Abstract
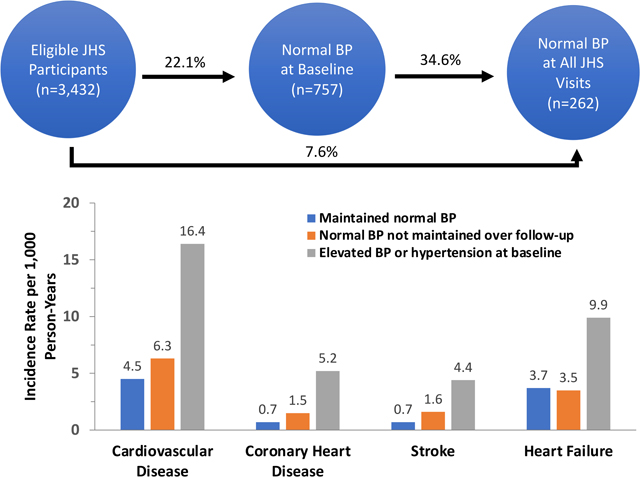
Although mean blood pressure (BP) increases with age, there may be a subset of individuals whose BP does not increase with age. Characterizing the population that maintains normal BP could inform hypertension prevention efforts. We determined the proportion of Jackson Heart Study participants that maintained normal BP at 3 visits over a median of 8 years. Normal BP was defined as systolic BP <120 mm Hg and diastolic BP <80 mm Hg without antihypertensive medication. We identified lifestyle and psychosocial factors associated with maintaining normal BP and calculated the incidence rate for cardiovascular disease (CVD). Overall, 757 of 3,432 participants (22.1%) had normal BP at baseline, and 262 of these participants (34.6%) maintained normal BP. Among participants with normal BP at baseline, normal body mass index (BMI; Risk Ratio [RR] 1.37; 95% confidence interval [CI]: 1.08–1.75), ideal physical activity (RR 1.28, 95%CI: 0.99–1.65) and never smoking (RR 1.48; 95%CI: 0.99–2.20) at baseline were associated with maintaining normal BP. Maintaining normal BMI (RR 1.42; 95%CI: 1.10–1.84) and ideal physical activity (RR 1.51; 95%CI: 1.18–1.94) at all study visits were associated with maintaining normal BP. The CVD incidence rate was 4.5, 6.3, and 16.4 per 1,000 person-years among participants who maintained normal BP, had normal BP at baseline but did not maintain normal BP and had elevated BP or hypertension at baseline, respectively, over 5.9 years of follow-up. These data suggest that maintaining normal BMI and ideal physical activity are potential approaches for African American adults to maintain normal BP.
Keywords: blood pressure, cardiovascular health, health behaviors, psychosocial factors, cardiovascular disease, primordial prevention
Graphical Abstract
High blood pressure (BP) is a major modifiable risk factor for cardiovascular disease (CVD) and mortality.1 The mean BP for the US population increases with age, with rises in BP occurring as early as childhood.2 Studies conducted among non-industrialized populations have reported relatively stable mean BP levels from 20 to 60 years of age, suggesting that the age-related increases in BP that occur in the US may not be an inevitable part of aging.3, 4 Even in the US, prior studies have reported that a subset of adults experience only minimal BP increases as they age.5, 6
On average, African Americans develop hypertension at younger ages and have a higher prevalence of hypertension compared with other racial/ethnic groups in the US.2, 7 The higher prevalence of hypertension among African Americans compared with whites may contribute to their higher risk for CVD events.8, 9 Efforts to reduce racial/ethnic BP disparities have predominately focused on improving BP control among adults with hypertension.7 Primordial prevention efforts that support maintaining normal BP across the life course could prevent the development of racial/ethnic disparities in hypertension. Lifestyle and psychosocial factors have been associated with the risk for hypertension,10–13 but little is known about the extent to which levels of these factors may protect against increases in BP over the life course, particularly among African Americans.
The objectives of this study were to determine the proportion of African Americans that maintain normal BP as they age, identify lifestyle and psychosocial factors that are associated with maintaining normal BP, and determine the rate of incident CVD among African Americans who maintain normal BP. To accomplish these goals, we analyzed data from the Jackson Heart Study (JHS).
Methods
Study population
Requests to access the data set from qualified researchers trained in human subject research protocols may be sent to the JHS publications committee at https://www.jacksonheartstudy.org. The JHS is a prospective, community-based, cohort study designed to investigate the etiology of CVD in African Americans.14 Between 2000 and 2004, the JHS enrolled 5,306 non-institutionalized African Americans ≥ 21 years of age from the Jackson, MS metropolitan area.14 Data were collected during a baseline examination in 2000–2004 (visit 1) and during two follow-up examinations in 2005–2008 (visit 2) and 2009–2013 (visit 3).14 We restricted the current analysis to JHS participants who completed all three examinations (n = 3,568). We excluded participants who were missing data on BP or antihypertensive medication use at any visit (n = 136). After these exclusions were applied, we included 3,432 participants in the analysis for identifying the proportion of participants who maintained normal BP and the lifestyle and psychosocial factors associated with maintaining normal BP. For determining CVD incidence rates, we further excluded participants who had a history of CVD at baseline (n = 284), did not provide consent for CVD event follow-up (n = 104) or had an adjudicated CVD event between visits 1 and 3 (n = 251). The JHS was approved by the institutional review boards of all participating institutions and all participants provided written informed consent at each study visit.14
Lifestyle factors
Height and weight were measured by trained technicians at each visit and were used to calculate body mass index (BMI, kg/m2). BMI was categorized as normal (<25 kg/m2), overweight (25 to < 30 kg/m2) or obese (BMI ≥ 30 kg/m2).15 Physical activity was assessed at visits 1 and 3 using a 30-item modified Baecke questionnaire16 and categorized into ideal, intermediate or poor levels as defined by the American Heart Association’s (AHA) Life’s Simple 7 metric (Table S1).15 Diet was assessed at baseline using a 158-item food frequency questionnaire with a healthy diet being defined as having ≥ 2 healthy diet components, based on the AHA’s Life’s Simple 7 metric.15 Alcohol consumption and cigarette smoking were assessed by self-report at visits 1 and 3 and categorized as ‘any’ or ‘no consumption’ for alcohol use and ‘ever’ or ‘never’ use for smoking. Maintenance of normal BMI, ideal physical activity, no alcohol consumption and never smoking was defined as having ideal levels of each factor at all visits at which they were assessed.
Psychosocial factors
Five psychosocial measures were included in this analysis: weekly stress, anger expression, daily discrimination, social support, and depressive symptoms. Weekly stress was assessed at baseline using the Weekly Stress Inventory (WSI).17 Total WSI scores were categorized into tertiles based on the distribution among eligible study participants. At baseline and visit 3, the Spielberger Trait Anger scale with two 8-item subscales, anger-in and anger-out, was used to assess participants’ reactions when feeling angry and each subscale was categorized into tertiles.17 At baseline and visit 3, daily discrimination was assessed by responses to 9 statements that captured common experiences of unfair treatment on a day-to-day basis.17 Responses were compiled into a summary score and categorized into tertiles.18 At basline, the Interpersonal Support Evaluation List (ISEL) was used to assess perceived availability of social support, which was categorized into tertiles.19 Depressive symptoms during the preceding week were measured using the 20-item Center for Epidemiological Studies Depression Scale (CES-D) at basline.17 Participants with CES-D scores ≥ 16 were categorized as having high depressive symptoms.20 Maintenance of ideal anger-in, anger-out, and daily discrimination were defined as having the lowest tertile of each factor at all visits at which they were assessed.
Blood pressure
At each study visit, trained technicians measured participants’ BP while they were seated after a 5-minute rest following a standardized protocol. Two BP measurements were taken at each visit, one minute apart, with an appropriately sized cuff on the participants’ right arm using a random-zero sphygmomanometer (Hawksley and Sons, Ltd, London, UK) at visits 1 and 2, and a semi-automatic oscillatory device (Omron HEM-907XL, Omron Healthcare Inc., Lake Forest, IL) at visit 3. Based on the results of a BP comparability study, all BP measurements taken with the random-zero sphygmomanometer were calibrated to the semi-automatic oscillatory device using robust regression.21 The two BP measurements taken at each visit were averaged. Normal BP was defined as systolic BP (SBP) < 120 mm Hg and diastolic BP (DBP) < 80 mm Hg without the use of antihypertensive medication. Elevated BP was defined as SBP between 120 and 129 mm Hg with DBP < 80 mm Hg without the use of antihypertensive medication. Hypertension was defined as SBP ≥ 130 mm Hg and/or DBP ≥80 mm Hg and/or the use of antihypertensive medication.22
Incident cardiovascular disease and all-cause mortality
Among participants without a history of CVD at baseline or an adjudicated event between baseline and visit 3, incident CVD was defined by the occurrence of coronary heart disease (CHD; non-fatal myocardial infarction or CHD death), stroke or heart failure hospitalization after JHS visit 3. The occurrence of CVD events was ascertained during annual telephone follow-up interviews with participants or proxy respondents. The interviews were conducted by trained staff and medical records for potential events were retrieved and adjudicated.23 If the JHS participant was deceased, physicians, medical examiners, coroners, and next of kin were contacted to obtain additional details about the events surrounding the death and death certificates were reviewed to identify CVD events.23 Participants were censored on the date of their first CVD event after visit 3, their last contact with the study, their death, or December 31, 2016, the last date for which outcomes were adjudicated, whichever occurred first.
Statistical analysis
The percentage of participants with normal BP at baseline was calculated, with all included study participants used as the denominator. Among participants with normal BP at baseline, we calculated the percentage who maintained normal BP at all three visits and summary statistics for characteristics of participants who maintained and did not maintain normal BP over follow-up. We also calculated the proportion of participants who maintained normal BP by levels of each lifestyle and psychosocial factor. We calculated risk ratios (RR) for maintaining normal BP associated with lifestyle and psychosocial factors using three multivariable Poisson regression models with robust standard error estimates. Model 1 included adjustment for age, sex and family income (<$25,000/year, ≥$25,000/year) at baseline. Model 2 included adjustment for the variables in model 1 and diet, physical activity, BMI, alcohol consumption and smoking at baseline. Model 3 included adjustment for the variables in model 2 and weekly stress, anger in, anger out, depressive symptoms, social support, and everyday discrimination at baseline. As BMI, physical activity, alcohol consumption, smoking, anger-in, anger-out, and discrimination were re-assessed at visits 2 and/or 3, we estimated the proportion of participants who maintained ideal levels of each of these factors across all visits at which they were assessed. We estimated the association between maintenance of ideal levels of each characteristic and maintenance of normal BP using Poisson regression models as described above. We conducted a sensitivity analysis where the outcome of maintaining normal BP was defined as having the same or lower SBP and DBP at visits 2 and 3 compared to baseline. We estimated the association between lifestyle and psychosocial characteristics and maintaining normal BP with no increases in SBP and DBP using Poisson regression models as described above.
After excluding participants with a history of CVD at baseline and those who had an adjudicated CVD event between baseline and visit 3, we calculated the crude incidence rates (IR) for the composite outcome of CVD, its individual components (CHD, stroke and heart failure) and all-cause mortality among participants who maintained normal BP. For comparison, we calculated the IR for CVD and all-cause mortality among participants who did not maintain normal BP across the three visits and among those with elevated BP or hypertension at baseline. Statistical significance was defined by a 2-sided P-value <0.05.
The number and percentage of participants with missing data for each variable are reported in Table S2. Missing data were accounted for by using multiple imputation with chained equations and 10 imputations.24 The fully conditional specifications regression algorithms were used for imputing continuous variables and logistic and discriminant algorithms were used for binary and categorical variables, respectively. All statistical analyses were performed with SAS 9.4 software (SAS Institute, Cary, NC).
Results
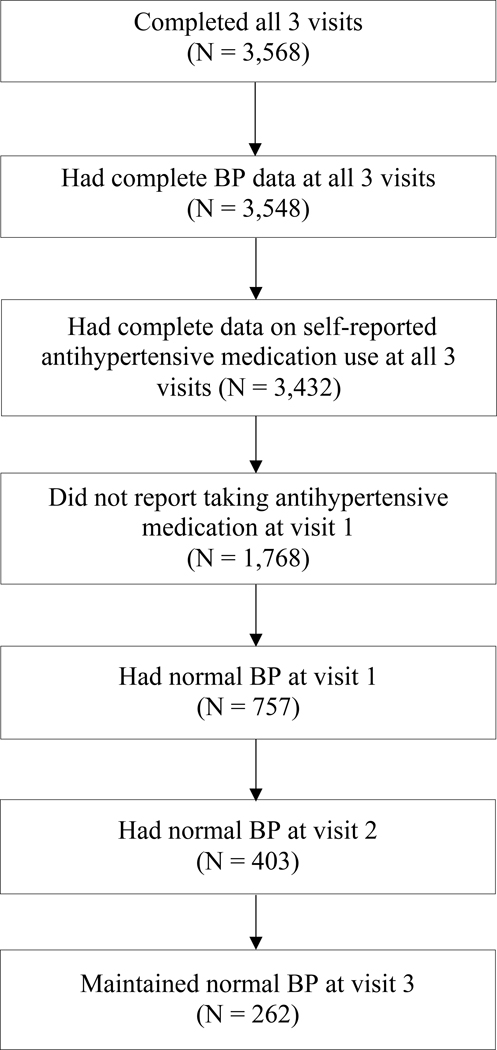
Among 3,432 JHS participants with BP and antihypertensive medication data at all 3 study visits, 757 (22.1%) participants had normal BP at baseline (Figure 1). Over a median of 8.0 years (25th–75th percentile: 7.3–8.2) of follow up, 262 of the 757 participants (34.6%) maintained normal BP at both follow-up examinations. Among participants with normal BP at baseline, those who maintained normal BP over follow up were younger, less likely to have an income < $25,000 at visit 3 and had a lower SBP at baseline compared to those who did not maintain normal BP (Table 1, Table S3). A larger proportion of participants who had normal BMI and ideal level of physical activity at baseline (43.3% and 40.9%, respectively) maintained normal BP compared to those with intermediate (32.7% and 34.8%, respectively) and poor (31.8% and 30.4%, respectively) levels (Table S4).
Figure 1:
Flow chart depicting the number of Jackson Heart Study participants included in the analysis and the number of participants who maintained normal blood pressure over follow-up
Abbreviations: BP - blood pressure
Table 1:
Characteristics of participants with normal blood pressure at baseline, overall, and among those who maintained and did not maintain normal blood pressure during follow-up.
| Maintained normal blood pressure | |||
|---|---|---|---|
| Characteristics | Overall (N = 757) |
Yes (N = 262) |
No (N = 495) |
| Socio-demographic characteristics | |||
| Age at visit 1, years | 46.4 (11.1) | 43.8 (10.9) | 47.7 (11.1) |
| Age at visit 2, years | 51.1 (11.1) | 48.5 (10.8) | 52.4 (11.0) |
| Age at visit 3, years | 54.4 (11.1) | 51.8 (10.9) | 55.8 (11.0) |
| Male | 33.4 | 33.2 | 33.5 |
| Income less than $25,000 at visit 1 | 25.0 | 26.5 | 24.2 |
| Income less than $25,000 at visit 3 | 23.9 | 19.1 | 26.5 |
| Systolic blood pressure, mm Hg | |||
| Visit 1 | 110.1 (6.6) | 107.4 (7.0) | 111.5 (5.9) |
| Visit 2 | 116.8 (12.5) | 107.7 (7.2) | 121.5 (12.1) |
| Visit 3 | 118.6 (13.9) | 108.2 (7.1) | 124.1 (13.5) |
| Diastolic blood pressure, mm Hg | |||
| Visit 1 | 70.2 (5.8) | 68.9 (5.5) | 70.9 (5.9) |
| Visit 2 | 71.8 (8.5) | 67.2 (6.0) | 74.2 (8.6) |
| Visit 3 | 73.7 (9.6) | 68.3 (6.0) | 76.6 (9.9) |
| Lifestyle factors | |||
| Body mass index at visit 1 | |||
| Obese | 41.2 | 37.8 | 43.0 |
| Overweight | 37.5 | 35.5 | 38.6 |
| Normal | 21.3 | 26.7 | 18.4 |
| Body mass index at visit 2 | |||
| Obese | 47.0 | 44.7 | 48.2 |
| Overweight | 37.7 | 34.4 | 39.5 |
| Normal | 15.3 | 21.0 | 12.3 |
| Body mass index at visit 3 | |||
| Obese | 50.0 | 45.4 | 52.4 |
| Overweight | 34.6 | 35.5 | 34.1 |
| Normal | 15.4 | 19.1 | 13.5 |
| Physical activity at visit 1 | |||
| Poor | 38.3 | 33.7 | 40.8 |
| Intermediate | 37.3 | 37.6 | 37.2 |
| Ideal | 24.3 | 28.7 | 22.0 |
| Physical activity at visit 3 | |||
| Poor | 35.9 | 33.5 | 37.1 |
| Intermediate | 35.8 | 36.1 | 35.7 |
| Ideal | 28.3 | 30.3 | 27.2 |
| Healthy diet at visit 1 | 38.9 | 36.1 | 40.3 |
| No alcohol consumption at visit 1 | 44.7 | 44.0 | 45.2 |
| No alcohol consumption at visit 3 | 44.3 | 42.7 | 45.1 |
| Never smoker at visit 1 | 87.6 | 85.6 | 91.3 |
| Never smoker at visit 3 | 89.6 | 88.6 | 91.5 |
| Psychosocial factors | |||
| Weekly stress at visit 1 | |||
| High | 33.3 | 32.1 | 34.0 |
| Moderate | 33.3 | 35.9 | 32.0 |
| Low | 33.3 | 32.0 | 34.0 |
| Anger in at visit 1 | |||
| High | 29.8 | 28.5 | 30.5 |
| Moderate | 34.3 | 36.7 | 33.0 |
| Low | 35.9 | 34.8 | 36.5 |
| Anger out at visit 1 | |||
| High | 33.3 | 30.2 | 35.0 |
| Moderate | 29.9 | 30.4 | 29.7 |
| Low | 36.8 | 39.4 | 35.3 |
| Anger in at visit 3 | |||
| High | 31.7 | 30.6 | 32.3 |
| Moderate | 35.5 | 37.0 | 34.8 |
| Low | 32.7 | 32.4 | 32.9 |
| Anger out at visit 3 | |||
| High | 37.5 | 38.3 | 37.0 |
| Moderate | 27.4 | 31.0 | 25.5 |
| Low | 35.2 | 30.7 | 37.5 |
| Daily discrimination score at visit 1 | |||
| High | 32.9 | 31.8 | 33.5 |
| Moderate | 34.7 | 37.5 | 33.3 |
| Low | 32.4 | 30.7 | 33.3 |
| Daily discrimination score at visit 3 | |||
| High | 32.7 | 31.5 | 33.3 |
| Moderate | 33.4 | 34.3 | 32.9 |
| Low | 34.0 | 34.2 | 33.8 |
| Social support: score at visit 1 | |||
| Low | 33.3 | 34.3 | 32.8 |
| Moderate | 31.5 | 33.3 | 30.6 |
| High | 35.1 | 32.4 | 36.6 |
| Depression score <16 at visit 1 | 78.4 | 78.5 | 78.4 |
Table values are mean (standard deviation) for continuous variables and percent for categorical variables.
Lifestyle and psychosocial factors associated with maintaining normal BP
After adjustment for sociodemographic, lifestyle, and psychosocial factors (Model 3), normal BMI (RR 1.39; 95% CI: 1.09–1.76), ideal physical activity levels (RR 1.25; 95% CI: 0.97–1.60) and never smoking (RR 1.48; 95% CI: 0.99 – 2.20) at baseline were associated with maintaining normal BP over follow-up (Table 2). There was no evidence of an association between healthy diet, no alcohol consumption, and ideal levels of psychosocial factors at baseline and maintaining normal BP.
Table 2:
Association of baseline lifestyle and psychosocial risk factors with maintaining normal blood pressure.
| Maintained normal blood pressure Risk ratios (95% confidence intervals) | |||
|---|---|---|---|
| Variables at baseline | Model 1 | Model 2 | Model 3 |
| Lifestyle factors | |||
| Body mass index | |||
| Obese | 1 (ref) | 1 (ref) | 1 (ref) |
| Overweight | 1.11 (0.88–1.41) | 1.11 (0.88–1.41) | 1.15 (0.91–1.47) |
| Normal | 1.35 (1.06–1.72) | 1.36 (1.07–1.73) | 1.39 (1.09–1.76) |
| Physical activity | |||
| Poor | 1 (ref) | 1 (ref) | 1 (ref) |
| Intermediate | 1.12 (0.88–1.41) | 1.10 (0.88–1.39) | 1.09 (0.86–1.37) |
| Ideal | 1.27 (0.99–1.63) | 1.25 (0.97–1.60) | 1.25 (0.97–1.60) |
| Diet | |||
| Poor diet | 1 (ref) | 1 (ref) | 1 (ref) |
| Healthy diet | 0.97 (0.79–1.20) | 0.97 (0.78–1.20) | 0.94 (0.76–1.17) |
| Alcohol consumption | |||
| Any | 1 (ref) | 1 (ref) | 1 (ref) |
| None | 1.05 (0.86–1.29) | 1.02 (0.83–1.26) | 1.02 (0.82–1.27) |
| Smoking | |||
| Ever | 1 (ref) | 1 (ref) | 1 (ref) |
| Never | 1.51 (1.03–2.22) | 1.51 (1.02–2.24) | 1.48 (0.99–2.20) |
| Psychosocial factors | |||
| Weekly stress | |||
| High | 1 (ref) | 1 (ref) | 1 (ref) |
| Moderate | 1.21 (0.85–1.73) | 1.28 (0.95–1.73) | 1.29 (0.95–1.75) |
| Low | 1.16 (0.74–1.81) | 1.21 (0.87–1.69) | 1.21 (0.84–1.73) |
| Anger in | |||
| High | 1 (ref) | 1 (ref) | 1 (ref) |
| Moderate | 1.18 (0.89–1.55) | 1.21 (0.85–1.71) | 1.18 (0.82–1.71) |
| Low | 1.10 (0.81–1.49) | 1.12 (0.81–1.56) | 1.06 (0.71–1.58) |
| Anger out | |||
| High | 1 (ref) | 1 (ref) | 1 (ref) |
| Moderate | 1.16 (0.87–1.55) | 1.12 (0.80–1.56) | 1.09 (0.77–1.54) |
| Low | 1.27 (0.97–1.67) | 1.18 (0.81–1.72) | 1.16 (0.77–1.75) |
| Daily discrimination | |||
| High | 1 (ref) | 1 (ref) | 1 (ref) |
| Moderate | 1.15 (0.91–1.45) | 1.13 (0.89–1.42) | 1.06 (0.83–1.36) |
| Low | 1.02 (0.79–1.31) | 1.01 (0.78–1.30) | 0.94 (0.71–1.24) |
| Social support | |||
| Low | 1 (ref) | 1 (ref) | 1 (ref) |
| Moderate | 1.02 (0.80–1.31) | 1.05 (0.82–1.36) | 1.04 (0.80–1.35) |
| High | 0.87 (0.68–1.12) | 0.91 (0.70–1.20) | 0.90 (0.66–1.22) |
| Depression | |||
| High | 1 (ref) | 1 (ref) | 1 (ref) |
| Low | 1.08 (0.84–1.39) | 1.01 (0.72–1.41) | 0.88 (0.60–1.29) |
Model 1 adjusted for age, sex, and income less than $25,000 at visit 1.
Model 2 adjusted for variables in model 1 and body mass index, physical activity, diet and alcohol consumption at visit 1.
Model 3 adjusted for variables in model 2 and weekly stress, anger in, anger out, daily discrimination, social support, and depression at visit 1.
Among participants who did and did not maintain normal BP over follow-up, 13.4% and 7.6% had normal BMI at baseline and maintained normal BMI over follow-up, respectively, and 16.0% and 8.9% had ideal physical activity at baseline and maintained ideal physical activity over follow-up, respectively (Table 3). Maintaining normal BMI (RR 1.46; 95% CI: 1.13–1.88) and ideal physical activity (RR 1.45; 95% CI: 1.14–1.85) were associated with maintaining normal BP after adjustment for sociodemographic, lifestyle and psychosocial factors at baseline (Table 4). There was no evidence of an association between maintaining no alcohol consumption, no smoking and ideal levels of psychosocial factors with maintaining normal BP.
Table 3:
Proportion of participants who maintained ideal levels of lifestyle and psychosocial factors among those who maintained and did not maintain normal blood pressure
| Maintained normal blood pressure | ||
|---|---|---|
| Maintenance of factors | Yes (N = 262) |
No (N = 495) |
| Lifestyle factors | ||
| Normal body mass index | 13.4 | 7.6 |
| Ideal physical activity | 16.0 | 8.9 |
| Ideal/no alcohol consumption | 33.9 | 36.2 |
| Ideal/never smoking | 84.7 | 88.5 |
| Psychosocial factors | ||
| Low anger-in | 16.1 | 15.9 |
| Low anger-out | 17.4 | 18.0 |
| Low daily discrimination | 19.1 | 19.0 |
Table values are column percent.
Table 4:
Association between maintaining ideal levels of lifestyle and psychosocial risk factors and maintaining normal blood pressure.
| Risk ratios (95% Confidence intervals) | |||
|---|---|---|---|
| Maintenance of factors* | Model 1 | Model 2 | Model 3 |
| Lifestyle factors | |||
| Body mass index | |||
| Did not maintain normal levels | 1 (ref) | 1 (ref) | 1 (ref) |
| Maintained normal levels | 1.43 (1.10–1.86) | 1.48 (1.15–1.90) | 1.46 (1.13–1.88) |
| Physical activity | |||
| Did not maintain ideal levels | 1 (ref) | 1 (ref) | 1 (ref) |
| Maintained ideal levels | 1.43 (1.12–1.83) | 1.43 (1.11–1.83) | 1.45 (1.14–1.85) |
| Alcohol consumption | |||
| Did not maintain ideal levels | 1 (ref) | 1 (ref) | 1 (ref) |
| Maintained ideal levels | 1.06 (0.85–1.31) | 1.01 (0.82–1.25) | 1.02 (0.81–1.28) |
| Smoking | |||
| Did not maintain ideal levels | 1 (ref) | 1 (ref) | 1 (ref) |
| Maintained ideal levels | 1.28 (0.92–1.78) | 1.26 (0.90–1.78) | 1.23 (0.87–1.73) |
| Psychosocial factors | |||
| Anger in | |||
| Did not maintain ideal levels | 1 (ref) | 1 (ref) | 1 (ref) |
| Maintained ideal levels | 1.15 (0.89–1.50) | 1.13 (0.87–1.47) | 1.09 (0.82–1.45) |
| Anger out | |||
| Did not maintain ideal levels | 1 (ref) | 1 (ref) | 1 (ref) |
| Maintained ideal levels | 1.06 (0.78–1.43) | 1.03 (0.76–1.40) | 1.01 (0.74–1.38) |
| Daily discrimination | |||
| Did not maintain ideal levels | 1 (ref) | 1 (ref) | 1 (ref) |
| Maintained ideal levels | 0.97 (0.75–1.24) | 1.01 (0.79–1.29) | 1.06 (0.82–1.38) |
This analysis was limited to lifestyle and psychosocial factors that were assessed at more than 1 study visit.
Model 1 adjusted for age, sex and income less than $25,000 at visit 1.
Model 2 adjusted for variables in model 1 and body mass index, physical activity, diet and alcohol consumption at visit 1.
Model 3 adjusted for variables in model 2 and weekly stress, anger in, anger out, daily discrimination, social support, and depression at visit 1.
Maintaining normal BP without an increase in SBP and DBP
Among participants with normal BP at baseline, 51 of the 757 participants (6.7%) did not have an increase in SBP or DBP during follow-up. After adjustment for sociodemographic, lifestyle, and psychosocial factors, ideal physical activity at baseline was associated with maintaining normal BP without an increase in SBP or DBP (RR 2.27; 95% CI: 1.12–4.60; Table S5). Maintaining ideal physical activity was also associated with maintaining normal BP without an increase in SBP or DBP (Table S6).
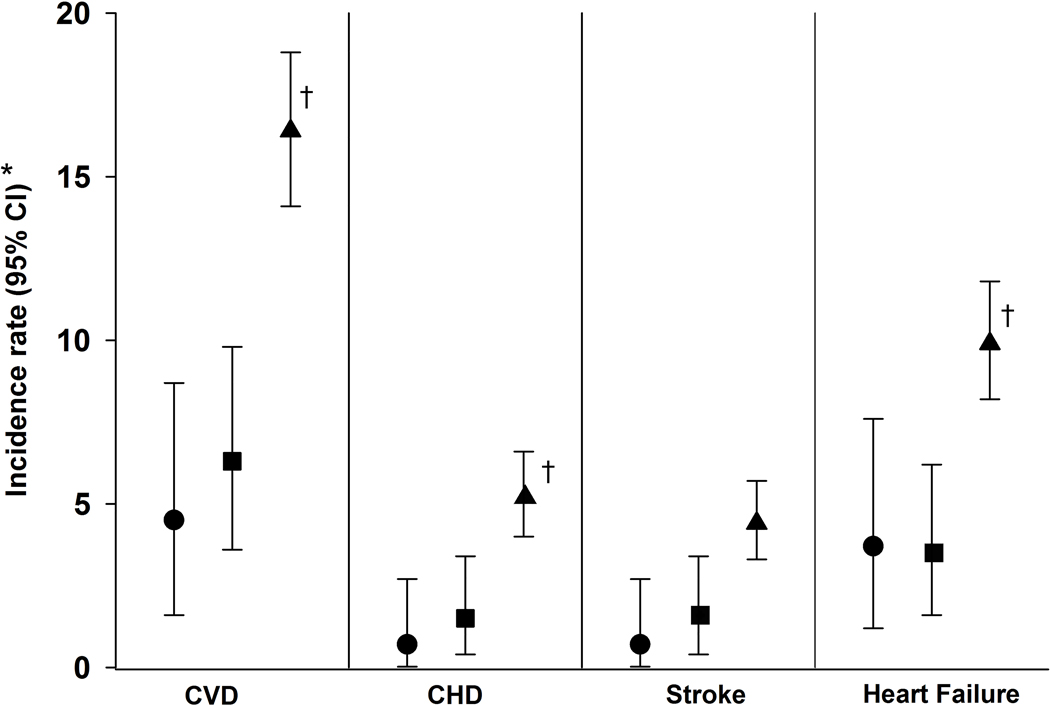
Risk for incident cardiovascular disease and crude all-cause mortality rates
Among 2,793 participants without a history of CVD at visit 3 there were 212 incident CVD events over a median of 5.9 years of follow‐up (Figure 2; Table S7). The IR for CVD was 4.5 (95% CI: 2.0–10.0), 6.3 (95% CI: 3.9–10.3) and 16.4 (95% CI: 14.2–18.9) per 1,000 person-years among participants who maintained normal BP, had normal BP at baseline but did not maintain normal BP and had elevated BP or hypertension at baseline, respectively. The all-cause mortality rate was lower among participants who maintained normal BP or had normal BP at baseline but did not maintain normal BP over follow-up compared to those with elevated BP or hypertension at baseline.
Figure 2:
Cardiovascular disease incidence rates by blood pressure status
● Maintained normal BP
■ Normal BP at baseline, did not maintain over follow-up
▲ Elevated BP or hypertension at baseline
BP, blood pressure; CI, confidence interval; CVD, cardiovascular disease; CHD, coronary heart disease
*Incidence rate per 1,000 person-years; Follow-up for CVD events began upon completion of JHS visit 3. Median follow-up in years (25th – 75th percentiles) = 5.9 (5.1–6.8)
†CVD incidence rate is higher than the rate among the maintaining normal BP category at p < 0.05.
P-values comparing those with normal blood pressure at baseline that did not maintain normal blood pressure over follow-up versus those who maintained normal blood pressure were p=0.469 for cardiovascular disease, p=0.511 for coronary heart disease, p=0.507 for stroke, p=0.927 for heart failure and p=0.509 for all-cause mortality.
P-values comparing those with elevated blood pressure or hypertension at baseline versus those who maintained normal blood pressure were p=0.002 for cardiovascular disease, p=0.053 for coronary heart disease, p=0.076 for stroke, p=0.032 for heart failure and p=0.003 for all-cause mortality.
P-values comparing those with normal blood pressure at baseline that did not maintain normal blood pressure over follow-up versus those with elevated blood pressure or hypertension at baseline were p<0.001 for cardiovascular disease, p=0.019 for coronary heart disease, p=0.043 for stroke, p=0.003 for heart failure and p<0.001 for all-cause mortality.
Discussion
In this prospective, community-based, cohort study, 34.6% of African American adults with normal BP at baseline maintained normal BP over 8 years of follow-up. Ideal levels of physical activity and BMI at baseline were associated with maintaining normal BP. However, only 43.3% and 40.9% of those with normal BMI and ideal physical activity at baseline maintained normal BP, respectively. Participants who maintained versus did not maintain ideal levels of BMI and physical activity over follow-up were more likely to maintain normal BP. Incident CVD and all-cause mortality were lower among participants who maintained normal BP over follow-up compared to those with elevated BP or hypertension at baseline.
Evidence from observational studies consistently shows that few US adults, particularly African Americans, reach older age without developing elevated BP or hypertension.25–28 African Americans are often viewed homogeneously as having the highest prevalence of hypertension in the world.26, 29 However, over one-third of African American participants in the current study who had normal BP at baseline maintained it over 8 years of follow-up. A prior study showed that adults with normal BP and total cholesterol <180 mg per deciliter who reported not smoking and not having diabetes at the age of 55 years were unlikely to develop CVD over their lifetime.30 With evidence suggesting that the majority of African Americans with normal BP at 25 years of age develop hypertension before 50 years of age,28 the biggest gains in prevention may result from maintaining normal BP from childhood and young adulthood through middle age. While maintaining normal BP is important, recent results from the Multi-Ethnic Study of Atherosclerosis (MESA) suggest that even within the normal range, lower SBP is associated with lower risk for CVD.31 These data emphasize the need to develop public health programs aimed at the prevention of increases in BP across the life course.
The increase in BP with age is often considered a consequence of structural changes in the cardiovascular system, including arterial stiffening and atherosclerosis.32, 33 On average, SBP increases by 7 to 15 mm Hg per decade of life after 40 years of age in industrialized societies.34–36 In the present study of African American adults with a mean age of 46 years at baseline, 6.7% of those with normal BP at baseline had no increase in BP over 8 years of follow-up. These results support a growing body of evidence that increases in BP with age in mid- to late- life are not uniform, but rather are heterogeneous and potentially avoidable, even among high-risk populations.5, 6, 35 Further research is needed to determine age periods over the life course when lifestyle and psychosocial factors exhibit the most influence on age-related increases in BP.
Despite the focus on cardiovascular health in the AHA’s 2020 goals, only a modest increase in the proportion of US adults with normal BP occurred over the past decade.29 Understanding the lifestyle and psychosocial factors that are associated with maintaining normal BP is of clinical and public health importance for informing strategies to maintain CVD health.37, 38 In the current study, normal BMI and ideal physical activity at baseline were associated with maintaining normal BP over follow-up. Associations between maintenance of normal BP, normal BMI and ideal physical activity over the life course reinforce the benefits of lifelong adoption of lifestyles that promote cardiovascular health. An abundance of evidence indicates that nonpharmacologic lifestyle interventions such as weight loss and increases in regular physical activity are effective in lowering BP in those with hypertension.22, 39 There is less evidence on strategies to motivate and support continuous use of positive lifestyle behaviors over time.40, 41 Identifying and addressing barriers to achieving and maintaining optimal levels of health behaviors is particularly pertinent for maintaining normal BP, given reports of persistent adverse levels of BMI and physical activity throughout the life course among those with and at increased risk for hypertension.42
Although the results of this study emphasize the importance of normal weight and ideal physical activity for maintaining normal BP, a large proportion of participants who maintained normal BP over follow-up had intermediate or poor levels of physical activity or BMI at baseline. Decades of research has documented that hypertension is a multifactorial condition involving interactions between sociodemographic, lifestyle, psychosocial, genetic and environmental factors.43, 44 Maintaining normal BP is presumably also multifactorial with ideal levels of a single component being insufficient for maintaining normal BP across the life course. In addition to the strong associations between ideal physical activity and normal BMI with maintaining normal BP, future studies should consider combinations of lifestyle, psychosocial and sociodemographic factors that support maintaining normal BP across longer periods of follow-up.
The large, well-characterized sample of African Americans in the JHS allowed us to evaluate the effects of several lifestyle and psychosocial factors on maintaining normal BP through mid- to late- life. Despite its strengths, the results of the current study should be considered in the context of potential and known limitations. African Americans in the JHS were recruited from a single metropolitan area, which may limit the generalizability of results. The mean age of participants with normal BP at baseline was 46 years and the median follow-up period was only 8 years. Future studies are needed to determine the factors associated with maintaining normal BP from young adulthood through middle age, over longer time periods and among other racial/ethnic groups. The evaluation of the association between psychosocial factors and maintaining normal BP has been limited by the absence of established cut points for most of the psychosocial measures. Ascertainment of CVD events for this analysis was restricted to a follow-up period of 5 years. Longer follow-up and a larger sample size would have allowed us to determine the effect of maintaining normal BP on the risk of CVD events with more precision.
Perspectives
Approximately one-third of African American adults in the current study maintained normal BP over a median of 8 years of follow up. Ideal levels of BMI and physical activity at baseline and the maintenance of these factors across study visits were associated with maintaining normal BP through mid- to late- life. However, a large proportion of participants who maintained normal BP over follow-up had intermediate or poor levels of physical activity or BMI at baseline. Participants who maintained normal BP had a low risk of developing CVD. These findings suggest that primordial prevention efforts should begin early in the life course and focus on achieving and preserving ideal levels of physical activity and BMI to protect against BP increases with age and reduce CVD.
Supplementary Material
Novelty and Significance.
What Is New?
Mean blood pressure (BP) usually increases with age. Characterizing the population that maintains normal BP across the life course could inform hypertension prevention efforts.
What Is Relevant?
Among participants with normal BP at baseline, 34.6% maintained normal BP over a median of 8 years of follow-up. Ideal levels of body mass index (BMI) and physical activity were associated with maintaining normal BP. Participants who maintained normal BP had a low risk of developing CVD.
Summary
These data suggest that maintaining normal BMI and ideal physical activity are potential approaches for maintaining normal BP.
Acknowledgements:
The Jackson Heart Study (JHS) is supported and conducted in collaboration with Jackson State University (HHSN268201800013I), Tougaloo College (HHSN268201800014I), the Mississippi State Department of Health (HHSN268201800015I) and the University of Mississippi Medical Center (HHSN268201800010I, HHSN268201800011I and HHSN268201800012I) contracts from the National Heart, Lung, and Blood Institute (NHLBI) and the National Institute on Minority Health and Health Disparities (NIMHD). The authors also wish to thank the staffs and participants of the JHS.
Sources of Funding
Drs. Hardy, Muntner and Shimbo receive support through R01HL139716 from the NHLBI. Drs. Muntner and Shimbo also receive research support through R01HL117323 from the NHLBI. Dr. Shimbo receives support through K24-HL125704 from the NHLBI. Dr. Tajeu receives research support through R01DK108628-05S1 from the National Institute of Diabetes and Digestive and Kidney Diseases and K01HL151974 from the NHLBI. Dr. Elfassy receives research support through K01MD014158 from the NIMHD. Dr. Reges thanks the American Heart Association for the Children’s Strategically Focused Research Networks (SFRN) postdoctoral fellowship (grant 17SFRN33700101), and the Israel Scholarship Education Foundation for their support.
Footnotes
Disclosures: Paul Muntner receives grant funding and consulting fees from Amgen Inc. unrelated to topic in the current manuscript.
References
- 1.Lewington S, Clarke R, Qizilbash N, Peto R and Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–13. [DOI] [PubMed] [Google Scholar]
- 2.Muntner P, He J, Cutler JA, Wildman RP and Whelton PK. Trends in blood pressure among children and adolescents. Jama. 2004;291:2107–13. [DOI] [PubMed] [Google Scholar]
- 3.Mueller NT, Noya-Alarcon O, Contreras M, Appel LJ and Dominguez-Bello MG. Association of Age With Blood Pressure Across the Lifespan in Isolated Yanomami and Yekwana Villages. JAMA Cardiology. 2018;3:1247–1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carvalho JJ, Baruzzi RG, Howard PF, Poulter N, Alpers MP, Franco LJ, Marcopito LF, Spooner VJ, Dyer AR, Elliott P and et al. Blood pressure in four remote populations in the INTERSALT Study. Hypertension. 1989;14:238–46. [DOI] [PubMed] [Google Scholar]
- 5.Allen NB, Siddique J, Wilkins JT, Shay C, Lewis CE, Goff DC, Jacobs DR Jr., Liu K and Lloyd-Jones D. Blood pressure trajectories in early adulthood and subclinical atherosclerosis in middle age. Jama. 2014;311:490–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Petruski-Ivleva N, Viera AJ, Shimbo D, Muntner P, Avery CL, Schneider ALC, Couper D and Kucharska-Newton A. Longitudinal Patterns of Change in Systolic Blood Pressure and Incidence of Cardiovascular Disease: The Atherosclerosis Risk in Communities Study. Hypertension (Dallas, Tex : 1979). 2016;67:1150–1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dorans KS, Mills KT, Liu Y and He J. Trends in Prevalence and Control of Hypertension According to the 2017 American College of Cardiology/American Heart Association (ACC/AHA) Guideline. J Am Heart Assoc. 2018;7. [DOI] [PMC free article] [PubMed]
- 8.Bibbins-Domingo K, Pletcher MJ, Lin F, Vittinghoff E, Gardin JM, Arynchyn A, Lewis CE, Williams OD and Hulley SB. Racial Differences in Incident Heart Failure among Young Adults. New England Journal of Medicine. 2009;360:1179–1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Howard G, Lackland DT, Kleindorfer DO, Kissela BM, Moy CS, Judd SE, Safford MM, Cushman M, Glasser SP and Howard VJ. Racial Differences in the Impact of Elevated Systolic Blood Pressure on Stroke Risk. JAMA Internal Medicine. 2013;173:46–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Booth JN 3rd, Abdalla M, Tanner RM, Diaz KM, Bromfield SG, Tajeu GS, Correa A, Sims M, Ogedegbe G, Bress AP, Spruill TM, Shimbo D and Muntner P. Cardiovascular Health and Incident Hypertension in Blacks: JHS (The Jackson Heart Study). Hypertension. 2017;70:285–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cuffee Y, Ogedegbe C, Williams NJ, Ogedegbe G and Schoenthaler A. Psychosocial risk factors for hypertension: an update of the literature. Curr Hypertens Rep. 2014;16:483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ford CD, Sims M, Higginbotham JC, Crowther MR, Wyatt SB, Musani SK, Payne TJ, Fox ER and Parton JM. Psychosocial Factors Are Associated With Blood Pressure Progression Among African Americans in the Jackson Heart Study. Am J Hypertens. 2016;29:913–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Glover LM, Cain-Shields LR, Wyatt SB, Gebreab SY, Diez-Roux AV and Sims M. Life Course Socioeconomic Status and Hypertension in African American Adults: The Jackson Heart Study. Am J Hypertens. 2020;33:84–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Taylor HA Jr., Wilson JG, Jones DW, Sarpong DF, Srinivasan A, Garrison RJ, Nelson C and Wyatt SB. Toward resolution of cardiovascular health disparities in African Americans: design and methods of the Jackson Heart Study. Ethn Dis. 2005;15:S6–4–17. [PubMed] [Google Scholar]
- 15.Lloyd-Jones Donald M, Hong Y, Labarthe D, Mozaffarian D, Appel Lawrence J, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli Gordon F, Arnett Donna K, Fonarow Gregg C, Ho PM, Lauer Michael S, Masoudi Frederick A, Robertson Rose M, Roger V, Schwamm Lee H, Sorlie P, Yancy Clyde W and Rosamond Wayne D. Defining and Setting National Goals for Cardiovascular Health Promotion and Disease Reduction. Circulation. 2010;121:586–613. [DOI] [PubMed] [Google Scholar]
- 16.Dubbert PM, Carithers T, Ainsworth BE, Taylor HA Jr., Wilson G and Wyatt SB. Physical activity assessment methods in the Jackson Heart Study. Ethn Dis. 2005;15:S6–56–61. [PubMed] [Google Scholar]
- 17.Payne TJ, Wyatt SB, Mosley TH, Dubbert PM, Guiterrez-Mohammed ML, Calvin RL, Taylor HA Jr., and Williams DR. Sociocultural methods in the Jackson Heart Study: conceptual and descriptive overview. Ethn Dis. 2005;15:S6–38–48. [PubMed] [Google Scholar]
- 18.Sims M, Wyatt SB, Gutierrez ML, Taylor HA and Williams DR. Development and psychometric testing of a multidimensional instrument of perceived discrimination among African Americans in the Jackson Heart Study. Ethnicity & disease. 2009;19:56–64. [PMC free article] [PubMed] [Google Scholar]
- 19.Payne TJ, Andrew M, Butler KR, Wyatt SB, Dubbert PM and Mosley TH. Psychometric evaluation of the interpersonal support evaluation list–short form in the ARIC study cohort. Sage Open. 2012;2:2158244012461923. [Google Scholar]
- 20.Weissman MM, Sholomskas D, Pottenger M, Prusoff BA and Locke BZ. Assessing depressive symptoms in five psychiatric populations: a validation study. Am J Epidemiol. 1977;106:203–14. [DOI] [PubMed] [Google Scholar]
- 21.Seals SR, Colantonio LD, Tingle JV, Shimbo D, Correa A, Griswold ME and Muntner P. Calibration of blood pressure measurements in the Jackson Heart Study. Blood Press Monit. 2019;24:130–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Whelton PK, Carey RM, Aronow WS, Casey DE Jr., Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr., Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr., JD Williamson and JT Wright Jr., 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2018;138:e426–e483. [DOI] [PubMed] [Google Scholar]
- 23.Keku E, Rosamond W, Taylor HA Jr., Garrison R, Wyatt SB, Richard M, Jenkins B, Reeves L and Sarpong D. Cardiovascular disease event classification in the Jackson Heart Study: methods and procedures. Ethn Dis. 2005;15:S6–62–70. [PubMed] [Google Scholar]
- 24.Dong Y and Peng CYJ. Principled missing data methods for researchers. SpringerPlus. 2013;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vasan RS, Beiser A, Seshadri S, Larson MG, Kannel WB, D’Agostino RB and Levy D. Residual lifetime risk for developing hypertension in middle-aged women and men: The Framingham Heart Study. Jama. 2002;287:1003–10. [DOI] [PubMed] [Google Scholar]
- 26.Muntner P, Carey RM, Gidding S, Jones DW, Taler SJ, Wright JT Jr., and Whelton PK. Potential US Population Impact of the 2017 ACC/AHA High Blood Pressure Guideline. Circulation. 2018;137:109–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carson AP, Howard G, Burke GL, Shea S, Levitan EB and Muntner P. Ethnic Differences in Hypertension Incidence Among Middle-Aged and Older Adults. Hypertension. 2011;57:1101–1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thomas SJ, Booth JN, Dai C, Li X, Allen N, Calhoun D, Carson AP, Gidding S, Lewis CE, Shikany JM, Shimbo D, Sidney S and Muntner P. Cumulative Incidence of Hypertension by 55 Years of Age in Blacks and Whites: The CARDIA Study. Journal of the American Heart Association. 2018;7:e007988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Jordan LC, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, O’Flaherty M, Pandey A, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Spartano NL, Stokes A, Tirschwell DL, Tsao CW, Turakhia MP, VanWagner LB, Wilkins JT, Wong SS and Virani SS. Heart Disease and Stroke Statistics Update: A Report From the American Heart Association. Circulation. 2019;139:e56–e528. [DOI] [PubMed] [Google Scholar]
- 30.Berry JD, Dyer A, Cai X, Garside DB, Ning H, Thomas A, Greenland P, Van Horn L, Tracy RP and Lloyd-Jones DM. Lifetime Risks of Cardiovascular Disease. New England Journal of Medicine. 2012;366:321–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Whelton SP, McEvoy JW, Shaw L, Psaty BM, Lima JAC, Budoff M, Nasir K, Szklo M, Blumenthal RS and Blaha MJ. Association of Normal Systolic Blood Pressure Level With Cardiovascular Disease in the Absence of Risk Factors. JAMA Cardiology. 2020;5:1011–1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McEniery CM, Wilkinson IB and Avolio AP. Age, Hypertension and Arterial Function. Clinical and Experimental Pharmacology and Physiology. 2007;34:665–671. [DOI] [PubMed] [Google Scholar]
- 33.Mitchell GF, Hwang S-J, Vasan RS, Larson MG, Pencina MJ, Hamburg NM, Vita JA, Levy D and Benjamin EJ. Arterial stiffness and cardiovascular events: the Framingham Heart Study. Circulation. 2010;121:505–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gurven M, Blackwell AD, Rodríguez DE, Stieglitz J and Kaplan H. Does Blood Pressure Inevitably Rise With Age? Hypertension. 2012;60:25–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wills AK, Lawlor DA, Matthews FE, Aihie Sayer A, Bakra E, Ben-Shlomo Y, Benzeval M, Brunner E, Cooper R, Kivimaki M, Kuh D, Muniz-Terrera G and Hardy R. Life Course Trajectories of Systolic Blood Pressure Using Longitudinal Data from Eight UK Cohorts. PLOS Medicine. 2011;8:e1000440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wolf-Maier K, Cooper RS, Banegas JR, Giampaoli S, Hense HW, Joffres M, Kastarinen M, Poulter N, Primatesta P, Rodríguez-Artalejo F, Stegmayr B, Thamm M, Tuomilehto J, Vanuzzo D and Vescio F. Hypertension prevalence and blood pressure levels in 6 European countries, Canada, and the United States. Jama. 2003;289:2363–9. [DOI] [PubMed] [Google Scholar]
- 37.Olsen MH, Angell SY, Asma S, Boutouyrie P, Burger D, Chirinos JA, Damasceno A, Delles C, Gimenez-Roqueplo A-P, Hering D, López-Jaramillo P, Martinez F, Perkovic V, Rietzschel ER, Schillaci G, Schutte AE, Scuteri A, Sharman JE, Wachtell K and Wang JG. A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: the Lancet Commission on hypertension. The Lancet. 2016;388:2665–2712. [DOI] [PubMed] [Google Scholar]
- 38.James SA. Primordial prevention of cardiovascular disease among African-Americans: a social epidemiological perspective. Preventive medicine. 1999;29:S84–9. [DOI] [PubMed] [Google Scholar]
- 39.Eckel RH, Jakicic JM, Ard JD, Jesus JMd, Miller NH, Hubbard VS, Lee I-M, Lichtenstein AH, Loria CM, Millen BE, Nonas CA, Sacks FM, Smith SC, Svetkey LP, Wadden TA and Yanovski SZ. 2013 AHA/ACC Guideline on Lifestyle Management to Reduce Cardiovascular Risk. Circulation. 2014;129:S76–S99. [DOI] [PubMed] [Google Scholar]
- 40.Hall KD and Kahan S. Maintenance of Lost Weight and Long-Term Management of Obesity. Med Clin North Am. 2018;102:183–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McPhee JS, French DP, Jackson D, Nazroo J, Pendleton N and Degens H. Physical activity in older age: perspectives for healthy ageing and frailty. Biogerontology. 2016;17:567–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pahigiannis K, Thompson-Paul AM, Barfield W, Ochiai E, Loustalot F, Shero S and Hong Y. Progress Toward Improved Cardiovascular Health in the United States. Circulation. 2019;139:1957–1973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kuneš J and Zicha J. The interaction of genetic and environmental factors in the etiology of hypertension. Physiological research. 2009;58:S33–S41. [DOI] [PubMed] [Google Scholar]
- 44.Kaplan M and Nunes A. The psychosocial determinants of hypertension. Nutrition, metabolism and cardiovascular diseases. 2003;13:52–59. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.