Summary
Background
The first wave of the COVID-19 pandemic hit New South Wales (NSW) Australia in early 2020, followed by a sharp state-wide lockdown from mid-March to mid-May. After the lockdown, there had been a low level of community transmission of COVID-19 over a year. Such pandemic experiences provide unique opportunity to understand the impact of the pandemic on paediatric health service use as countries emerge from the pandemic.
Methods
We examined the difference between the observed and the predicted numbers of inpatient admissions and emergency department (ED) attendances, respectively, related to chronic, acute infectious and injury conditions, for each month during the COVID-19 period (January 2020-February 2021), based on the numbers from 2016 to 2019, using records from two major paediatric hospitals in NSW. All analyses were conducted using autoregressive error models and were stratified by patient age, sex and socioeconomic status.
Findings
Health service use was significantly lower than predicted for admissions and/or ED attendances related to chronic conditions, acute infections, and injury during the lockdown in 2020. Change in health service use varied by chronic conditions, from the largest decrease for respiratory conditions (40-78%) to non-significant change for cancer and mental health disorders. After the lockdown, health service use for most health conditions returned to pre-COVID-19 predicted levels. However, for mental health disorders, increased health service use persisted from June 2020 up to February 2021 by 30-55%, with higher increase among girls aged 12-17 years and those from socioeconomically advantaged areas. There was persistently lower health service use for acute infections and increased health service use for injuries. Differences by socio-demographic factors were noted for mental health disorders and injuries.
Interpretation
The immediate return to pre-COVID-19 levels for most chronic conditions after the first lockdown in NSW highlights the healthcare needs for children affected by chronic conditions. Persistently lower health service use for acute infections is likely attributable to the decreased social contact. Sustained and targeted mental health support is essential to address the potentially increased demand for services among children during and beyond the pandemic.
Funding
Financial Markets Foundation for Children Chair (RL, NN), NHMRC Investigator Grant (APP1197940) (NN), NHMRC Career Development fellowship (GNT1158954) (SW)
Keywords: COVID-19, Paediatric health service, Mental health, Chronic health condition, Acute infectious conditions, Injury
Research in context.
Evidence before this study
The COVID-19 pandemic has had a large impact on non-COVID-19 related health service use, largely due to the social restriction measures and change in people's healthcare seeking behaviours. We searched PubMed for articles published on non-COVID-19 related health service use among children and adolescents since the start of the pandemic, using the search terms including “children” and “adolescents”, “hospital inpatient admission” or “emergency department (ED)”, “health service use” or “healthcare”. Most previous research was conducted in North America, Europe, and China, particularly in settings where community transmission remained widespread. The research has shown a significant decrease in paediatric health service use in both inpatient and ED settings within the first six months of the pandemic. There was a consistent decrease in health service use related to respiratory infections (reduced by 70-80%), and a smaller or no decrease for health service use related to more complex conditions such as diabetic complications, cancer, and mental health disorders, compared to pre-COVID years. However, there has been no examination of the longer-term trend in paediatric health service use across a broader range of health conditions, when there was a minimal community transmission of COVID-19 cases after the lockdown ended. Additionally, there has been limited understanding of the change in paediatric health service use by key socio-demographic factors including age, sex and socioeconomic status to identify groups of children most affected by the pandemic.
Added value of this study
The experiences following the first wave of the pandemic in New South Wales (NSW) Australia in 2020, with its lower prevalence of community infections of COVID-19 and a sharp 2-month lockdown, has enabled us to examine the paediatric health service use over a year since the pandemic outbreak, within the 2-month lockdown and the 10-month post-lockdown periods. We analysed medical records routinely collected over five years by the largest paediatric healthcare provider in Australia to examine inpatient admissions and ED attendances related to various chronic health conditions (including seven specific types of conditions including cancer, respiratory, metabolic, musculoskeletal, neurological, cardiovascular, and mental health conditions), acute infectious conditions, and childhood injury before (2016-2019) and during (January 2020-February 2021) the pandemic. Our results show paediatric health service use related to most chronic conditions and acute infectious conditions was significantly lower than predicted during the lockdown and, for chronic conditions, a quick return to the predicted levels (based on the pre-COVID-19 numbers) after the lockdown. Notably, health service use related to mental health disorders was persistently higher than predicted by 30-55% post-lockdown, with a greater increase for adolescent girls (12-17 years old) and children from the most advantaged areas. The number of injury-related health service use, in particular hospital admissions, was also persistently higher than predicted in the post-lockdown period.
Implications of all the available evidence
Our results provide unique insights into the potential longer-term impacts of the pandemic on paediatric health service use, which can help inform post-lockdown paediatric healthcare planning as countries emerge from the pandemic. Our results also highlight the need for sustained and targeted delivery of mental health services for children and adolescents during and beyond the pandemic.
Alt-text: Unlabelled box
Introduction
A dramatic decrease in non-COVID-19 related paediatric health service use within the first six months of the COVID-19 pandemic has been documented across multiple countries.1, 2, 3, 4 This followed the introduction of public health strategies, such as social lockdown measures, promotion of social distancing and good hygiene practices, to control the spread of SARS-CoV-2. This reduction in health service use has been shown to have both positive and negative impacts on child and adolescent health.5, 6, 7, 8 For example, a large decrease in health service use was associated with a 70-80% reduction in respiratory infections compared with previous years or predicted numbers,5,6 likely due to physical distancing and mask wearing.9 However, social restrictions and reported delay in healthcare seeking, largely due to parental concerns for acquiring COVID-19 infection, may have caused deferred diagnosis and treatment of health conditions.7,8
There have been significant concerns about disruptions caused by the pandemic on health service use by children with complex and severe health conditions, whose symptoms may have worsened and disease management may have been negatively affected.10,11 This may cause greater healthcare needs among these children in the long term as the pandemic continues. However, current studies have predominantly examined the health service use within the first six months of the pandemic when the levels of the community transmission of COVID-19 in many settings remained high, and no longer-term trend in health service use across health conditions have been reported6,12, 13, 14, 15. Additionally, most studies have not explored the impacts of the pandemic by key socio-demographic factors such as age, sex and socioeconomic status to identify the characteristics of children most affected by the pandemic.
Different from most other countries, the case numbers have been relatively low across Australia.16 In the most populous State, New South Wales (NSW), the first state-wide lockdown was implemented from mid-March, in response to the rapid increase in the number of COVID-19 cases from early March 2020, with the highest daily number of 213. The lockdown eased from mid-May 2020, and the daily number of new cases had since remained at a low level until the second state-wide lockdown starting from 27 June 2021 (persisting at the time of writing this paper)17 (Supplementary Figure 1). During the first lockdown in NSW, schools were only open to children of essential workers and the majority of students received online learning until they returned to full-time schooling in late May 2020. By late June, 463 children aged 0-17 years were diagnosed with COVID-19, with 9 hospitalised and 0 death across NSW.18,19 Although NSW is presently in its second wave of the pandemic, the COVID-19 experiences prior to this current pandemic have provided a unique opportunity that allows us to understand the impact of the pandemic on paediatric health service use over a year (comparatively much longer to most existing studies) when the community transmission was minimal following a sharp and brief lockdown. Such investigations can help inform paediatric healthcare planning during and beyond the pandemic, and the increase in healthcare needs is anticipated to be significantly magnified in places with longer and often multiple lockdown periods.20
This study aimed to assess the impact of the COVID-19 pandemic on paediatric hospital inpatient admissions and emergency department (ED) attendances in the first year since the first state-wide lockdown started (March 2020 to February 2021), using medical records routinely collected by major paediatric tertiary hospitals in NSW. We examined health service use for various chronic conditions, acute infections and childhood injuries, and conducted the analysis by patient age, sex, and socioeconomic status, considering the epidemiological variation and socioeconomic disparities in health service use by these factors.21
Methods
Study population and setting
This was a time series analysis of all inpatient admissions and ED attendances among children aged 0-17 years recorded by the Sydney Children's Hospitals Network (SCHN) from January 2016 to February 2021. We defined years 2016-2019 as the pre-COVID period, the most recent years before the COVID-19 pandemic which can best predict the linear and seasonal patterns of health service use in 2020, had the pandemic not occurred. We defined January 2020 to February 2021 as the COVID period, which included the first state-wide lockdown (mid-March to mid-May 2020) and the post-lockdown (mid-May 2020–February 2021) periods (Supplementary Figure 1).
Data sources
We analysed all de-identified individual records of inpatient admissions and ED attendances from SCHN, the largest paediatric healthcare provider in Australia, caring for over 120,000 families and providing around 50,000 inpatient admissions and 90,000 ED attendances annually. The admissions records contain information about patient demographics (e.g., age, sex, residential postcode), admission and discharge dates, principal diagnosis chiefly responsible for the admission, and up to 50 additional diagnoses of health conditions that may coexist at the time of admission, develop subsequently, or affect the treatment or length of stay. All diagnoses were coded using the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Australian Modification (ICD-10-AM). The ED records include information about patient demographics, date of attendance, and diagnosis established after an ED assessment coded using the SNOMED-CT Australian Extension codes (SNOMED CT-AU) or the ICD-10-AM codes. We converted SNOMED CT-AU codes into ICD-10-AM codes using the snoMAP-Starter AU, a map product developed by the Australian e-Health Research Centre.22
Identification of health conditions
We examined three categories of health conditions, which impose a high disease burden to children,23,24 including major chronic conditions, acute infections, and childhood injuries. We identified health conditions using relevant ICD-10-AM codes recorded as principal or additional diagnosis for inpatient admissions, and as diagnosis at discharge for ED attendances. We identified seven specific chronic conditions using the validated list of ICD codes developed by Hardelid et al.,24 such as mental health/behavioural, respiratory, and neurological conditions. For acute infections, we included high morbidity conditions such as bronchiolitis, acute otitis media, pneumonia and influenza.25 For injuries, we combined together unintentional and intentional events.26
Patient socio-demographics
We included patient age category (<1 year, 1-4, 5-11, 12-17 years), sex (male, female) and socioeconomic status as stratification factors. Patient residential postcode was converted to a socioeconomic disadvantage quartile based on the Index of Relative Socioeconomic Disadvantage developed by the Australian Bureau of Statistics.27 This index summarises a range of socioeconomic factors (eg, income, education and employment status) of the households within each postcode area.27
Data analysis
We compared the numbers of inpatient admissions and ED attendances, respectively, in the pre-COVID-19 and COVID-19 periods. Due to seasonality in time series, we employed autoregressive error models to predict the number of inpatient admissions and ED attendances, respectively, for each month during the COVID period, using the monthly numbers observed during the pre-COVID-19 period. The predicted numbers represent expected levels of health service use from January 2020 to February 2021, had the pandemic not occurred. We examined Durbin-Watson (D-W) statistics for twelve orders of autocorrelation (seasonality) and used the backward elimination method to determine the significant (p<0.05) orders of autocorrelation. We tested the model fit using mean absolute percentage error (MAPE), quantile plots for residual normality, autocorrelation functions (ACFs), and autoregressive-conditional heteroscedasticity (ARCH) models for residual variance constancy. We used the maximum likelihood (ML) method to estimate the model parameters for prediction and constructing 95% confidence intervals (CIs). We used the formula to calculate the percentage difference between the predicted and the observed numbers for each month during the COVID-19 period, for each health condition. All analyses were stratified by patient age category, sex and socioeconomic disadvantage quartile. Missing data were minimal, affecting less than 1.6% of all records; thus, we did not impute data. Additional information about data analysis is in the Supplement. We used SAS (Enterprise Guide) statistical software version 7.1 (SAS Institute Inc., Cary, NC, USA).28
Ethics committee approval
This study was approved by the Sydney Children's Hospitals Network Human Research Ethics Committee (2020/ETH01432).
Role of the funding source
The funding sources had no role in the design and execution of this study, analysis and interpretation of the data, or decision to submit results.
Results
Patient demographics
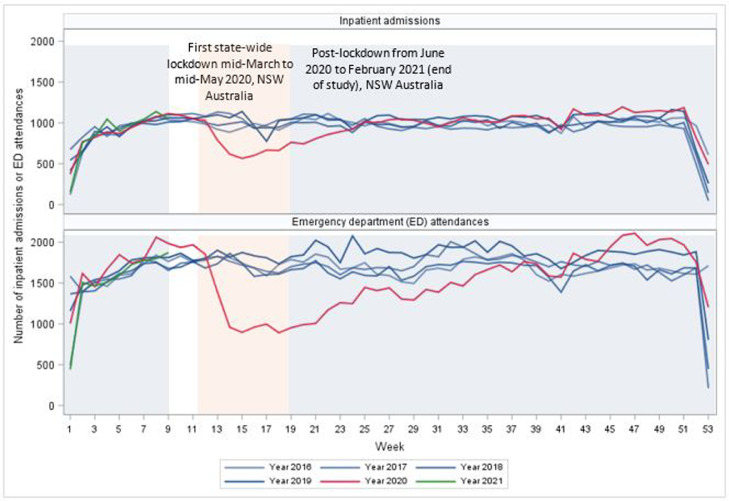
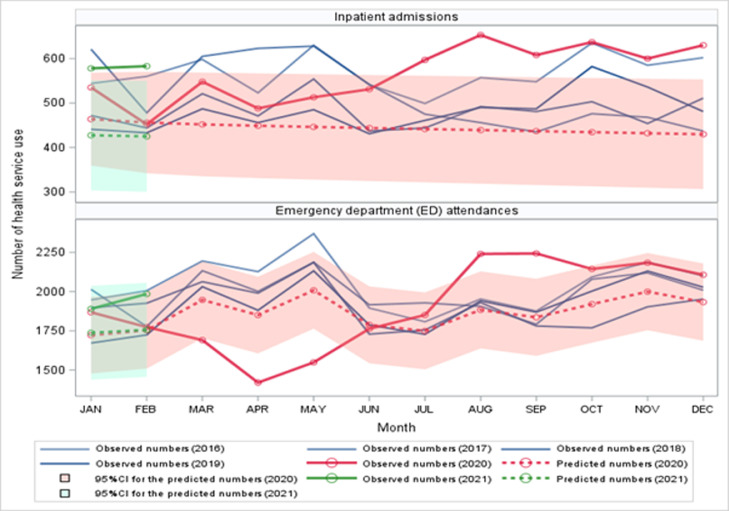
There were a total of 204,328 admissions and 359,377 ED attendances over the four pre-COVID-19 years (average annual number was 51,082 and 89,844, respectively), and 57,999 inpatient admissions and 96,049 ED attendances during the COVID-19 period. Figure 1 shows that the number of inpatient admissions and ED attendances dropped drastically during the first state-wide lockdown and progressively returned to the pre-COVID-19 levels after the lockdown was relaxed. Table 1 shows more admissions and ED attendances occurred among males (57%) than females (43%), and around two-thirds of admissions (63.3%) and ED attendances (69.2%) occurred among children aged 1-11 years. Children who resided in the most socioeconomically advantaged areas (the top quartile) accounted for more than one-third of admissions (36.0%) and ED attendances (40.2%). The proportion was similar between the pre-COVID-19 and the COVID-19 period.
Figure 1.
Health service use related to any health condition in SCHN during the pre-COVID (years 2016-2019) and the COVID (years 2020-2021) periods in NSW Australia.
Table 1.
Patient demographics for all inpatient admissions or ED attendances
| Inpatient admissions |
ED attendances |
|||
|---|---|---|---|---|
| Years 2016-2019 (pre-COVID) | 2020 – February 2021 (COVID) | Years 2016-2019 (pre-COVID) | 2020 – February 2021 (COVID) | |
| Number (Column %) | Number (Column %) | Number (Column %) | Number (Column %) | |
| Total number of admissions | 204328 (100) | 57999 (100) | 359377 (100) | 96049 (100) |
| Patient sex | ||||
| Male | 117462 (57.5) | 33263 (57.4) | 204384 (56.9) | 54041 (56.3) |
| Female | 86680 (42.4) | 24650 (42.5) | 154343 (43.0) | 41734 (43.5) |
| Unknown | 186 (0.1) | 86 (0.2) | 650 (0.2) | 274 (0.3) |
| Patient age (year) | ||||
| < 1 | 32213 (15.8) | 8551 (14.7) | 59674 (16.6) | 15282 (15.9) |
| 1 – 4 | 67618 (33.1) | 18652 (32.2) | 140083 (39.0) | 37118 (38.6) |
| 5 – 11 | 62648 (30.7) | 17147 (29.6) | 109748 (30.5) | 28338 (29.5) |
| 12 – 17 | 41849 (20.5) | 13649 (23.5) | 49872 (13.9) | 15311 (15.9) |
| Patient residence socioeconomic disadvantage quartiles (postcode-level) | ||||
| Q1 - most disadvantaged | 48314 (23.7) | 13478 (23.2) | 70313 (19.6) | 17968 (18.7) |
| Q2 | 32092 (15.7) | 8825 (15.2) | 39504 (11.0) | 10013 (10.4) |
| Q3 | 47236 (23.1) | 14023 (24.2) | 102243 (28.5) | 27328 (28.5) |
| Q4 – most advantaged | 73409 (35.9) | 21084 (36.4) | 143275 (39.9) | 39615 (41.2) |
| Unknown | 3277 (1.6) | 589 (1.0) | 4042 (1.1) | 1125 (1.2) |
| Hospitals | ||||
| The Children's Hospital at Westmead | 133496 (65.3) | 40001 (69.0) | 215205 (59.9) | 58377 (60.8) |
| Sydney Children's Hospital, Randwick | 70832 (34.7) | 17998 (31.0) | 144172 (40.1) | 37672 (39.2) |
Proportion of health conditions
Chronic conditions, acute infectious conditions, and injuries accounted for 53.1%, 17.1%, and 12.4% of all admissions respectively; and 7.4%, 19.4%, and 26.6% of all ED attendances, respectively. The remaining 27.8% of admissions and 46.8% of ED attendances were related to other non-specific conditions commonly including abnormalities of breathing, abdominal pain, and viral infection of unspecified site (Supplementary Tables 2A-2B). Table 2 shows that the proportion of admissions and ED attendances related to chronic conditions, acute infectious conditions and injuries was similar between the pre-COVID-19 and the COVID-19 period.
Table 2.
Proportion of health service use for each health condition
| Inpatient admissions |
ED attendances |
|||
|---|---|---|---|---|
| Years 2016-2019 (pre-COVID) | 2020 – February 2021 (COVID) | Years 2016-2019 (pre-COVID) | 2020 – February 2021 (COVID) | |
| Number (Column %)2 | Number (Column %) | Number (Column %) | Number (Column %) | |
| Total number of admissions | 204328 (100) | 57999 (100) | 359377 (100) | 96049 (100) |
| Total Chronic conditions related3 | 107946 (52.8) | 31789 (54.8) | 26594 (7.4) | 7004 (7.3) |
| Mental health/behavioural | 8162 (7.6) | 3508 (11) | 4086 (15.4) | 1351 (19.3) |
| Cancer/blood disorders | 29249 (27.1) | 8685 (27.3) | 2348 (8.8) | 743 (10.6) |
| Chronic infections | 738 (0.7) | 213 (0.7) | 164 (0.6) | 43 (0.6) |
| Respiratory | 17521 (16.2) | 4648 (14.6) | 6242 (23.5) | 1273 (18.2) |
| Metabolic 4 | 32473 (30.1) | 9959 (31.3) | 3150 (11.8) | 840 (12.0) |
| Musculoskeletal/skin | 19583 (18.1) | 5298 (16.7) | 3114 (11.7) | 707 (10.1) |
| Neurological | 24816 (23.0) | 7100 (22.3) | 5973 (22.5) | 1645 (23.5) |
| Cardiovascular | 9445 (8.8) | 2670 (8.4) | 113 (0.4) | 19 (0.3) |
| Non-specific chronic conditions | 7792 (7.2) | 2603 (8.2) | 1404 (5.3) | 383 (5.5) |
| Total Acute infectious conditions related | 35426 (17.3) | 9347 (16.1) | 70783 (19.7) | 17609 (18.3) |
| Total Injury related5 | 24620 (12.1) | 7953 (13.7) | 94225 (26.2) | 26709 (27.8) |
| Unintentional injuries | 23373 (94.9) | 7452 (93.7) | 748 (0.8) | 217 (0.8) |
| Intentional injuries | 859 (3.5) | 435 (5.5) | 1117 (1.2) | 333 (1.2) |
| Unspecified intent | 388 (1.6) | 66 (0.8) | 92360 (98.0) | 26159 (97.9) |
Each admission episode may have multiple diagnoses. Thus, the sum of the proportions of health conditions may exceed 100%.
The denominators for the propotion in italic were the total number of health service use on the first row; the denominators for other proportions were the category's total number of health service use
Chronic conditions that require severity criteria for identification were not included in the calculation of ED attendances. 4 Metabolic/endocrine/digestive/renal/genitourinary conditions
As there is only one diagnosis available in the ED data, the majority of injury records are coded with an ICD consequence code (ie, S or T codes) and do not have an external code that helps determine the intent involved in the injury.
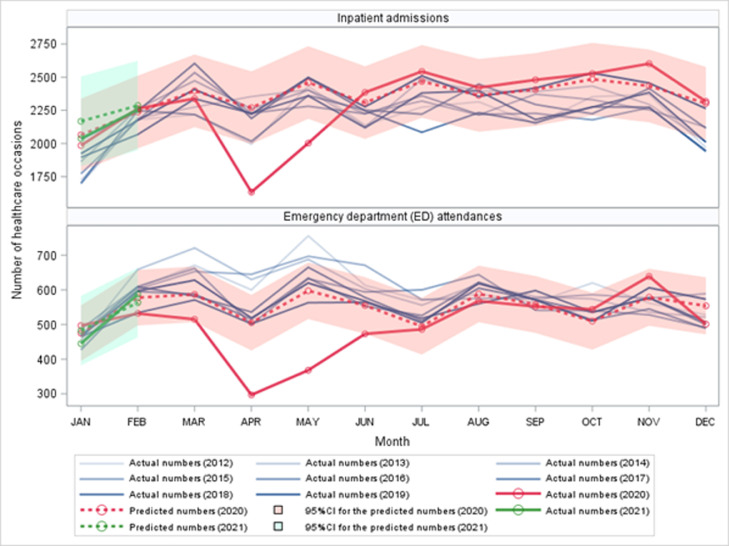
Chronic conditions
Table 3andFigure 2 show that the number of admissions related to any chronic condition was lower than predicted by 29.3% in April 2020 (observed n=1633, 95%CI 18.4%-37.6%) and 18.8% in May (n=2002, 95%CI 7.3%-27.9%). There was also a decrease in the number of ED attendances for any chronic condition than predicted by around 40% in both April (n=297, 40.8%, 95%CI 29.4%-49.0%) and May (n=368, 38.4%, 95%CI 27.8%-46.2%).
Table 3.
Observed number and predicted difference of health service use related to any chronic health condition in 2020 and 2021⁎
| Month in 2020 – 21 | Hospital inpatient admissions |
Emergency department (ED) attendances 2 |
||
|---|---|---|---|---|
| Observed number | Difference % (95%CI) 1 | Observed number | Difference % (95%CI) 1 | |
| JAN | 1985 | -6.99 (-18.67, 8.6) | 497 | -1.24 (-13.86, 15.72) |
| FEB | 2264 | -0.66 (-12.45, 14.79) | 532 | -10.81 (-20.65, 1.81) |
| MAR | 2338 | -3.11 (-14.05, 11.02) | 515 | -8.04 (-18.8, 6.00) |
| APR | 1633 | -29.26 (-37.58, -18.39)⁎⁎⁎ | 297 | -40.76 (-48.96, -29.4)⁎⁎⁎ |
| MAY | 2002 | -18.86 (-27.86, -7.3)⁎⁎ | 368 | -38.35 (-46.2, -27.81)⁎⁎⁎ |
| JUN | 2385 | 1.79 (-10.04, 17.21) | 473 | -15.53 (-26.92, 0.07) |
| JUL | 2543 | 2.66 (-8.71, 17.28) | 486 | -5.75 (-19.54, 13.75) |
| AUG | 2421 | 1.27 (-10.32, 16.3) | 568 | -5.05 (-17.57, 11.95) |
| SEP | 2480 | 2.12 (-9.42, 17.02) | 552 | -2.13 (-15.72, 16.69) |
| OCT | 2527 | 1.31 (-9.89, 15.67) | 544 | 3.41 (-11.86, 25.08) |
| NOV | 2602 | 6.05 (-5.85, 21.4) | 639 | 6.94 (-7.28, 26.32) |
| DEC | 2317 | -1.22 (-12.77, 13.86) | 501 | -11.56 (-23.89, 5.52) |
| JAN | 2037 | -10.42 (-22.86, 6.79) | 445 | -15.71 (-28.78, 3.23) |
| FEB | 2255 | -4.36 (-17.26, 13.29) | 587 | -0.88 (-14.8, 18.49) |
Percentage difference was calculated using the formula , where the predicted value was estimated based on the 2016-2019 monthly number of healthcare occasions using the autoregressive error models.
ED data do not include the chronic conditions that involve the severity criteria for identification (Hardelid et al. [24])
p<.001
p<.01
p<.05
Figure 2.
Health service use related to any chronic health condition in SCHN during the pre-COVID (years 2016-2019) and COVID (years 2020-2021) periods in NSW Australia.
Decrease in health service use occurred to most specific chronic conditions in April and May 2020, with a larger decrease for respiratory conditions (40-50% decrease for admissions and 77% decrease for ED attendances) and a smaller decrease for cancer/blood disorders (Supplementary Figures 2A-2B, Supplementary Tables 3A-3F). From June 2020, the monthly numbers of health service use related to most chronic conditions were generally within the pre-COVID predicted confidence intervals. The pattern described above was overall consistent across groups of patients by age, sex, and socioeconomic status (Supplementary Tables 4-6, Supplementary Figures 3-5).
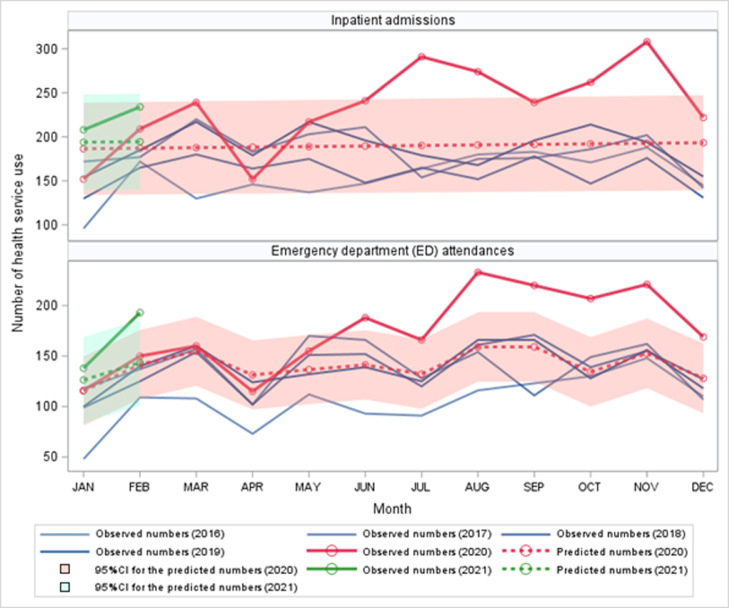
For mental health/behavioural disorders, inpatient admissions and ED attendances occurred mainly among children aged 12-17 years (Supplementary Table 7). Figure 3 shows no significant decrease in health service use related to mental health disorders during the lockdown period from mid-March to mid-May 2020. However, the numbers were consistently higher than predicted after the lockdown, by 25-55% for admissions from July to November 2020 and a similar increase for ED attendances from June 2020 to February 2021 (except January) (Table 4). The magnitude and duration of the increase in mental health related service use was generally greater for females (40-70% increase for inpatient admissions and ED attendances) than males (33-60% increase for inpatient admissions and no significant increase for ED attendances) (Supplementary Table 8) and higher among patients who lived in the most advantaged areas (42-80% increase for inpatient admissions and 35-111% increase for ED attendances) than those from less advantaged areas (Supplementary Table 9).
Figure 3.
Health service use related to any mental health/behaviour disorders in SCHN during the pre-COVID (years 2016-2019) and COVID-affected (years 2020-2021) periods in NSW Australia.
Table 4.
Observed number and predicted difference of health service use related to any mental health/behavioural disorders in 2020 and 2021
| Month in 2020 – 21 | Hospital inpatient admissions |
Emergency department (ED) attendances 2 |
||
|---|---|---|---|---|
| Observed number | Difference % (95%CI) 1 | Observed number | Difference % (95%CI) 1 | |
| JAN | 152 | -18.51 (-36.38, 13.32) | 116 | 0.48 (-22.47, 42.7) |
| FEB | 209 | 11.68 (-12.8, 55.25) | 150 | 5.9 (-14.69, 39.61) |
| MAR | 239 | 27.29 (-0.6, 76.9) | 160 | 3.38 (-15.34, 32.75) |
| APR | 152 | -19.31 (-36.98, 12.11) | 115 | -12.43 (-30.55, 18.5) |
| MAY | 217 | 14.81 (-10.31, 59.49) | 155 | 13.46 (-9.32, 51.52) |
| JUN | 241 | 27.09 (-0.71, 76.53) | 188 | 33.1 (7.06, 75.87)⁎⁎ |
| JUL | 291 | 52.96 (19.51, 112.43)⁎⁎⁎ | 166 | 25.59 (-0.34, 69.77) |
| AUG | 274 | 43.56 (12.17, 99.35)⁎⁎ | 233 | 46.53 (20.44, 87.03)⁎⁎⁎ |
| SEP | 239 | 24.82 (-2.47, 73.31) | 220 | 38.29 (13.66, 76.56)⁎⁎⁎ |
| OCT | 262 | 36.39 (6.57, 89.37)* | 207 | 54.09 (22.59, 107.39)⁎⁎⁎ |
| NOV | 308 | 59.82 (24.88, 121.9)⁎⁎⁎ | 221 | 44.74 (18.02, 87.1)⁎⁎⁎ |
| DEC | 222 | 14.82 (-10.28, 59.44) | 169 | 32.10 (3.97, 81.09)* |
| JAN | 208 | 7.24 (-16.21, 48.91) | 138 | 9.23 (-18.27, 64.62) |
| FEB | 234 | 20.26 (-6.04, 67.01) | 193 | 34.49 (3.70, 91.27)* |
Percentage difference was calculated using the formula , where the predicted value was estimated based on the 2016-2019 monthly number of healthcare occasions using the autoregressive error models.
ED data do not include the chronic conditions that involve the severity criteria for identification (Hardelid et al. [24])
p<.001
p<.01
p<.05
Acute infectious conditions
Health service use for acute infectious conditions mainly occurred among children younger than 5 years (Supplementary Table 10). Table 5 shows the numbers in April and May 2020 were 46-62% lower for inpatient admissions and 71% lower for ED attendances than predicted. After the lockdown, the number of acute infectious conditions remained lower than predicted up to October 2020 (16-38% lower for inpatient admissions and 35-56% lower for ED attendances), with around 10% increase in November and December 2020 (Figure 4). This pattern was consistent across patients by sex and socioeconomic status (Supplementary Tables 11-12).
Table 5.
Observed number and predicted difference of health service use related to acute infectious conditions in 2020 and 2021
| Month in 2020 – 21 | Hospital inpatient admissions |
Emergency department (ED) attendances |
||
|---|---|---|---|---|
| Observed number | Difference % (95%CI) 1 | Observed number | Difference % (95%CI) 1 | |
| JAN | 633 | -6.51 (-21.31, 15.14) | 1373 | -18.81 (-30.97, -1.43)* |
| FEB | 725 | 2.74 (-14.19, 28) | 1600 | -4.27 (-21.14, 21.78) |
| MAR | 725 | -9.97 (-23.45, 9.28) | 1781 | 5.27 (-14.13, 35.98) |
| APR | 337 | -61.77 (-67.09, -54.39)⁎⁎⁎ | 492 | -71.45 (-76.76, -62.98)⁎⁎⁎ |
| MAY | 480 | -46.06 (-53.52, -35.75)⁎⁎⁎ | 512 | -71.8 (-76.89, -63.82)⁎⁎⁎ |
| JUN | 583 | -37.3 (-45.65, -25.9)⁎⁎⁎ | 833 | -55.69 (-63.52, -43.56)⁎⁎⁎ |
| JUL | 634 | -35.65 (-43.81, -24.72)⁎⁎⁎ | 869 | -54.2 (-62.28, -41.72)⁎⁎⁎ |
| AUG | 633 | -37.65 (-45.35, -27.43)⁎⁎⁎ | 985 | -47.7 (-57.01, -33.23)⁎⁎⁎ |
| SEP | 759 | -23.08 (-32.82, -10.03)⁎⁎⁎ | 1171 | -35.47 (-47.35, -16.67)⁎⁎⁎ |
| OCT | 760 | -16.22 (-27.64, -0.52)* | 1433 | -18.65 (-34.03, 6.07) |
| NOV | 954 | 11.16 (-4.74, 33.44) | 1998 | 10.52 (-9.97, 43.1) |
| DEC | 889 | 7.54 (-8.35, 30.09) | 2012 | 11.56 (-9.95, 46.56) |
| JAN | 584 | -24.65 (-37.71, -4.65)⁎⁎ | 1218 | -32.17 (-45.93, -9.02)⁎⁎ |
| FEB | 651 | -15.41 (-31.13, 9.6) | 1332 | -25.9 (-41.52, 1.13) |
Percentage difference was calculated using the formula , where the predicted value was estimated based on the 2016-2019 monthly number of healthcare occasions using the autoregressive error models.
p<.001
p<.01
p<.05
Figure 4.
Health service use related to acute infectious conditions in SCHN during the pre-COVID (years 2016-2019) and COVID-affected (years 2020-2021) periods in NSW Australia.
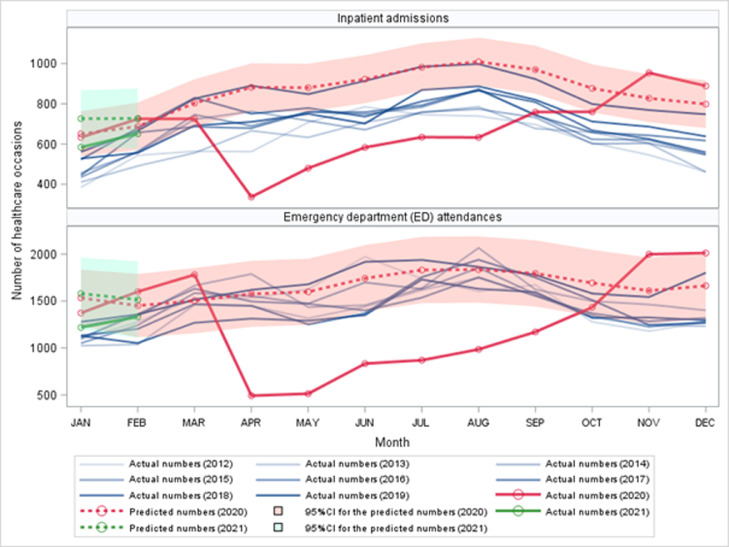
Injury
Injury-related health service use mainly occurred among children older than 1 year (Supplementary Table 13). The number of injury-related inpatient admissions during the first state-wide lockdown was not significantly different from predicted, but it was generally 35-48% higher than predicted from July to December 2020 (Table 6, Figure 5). In contrast, the number of injury-related ED attendances was 23% lower than predicted in April and May 2020; however, it was around 20% higher than predicted in August and September 2020, specifically for males (Supplementary Table 14). This post-lockdown increase in injury-related health service use was generally higher for children aged 5-11 years (Supplementary Table 13) and those from more advantaged areas (Supplementary Table 15).
Table 6.
Observed number and predicted difference of health service use related to injuries in 2020 and 2021
| Month in 2020 – 21 | Hospital inpatient admissions |
Emergency department (ED) attendances |
||
|---|---|---|---|---|
| Observed number | Difference % (95%CI) 1 | Observed number | Difference % (95%CI) 1 | |
| JAN | 535 | 15.34 (-5.87, 48.88) | 1868 | 8.49 (-4.96, 26.39) |
| FEB | 452 | -0.92 (-20.74, 32.12) | 1774 | 1.17 (-11.19, 17.53) |
| MAR | 548 | 21.25 (-3.62, 63.44) | 1691 | -13.14 (-22.82, -0.68) * |
| APR | 488 | 8.71 (-13.89, 47.39) | 1420 | -23.26 (-32.22, -11.58)⁎⁎⁎ |
| MAY | 513 | 14.94 (-9.19, 56.53) | 1549 | -22.87 (-31.25, -12.17)⁎⁎⁎ |
| JUN | 531 | 19.62 (-5.71, 63.58) | 1763 | -1.41 (-13.29, 14.24) |
| JUL | 597 | 35.21 (6.33, 85.64)* | 1851 | 5.8 (-7.2, 23.05) |
| AUG | 653 | 48.69 (16.66, 104.96)⁎⁎⁎ | 2240 | 18.94 (5.23, 36.77)⁎⁎ |
| SEP | 608 | 39.18 (8.95, 92.66)⁎⁎ | 2243 | 22.15 (7.73, 41.02)⁎⁎ |
| OCT | 637 | 46.61 (14.48, 103.8)⁎⁎ | 2144 | 11.67 (-1.01, 28.08) |
| NOV | 600 | 38.84 (8.16, 93.84)⁎⁎ | 2184 | 9.21 (-2.76, 24.55) |
| DEC | 630 | 46.58 (13.9, 105.56)⁎⁎ | 2107 | 8.99 (-3.33, 24.92) |
| JAN | 578 | 35.22 (4.8, 90.5)* | 1890 | 8.77 (-7.21, 31.39) |
| FEB | 583 | 37.14 (6.02, 94.11)* | 1985 | 13.01 (-3.46, 36.27) |
Percentage difference was calculated using the formula , where the predicted value was estimated based on the 2016-2019 monthly number of healthcare occasions using the autoregressive error models.
p<.001
p<.01
p<.05
Figure 5.
Health service use related to injuries in SCHN during the pre-COVID (years 2016-2019) and COVID-affected (years 2020-2021) periods in NSW Australia.
Discussion
To our knowledge, this is the first study to examine the long-term (one year since the lockdown started) impact of the COVID-19 pandemic on paediatric health service use for a wide range of health conditions at a large state-wide paediatric healthcare provider. Our findings converge with previous research showing rapidly reduced paediatric health service use following the implementation of the lockdown1,3,29 and that the decline for most chronic conditions was only evident during the lockdown. After the lockdown, the service use generally returned to the pre-COVID predicted levels. However, there was a persistent increase in health service use related to mental health disorders and injuries, and a persistent reduction for acute infectious conditions after the lockdown.
The immediate return to pre-COVID predicted levels for most chronic health conditions post-lockdown has highlighted the healthcare needs for children affected by chronic conditions. Similar to previous studies, the reduction in health service use was largely related to chronic respiratory conditions such as asthma6,12,29; while, smaller reductions occurred in cancer and metabolic conditions3,.6,29 The duration of decline in health service use related to chronic conditions was shorter in this study than that reported in the US where the reduction in health service use lingered for at least three months with extended pandemic12,.29,30 Further, the reduction during the lockdown was generally not translated into significantly excessive occasions of health service use for chronic conditions post-lockdown within the study period. These findings may be attributable to the sharp and stringent social restriction measures implemented across Australia compared to most other nations when the pandemic emerged in early 2020. These measures include national border closure, hotel quarantine for returning Australians, suspension of elective surgeries, restrictions on social gatherings, and partial school closure. These measures helped to effectively control the community transmission of COVID-19, resulting in low case numbers and rapid easing of restrictions in NSW. Additionally, SCHN ramped up proactive telehealth outpatient care during the pandemic, and this may have helped avoid the accumulation of a large number of patients with unmet healthcare needs during the lockdown, which may otherwise have overburdened the healthcare systems.31
Mental health problems have been one of the major concerns during the COVID-19 pandemic. Online surveys of community samples of children and adolescents have shown three-quarters of the sample experienced worsening mental health difficulties in Australian (72% were girls),32 higher than other countries (one-third to two-thirds) during the early months of the pandemic33, 34, 35. To our knowledge, this current study is the first to show a persistent increase in paediatric mental health related hospital service use within a year after the pandemic outbreak. This trend is in line with the increased use of crisis and online mental health services in NSW.36 Further, the number of new clients of all-age group visiting community mental health services increased by 14% in June after a 6% decrease during the lockdown in NSW.37 The surge in mental health problems may be associated with the widespread social isolation, pandemic-related financial difficulties, and reduced access to mental health services.38 Research in 2015 has shown that 50% and 40% of Australian 4-17 year olds with mental health problems received community- and school-based mental health services respectively, and this proportion increased to 80% and 70% for those with severe mental health problems.39 Reduced access to these services during the pandemic may have not only aggravated the symptoms of children with existing mental health difficulties, but also disrupted their contact with the safety network of schools, peers, health and social welfare professionals that play a key role in supporting children's socioemotional wellbeing20,.32,40
The post-pandemic increase in mental health related health service use should be understood in the context of a steady increase in mental health problems among young people over the last decade both within Australia and internationally.41,42 The pandemic and the lockdown measures have potentially exacerbated (and reinforced) the long-standing issues among young people, such as social disconnectedness, loneliness, and uncertainty about their future.41,42 Our findings call for additional and sustained support to address these issues. The Australian Government has introduced health and financial packages to mitigate the impact of the pandemic on people's mental health outcomes, such as Better Access Pandemic Support which provides additional subsidised psychological therapy sessions to people affected by a psychiatric disorder.
Our results show the increase in mental health related service use was more noticeable among adolescent girls. This is consistent with the findings of several studies showing a higher prevalence of emotional problems among girls than boys during the COVID-19 pandemic.34,43 Research has shown crises like the COVID-19 pandemic is more likely to induce depression, anxiety, and post-traumatic stress disorder.38 These disorders are twice as likely to affect females than males.44,45 However, our finding does not suggest that boys need less mental health support. Research has shown more boys than girls experienced a deterioration in externalising problems or neurodevelopmental disorders during the pandemic.33,46 However, most patients with externalising disorders are likely to use community or private healthcare instead of inpatient or ED services.47 The reason for the greater increase in mental health related service use among children in the most socioeconomically advantaged group compared with their peers from less advantaged groups may be due to differences in access to relevant services, with most community-based private clinics being closed during the lockdown necessitating those from socioeconomically advantaged background to seek help from public services. Research from Norway43 and Canada35 found that children from families with more economic difficulties had a smaller increase in emotional problems during the pandemic. Like Canada, the Australian government provided financial and employment assistance packages such as the Coronavirus Supplement and the JobKeeper Payment, which may have benefited low-income families more in the sense that these financial benefits may have exceeded incomes from low-paying employment,35 thus resulting in less familial financial distress.
The persistently reduced health service use for acute infectious conditions is corroborated by previous research5,.12,29 This reduction may be associated with the effects of social lockdown and good hygiene practice, suggesting that the risk of paediatric acute infections is modifiable by changes in health and social behaviours.5,48 Further, our result of the increase in acute infections related hospital service use towards the end of year 2020 suggests a shifted season for acute infections, which has been evidenced in other Australian studies particularly on respiratory syncytial virus.49,50
During the lockdown, there was a 30% reduction in injury-related ED attendances, which was consistent with previous research.51,52 However, there was a significant increase after the lockdown, particularly for inpatient admissions. This may be because children spent more time indoors even during the post-lockdown period hence being more subject to home environmental factors conducive to injuries.
Strengths and Limitations
The strength of our study is the unique experiences within one year after the pandemic outbreak in NSW in 2020, which has enabled us to examine the long-term change in paediatric health service use. This study was based on routinely collected administrative health data comprising all hospital admissions and ED attendances with records systematically coded by the main tertiary paediatric healthcare provider.
This study has several limitations. We could not delineate to what extent the reduction in health service use was attributed to decreases in incidence, parent-initiated hospital avoidance, or reduced access to health services. Second, the sample size was small for some critical conditions in a crisis like the COVID-19 pandemic such as assault and maltreatment, especially when we stratified the analysis by sociodemographic factors. Third, only 2% of injury-related ED attendances were coded with an intent, limiting our capacity to explore health service use for injuries. Fourth, we identified health conditions using both principal and additional diagnoses, but we could not determine how an additional diagnosis contributed to the admission. However, we used the same method to identify health conditions over time to ensure the comparability before and during the pandemic. Last, we did not have primary healthcare data, which has limited our capacity to understand the full picture of health service use by children during the pandemic, and how the lockdown has delayed the diagnosis or the treatment of children whose health condition requires a timely delivery of care. A study on healthcare activity in NSW has shown a 22% decrease in primary care consultations from March to June 2020, with no specific information for children,37 thus further investigations are warranted.
Conclusion
Health service use decreased during the sharp lockdown in NSW in 2020, but the use of services for most chronic health conditions returned to the pre-COVID-19 levels immediately after the lockdown. Public health measures used to contain the spread of COVID-19 may have been effective in reducing acute infections in young children. The persistent increase in paediatric mental health related presentations after the pandemic highlights the need for sustained and targeted delivery of mental health services for children during and beyond the pandemic. It is important to monitor the direct and the indirect child health outcomes as the pandemic evolves in years to come.
Contributors
RL and NH conceptualised the study. JS provided the data. NH analysed the data and completed the first manuscript. All authors edited the manuscript and contributed to results interpretation. NH and JS had full access to all the data analysed in this study. All authors have reviewed and approved the final manuscript.
Data sharing statement
Data used in these analyses are held by the Sydney Children's Hospitals Network (SCHN). Data are only available on request to SCHN with appropriate ethical approval for use.
Declaration of Competing Interest
We declare no competing interests.
Acknowledgments
We acknowledged the Sydney Children's Hospitals Network for providing the data.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lanwpc.2021.100311.
Appendix. Supplementary materials
References
- 1.Isba R, Edge R, Jenner R, Broughton E, Francis N, Butler J. Where have all the children gone? Decreases in paediatric emergency department attendances at the start of the COVID-19 pandemic of 2020. Archives of Disease in Childhood. 2020;105(7):704. doi: 10.1136/archdischild-2020-319385. [DOI] [PubMed] [Google Scholar]
- 2.Keyes D, Hardin B, Sweeney B, Shedden K. Change in urban and non-urban pattern of ED use during the COVID-19 pandemic in 28 Michigan hospitals: an observational study. BMJ Open. 2021;11(2) doi: 10.1136/bmjopen-2020-043024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dopfer C, Wetzke M, Zychlinsky Scharff A, et al. COVID-19 related reduction in pediatric emergency healthcare utilization – a concerning trend. BMC Pediatrics. 2020;20(1):427. doi: 10.1186/s12887-020-02303-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang H, Guo L-W, Gao Y-Y, Yao H, Xie Z-K, Zhang W-X. The Impact of the COVID-19 Pandemic on Pediatric Clinical Practice in Wenzhou, China: A Retrospective Study. Frontiers in Pediatrics. 2020;8(664) doi: 10.3389/fped.2020.585629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Britton PN, Hu N, Saravanos G, et al. COVID-19 public health measures and respiratory syncytial virus. Lancet Child Adolesc Health. 2020;4(11):e42–ee3. doi: 10.1016/S2352-4642(20)30307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DeLaroche AM, Rodean J, Aronson PL, et al. Pediatric Emergency Department Visits at US Children's Hospitals During the COVID-19 Pandemic. Pediatrics. 2020 doi: 10.1542/peds.2020-039628. [DOI] [PubMed] [Google Scholar]
- 7.Kadambari S, Abo Y-N, Phuong LK, Osowicki J, Bryant PA. Decrease in Infection-related Hospital Admissions During COVID-19: Why Are Parents Avoiding the Doctor? The Pediatric Infectious Disease Journal. 2020;39(11):e385–e3e6. doi: 10.1097/INF.0000000000002870. [DOI] [PubMed] [Google Scholar]
- 8.Watson G, Pickard L, Williams B, Hargreaves D, Blair M. ‘Do I, don't I?’ A qualitative study addressing parental perceptions about seeking healthcare during the COVID-19 pandemic. Archives of Disease in Childhood. 2021 doi: 10.1136/archdischild-2020-321260. archdischild-2020-321260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brooks JT, Butler JC. Effectiveness of Mask Wearing to Control Community Spread of SARS-CoV-2. JAMA. 2021;325(10):998–999. doi: 10.1001/jama.2021.1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brisca G, Vagelli G, Tagliarini G, et al. The impact of COVID-19 lockdown on children with medical complexity in pediatric emergency department. Am J Emerg Med. 2021;42:225–227. doi: 10.1016/j.ajem.2020.11.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Graetz D, Agulnik A, Ranadive R, et al. Global effect of the COVID-19 pandemic on paediatric cancer care: a cross-sectional study. The Lancet Child & Adolescent Health. 2021;5(5):332–340. doi: 10.1016/S2352-4642(21)00031-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pelletier JH, Rakkar J, Au AK, Fuhrman D, Clark RSB, Horvat CM. Trends in US Pediatric Hospital Admissions in 2020 Compared With the Decade Before the COVID-19 Pandemic. JAMA Network Open. 2021;4(2) doi: 10.1001/jamanetworkopen.2020.37227. e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liguoro I, Pilotto C, Vergine M, Pusiol A, Vidal E, Cogo P. The impact of COVID-19 on a tertiary care pediatric emergency department. Eur J Pediatr. 2021;180(5):1497–1504. doi: 10.1007/s00431-020-03909-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goldman RD, Grafstein E, Barclay N, Irvine MA. Portales-Casamar E. Paediatric patients seen in 18 emergency departments during the COVID-19 pandemic. Emergency Medicine Journal. 2020;37(12):773–777. doi: 10.1136/emermed-2020-210273. [DOI] [PubMed] [Google Scholar]
- 15.Cheek JA, Craig SS, West A, Lewena S, Hiscock H. Emergency department utilisation by vulnerable paediatric populations during the COVID-19 pandemic. Emerg Med Australas. 2020;32(5):870–871. doi: 10.1111/1742-6723.13598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization. WHO Coronavirus Disease COVID-19) dashboard. 2021 https://covid19.who.int/ (accessed 07 June 2021. [Google Scholar]
- 17.Data NSW NSW COVID-19 cases data. 2021 https://data.nsw.gov.au/nsw-covid-19-data/cases [Google Scholar]
- 18.NSW Health COVID-19 weekly surveillance in NSW epidemiological week 23. ending 12 June 2021. 2021 [Google Scholar]
- 19.NSW Health COVID-19 weekly surveillance in NSW epidemiological week 32. ending 14 August 2021. 2021 [Google Scholar]
- 20.Golberstein E, Wen H, Miller BF. Coronavirus Disease 2019 (COVID-19) and Mental Health for Children and Adolescents. JAMA Pediatrics. 2020;174(9):819–820. doi: 10.1001/jamapediatrics.2020.1456. [DOI] [PubMed] [Google Scholar]
- 21.Bambra C, Riordan R, Ford J, Matthews F. The COVID-19 pandemic and health inequalities. Journal of Epidemiology and Community Health. 2020;74(11):964–968. doi: 10.1136/jech-2020-214401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lawley M, Truran D, Hansen D, Good N, Staib A, Sullivan C. SnoMAP: Pioneering the Path for Clinical Coding to Improve Patient Care. Studies in health technology and informatics. 2017;239:55–62. [PubMed] [Google Scholar]
- 23.Child G, Collaborators AH Diseases, Injuries, and Risk Factors in Child and Adolescent Health, 1990 to 2017: Findings From the Global Burden of Diseases, Injuries, and Risk Factors 2017 Study. JAMA Pediatrics. 2019;173(6) doi: 10.1001/jamapediatrics.2019.0337. e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.AIHW . Cat. no. PHE 167. Australian Institute of Health and Welfare; Canberra: 2012. A picture of Australia's children 2012. [Google Scholar]
- 25.Braithwaite J, Hibbert PD, Jaffe A, et al. Quality of health care for children in Australia, 2012-2013. Jama. 2018;319(11):1113–1124. doi: 10.1001/jama.2018.0162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.AIHW . Australian Institute of Health Welfare; Canberra: 2021. Hospitalised injury in children and young people, 2017–18. [Google Scholar]
- 27.Australian Bureau of Statistics . Australian Bureau of Statistics; Canberra: 2008. An introduction to socioeconomic indexes for areas (SEIFA), 2006. [Google Scholar]
- 28.SAS Institute Inc . SAS/ETS® 141 User's Guide. SAS Institute Inc; Cary, NC: 2015. Chapter 9 The AUTOREG Procedure. [Google Scholar]
- 29.Markham JL, Richardson T, DePorre A, et al. Inpatient Use and Outcomes at Children's Hospitals During the Early COVID-19 Pandemic. Pediatrics. 2021 doi: 10.1542/peds.2020-044735. [DOI] [PubMed] [Google Scholar]
- 30.Pines JM, Zocchi MS, Black BS, et al. Characterizing pediatric emergency department visits during the COVID-19 pandemic. Am J Emerg Med. 2021 doi: 10.1016/j.ajem.2020.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.SCHN . Sydney Children's Hospitals Network; Sydney: 2021. Sydney Children's Hospitals Network 2020 Annual Review. [Google Scholar]
- 32.Li SH, Beames JR, Newby JM, Maston K, Christensen H, Werner-Seidler A. The impact of COVID-19 on the lives and mental health of Australian adolescents. Eur Child Adolesc Psychiatry. 2021:1–13. doi: 10.1007/s00787-021-01790-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ravens-Sieberer U, Kaman A, Erhart M, Devine J, Schlack R, Otto C. Impact of the COVID-19 pandemic on quality of life and mental health in children and adolescents in Germany. European Child & Adolescent Psychiatry. 2021 doi: 10.1007/s00787-021-01726-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhou S-J, Zhang L-G, Wang L-L, et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. European Child & Adolescent Psychiatry. 2020;29(6):749–758. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cost KT, Crosbie J, Anagnostou E, et al. Mostly worse, occasionally better: impact of COVID-19 pandemic on the mental health of Canadian children and adolescents. European Child & Adolescent Psychiatry. 2021 doi: 10.1007/s00787-021-01744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Australian Institute of Health and Welfare Mental health services in Australia. 2021 https://www.aihw.gov.au/reports/mental-health-services/mental-health-services-in-australia/report-contents/mental-health-impact-of-covid-19#references AIHW. [Google Scholar]
- 37.Sutherland K, Chessman J, Zhao J, et al. Impact of COVID-19 on healthcare activity in NSW, Australia. Public Health Res Pract. 2020;30(4) doi: 10.17061/phrp3042030. [DOI] [PubMed] [Google Scholar]
- 38.Guessoum SB, Lachal J, Radjack R, et al. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Johnson SE, Lawrence D, Hafekost J, et al. Service use by Australian children for emotional and behavioural problems: Findings from the second Australian Child and Adolescent Survey of Mental Health and Wellbeing. Aust N Z J Psychiatry. 2016;50(9):887–898. doi: 10.1177/0004867415622562. [DOI] [PubMed] [Google Scholar]
- 40.Tromans S, Chester V, Harrison H, Pankhania P, Booth H, Chakraborty N. Patterns of use of secondary mental health services before and during COVID-19 lockdown: observational study. BJPsych Open. 2020;6(6):e117. doi: 10.1192/bjo.2020.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Twenge JM, Cooper AB, Joiner TE, Duffy ME, Binau SG. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005-2017. J Abnorm Psychol. 2019;128(3):185–199. doi: 10.1037/abn0000410. [DOI] [PubMed] [Google Scholar]
- 42.Hall S, Fildes J, Perrens B, et al. Mission Australia; Sydney, NSW: 2019. Can we Talk? Seven Year Youth Mental Health Report - 2012-2018. [Google Scholar]
- 43.Hafstad GS, Sætren SS, Wentzel-Larsen T, Augusti E-M. Adolescents’ symptoms of anxiety and depression before and during the Covid-19 outbreak – A prospective population-based study of teenagers in Norway. The Lancet Regional Health – Europe. 2021;5 doi: 10.1016/j.lanepe.2021.100093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Thapar A, Collishaw S, Pine DS, Thapar AK. Depression in adolescence. The Lancet. 2012;379(9820):1056–1067. doi: 10.1016/S0140-6736(11)60871-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Trickey D, Siddaway AP, Meiser-Stedman R, Serpell L, Field AP. A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clinical Psychology Review. 2012;32(2):122–138. doi: 10.1016/j.cpr.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 46.Masi A, Mendoza Diaz A, Tully L, et al. Impact of the COVID-19 pandemic on the well-being of children with neurodevelopmental disabilities and their parents. J Paediatr Child Health. 2021;57(5):631–636. doi: 10.1111/jpc.15285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lawrence D, Johnson S, Hafekost J, Boterhoven DHK, Sawyer M AJ, Zubrick S. Department of Health; Canberra, ACT, Australia: 2015. The Mental Health of Children and Adolescents: Report on the Second Australian Child and Adolescent Survey of Mental Health and Wellbeing. [Google Scholar]
- 48.Yeoh DK, Foley DA, Minney-Smith CA, et al. Impact of Coronavirus Disease 2019 Public Health Measures on Detections of Influenza and Respiratory Syncytial Virus in Children During the 2020 Australian Winter. Clinical Infectious Diseases. 2020;72(12):2199–2202. doi: 10.1093/cid/ciaa1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.McNab S, Ha Do LA, Clifford V, et al. Changing Epidemiology of Respiratory Syncytial Virus in Australia - delayed re-emergence in Victoria compared to WA/NSW after prolonged lock-down for COVID-19. Clin Infect Dis. 2021 doi: 10.1093/cid/ciab240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Saravanos G, Hu N, Homaira N, et al. RSV epidemiology in children in southeast Australia before and during COVID-19. Under rebuttals/revisions. 2021 [Google Scholar]
- 51.Choi DH, Jung JY, Suh D, et al. Impact of the COVID-19 Outbreak on Trends in Emergency Department Utilization in Children: a Multicenter Retrospective Observational Study in Seoul Metropolitan Area, Korea. J Korean Med Sci. 2021;36(5):e44. doi: 10.3346/jkms.2021.36.e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Palmer CS, Teague WJ. Childhood injury and injury prevention during COVID-19 lockdown - stay home, stay safe? Injury. 2021;52(5):1105–1107. doi: 10.1016/j.injury.2021.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.