Abstract
Ocular cysticercosis is caused by the larval form of pork tapeworm for which humans and pigs are the intermediate hosts. Intense inflammation secondary to immunological reaction is the hallmark feature of the infection, which can affect almost any tissue of the host. Orbital imaging yields specific features suggestive of the diagnosis. Although medical management is the recommended treatment for extra-ocular and retro-orbital cysticercosis, surgical removal has also been suggested by several authors. Here, we report two cases of subconjunctival cysticercosis, successfully managed with medical treatment alone using oral steroid and albendazole. Surgical excision for subconjunctival cysticercosis is associated with complications which can be observed even with the most experienced hands. Through these two cases, we wish to sensitize the practicing physicians regarding the most common ocular infestation seen in the developing countries along with brief literature review on the management protocols to be followed before any surgical reference.
Keywords: Albendazole, extra-ocular cysticercosis, retro-orbital cysticercosis, subconjunctival cysticercosis
Introduction
Infestation by the larval form of pork tapeworm, Taenia solium, causes cysticercosis, with increased predilection for skeletal muscles, heart muscle, central nervous system, and eye.[1] Ocular cysticercosis is one of the most frequent parasitic infections leading to blindness in developing countries with poor sanitation. The commonest site for lodgement is extra-ocular muscles, adnexa followed by subconjunctival space. Retro-orbital space is least commonly affected.[2] Inoculation leads to severe immune-mediated inflammatory reaction causing oedema and compression of the surrounding structures. Most common presenting symptoms are motility restriction and diplopia, followed by redness of the eye and lid swelling, while reduced vision is the least commonly observed symptom.[3] Diagnosis is based on history, clinical examination, and specific radiological findings on ultrasound and computed tomography (CT). Imaging modality of choice is B scan ultrasonography (USG) which depicts presence of hyperechoic scolex.[4] Management remains a challenge for health-care providers due to absence of definitive guidelines. Although medical management is the preferred modality, some authors have reported increased incidence of inflammatory reaction following oral albendazole therapy. Early surgical management has led to anatomical success rate of 75%, while functional success rate of 50% in good surgical hands.[5]
We report two cases of large subconjunctival cysticercosis, which resolved completely on oral and topical steroids followed by albendazole without any inflammatory reaction. An informed written consent was taken from the parents which were followed by approval from institution ethical committee for reporting of the cases.
Case 1
An 8-year-old girl presented to clinic with a firm and mobile cystic swelling in the right eye measuring 15 × 12 mm, located in the temporal quadrant. It was asymptomatic, insidious in onset and constant in size for the past 6 months. Examination revealed visual acuity of 6/6 in both the eyes. Left eye was grossly normal. B-scan ocular USG of the right eye demonstrated presence of a scolex without any muscular involvement. Rest of the ocular examination was normal. MRI brain revealed associated calcified neurocysticercosis (NCC) in the left parietal lobe. Enzyme-linked immunosorbent assay (ELISA) for anti-cysticercal antibodies was found to be negative.
Case 2
A 13-year-old girl presented to clinic with diplopia and large, mobile cystic swelling measuring 18 × 15 mm in the nasal quadrant of right eye for the past 10 months. Visual acuity was normal for both eyes. Ocular evaluation revealed right eye exotropia with restriction of adduction while left eye was grossly normal. ELISA was positive and CT of brain was suggestive of presence of a calcified cyst in the right frontal lobe suggesting associated NCC. CT of the orbit revealed presence of scolex. There was no evidence of intra-ocular cyst.
Management
Both patients were started with topical steroids along with oral steroids at 1 mg/kg/day followed by oral albendazole at 15 mg/kg/day. Systemic steroids were tapered and stopped gradually over 4 weeks, while albendazole was continued for 6 weeks along with the topical steroids.
Outcome
In the first patient, the cyst started to decrease in size and resolved completely over 8 weeks from the presentation [Figure 1]. In the second patient, there was no significant change in the size of the cyst after 4 weeks of albendazole. At around sixth week, there was spontaneous extrusion of the cyst [Figure 2]. Topical steroids and anti-inflammatory drops were continued for another 4 weeks and were gradually stopped. No ocular inflammation was observed during the treatment in either of the patients.
Figure 1.
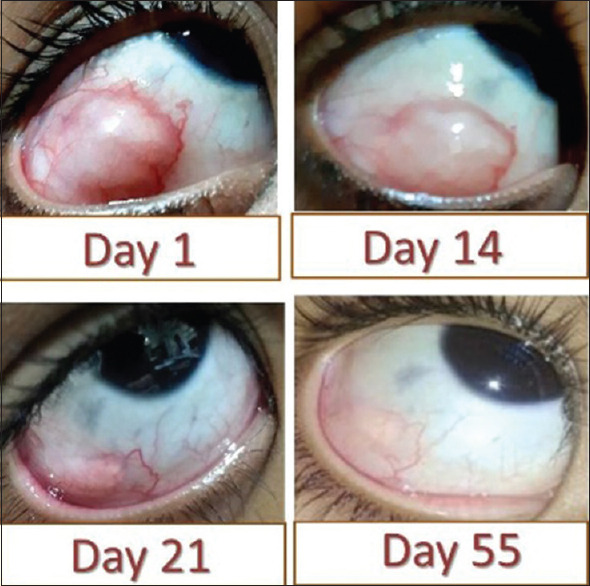
Depicts large ocular cysticercosis involving the infratemporal region of the right eye, of an 8-year-old girl. At day 1 of presentation, the cyst was tense with surrounding hyperemia, which subsequently involuted with medical management alone, complete disappearance was seen by the day 55 of presentation
Figure 2.
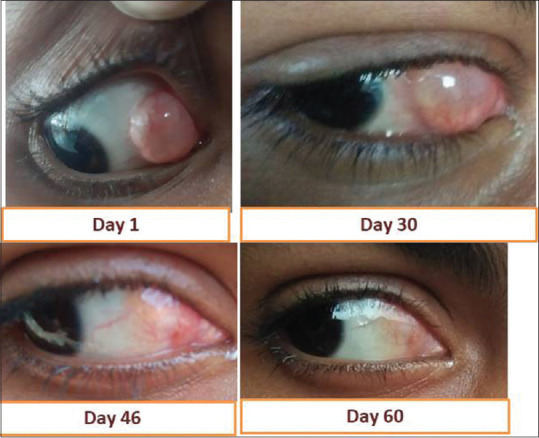
Depicts large ocular cysticercosis involving the nasal quadrant of the right eye of a 13-year-old girl. There was increase in inflammation with lid oedema at day 30 of medical therapy. Subsequently, the cyst got spontaneously extruded by day 45 of medical management. On follow-up, at day 60, there was no evidence of the cyst
On follow-up, both the patients have no residual deficit in the eye and have shown complete resolution of the cystic lesion without any complications.
Discussion
Cysticercosis frequently affects people with poor sanitation and hygienic practices with a higher prevalence in developing countries. Nervous system involvement as NCC is the most common manifestation of the parasite, while ocular is the least common one (13–46%).[6]
Cysticerci can involve any part of the eye or its adnexal structures. From a meta-analysis of 500 published cases on ocular cysticercosis, it was observed that retina and subretinal space were most frequently affected (41%) followed by the vitreous cavity (27%). Subconjunctival space (21%), anterior segment (8%), lids, and orbit were least commonly affected (4%).[7,8] In India, extra-ocular cysts are frequently reported, as compared to the western world where intraocular cysticercosis is most prevalent.[9]
Medical management with albendazole and oral steroids has been reported as the standard of care for extra-ocular cysticercosis. Albendazole, an antihelmithic drug, acts by interfering with the Adenosine Triphosphate (ATP) production within the parasite by inhibiting its glucose uptake.[8,9,10,11] Complete clinical improvement has been defined as the resolution of all ocular signs with involution of cyst on radiological scans or spontaneous extrusion of the cyst from the eye.[10]
Surgical management in the form of excisional biopsy has also been reported in the literature for the management of subconjunctival cysts.[2,12] However, they have been associated with serious surgical challenges due to a high incidence of intraoperative rupture, large size, deeper situation in the orbit, or attachment to the important orbital structures. Surgical excision can also be associated with postoperative fibrotic response leading to restrictive ocular motility disorders, strabismus, and diplopia.[2] Although medical management is the primary modality of choice, surgery is being done more frequently for the management of ocular cysts due to fear of inciting inflammatory reaction, secondary to the systemic drugs used.[1,2,12,13]
In both our patients, we found that albendazole along with topical and systemic steroids have led to complete resolution of the subconjunctival cyst without any untoward effects. Hence, these cases not only add to the existing literature but also highlight the fact that not all subconjunctival cysticercosis needs a surgical intervention. In a developing economy where cost of surgery with its added complications can be an additional burden on the society, it is imperative to sensitize the practicing physicians regarding the management of the most common ocular infestation.
Conclusion
In ocular cysticercosis with extra-ocular involvement, a complete trial of medical management should be given before any active surgical intervention is undertaken.
Key points
Orbital cysticercosis is the most common cause of blindness in developing countries with poor sanitary conditions.
History, clinical examination, and radiological evaluation aid in the diagnosis.
Medical management is the preferred treatment for orbital cysticercosis and should be started after diagnosis is made before considering more invasive surgical approaches for the management.
Medical management is not indicated in intra-ocular cysticercosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Das S. Anterior orbital cysticercosis: A case presentation. Kerala J Ophthalmol. 2017;29:230–3. [Google Scholar]
- 2.Dhiman R, Devi S, Duraipandi K, Chandra P, Vanathi M, Tandon R, et al. Cysticercosis of the eye. Int J Ophthalmol. 2017;10:1319–24. doi: 10.18240/ijo.2017.08.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Salim S, Alam MS, Backiavathy V, Raichura ND, Mukherjee B. Orbital cysticercosis: Clinical features and management outcomes. Orbit. doi: 10.1080/01676830.2020.1833942. doi: 10.1080/01676830.2020.1833942. [DOI] [PubMed] [Google Scholar]
- 4.Hamal D, Kafle S, Kafle P, Poudyal P, Lamichhane B, Limbu B. Orbital myocysticercosis different presentation and management in Eastern Nepal. Nepalese J Ophthalmol. 2020;12:125–32. doi: 10.3126/nepjoph.v12i1.24771. [DOI] [PubMed] [Google Scholar]
- 5.García Franco R, Arias Gómez A, Guzman Cerda J, García Roa M, Ramirez Neria P. Submacular cysticercosis successfully treated through conservative management: Case report. Case Rep Ophthalmol. 2020;11:315–21. doi: 10.1159/000508030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Atul K, Kumar TH, Mallika G, Sandip M. Socio-demographic trends in ocular cysticercosis. Acta Ophthalmol Scand. 1995;73:438–41. doi: 10.1111/j.1600-0420.1995.tb00304.x. [DOI] [PubMed] [Google Scholar]
- 7.Singh RY. Subconjunctival cysticercus cellulosae. Indian J Ophthalmol. 1993;41:188–9. [PubMed] [Google Scholar]
- 8.Ziaei M, Elgohary M, Bremner FD. Orbital cysticercosis, case report and review. Orbit. 2011;30:230–5. doi: 10.3109/01676830.2011.587938. [DOI] [PubMed] [Google Scholar]
- 9.Grover AK, Puri P. Orbital myocysticercosis presenting as subconjunctival abscess. Ind J Ophthalmol. 1996;44:229–31. [PubMed] [Google Scholar]
- 10.Rath S, Honavar SG, Naik M, Anand R, Agarwal B, Krishnaiah S, et al. Orbital cysticercosis: Clinical manifestations, diagnosis, management, and outcome. Ophthalmology. 2010;117:600–5.e1. doi: 10.1016/j.ophtha.2009.07.030. [DOI] [PubMed] [Google Scholar]
- 11.Bodh SA, Kamal S, Kumar S, Goel R, Nagpal S, Aditya K. Orbital cysticercosis. DJO. 2012;23:99–103. [Google Scholar]
- 12.Sujata S. Giriyan, Niraj Kumar Nirala. “Subconjunctival Cysticercosis: Case Report and Review of Literature”. International Journal of Science and Research (IJSR) 2016;5:1939–42. [Google Scholar]
- 13.Auzemery A, Andriantsimahavandy A, Esterre P, Bouat C, Boitte JP, Huguet P. La cysticercose oculaire [Ocular cysticercosis] Med Trop (Mars) 1995;55:429–33. [PubMed] [Google Scholar]


