Abstract
Introduction
Abdominal surgery is associated with common complications, including decreased or poor appetite, abdominal distension, abdominal pain caused by decreased or absent gastrointestinal motility, anal arrest with flatus and defecation, and nausea and vomiting resulting from the use of anaesthetics and opioid analgesics. These complications seriously affect postoperative recovery, prolong hospital stay and aggravate patient burden. This study aims to investigate for the first time the efficacy of transcutaneous electrical acupoint stimulation (TEAS) combined with electroacupuncture (EA) therapy for rapid recovery after laparotomy for gastrointestinal surgery. There have been no clinical studies of this combination therapy.
Methods and analysis
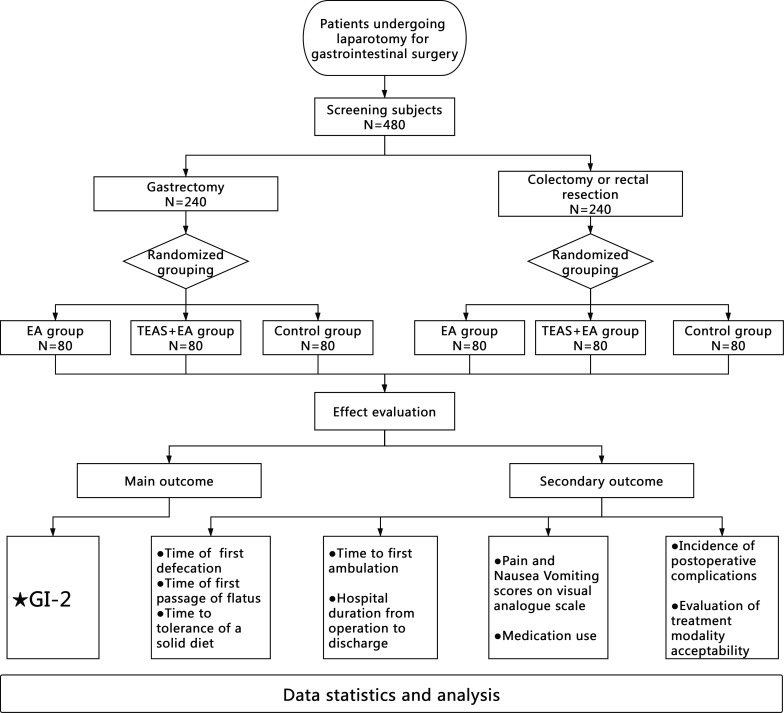
This will be a prospective, single-centre, three-arm, randomised controlled trial. A total of 480 patients undergoing abdominal surgery will be stratified according to surgery type (ie, gastric or colorectal procedure) and randomised into three groups; namely, the EA, TEAS +EA and control groups. The control group will receive enhanced recovery after surgery (ERAS)-standardised perioperative management, including preoperative education, optimising the anaesthesia scheme, avoiding intraoperative hypothermia, restrictive fluid infusion and reducing surgical trauma. The EA group will receive EA stimulation at LI4, PC6, ST36, ST37 and ST39 based on the ERAS-standardised perioperative management. Moreover, the TEAS +EA group will receive ERAS-standardised perioperative management; EA stimulation at the LI4, PC6, ST36, ST37 and ST39; and TEAS stimulation at ST21 and SP15. The primary outcome will be the GI-2 (composite outcome of time to first defaecation and time to tolerance of a solid diet). Secondary outcomes will include the time of first passage of flatus, time to first defaecation, time to tolerance of a solid diet, time to first ambulation, hospital duration from operation to discharge, pain and nausea vomiting scores on the Visual Analogue Scale, medication use, incidence of postoperative complications and evaluation of treatment modality acceptability. All statistical analyses will be performed based on the intention-to-treat principle.
Ethics and dissemination
Ethics approval has been granted by the Ethics Committee on Biomedical Research, West China Hospital of Sichuan University (approval number: 2021; number 52). The results are expected to be published in peer-reviewed journals.
Trial registration number
ChiCTR2100045646.
Keywords: complementary medicine, pain management, gastroenterology
Strengths and limitations of this study.
A randomised controlled trial of 480 patients will be conducted to evaluate the efficacy of transcutaneous electrical acupoint stimulation combined with electroacupuncture therapy for rapid recovery after laparotomy for gastrointestinal surgery.
The trial feasibility has been examined in a pilot randomised trial of 120 patients, included 60 patients with laparotomy stomach tumour resection and 60 patients with laparotomy colon tumour resection.
This trial will be conducted using rigorous methods; for example, the patients will be randomly assigned to three groups; the data will undergo blind statistical analysis; and the interventionists, efficacy evaluators and statisticians will be separated.
This trial did not include a sham control arm, the analysis of the placebo response or effect was lacking.
Introduction
The most common postoperative complications in laparotomy for gastrointestinal surgery include gastrointestinal dysfunction, pain, postoperative nausea and vomiting (PONV), etc. These result from numerous factors, including the intraoperative use of anaesthetic drugs, surgical trauma, peritoneal irritation or inflammatory response and postoperative use of analgesic drugs.1–3 Rapid postoperative rehabilitation can prevent or reduce intraperitoneal adhesion; reduce the incidence of complications, including intestinal obstruction and intestinal infection; prevent secondary surgery, reduce opioid usage and alleviate pain. Moreover, it can promote prompt recovery of the patients’ oral diet, reduce the use of parenteral nutrition, shorten the hospitalisation duration and reduce hospitalisation costs.4–8
Enhanced recovery after surgery (ERAS) is based on evidence-based medicine and is a standardised, collaborative and multidisciplinary optimisation management protocol for the perioperative period. It allows a reduction in the physiological and psychological traumatic stress response, as well as postoperative complications; a faster postoperative recovery; a shorter postoperative hospitalisation time and a reduction in patient costs.9 This concept was initially proposed by the Danish Medical Scientist Kehlet in 1997.10 After >20 years of practice and optimisation, the ERAS concept and pathway have been popularised and rapidly applied worldwide.11 Although a series of perioperative ERAS measures can accelerate recovery, there remains room for improvement in the prevention and treatment of postoperative gastrointestinal dysfunction and PONV, as well as in the reduction of opioid use.12
Acupuncture exerts therapeutic effects by regulating gastrointestinal dynamics, analgesia and antiemetics. It is widely considered that a degree of postoperative gastrointestinal dysfunction is an inevitable normal physiological response after abdominal surgery.13 Several studies have demonstrated that acupuncture can significantly relieve postoperative abdominal pain and distension, promote intestinal ventilation, and promptly restore the patient’s diet.14 15 Acupuncture can enhance gastric dilatation through the sympathetic nerve to promote gastric emptying16 17; moreover, the vasoactive intestinal peptide is involved in electroacupuncture (EA)-mediated gastric motility regulation.
Studies have shown that Zusanli (ST36), Shangjuxu (ST37) and Xiajuxu (ST39) stimulation can effectively improves gastrointestinal transit by reducing local inflammation of the intestinal musculature.18 Hegu(LI4) is a pair of acupoints belonging to the Large Intestinal meridian, Daheng(SP15) is a pair of acupoints belonging to the Spleen meridian, Liangmen(ST21) is a pair of acupoints belonging to the Stomach meridian. They have the effect of assisting gastrointestinal function recovery, so they are also commonly used in clinical practice.19–21
Additionally, acupuncture can facilitate postoperative multimodal analgesia. Postoperative analgesia is among the core ERAS components. Its principles include sufficient analgesia and minimisation of opioid usage. Adequate postoperative analgesia can reduce excessive stress, help patients get out of bed quickly and promote recovery. Opioids, which are the main traditional postoperative analgesic drugs, can easily cause postoperative nausea, vomiting and other complications. Reducing opioid usage allows early recovery of patients. There have been numerous studies on the mechanisms underlying acupuncture analgesia from the perspectives of electrophysiology, neurochemistry, molecular biology and brain imaging.22–24 Moreover, numerous clinical studies have shown that acupuncture can significantly reduce postoperative pain and opioid use after total hip replacement, craniotomy, abdominal surgery and kidney stone surgery.25–28 Therefore, based on the ERAS clinical pathway, acupuncture analgesia may better control wound pain and reduce the use of analgesics, including opioids, and therefore, accelerate patient recovery.29
PONV is a common complication after surgical anaesthesia and analgesia with opioids that can cause dehydration, electrolyte imbalance, wound cracking and discharge delay. PONV is another important factor that affects the recovery of patients.30 Studies have shown that Neiguan (PC6) stimulation can effectively prevent PONV.31 32 Transcutaneous electrical acupoint stimulation (TEAS) is more effective than intravenous ondansetron; additionally, using TEAS combined with drugs can enhance the antiemetic effects of ondansetron.33
Numerous studies have supported the application of acupuncture in postoperative rehabilitation; however, there are differences in efficacy across different acupuncture schemes. Currently, EA is the most common acupuncture scheme for rapid postoperative rehabilitation, with TEAS being the second most common scheme. Although TEAS avoids pain resulting from acupuncture needles, its efficacy is slightly worse than that of EA and it has relatively limited clinical application.34 However, our previous clinical experience and preliminary trials suggested that combining TEAS with EA may have a better curative effect than the conventional EA treatment.35–37 Moreover, this combination could provide an improved acupuncture treatment protocol for rapid rehabilitation after laparotomy for gastrointestinal surgery. It may promote the recovery of gastrointestinal function more quickly, reduce pain more obviously, shorten the duration of postoperative hospital stay and reduce patient hospitalisation costs, etc.
Therefore, this prospective, single-centre, three-arm, single-blind, randomised controlled trial (RCT) aims to evaluate the efficacy of TEAS combined with EA therapy for rapid recovery after laparotomy for gastrointestinal surgery.
Methods and analysis
Design
This will be a single-centre, prospective RCT with a three-arm parallel grouping design. The trial protocol V.2.0, date 31 March 2021. The study will be conducted at the West China Hospital of Sichuan University (WCHSU) from April 2021 to March 2023. All the participants will be required to provide written informed consent in accordance with the most recent version of the Declaration of Helsinki. Figure 1 presents the study flow chart.
Figure 1.
Flow chart of the study protocol. EA, electroacupuncture; TEAS, transcutaneous electrical acupoint stimulation; GI-2, composite outcome of time to first defaecation and time to tolerance of a solid diet.
Patient population and setting
A total of 480 Chinese patients undergoing laparotomy for gastrointestinal surgery will be sequentially enrolled at the WCHSU after fulfilling the eligibility criteria and signing informed consent. A clinical assistant with institutional review board training will be in charge of patient enrolment.
Eligibility criteria
The inclusion criteria will be as follows: (1) male and female patients aged 18–70 years; (2) laparotomy tumour resection under general anaesthesia (stomach, colon and rectum) and (3) volunteering to participate in this study and signing an informed consent form.
The exclusion criteria will be as follows: (1) surgical incision or scar on the meridian of ST21/SP15, (2) local skin infection at acupoints, (3) inability to complete the Visual Analogue Scale (VAS) and (4) allergy to metal or severe needle fear, intolerance of TEAS or EA treatment, (5) uncontrolled diabetes, severe cardiac, central nervous, psychiatric disorders or coagulopathy; (6) cardiac pacemaker and (7) participation in other clinical trials.
Withdrawal criteria: Participants meeting any of the following criteria will be withdrawn from the study: (1) occurrence of serious adverse events; (2) participants with serious complications or other serious diseases requiring emergency measures, (3) being required to withdraw during the test and (4) violation of the test programme. Withdrawn patients will not be replaced.
Randomisation and blinding
This study will have a single-blind design. The patient will be blinded to the group allocation; moreover, patients in the same ward will be separated by a bed curtain when receiving acupuncture treatment, with only the research leader and acupuncturist being aware of the treatment allocation. The randomised grouping plan will be designed using SPSS V.22.0. According to the plan, 480 patients will be randomly divided into three groups according to a ratio of 1:1:1: EA, TEAS+EA and control groups. The group scheme will be kept in a confidential envelope; further, the research leader will randomly distribute the included patients to each group following the distribution plan in the envelope. Additionally, the research leader will only inform the acupuncturist responsible for the operation. Efficacy evaluation will be conducted blinded to the grouping allocation. Blind statistical analysis will be used in the data summary stage. Operators, efficacy evaluators and statisticians will be separated.
Intervention
All acupoints will be determined based on the National Standard of Nomenclature and Location of Acupuncture Points (GB/T 12 346-2006).38 All practitioners performing the treatment must have an acupuncturist qualification certificate with independent clinical experience for >2 years. The acupuncturists will not be replaced during the experiments.
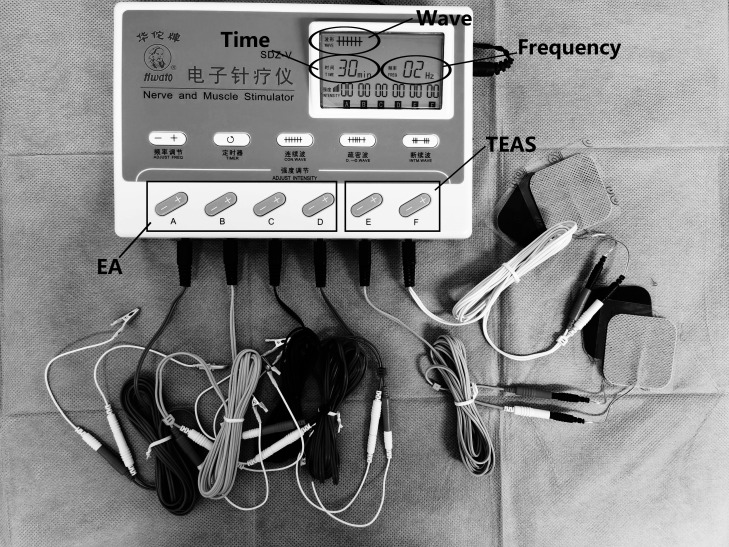
All patients will receive standardised perioperative management by ERAS, including preoperative education, optimisation of anaesthesia scheme, avoidance of intraoperative hypothermia, restrictive fluid infusion and reduction of surgical trauma. Regarding the electronic acupuncture treatment instrument (Hwato, SDZ-V, Suzhou Medical Supplies Factory), the current frequency will be continuous wave 2 Hz, the current intensity will be measured in degrees as tolerated by the patient; moreover, the treatment duration will last 30 min (figure 2). The treatment will be initiated from the first postoperative day, once daily in the morning, until the patient regains defecation and could tolerate transoral solid food.
Figure 2.
Instrument and parameter. EA, electroacupuncture; TEAS, transcutaneous electrical acupoint stimulation.
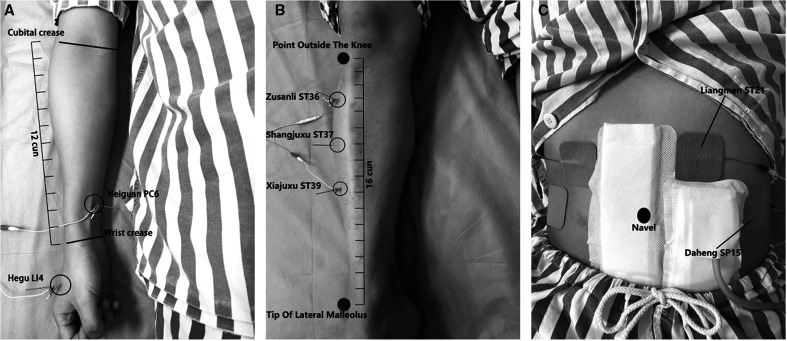
In the EA group (EA is added at the base of basic treatment), treatment will be bilaterally performed at five acupoint pairs: Hegu (LI4), Neiguan (PC6), Zusanli (ST36), Shangjuxu (ST37) and Xiajuxu (ST39). LI4 is an acupoint of the large intestine meridian and is located on the dorsum of the hand between the first and second metacarpal bones. PC6 belongs to the pericardium meridian and is located between the flexor carpi radialis muscle tendon and the palmaris longus tendon, 2 Cun above the wrist crease. ST36, ST37 and ST39 are acupoints of the stomach meridian. ST36 is located on the lateral side of the lower leg, 3 Cun below the lateral border of the knee and one finger width lateral to the anterior border of the tibia. ST37 is located 3 Cun below ST36. ST39 is located 3 Cun below ST37. After skin disinfection with a disposable disinfecting cotton swab, sterile and disposable stainless steel needles (0.25×40 mm, Suzhou Jiajian, Jiangsu, China) will be quickly and perpendicularly inserted into the skin acupoints at a depth of 25–30 mm. The duration of reinforcing-reducing manipulation of twirling and rotating needles should be used for 1 min to achieve de qi (a composite of sensations including soreness, numbness, distention, heaviness and other sensations), which significantly contributes to acupuncture efficacy. The ipsilateral Neiguan, Hegu, Zusanli and Xiajuxu will be separately connected to one electrode set, and therefore yielding four electrode sets (figure 3A, B).
Figure 3.
Localisation of acupoints and electrode connection.
For the TEAS+EA group, treatment will be based on the EA group with the addition of two pairs of bilateral abdominal acupoints: Liangmen (ST21) and Daheng (SP15). Additionally, ST21 is an acupoint of the stomach meridian that is located 4 Cun above the umbilicus and 2 Cun open next to the anterior median line. SP15 is an acupoint of the spleen meridian, located 4 Cun beside the umbilicus and lateral to the rectus abdominis muscle. Abdominal acupoints will be stimulated using a self-adhesive electrode pad with electrical conductivity; additionally, the ipsilateral Liangmen will be connected to the Daheng set of electrodes. The ipsilateral Neiguan, Hegu, Zusanli and Xiajuxu acupoints will be connected to one electrode set to yield a total of six sets of electrodes (figure 3A–C).
The control group will receive ERAS-standardised perioperative management without acupuncture treatment.
Outcome measures
Main outcome
The primary outcome will be the GI-2 (Gastrointestinal-2, composite outcome of time to first defaecation and time to tolerance of a solid diet). Participants will be visited and evaluated by efficacy evaluators at the end of each treatment.
Secondary outcome
The secondary outcomes include the time of first passage of flatus, time to first defaecation, time to tolerance of a solid diet, time to first ambulation, hospital duration from operation to discharge, pain and nausea vomiting scores on the VAS (from 0 (no at all) to 10 (the worst)), medication use(name, frequency and dosage of analgesic drugs and antiemetic agents), incidence of postoperative complications(include intra-abdominal infection, intestinal ischaemia and necrosis, anastomotic leak, pulmonary infection, etc), and evaluation of treatment modality acceptability(classified into five grades: very acceptable, moderately acceptable, somewhat acceptable, moderately unacceptable and totally unacceptable). Participants will be visited and evaluated by efficacy evaluators at the end of each treatment.
We add GI-2 as a primary outcome outcome to the original protocol after recruitment of the study had already begun. GI-2 is a time indicator, which will be calculated from two existing outcomes (time to first defaecation and time to tolerance of oral diet). There will be no harm to subjects, no additional cost and no more work.
Safety evaluation
All adverse events will be recorded on the adverse event record sheet by the acupuncturist and participants at any time during the study period. Adverse events to be recorded include fainting during acupuncture treatment, needle breaking, unbearable acupuncture pain, local haematoma, infection and any other discomfort or accident. The intensity and causality of each adverse event will be evaluated and recorded. If any serious adverse events occur due to an intervention, the intervention will be immediately stopped; further, appropriate corrective action will be taken. Serious adverse events will be promptly reported to the institutional review board within 24 hours until 30 days after the end of the trial.
Sample size calculation
The stratification factors will be gastrectomy and colorectal resection, with each layer being divided into three groups: the group ratio will be 1:1:1. The main efficacy indicator will be the GI-2 (composite outcome of time to first postoperative defaecation and time to tolerance of a solid diet). Given the lack of reports on TEAS+EA for promoting postoperative recovery, we conducted a preliminary experiment. The preliminary experimental results indicated that the GI-2 of laparotomy gastrectomy surgery in the control, EA and TEAS+EA groups was 113.1±37.5 hours, 86.9±36.1 hours and 80.1±33.2 hours, respectively, Additionally, in the control group, the GI-2 of laparotomy colorectal surgery in the control, EA and TEAS+EA groups was 106.2±35.9 hours, 85.6±33.1 hours and 78.5±36.3 hours, respectively. The sample size was determined using PASS V.11 with α=0.05 (two sided) and β=0.1 (90% power). The required sample size will be 60 patients per group. Assuming that 20% of patients will be lost to follow-up, we chose a sample size of 80 participants for each group, with a total sample size of 480 participants.
Statistical analysis
Statistical analysis will be conducted by independent third-party professional statisticians. All data will be collected by efficacy evaluators. Data analysis will be performed using the intention processing principle in SPSS V.22.0. Statistical results will be reported using a two-sided test, with statistical significance being set at p< 0.05. Continuous variables will be expressed as: mean (SD), median (IQR) or minimum and maximum. For comparisons between treatment groups, analyses of variance will be used for normally distributed variables, and the Kruskal-Wallis H test will be used for non-normally distributed variables. Categorical variables will be expressed as numbers (%), and will be analysed via χ2 tests for between-group comparisons.
Patient and public involvement
Patients and/or the public were not involved in study design or conduct of the study. The present trial was developed by acupuncturists based on previous clinical experience and literature. The expected outcomes are commonly used to assess rapid postoperative recovery in clinical practice. The cost of interventions and outcome measurements will be maintained using the study funding; therefore, it was not considered a significant burden and met the patient preferences. The results will be disseminated to the participants via the WCHSU website.
Discussion
Several studies have demonstrated the efficacy of acupuncture in rapid postoperative rehabilitation.39 Previous clinical experience and studies have shown that acupuncture on the distal limb acupoints is mostly selected for rehabilitation after abdominal surgery, which may be associated with several factors, including the presence of surgical wounds after abdominal surgery, postoperative changes in the structure and state of abdominal organs affecting acupuncture needle manipulation and safety. However, recent studies have shown that abdominal and limb acupoints facilitate improvement of abdominal pain and the distension degree; moreover, abdominal acupoints have a more optimal effect on improving the degree of abdominal pain.40 In this study, based on extensive clinical practice, TEAS will be applied to abdominal acupoints, which is safer than EA based on acupuncture on the meridians of the distal extremities; moreover, the SP15 and ST21 chosen for abdominal surgery are unconventional incision positions that facilitate manipulation. Additionally, they are both antiemetic, promote gastrointestinal motility and relieve abdominal pain. Some previous studies on acupuncture for gastrointestinal symptoms have shown that SA although have some placebo effect, but EA might have greater benefits than SA(Sham-acupuncture),15 41 42 so we did not include sham control in this study. Therefore, the main purpose of this three-arm randomised controlled study is to evaluate whether TEAS combined with EA therapy is effective at allowing rapid recovery after laparotomy for gastrointestinal surgery is more effective and beneficial, and further improving patient satisfaction.
Ethics and dissemination
Personal information and study data of all participants will be recorded in case report forms. Moreover, data involving patient privacy will be anonymised, protected by code and securely kept in a locked cabinet in the WCHSU accessed only by the research team. On completion of the trial and data verification, the case report forms will be transferred to the Science and Technology Department of Sichuan Province for safe archival purposes for 10 years before being destroyed. Data for use or analysis following study completion will be available from the corresponding author on reasonable request. The study results will be presented at national and international scientific conferences and submitted for publication in a peer-reviewed journal.
This study has been approved by the Ethics Committee on Biomedical Research, WCHSU in April 2021. The approval number is 2021 (52). The trial protocol strictly adheres to the principles of the latest Declaration of Helsinki. Patient consent for publication is not required.
Supplementary Material
Footnotes
HL and QW contributed equally.
Contributors: HL and QW contributed equally to this article, participated in the study design, drafted the manuscript and recruited patients. LL and YZ are responsible for the treatment of patients. HH and YH are responsible for collecting the data. NL and XW are responsible for monitoring this study. All authors contributed to manuscript revision and have read and approved the submitted version.
Funding: This study will be supported by the Sichuan Science and Technology Program (grant number: 2021YFS0254).
Disclaimer: The funding bodies are not involved in study design, data collection, analysis, interpretation of results, and the manuscript.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s)
References
- 1.Leslie JB, Viscusi ER, Pergolizzi JV, et al. Anesthetic Routines: the anesthesiologist's role in Gi recovery and postoperative ileus. Adv Prev Med 2011;2011:1–10. 10.4061/2011/976904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gan TJ, Belani KG, Bergese S, et al. Fourth consensus guidelines for the management of postoperative nausea and vomiting. Anesth Analg 2020;131:411–48. 10.1213/ANE.0000000000004833 [DOI] [PubMed] [Google Scholar]
- 3.Bragg D, El-Sharkawy AM, Psaltis E, et al. Postoperative ileus: recent developments in pathophysiology and management. Clin Nutr 2015;34:367–76. 10.1016/j.clnu.2015.01.016 [DOI] [PubMed] [Google Scholar]
- 4.Ni C-Y, Wang Z-H, Huang Z-P, et al. Early enforced mobilization after liver resection: a prospective randomized controlled trial. Int J Surg 2018;54:254–8. 10.1016/j.ijsu.2018.04.060 [DOI] [PubMed] [Google Scholar]
- 5.Ren QP, Luo Y-L, Xiao FM, et al. Effect of enhanced recovery after surgery program on patient-reported outcomes and function recovery in patients undergoing liver resection for hepatocellular carcinoma. Medicine 2020;99:e20062. 10.1097/MD.0000000000020062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harryman C, Plymale MA, Stearns E, et al. Enhanced value with implementation of an eras protocol for ventral hernia repair. Surg Endosc 2020;34:3949–55. 10.1007/s00464-019-07166-2 [DOI] [PubMed] [Google Scholar]
- 7.Medbery RL, Fernandez FG, Khullar OV. Eras and patient reported outcomes in thoracic surgery: a review of current data. J Thorac Dis 2019;11:S976–86. 10.21037/jtd.2019.04.08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Noba L, Rodgers S, Chandler C, et al. Enhanced recovery after surgery (ERAS) reduces hospital costs and improve clinical outcomes in liver surgery: a systematic review and meta-analysis. J Gastrointest Surg 2020;24:918–32. 10.1007/s11605-019-04499-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ljungqvist O, Scott M, Fearon KC. Enhanced recovery after surgery: a review. JAMA Surg 2017;152:292–8. 10.1001/jamasurg.2016.4952 [DOI] [PubMed] [Google Scholar]
- 10.Wilmore DW, Kehlet H. Management of patients in fast track surgery. BMJ 2001;322:473–6. 10.1136/bmj.322.7284.473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McLeod RS, Aarts M-A, Chung F, et al. Development of an enhanced recovery after surgery guideline and implementation strategy based on the Knowledge-to-action cycle. Ann Surg 2015;262:1016–25. 10.1097/SLA.0000000000001067 [DOI] [PubMed] [Google Scholar]
- 12.Prabhakaran S, Misra S, Magila M, et al. Randomized controlled trial comparing the outcomes of enhanced recovery after surgery and standard recovery pathways in laparoscopic sleeve gastrectomy. Obes Surg 2020;30:3273–9. 10.1007/s11695-020-04585-2 [DOI] [PubMed] [Google Scholar]
- 13.Miedema BW, Johnson JO. Methods for decreasing postoperative gut dysmotility. Lancet Oncol 2003;4:365–72. 10.1016/S1470-2045(03)01118-5 [DOI] [PubMed] [Google Scholar]
- 14.Li H, He T, Xu Q, et al. Acupuncture and regulation of gastrointestinal function. World J Gastroenterol 2015;21:8304–13. 10.3748/wjg.v21.i27.8304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ng SSM, Leung WW, Mak TWC, et al. Electroacupuncture reduces duration of postoperative ileus after laparoscopic surgery for colorectal cancer. Gastroenterology 2013;144:307–13. 10.1053/j.gastro.2012.10.050 [DOI] [PubMed] [Google Scholar]
- 16.Takahashi T. Mechanism of acupuncture on neuromodulation in the Gut-A review. Neuromodulation: Technology at the Neural Interface 2011;14:8–12. 10.1111/j.1525-1403.2010.00295.x [DOI] [PubMed] [Google Scholar]
- 17.Tada H, Fujita M, Harris M, et al. Neural mechanism of acupuncture-induced gastric relaxations in rats. Dig Dis Sci 2003;48:59–68. 10.1023/A:1021730314068 [DOI] [PubMed] [Google Scholar]
- 18.Yang N-N, Ye Y, Tian Z-X, et al. Effects of electroacupuncture on the intestinal motility and local inflammation are modulated by acupoint selection and stimulation frequency in postoperative ileus mice. Neurogastroenterol Motil 2020;32:e13808. 10.1111/nmo.13808 [DOI] [PubMed] [Google Scholar]
- 19.Ma J, Wang Y, Fan D. Clinical study of Acupoint catgut embedding in the treatment of chronic functional constipation. Journal of Sichuan of Traditional Chinese Medicine 2015;33:161–2. [Google Scholar]
- 20.S J-hua. Clinical observation of acupuncture plus flash cupping for gastroparesis in senile type 2 diabetes. Shanghai J Acu-mox 2018;37:1132–5. [Google Scholar]
- 21.Zhang W-B, Wu A, Litscher G, et al. Effects and mechanism of acupuncture based on the principle of meridians. Evid Based Complement Alternat Med 2013;2013:1–2. 10.1155/2013/684027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhao Z-Q. Neural mechanism underlying acupuncture analgesia. Prog Neurobiol 2008;85:355–75. 10.1016/j.pneurobio.2008.05.004 [DOI] [PubMed] [Google Scholar]
- 23.Hauck M, Schröder S, Meyer-Hamme G, et al. Acupuncture analgesia involves modulation of pain-induced gamma oscillations and cortical network connectivity. Sci Rep 2017;7:16307. 10.1038/s41598-017-13633-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cui X, Liu K, Xu D, et al. Mast cell deficiency attenuates acupuncture analgesia for mechanical pain using c-kit gene mutant rats. J Pain Res 2018;11:483–95. 10.2147/JPR.S152015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wu M-S, Chen K-H, Chen I-F, et al. The efficacy of acupuncture in post-operative pain management: a systematic review and meta-analysis. PLoS One 2016;11:e0150367. 10.1371/journal.pone.0150367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Capodice JL, Parkhomenko E, Tran TY, et al. A randomized, double-blind, sham-controlled study assessing electroacupuncture for the management of postoperative pain after percutaneous nephrolithotomy. J Endourol 2019;33:194–200. 10.1089/end.2018.0665 [DOI] [PubMed] [Google Scholar]
- 27.Chen C-C, Yang C-C, Hu C-C, et al. Acupuncture for pain relief after total knee arthroplasty: a randomized controlled trial. Reg Anesth Pain Med 2015;40:31–6. 10.1097/AAP.0000000000000138 [DOI] [PubMed] [Google Scholar]
- 28.Asmussen S, Maybauer DM, Chen JD, et al. Effects of acupuncture in anesthesia for craniotomy: a meta-analysis. J Neurosurg Anesthesiol 2017;29:219–27. 10.1097/ANA.0000000000000290 [DOI] [PubMed] [Google Scholar]
- 29.Mitra S, Carlyle D, Kodumudi G, et al. New advances in acute postoperative pain management. Curr Pain Headache Rep 2018;22:35. 10.1007/s11916-018-0690-8 [DOI] [PubMed] [Google Scholar]
- 30.Kovac AL. Update on the management of postoperative nausea and vomiting. Drugs 2013;73:1525–47. 10.1007/s40265-013-0110-7 [DOI] [PubMed] [Google Scholar]
- 31.Lee A, Chan SKC, Fan LTY. Stimulation of the wrist acupuncture point PC6 for preventing postoperative nausea and vomiting. Cochrane Database Syst Rev 2015;2015:Cd003281. 10.1002/14651858.CD003281.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim YH, Kim KS, Lee HJ, et al. The efficacy of several neuromuscular monitoring modes at the p6 acupuncture point in preventing postoperative nausea and vomiting. Anesth Analg 2011;112:819–23. 10.1213/ANE.0b013e31820f819e [DOI] [PubMed] [Google Scholar]
- 33.Gan TJ, Jiao KR, Zenn M, et al. A randomized controlled comparison of electro-acupoint stimulation or ondansetron versus placebo for the prevention of postoperative nausea and vomiting. Anesth Analg 2004;99:1070–5. 10.1213/01.ANE.0000130355.91214.9E [DOI] [PubMed] [Google Scholar]
- 34.Chen K-B, Huang Y, Jin X-L, et al. Electroacupuncture or transcutaneous electroacupuncture for postoperative ileus after abdominal surgery: a systematic review and meta-analysis. Int J Surg 2019;70:93–101. 10.1016/j.ijsu.2019.08.034 [DOI] [PubMed] [Google Scholar]
- 35.Chen J, Zhang Y, Li X, et al. Efficacy of transcutaneous electrical acupoint stimulation combined with general anesthesia for sedation and postoperative analgesia in minimally invasive lung cancer surgery: a randomized, double-blind, placebo-controlled trial. Thorac Cancer 2020;11:928–34. 10.1111/1759-7714.13343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hou L, Xu L, Shi Y, et al. Effect of electric acupoint stimulation on gastrointestinal hormonesand motility among geriatric postoperative patients with gastrointestinaltumors. J Tradit Chin Med 2016;36:450–5. 10.1016/s0254-6272(16)30061-9 [DOI] [PubMed] [Google Scholar]
- 37.Sun K, Xing T, Zhang F, et al. Perioperative transcutaneous electrical Acupoint stimulation for postoperative pain relief following laparoscopic surgery: a randomized controlled trial. Clin J Pain 2017;33:340–7. 10.1097/AJP.0000000000000400 [DOI] [PubMed] [Google Scholar]
- 38.Committee CNSA, Committee CISM . National standard of the people’s Republic of China “Nomenclature and Location of Acupuncture Points”(GB / T 12346-2006. Beijing: China Standards Press, 2006. [Google Scholar]
- 39.Xin C, Sun J-H. [The value of acupuncture-moxibustion in enhance recovery after surgery]. Zhongguo Zhen Jiu 2020;40:679–82. 10.13703/j.0255-2930.20190501-0005 [DOI] [PubMed] [Google Scholar]
- 40.Li H-J, Zhao Y, Wen Q, et al. [Comparison of Clinical Effects of Electroacupuncture of Abdominal and Limb Acupoints in the Treatment of Acute Pancreatitis]. Zhen Ci Yan Jiu 2018;43:725–9. 10.13702/j.1000-0607.170351 [DOI] [PubMed] [Google Scholar]
- 41.Liu Z, Yan S, Wu J, et al. Acupuncture for chronic severe functional constipation: a randomized trial. Ann Intern Med 2016;165:761–9. 10.7326/M15-3118 [DOI] [PubMed] [Google Scholar]
- 42.Wang C-P, Kao C-H, Chen W-K, et al. A single-blinded, randomized pilot study evaluating effects of electroacupuncture in diabetic patients with symptoms suggestive of gastroparesis. J Altern Complement Med 2008;14:833–9. 10.1089/acm.2008.0107 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.