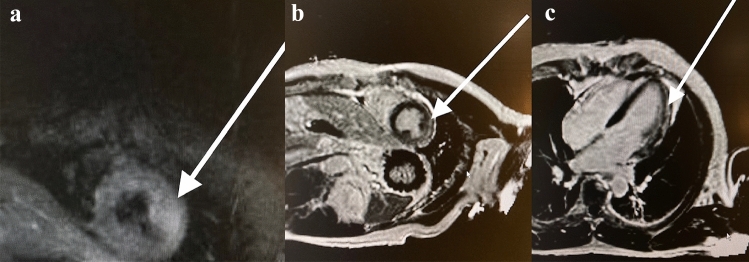
Against this background, we report on a 60-year-old man with normal body mass index (189 cm, 84 kg) and empty cardiovascular anamnesis despite a WHO degree I arterial hypertension. On July 1st, 2021, he received his 2nd dose of mRNA-vaccine (mRNA-1273, Moderna), and developed a typical vaccination reaction with 39 °C fever and dizziness. About 24 h after vaccination, he had palpitations and after 36 h, he fainted and lost consciousness for some seconds. He was admitted to our hospital where the ECG showed sinus rhythm and no signs of ischemia. Fast track echocardiography was normal, but the troponin T (Roche Cardiac T cobas h232) at admission was elevated to 160 ng/L (cutoff 50 ng/L) and together with the preceding syncope an urgent coronary angiography was indicated. A coronary heart disease was excluded this way. A cardiac magnet resonance imaging (CMRI) was performed next day (80 h after vaccination) and showed a focal edema of anterolateral medial wall in the T2 sequences (Fig. 1a) and a corresponding subepicardial late enhancement in the short axis and four-chamber view (Fig. 1b, c), both consistent with the diagnosis of a myocarditis. The patient remained free of symptoms, the troponin declined to the normal range and he was discharged at day 5. The echocardiography a week and a month later remained normal, so that we presume a complete recovery.
Fig. 1.
a Cardiac MRI, T2 sequence, arrow indicating focal edema anterolateral medial (criterion 1 in ESC definition). b Short-axis view showing subepicardial gadolinium late enhancement anterolateral medial (criterion 3 in ESC definition [4]). c Corresponding four-chamber view
Our patient presented a typical pattern of transient clinical symptoms and MRI images of myocarditis in a very close and suggestive time relation; however, a causality between the mRNA vaccination and the myocarditis has not been proven. The CDC case definition of confirmed myocarditis [1] is fully met by (a) palpitations and syncope ( 1 clinical symptoms), (b) CMRI findings consistent with myocarditis [4], (c) troponin level above upper limit and (d) exclusion of other causes. In contrast to the increasing number of reported cases of myocarditis after mRNA vaccination, our patient was 60 years old, and in this age group, no case of vaccine-related myocarditis has been reported to the responsible German authority up to now [2]. We classified the patient in a low-risk group because of his rapid and complete clinical recovery, the return of troponin into normal values within 24 h and the normal LVEF in both echocardiography and CMRI. We, therefore, refrained from both endomyocardial biopsy and wearable defibrillator vest. Until today, there are no cases with proven ventricular arrhythmias due to vaccine-induced myocarditis. The only published case with cardiac arrest associated with mRNA1237 was caused by pericardial tamponade [5]. A similar benign course of myocarditis has been reported in a large cohort within the U.S. military health system, summing up to 23 cases per 2.9 million vaccine doses [6]. Another series of 6 case reports from Israel included 5 patients between 16 and 29 years, which did not need a coronary angiography because of the younger age [7]. The majority of cases occurred within 6 days after 2nd vaccination [2]. Both the mRNA-1273 (SpikeVax, Moderna) and the BNT162b2 (Comirnaty, BioNTech-Pfizer) vaccine could induce a myocarditis [8, 9], caused perhaps by a hypothesized molecular mimicry between the spike protein of SARS-CoV2 and self-antigens [10]. Furthermore, “dysregulated immune response to mRNA, activation of immunological pathways, and dysregulated cytokine expression” have been proposed as mechanisms [10]. To our knowledge, nearly all reported patients recovered completely and one must keep in mind that there is a significantly higher risk of myocarditis from COVID-19 infection itself compared to COVID-19 vaccination [10–12]. The latest report of the German Paul-Ehrlich-Institut from August 19, 2021 listed 393 cases of peri- or myocarditis per 69 million doses of BNT165b2 (BioNTech-Pfizer) and 49 cases per 8.5 million doses of mRNA-1273 (Moderna) [2]. This gave reason to an updated product information and a red-hand-letter of the responsible authority which indicate explicitly on this complication. Our short report also intends to alert physicians and authorities to this rare side effect of mRNA vaccination.
Acknowledgements
The authors wish to thank their patient for his consent to publish his case and the MRI images. The written consent formulation has been transferred to the journal.
Abbreviations
- BNT165b2
BioNTech-Pfizer COVID-19 vaccine
- CDC
Center for Disease Control of the USA
- CMRI
Cardiac magnetic resonance imaging
- mRNA-1273
Moderna COVID-19 vaccine
- PEI
Paul-Ehrlich-Institut
- WHO
World Health Organization
Author contributions
DH and MNU wrote the manuscript and treated the patient; AL performed the cardiac; MRI, DH and IA treated the patient; and DH, MNU, AL and IA reviewed the manuscript.
Funding
None.
Declarations
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Gargano JW, Wallace M, Hadler SC, Langley G, Su JR, Oster ME, Broder KR, Gee J, Weintraub E, Shimabukuro T, Scobie HM, Moulia D, Markowitz LE, Wharton M, McNally VV, Romero JR, Keipp Talbot H, Lee GM, Daley MF, Oliver SE. Use of mRNA COVID-19 vaccine after reports of myocarditis among vaccine recipients: update from the advisory committee on immunization practices—united states. MMWR Morb Mortal Wkly Rep. 2021;70(27):977–982. doi: 10.15585/mmwr.mm7027e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sicherheitsbericht. Verdachtsfälle von Nebenwirkungen und Impfkomplikationen nach Impfung zum Schutz vor COVID-19 seit Beginn der Impfkampagne am 27.12.2020 bis zum 31.7.2021. Tabelle 5 Seite 17. http://pei.de/dossiers/sicherheitsberichte
- 3.Rosenblum HG, Hadler SC, Moulia D, Shimabukuro TT, Su JR, Tepper NK, Ess KC, Jane Woo E, Mba-Jonas A, Alimchandani M, Nair N, Klein NP, Hanson KE, Markowitz LE, Wharton M, McNally VV, Romero JR, Keipp Talbot H, Lee GM, Daley MF, Mbaeyi SA, Oliver SE. Use of COVID-19 vaccines after reports of adverse events among adult recipients of janssen (johnson & johnson) and mRNA COVID-19 vaccines (pfizer-BioNTech and moderna): update from the advisory committee on immunization practices—united states. MMWR Morb Mortal Wkly Rep. 2021;70(32):1094–1099. doi: 10.15585/mmwr.mm7032e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Caforio ALP, Pankuweit S, Arbustini E, Basso C, Gimeno-Blanes J, Felix SB, Fu M, Helio T, Heymans S, Jahns R, Klingel K, Linhart A, Maisch B, McKenna W, Mogensen J, Pinto YM, Ristic A, Schultheiss H-P, Seggewiss H, Tavazzi L, Thiene G, Yilmaz A, Charron P, Elliott PM. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the european society of cardiology working group on myocardial and pericardial diseases. Eur Heart J. 2013;34(33):2636–2648. doi: 10.1093/eurheartj/eht210. [DOI] [PubMed] [Google Scholar]
- 5.Khogali F, Abdelrahman R. Unusual presentation of acute perimyocarditis following SARS-COV-2 mRNA-1237 moderna vaccination. Cureus. 2021;13(7):e16590. doi: 10.7759/cureus.16590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Montgomery J, Ryan M, Engler R, Hoffman D, McClenathan B, Collins L, Loran D, Hrncir D, Herring K, Platzer M, Adams N, Sanou A, Cooper LT. Myocarditis following immunization with mRNA COVID-19 vaccines in members of the US military. JAMA Cardiol. 2021;6(10):1202–1206. doi: 10.1001/jamacardio.2021.2833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mouch SA, Roguin A, Hellou E, Ishai A, Shoshan U, Mahamid L, Zoabi M, Aisman M, Goldschmid N, Yanay NB. Myocarditis following COVID-19 mRNA vaccination. Vaccine. 2021;39(29):3790–3793. doi: 10.1016/j.vaccine.2021.05.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim HW, Jenista ER, Wendell DC, Azevedo CF, Campbell MJ, Darty SN, Parker MA, Kim RJ. Patients with acute myocarditis following mRNA COVID-19 vaccination. JAMA Cardiol. 2021;6(10):1196–1201. doi: 10.1001/jamacardio.2021.2828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Albert E, Aurigemma G, Saucedo J, Gerson DS. Myocarditis following COVID-19 vaccination. Radiol Case Rep. 2021;16(8):2142–2145. doi: 10.1016/j.radcr.2021.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bozkurt B, Kamat I, Hotez PJ. Myocarditis with COVID-19 mRNA vaccines. Circul. 2021;144(6):471–484. doi: 10.1161/CIRCULATIONAHA.121.056135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Imazio M, Klingel K, Kindermann I, Brucato A, De Rosa FG, Adler Y, De Ferrari GM. COVID-19 pandemic and troponin: indirect myocardial injury, myocardial inflammation or myocarditis? Heart. 2020;106(15):1127–1131. doi: 10.1136/heartjnl-2020-317186. [DOI] [PubMed] [Google Scholar]
- 12.Breitbart P, Koch A, Schmidt M, Magedanz A, Lindhoff-Last E, Voigtländer T, Schmermund A, Mehta RH, Eggebrecht H. Clinical and cardiac magnetic resonance findings in post-COVID patients referred for suspected myocarditis. Clin Res Cardiol. 2021;26:1–9. doi: 10.1007/s00392-021-01929-5. [DOI] [PMC free article] [PubMed] [Google Scholar]