Abstract
Purpose:
The relationship of magnetic resonance imaging (MRI) measures of rotator cuff intramuscular fatty infiltration (FI) to shoulder range of motion (ROM) and strength are not well understood. Our purpose was to determine if supraspinatus quantitative Dixon fat fraction has superior correlation to shoulder ROM and strength as compared to semiquantitative Goutallier grade.
Methods:
Thirty-seven study subjects received shoulder MRI; and measurement of ipsilateral shoulder forward flexion ROM, abduction ROM and abduction strength. Supraspinatus Dixon fat fraction was measured on 6-point Dixon MRI by 2 diagnostic radiology residents. Supraspinatus Goutallier grade was assessed on T1-weighted MRI by 2 musculoskeletal radiologists. Questionnaires recorded demographics. Based on characteristics, study subjects were divided into 3 groups: Group 1, neither shoulder pain nor full-thickness supraspinatus tendon (SST) tear (n = 17; mean age, 63.0 ± 10.1 years); Group 2, positive complaint of shoulder pain but without full-thickness SST tear (n = 7; mean age, 57.4 ± 9.9 years); Group 3, positive complaint of shoulder pain and full-thickness SST tear (n = 13; mean age, 63.6 ± 8.1 years). One-way analysis of variance compared groups. Spearman (rho) rank order correlation was performed to determine correlation of supraspinatus Dixon fat fraction, or Goutallier grade, with measures of ROM and strength for the study population. Reliability analyses were performed for Dixon fat fraction and Goutallier grade.
Results:
No significant differences were present among groups for age. Significant differences existed among groups for forward flexion ROM (P = 0.001), abduction ROM (P < 0.001), Dixon fat fraction (P = 0.004) and Goutallier grade (P = 0.012). Dixon fat fraction showed statistically significant inverse correlations with forward flexion ROM (rho = 0.47; P = 0.005), abduction ROM (rho = 0.35, P = 0.041), and abduction strength (rho = 0.42; P = 0.013). Goutallier grade demonstrated weak inverse correlation that lacked statistical significance (P > 0.05) for the same measures. Dixon fat fraction showed strong interobserver and intraobserver reliability with intraclass correlation coefficients of 0.956 and 0.999, respectively. Goutallier grade showed poor interobserver (kappa, 0.188) and moderate intraobserver (kappa, 0.608) reliability.
Conclusion:
Supraspinatus Dixon fat fraction has superior correlation to shoulder ROM and strength relative to Goutallier grade on MRI.
Introduction
One out of every 4 adults over the age of 60 years suffers from rotator cuff (RC) tear in the general population, with supraspinatus tendon (SST) tear the most prevalent.1,2 Nearly 300,000 RC tears receive rotator cuff repair (RCR) surgery at a cost of up to $12 billion dollars annually in the United States.3 Eighty-six percent of RCR surgery is performed for adults 45 years and older, but adults between the ages of 65–74 years demonstrate the highest estimated utilization rates at 28.3 per 10,000 persons.4 Costs related to RC tear are likely to rise further over time given the expected growth of the geriatric population in the coming years.
Evaluation of shoulder strength and range of motion (ROM) are primary factors for orthopedic surgeons to consider when evaluating patients with suspected RC tear. Shoulder weakness, decreased ROM, and pain are common among patients with symptomatic RC tear, but not all individuals with these symptoms and signs have RC tear.5 Impaired shoulder function and pain are the indications for surgical intervention for RC tears.6 For individuals who are ultimately offered an operative intervention for RC tear, the goals of RCR surgery include improving shoulder strength and ROM, as well as decreasing shoulder pain.5,7,8 Operative treatment for RC tears has been shown to be superior to nonoperative treatment, but there is variability in pain relief and restoration of shoulder function.6
Quantification of rotator cuff muscle quality in patients with RC tear is another key parameter for clinical decision-making. Magnetic resonance imaging (MRI) is the leading modality for evaluation of RC intramuscular fatty infiltration (FI) and RC tear in the United States. MRI aids clinical decision-making by accurately determining if a RC tear is present in patients who present clinically with shoulder pain, weakness and/or decreased ROM, and also by classifying the pattern and size of the RC tear when present. For muscle quality, animal and human studies support the concept that degree of FI on preoperative imaging studies is predictive of postsurgical outcomes following RCR surgery.7–12 Animal studies also suggest that the amount of FI is inversely related to RC muscle strength.13 Studies suggest that the presence of full-thickness RC tear is the key factor that leads to a significant increase in FI over time, as compared to shoulders with only partial-thickness RC tear or no tendon tear.14–16
The most commonly used imaging measure of FI in clinical practice and research has been the semiquantitative Goutallier classification system, due to its ease of use.7,12,17,18 The main limitation of Goutallier grade as a measure of FI is poor to moderate reliability.15,16,19–21 Quantitative measures of FI, such as multiecho Dixon and iterative decomposition of water and fat with echo asymmetry and least-squares estimation (IDEAL), have been, in recent literature, suggested to be a reliable alternative to the Goutallier Classification system.15,16,22–25 The 6-point Dixon MRI method improves accuracy in the estimation of FI as compared to older 2-point Dixon sequences, by relatively decreasing T1 effects and T2* decay and more effectively separating fat and water signal.22,26
MRI measures of FI have been suggested to have an association with the subjective self-reported American Shoulder and Elbow Surgeon score in older adults.16 However, the relationship of quantitative and semiquantitative measures of supraspinatus FI to objective measures of ROM and strength is not well understood. The purpose of our pilot study was to determine if supraspinatus fat fraction by quantitative 6-point Dixon MRI has superior correlation with shoulder ROM and strength as compared to semiquantitative Goutallier grade by T1-weighted MRI. We hypothesized that supraspinatus quantitative Dixon fat fraction would have superior correlation to shoulder ROM and strength as compared to semiquantitative Goutallier grade.
Methods
Study Population
The study was approved by the authors’ institutional review board and complied with the Health Insurance Portability and Accountability Act. Informed written consent was obtained from each study subject. A total of 41 shoulders in 38 study subjects were enrolled following self-referral in response to local advertisement or by referral from one of 3 orthopedic surgeons, during a 1-year recruitment period in 2017. Following enrollment, all study subjects received shoulder MRI with the same imaging protocol at the institution’s MRI research facility. The study design did not include evaluation of any preexisting clinical shoulder MRI which may have existed prior to enrollment. The inclusion criterion was an age between 40 years and 85 years. The study subjects were divided into 3 groups, following completion of their research shoulder MRI scan: Group 1 – neither shoulder pain nor full-thickness SST tear; Group 2 – positive complaint of shoulder pain but without full-thickness SST tear; Group 3 – positive complaint of shoulder pain and full-thickness SST tear of any size (Fig 1). The exclusion criteria were (1) contraindication to MRI, (2) chronic upper extremity paralysis, (3) history of prior RCR surgery or joint replacement for the ipsilateral shoulder; or (4) not fitting a definition to be included into Group 1, Group 2 or Group 3.
FIG 1.

Example shoulder MR images of study subjects included in each group. (A) Oblique coronal short tau inversion recovery (STIR) MR image of a 66-year-old man with no supraspinatus (SST) tear, representative of study subjects in Groups 1 and 2. (B) Oblique coronal STIR MR image of a 43-year-old man showing an partial-thickness articular-sided SST tear (white arrow), also representative of study subjects in Groups 1 and 2. (C) Oblique coronal STIR MR image of a 66-year-old man showing a full-thickness SST tear (orange bracket), representative of study subjects in Group 3. (Color version of figure is available online.)
Study subjects who reported a score of ≥2 on an 11-point visual analog scale (VAS), were defined as having shoulder pain; study subjects who reported ≤1 on VAS were defined as not having shoulder pain.5,16 Study subjects included in Groups 1 and 2 included SST which were intact, with tendinopathy or partial tear.Prior studies suggest that levels of FI are similar for shoulders with partial-thickness RC tear when compared to shoulders with no tear.14–16 Three study subjects had bilateral shoulder MRI performed; only one shoulder MRI from each of these study subjects was included in the analysis to ensure that each study subject represented an independent sample. One study subject was excluded for failing to meet the definition to be included into Group 1, Group 2, or Group 3, having a full-thickness SST without shoulder pain. Following exclusions, a total of 37 study subjects were included in the analysis.
MRI
All shoulder MRI examinations were performed at 3.0T (Magnetom Trio or Magnetom Prismafit; Siemens Healthcare, Erlangen, Germany) using a 4-channel flexible coil, with study subjects in a standard supine position. The imaging protocol included a 2-dimensional (2D) turbo spin-echo oblique sagittal T1-weighted sequence (matrix, 448 × 202; repetition time ms (TR)/echo time[s] (TE) ms, 600/24; field of view (FOV), 160 × 160 mm2; number of averages, 1; slice thickness, 4mm); and axial, oblique sagittal and oblique coronal 2D short tau inversion recovery (matrix, 256 × 202; TR/TE ms, 4420/50; inversion time 180 ms; FOV, 160 × 160 mm2, number of acquisitions, 1; slice thickness, 4mm). A 3-dimensional 6-point Dixon volumetric sequence was also obtained in the sagittal orientation (matrix, 320 × 250; TR, 9 ms, TE,1.35, 2.65, 3.95, 5.25, 6.55, 7.85 ms; flip angle, 9; FOV 400 × 324 mm2; number of averages, 1; slice thickness, 3.5 mm), with an imaging time of less than one minute. Oblique sagittal Dixon fat fraction maps were reconstructed from the 6-point Dixon sequence in an automated fashion.
Clinical Evaluation
An independent evaluation was performed for each shoulder ipsilateral to the MRI, on the same date as the shoulder MRI examination. Study subjects completed questionnaires including demographic information, Charlson Comorbidity Index (CCI), past surgical history, and VAS pain score (minimum, 0; maximum, 10) for the ipsilateral shoulder. The CCI is an analytic tool designed to quantify the burden of chronic medical conditions for an individual, allowing for the degree of comorbidity among study subjects to be compared in research studies. Lower scores indicate that fewer chronic medical conditions are present, while higher scores represent a greater burden of comorbidity.27
A single examiner, blind to MRI findings, performed a brief physical examination of the shoulder for all study subjects at our MRI research center on the same day that shoulder MRI was performed. The examiner was a clinical research specialist at our institution, with credentials of Bachelor of Medicine-Bachelor of Surgery. All study subjects were evaluated in a seated position with the examiner standing adjacent to the shoulder ipsilateral to the MRI examination. Active abduction strength of the shoulder was measured with a portable hand-held dynamometer placed by the examiner at the study subject’s proximal forearm (90° abduction in scapular plane with hand in a fist and thumb pointing to the floor). Study subjects were instructed to push the dynamometer during active abduction as hard as they could while being resisted by the examiner. Three separate trials of abduction strength were recorded. The maximum recorded abduction strength of the 3 trials was used for analysis. Maximum active forward flexion ROM and active abduction ROM were measured by the examiner using a portable hand-held goniometer. One trial was conducted each for active forward flexion and active abduction ROM. For forward flexion ROM starting with their hand resting adjacent to their thigh, study subjects were asked to lift their upper limb straight out and up in front of them as high as the could reach. For abduction ROM starting with their hand resting adjacent to their thigh, study subjects were asked to abduct their upper limb from their side as high as the could reach.
MR Image Analysis
DICOM image modules containing a deidentified single oblique sagittal T1 MR image corresponding to the Y-view, the lateral-most slice where the scapular body contacts the spine, for each shoulder MRI were created on a 3D visualization system viewer (Aquarius iNtuition Edition, version 4.4; TeraRecon Inc., Foster City, CA).16,23,28–30 A blinded musculoskeletal radiologist with >25 year experience independently assigned a Goutallier grade for each supraspinatus muscle, based on the 5-point Goutallier classification scale: grade 0, no fat; grade 1, streaks of fat; grade 2, muscle > fat; grade 3, muscle = fat; grade 4, muscle < fat (Fig 2A and C).16–18 At no less than 4 weeks later, the same blinded musculoskeletal radiologist independently assigned a Goutallier grade for each supraspinatus to determine intraobserver reliability. A second blinded musculoskeletal radiologist with >25 years of experience independently assigned a Goutallier grade for each supraspinatus muscle in order to determine interobserver reliability. For each study subject, the mean Goutallier grade between the first reads of the blinded musculoskeletal radiologists was used for analysis. Both musculoskeletal radiologists independently reviewed identical Goutallier grade classification training modules prior to beginning evaluation of study subject MR images.
FIG 2.
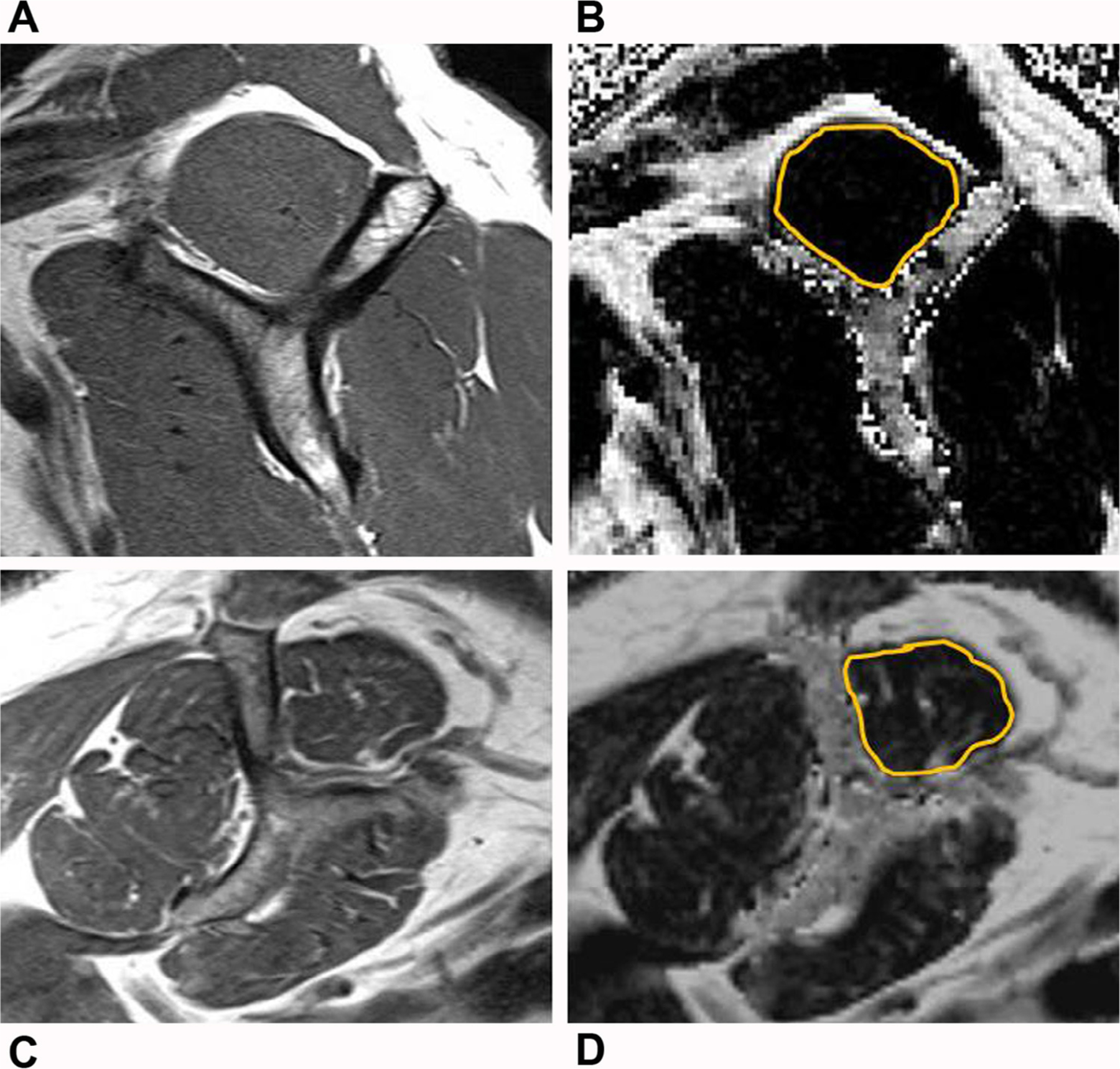
Example shoulder MR images showing methods of supraspinatus muscle analysis. (A) Oblique sagittal T1-weighted MR Y-shaped view image of a 58-year-old male study subject used to determine Goutallier grade. (B) Oblique sagittal Dixon fat fraction map image, corresponding to the T1-weighted MR Y view. The gold outline denotes the manually delineated region of interest placed about the supraspinatus muscle for Dixon fat fraction analysis. (C and D) Oblique sagittal T1-weighted MR Y-shaped view and corresponding oblique sagittal Dixon fat fraction map images for supraspinatus muscle analysis in a 66-year-old female study subject.
DICOM image modules containing a deidentified single oblique sagittal 6-point Dixon MR fat fraction map image corresponding to the T1 MR Y-shaped view image was used to determine Dixon fat fraction. A blinded radiology resident independently calculated the Dixon fat fraction for each supraspinatus muscle on 6-point Dixon MR fat fraction maps by manual delineation using Medical Image Processing, Analysis and Visualization software (MIPAV, version 7, National Institutes of Health, Bethesda, MD) (Fig 2B and D).16,23 The region of interest was drawn at the outer margin of the supraspinatus muscle, without inclusion of adjacent bone or perimuscular fat. At no less than 4 weeks later, the same blinded radiology resident independently calculated the Dixon fat fraction again for each supraspinatus muscle to determine intraobserver reliability. A second blinded radiology resident independently calculated the Dixon fat fraction for each supraspinatus muscle on 6-point Dixon MR fat fraction maps by manual delineation using theMIPAV software, in order to determine interobserver reliability. For each study subject, the mean Dixon fat fraction value between the first reads of the blinded radiology residents was used for analysis.
A third musculoskeletal radiologist with >8 years of experience independently reviewed each shoulder MRI to determine the presence of tendinopathy, partial-thickness tear, and/or full-thickness tear of the supraspinatus, infraspinatus, subscapularis, and teres minor tendons. The mediolateral and anteroposterior dimensions of full-thickness RC tears were recorded.16
Statistical Analysis
Statistical analysis was performed using Stata statistical software version 14 (StataCorp LP, College Station, TX). Baseline characteristics for the groups were compared with the one-way ANOVA or chi-sqaure test. Pairwise comparisons were conducted for one-way analysis of variance when appropriate. Determination of heterogeneity of effects was performed for the entire study sample to test supraspinatus Dixon fat fraction or Goutallier grade for statistical interaction with sex for the outcomes of forward flexion ROM, abduction ROM, or abduction strength. Spearman (rho) rank order correlation with 95% Confidence Interval (CI) was performed for supraspinatus Dixon fat fraction, Goutallier grade, or pain score with forward flexion ROM, abduction ROM, and abduction strength. Intraobserver and interobserver reliability for supraspinatus Dixon were determined by the intraclass correlation coefficient. Intraobserver and inter-observer reliability for supraspinatus Goutallier grade were determined by calculating weighted kappa statistic. A P value <0.05 was considered to indicate a significant difference.
Results
(A). Group Characteristics
Group Comparisons
There were no significant differences in age, percentage male, or comorbidity among groups (Table 1). Statistically significant differences existed among the groups for forward flexion ROM (P = 0.001), abduction ROM (P < 0.001), Dixon fat fraction (P = 0.004), and Goutallier grade (P = 0.012). For each of these variables, Group 1 displayed the highest mean ROM and lowest mean FI while Group 3 demonstrated the lowest mean ROM and highest mean FI.
TABLE 1.
Characteristics of study subjects
| Group 1 (n = 17)−Pain−Full-Thickness SST Tear | Group 2 (n = 7)+ Pain−Full-Thickness SST Tear | Group 3 (n = 13)+Pain+ Full-Thickness SST Tear | P | |
|---|---|---|---|---|
| Age, years | 63.0 ± 10.1 | 57.4 ± 9.9 | 63.6 ± 8.1 | 0.344 |
| Male, % | 52.9 | 71.4 | 46.2 | 0.553 |
| CCI | 2.4 ± 1.5 | 1.9 ± 1.7 | 2.8 ± 2.2 | 0.508 |
| Forward flexion ROM, ° | 160.9 ± 19.8 | 137.1 ± 24.3 | 120.8 ± 35.5 | 0.001 |
| Abduction ROM,° | 140.3 ± 19.6 | 120.0 ± 21.4 | 100.4 ± 31.9 | <0.001 |
| Abduction strength, lbs. | ||||
| Men | 14.3 ± 3.1 | 12.1 ± 2.3 | 10.5 ± 5.1 | 0.127 |
| Women | 9.8 ± 2.2 | 7.0 ± 3.2 | 5.3 ± 1.3 | 0.004 |
| Dixon fat fraction* | 3.2% ± 2.2% | 2.9% ± 3.3 | 7.9% ± 5.3% | 0.004 |
| Goutallier Grade* | 0.7 ± 0.4 | 0.7 ± 0.4 | 1.3 ± 0.6 | 0.012 |
Values are mean ± standard deviation unless otherwise noted. CCI, Charlson Comorbidity Index; ROM, range of motion; SST, supraspinatus tendon.
supraspinatus muscle.
Range of Motion and Strength
Pairwise comparisons were statistically significant between Group 1 and Group 3 for forward flexion ROM (P = 0.001) and abduction ROM (P < 0.001). Significant differences existed for abduction strength in women among the groups (P = 0.004), with Group 1 women having the highest mean abduction strength and Group 3 women having the lowest mean abduction strength. Pairwise comparisons for women abduction strength, only demonstrated a significant difference between Group 1 and Group 3 (P = 0.003). One female study subject in the Group 3 declined to perform the forward flexion ROM and abduction strength tests. Although the study did not demonstrate a statistically significant difference in abduction strength in men among the groups, the comparison suggests a trend (P = 0.127) with men in Group 1 demonstrating the highest mean abduction strength and Group 3 the lowest mean abduction strength.
Dixon Fat Fraction and Goutallier Grade
For Dixon fat fraction, pairwise comparisons between Group 1 and Group 3 (P = 0.006) and between Group 2 and Group 3 (P = 0.022) were statistically significant, while no difference existed between Group 1 and Group 2 (P = 0.985). For Goutallier grade, pairwise comparisons between Group 1 and Group 3 (P = 0.016) was statistically significant; Group 2 compared to Group 3 (P = 0.056) suggested a trend toward significance, while no difference existed between Group 1 and Group 2 (P = 0.995).
Group 3 Characteristics
Study subjects in Group 3 had a mean maximum supraspinatus full-thickness tendon tear size of 2.1 ± 1.5 cm, stemming from the larger of the mediolateral or anteroposterior dimension of each SST tear. Six were isolated to the SST, 6 were in combination with a full-thickness tear of the infraspinatus tendon, and 1 was in combination with full-thickness infraspinatus and subscapularis tendons.
(B). Influence of Sex on Supraspinatus FI
Dixon Fat Fraction
The variable of sex was evaluated for the appropriateness of combining men and women in analyses when testing for correlation of Dixon fat fraction with shoulder ROM and strength outcomes. Evaluation of the entire study population (n = 35; 2 subjects did not have Dixon fat fraction) showed no significant heterogeneity of effect for Dixon fat-fraction* sex for the outcomes of forward flexion ROM (P = 0.237), abduction ROM (P = 0.256) and abduction strength (P = 0.596). Since there was no significant heterogeneity of effect by sex, men and women in the study population were analyzed together.
Goutallier Grade
The variable of sex was evaluated for the appropriateness of combining men and women in analyses when testing for correlation of Goutallier grade with shoulder ROM and strength outcomes. Evaluation of the entire study population (n = 37) showed no significant heteogeneity of effect for Goutallier-Grade* sex for the outcomes of forward flexion ROM (P = 0.486), abduction ROM (P = 0.243) and abduction strength (P = 0.490). Since there was no significant heterogeneity of effect by sex, men and women in the study population were analyzed together.
(C). Correlation
Dixon Fat Fraction
Dixon fat fraction for the study population showed statistically significant inverse correlations with forward flexion ROM (rho = −0.47 [95% CI: −0.70, −0.16]; P = 0.005), abduction ROM (rho = −0.35 [95% CI: −0.61, −0.02]; P = 0.041) and abduction strength (rho = −0.42 [95% CI: −0.67, −0.10]; P = 0.013; Figs. 3 and 4). Dixon fat fraction for Group 1 showed significant inverse correlation with forward flexion ROM (rho = −0.54 [95% CI: −0.81, −0.09]; P = 0.024), but inverse correlation without statistical significance for abduction ROM and abduction strength. Dixon fat fraction for Group 2 and Group 3 also showed inverse correlation without statistical significance for forward flexion ROM, abduction ROM and abduction strength.
FIG 3.
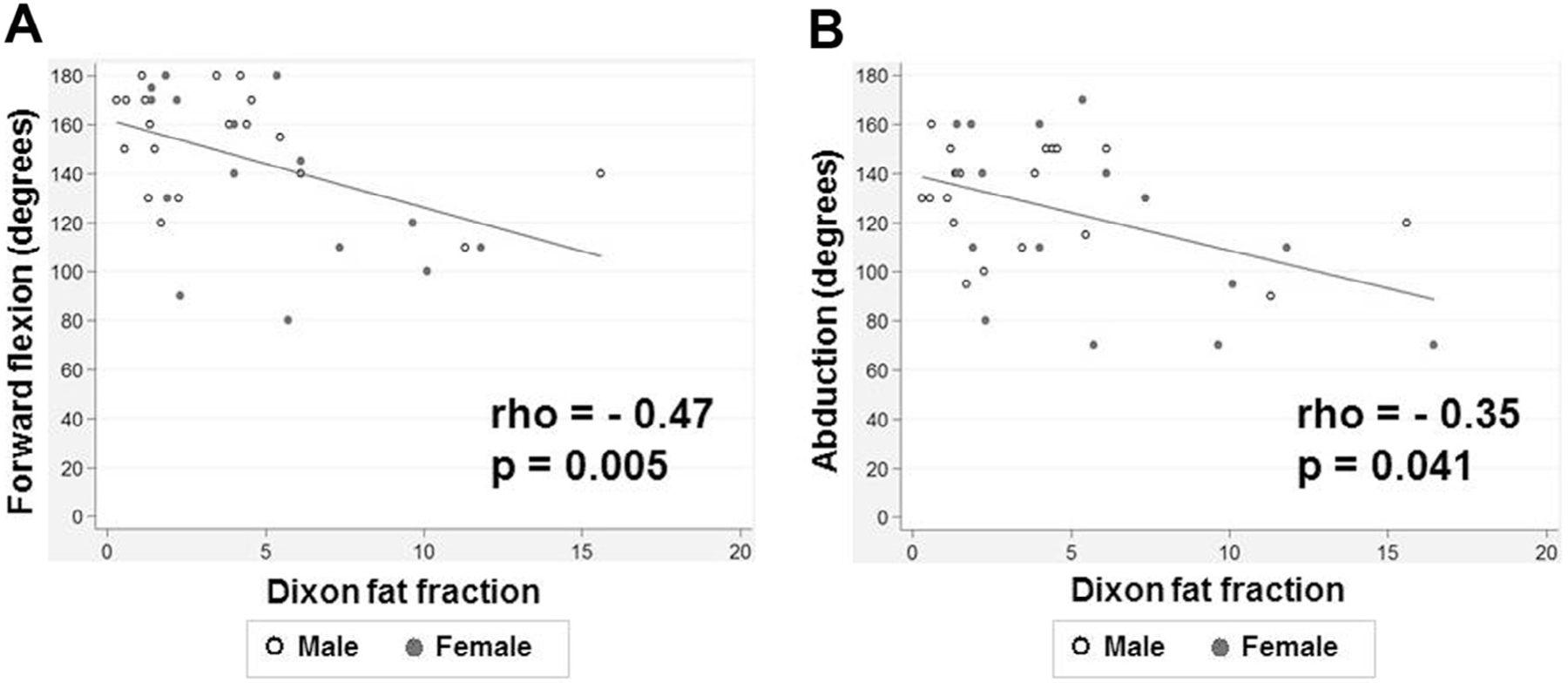
Correlation of Dixon fat fraction with shoulder range of motion (ROM). Scatter plots show a significant inverse correlation of supraspinatus Dixon fat fraction with (A) forward flexion ROM and (B) abduction ROM. Dixon fat fraction is expressed as a percentage.
FIG. 4.
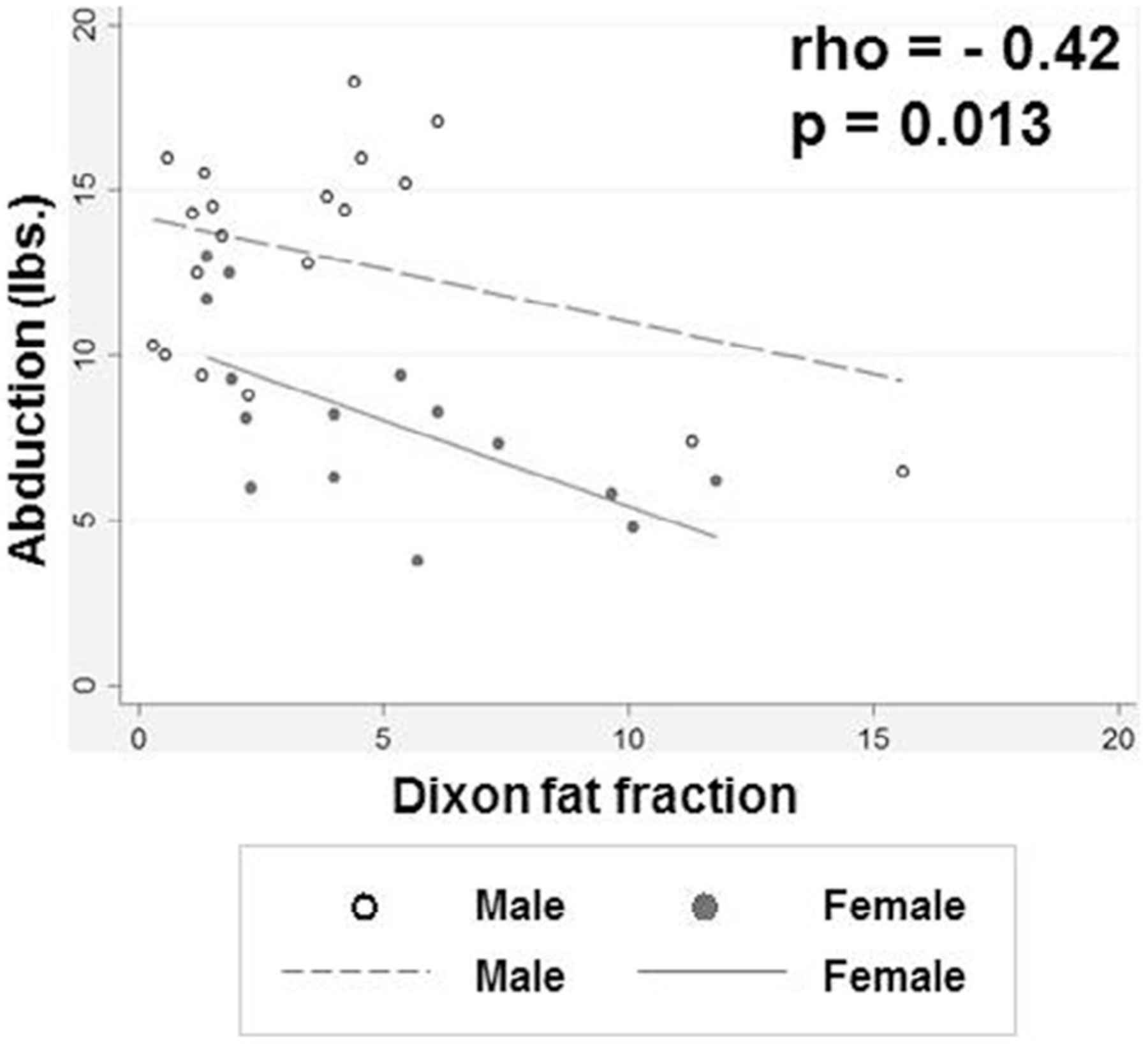
Correlation of Dixon fat fraction with shoulder strength. Scatter plot shows significant inverse correlation of supraspinatus Dixon fat fraction with abduction strength. Men and women demonstrate different baselines of abduction strength, but otherwise show a similar relationship between Dixon fat fraction and abduction strength. Dixon fat fraction is expressed as a percentage.
Goutallier Grade
Goutallier grade for the study population demonstrated weak inverse correlation that lacked statistical significance: forward flexion ROM (rho = −0.29 [95% CI: −0.56, 0.04]; P = 0.089), abduction ROM (rho = −0.23 [95% CI: −0.52, 0.10]; P = 0.170) and abduction strength (rho = −0.18 [95% CI: −0.48, 0.16]; P = 0.287). Goutallier grade in Group 1, Group 2 and Group 3 lacked statistical significance for correlation with forward flexion ROM, abduction ROM, and abduction strength.
Shoulder Pain
Shoulder pain demonstrated a moderate inverse correlation with the outcomes of forward flexion ROM (rho = −0.56 [95% CI: −0.75, −0.28]; P < 0.001) and abduction ROM (rho = −0.56 [95% CI: −0.75, −0.29]; P < 0.001). Shoulder pain demonstrated a moderate inverse correlation with abduction strength (rho = −0.46 (95% CI: −0.69, −0.16]; P = 0.005).
(D). Reliability
Interobserver and intraobserver reliability were strong to near perfect for supraspinatus Dixon fat fraction, with intraclass correlation coefficients of 0.956 and 0.999, respectively (Table 2). Interobserver reliability and intraobserver reliability for supraspinatus Goutallier grade were poor (kappa, 0.188) and moderate (kappa, 0.608), respectively.
TABLE 2.
Interobserver and intraobserver reliability for supraspinatus Dixon fat fraction and Goutallier grade for the study population
| Interobserver reliability | Intraobserver reliability | |
|---|---|---|
| Dixon fat fraction* | 0.956 | 0.999 |
| Goutallier grade† | 0.188 | 0.608 |
Intraclass correlation coefficient.
Weighted kappa statistic.
Discussion
Our pilot study found that supraspinatus quantitative Dixon fat fraction has superior correlation to shoulder ROM and strength relative to semiquantitative Goutallier grade. Dixon fat fraction demonstrates significant moderate inverse correlation to shoulder forward flexion ROM and abduction strength, and weak inverse correlation to abduction ROM; while Goutallier grade demonstrates only weak or very weak inverse correlation with the same measures without statistical significance. This study adds to the body of knowledge that quantitative MRI improves stratification of research study subjects or clinical patients based on FI, as compared to semiquantitative MRI methods.
Quantitative multiecho Dixon and IDEAL techniques allow high spatial resolution for accurate assessment of FI via MR chemical shift imaging.31 These methods facilitate quantification of FI as a continuous variable on a scale of 0–100, comparable to single voxel spectroscopy.22,25 The multiecho Dixon MRI fat fraction quantifies FI as the average proportion of fat signal within each image voxel, inside a drawn region of interest on a Dixon fat fraction map. Our finding of superior interobserver and intraobserver reliability for supraspinatus muscle Dixon fat fraction on shoulder MRI, as compared to Goutallier grade, is consistent with previous human and animal studies.16,22,28,32 Our study again highlights the subpar reproducibility of the semiquantitative Goutallier classification system.15,16,19–21,33 Investigators have attempted to improve the reproducibility of the 5-point Goutallier grading primarily by reducing the classification system to a modified 2- or 3-point ordinal scale.7,8,21,34 The use of modified Goutallier grading scales may improve reproducibility as compared to the 5-point scale, but may unintentionally limit the usefulness of the classification system. The negative trade-off when implementing modified Goutallier grading scales in research studies is the potential for the introduction of bias into the study design, by reducing stratification among study subjects and increasing the number of misclassification errors.16
Our findings are in-line with prior literature that suggests that MRI measures of supraspinatus FI correlate to abduction strength. Valencia et al, showed that the amount of FI at 6 and 12 weeks following tenotomy is a strong indicator of supraspinatus muscle contractile force in a rabbit model, with greater amounts of FI correlating to greater loss of muscular strength.13 Nardo et al, in a retrospective study of shoulders with symptoms of RC tear found moderate correlation between supraspinatus quantitative fat fraction and abduction strength.25 Gladstone et al, demonstrated a moderate inverse correlation between a preoperative supraspinatus 2-point modified Goutallier grade and forward elevation strength in a population receiving RCR surgery for symptomatic full-thickness RC tear.7
Nakamura et al, also found an inverse correlation between a baseline supraspinatus modified 3-point Goutallier grade and abduction strength in a population receiving conservative management for full-thickness RC tear.34 To the contrary, our results concur with the findings of Nardo et al, that supraspinatus Goutallier grade did not have significant correlation with abduction strength.25 The results of our study demonstrate that supraspinatus Dixon fat fraction correlates with forward flexion ROM, abduction ROM, and abduction strength; but does not establish a causal relationship.
Our results are in-line with literature that suggests that full-thickness SST tear is associated with significant increases in FI, as compared to rotator cuff muscles with only partial-thickness tear or with no tendon tear.14–16 Painful shoulders with full-thickness SST tear in Group 3 demonstrated significantly higher mean Dixon fat fraction when compared to shoulders in either Group 1 or Group 2 who were without full-thickness tear. Shoulders in Group 1 and Group 2 showed no difference in mean Dixon fat fraction (P = 0.985) or Goutallier grade (P = 0.995).
As expected, shoulder pain was detrimental to performance on physical examination and had a significant moderate inverse correlation with forward flexion ROM, abduction ROM and abduction strength in the study population. Average ROM and strength for study subjects without shoulder pain was superior compared to those with shoulder pain. Although lacking statistical significance, study subjects in our study with both pain and full-thickness SST tear on average had inferior strength and ROM, as compared to study subjects with only pain but no full-thickness SST tear. Future studies with a larger sample size will be needed to confirm these observations.
The routine use of multiecho Dixon MRI techniques for evaluation of FI in patients with RC tear is becoming feasible in clinical practice, as commercial software packages are now readily available from MRI scanner manufacturers.16 Total imaging time for the 6-point Dixon MRI sequence can be performed in less than 1 minute, and postprocessing production of the Dixon fat fraction map can be automated. Most widely available commercial picture archiving and computer systems in use today possess the imaging software tools necessary for the rapid measure of RC muscle Dixon fat fraction on shoulder MRI.16
Limitations
The study was performed at a single time point. The sample size was small reflective of a pilot study, but the study sample was still able to identify significant correlations and differences among the groups for the study population. The sample size limited the statistical power to address the confounding of shoulder pain and presence of full-thickness RC tear for correlation to shoulder ROM and strength for each individual group. The sample size also may have limited power to detect statistically significant correlation for Goutallier grade with forward flexion ROM, abduction ROM and abduction strength. Future longitudinal studies with a larger sample will be necessary to verify the study results. The study population was a convenience sample composed of self-referred or orthopedic-surgeon-referred study subjects, and selection bias may limit the generalizability of the study. We also did not stratify the full-thickness SST tears in Group 3 by tear size, although tear severity is suggested not to be a consistent predictor of shoulder dysfunction or pain and animal models suggest that accelerated deposition of FI occurs in the presence of full-thickness tear even without tendon retraction.5,35,36 The physical examination only provided an indirect measure of the contribution of the supraspinatus muscle to shoulder strength and ROM, since the supraspinatus muscle could not be isolated for testing. We determined supraspinatus muscle Goutallier grade and Dixon fat fraction on single 2D Y-view oblique sagittal images that are well-described in the literature but may not be representative of the entire supraspinatus muscle. However, feasible current methods for quantification of fat content for the entire supraspinatus muscle are not available, and analyses based on the Y-view are widely performed.28–30,37 Our study results may not be generalizable to populations with severe intramuscular fatty infiltration of the supraspinatus muscle, since no study subject had a classification of Goutallier grade 3 or 4. However, shoulders that lack advanced stages of FI have been described as an ideal population for study, since populations with Goutallier grade ≤2 are the most relevant candidates for orthopaedic surgeons to consider for potential RCR surgery during clinical decision-making process for individuals who present with symptomatic RC tear.18 Future studies may be necessary to test the reliability of Dixon fat fraction in RC muscles that are Goutallier grade ≥3. The study population also exhibited a low burden of co-morbidity. Our study may not be applicable to populations with high levels of co-morbidity.
Conclusion
Quantitative Dixon fat fraction of the supraspinatus muscle correlates to shoulder ROM and strength and shows superior correlation relative to semi-quantitative Goutallier grade on MRI. Future larger studies will be useful to confirm these results and to determine if Dixon fat fraction has superior correlation to change in shoulder physical outcome measures over time as compared to Goutallier grade.
Disclosures
Derik L. Davis, MD received partial salary support from the University of Maryland Claude D. Pepper Older Americans Independence Center (NIA 2P30AG028747). R. Frank Henn III, MD received research support from Arthrex, Inc.
Mohit N. Gilotra, MD received support from Arthrex, Inc. for speaking events, education and travel.
Funding
This manuscript was supported by a research seed grant in 2016 from the Radiological Society of North America Research & Education Foundation and Hitachi Medical Systems RSD1614 (PI: Dr. Derik L. Davis).
Footnotes
IRB: The institutional review board for this study was approved by the University of Maryland, Baltimore.
References
- 1.Yamamoto A, Takagishi K, Osawa T, et al. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg 2010;19:116–20. [DOI] [PubMed] [Google Scholar]
- 2.Melis B, Nemoz C, Walch G. Muscle fatty infiltration in rotator cuff tears: Descriptive analysis of 1688 cases. Orthop Traumatol Surg Res 2009;95:319–24. [DOI] [PubMed] [Google Scholar]
- 3.McElvany MD, McGoldrick E, Gee AO, et al. Rotator cuff repair: Published evidence on factors associated with repair integrity and clinical outcome. Am J Sports Med 2015;43:491–500. [DOI] [PubMed] [Google Scholar]
- 4.Jain NB, Higgins LD, Losina E, et al. Epidemiology of musculoskeletal upper extremity ambulatory surgery in the United States. BMC Musculoskelet Disord 2014;15:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McMahon PJ, Prasad A, Francis KA. What is the prevalence of senior-athlete rotator cuff injuries and are they associated with pain and dysfunction? Clin Orthop Relat Res 2014;472:2427–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Piper CC, Hughes AJ, Ma Y, et al. Operative versus nonoperative treatment for the management of full-thickness rotator cuff tears: a systematic review and meta-analysis. J Shoulder Elbow Surg 2018;27:572–6. [DOI] [PubMed] [Google Scholar]
- 7.Gladstone JN, Bishop JY, Lo IK, et al. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med 2007;35:719–28. [DOI] [PubMed] [Google Scholar]
- 8.Liem D, Lichtenberg S, Magosch P, et al. Magnetic resonance imaging of arthroscopic supraspinatus tendon repair. J Bone Joint Surg Am 2007;89:1770–6. [DOI] [PubMed] [Google Scholar]
- 9.Gerber C, Meyer DC, Schneeberger AG, et al. Effect of tendon release and delayed repair on the structure of the muscles of the rotator cuff: An experimental study in sheep. J Bone Joint Surg Am 2004;86-A:1973–82. [DOI] [PubMed] [Google Scholar]
- 10.Uhthoff HK, Matsumoto F, Trudel G, et al. Early reattachment does not reverse atrophy and fat accumulation of the supraspinatus An experimental study in rabbits. J Orthop Res 2003;21:386–92. [DOI] [PubMed] [Google Scholar]
- 11.Uhthoff HK, Coletta E, Trudel G. Effect of timing of surgical SSP tendon repair on muscle alterations. J Orthop Res 2014;32:1430–5. [DOI] [PubMed] [Google Scholar]
- 12.Deniz G, Kose O, Tugay A, et al. Fatty degeneration and atrophy of the rotator cuff muscles after arthroscopic repair: Does it improve, halt or deteriorate? Arch Orthop Trauma Surg 2014;134:985–90. [DOI] [PubMed] [Google Scholar]
- 13.Valencia AP, Lai JK, Iyer SR, et al. Fatty infiltration is a prognostic marker of muscle function after rotator cuff tear. Am J Sports Med 2018;46:2161–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim HM, Dahiya N, Teefey SA, et al. Relationship of tear size and location to fatty degeneration of the rotator cuff. J Bone Joint Surg Am 2010;92:829–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee S, Lucas RM, Lansdown DA, et al. Magnetic resonance rotator cuff fat fraction and its relationship with tendon tear severity and subject characteristics. J Shoulder Elbow Surg 2015;24:1442–51. [DOI] [PubMed] [Google Scholar]
- 16.Davis DL, Zhuo J, Almardawi R, et al. Association of patient self-reported shoulder scores to quantitative and semi-quantitative MRI measures of rotator cuff intramuscular fatty infiltration: A pilot study. AJR Am J Roentgenol 2019;213:1307–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goutallier D, Postel JM, Bernageau J, et al. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994:78–83. [PubMed] [Google Scholar]
- 18.Fuchs B, Weishaupt D, Zanetti M, et al. Fatty degeneration of the muscles of the rotator cuff: Assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg 1999;8:599–605. [DOI] [PubMed] [Google Scholar]
- 19.Lippe J, Spang JT, Leger RR, et al. Inter-rater agreement of the Goutallier, Patte, and Warner classification scores using preoperative magnetic resonance imaging in patients with rotator cuff tears. Arthroscopy 2012;28:154–9. [DOI] [PubMed] [Google Scholar]
- 20.Oh JH, Kim SH, Choi JA, et al. Reliability of the grading system for fatty degeneration of rotator cuff muscles. Clin Orthop Relat Res 2010;468:1558–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Slabaugh MA, Friel NA, Karas V, et al. Interobserver and intraobserver reliability of the Goutallier classification using magnetic resonance imaging: Proposal of a simplified classification system to increase reliability. Am J Sports Med 2012;40:1728–34. [DOI] [PubMed] [Google Scholar]
- 22.Agten CA, Rosskopf AB, Gerber C, et al. Quantification of early fatty infiltration of the rotator cuff muscles: Comparison of multi-echo Dixon with single-voxel MR spectroscopy. Eur Radiol 2016;26:3719–27. [DOI] [PubMed] [Google Scholar]
- 23.Davis DL, Kesler T, Gilotra MN, et al. Quantification of shoulder muscle intramuscular fatty infiltration on T1-weighted MRI: A viable alternative to the Goutallier classification system. Skeletal Radiol 2019;48:535–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Horiuchi S, Nozaki T, Tasaki A, et al. Reliability of MR quantification of rotator cuff muscle fatty degeneration using a 2-point Dixon technique in comparison with the Goutallier classification: Validation study by multiple readers. Acad Radiol 2017;24:1343–51. [DOI] [PubMed] [Google Scholar]
- 25.Nardo L, Karampinos DC, Lansdown DA. Quantitative assessment of fat infiltration in the rotator cuff muscles using water-fat MRI. J Magn Reson Imaging 2014;39:1178–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grimm A, Meyer H, Nickel MD, et al. Evaluation of 2-point, 3-point, and 6-point Dixon magnetic resonance imaging with flexible echo timing for muscle fat quantification. Eur J Radiol 2018;103:57–64. [DOI] [PubMed] [Google Scholar]
- 27.Varkey DT, Patterson BM, Creighton RA, et al. Initial medical management of rotator cuff tears: A demographic analysis of surgical and nonsurgical treatment in the United States Medicare population. J Shoulder Elbow Surg 2016;25:e378–85. [DOI] [PubMed] [Google Scholar]
- 28.Nozaki T, Tasaki A, Horiuchi S, Ochi J, et al. Predicting retear after repair of full-thickness rotator cuff tear: Two-point Dixon MR imaging quantification of fatty muscle degeneration-initial experience with 1-year follow-up. Radiology 2016;280:500–9. [DOI] [PubMed] [Google Scholar]
- 29.Mellado JM, Calmet J, Olona M, et al. Surgically repaired massive rotator cuff tears: MRI of tendon integrity, muscle fatty degeneration, and muscle atrophy correlated with intraoperative and clinical findings. AJR Am J Roentgenol 2005;184:1456–63. [DOI] [PubMed] [Google Scholar]
- 30.Yoo JC, Ahn JH, Yang JH, Koh KH, et al. Correlation of arthroscopic repairability of large to massive rotator cuff tears with preoperative magnetic resonance imaging scans. Arthroscopy 2009;25:573–82. [DOI] [PubMed] [Google Scholar]
- 31.Kumar D, Karampinos DC, MacLeod TD, et al. Quadriceps intramuscular fat fraction rather than muscle size is associated with knee osteoarthritis. Osteoarthritis Cartilage 2014;22:226–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gerber C, Meyer DC, Fluck M, et al. Anabolic steroids reduce muscle degeneration associated with rotator cuff tendon release in sheep. Am J Sports Med 2015;43:2393–400. [DOI] [PubMed] [Google Scholar]
- 33.Spencer EE Jr., Dunn WR, Wright RW, et al. Interobserver agreement in the classification of rotator cuff tears using magnetic resonance imaging. Am J Sports Med 2008;36:99–103. [DOI] [PubMed] [Google Scholar]
- 34.Nakamura Y, Yokoya S, Harada Y, et al. The prospective evaluation of changes in fatty infiltration and shoulder strength in nonsurgically treated rotator cuff tears. J Orthop Sci 2017;22:676–81. [DOI] [PubMed] [Google Scholar]
- 35.Dunn WR, Kuhn JE, Sanders R, et al. Symptoms of pain do not correlate with rotator cuff tear severity: A cross-sectional study of 393 patients with a symptomatic atraumatic full-thickness rotator cuff tear. J Bone Joint Surg Am 2014;96:793–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Uhthoff HK, Coletta E, Trudel G. Intramuscular fat accumulation and muscle atrophy in the absence of muscle retraction. Bone Joint Res 2014;3(4):117–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Santago AC, Vidt ME 2nd, Tuohy CJ, et al. Quantitative analysis of three-dimensional distribution and clustering of intramuscular fat in muscles of the rotator cuff. Ann Biomed Eng 2016;44:2158–67. [DOI] [PMC free article] [PubMed] [Google Scholar]


