Abstract
Background:
The purpose of this retrospective study was to clarify the operative outcomes of the side-locking loop suture (SLLS) technique accompanied by autologous semitendinosus tendon grafting for chronic Achilles tendon rupture.
Methods:
A chart review was conducted of consecutive patients treated with the SLLS technique at our department from 2012 to 2017. Postoperatively, a below-knee splint was applied for 2 weeks in 20 degrees of plantar flexion and then active range of motion exercise was started. Partial weightbearing exercise was allowed at 4 weeks according to patient tolerance, and full weightbearing without crutches was allowed at 8 weeks. The American Orthopaedic Foot & Ankle Society (AOFAS) ankle-hindfoot scale score and the Achilles tendon rupture score (ATRS) were used to evaluate clinical outcomes preoperatively and at the final follow-up.
Results:
Ten patients (6 men, 4 women) were included in the analysis. Mean AOFAS ankle-hindfoot scale score increased significantly from 64.2 ± 5.6 points preoperatively to 95.0 ± 5.3 points at the final follow-up (P < .001). The mean ATRS also increased significantly from 29.8 ± 4.4 points to 86.2 ± 7.7 points, respectively (P < .001). Mean time between surgery and ability to perform 20 continuous double-leg heel raises of the operated foot was 13.5 ± 3.4 (range 10-18) weeks. One patient complained of postoperative hypoesthesia in the foot, which had spontaneously resolved by 3 months after surgery.
Conclusion:
The SLLS technique accompanied by autologous semitendinosus tendon grafting provided successful operative outcomes for patients with chronic Achilles tendon rupture regardless of the size of the defect, and thus long-term orthotic use was not needed after surgery.
Level of Evidence:
Level IV, retrospective case series.
Keywords: chronic Achilles tendon rupture, side-locking loop suture, autologous semitendinosus tendon grafting, early postoperative rehabilitation
Introduction
Chronic Achilles tendon rupture is commonly defined as Achilles tendon rupture that occurs at least 4-6 weeks after the initial injury. 3,23 Same as the acute Achilles tendon repair, end-to-end suturing can be used to repair the rupture site in the case with a small rupture gap (typically, <2.5 cm). 15 However, performing end-to-end suturing is typically challenging in such cases, and additional operative procedures are needed to reconstruct the degenerative tendon after rupture. Various reconstructive operative techniques are described in the literature, including V-Y tendon plasty, 10 turndown flap, 7 tendon transfer, 1,14,30 and autograft 16 -18 or allograft 9 reconstruction, and each has its own advantages and disadvantages as well as different postoperative protocols, including the application of a cast, splint fixation, or foot orthosis. 1,6,7,9,10,14,16 -18,24,26,27,30 As such, no gold standard procedure for chronic Achilles tendon rupture has been established.
In 2010, a new side-locking loop suture (SLLS) technique that provides a maximum tensile strength of approximately 900 to 950 N was reported for the repair of acute Achilles tendon rupture. 32 This suture technique consists of a core suture using a United States Pharmacopeia (USP) no. 5 braided polyblend suture and a peripheral suture with the addition of a cross-stitch suture using a USP no. 2 monofilament polypropylene suture. Compared with other suture technique such as Kessler suture, the high tensile strength afforded by SLLS technique allows the patient to walk without the use of an orthosis in the early postoperative period, 32 and several studies have reported successful outcomes for acute Achilles tendon rupture. 11,20,32,33 Since 2012, we have been treating chronic rupture of Achilles tendon using the SLLS technique and autologous semitendinosus tendon grafting, without the need for an orthosis during weightbearing exercise in the early postoperative period.
The purpose of this study was to clarify the operative outcomes of the SLLS technique accompanied by autologous semitendinosus tendon grafting for chronic Achilles tendon rupture. We hypothesized that SLLS accompanied by autologous semitendinosus tendon grafting can achieve good prognosis without the use of specific orthoses, such as controlled ankle motion boot and ankle foot orthoses, during rehabilitation in cases of chronic Achilles tendon rupture. To our knowledge, this is the first clinical study to report use of the SLLS technique accompanied by autologous semitendinosus tendon grafting for chronic Achilles tendon rupture.
Materials and Methods
This retrospective study was approved by the institutional review board of our hospital. Written informed consent was obtained from all participants.
Patients
A retrospective chart review was conducted of consecutive patients treated at our department from 2012 to 2017. Three senior foot and ankle surgeons performed all operative procedures and decided on pre- and postoperative care. The diagnosis of chronic rupture of Achilles tendon was made by a confirmed duration of more than 4 weeks between initial injury and the initial visit to our institution, disability in daily living (ie, in walking and climbing stars), inability to perform a single-limb heel raise, palpable defect or tenderness over the Achilles tendon, and a positive Thompson test. All patients underwent magnetic resonance imaging (MRI) to evaluate the rupture and determine the size of the defect. All cases included in this study had more than 40 mm rupture gap in the MRI evaluation. Operative treatment was indicated for all patients except those with poorly controlled heart disease, diabetes mellitus, peripheral vascular disease, or autoimmune disease, because those have a higher risk of wound infection than those without it. 5 Patients with less than 1 year of postoperative follow-up were excluded for the analysis of this study.
Operative Technique
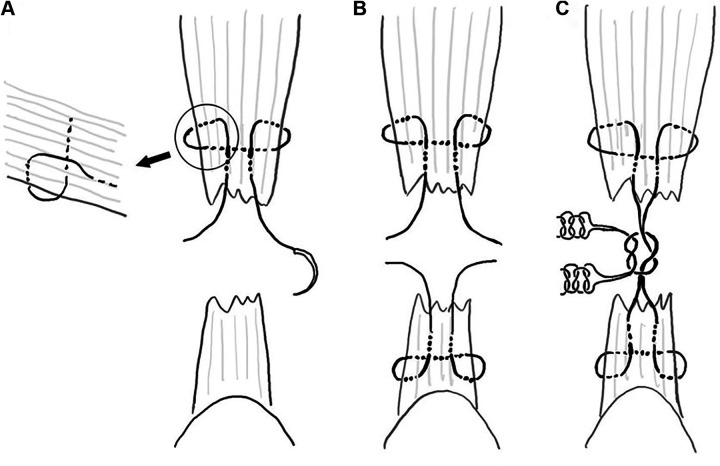
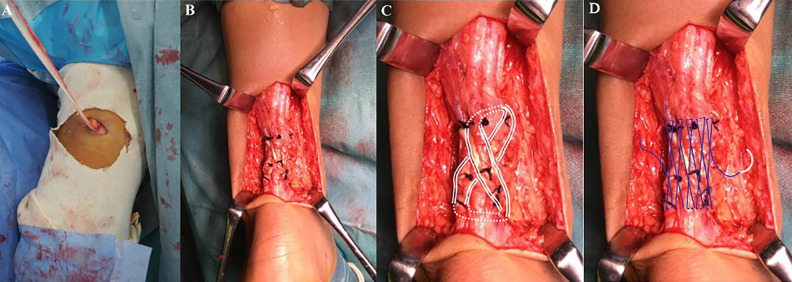
The surgery was performed under general or lumbar spinal anesthesia in the prone position with the application of a pneumatic tourniquet on the ipsilateral thigh. After inflation of the tourniquet to 280 mm Hg, the ruptured Achilles tendon was exposed through a longitudinal skin incision along the slightly medial to the center of Achilles tendon. We selected this approach because medial para-Achilles incision makes this procedure itself more complicated, and we want to avoid the skin break that may occur more frequently because of cutting the skin over the center of Achilles tendon. The remaining paratenon was gently dissected from the tendon, and scar tissue seen between the proximal and distal stumps was resected (Figure 1). The degenerative tendon tissue was adequately debrided, and the proximal side of the tendon stump was sutured using the SLLS technique with USP no. 5 braided polyblend suture (FiberWire; Arthrex Inc, Naples, FL). Figure 2 illustrates the SLLS technique. In the SLLS technique for the proximal stump, the transverse component of the suture was placed and the vertical component of the suture was then passed through the tendon from the posterior to the anterior at a point slightly proximal to the transverse component. Then, the longitudinal component of the suture was brought anterior to the tendon at a point slightly distal to the transverse component into the proximal part of the tendon. In the SLLS technique for the distal stump, the vertical component penetrated the tendon at a point slightly distal to the transverse component, and penetration with the longitudinal component was started at a point slightly proximal to the transverse component (Figure 2A). The 2 proximal and distal ends were tied with an anti-slip knot 19 as the core suture with the operated ankle in neutral position, which was decided based on the neutral position of the uninjured ankle. On this suture, we sutured both sides of the thread with a manual maximal pulling force for the thread applied at the proximal end and with a pulling force that resulted in neutral position of ankle plantar flexion for the thread applied at the distal end. For the anti-slip knot, first, a surgeon’s knot was made between each of the 2 proximal and 2 distal ends, and then both ends were secured with 3 throws in the manner of a reef knot (Figure 2B). Next, the ipsilateral autologous semitendinosus tendon was harvested through a small transverse incision at the medial side of the popliteal fossa using a tendon harvester (Figure 3A). After using the SLLS technique, all patients had a >20-mm gap between the tendons’ proximal and distal ends. The harvested semitendinosus tendon was then grafted onto the defect between each stump after placing a core suture with the SLLS technique. First, the autograft was passed through a small incision, which was created in the substance of the proximal stump at a level just distal to the transverse component of the SLLS. The graft was then pulled distally in a crisscross manner to form a figure of 8 on the defect between each tendon stump; each end of the autograft was passed through a small incision created in the substance of the distal stump at a level just proximal to the transverse component of the SLLS. The autograft was sutured to the Achilles tendon at each entry and exit point, and each end of the autograft was pulled up proximally and sutured to the proximal tendon stump (Figure 3B and C). Finally, a cross-stitch suture was added using a USP no. 2 monofilament polypropylene suture to reinforce the suture strength of SLLS technique 11,20,32,33 (Figure 3D).
Figure 1.
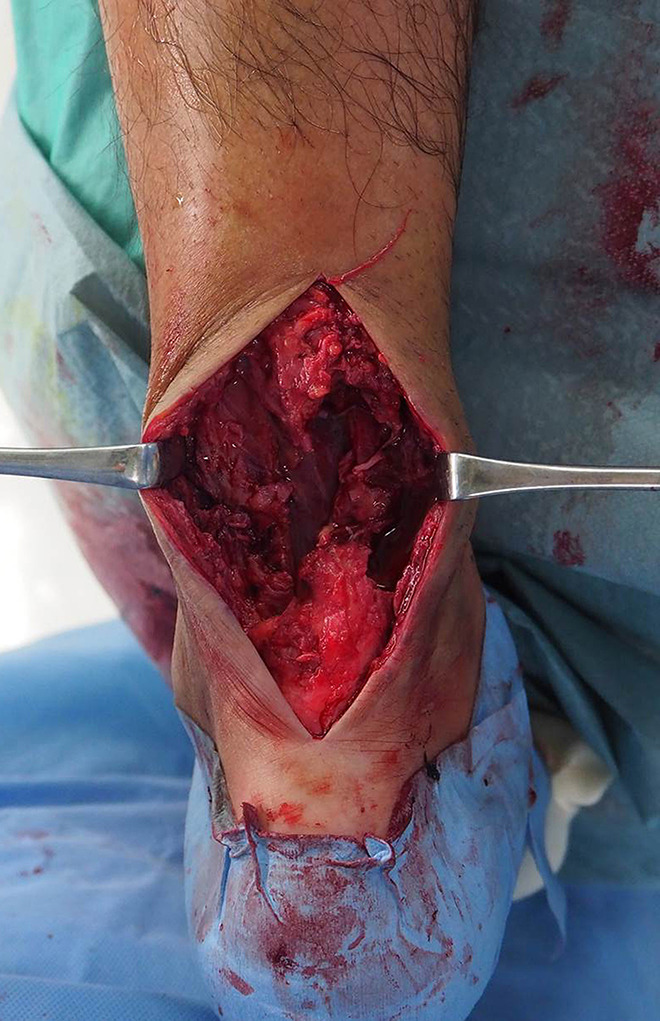
Intraoperative photograph showing the Achilles tendon with a large defect after debridement of degenerative tissue.
Figure 2.
Illustration showing the step-by-step procedure for the SLLS technique. (A) Application of the 2-strand SLLS technique on the proximal side. (B) Application of the 2-strand SLLS technique on the proximal and distal sides. (C) Anti-slip knot technique. First, the inside and outside are lumped together, and a surgeon’s knot is made between the 2 proximal and 2 distal sutures and then both ends are secured with 3 throws in the manner of a reef knot. SLLS, side-locking loop suture.
Figure 3.
Intraoperative photograph showing (A) harvest of the autologous semitendinosus tendon through a small transverse incision at the medial side of the popliteal fossa and (B and C) the grafted autologous semitendinosus tendon in a crisscross manner to form a figure of 8 on the defect. Finally, (D) a cross-stitch suture was added using a USP number 2 monofilament polypropylene suture.
Postoperative Protocol
A below-knee splint was applied with the ankle in 20 degrees of plantarflexion for 2 weeks postoperatively. At splint removal, the suture was also removed. Active range of motion exercise was started at this time. Partial weightbearing exercise was allowed at 4 weeks postoperatively according to patient tolerance, and full weightbearing without crutches was allowed at 8 weeks postoperatively. Double-leg heel raises and muscle strengthening exercises were started at this time, and once patients were able to perform 20 continuous double-leg heel raises, they were allowed to gradually engage in athletic exercises. They were subsequently advised to return to athletic activity only when they felt comfortable to do so.
Clinical Evaluation
Clinical outcomes were evaluated by comparing the preoperative American Orthopaedic Foot & Ankle Society (AOFAS) ankle-hindfoot scale score 12 and the Achilles tendon rupture score (ATRS) 22 with values obtained at the final follow-up. The AOFAS ankle-hindfoot scale score is not validated as an endpoint for Achilles tendon rupture. On the other hand, because the AOFAS ankle-hindfoot scale score is often used in the past literature, this study used the AOFAS ankle-hindfoot scale score, which is easy to compare with the results of past studies, and ATRS, which is validated as an evaluation item for Achilles tendon rupture. The time between surgery and ability to perform 20 continuous single-leg heel raises in the operated foot was determined for each patient. Furthermore, all patients were evaluated radiologically by MRI at 1 year postoperatively to confirm regeneration in the defect between each stump. Surgery-related complications were also recorded.
Statistical Analysis
Mean AOFAS ankle-hindfoot scale score and ATRS before surgery were compared with values obtained at final follow-up using the paired t test. All statistical analyses were performed using StatView version 5.0 software (SAS Institute Inc, Cary, NC). A P value <.001 was considered statistically significant.
Results
In total, 3 of 13 potentially eligible patients were excluded because 2 patients had less than 1 year of follow-up and surgery was contraindicated in 1 because of poorly controlled diabetes mellitus. Thus, 10 patients (6 men, 4 women; mean age 51.7 [range 33-72] years) were included in the final analysis (Table 1). Mean size of the tendon defect was 52.9 (range 40-68) mm. Mean duration of postoperative follow-up was 35.5 ± 13.4 (range 14-50) months.
Table 1.
Demographic Data of the Patients in This Series.
| Patient | Age (y) | Sex (F/M) | Side (L/R) | Time Between Injury and Surgery (mo) | Length of Defect (mm) | Postoperative Follow-up Period (mo) |
|---|---|---|---|---|---|---|
| 1 | 44 | M | R | 8 | 40 | 18 |
| 2 | 33 | M | L | 4 | 52 | 24 |
| 3 | 69 | M | L | 6 | 43 | 36 |
| 4 | 52 | M | L | 4 | 64 | 48 |
| 5 | 38 | F | L | 8 | 45 | 48 |
| 6 | 33 | F | L | 14 | 55 | 31 |
| 7 | 62 | F | L | 12 | 54 | 24 |
| 8 | 61 | M | L | 5 | 68 | 48 |
| 9 | 53 | M | L | 6 | 50 | 50 |
| 10 | 72 | F | L | 5 | 58 | 38 |
| Mean ± SD | 51.7 ± 14.3 | 4/6 | 9/1 | 7.2 ± 3.4 | 52.9 ± 8.9 | 36.5 ± 11.9 |
Abbreviations: F, female; L, left; M, male; R, right.
Tables 2 and 3 summarizes the clinical outcomes. Mean AOFAS ankle-hindfoot scale score increased significantly from 64.2 ± 5.6 (range 58-72) points preoperatively to 95.0 ± 5.3 (range 90-100) points at the final follow-up (P < .001), as did mean ATRS, from 29.8 ± 4.4 (range 22-35) points to 86.2 ± 7.7 (range 70-94), respectively (P < .001). Mean time between surgery and ability to perform 20 continuous double-leg heel raises of the operated foot was 13.5 ± 3.4 (range 10-18) weeks. One patient complained of postoperative hypoesthesia in the operated foot in an area corresponding to the area supplied mainly by the sural nerve; however, this spontaneously resolved by 3 months after surgery. None of the patients developed wound dehiscence needing a supplemental procedure or treatment for wound infection. Radiologic evaluation by MRI at 1 year after surgery revealed continuity of the Achilles tendon in all patients (Figure 4).
Table 2.
Clinical Outcomes.
| Score (Mean ± SD) | Preoperative | Final Follow-up | P Value |
|---|---|---|---|
| AOFAS ankle-hindfoot scale score | 64.2 ± 5.6 | 95.0 ± 5.3 | <.001 |
| ATRS | 29.5 ± 4.4 | 86.2 ± 7.7 | <.001 |
Abbreviations: AOFAS, American Orthopaedic Foot & Ankle Society ankle-hindfoot scale; ATRS, Achilles tendon rupture score; SD, standard deviation.
Table 3.
Breakdown of Outcomes of ATRS Score.a
| Age, Gender | Strength | Fatigue | Stiffness | Pain | ADL | Uneven Surfaces | Upstairs or Uphill | Running | Jumping | Physical Labor | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 44, M | 9 | 9 | 8 | 9 | 8 | 8 | 8 | 7 | 7 | 7 | 80 |
| 33, M | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 8 | 8 | 8 | 94 |
| 69, M | 8 | 9 | 8 | 8 | 8 | 7 | 8 | 8 | 7 | 8 | 79 |
| 52, M | 9 | 9 | 9 | 9 | 8 | 8 | 8 | 8 | 8 | 8 | 84 |
| 38, F | 10 | 10 | 9 | 10 | 10 | 10 | 9 | 8 | 8 | 8 | 92 |
| 33, F | 9 | 9 | 9 | 10 | 10 | 9 | 10 | 9 | 8 | 8 | 91 |
| 62, F | 8 | 7 | 7 | 8 | 8 | 7 | 7 | 6 | 6 | 6 | 70 |
| 61, M | 9 | 10 | 9 | 10 | 10 | 9 | 10 | 9 | 8 | 8 | 92 |
| 53, M | 9 | 9 | 10 | 9 | 10 | 10 | 9 | 8 | 8 | 8 | 90 |
| 72, F | 9 | 9 | 9 | 10 | 10 | 10 | 9 | 8 | 8 | 8 | 90 |
Abbreviations: ADL, activities of daily living; ATRS, Achilles Tendon Rupture Score, M, male, F, female.
a Items—Strength: Are you limited because of decreased strength in the calf / Achilles tendon / foot? Fatigue: Are you limited because of fatigue in the calf / Achilles tendon / foot? Stiffness: Are you limited because of stiffness in the calf / Achilles tendon / foot? Pain: Are you limited because of pain in the calf / Achilles tendon / foot? ADL: Are you limited during activities of daily living? Uneven surfaces: Are you limited when walking on uneven surfaces? Upstairs or uphill: Are you limited when walking quickly upstairs or uphill? Running: Are you limited during activities that include running? Jumping: Are you limited during activities that include jumping? Physical Labor: Are you limited in performing hard physical labor?
Figure 4.
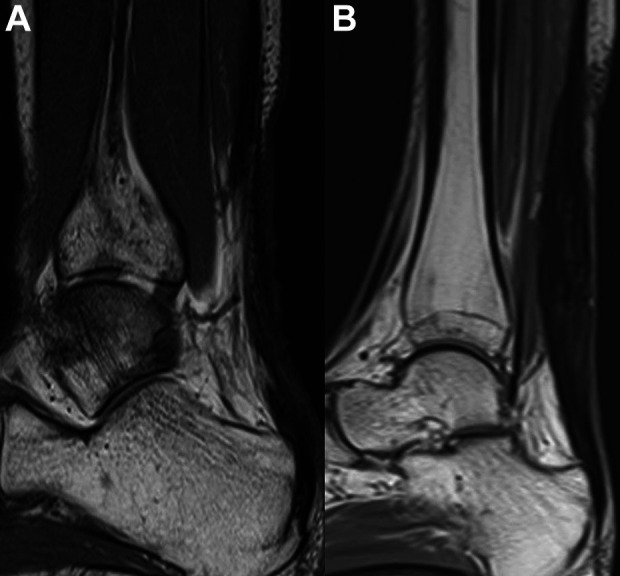
(A) Preoperative and (B) postoperative magnetic resonance image showing insufficient tendon tissue preoperatively compared with sufficient tendon tissue after reconstructive surgery.
Discussion
There is currently no operative treatment algorithm based on a high level of evidence that takes into account the size of a tendon defect in chronic Achilles tendon rupture. However, the gastrocnemius fascial V-Y advancement flap, Achilles tendon turn down flap, or flexor hallucis longus (FHL) tendon transfer techniques have been commonly used for intermediate-sized tendon defects. 13,27 Some studies have revealed good operative outcomes for the gastrocnemius fascial V-Y advancement flap and Achilles tendon turn down flap techniques, but these procedures seem to be disadvantaged by the loss of plantar flexion strength after surgery because of injury to part of the triceps surae. 4,15 FHL tendon transfer has also been reported as an effective procedure for chronic Achilles tendon rupture because the tendon is strong enough to substitute for the injured Achilles tendon and its axis closely replicates that of the tendon. 3 However, Lever et al 14 reported an approximate 60% loss of hallux interphalangeal joint flexion strength after harvesting the FHL tendon for the repair of chronic Achilles tendon rupture, and this may disturb daily barefoot activity, which is common in Japanese indoor life. On the other hand, a semitendinosus or gracilis tendon autograft, an allograft, or synthetic material has been recommended for large tendon defects, 4 defined as greater than 50 6,21 or 60 mm 6,16 -18 in length. Also, Yasuda et al 31 described a novel operative technique that applied Krackow sutures with the grafting using interposed scar tissue located between the tendon stumps. 30 Although these studies reported good prognosis for operative outcome, these procedures were accompanied by long-term immobilization with a cast, splint, or foot orthosis after surgery. 6,16 -18 This is because of the accompanying gastrocnemius fascial V-Y advancement flap, Achilles tendon turn down flap, and FHL tendon transfer, 1,7,9,14,30 interposed scar tissue, as the initial strength between stumps in these procedures was not enough strong to permit early movement of the ankle. The recent advancement of the Achilles tendon’s operative approach is a minimally invasive surgery, including a small skin incision and arthroscopic view. 19 Previous studies demonstrated the excellent outcomes via a minimally invasive tendon transfer; however, technical demand is a concern.
In the present study, we applied the SLLS technique using USP no. 5 braided polyblend suture as a core suture between stumps after adequate debridement of the degenerative tendon. 32 In 2010, Yotsumoto et al 33 performed a biomechanical study using bovine tendons of the medial heads of the gastrocnemius. They measured the ultimate tensile strength of the SLLS technique using a USP no. 5 braided polyblend suture and revealed the mean ultimate tensile strength to be 748 N. This is greater than 661 N, the reported tensile strength of the Achilles tendon during bicycle riding. 8 Because autologous semitendinosus tendon grafting was added to the technique described here, based on this biomechanical evidence we presumed the initial tensile strength would be greater than 748 N and we decided on a 2-week immobilization period, which is the conventional duration for normal healing of a sutured skin wound. We also decided to allow partial weightbearing exercise without any splint or orthosis at 4 weeks after surgery because we knew empirically that approximately 2 weeks were needed to achieve active dorsal flexion of 0° or more based on our perioperative observation of patients with acute Achilles tendon repair treated using the SLLS technique. 8
In this study, the SLLS technique accompanied by autologous semitendinosus tendon grafting was applied regardless of the size of the defect. Mean defect size in this study was 52.9 mm, and there were 3 cases with defects measuring less than 50 mm. Although these 3 cases could have been managed with the gastrocnemius fascial V-Y advancement flap, Achilles tendon turn down flap, or FHL tendon transfer technique, we had some concern about complications such as loss of plantar flexion strength or hallux interphalangeal joint flexion strength. 4,14,15 Furthermore, these procedures require long-term splinting or cast immobilization accompanied by the use of a foot orthosis postoperatively. 1,7,9,14,30 Regarding the technically demanding, the current technique is of relatively low difficulty because of the open approach that has been used for Acute Achilles tendon repair.
Harvesting the autologous semitendinosus tendon, which was performed via a small popliteal incision in this study, is an established operative procedure in anterior cruciate ligament reconstructive surgery, 28 and studies with high-level evidence have demonstrated regeneration of the harvested semitendinosus tendon after surgery. 25,29 The patients included in this study had no complaints in the harvesting of the knee; however, there is a potential risk of iatrogenic saphenous nerve injury and theoretical knee flexion weakness. The use of allograft tendons can be another option required by further research to confirm its benefit and risk for this operative technique.
This study has several limitations. These include the retrospective design, small number of patients, medium-term follow-up, lack of control cases, lack of the objective evaluation of the plantar flexion strength, and no direct comparison with other operative methods such as traditional autologous tendon grafting without a strong core suture. Also, this study did not evaluate the elongation of the repaired tendon, despite the relatively aggressive postoperative protocol. The outcomes of the ATRS scores show no patients reach 10 points of 10 in the running, jumping, and physical labor, which includes the possibility of the elongation of the repaired tendon. However, we believe that single-arm research is also of sufficient significance and those limitations suggest the concern of further research. As shown in past studies, it is practically difficult to obtain the number of cases of foot and ankle diseases collectively, so many studies of foot and ankle diseases are single-arm studies and these research results are improving our clinical practice and research activities. 2,3,25,28,34 The other limitation was this study did not describe the time frame to return to sport because all subjects included in this study were nonathletes. Although patients with chronic Achilles tendon rupture are relatively rare, a multicenter matched-pair study could be an option to address these limitations.
Despite these limitations, our findings suggest that the SLLS technique accompanied by autologous semitendinosus tendon grafting may be effective in the operative treatment of chronic Achilles tendon rupture regardless of the defect size and may facilitate early postoperative rehabilitation without long-term splinting or use of a special orthosis.
Further studies with longer follow-up are necessary to validate our findings before the technique described here could be considered an effective operative treatment in practice.
Conclusion
The SLLS technique accompanied by autologous semitendinosus tendon grafting provided successful operative outcomes for patients with chronic Achilles tendon rupture regardless of the size of the defect, and thus long-term immobilization or use of an orthosis was not needed after surgery. Further studies with longer follow-up are necessary to validate our findings before the technique described here could be considered an effective operative treatment in practice.
Supplemental Material
Supplemental Material, sj-pdf-1-fao-10.1177_24730114211003541 for Operative Outcome of Side-Locking Loop Suture Technique Accompanied by Autologous Semitendinosus Tendon Grafting for Chronic Rupture of Achilles Tendon by Keisuke Tsukada, Youichi Yasui, Maya Kubo, Shinya Miki, Kentaro Matsui, Jun Sasahara, Hirotaka Kawano and Wataru Miyamoto in Foot & Ankle Orthopaedics
Footnotes
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional review board of the authors' institution and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Kentaro Matsui, MD,  https://orcid.org/0000-0003-4342-3575
https://orcid.org/0000-0003-4342-3575
References
- 1. Abubeih H, Khaled M, Saleh WR, Said GZ. Flexor hallucis longus transfer clinical outcome through a single incision for chronic Achilles tendon rupture. Int Orthop. 2018;42(11):2699–2704. [DOI] [PubMed] [Google Scholar]
- 2. Apinun J, Jenvorapoj S, Arirachakaran A, Kongtharvonskul J. Clinical outcomes of chronic Achilles tendon rupture treated with flexor hallucis longus grafting and flexor hallucis longus grafting plus additional augmentation: a meta-analysis. Foot Ankle Surg. 2020;26(7):717–722. [DOI] [PubMed] [Google Scholar]
- 3. Barske HL, Baumhauer J. Quality of research and level of evidence in foot and ankle publications. Foot Ankle Int. 2012;33(1):1–6. [DOI] [PubMed] [Google Scholar]
- 4. Den Hartog BD. Surgical strategies: delayed diagnosis or neglected Achilles’ tendon ruptures. Foot Ankle Int. 2008;29(4):456–463. [DOI] [PubMed] [Google Scholar]
- 5. Dombrowski M, Murawski CD, Yasui Y, et al. Medical comorbidities increase the rate of surgical site infection in primary Achilles tendon repair. Knee Surg Sports Traumatol Arthrosc. 2019;27(9):2840–2851. [DOI] [PubMed] [Google Scholar]
- 6. Dumbre Patil SS, Dumbre Patil VS, Basa VR, Dombale AB. Semitendinosus tendon autograft for reconstruction of large defects in chronic Achilles tendon ruptures. Foot Ankle Int. 2014;35(7):699–705. [DOI] [PubMed] [Google Scholar]
- 7. El Shewy MT, El Barbary HM, Abdel-Ghani H. Repair of chronic rupture of the Achilles tendon using 2 intratendinous flaps from the proximal gastrocnemius-soleus complex. Am J Sports Med. 2009;37(8):1570–1577. [DOI] [PubMed] [Google Scholar]
- 8. Gregor RJ, Komi PV, Järvinen M. Achilles tendon forces during cycling. Int J Sports Med. 1987;8(suppl 1):9–14. [DOI] [PubMed] [Google Scholar]
- 9. Gross CE, Nunley JA. Treatment of neglected Achilles tendon ruptures with interpositional allograft. Foot Ankle Clin. 2017;22(4):735–743. [DOI] [PubMed] [Google Scholar]
- 10. Guclu B, Basat HC, Yildirim T, Bozduman O, Us AK. Long-term results of chronic Achilles tendon ruptures repaired with V-Y tendon plasty and fascia turndown. Foot Ankle Int. 2016;37(7):737–742. [DOI] [PubMed] [Google Scholar]
- 11. Imade S, Mori R, Uchio Y. Modification of side-locking loop suture technique using an antislip knot for repair of Achilles tendon rupture. J Foot Ankle Surg. 2013;52(4):553–555. [DOI] [PubMed] [Google Scholar]
- 12. Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15(7):349–353. [DOI] [PubMed] [Google Scholar]
- 13. Kraeutler MJ, Purcell JM, Hunt KJ. Chronic Achilles tendon ruptures. Foot Ankle Int. 2017;38(8):921–929. [DOI] [PubMed] [Google Scholar]
- 14. Lever CJ, Bosman HA, Robinson AHN. The functional and dynamometer-tested results of transtendinous flexor hallucis longus transfer for neglected ruptures of the Achilles tendon at six years’ follow-up. Bone Joint J. 2018;100-B(5):584–589. [DOI] [PubMed] [Google Scholar]
- 15. Maffulli N, Ajis A. Management of chronic ruptures of the Achilles tendon. J Bone Joint Surg Am. 2008;90(6):1348–1360. [DOI] [PubMed] [Google Scholar]
- 16. Maffulli N, Del Buono A, Spiezia F, et al. Less-invasive semitendinosus tendon graft augmentation for the reconstruction of chronic tears of the Achilles tendon. Am J Sports Med. 2013;41(4):865–871. [DOI] [PubMed] [Google Scholar]
- 17. Maffulli N, Loppini M, Longo UG, Maffulli GD, Denaro V. Minimally invasive reconstruction of chronic Achilles tendon ruptures using the ipsilateral free semitendinosus tendon graft and interference screw fixation. Am J Sports Med. 2013;41(5):1100–1107. [DOI] [PubMed] [Google Scholar]
- 18. Maffulli N, Spiezia F, Testa V, et al. Free gracilis tendon graft for reconstruction of chronic tears of the Achilles tendon. J Bone Joint Surg Am. 2012;94(10):906–910. [DOI] [PubMed] [Google Scholar]
- 19. Maffulli N, Via AG, Oliva F. Chronic Achilles tendon rupture. Open Orthop J. 2017;11:660–669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Miyamoto W, Imade S, Innami K, Kawano H, Takao M. Acute Achilles tendon rupture treated by double side-locking loop suture technique with early rehabilitation. Foot Ankle Int. 2017;38(2):167–173. [DOI] [PubMed] [Google Scholar]
- 21. Myerson MS. Achilles tendon ruptures. Instr Course Lect. 1999;48:219–230. [PubMed] [Google Scholar]
- 22. Nilsson-Helander K, Thomeé R, Silbernagel KG, et al. The Achilles tendon total rupture score (ATRS): development and validation. Am J Sports Med. 2007;35(3):421–426. [DOI] [PubMed] [Google Scholar]
- 23. Nishimura K, Mori R, Miyamoto W, Uchio Y. A new technique for small and secure knots using slippery polyethylene sutures. Clin Biomech (Bristol, Avon). 2009;24(4):403–406. [DOI] [PubMed] [Google Scholar]
- 24. Padanilam TG. Chronic Achilles tendon ruptures. Foot Ankle Clin. 2009;14(4):711–728. [DOI] [PubMed] [Google Scholar]
- 25. Papalia R, Franceschi F, D’Adamio S, et al. Hamstring tendon regeneration after harvest for anterior cruciate ligament reconstruction: a systematic review. Arthroscopy. 2015;31(6):1169–1183. [DOI] [PubMed] [Google Scholar]
- 26. Schweitzer KM, Jr, Dekker TJ, Adams SB. Chronic Achilles ruptures: reconstructive options. J Am Acad Orthop Surg. 2018;26(21):753–763. [DOI] [PubMed] [Google Scholar]
- 27. Shelton WR, Fagan BC. Autografts commonly used in anterior cruciate ligament reconstruction. J Am Acad Orthop Surg. 2011;19(5):259–264. [DOI] [PubMed] [Google Scholar]
- 28. Song YJ, Hua YH. Tendon allograft for treatment of chronic Achilles tendon rupture: a systematic review. Foot Ankle Surg. 2019;25(3):252–257. [DOI] [PubMed] [Google Scholar]
- 29. Suijkerbuijk MAM, Reijman M, Lodewijks SJ, Punt J, Meuffels DE. Hamstring tendon regeneration after harvesting: a systematic review. Am J Sports Med. 2015;43(10):2591–2598. [DOI] [PubMed] [Google Scholar]
- 30. Wegrzyn J, Luciani JF, Philippot R, et al. Chronic Achilles tendon rupture reconstruction using a modified flexor hallucis longus transfer. Int Orthop. 2010;34(8):1187–1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Yasuda T, Shima H, Mori K, Kizawa M, Neo M. Direct repair of chronic Achilles tendon ruptures using scar tissue located between the tendon stumps. J Bone Joint Surg Am. 2016;98(14):1168–1175. [DOI] [PubMed] [Google Scholar]
- 32. Yotsumoto T, Miyamoto W, Uchio Y. Novel approach to repair of acute Achilles tendon rupture: early recovery without postoperative fixation or orthosis. Am J Sports Med. 2010;38(2):287–292. [DOI] [PubMed] [Google Scholar]
- 33. Yotsumoto T, Mori R, Hatanaka H, Uchio Y. Optimally strong tendon repair using braided polyethylene strand: 2-strand heavy-gauge locking technique vs. multiple-strand technique. Clin Biomech (Bristol, Avon). 2010;25(8):835–839. [DOI] [PubMed] [Google Scholar]
- 34. Zaidi R, Abbassian A, Cros S, Guha A, Cullen N, Singh D, Goldberg A. Levels of evidence in foot and ankle surgery literature: progress from 2000 to 2010? J Bone Joint Surg Am. 2012;94(15):e1121–10. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-fao-10.1177_24730114211003541 for Operative Outcome of Side-Locking Loop Suture Technique Accompanied by Autologous Semitendinosus Tendon Grafting for Chronic Rupture of Achilles Tendon by Keisuke Tsukada, Youichi Yasui, Maya Kubo, Shinya Miki, Kentaro Matsui, Jun Sasahara, Hirotaka Kawano and Wataru Miyamoto in Foot & Ankle Orthopaedics