Abstract
Ceruminous adenoma is described as a glandular neoplasm of ceruminous glands. It is seen for less than one percent of all external ear tumours. Ceruminous adenoma cases were reported to have recurrence and residual tumour, however there was no malignant transformation known in ceruminous adenoma up to this date. Here, we report a young adult woman with two years history of progressive reduced hearing and tinnitus of the right ear. She was proven to have right moderate conductive hearing loss with pure tone audiometry. There was a cystic mass with serous content arising from the posterior wall of the right ear canal. We proceeded with wide local excision of the mass via trans-canal approach. Ceruminous adenoma was confirmed with histopathology and immunohistochemistry of CK7 staining. The hearing impairment was resolved completely post excision and there was no recurrence of the tumour on one year follow-up. We concluded wide local excision with appropriate margin of the mass is adequate to prevent recurrence in ceruminous adenoma cases.
Keywords: Adenoma, ear canal, benign neoplasm
ÖZ
Serüminöz adenom, serüminöz bezlerdeki tümör olarak tanımlanır. Tüm dış kulak tümörlerinin yüzde birinden azını oluşturmaktadır. Serüminöz adenom olgularında tekrarlama ve artık tümör kalma durumları bildirilmiştir ancak bu tarihe kadar serüminöz adenomda bilinen kötücül transformasyon saptanmamıştır. Bu çalışmada, sağ kulakta iki yıllık ilerleyici işitme azalması ve kulak çınlaması öyküsü olan genç bir yetişkin kadını sunuyoruz. Saf ton odyometresi ile orta derecede iletim tipi işitme kaybına sahip olduğu kanıtlanmıştır. Sağ kulak kanalı arka duvarından kaynaklanan seröz içerikli kistik kitle bulunmuştur. Trans-kanal yaklaşımla kitlenin geniş lokal eksizyonunu gerçekleştirilmiştir. Serüminöz adenom, CK7 boyama histopatolojisi ve immünohistokimyası ile doğrulanmıştır. İşitme bozukluğu eksizyon sonrası tamamen düzeldi ve bir yıllık takipte tümör tekrarı saptanmamıştır. Serüminöz adenom olgularında tekrarları önlemek için sağlıklı kitle marjına sahip geniş lokal eksizyonun yeterli olduğu sonucuna vardık.
Keywords: Adenom, kulak kanalı, iyicil tümör
Introduction
The external auditory canal (EAC) contains modified apocrine sweat glands, which are ceruminous glands and sebaceous glands1,2. Ceruminous glands are located deep to the sebaceous gland, within the dermis at the outer third of the external auditory canal3. Wetli et al. classified ceruminous gland tumours as having benign and malignant neoplasm, whereas ceruminous adenoma was described as benign ceruminous gland tumour4.
Ceruminous adenoma (CA) is described as a glandular neoplasm of ceruminous glands1,5. CA is also known as ‘ceruminoma’, a rare type of external auditory canal tumour that accounts for less than one percent of all external ear tumours and usually affects adult and middle-aged (52-55 years) patients3,5. In 1991, the term ‘ceruminoma’ was excluded because it expresses a more general definition that comprises a heterogenous group of external ear canal tumours with various neoplastic potentials2,6. A study on 41 cases of ceruminous adenoma between 1970 and 2000 reported the recurrence or residual of tumours requiring a second surgery; none of the cases involved a malignant transformation3.
Case Report
A healthy 34-year-old woman presented progressively worsening hearing in the right ear for two years. Her hearing loss was accompanied by persistent non-pulsatile tinnitus. No history of ear pain or vertigo was reported. There was no bleeding from the right ear and no history of recurrent ear discharge. The left ear was asymptomatic. The patient did not notice any facial asymmetry or facial numbness. She had not experienced headaches, blurry vision or nausea and vomiting, which might suggest increased intracranial pressure. She had no history of head or ear trauma, and there was no preauricular swelling or neck swelling. Her appetite was normal, and she maintained a healthy weight.
Also, there wasn’t symptoms signifying chronic tuberculosis infection of the ear, such as tuberculosis contact, night sweat or recurrent fever. There wasn’t any nasal symptom, such as epistaxis, nose blockage, or nasal discharge. The family history did not reveal hearing loss or any malignancy. She was a non-smoker and did not consume alcohol.
An examination of the patient revealed normal vital signs of a healthy adult with intact bilateral facial nerve function. Bilateral ear pinna was normal with no swelling or tenderness. The bilateral mastoid area was not swollen or tender. There was flaky skin around the bilateral ears that extended to the scalp, indicating seborrheic dermatitis.
An otoscopic examination of the right ear revealed a mass arising from the superior wall of the external auditory canal. The mass was lobulated, non-pulsatile without blood. There was no pus or discharge seen. The tympanic membrane was obscured by the mass. The left external auditory canal and tympanic membrane appeared to be normal. The Rinne test results were positive for both ears, but a Weber showed lateralization to the right ear. The free field voice test revealed normal hearing in the left ear and mild to moderate hearing loss in the right ear. This result suggested mild to moderate conductive hearing loss of the right ear, which was later confirmed with pure tone audiometry (PTA) (Figure 1). Tympanometry also reported lower canal volume in the right ear than in the left ear.
Figure 1.
PTA done on the first appointment showed right moderate conductive hearing loss.
High-resolution computed tomography of the temporal bone was reported as a soft tissue lesion occupying the right external ear canal, measured at 1.2 x 0.5 x 0.7 cm (Figure 2). This was most likely because the roof of the external ear canal was located 0.6 cm distal to the tympanic membrane. The adjacent external ear canal wall was minimally eroded. However, the scutum was sharp, and there was no involvement of the middle ear or inner ear. The left ear was reported as normal and both facial canals were intact.
Figure 2.
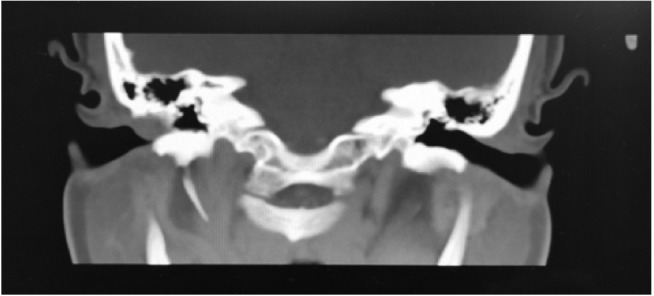
HRCT Temporal
(Tissue window: coronal view)
The arrow pointed to a soft tissue lesion occupying the right external ear canal.
The patient was put under general anesthesia. A microscopic examination revealed a mass arising from the posterior wall of the right EAC (Figure 3). The skin overlying the mass was intact and was soft on palpation. With a microscopic surgical approach, serous fluid was drained from the mass during excision, and the mass was excised completely from the posterior wall of the EAC. Following the mass removal, keratin was seen medially from the location where the mass was attached. There was irregular bony and unhealthy cartilage and soft tissue along the posterior wall of the right EAC. The irregular bone was smoothened, and the unhealthy overlying tissue was removed. Anterior tympanotomy was then performed. Normal middle ear mucosa was observed in the right ear.
Figure 3.

Examination under anaesthesia.
It revealed mass arising from posterior wall of the right EAC.
The overlying skin of the mass was intact. Arrow pointed towards the mass.
A histopathological examination of the right EAC mass revealed circumscribed glandular proliferation in a cribriform, cystic, and solid pattern. The glands were lined by uniform inner cuboidal cells and outer spindled myoepithelial cells (Figure 4). Neither mitosis nor necrosis was observed. There was also no evidence of malignancy. An immunohistochemistry study showed that the inner cuboidal cells were positive to CK7. (Figure 5). These histopathological features were consistent with ceruminous adenoma.
Figure 4.

The right EAC mass showed circumscribed uniform glandular proliferation (Hematoxylin & Eosin, 4x magnification).
Figure 5.

The inner cuboidal cells are CK7-positive by immunohistochemistry (4x magnification) It also showed inner cuboidal cells.
The keratin specimen exhibited loose keratin flakes without a squamous epithelial layer, while the unhealthy cartilage of the posterior wall of the right EAC showed mild chronic inflammatory cell infiltration. The medial margin of the mass showed no evidence of malignancy. Following the excision of the mass, there was no recurrence within a year, and repeated PTA showed improved hearing (Figure 6).
Figure 6.
PTA post excision of the mass showed normal hearing bilaterally.
Discussion
CA has been defined as “well-differentiated, benign, localized proliferation of glands histologically similar to normal ceruminous glands” 7. Ceruminous neoplasm accounts for only 2.4% of all ear neoplasms8, while CA is reported in less than 1% of all benign tumours of external auditory meatus5. Less than 150 cases of CA have been reported-though its incidence is more than reported, most physicians were not adequately experienced in the management of these cases9.
The mean age group for patients diagnosed with CA is 52-55 years; however, CA affects people of a wide age range of 12-85 years old3,5. A few pediatric cases have been reported, this may be associated with apocrine glands’ congenital deformity like nevus sebaceous of Jadassohn2. Males and females are equally affected by CA.
Patients diagnosed with CA generally complain of progressive hearing problems and tend to have nontender masses in the affected external auditory canal3,9. The occupied mass might also cause ear irritation, ear bleeding3, or other symptoms such as otalgia and ear discharges in the presence of concurrent otitis externa or chronic otitis media9,10. Facial asymmetry and excruciating pain might suggest something more severe, such as malignancy.
The patient observed in the present case report was a healthy adult female with no syndromic features. She was having trouble hearing in the right ear and had bothersome tinnitus. However, there was no alarming symptom, and so she only sought treatment after the symptoms persisted for two years. Her prior history of right ear discharge might be because she experienced concurrent right otitis externa, which was already resolved by the time of presentation.
The management of ceruminous gland tumour was described comprehensively in a 1983 published study in which it was concluded that wide excision biopsy should be done for EAC masses1,11. If the mass diagnosis was CA with a clear margin (reported after the confirmation of an experienced pathologist), no further treatment should be started for the patient11,12. Malignancy should be suspected in histopathology with infiltrating margin and tumours with significant nuclear pleomorphism or a brisk mitotic rate13,14.
Immunohistochemistry was used to highlight the biphasic nature of the tumour cells but it not might be necessity for diagnosis5. The ceruminous glands showed dual differentiation and were composed of an inner glandular epithelial layer and an outer myoepithelial layer, where both layers were reported to have positive staining for cytokeratin15.
In the present case study, the patient’s histopathology was reported as CA and confirmed by a pathologist. There was no mitosis and no significant nuclear pleomorphism to suggest malignancy. Unhealthy cartilage was involved, and a medial margin showed no malignant changes. An adequate wide local excision biopsy was performed. Immunohistochemistry showed that the luminal cells were positive for CK7.
The literature reports that recurrence is rare in a follow up of 15 years time period 3,6,10. Four out of 41 patients were reported to have recurrence, and all of them were treated by a second surgery3. The literature didn’t show any report of malignant changes for CA. The patient examined in the present study was followed up three weeks after her operation-all wounds appeared to be healing properly, and no recurrence was noted.
Conclusion
The present study describes a patient with a history of ear blockage, hearing loss and tinnitus with benign swelling occupying the external auditory canal (but no history of alarming symptoms such as facial nerve palsy or excruciating headaches). Histopathology and immunohistochemistry of CK7 staining confirmed the benign nature of it and sufficient evidence to diagnose CA. No further treatment was necessary once the diagnosis was established. Recurrence was not expected after adequate wide local excisions were performed on the patient.
References
- 1.Lassaletta L, Patrón M, Olóriz J, Pérez R, Gavilán J. Avoiding misdiagnosis in ceruminous gland tumours. Auris Nasus Larynx. 2003;30:287–90. doi: 10.1016/s0385-8146(03)00055-5. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 2.Niemczyk E, Niemczyk K, Małdyk J, Zawadzka-Głos L. Ceruminousadenoma (ceruminoma) arising in a nevus sebaceus of jadassohn within the external auditory canal of a 3 year-old boy - a case report. Int J Pediatr Otorhinolaryngol. 2015;79:1932–4. doi: 10.1016/j.ijporl.2015.07.019. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 3.Thompson LDR, Nelson BL, Barnes EL. Ceruminous adenomas: a clinicopathologic study of 41 cases with a review of the literature. Am J Surg Pathol. 2004;28:308–18. doi: 10.1097/00000478-200403000-00003. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 4.Wetli CV, Pardo V, Millard M, Gerston K. Tumors of ceruminous glands. Cancer. 1972;29:1169–78. doi: 10.1002/1097-0142(197205)29:5<1169::aid-cncr2820290507>3.0.co;2-8. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 5.Thompson LDR. Ear ceruminous adenoma. Ear Nose Throat J. 2011;90:304–5. doi: 10.1177/014556131109000706. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 6.Mills RG, Douglas-Jones T, Williams RG. ‘Ceruminoma’ - a defunct diagnosis. J Laryngol Otol. 1995;109:180–8. [CrossRef] [PubMed] [Google Scholar]
- 7.Elsürer Ç, Şenkal HA, Baydar DE, Sennaroğlu L. Ceruminous adenoma mimicking furunculosis in the external auditory canal. Eur Arch Otorhinolaryngol. 2007;264:223–5. doi: 10.1007/s00405-006-0166-z. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 8.Nagarajan P. Ceruminous neoplasms of the ear. Head Neck Pathol. 2018;12:350–61. doi: 10.1007/s12105-018-0909-3. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yamamoto E, Tabuchi K, Mori K. Ceruminous adenoma in the osseous external auditory canal (a case report). J Laryngol Otol. 1987;101:940–5. doi: 10.1017/s0022215100103020. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 10.Psillas G, Krommydas A, Karayannopoulou G, Chatzopoulos K, Kanitakis J, Markou K. Ceruminous adenoma of the external auditory canal: a case report with imaging and pathologic findings. Case Rep Med. 2015;2015:359627. doi: 10.1155/2015/359627. [CrossRef] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mansour P, George MK, Pahor AL. Ceruminous gland tumours: a reappraisal. J Laryngol Otol. 1992;106:727–32. doi: 10.1017/s0022215100120717. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 12.Giuseppe M, Serena B, Sandro B et al. Adenoma of the ceruminous gland (ceruminoma). Otol Neurotol. 2011;32:e14–e15. doi: 10.1097/MAO.0b013e3181db7545. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 13.Iqbal A, Newman P. Ceruminous gland neoplasia. Br J Plast Surg. 1998;51:317–20. doi: 10.1054/bjps.1997.0075. [CrossRef] [DOI] [PubMed] [Google Scholar]
- 14.Shim JW. Ceruminous gland adenocarcinoma of external ear canal. Korean J Pathol. 2007;41:66–8. Available from: https://www.jpatholtm.org/upload/pdf/kjp-41-1-66.pdf. [Google Scholar]
- 15.Ito K, Ito T, Tsukuda M, Kanisawa M. An immunohistochemical study of adenoid cystic carcinoma of the external auditory canal. Eur Arch Otorhinolaryngol. 1993;250:240–4. doi: 10.1007/BF00171533. [CrossRef] [DOI] [PubMed] [Google Scholar]




