Abstract
Objectives
To evaluate the association between immigration status and all-cause mortality in different disease cohorts, and the impact of loss to follow-up on the observed associations.
Design
Population-based retrospective cohort study using linked administrative health data in Ontario, Canada.
Setting
We followed adults with a first-ever diagnosis of ischaemic stroke, cancer or schizophrenia between 2002 and 2013 from index event to death, loss to follow-up, or end of follow-up in 2018.
Primary and secondary outcome measures
Our outcomes of interest were all-cause mortality and loss to follow-up. For each disease cohort, we calculated adjusted HRs of death in immigrants compared with long-term residents, adjusting for demographic characteristics and comorbidities, with and without censoring for those who were lost to follow-up. We calculated the ratio of two the HRs and the respective CL using bootstrapping methods.
Results
Immigrants were more likely to be lost to follow-up than long-term residents in all disease cohorts. Not accounting for this loss to follow-up overestimated the magnitude of the association between immigration status and mortality in those with ischaemic stroke (HR of death before vs after accounting for censoring: 0.78 vs 0.83, ratio=0.95; 95% CL 0.93 to 0.97), cancer (0.74 vs 0.78, ratio=0.96; 0.95 to 0.96), and schizophrenia (0.54 vs 0.56, ratio=0.97; 0.96 to 0.98).
Conclusions
Immigrants to Canada have a survival advantage that varies by the disease studied. The magnitude of this advantage is modestly overestimated by not accounting for the higher loss to follow-up in immigrants.
Keywords: epidemiology, social medicine, public health
Strengths and limitations of this study.
This is the first study in Canada to compare the rates of loss to follow-up in a population-based sample of immigrants and long-term residents with stroke, cancer or schizophrenia.
Using appropriate statistical analyses, we compared the hazard of mortality, adjusted for confounders, between immigrants and long-term residents with and without accounting for loss to follow-up.
Loss to follow-up was determined using administrative data definitions which may not be complete.
Long-term residents consisted of Canadian born and those who migrated before 1985, limiting generalisability of the findings to all immigrants.
Introduction
Studies from high-income countries, including Canada, have shown that immigrants have a lower mortality compared with host populations.1–3 This immigrant health advantage has been observed not only for all-cause mortality, but also for cardiovascular4 and cancer mortality,5 and for the incidence of non-communicable chronic conditions such as cardiovascular disease,6 cancer7 and schizophrenia.8
This phenomenon has been termed the healthy immigrant effect, and is partly attributed to a selection bias whereby only those who are healthy and have human capital are able to migrate.9 10 However, another potential explanation for the observed immigrant health advantage is a phenomenon termed the salmon effect, whereby immigrants return to their home countries when they are gravely ill.11 Thus, they are lost to follow-up and not accounted for in studies that rely on mortality statistics that do not record emigration.12 Such lack of complete follow-up was identified in a large-scale meta-analysis on immigrant mortality in which none of the included 96 studies accounted for loss to follow-up and only 29 (28%) studies identified loss to follow-up as an issue.13 Previous work in both observational studies and randomised controlled trials has shown that unbalanced loss to follow-up in two comparison groups can lead to biased estimates of association.14 15
The aims of this study were to use linked population-based data from Ontario, Canada to evaluate the association between immigration status and all-cause mortality after a new diagnosis of ischaemic stroke, cancer, or schizophrenia, to quantify loss to follow-up in immigrants compared with long-term residents, and to determine how accounting for loss to follow-up influences the association between immigration status and all-cause mortality in each disease cohort.
Methods
Patient and public involvement statement
Patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research
Setting and population
Ontario is Canada’s most populous province, with an estimated population of 14 million.16 In 2016, approximately 3.8 million immigrants were living in Ontario, accounting for about 30% of the total population.17 All residents of Ontario (except for undocumented migrants and those visiting) are covered by the provincial health plan that includes physician services, hospital and emergency care, and investigations ordered by physicians. The linked administrative databases in Ontario capture all healthcare system contacts of insured Ontario residents.
We created three separate incident disease cohorts of ischaemic stroke, primary cancer and schizophrenia using validated case definitions for incidence during an ascertainment period of 1 April 2002 to 31 March 2012 (online supplemental e-table 1). We focused on these three diseases because they are chronic conditions associated with high morbidity that require regular healthcare system contact (which is captured in administrative databases) following the diagnosis, and because management of these conditions may benefit from family and social supports, which can be a factor in emigration. We identified patients with ischaemic stroke using the Ontario Stroke Registry which is a province-wide registry that includes data on a random sample of consecutive patients seen at over 150 hospitals in Ontario.18 Data collection for the registry was performed by chart abstractors with neurological expertise, with the final diagnosis and other data elements obtained through review of clinical and neuroimaging data. We identified patients with a diagnosis of a primary malignant cancer from the Ontario Cancer Registry, a population-based registry, which is created by combining information from discharge and day surgery summaries, pathology reports with any mention of cancer, or records of patients referred to specialised institutions treating patients with cancer in Ontario.19 It captures approximately 95% of all cancer diagnoses in the province.19 We identified patients with schizophrenia based on a validated algorithm whereby a diagnosis of schizophrenia was made if the patient had one or more hospital admissions and/or three or more outpatient visits with a diagnosis of schizophrenia or schizoaffective disorder.20
bmjopen-2020-046377supp001.pdf (1.3MB, pdf)
Within each disease cohort, we excluded prevalent cases if they had a diagnosis of the specific disease prior to 1 April 2002. If patients had multiple cohort-defining events during the ascertainment period, only information at the time of the first cohort-defining event was recorded. We excluded patients who were younger than 18 years or older than 104 years at the time of the index event, those who resided in long-term care homes at the time of the index event, and those who resided in rural areas (population <10 000) because most immigrants (>95%) reside in large urban areas.
Using unique identifiers, we linked these cohorts to population-based data held securely at ICES (formerly known as the Institute for Clinical Evaluative Sciences), Toronto. ICES is a prescribed entity under the Ministry of Health and Long-Term Care where Ontario’s public health services data sets are stored, linked and used for research. We obtained information on neighbourhood-level income (in quintiles) based on the postal-code files, and on previous diagnoses of hypertension,21 diabetes,22 chronic obstructive pulmonary disease (COPD),23 congestive heart failure (CHF)24 and atrial fibrillation25 using validated case definitions (online supplemental e-table 1).
Exposure and outcomes
Our exposure of interest was immigration status obtained from the Ministry of Immigration, Refugee and Citizenship (IRCC) Permanent Resident Database which collected information on all immigrants who arrived in Ontario after 1985. As information on immigration status was only available after 1985, we classified individuals born outside of Canada who arrived in Ontario after 1985 as immigrants, and those born in Canada or those who were born outside of Canada but arrived before 1985 as long-term residents.
Our primary outcome was death from any cause, which was obtained from the death registry along with the date of death. We set the end date of follow-up as 31 March 2018.
We determined each person’s date of last contact with the health system by using administrative databases to identify any contact with healthcare system such as a visit to a doctor’s office, refill of prescriptions (in those over 65 years), hospitalisation or emergency visits, receipt of home care, or admission to a rehabilitation facility (online supplemental e-table 2) until 31 January 2020, the latest date for which information from the administrative databases was available. The healthcare system contact could be for any reason, and not pertaining to the index diagnosis alone. Those who were not recorded as dying prior to 31 March 2018 (end date of follow-up), and who had their last health system contact prior to this date were flagged as lost to follow-up at the date of last health system contact (online supplemental e-figure 1).
Statistical analyses
Analyses were conducted separately in each disease cohort. We compared baseline characteristics between immigrants and long-term residents within each disease cohort using the χ2 test for categorical variables and the Wilcoxon rank sum test for continuous variables.
We used the time of the index diagnosis as time zero. We estimated unadjusted cumulative incidence functions for death and loss to follow-up in immigrants and long-term residents, separately. We developed multivariable cause-specific hazards models to estimate the adjusted HR of loss to follow-up in immigrants compared with long-term residents accounting for death as a competing event, and adjusting for age, sex, neighbourhood-level income, hypertension, diabetes, COPD, CHF and atrial fibrillation.
We then fit two multivariable Cox proportional hazards models to estimate the adjusted HR of death in immigrants compared with long-term residents, adjusting for demographic information and chronic conditions as before. In the first model, which did not account for loss to follow-up, we censored individuals only on 31 March 2018. In the second model, which accounted for loss to follow-up, we censored individuals on the first of either 31 March 2018, or the date of last health system contact.
We then calculated a ratio of the two adjusted HRs obtained from these two models and calculated 95% CLs around this ratio using percentile-based bootstrapping methods and 1000 bootstrap samples. If the CLs for the ratio included 1, it would suggest that there is no statistical difference between the adjusted HRs obtained with and without accounting for loss to follow-up. The direction and magnitude of the difference between two HRs can be inferred based on the ratio, with values under 1 suggesting overestimation of the association between immigration status and mortality when not accounting for loss to follow-up. We similarly obtained adjusted HRs of death for each covariate in the multivariable models using two separate models, with and without accounting for loss to follow-up. Using the methods described above, we also evaluated whether the association between other covariates and mortality changed after accounting for loss to follow-up. All analyses were conducted using SAS V.9.4 Copyright 2002–2012 by SAS Institute.
Sensitivity analyses
We redefined the date of last healthcare system contact as the recorded date plus 180 days to account for patients who may not interact with healthcare system for up to 6 months (online supplemental e-figure 2) and then recalculated the adjusted hazard of death accounting for loss to follow-up for each disease cohort. We chose a lag-time of 6 months because all patients in this study had a chronic condition that would typically require follow-up within this time frame.
To evaluate how the association between immigration status and mortality would change if those lost to follow-up had died, we recalculated the adjusted hazard of death in immigrants compared with long-term residents in two hypothetical scenarios in which patients, irrespective of their immigration status, were considered to have died at 30 days or 1 year following their last recorded health system contact.
Results
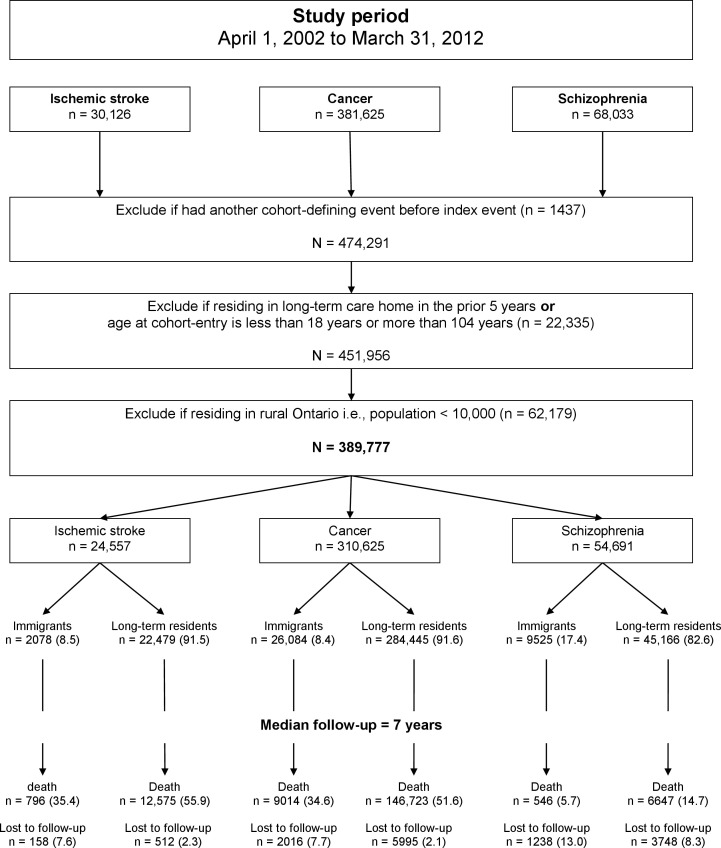
The total study sample included 389 777 people (9.7% immigrants). Of these, 24 557 had ischaemic stroke, 310 529 had cancer and 54 691 had schizophrenia (figure 1). A greater proportion of patients with schizophrenia were immigrants (17.4%) compared with those with ischaemic stroke (8.5%) or cancer (8.4%) (table 1). Irrespective of the underlying diagnosis, immigrants were younger at the time of the diagnosis and more likely to reside in a low-income neighbourhood compared with long-term residents (table 1). Other characteristics of the study cohorts are shown in table 1 and online supplemental e-table 3.
Figure 1.
Cohort selection and follow-up. Footnote: values in parenthesis represent proportion.
Table 1.
Baseline characteristics in immigrants and long-term residents with a first-ever diagnosis of ischaemic stroke, cancer or schizophrenia between 2002 and 2012 in Ontario, Canada
| Ischaemic stroke | Cancer | Schizophrenia | ||||
| Immigrants | Long-term residents | Immigrants | Long-term residents | Immigrants | Long-term residents | |
| 2078 (8.5) | 22 479 (91.5) | 26 084 (8.4) | 284 445 (91.6) | 9525 (17.4) | 45 166 (82.6) | |
| Female, n (%) | 982 (47.3) | 10 697 (47.6) | 13 602 (52.1) | 130 324 (45.8) | 4346 (45.6) | 19 943 (44.2) |
| Median age in years at index event (Q1–Q3) | 68 (55–78) | 74 (63–82) | 58 (48–70) | 67 (58–76) | 34 (25–45) | 40 (26–53) |
| Neighbourhood-level income, n (%) | ||||||
| Lowest quintile (first) | 668 (32.1) | 5043 (22.4) | 7041 (27.0) | 50 044 (17.6) | 3803 (39.9) | 13 525 (29.9) |
| Highest quintile (fifth) | 201 (9.7) | 4330 (19.3) | 3326 (12.8) | 62 667 (22.0) | 734 (7.7) | 6434 (14.2) |
| Hypertension, n (%) | 1420 (68.3) | 16 046 (71.4) | 11 120 (42.6) | 152 177 (53.5) | 1165 (12.2) | 8253 (18.3) |
| Diabetes, n (%) | 727 (35.0) | 6495 (28.9) | 4850 (18.6) | 53 444 (18.8) | 737 (7.7) | 4178 (9.3) |
| Congestive heart failure, n (%) | 258 (12.4) | 3728 (16.6) | 878 (3.4) | 20 721 (7.3) | 59 (0.6) | 807 (1.8) |
| COPD, n (%) | 111 (5.3) | 2547 (11.3) | 1023 (3.9) | 31 745 (11.2) | 60 (0.6) | 1494 (3.3) |
| Atrial fibrillation, n (%) | 243 (11.7) | 3786 (16.8) | 777 (3.0) | 19 278 (6.8) | 34 (0.4) | 525 (1.2) |
COPD, chronic obstructive pulmonary disease.
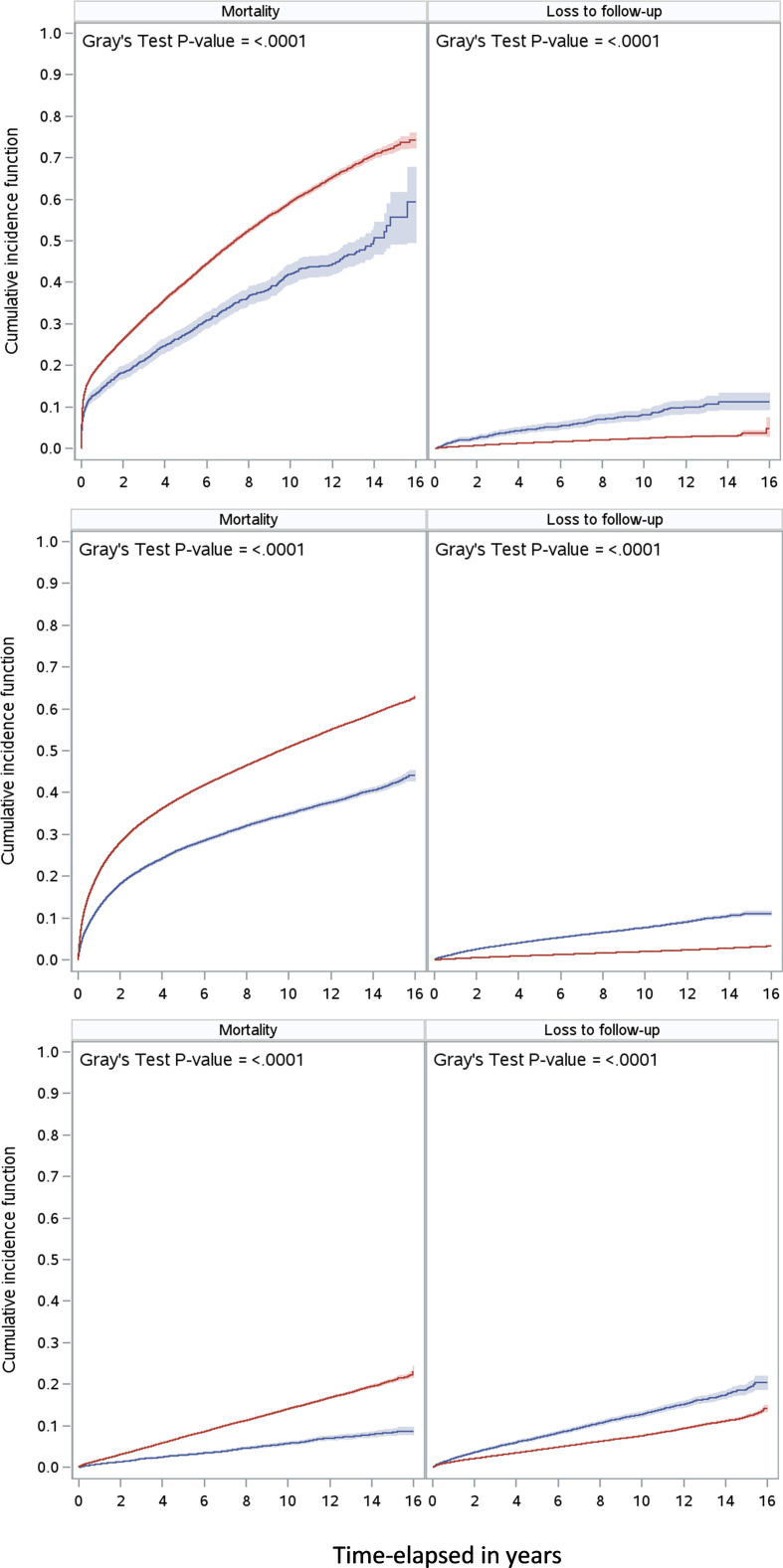
During a median follow-up of 7 years, 13 667 people (3.5%) were lost to follow-up across the three disease cohorts. A greater proportion of patients with schizophrenia were lost to follow-up (9.1%) than patients with ischaemic stroke (2.7%) or cancer (2.6%) (table 2). Immigrants were more likely than long-term residents to be lost to follow-up in all disease cohorts (table 2 and figure 2); however, the magnitude of association between immigration status and loss to follow-up was greater in patients with ischaemic stroke (HR 2.87; 95% CI 2.38 to 3.44) and cancer (HR 3.07; 95% CI 2.91 to 3.23) than schizophrenia (HR 1.54; 95% CI 1.44 to 1.64; table 2).
Table 2.
Loss to follow-up and mortality in immigrants and long-term residents in Ontario, Canada
| Ischaemic stroke | Cancer | Schizophrenia | ||||
| Immigrants | Long-term residents | Immigrants | Long-term residents | Immigrants | Long-term residents | |
| N (%) | 2078 (8.5) | 22 479 (91.5) | 26 084 (8.4) | 284 445 (91.6) | 9525 (17.4) | 45 166 (82.6) |
| Loss to follow-up, n (%) | 158 (7.6) | 512 (2.3) | 2016 (7.7) | 5995 (2.1) | 1238 (13.0) | 3748 (8.3) |
| Adjusted HR of loss to follow-up (95% CI)* accounting for the competing risk of death | 2.87 (2.38 to 3.44) | 1.00 | 3.07 (2.91 to 3.23) | 1.00 | 1.54 (1.44 to 1.64) | 1.00 |
| Death, n (%) | 796 (35.4) | 12 575 (55.9) | 9014 (34.6) | 146 723 (51.6) | 546 (5.7) | 6647 (14.7) |
| Unadjusted HR of death (95% CI) | 0.61 (0.56 to 0.65) | 1.00 | 0.60 (0.59 to 0.62) | 1.00 | 0.39 (0.35 to 0.42) | 1.00 |
| Adjusted HR* (95% CI) not accounting for loss to follow-up | 0.78 (0.73 to 0.84) | 1.00 | 0.74 (0.73 to 0.76) | 1.00 | 0.54 (0.50 to 0.59) | 1.00 |
| Adjusted HR* (95% CI) accounting for loss to follow-up | 0.83 (0.77 to 0.89) | 1.00 | 0.78 (0.76 to 0.79) | 1.00 | 0.56 (0.51 to 0.61) | 1.00 |
| Sensitivity analyses‡ | ||||||
| Death within 30 days of loss to follow-up Adjusted HR (95% CI) |
0.93 (0.87 to 1.00) | 1.00 | 0.90 (0.88 to 0.91) | 1.00 | 1.00 (0.95 to 1.05) | 1.00 |
| Death within 1 year of loss to follow-up Adjusted HR (95% CI) |
0.93 (0.87 to 0.99) | 1.00 | 0.89 (0.87 to 0.91) | 1.00 | 1.00 (0.95 to 1.06) | 1.00 |
*Multivariable model adjusting for the following: age, sex, neighbourhood-level income, and comorbidities (known hypertension, diabetes, congestive heart failure, chronic obstructive pulmonary disease, and atrial fibrillation).
†Censoring those who were lost to follow-up, which was determined when date of last health system contact occurred before end of follow-up among those alive.
‡Assigning date of death among those lost to follow-up and recalculating adjusted hazard of death.
Figure 2.
Unadjusted cumulative incidence functions in immigrants (blue) and long-term residents (red) showing probabilty of death and of loss to follow-up in patients with ischaemic stroke (top), cancer (middle) and schizophrenia (bottom).
During 2.7 million person years of follow-up, 176 301 deaths were recorded across the three disease cohorts. The crude mortality rate was highest in patients who had an ischaemic stroke (95.3 per 1000 person years) followed by cancer (76.8 per 1000 person year) and schizophrenia (13.7 per 1000 person years). In all three disease cohorts, the unadjusted hazard of mortality was lower in immigrants compared with long-term residents (table 2 and figure 2). This remained true even after adjusting for baseline differences in age, comorbidity and area-level socioeconomic status, with an adjusted HR of death in immigrants compared with long-term residents of 0.78 (95% CI 0.73 to 0.84) in patients who had an ischaemic stroke, an HR of 0.74 (95% CI 0.73 to 0.76) in patients with cancer, and an HR of 0.54 (95% CI 0.50 to 0.59) in patients with schizophrenia (table 2). The magnitude of the mortality advantage in immigrants compared with long-term residents attenuated after accounting for loss to follow-up, with adjusted HR of death in immigrants compared with long-term residents of 0.83 (95% CI 0.77 to 0.89) for ischaemic stroke, 0.78 (95% CI 0.76 to 0.79) for cancer, and 0.56 (95% CI 0.51 to 0.61) for schizophrenia (table 2).
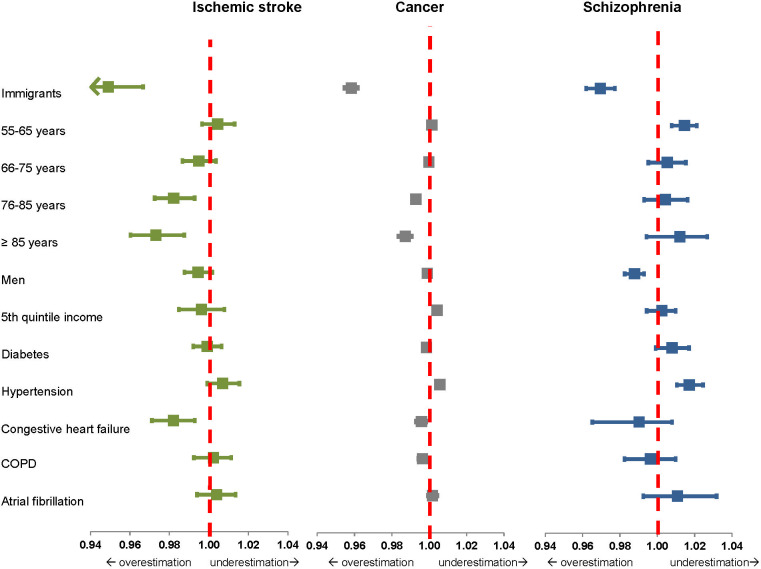
The ratio of the two adjusted HRs obtained using models with and without accounting for loss to follow-up was 0.95 (95% CL 0.93 to 0.97) for ischaemic stroke, 0.96 (95% CL 0.95 to 0.96) for cancer and 0.97 (95% CL 0.96 to 0.98) for schizophrenia, suggesting that not accounting for loss to follow-up overestimated the mortality advantage in immigrants in all cohorts (figure 3). This is equivalent to a relative change in the HR of death (in immigrants vs long-term residents) of 5% for ischaemic stroke, 4% for cancer and 3% for schizophrenia. The effect of not accounting for loss to follow-up on the association between other covariates and mortality is shown in figure 3.
Figure 3.
Ratios of adjusted HRs of death obtained using two multivariable cox-regression models with and without accounting for loss to follow-up. Each box represents the point estimate of this ratio, and the error bars represent 95% CLs. Values less than 1 suggest overestimation of the magnitude of association when loss to follow-up is not accounted for. Footnote: immigrants are compared with long-term residents; age less than 55 years is the comparison group; and the fifth quintile of income represent the HR of death in the highest quintile compared with lowest quintile based on neighbourhood-level income. COPD, chronic obstructive pulmonary disease.
Sensitivity analyses
Using a lag time of 6 months in determining the date of last healthcare system contact, to account for patients who have less frequent contact with the healthcare system, did not alter the association between immigration status and mortality for any disease cohort (online supplemental e-table 4).
In hypothetical scenarios in which, irrespective of immigration status, patients lost to follow-up were considered to be dead at 30 days and 1 year after loss to follow-up, the healthy immigrant advantage was eliminated in patients with schizophrenia and attenuated in patients who had an ischaemic stroke and cancer (table 2).
Discussion
In this study using linked population-based data on over 380 000 patients with a new diagnosis of ischaemic stroke, cancer and schizophrenia, we demonstrated that immigrants have a survival advantage but are also more likely to be lost to follow-up compared with long-term residents, with variations in the magnitude of both the mortality advantage and the proportion lost to follow-up across the disease groups studied. Not accounting for loss to follow-up overestimated the immigrant health advantage.
Our finding of lower mortality in immigrants compared with long-term residents who had a stroke, cancer and schizophrenia is consistent with previous studies, including a large-scale meta-analysis of over 15.2 million immigrants across 92 countries.13 Potential explanations for lower mortality in immigrants include self-selection of immigrants based on health prior to migration,26 a healthier lifestyle in immigrants27 and return migration.28 We found that immigrants with schizophrenia had the greatest mortality advantage compared with those who had an ischaemic stroke or cancer. Possible explanations include the relatively younger age of immigrants and long-term residents with schizophrenia, variations in disease-specific healthcare provision in immigrants compared with long-term residents,29 30 or other unmeasured confounders. While certain immigrant subgroups such as refugees or asylum seekers may be at increased risk of poor mental health outcomes31 and mortality,32 the magnitude of the mortality advantage in immigrants with schizophrenia observed in our study is consistent with previous reports of lower suicide rates in immigrants compared with long-term residents across different ethnic groups in the USA33 and in Canadian youth.34
In our study, loss to follow-up could be explained by either emigration from the province or by failure to access the healthcare system while remaining in the province. Since the medical conditions included in our cohorts typically require ongoing care, it is likely that emigration rather than failure to access the healthcare system accounts for the majority of the loss to follow-up in our study. Although our study does not provide information on the ultimate destination of those emigrating, return to a home country and family supports at the end of life (the so-called salmon effect) has been described in immigrants with chronic conditions with physical healthcare needs such as ischaemic stroke or cancer.35 36 In contrast, those with schizophrenia may have less contact with the healthcare system because of their relatively young age or because of challenges in access related to mental illness, and may be less likely to return to their home country because of stigma related to mental health diagnoses in some countries of origin.37 38 Our study did not allow us to determine whether loss to follow-up varied with disease severity, and previous studies have yielded inconsistent findings. For example, higher comorbidity in Denmark was associated with lower rates of emigration in immigrants whereas self-reported poor health in the USA was associated with higher rates of emigration in Mexican immigrants.39 40
Because immigration status was directly related to the censoring event, loss to follow-up, we found that accounting for loss to follow-up altered the magnitude of the association between immigration status and mortality. Thus, previous estimates of the mortality advantage in immigrants that have relied on death statistics alone and did not account for loss to follow-up may have overestimated the immigrant health advantage.3 12 41 Consistent with this, a study from England and Wales found that although there was an immigrant mortality advantage, the magnitude of the association between immigration status and mortality was lower in all three hypothetical scenarios of immigrants’ exits out of the country.42 We found that accounting for loss to follow-up did not change the magnitude of the association between mortality and other variables of interest included in the multivariable models, except for older age in the ischaemic stroke and cancer cohorts. This suggests that studies using administrative health data to evaluate the association between other covariates (sex, income or comorbidities) and mortality could yield adequate results even if they fail to account for loss to follow-up.
Our study is strengthened by the use of comprehensive administrative databases that allowed us to identify loss of health system contact in three separate chronic disease cohorts. The findings are likely to be generalisable to other jurisdictions with immigrant populations and to other disease conditions not included in this study, but the magnitude of bias may vary depending on the disease condition, healthcare jurisdiction, and immigrant-related variables (country of origin, time since immigration or immigration class).
Some limitations merit discussion. We were only able to define people as immigrants based on their immigration records, and because these were collected systematically only after 1985, immigrants who arrived prior to 1985 had to be classified as long-term residents. We did not have information on factors such as physical activity43 and smoking,44 or other chronic conditions that may be associated with mortality, and we did not have information specific to each disease condition such as disease severity, disability, response to treatment, or palliative care status, all of which could influence mortality. Because we only included people with a known medical condition, we are unable to comment on patterns of loss to follow-up in healthy immigrants and long-term residents. We used area-level income as a proxy for socioeconomic status, and recognise that this may not reflect individual level income or other measures of socioeconomic status such as wealth, education, or occupation. We also assumed that loss of health system contact equated to patients leaving the healthcare jurisdiction rather than reflecting an excellent recovery negating the need for ongoing medical management. However, the misclassification introduced by this assumption should not vary based on immigration status. In addition, we assumed that, at least in immigrants, loss to follow-up was likely to be due to emigration to their home countries rather than to other parts of Canada or onwards to other regions of the world. A study from the IRCC found that only 9% of immigrants who landed in Ontario between 1991 and 2006 had moved to other provinces by 2006.45 Lastly, movement of individuals in and out of a healthcare jurisdiction is a dynamic process, and those who emigrate can return. If such individuals return after the end date of follow-up, they could be falsely censored at the date of their emigration.
This study highlights the lower mortality in immigrants compared with long-term residents previously observed in other studies, but also demonstrates that inadequate handling of loss to follow-up can lead to biased estimates of the immigrant health advantage, as immigrant deaths may not be captured if immigrants return to their home region when gravely ill. Based on these findings, we recommend that future studies comparing mortality and other long-term outcomes in immigrants and non-immigrants carefully record loss to follow-up in both groups, quantify it, and account for it using appropriate methodology. When this information is not available, other measures could include use of updated postal code files during follow-up,46 measuring outcomes in the short term, or assuming specific rates of emigration based on previous reports. Future research could evaluate reasons for the variation in the magnitude of the association between immigration status and mortality based on the disease cohort, and evaluate the association between immigration-specific (immigration class, country of origin and time since immigration) and disease-specific (severity, palliative status and disease-related disability) factors and loss to follow-up.
Supplementary Material
Footnotes
Twitter: @moirakapral
Contributors: MV, JF and MKK were involved in the concept and design. MV, PA and JF were involved in data acquisition, and analysis. FS and MKK were involved in the primary data acquisition data for Ontario Stroke Registry. All authors were involved in developing the project and interpreting the results. MV was responsible for drafting the manuscript which was critically revised by everyone. MKK supervised the study and is the guarantor.
Funding: This study was funded from Heart and Stroke Foundation of Canada (HSFC GIA19-26333). MKK and PCA hold Mid-Career Investigator Awards from the Heart and Stroke Foundation of Canada. MKK holds the Lillian Love Chair in Women’s Health from the University Health Network/University of Toronto. MVV holds a Fellowship Award from the Canadian Institutes of Health Research.
Disclaimer: The study was supported by ICES (formerly the Institute for Clinical Evaluative Sciences), which is supported by an annual grant from the Ontario Ministry of Health and Long-Term Care. Data were made available with help from the Immigration, Refugees and Citizenship Canada. Parts of this material are based on data and/or information compiled and provided by the Canadian Institute for Health Information. The analyses, opinions, results and conclusions reported in this article are those of the authors and are independent from the funding sources. No endorsement by ICES, the Ontario Ministry of Health and Long-Term Care, Canadian Institute for Health Information, or the Immigration, Refugees and Citizenship Canada is intended or should be inferred.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. The data used in this study is held securely in coded form at ICES. Data sharing agreements prohibit ICES from making the dataset publicly available, but access may be granted to those who meet prespecified criteria for confidential access. Please contact corresponding author for details.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study was approved by Research Ethics Board at Sunnybrook Health Sciences Centre, Canada (ID: 158-2017).
References
- 1.Vang Z, Sigouin J, Flenon A. The healthy immigrant effect in Canada: a systematic review. Population Change and Lifecourse Strategic Knowledge Cluster Discussion Paper Series/Un Réseau stratégique de connaissances Changements de population et parcours de vie Document de travail 2015;3:Article 4. [Google Scholar]
- 2.Syse A, Dzamarija MT, Kumar BN, et al. An observational study of immigrant mortality differences in Norway by reason for migration, length of stay and characteristics of sending countries. BMC Public Health 2018;18:508. 10.1186/s12889-018-5435-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Omariba DWR, Ng E, Vissandjée B. Differences between immigrants at various durations of residence and host population in all-cause mortality, Canada 1991-2006. Popul Stud 2014;68:339–57. 10.1080/00324728.2014.915050 [DOI] [PubMed] [Google Scholar]
- 4.McKeigue PM, Marmot MG. Mortality from coronary heart disease in Asian communities in London. BMJ 1988;297:903. 10.1136/bmj.297.6653.903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheung MC, Earle CC, Fischer HD, et al. Impact of immigration status on cancer outcomes in Ontario, Canada. J Oncol Pract 2017;13:e602–12. 10.1200/JOP.2016.019497 [DOI] [PubMed] [Google Scholar]
- 6. Tu JV, Chu A, Donovan LR. The cardiovascular health in ambulatory care research team (CANHEART). Circulation 2015;8:204–12. [DOI] [PubMed] [Google Scholar]
- 7.Paszat L, Sutradhar R, Liu Y, et al. Risk of colorectal cancer among immigrants to Ontario, Canada. BMC Gastroenterol 2017;17:85. 10.1186/s12876-017-0642-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anderson KK, Cheng J, Susser E, et al. Incidence of psychotic disorders among first-generation immigrants and refugees in Ontario. CMAJ 2015;187:E279–86. 10.1503/cmaj.141420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marmot MG, Adelstein AM, Bulusu L. Lessons from the study of immigrant mortality. Lancet 1984;1:1455–7. 10.1016/S0140-6736(84)91943-3 [DOI] [PubMed] [Google Scholar]
- 10.McDonald JT, Kennedy S. Insights into the 'healthy immigrant effect': health status and health service use of immigrants to Canada. Soc Sci Med 2004;59:1613–27. 10.1016/j.socscimed.2004.02.004 [DOI] [PubMed] [Google Scholar]
- 11.Markides KS, Eschbach K. Aging, migration, and mortality: current status of research on the Hispanic paradox. J Gerontol B Psychol Sci Soc Sci 2005;60 Spec No 2:S68–75. 10.1093/geronb/60.Special_Issue_2.S68 [DOI] [PubMed] [Google Scholar]
- 12.Khan AM, Urquia M, Kornas K, et al. Socioeconomic gradients in all-cause, premature and avoidable mortality among immigrants and long-term residents using linked death records in Ontario, Canada. J Epidemiol Community Health 2017;71:625–32. 10.1136/jech-2016-208525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aldridge RW, Nellums LB, Bartlett S, et al. Global patterns of mortality in international migrants: a systematic review and meta-analysis. Lancet 2018;392:2553–66. 10.1016/S0140-6736(18)32781-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Akl EA, Briel M, You JJ, et al. Potential impact on estimated treatment effects of information lost to follow-up in randomised controlled trials (LOST-IT): systematic review. BMJ 2012;344:e2809. 10.1136/bmj.e2809 [DOI] [PubMed] [Google Scholar]
- 15.Greenland S. Response and follow-up bias in cohort studies. Am J Epidemiol 1977;106:184–7. 10.1093/oxfordjournals.aje.a112451 [DOI] [PubMed] [Google Scholar]
- 16.Ontario.ca . Ontario demographic Quarterly: highlights of first quarter, 2020. Available: https://www.ontario.ca/page/ontario-demographic-quarterly-highlights-first-quarter-2020
- 17.Government of Canada SC . The daily — immigration and ethnocultural diversity: key results from the 2016 census, 2017. Available: http://www.statcan.gc.ca/daily-quotidien/171025/dq171025b-eng.htm
- 18.Kapral MK, Hall RE, Silver FL, et al. Registry of the Canadian stroke network. Report on the 2004/05 Ontario stroke audit. Available: https://www.ices.on.ca/~/media/Files/Atlases-Reports/2009/RCSN-report-on-2004-05-Ontario-stroke-audit/Full-report.ashx
- 19.Hall S, Schulze K, Groome P, et al. Using cancer registry data for survival studies: the example of the Ontario cancer registry. J Clin Epidemiol 2006;59:67–76. 10.1016/j.jclinepi.2005.05.001 [DOI] [PubMed] [Google Scholar]
- 20.Kurdyak P, Lin E, Green D, et al. Validation of a population-based algorithm to detect chronic psychotic illness. Can J Psychiatry 2015;60:362–8. 10.1177/070674371506000805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tu K, Chen Z, Lipscombe LL, et al. Prevalence and incidence of hypertension from 1995 to 2005: a population-based study. CMAJ 2008;178:1429–35. 10.1503/cmaj.071283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hux JE, Ivis F, Flintoft V, et al. Diabetes in Ontario: determination of prevalence and incidence using a validated administrative data algorithm. Diabetes Care 2002;25:512–6. 10.2337/diacare.25.3.512 [DOI] [PubMed] [Google Scholar]
- 23.Gershon AS, Wang C, Guan J, et al. Identifying individuals with physcian diagnosed COPD in health administrative databases. COPD 2009;6:388–94. 10.1080/15412550903140865 [DOI] [PubMed] [Google Scholar]
- 24.Schultz SE, Rothwell DM, Chen Z, et al. Identifying cases of congestive heart failure from administrative data: a validation study using primary care patient records. Chronic Dis Inj Can 2013;33:160–6. 10.24095/hpcdp.33.3.06 [DOI] [PubMed] [Google Scholar]
- 25.Tu K, Nieuwlaat R, Cheng SY, et al. Identifying patients with atrial fibrillation in administrative data. Can J Cardiol 2016;32:1561–5. 10.1016/j.cjca.2016.06.006 [DOI] [PubMed] [Google Scholar]
- 26.Osypuk TL, Alonso A, Bates LM. Understanding the healthy immigrant effect and cardiovascular disease: looking to big data and beyond. Circulation 2015;132:1522–4. 10.1161/CIRCULATIONAHA.115.018707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yi SS, Thorpe LE, Zanowiak JM, et al. Clinical characteristics and lifestyle behaviors in a population-based sample of Chinese and South Asian immigrants with hypertension. Am J Hypertens 2016;29:941–7. 10.1093/ajh/hpw014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abraído-Lanza AF, Dohrenwend BP, Ng-Mak DS, et al. The Latino mortality paradox: a test of the "salmon bias" and healthy migrant hypotheses. Am J Public Health 1999;89:1543–8. 10.2105/AJPH.89.10.1543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yarnell CJ, Fu L, Manuel D, et al. Association between immigrant status and end-of-life care in Ontario, Canada. JAMA 2017;318:1479–88. 10.1001/jama.2017.14418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen A, Kazanjian A. 516: ethnicity, time in Canada and Pap testing among recent immigrants to British Columbia, Canada. Am J Epidemiol 2005;161:S129. 10.1093/aje/161.Supplement_1.S129c [DOI] [Google Scholar]
- 31.Berthold SM, Kong S, Mollica RF, et al. Comorbid mental and physical health and health access in Cambodian refugees in the US. J Community Health 2014;39:1045–52. 10.1007/s10900-014-9861-7 [DOI] [PubMed] [Google Scholar]
- 32.Hollander A-C. Social inequalities in mental health and mortality among refugees and other immigrants to Sweden--epidemiological studies of register data. Glob Health Action 2013;6:21059. 10.3402/gha.v6i0.21059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Borges G, Orozco R, Rafful C, et al. Suicidality, ethnicity and immigration in the USA. Psychol Med 2012;42:1175–84. 10.1017/S0033291711002340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Saunders NR, Lebenbaum M, Stukel TA, et al. Suicide and self-harm trends in recent immigrant youth in Ontario, 1996-2012: a population-based longitudinal cohort study. BMJ Open 2017;7:e014863. 10.1136/bmjopen-2016-014863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bonifazi C, Paparusso A. Remain or return home: the migration intentions of first-generation migrants in Italy. Popul Space Place 2019;25:e2174. 10.1002/psp.2174 [DOI] [Google Scholar]
- 36.Diaz CJ, Koning SM, Martinez-Donate AP. Moving beyond salmon bias: Mexican return migration and health selection. Demography 2016;53:2005–30. 10.1007/s13524-016-0526-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Saunders NR, Gill PJ, Holder L, et al. Use of the emergency department as a first point of contact for mental health care by immigrant youth in Canada: a population-based study. CMAJ 2018;190:E1183–91. 10.1503/cmaj.180277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Derr AS. Mental health service use among immigrants in the United States: a systematic review. Psychiatr Serv 2016;67:265–74. 10.1176/appi.ps.201500004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Norredam M, Hansen OH, Petersen JH, et al. Remigration of migrants with severe disease: myth or reality?--a register-based cohort study. Eur J Public Health 2015;25:84–9. 10.1093/eurpub/cku138 [DOI] [PubMed] [Google Scholar]
- 40.Arenas E, Goldman N, Pebley AR, et al. Return migration to Mexico: does health matter? Demography 2015;52:1853–68. 10.1007/s13524-015-0429-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kennedy S, Kidd MP, McDonald JT, et al. The healthy immigrant effect: patterns and evidence from four countries. J Int Migr Integr 2015;16:317–32. 10.1007/s12134-014-0340-x [DOI] [Google Scholar]
- 42.Wallace M, Kulu H. Low immigrant mortality in England and Wales: a data artefact? Soc Sci Med 2014;120:100–9. 10.1016/j.socscimed.2014.08.032 [DOI] [PubMed] [Google Scholar]
- 43.Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: global burden of disease study. Lancet 1997;349:1436–42. 10.1016/S0140-6736(96)07495-8 [DOI] [PubMed] [Google Scholar]
- 44.GBD 2015 Tobacco Collaborators . Smoking prevalence and attributable disease burden in 195 countries and territories, 1990-2015: a systematic analysis from the global burden of disease study 2015. Lancet 2017;389:1885–906. 10.1016/S0140-6736(17)30819-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Canada.ca . Interprovincial mobility of immigrants in Canada 2006-2011, 2020. Available: https://www.canada.ca/en/immigration-refugees-citizenship/corporate/reports-statistics/research/interprovincial-mobility-immigrants-canada-2006-2011.html
- 46.Youens D, Preen DB, Harris MN, et al. The importance of historical residential address information in longitudinal studies using administrative health data. Int J Epidemiol 2018;47:69–80. 10.1093/ije/dyx156 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-046377supp001.pdf (1.3MB, pdf)
Data Availability Statement
Data are available upon reasonable request. The data used in this study is held securely in coded form at ICES. Data sharing agreements prohibit ICES from making the dataset publicly available, but access may be granted to those who meet prespecified criteria for confidential access. Please contact corresponding author for details.