Abstract
Introduction:
The lack of national fetal alcohol spectrum disorder (FASD) prevalence estimates represents an important knowledge gap.
Methods:
Using data from the 2019 Canadian Health Survey on Children and Youth, the prevalence of FASD was examined by age, sex and Indigenous identity. Median age of diagnosis and comorbid long-term health conditions were also assessed.
Results:
The prevalence of FASD among Canadian children and youth living in private dwellings was 1 per 1000 (0.1%). The prevalence was significantly higher among those who identified as Indigenous and lived off reserve (1.2%).
Conclusion:
These findings are in keeping with FASD prevalence studies that used similar passive surveillance methods. They provide a starting point to better understanding the prevalence and burden of FASD in Canada.
Keywords: fetal alcohol spectrum disorder, prevalence, public health surveillance, child health, Canadian Health Survey on Children and Youth
Highlights
In 2019, the prevalence of FASD among Canadian children and youth aged 1 to 17 years living in private dwellings was 1 per 1000 (0.1%).
Canadian children and youth who identified as Indigenous and lived off reserve had a significantly higher prevalence of FASD than those who did not identify as Indigenous (1.2% versus 0.1%).
The median age of diagnosis for children and youth with FASD was 5.7 years old.
Most children and youth with FASD had at least one other longterm condition.
We need national surveillance of FASD to better understand the prevalence of this condition.
Introduction
Fetal alcohol spectrum disorder (FASD) is a diagnostic term used to describe the impacts on the brain and body of individuals prenatally exposed to alcohol.1,2 FASD is a lifelong disability. Individuals with FASD will experience some degree of challenges in their daily living and need support with motor skills, physical health, learning, memory, attention, communication, emotional regulation and social skills to reach their full potential.
Each individual with FASD is unique and has areas of both strengths and challenges.3
A significant amount of evidence has accumulated to support prevention and to help in the early identification and diagnosis as well as in estimating prevalence of FASD.4 Various methodologies have been used and tested to estimate prevalence, mostly focussing on specific geographical areas and vulnerable populations.5-7 Prevalence estimates for Canada have neither been consistent nor national in scope. Prevalence of FASD is inherently difficult to measure, mainly because of the challenges associated with recognition, screening and diagnosis.8 There is no specific biological or genetic marker for FASD. In addition, many children who were adversely affected by prenatal exposure to alcohol will not present with the physical characteristics of FASD such as dysmorphic facial features.9 Canadian diagnostic guidelines require detailed information on prenatal alcohol exposure for confirmed diagnoses, which is not always available.9 This makes identifying FASD challenging in all but the most severe cases.1
The lack of national FASD prevalence estimates represents an important knowledge gap in informing the public health response. This article aims to provide initial national estimates of the magnitude of FASD prevalence using the 2019 Canadian Health Survey on Children and Youth (CHSCY).
Methods
The 2019 CHSCY surveyed a national sample of Canadians aged 1 to 17 years, as of 31 January 2019, living in private dwellings in the ten provinces and three territories (n = 39 951; response rate 52.1%).10,11 Excluded from the survey’s coverage are children and youth living on First Nation reserves and other Indigenous settlements in the provinces, in foster homes and in institutions.10 Data were collected via selfreported questionnaire administered to the person most knowledgeable about the child/youth (aged 1–17 years).11
Children and youth were identified as having FASD if the respondent answered “yes” to the question: “Has this child been diagnosed with any of the following longterm conditions? – Fetal Alcohol Spectrum Disorder, also known as FASD.”12
The following select sociodemographic and health-related variables were included in this study: age (1–11 years vs. 12–17 years), sex (male vs. female) and Indigenous identity (First Nations/Mtis/Inuit vs. non-Indigenous).
The median age of diagnosis was derived from the question: “How old was this child when first diagnosed with the following conditions? – Fetal Alcohol Spectrum Disorder, also known as FASD.”12
Children/youth were identified as having another long-term condition if the respondent answered “yes” to the question: “Has this child been diagnosed with any of the following long-term conditions?” Conditions included asthma, diabetes, epilepsy, anxiety disorder, mood disorder, eating disorder, learning disability/disorder, attention deficit disorder/attention deficit hyperactivity disorder (ADD/ADHD), autism spectrum disorder and other unspecified conditions.12
Descriptive analyses were conducted to examine the prevalence of FASD among Canadian children and youth. Where relevant, the estimates for those with FASD were compared to those without this diagnosis. All estimates were weighted to be representative of the Canadian population aged 1 to 17 years, and we used the bootstrap method to calculate variance estimates, including 95% confidence intervals (CI) and coefficients of variation. All analyses were carried out using the statistical package SAS Enterprise Guide version 7.1.13 Results were suppressed if the sampling variability was high (coefficient of variation was over 35%).
Results
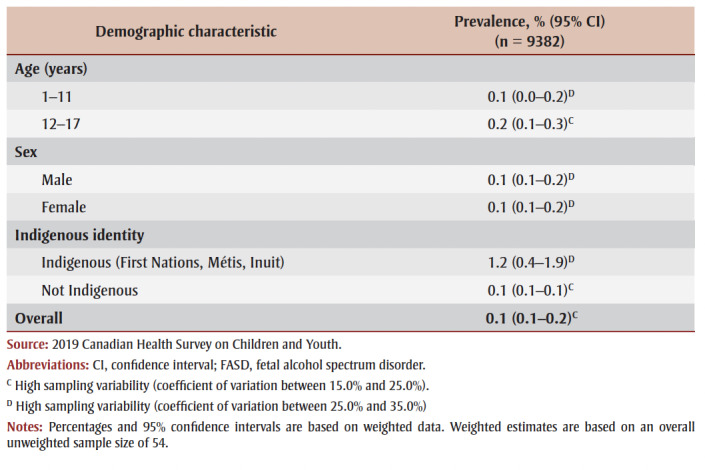
In 2019, an estimated 9400 (based on an unweighted sample size of 54), or 1 per 1000 Canadian children and youth aged 1 to 17 years, had been diagnosed with FASD (0.1%C; 95% CI: 0.1–0.2) (Table 1). This represents 1 per 1000 children/youth aged 1 to 11 years (0.1%D; 95% CI: 0.0– 0.2) and 2 per 1000 aged 12 to 17 years (0.2%C; 95% CI: 0.1–0.3). The prevalence was the same for male and female children and youth.
Table 1. Prevalence of FASD among children and youth, 1–17 years old, by select demographic characteristics, Canada, 2019.
|
While data were available to examine various socioeconomic variables, such as ethnicity (visible minority/not visible minority), urban/rural status, income and education, the high sampling variability associated with the resulting estimates did not allow for these to be reported.
The prevalence of FASD among Indigenous children and youth living off reserve was 1.2%D (95% CI: 0.4–1.9) compared to 0.1%C (95% CI: 0.1–0.1) for non-Indigenous children (Table 1). These estimates, while statistically significantly different, should be interpreted with caution as they are associated with high coefficients of variation.
The median age of diagnosis for children and youth with FASD was 5.7 years old (95% CI: 3.8–7.6); this did not differ statistically significantly when examined by sex or other sociodemographic variables (data not shown).
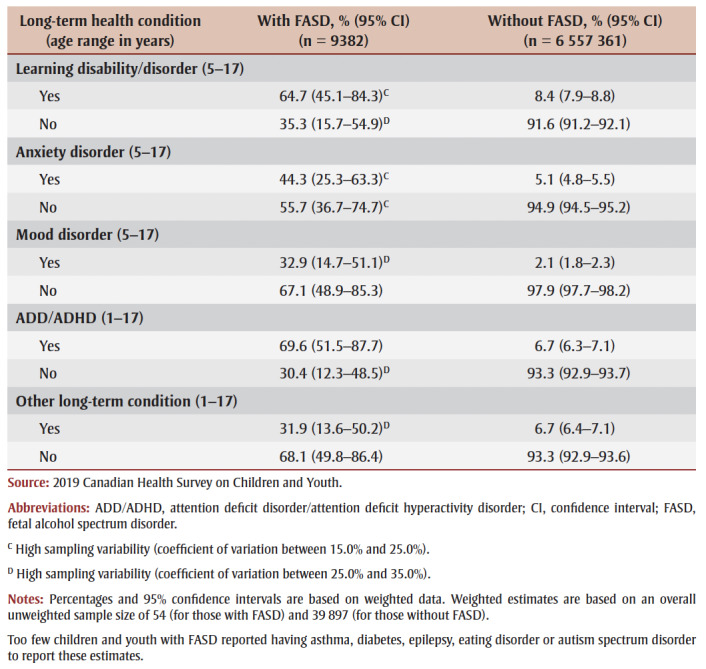
FASD is a condition associated with a high number of comorbidities.14 The majority (82.7%; 95% CI: 66.5–98.9) of children and youth with FASD had at least one other long-term condition compared with just under a quarter (23.4%; 95% CI: 22.8–24.0) of those without FASD. Of those aged 5 to 17 years, 64.7%C (95% CI: 45.1–84.3) had a diagnosed learning disability/ disorder; 44.3%C (95% CI: 25.3– 63.3) had a diagnosed anxiety disorder; and 32.9%D (95% CI: 14.7–51.1) had a diagnosed mood disorder (Table 2). Of those aged 1 to 17 years, 69.6% (95% CI: 51.5–87.7) had diagnosed ADD/ADHD and 31.9%D (95% CI: 13.6–50.2) had other non-specified diagnosed long-term conditions (Table 2).
Table 2. Long-term health conditions among children and youth, 1–17 years old, with or without FASD, Canada, 2019.
|
Discussion
Based on the data from the 2019 CHSCY, the estimated national prevalence of diagnosed FASD among children and youth aged 1 to 17 years is 1 per 1000 or 0.1%C. No statistically significant differences were found between males and females, but the prevalence of FASD was higher among children and youth identifying as Indigenous and living off reserve.
Canadian prevalence studies of FASD have employed various methods including clinical examinations and active case ascertainment while focussing on different population groups, jurisdictions and age ranges.5,15 Published Canadian estimates range from 0.09%, using an early childhood development instrument,5 to 1.4% to 4.4%, using active methods of case ascertainment.15,16 Similar studies conducted in Australia, the United States and countries in Western Europe, albeit using different methods and covering different ages, found FASD prevalence ranges between 1% and 5% among children.6,17-20 Our finding of 0.1% is in the lower end of this range, but is in keeping with studies that used a passive case ascertainment approach,5 although far lower than those using an active case ascertainment method.15
Canadian children and youth who identified as Indigenous and who lived off reserve had a significantly higher prevalence of FASD than those who did not (1.2% versus 0.1%). Data from the CHSCY cannot be examined for differences in diagnostic practices, access to care or other factors that could account for the differences in prevalence. However, this estimate is in line with other studies that focussed on Indigenous populations.21 One study found that the pooled prevalence of FASD among Indigenous children and youth living on and off reserve in Canada was 8.7%, compared to 0.5% in the general population.21 Similar patterns were found among children and youth in Western Australia and the southwest United States, also with large Indigenous populations. 6,7,22 These studies reported FASD prevalence estimates from 2%6 to close to 20%.7 The prevalence of FASD among First Nations children living on reserve has decreased over time: the 2015–2016 First Nations Regional Health Survey reported the prevalence to be 0.5%, down from 1.8% in 2002– 2003.23
The difference in prevalence rates among Indigenous children and youth living off reserve and non-Indigenous children and youth cannot be associated solely with differences in prenatal alcohol exposure. Interconnected and complex factors have been identified and linked to FASD and prenatal alcohol exposure. These factors include the devastating effects of colonization, including residential school experiences, and the ongoing economic and social marginalization that Indigenous peoples experience.24
Strengths and limitations
A strength of this study is that the 2019 CHSCY is a national, population-based survey that covers a wide range of topics and allows for an in-depth look into the health and sociodemographic characteristics of Canadian children and youth. At present, the CHSCY is the only national source of data allowing the calculation of national FASD prevalence estimates. Nevertheless, despite representing 98% of the Canadian population, the CHSCY does not include population groups of children and youth with known higher prevalence rates of FASD,21,25 that is, those living on First Nations reserves and other Indigenous settlements in the provinces, in foster homes or in institutions. These exclusions may have resulted in underestimating the prevalence of FASD among Canadian children and youth.
While acceptable for reporting, the number of FASD cases in this analysis was small. Analyses to investigate the role of sociodemographic factors among those with FASD could not be reported due to high sampling variability. Furthermore, as stigma may be attached to a diagnosis of FASD, underreporting can be expected.15
In this analysis, over three-quarters of children and youth with FASD had another co-occurring condition. Popova and others14 hypothesized that the number of cooccurring conditions in individuals with FASD could account for lower than expected prevalence estimates of FASD. These other conditions could be behind sought-after medical attention, leading to an underdiagnosis of the underlying cause (i.e. FASD) of the comorbidity.14
Passive approaches to data collection, such as the CHSCY, are more efficient and representative, but tend to generate the lowest estimates for the reasons noted above. Active and clinical approaches, while producing higher prevalence estimates and more detail on FASD cases, are more expensive and time consuming, and thus usually target particular geographical areas of interest or subpopulations.4
C High sampling variability (coefficient of variation between 15.0% and 25.0%).
D High sampling variability (coefficient of variation between 25.0% and 35.0%).
Conclusion
National surveillance of FASD is needed to gain a better understanding of the estimated prevalence and provide baseline numbers against which future public health actions can be evaluated. Using data from the 2019 CHSCY, we estimated the prevalence of FASD among Canadian children and youth living in private dwellings to be 1 per 1000.
This analysis presents, to our knowledge, the first national FASD prevalence estimate in Canada. It provides a starting point to identify the burden of this preventable condition. In light of the existing challenges, a combination of passive and active surveillance approaches and/or data sources may be required to establish FASD surveillance in Canada.
Acknowledgements
The data shown in the tables are based on the results of the Canadian Health Survey on Children and Youth (CHSCY), Statistics Canada, 2019. We would also like to acknowledge the assistance of the Advisory Committee on Indigenous Women’s Wellbeing and Dr. Jocelynn Cook for their insightful comments on this manuscript.
Conflicts of interest
None.
Authors’ contributions and statement
SP analyzed the data, and AP and SP drafted the paper. All authors contributed to the study concept, informed the data analysis, assisted in the interpretation of results, critically revised the manuscript and approved the final version.
The content and views expressed in this At-a-glance article are those of the authors and do not necessarily reflect those of the Government of Canada.
References
- Cook JL, Green CR, Lilley CM, et al. Fetal alcohol spectrum disorder: a guideline for diagnosis across the lifespan. CMAJ. 2016:191–7. doi: 10.1503/cmaj.141593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones KL, Smith DW, Ulleland CN, Streissguth P, et al. Pattern of malformation in offspring of chronic alcoholic mothers. Lancet. 1973;301((7815)):1267–71. doi: 10.1016/s0140-6736(73)91291-9. [DOI] [PubMed] [Google Scholar]
- Harding K, Flannigan K, McFarlane A, et al. CanFASD. Vancouver(BC): Policy action paper: toward a standard definition of fetal alcohol spectrum disorder in Canada. [Google Scholar]
- May PA, Gossage JP, et al. Estimating the prevalence of fetal alcohol syndrome. Alcohol Res Health. 2001:159–67. [PMC free article] [PubMed] [Google Scholar]
- Pei J, Reid-Westoby C, Siddiqua A, et al, et al. Teacher-reported prevalence of FASD in kindergarten in Canada: association with child development and problems at home. J Autism Dev Disord. 2021;51((2)):433–43. doi: 10.1007/s10803-020-04545-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox DJ, Pettygrove S, Cunniff C, et al, et al. Fetal alcohol syndrome among children aged 7–9 years — Arizona, Colorado, and New York, 2010. Fox DJ, Pettygrove S, Cunniff C, et al. 2015;64((3)):54–7. [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick JP, Latimer J, Olson HC, et al, et al. Prevalence and profile of neurodevelopment and fetal alcohol spectrum disorder (FASD) amongst Australian Aboriginal children living in remote communities. Res Dev Disabil. 2017:114–26. doi: 10.1016/j.ridd.2017.04.001. [DOI] [PubMed] [Google Scholar]
- Flannigan K, Unsworth K, Harding K, et al. CanFASD. Vancouver(BC): The prevalence of fetal alcohol spectrum disorder. [Google Scholar]
- Chudley AE, et al. Diagnosis of fetal alcohol spectrum disorder: current practices and future considerations. Biochem Cell Biol. 2018;96((2)):231–6. doi: 10.1139/bcb-2017-0106. [DOI] [PubMed] [Google Scholar]
- Statistics Canada. Ottawa(ON): Canadian Health Survey on Children and Youth (CHSCY) [Google Scholar]
- 2019 Canadian Health Survey on Children and Youth (CHSCY): User Guide. Statistics Canada. 2020 [Google Scholar]
- Canadian Health Survey on Children and Youth -2019: Questionnaire. Statistics Canada. :Questionnaire–6. [Google Scholar]
- . Cary (NC): SAS Institute Inc. . Statistical Analysis System Enterprise Guide version 7 [Google Scholar]
- Popova S, Lange S, Shield K, et al, et al. Comorbidity of fetal alcohol spectrum disorder: a systematic review and meta-analysis. Lancet. 2016;387((10022)):978–87. doi: 10.1016/S0140-6736(15)01345-8. [DOI] [PubMed] [Google Scholar]
- Popova S, Lange S, Poznyak V, et al, et al. Population-based prevalence of fetal alcohol spectrum disorder in Canada. BMC Public Health. 2019;19((1)):845–87. doi: 10.1186/s12889-019-7213-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thanh NX, Jonsson E, Salmon A, Sebastianski M, et al. Incidence and prevalence of fetal alcohol spectrum disorder by sex and age group in Alberta, Canada. J Popul Ther Clin Pharmacol. 2014;21((3)):e395–404. [PubMed] [Google Scholar]
- Mutch RC, Watkins R, Bower C, et al. Fetal alcohol spectrum disorders: notifications to the Western Australian Register of Developmental Anomalies. J Paediatr Child Health. 2015;51((4)):433–6. doi: 10.1111/jpc.12746. [DOI] [PubMed] [Google Scholar]
- May PA, Baete A, Russo J, et al, et al. Prevalence and characteristics of fetal alcohol spectrum disorders. Pediatrics. 2014;134((5)):855–66. doi: 10.1542/peds.2013-3319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Chambers CD, Kalberg WO, et al, et al. Prevalence of fetal alcohol spectrum disorders in 4 US communities. JAMA. 2018;319((5)):474–82. doi: 10.1001/jama.2017.21896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Gossage JP, Kalberg WO, et al, et al. Prevalence and epidemiologic characteristics of FASD from various research methods with an emphasis on recent in-school studies. Dev Disabil Res Revs. 2009;15((3)):176–92. doi: 10.1002/ddrr.68. [DOI] [PubMed] [Google Scholar]
- Popova S, Lange S, Probst C, Parunashvilia N, Rehmabde J, et al. Prevalence of alcohol consumption during pregnancy and Fetal Alcohol Spectrum Disorders among the general and Aboriginal populations in Canada and the United States. Eur J Med Genet. 2017;60((1)):32–48. doi: 10.1016/j.ejmg.2016.09.010. [DOI] [PubMed] [Google Scholar]
- Montag AC, Romero R, Jensen T, et al, et al. The prevalence of fetal alcohol spectrum disorders in an American Indian community. Int J Environ Res Public Health. 2019;16((12)):2179–48. doi: 10.3390/ijerph16122179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First Nations Information Governance Centre. Akwesasne(ON): FNIGC data online: percentage of First Nations children diagnosed with a mental health condition or FASD [database] [Google Scholar]
- Tait C, et al. Aboriginal Healing Foundation. Ottawa(ON): 2003. Fetal alcohol syndrome among Aboriginal people in Canada: review and analysis of the intergenerational links to residential schools. [Google Scholar]
- Bower C, Watkins RE, Mutch RC, et al, et al. Fetal alcohol spectrum disorder and youth justice: a prevalence study among young people sentenced to detention in Western Australia. BMJ Open. 2018;8((2)):e019605–48. doi: 10.1136/bmjopen-2017-019605. [DOI] [PMC free article] [PubMed] [Google Scholar]


