Abstract
Purpose:
Cardiac rehabilitation (CR) has been shown to improve functional status, quality of life, and recurrent cardiovascular disease (CVD) events. Despite its demonstrated compelling benefits and guideline recommendation, CR is underutilized, and there are significant disparities in CR utilization particularly by race, ethnicity, sex, and socioeconomic status. The purpose of this review is to summarize the evidence and drivers of these disparities and recommend potential solutions.
Methods:
In this review, key studies documenting disparities in CR referrals, enrollment, and completion are discussed. Additionally, potential mechanisms for these disparities are summarized and strategies are reviewed for addressing them.
Summary:
There is a wealth of literature demonstrating disparities among racial and ethnic minorities, women, those with lower income and education attainment, and those living in rural and dense urban areas. However, there was minimal focus on how the social determinants of health contribute to the observed disparities in CR utilization in many of the studies reviewed. Interventions such as automatic referrals, inpatient liaisons, mitigation of economic barriers, novel delivery mechanisms, community partnerships, and health equity metrics to incentivize healthcare organizations to reduce care disparities are potential solutions.
This review confirms disparities in CR among patients who might benefit the most from CR by reduction in recurrent CVD events and improved survival which are driven by negative social determinants of health. Innovative strategies to overcome barriers to CR participation in special populations are necessary for successfully closing these healthcare gaps.
Keywords: health disparities, race, sex, socioeconomic status, region, cardiac rehabilitation
Condensed Abstract:
This review describes disparities in utilization of cardiac rehabilitation (CR) by race and ethnicity, sex, and geography. Further, the intersection of social determinants of health on observed disparities based on individual characteristics are described. Despite the proven benefits of CR, significant disparities in patient referrals, enrollment, and completion remain. Relevant literature documenting these disparities, their potential mechanisms, and means for disparity reduction are discussed.
Cardiovascular disease (CVD) is the greatest cause of morbidity and mortality in the United States (US) and worldwide.1 Individuals with incident CVD events are at high risk of recurrent events, rehospitalization, and death.2 Secondary prevention strategies including pharmacotherapies, aggressive risk-factor control, and lifestyle modification have all been shown to reduce the risk of subsequent adverse CVD outcomes.1
Cardiac rehabilitation (CR), an effective secondary prevention strategy for patients who have experienced a CVD event, is highly underutilized. 3–7 Research has shown that CR reduces mortality and recurrent CVD events by up to 26%, and 47%, respectively3 and is also associated with improved functional status and quality of life. American College of Cardiology/American Heart Association clinical guidelines recommend CR for patients after acute myocardial infarction (MI), coronary artery bypass graft surgery (CABG), percutaneous coronary intervention (PCI), heart valve surgery, chronic stable angina, chronic heart failure with reduced ejection fraction, and heart/lung transplantation. Medicare and most commercial health insurers reimburse CR services for patients with a qualifying indication. Out of nearly 2.1 million patients with CVD events eligible for CR annually, national estimates of CR participation range from 20–30%.8–10 More recently, low utilization has been exacerbated by lack of access and reduced capacity for center-based CR due to the coronavirus disease 2019 (COVID-19) pandemic.11 Previous work has documented specific disparities in CR utilization based on individual characteristics of race, ethnicity, sex, and socioeconomic status (SES).12 A review in 2011 by Valencia et al. described widespread disparities to CR participation by race, ethnicity, SES, and rurality.12 The purpose of this review is to update the literature since 2011 with select key literature, and to provide insights of the significant role that the social determinants of health (SDOH) contribute to observed disparities in CR utilization based on individual characteristics and region. Lastly, we provide relevant recommendations to address these pervasive disparities.
REVIEW OF RELEVANT LITERATURE
Participation in CR reflects referral, defined as a physician order, a discussion with the patient, and the receipt of the referral by a CR program.10 An abundance of data show that disparities in CR participation stem, in part, from low referral rates by healthcare providers. Participation in ≥1 CR session is defined as enrollment, while attending the standard program of either 32 – 36 sessions over a 3 mo period is considered completion in the majority of CR programs.10,13 This review provides insight on the importance of considering the SDOH in enhancing CR participation, particularly for under-resourced racial and ethnic minority groups. The SDOH are defined by the U.S. Department of Health and Human Services as “conditions in the environments in which people are born, live, learn, work, play, and worship” that affect health outcomes.14 Negative SDOH include limited access to educational opportunities, employment, and health care as well as food and housing insecurity.15
DISPARITIES IN CARDIAC REHABILITATION BY RACE AND ETHNICITY
Physician referral is one of the most important predictors of subsequent CR enrollment.16 Studies examining differences in referral rates mainly come from nationwide quality improvement registries or single center studies thus limiting their generalizability to real world clinical practice. However, findings from these studies have illuminated disparities in referral rates by race and ethnicity.
In a retrospective analysis of 50,000 patients, from 551 hospitals across the US with MI between 2003 and 2009 from hospitals enrolled in the Get With The Guidelines Registry, referral rates at hospital discharge were significantly lower for racial and ethnic minorities.17 African Americans, Hispanics, Asians, and other minorities were 20, 36, 50, and 22% less likely to be referred to CR, respectively, than White patients.17 The major strength of this study was its provision of population-based, national-level data with rigorous ascertainment of CR referral order pattern. The study limitations included a lack of more recent data, low proportion of racial and ethnic minorities (82% White), and residual confounding (patient-centered factors such as lack of access to CR). In addition, the voluntary and quality improvement nature of the patient registry may not be reflective of routine clinical practice and diverse CVD patients. Lastly, while the investigators adjusted for demographics, clinical characteristics, hospital characteristics and patients’ insurance status, there was limited information on other SDOH to account for the demonstrated racial/ethnicity gaps in CR referrals.
Similarly, the Get with the Guidelines Registry from the National Cardiovascular Data Registry (NCDR) Acute Coronary Treatment and Intervention Outcomes Network – ACTION Registry from 2007 and 2012, showed that overall CR referrals improved from 72.9% in 2007 to 80.7% by 2012, but that African Americans and Hispanics had significantly lower odds of referral to CR (OR=0.75: 95% CI, 0.65–0.87; OR=0.64: 95% CI, 0.52–0.79, respectively).18 Nonetheless, there were several limitations of this study including that it encompassed data from a voluntary quality improvement registry of hospitals providing CR referral data, thus it may not be representative of low-resourced hospitals. As such, the investigators acknowledged that their findings may overestimate CR referral rates. Also, the analyses did not specifically account for patient-level SDOH that could have influenced the observed racial disparities.
These findings were consistent with another large study of 1.5 million consecutive patients who underwent PCI between 2009 and 2012, across 1,310 US hospitals enrolled in the NCDR Cath-PCI Registry. Referral rates were 59% after PCI and no significant differences by race were found. However, when restricting the analyses to patients on Medicare, African Americans were significantly less likely to be referred to CR compared to their White counterparts (OR=0.94: 95% CI, 0.896–0.995).19 Similar to the previous registry studies, there was limited focus on the SDOH.
While all of these studies have consistently shown disparities in rates of referrals by race, when viewed as a conglomerate, they all have similar limitations. Although published within the last 10 yr, the data analyzed within the studies are in general > 10 yr old and may not be reflective of current clinical practice in the digital age of electronic health records, and increased use of automated electronic CR referrals. In addition, the study’s participants were relatively homogenous (>80% White) and lack patient diversity with relatively low proportions of racial and ethnic minority groups. Additionally, the majority of the data analyses in these studies compare non-Hispanic White to non-White racial and ethnic minority groups, which may reflect a broader issue of structural racism.20 As outlined by a recent American Heart Association Scientific Statement, proper use of US Census-delineated race and ethnicity classifications is preferred as a best practice for publishing disparities research. The exclusion of diverse racial and ethnic populations may not be intentional, but may be a result of lack of diversity in cardiovascular clinical trials and medical research.21,22 More studies are needed on referral practices specifically for Native Americans, Hispanics, and Asians. Lastly data on the SDOH (e.g., income, education attainment, neighborhood characteristics) were not adjusted for in these studies, thus the role and magnitude of influence that individual characteristics or the SDOH play as drivers of these observed disparities in referrals remains unknown.
Disparities also manifest in lower enrollment and completion rates among racial and ethnic minorities. A cross-sectional examination of 260,000 Medicare beneficiaries with acute MI or CABG showed that White patients were 33% more likely to participate in ≥1 CR session compared to racial and ethnic minority patients.8 Two decades later not much progress had been made in CR participation as demonstrated by a follow-up study by Ritchey et al. which showed similar findings.9 Among nearly 360,000 Medicare beneficiaries hospitalized for a CVD event with a CR indication, African American, Hispanic, and Asian patients were 30, 37, and 20% less likely to enroll in CR compared to Whites. Both of these studies, and others,23,24 confirmed low participation rates among largely racial and ethnic minority Medicare beneficiaries.
Single center studies have demonstrated consistent findings. Among > 800 patients cared for at an academic medical center in New York serving a predominantly Hispanic patient population, Whites were more likely to enroll in CR compared to racial and ethnic minority groups (OR=1.78: 95% CI, 1.13–2.80).25 Similarly, Whites were 60% more likely to complete CR.25 While data is limited for Native Americans, it has been reported that CR programs in US Native American communities are virtually non-existent.26
DISPARITIES IN CARDIAC REHABILITATION BY SEX AND GENDER
Significant disparities by sex and gender also exist in CR referrals, as shown in numerous studies. Women with ischemic heart disease eligible for CR are less likely to have a written referral and receive instructions on CR compared to men. A recent meta-analysis of 19 observation studies examining differences in referral rates by sex among over 240,000 participants found that women were 32% less likely to be referred to CR compared to men despite similar eligibility.27 Registry data have shown consistent findings. In the Get With The Guidelines Registry, women were less likely to be referred to CR (adjusted OR=0.88: 95% CI, 0.85 – 0.92) despite adjustment for age, demographic and other clinical characteristics.17 Similarly, in a claims registry in Michigan, women discharged after hospitalization for PCI for symptomatic CHD were less likely to be referred to CR after adjustment for age and other demographics (adjusted OR=0.94: 95% CI, 0.92 – 0.96).28
One of the largest known cohorts examining sex and gender disparities in CR is within the APPROACH (Alberta Provincial Project for Outcomes Assessment in Coronary Heart Disease) database of 36,264 consecutive patients (24.6% women) undergoing coronary angiography for symptomatic CAD.29 The study found that women had 25% lower odds of being referred to CR. The women in the cohort were older, with more CVD risk factors and comorbid conditions, but these associations persisted despite adjustment for age and clinical characteristics. In terms of outcomes, women who were referred and attended CR had a survival benefit compared to those who were not referred. While Canada has a universal healthcare system which limits generalizability to other health systems, this study provides substantial evidence pointing to the existence of sex and gender-related referral bias.
After referral, the majority of studies show that women, particularly racial and ethnic minority women, enroll and complete CR at lower rates than men. Data from two recent meta-analyses confirm these findings. Sun et al. included 21 studies (n = 349,058) examining factors associated with CR participation and found that women were 41% less likely to enroll in CR.30 A meta-analysis by Samayoa et al. of 26 studies (n = 297,719), found that women were 36% less likely to enroll in CR compared to men.31 In the APPROACH database, compared to men who were referred, women who were referred were less likely to attend or complete CR.29 Additionally, US population-based estimates of sex disparities in CR participation among Medicare beneficiaries have remained relatively unchanged for the past 20 yr.8,9 Older data suggests that racial and ethnic minority women in particular have lower adherence and completion rates in CR despite the known mortality benefits and are more likely to withdraw from CR due to work conflicts.29,32 On the other hand, other studies show similar enrollment rates among men and women once referred.33 Despite such compelling data, limitations of these studies are the lack of exploration of sociodemographic characteristics such as insurance type, education attainment, and employment status that could potentially explain the observed disparities by sex and gender.
DISPARITIES IN CARDIAC REHABILITATION BY SOCIOECONOMIC STATUS
Socioeconomic status as measured by several individual (e.g., income, education attainment, occupation, medical assistance such as Medicaid) and environmental indicators (e.g., area deprivation index or median income based on zip code data) has been shown to have a significant impact on CVD development and outcomes.34 Individuals with low SES and CVD face a disproportionately higher risk of recurrent events and mortality compared to those with high SES.35
However, data shows that patients with low SES are less likely to be referred to CR. Among the 1.5 million patients in the NCDR Cath-PCI Registry, those on Medicaid had a significantly lower likelihood of being referred to CR compared to those with private insurance (OR=0.979: 95% CI, 0.960 – 0.998).19 Among nearly 1,800 patients with symptomatic CHD with an indication for CR discharged from 11 hospitals in Ontario, Canada, patients with low SES were significantly less likely to be referred to or enrolled in CR.36
Enrollment in CR and completion rates are also low among patients with low SES.37 In 1997, < 6% of dual eligible Medicare and Medicaid beneficiaries (as a surrogate to classify low SES patients) enrolled in CR, compared to > 20% who were on Medicare only.8 Significant differences remained in a 2016 examination of Medicare claims; dual eligible Medicare/Medicaid beneficiaries still enrolled in CR at lower rates compared to those on Medicare only (OR=0.65: 95% CI, 0.59 – 0.71).9 In their analysis of CR use among Medicare beneficiaries, Suaya et al. made notable efforts to include a variety of socioeconomic variables such as zip code characteristics of patient’s residence including degree of urbanization, income, proportion of the population at or below the poverty level, and proportion with college education.8 They found that patients residing in zip codes with the highest levels of urbanization and poverty were 36 and 17% less likely to use CR than those living in the most rural or least impoverished areas, respectively (P<.001). Ritchey and colleagues also acknowledged the importance of financial barriers on CR participation rates citing transportation, employment and issues with supplemental issues—all high-risk factors also of consideration in racial and ethnic minority groups.9
Income is also correlated with CR enrollment and completion in multiple studies.38 In the Southern Community Cohort Study, among > 4,000 participants with symptomatic CHD as an indication for CR, individuals with a higher household income (>$25,000) were 68% more likely to initiate CR than individuals making < $15,000.39 Education level has also consistently been a strong predictor of CR enrollment; those with less than high school education are less likely to enroll and complete CR compared to those with college education or greater.30,38 The effect of education persists despite controlling for income.38 In one study, state-by-state variation in CR enrollment was correlated with state-by-state variation in high school graduation rates.38 Area-level factors also influenced enrollment and completion; those living in the most deprived neighborhoods were less likely to enroll in CR compared to those in the least deprived neighborhoods.8,39
GEOGRAPHIC DISPARITIES IN ACCESS TO CARDIAC REHABILITATION
There is a dearth of more recent research examining disparities in CR utilization by geography. However, older studies still provide important insight into existing disparities by region.
Distance to the CR center, particularly in rural areas, is a significant barrier to referral, enrollment, and completion.40 For example, Curnier et al. compared population density based on the 2000 census and active, certified CR programs in the US.41 They found significant variations in CR availability by geography; northeastern states had 1 program/428 square mi compared to < 1 program/2,689 square mi in the northwestern states. Compared to patients with MI or CABG living ≤ 1.5 mi of a CR center, those living ≤ 3, ≤15, and > 15 mi from a CR center were 7, 42, and 71% less likely to enroll in CR, respectively.8 Furthermore, southern states had participation rates of 6 – 13%, while north-central states had participation rates as high as 24 – 42%.38 Among 1.5 million patients with PCI in the NCDR database, those living in midwestern states had 7.3 higher odds of referral to CR compared to those in southern states.19
Even if rural patients are referred and enroll, they are less likely to complete CR. One study examined 1,800 patients with an indication for CR discharged from 11 hospitals in Ontario, Canada between 2006 and 2008.36 Patients from rural areas who reported driving > 30 min to a CR center had similar proportions of referrals, enrollment, and participation compared to urban patients; however, they were less likely to complete CR.36 Among 254 rural patients with symptomatic CHD who were referred to CR, 28% participated in >1 session, but only 17% of those completed a full CR course, with distance from the center reported as the greatest barrier to completion.42 Richet et al. found interesting geographic variation in CR use in the US, with the Southeast and Appalachia US regions having the lowest participation but highest completion and the Midwest having the highest participation but lowest completion.9
Regions with high population density also have impediments to CR.41 For example, in cities like New York, there is only 1 program/728,000 residents.41 This is in contrast to Nebraska, which has 1 program/23,000 residents. Urban hospitals serving racial and ethnic minority patients may not always have a CR center affiliated with them, and physicians are less likely to refer to other facilities for fear of losing their patient base.37 The Get with the Guidelines Registry confirmed these regional differences due to population density; compared to those in the northeast, midwestern states had a higher likelihood of referral to CR (adjusted OR=2.51: 95% CI, 1.38 – 4.58).17
DISCUSSION
This review provides a contemporary summary of peer-reviewed literature documenting the existing, and persistent disparities in utilization of CR by race/ethnicity, sex, SES, and geography. Although limited in quantity, the studies included in this review provide support for the necessity of more intentional efforts to reduce these disparities. This will require a more nuanced understanding of the underlying mechanisms by which these disparities occur, including the overarching influence of the SDOH on their propagation. In this discussion, we will examine research describing potential sources of these disparities including implicit bias, discrimination, and structural barriers at the institutional and health system levels.
Mechanisms for racial and ethnic disparities in CR
Several mechanisms are hypothesized to exacerbate disparities in CR utilization among racial and ethnic minority groups. The intersectionality of individual and community level SES and race/ethnicity may play a role in observed disparities as these groups are more likely to carry a high burden of negative SDOH leading to their low engagement with CR. Scarcity of CR centers in rural areas and in urban hospital systems that serve predominantly minority patients also significantly influence racial and ethnic disparities in referral and enrollment.37 This is supported by an investigation by Aragam et al. showing that disparities in CR referrals were pronounced in hospitals that cared for predominantly minority patients.28
Healthcare provider factors may also drive these disparities. One mechanism is through differences in referrals for CVD-related procedures such as PCI or CABG. Data shows that compared to Whites with symptomatic CHD, African Americans are less likely to be referred for PCI or CABG.43,44 Compared to patients who have medically managed CHD, those who undergo procedures (e.g., CABG or PCI) are more likely to be referred to CR thus exacerbating racial disparities in CR.9 Patients’ insurance status may also pose a challenge for CR referrals and enrollment. Racial and ethnic minorities in the US are more likely to have Medicaid or be uninsured compared to Whites, which may contribute to lower referrals and enrollment.45,46 Patients on Medicaid or medical assistance are less likely to be referred to CR compared to patients on commercial insurance plans.19 Additionally, while patients on Medicaid have no associated CR copays, lower-tier insurance plans may have inadequate coverage for CR or prohibitive copays, resulting in lower enrollment rates.37,45 Lack of healthcare provider awareness of CR, skepticism about its benefits, lack of access to CR facilities, and misconceptions on eligibility and reimbursements may play a role in lower referrals, particularly from safety net hospitals that serve predominantly minority patients.37
Additionally, implicit bias has been suggested as a reason why racial and ethnic minorities may be less likely to be referred to CR.47 Physicians caring for racial and ethnic minorities are less likely to encourage them to participate in CR or actually refer to them CR.37 In one study examining provider perspectives towards CR, clinicians held the belief that African Americans and other minorities had negative attitudes toward exercise that would result in their lower participation and adherence to CR.37
The most significant barriers to CR enrollment described by African American patients were lack of insurance, constraints by insurance coverage on participation, and prohibitive out-of-pocket costs such as copays, and transportation difficulties.37 Self-perceived discrimination, dissatisfaction with the doctor-patient relationship, and trustworthiness of the health system have also been proposed as factors that lower participation rates .12 Among non-English speaking minorities, language barriers play a role in lower referrals and enrollment. In one study in Canada, prior to interpreter services being universally offered, patients who required interpreter services were less likely to be referred to CR compared to their counterparts. 48 Language barriers adversely impact all phases CR utilization including referral, enrollment, and completion.49
Structural racism is increasingly recognized as an underlying cause of health-related disparities in the US. While there is data on disparities in CVD risk factors, control, and outcomes, the impact of structural racism on CVD and CR access in particular are not well understood and are worthy of in-depth, future investigation.50
Mechanisms for sex and gender disparities in CR
Literature suggests that multiple factors related to sex and gender impact CR participation. Barriers to participation may occur at the healthcare provider level manifesting as lower referral rates.29 Data suggests that physicians discuss and endorse CR with men more often than women. There are a few hypothesized reasons for the lower referral rates. One, in general women may be older with more comorbidities at the time of their CVD event, and physicians may adjust referral patterns based on patient comorbidity burden (i.e. less likely to refer their older and sicker patients).29,51 However, many studies show differences persist despite adjustment for age. Another reason is implicit bias among healthcare providers that women may benefit less from CR or be less likely to attend than men.52 Also, psychosocial factors such as social support and anxiety may play a larger role in enrollment among women compared to men.51 Gender-related factors including those in which women may face more competing responsibilities related to work or home, or feel guilty about enrolling in CR due to their responsibilities can lead to low CR participation.52 Further, women may face more financial barriers related to enrollment or attendance in CR.52
Mechanisms for socioeconomic disparities in CR
Existing literature has documented multiple barriers to accessing health services such as CR for patients with low SES in urban areas.53 These barriers in access are predominantly related to adverse SDOH such as cost,36 transportation,36 inadequate facilities,37 interpersonal barriers such as mistrust,37 time constraints,54,55 lack of awareness or social supports to seek care,37 and systemic barriers such as physician perceptions (lower health literacy, lower likelihood of complying with medical advice) and fewer referrals.37,56 The COVID-19 pandemic has drastically reduced in-person health services utilization thus has significantly impacted use of center-based CR. Many CR programs substituted telemedicine-based services such as home-based, virtual CR. However, significant disparities by SES have been documented in the use of telehealth during the pandemic.57–58 In addition, the pandemic has had a devastating impact on patients of lower SES, particularly racial and ethnic minorities, further widening healthcare inequities.59–61
APPLICATION TO PRACTICE: POTENTIAL SOLUTIONS
There is an abundance of literature on practical strategies to address known barriers, improve CR referral and enrollment, thus addressing disparities in CR participation (Figure 1).10
Figure 1.
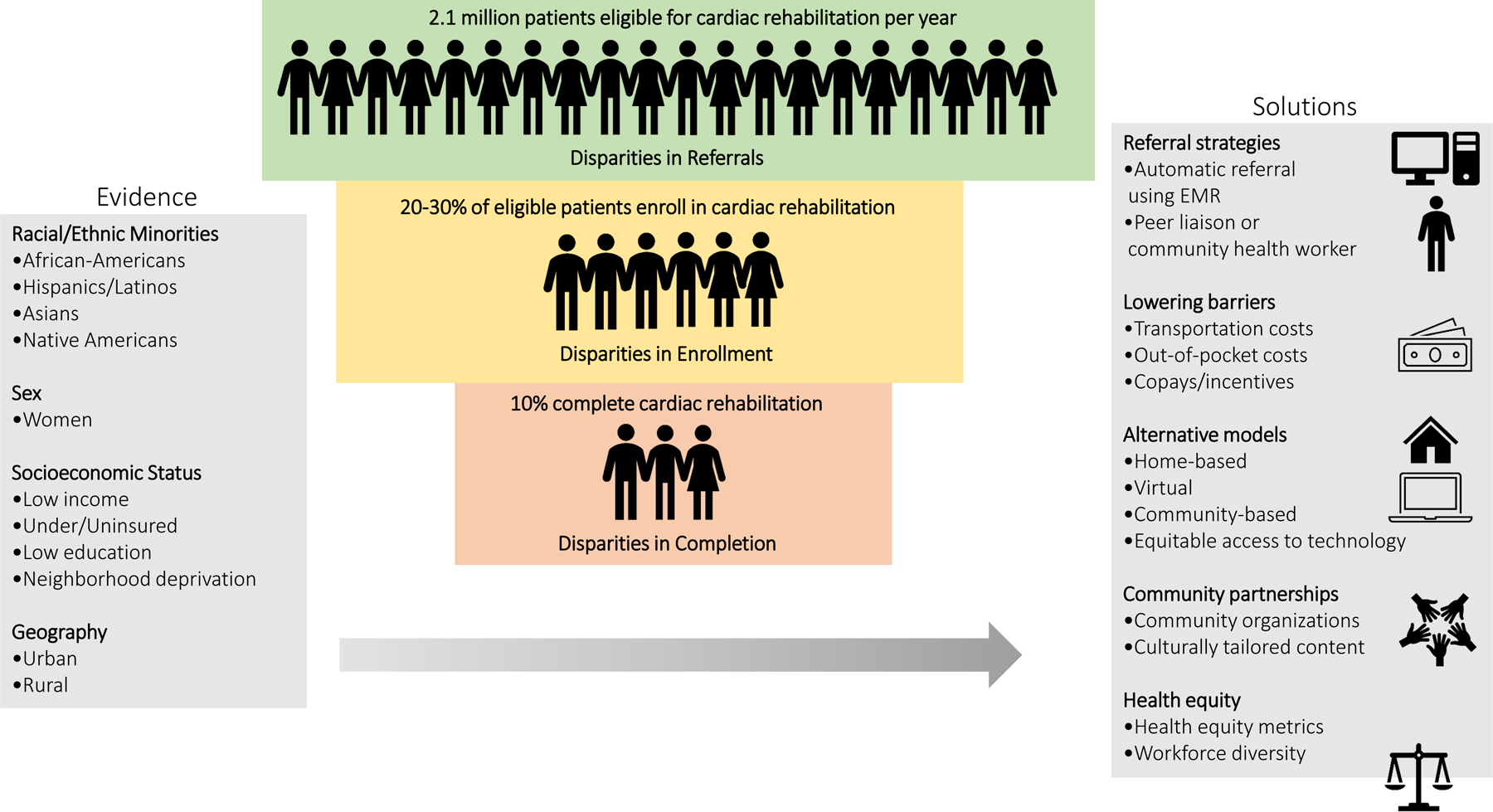
Disparities in Cardiac Rehabilitation.
Referral strategies
Referrals, which include both the order and a discussion with the patient, are a significant factor in CR utilization. One evidence-based strategy to improve physician referrals is to create automatic referrals to CR via electronic health records at the time of hospital discharge.10 These can be issued for specific qualifying diagnoses and thus capture the majority of patients with an indication. Grace and colleagues found that automatic referrals of eligible patients to CR in Canada through electronic health records led to a three-fold increase in CR referrals and doubled enrollment rates compared to usual care.62 In addition, systematic referrals were also shown to increase equitable access and enrollment rates among socioeconomically disadvantaged patients with CVD including those with obesity and functional status limitations from Ontario hospitals.63 While the US healthcare system differs from its Canadian counterpart, due to lack of single payer insurance, there is evidence to suggest that automatic referrals could increase CR enrollment by systematizing referrals and reducing biases.10,64
Staff liaisons who can meet with patients prior to discharge to discuss CR and help them navigate the referral process has also been shown to boost referrals.62 Grace et al. showed that the combination of automatic referrals and patient liaisons significantly increased CR referrals and enrollment compared to usual care (OR=4.45: 95% CI, 1.98 – 10.00).62 Culturally sensitive liaisons who share some characteristics with the patients such as belonging to a peer group65 or community health workers may be a way to reduce disparities by assisting with healthcare navigation after hospital discharge.66 These liaisons can also provide encouragement toward CR participation and help to identify and target barriers to enrollment which is particularly important for under-represented patient groups with a high burden of adverse SDOH.
Many patients face significant barriers from copays, out-of-pocket, and transportation costs. Elimination of these costs, or assistance with navigation of these barriers,67 and financial incentives,68 could help improve CR enrollment.10
Improving access through alternative CR delivery models
One significant cause of disparities is difficulty accessing CR due to logistical difficulties and this has been more pronounced during the COVID-19 public health crisis.11,37 Alternatives to center-based CR through digital platforms have been shown to achieve similar improvements in CVD outcomes.69 These primarily home-based modalities have the potential to expand CR to more eligible patients who may have limitations to participating in center-based CR.70–73 In addition, the use of text messaging and mobile applications to engage with patients and track participation has been shown to improve outcomes in CR and may complement home-based CR.74
Home-based CR programs can be an alternative to making it accessible to patients.69 Historically, one of the challenges of home-based CR is lack of reimbursement. However, the COVID-19 pandemic has resulted in CR center closures and reductions in CR capacity, which has resulted in CMS approving reimbursement for home-based CR during the public health emergency and a rapid expansion of mobile platforms to support home based CR.75 However, for racial and ethnic minorities, patients with lower SES and patients in rural areas, access to the Internet, devices and tele-health services may be more challenging.57,76 Efforts at equitable access to technology and innovative home-based CR models that include all the key CR components are needed.58,77–79
Community partnerships
Partnerships with trusted community organizations such as churches or community recreation centers (e.g., YMCA) have the potential to increase enrollment by enhancing trust, cultural sensitivity, and access.80,81 In addition, developing program content with community member input that is culturally and linguistically tailored to patients’ needs could potentially increase adherence to CR among socially and economically disadvantaged populations.10 Community-based participatory research strategies to design culturally relevant, lifestyle interventions through academic-community partnerships have demonstrated positive outcomes on cardiovascular health outcomes in African Americans.82 These approaches could be translated to the development of more patient-centric CR programs within the context of SDOH to combat racial and ethnic disparities in CR.
Healthcare Delivery
Promoting diversity in CR staff could be another potential way of improving health equity in CR. Research has shown that racial and ethnic concordance between patients and providers results in higher rates of health-service utilization, patient satisfaction, and adherence to treatment. 83 The American Association of Cardiac and Pulmonary Rehabilitation (AACVPR) surveyed its members in 2010 and found that among nearly 1,000 respondents, only 1% were African American.84 Improving patient-provider relationships by increasing diversity among CR health professionals, may lead more trust, patient satisfaction, and to higher participation in CR.12 Cultural competence in health care also contributes to better patient-provider relationships, increased patient satisfaction and higher quality of care.85 Therefore, integration of health equity, cultural competence and implicit bias training among CR professionals, may result in higher enrollment and completion rates, particularly among racial and ethnic minorities.12,85–86
Efforts are underway to measure the impact that hospitals and health systems have on community health by serving their surrounding disadvantaged communities using health equity metrics.87 Potentially including high-quality CR as a health equity metric to ensure that hospitals are accountable for offering evidence-based preventive services such as CR to their communities in both urban and rural areas, may be another step in achieving equity in CR.87 As aforementioned integration of electronic health records for systematic referrals and longitudinal surveillance of CR demographics (i.e., proportion of women, racial and ethnic minority groups, etc.) should also be included within CR health equity metrics. In addition, the required and enhanced ascertainment and documentation of the SDOH in electronic health records, could assist in addressing barriers to CR participation, care coordination lapses, patient-clinician shared decision making, and resource allocation to underserved patients—all key in achieving equity in CR.88
SUMMARY
Each year, nearly 2.1 million individuals have a cardiac event making them eligible for CR, however, < 30% of them participate.10 This translates to an enormous volume of missed opportunities in health benefits, especially among special patient population groups.9 Cardiac rehabilitation is underutilized by racial and ethnic minorities, women, and individuals with low SES. Additionally, disparities in CR exist in both rural and dense urban areas. Rigorous, population-based data on longitudinal utilization patterns among all eligible patients, with more precise information on race, ethnicity, and SES are lacking. Furthermore, while many factors contribute to these observed disparities, the SDOH undergird and exacerbate inequities in CR access and participation. More up-to-date data are needed in this regard, especially in the devastating aftermath of COVID-19 on vulnerable populations and with the increased adoption of telemedicine.11 Future research and efforts should focus on understanding the etiology of CR disparities, development of authentic community partnerships and increasing workforce diversity. Finally, standardization and longitudinal surveillance of quality metrics of health equity for CR access, referrals and enrollment to track progress in eliminating disparities in CR are essential.87
Acknowledgement:
We thank Courtney McQueen, PhD and Mrs. Tessa Flies for editing and review services.
Sources of Funding: Dr. Mathews was supported by Diversity Supplement under ARIC Contract Grant Number Contract HHSN268201700002I/75N92019F00074 from the National Heart, Lung, and Blood Institute, National Institutes of Health. Dr. Brewer was supported by the American Heart Association-Amos Medical Faculty Development Program (Grant No. 19AMFDP35040005), the National Institutes of Health (NIH)/National Institute on Minority Health and Health Disparities (NIMHD) (Grant No. 1 R21 MD013490–01) and the Centers for Disease Control and Prevention (CDC) (Grant No. CDC-DP18–1817) during the implementation of this work. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of NIH or CDC.
Footnotes
Conflicts of interest: None
REFERENCES
- 1.Virani SS, Alonso A, Benjamin EJ, et al. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation 2020:CIR0000000000000757. [DOI] [PubMed] [Google Scholar]
- 2.Chaudhry SI, Khan RF, Chen J, et al. National trends in recurrent AMI hospitalizations 1 year after acute myocardial infarction in Medicare beneficiaries: 1999–2010. J Am Heart Assoc 2014;3(5):e001197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lawler PR, Filion KB, Eisenberg MJ. Efficacy of exercise-based cardiac rehabilitation post-myocardial infarction: a systematic review and meta-analysis of randomized controlled trials. Am Heart J 2011;162(4):571–584 e572. [DOI] [PubMed] [Google Scholar]
- 4.Anderson L, Thompson DR, Oldridge N, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev 2016(1):CD001800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shields GE, Wells A, Doherty P, Heagerty A, Buck D, Davies LM. Cost-effectiveness of cardiac rehabilitation: a systematic review. Heart 2018;104(17):1403–1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thomas RJ, Balady G, Banka G, et al. 2018 ACC/AHA Clinical Performance and Quality Measures for Cardiac Rehabilitation. A Report of the American College of Cardiology/American Heart Association Task Force on Performance Measures 2018;71(16):1814–1837. [DOI] [PubMed] [Google Scholar]
- 7.CMS. Decision Memo for Cardiac Rehabilitation (CR) Programs - Chronic Heart Failure (CAG-00437N). In: Services CfMaM, ed2014. [Google Scholar]
- 8.Suaya JA, Shepard DS, Normand SL, Ades PA, Prottas J, Stason WB. Use of cardiac rehabilitation by Medicare beneficiaries after myocardial infarction or coronary bypass surgery. Circulation 2007;116(15):1653–1662. [DOI] [PubMed] [Google Scholar]
- 9.Ritchey MD, Maresh S, McNeely J, et al. Tracking Cardiac Rehabilitation Participation and Completion Among Medicare Beneficiaries to Inform the Efforts of a National Initiative. Circ Cardiovasc Qual Outcomes 2020;13(1):e005902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ades PA, Keteyian SJ, Wright JS, et al. Increasing Cardiac Rehabilitation Participation From 20% to 70%: A Road Map From the Million Hearts Cardiac Rehabilitation Collaborative. Mayo Clin Proc 2017;92(2):234–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Epstein E, Patel N, Maysent K, Taub PR. Cardiac Rehab in the COVID Era and Beyond: mHealth and Other Novel Opportunities. Curr Cardiol Rep 2021;23(5):42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Valencia HE, Savage PD, Ades PA. Cardiac rehabilitation participation in underserved populations. Minorities, low socioeconomic, and rural residents. J Cardiopulm Rehabil Prev 2011;31(4):203–210. [DOI] [PubMed] [Google Scholar]
- 13.Farias-Godoy A, Chan S, Claydon VE, et al. The Impact of Reduced Cardiac Rehabilitation on Maximal Treadmill Exercise Time: A RANDOMIZED CONTROLLED TRIAL. J Cardiopulm Rehabil Prev 2018;38(1):24–30. [DOI] [PubMed] [Google Scholar]
- 14.Social Determinants of Health HealthyPeople.gov. https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health. Accessed.
- 15.Brewer LC, Hayes SN, Cooper LA. Have a Heart: Addressing the Gradient of Social Determinants of Health During the COVID-19 Era. JACC Case Rep 2020;2(12):2024–2026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ades PA, Waldmann ML, McCann WJ, Weaver SO. Predictors of cardiac rehabilitation participation in older coronary patients. Arch Intern Med 1992;152(5):1033–1035. [PubMed] [Google Scholar]
- 17.Li S, Fonarow GC, Mukamal K, et al. Sex and Racial Disparities in Cardiac Rehabilitation Referral at Hospital Discharge and Gaps in Long-Term Mortality. J Am Heart Assoc 2018;7(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beatty AL, Li S, Thomas L, Amsterdam EA, Alexander KP, Whooley MA. Trends in referral to cardiac rehabilitation after myocardial infarction: data from the National Cardiovascular Data Registry 2007 to 2012. J Am Coll Cardiol 2014;63(23):2582–2583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aragam KG, Dai D, Neely ML, et al. Gaps in referral to cardiac rehabilitation of patients undergoing percutaneous coronary intervention in the United States. J Am Coll Cardiol 2015;65(19):2079–2088. [DOI] [PubMed] [Google Scholar]
- 20.Breathett K, Spatz ES, Kramer DB, et al. The Groundwater of Racial and Ethnic Disparities Research: A Statement From Circulation: Cardiovascular Quality and Outcomes. Circ Cardiovasc Qual Outcomes 2021;14(2):e007868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang T, Tsang W, Wijeysundera HC, Ko DT. Reporting and representation of ethnic minorities in cardiovascular trials: a systematic review. Am Heart J 2013;166(1):52–57. [DOI] [PubMed] [Google Scholar]
- 22.Michos ED, Reddy TK, Gulati M, et al. Improving the enrollment of women and racially/ethnically diverse populations in cardiovascular clinical trials: An ASPC practice statement. Am J Prev Cardiol 2021;8:100250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Patel DK, Duncan MS, Shah AS, et al. Association of Cardiac Rehabilitation With Decreased Hospitalization and Mortality Risk After Cardiac Valve Surgery. JAMA Cardiol 2019;4(12):1250–1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Patel KS, Brown JD. Disparities in the Use of Cardiac Rehabilitation after a Myocardial Infarction in the United States. J Clin Med 2019;8(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Prince DZ, Sobolev M, Gao J, Taub CC. Racial disparities in cardiac rehabilitation initiation and the effect on survival. PM R 2014;6(6):486–492. [DOI] [PubMed] [Google Scholar]
- 26.Van Dyk H, Kim P, Galloway J, Moore M, Cowher J, Jones J. Cardiac Rehabilitation and Secondary Prevention of Coronary Heart Disease in Native Communities. The IHS Primary Care Provider 2006;31(March 2006). [Google Scholar]
- 27.Colella TJ, Gravely S, Marzolini S, et al. Sex bias in referral of women to outpatient cardiac rehabilitation? A meta-analysis. Eur J Prev Cardiol 2015;22(4):423–441. [DOI] [PubMed] [Google Scholar]
- 28.Aragam KG, Moscucci M, Smith DE, et al. Trends and disparities in referral to cardiac rehabilitation after percutaneous coronary intervention. Am Heart J 2011;161(3):544–551 e542. [DOI] [PubMed] [Google Scholar]
- 29.Colbert JD, Martin BJ, Haykowsky MJ, et al. Cardiac rehabilitation referral, attendance and mortality in women. Eur J Prev Cardiol 2015;22(8):979–986. [DOI] [PubMed] [Google Scholar]
- 30.Sun EY, Jadotte YT, Halperin W. Disparities in Cardiac Rehabilitation Participation in the United States: A SYSTEMATIC REVIEW AND META-ANALYSIS. J Cardiopulm Rehab Prev 2017;37(1):2–10. [DOI] [PubMed] [Google Scholar]
- 31.Samayoa L, Grace SL, Gravely S, Scott LB, Marzolini S, Colella TJ. Sex differences in cardiac rehabilitation enrollment: a meta-analysis. Can J Cardiol 2014;30(7):793–800. [DOI] [PubMed] [Google Scholar]
- 32.Cannistra LB, O’Malley CJ, Balady GJ. Comparison of outcome of cardiac rehabilitation in black women and white women. Am J Cardiol 1995;75(14):890–893. [DOI] [PubMed] [Google Scholar]
- 33.Weingarten MN, Salz KA, Thomas RJ, Squires RW. Rates of enrollment for men and women referred to outpatient cardiac rehabilitation. J Cardiopulm Rehabil Prev 2011;31(4):217–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schultz WM, Kelli HM, Lisko JC, et al. Socioeconomic Status and Cardiovascular Outcomes: Challenges and Interventions. Circulation 2018;137(20):2166–2178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Patil S, Shah M, Patel B, Agarwal M, Ram P, Alla VM. Readmissions Among Patients Admitted With Acute Decompensated Heart Failure Based on Income Quartiles. Mayo Clin Proc 2019;94(10):1939–1950. [DOI] [PubMed] [Google Scholar]
- 36.Shanmugasegaram S, Oh P, Reid RD, McCumber T, Grace SL. Cardiac rehabilitation barriers by rurality and socioeconomic status: a cross-sectional study. Int J Equity Health 2013;12:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mead H, Ramos C, Grantham SC. Drivers of Racial and Ethnic Disparities in Cardiac Rehabilitation Use: Patient and Provider Perspectives. Med Care Res Rev 2016;73(3):251–282. [DOI] [PubMed] [Google Scholar]
- 38.Gaalema DE, Higgins ST, Shepard DS, Suaya JA, Savage PD, Ades PA. State-by-state variations in cardiac rehabilitation participation are associated with educational attainment, income, and program availability. J Cardiopulm Rehabil Prev 2014;34(4):248–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bachmann JM, Huang S, Gupta DK, et al. Association of Neighborhood Socioeconomic Context With Participation in Cardiac Rehabilitation. J Am Heart Assoc 2017;6(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shanmugasegaram S, Gagliese L, Oh P, et al. Psychometric validation of the cardiac rehabilitation barriers scale. Clin Rehabil 2012;26(2):152–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Curnier DY, Savage PD, Ades PA. Geographic distribution of cardiac rehabilitation programs in the United States. J Cardiopulm Rehabil 2005;25(2):80–84. [DOI] [PubMed] [Google Scholar]
- 42.Johnson JE, Weinert C, Richardson JK. Rural residents’ use of cardiac rehabilitation programs. Public Health Nurs 1998;15(4):288–296. [DOI] [PubMed] [Google Scholar]
- 43.Ayanian JZ, Udvarhelyi IS, Gatsonis CA, Pashos CL, Epstein AM. Racial differences in the use of revascularization procedures after coronary angiography. JAMA 1993;269(20):2642–2646. [PubMed] [Google Scholar]
- 44.Angraal S, Khera R, Wang Y, et al. Sex and Race Differences in the Utilization and Outcomes of Coronary Artery Bypass Grafting Among Medicare Beneficiaries, 1999–2014. J Am Heart Assoc 2018;7(14). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Koehler Hildebrandt AN, Hodgson JL, Dodor BA, Knight SM, Rappleyea DL. Biopsychosocial-Spiritual Factors Impacting Referral to and Participation in Cardiac Rehabilitation for African American Patients: A SYSTEMATIC REVIEW. J Cardiopulm Rehab Prev 2016;36(5):320–330. [DOI] [PubMed] [Google Scholar]
- 46.Buchmueller TC, Levinson ZM, Levy HG, Wolfe BL. Effect of the Affordable Care Act on Racial and Ethnic Disparities in Health Insurance Coverage. Am J Public Health 2016;106(8):1416–1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cooper LA, Roter DL, Carson KA, et al. The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J Public Health 2012;102(5):979–987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brady S, Purdham D, Oh P, Grace S. Clinical and sociodemographic correlates of referral for cardiac rehabilitation following cardiac revascularization in Ontario. Heart Lung 2013;42(5):320–325. [DOI] [PubMed] [Google Scholar]
- 49.Vanzella LM, Oh P, Pakosh M, Ghisi GLM. Barriers to Cardiac Rehabilitation in Ethnic Minority Groups: A Scoping Review. J Immig Minor Health 2021;23(4):824–839. [DOI] [PubMed] [Google Scholar]
- 50.Churchwell K, Elkind MSV, Benjamin RM, et al. Call to Action: Structural Racism as a Fundamental Driver of Health Disparities: A Presidential Advisory From the American Heart Association. Circulation 2020;142(24):e454–e468. [DOI] [PubMed] [Google Scholar]
- 51.Cossette S, Maheu-Cadotte MA, Mailhot T, et al. Sex- and Gender-Related Factors Associated With Cardiac Rehabilitation Enrollment: A SECONDARY ANALYSIS AMONG SYSTEMATICALLY REFERRED PATIENTS. J Cardiopulm Rehabil Prev 2019;39(4):259–265. [DOI] [PubMed] [Google Scholar]
- 52.Supervia M, Medina-Inojosa JR, Yeung C, et al. Cardiac Rehabilitation for Women: A Systematic Review of Barriers and Solutions. Mayo Clin Proc 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Koehler Hildebrandt AN, Hodgson JL, Dodor BA, Knight SM, Rappleyea DL. Biopsychosocial-Spiritual Factors Impacting Referral to and Participation in Cardiac Rehabilitation for African American Patients: A SYSTEMATIC REVIEW. J Cardiopulm Rehabil Prev 2016;36(5):320–330. [DOI] [PubMed] [Google Scholar]
- 54.Bennett KK, Smith AJ, Harry KM, et al. Multilevel Factors Predicting Cardiac Rehabilitation Attendance and Adherence in Underserved Patients at a Safety-Net Hospital. J Cardiopulm Rehabil Prev 2019;39(2):97–104. [DOI] [PubMed] [Google Scholar]
- 55.Bennett KK, Smith AJ, Harry KM, et al. Multilevel Factors Predicting Cardiac Rehabilitation Attendance and Adherence in Underserved Patients at a Safety-Net Hospital. J Cardiopulmon Rehab Prev 2019;39(2):97–104. [DOI] [PubMed] [Google Scholar]
- 56.Kangovi S, Barg FK, Carter T, et al. Challenges faced by patients with low socioeconomic status during the post-hospital transition. J Gen Intern Med 2014;29(2):283–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Darrat I, Tam S, Boulis M, Williams AM. Socioeconomic Disparities in Patient Use of Telehealth During the Coronavirus Disease 2019 Surge. JAMA Otolaryngology–Head & Neck Surgery 2021;147(3):287–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Shaw J, Brewer LC, Veinot T. Recommendations for Health Equity and Virtual Care Arising From the COVID-19 Pandemic: Narrative Review. JMIR Form Res 2021;5(4):e23233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Williams DR, Cooper LA. COVID-19 and Health Equity-A New Kind of “Herd Immunity”. JAMA 2020;323(24):2478–2480. [DOI] [PubMed] [Google Scholar]
- 60.Owen WF Jr., Carmona R, Pomeroy C. Failing Another National Stress Test on Health Disparities. JAMA 2020;323(19):1905–1906. [DOI] [PubMed] [Google Scholar]
- 61.Green H, Fernandez R, MacPhail C. The social determinants of health and health outcomes among adults during the COVID-19 pandemic: A systematic review. Public Health Nurs 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Grace SL, Russell KL, Reid RD, et al. Effect of cardiac rehabilitation referral strategies on utilization rates: a prospective, controlled study. Arch Intern Med 2011;171(3):235–241. [DOI] [PubMed] [Google Scholar]
- 63.Grace SL, Leung YW, Reid R, et al. The role of systematic inpatient cardiac rehabilitation referral in increasing equitable access and utilization. J Cardiopulm Rehabil Prev 2012;32(1):41–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gravely-Witte S, Leung YW, Nariani R, et al. Effects of cardiac rehabilitation referral strategies on referral and enrollment rates. Nat Rev Cardiol 2010;7(2):87–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Benz Scott L, Gravely S, Sexton TR, Brzostek S, Brown DL. Effect of patient navigation on enrollment in cardiac rehabilitation. JAMA Intern Med 2013;173(3):244–246. [DOI] [PubMed] [Google Scholar]
- 66.Kangovi S, Mitra N, Grande D, Huo H, Smith RA, Long JA. Community Health Worker Support for Disadvantaged Patients With Multiple Chronic Diseases: A Randomized Clinical Trial. Am J Public Health 2017;107(10):1660–1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Choudhry NK, Avorn J, Glynn RJ, et al. Full coverage for preventive medications after myocardial infarction. New Engl J M ed 2011;365(22):2088–2097. [DOI] [PubMed] [Google Scholar]
- 68.Gaalema DE, Elliott RJ, Savage PD, et al. Financial Incentives to Increase Cardiac Rehabilitation Participation Among Low-Socioeconomic Status Patients: A Randomized Clinical Trial. JACC Heart failure 2019;7(7):537–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Thomas RJ, Beatty AL, Beckie TM, et al. Home-Based Cardiac Rehabilitation: A Scientific Statement From the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. J Am Coll Cardiol 2019;74(1):133–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Drwal KR, Forman DE, Wakefield BJ, El Accaoui RN. Cardiac Rehabilitation During COVID-19 Pandemic: Highlighting the Value of Home-Based Programs. Telemed J E Health 2020;26(11):1322–1324. [DOI] [PubMed] [Google Scholar]
- 71.Fleg JL, Keteyian SJ, Peterson PN, et al. Increasing Use of Cardiac and Pulmonary Rehabilitation in Traditional and Community Settings: OPPORTUNITIES TO REDUCE HEALTH CARE DISPARITIES. J Cardiopulm Rehabil Prevent 2020;40(6):350–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ramachandran HJ, Jiang Y, Tam WWS, Yeo TJ, Wang W. Effectiveness of home-based cardiac telerehabilitation as an alternative to Phase 2 cardiac rehabilitation of coronary heart disease: a systematic review and meta-analysis. Eur J Prev Cardiol 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lear SA, Singer J, Banner-Lukaris D, et al. Randomized trial of a virtual cardiac rehabilitation program delivered at a distance via the Internet. Circ Cardiovasc Qual Outcomes 2014;7(6):952–959. [DOI] [PubMed] [Google Scholar]
- 74.Lounsbury P, Elokda AS, Gylten D, Arena R, Clarke W, Gordon EEI. Text-messaging program improves outcomes in outpatient cardiovascular rehabilitation. Int J Cardiol Heart Vasc 2015;7:170–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Extension of COVID-19 Pandemic extends Opportunities for Delivery of Cardiac and Pulmonary Rehabilitation [press release] 2020. [Google Scholar]
- 76.Mitchell UA, Chebli PG, Ruggiero L, Muramatsu N. The Digital Divide in Health-Related Technology Use: The Significance of Race/Ethnicity. Gerontologist 2019;59(1):6–14. [DOI] [PubMed] [Google Scholar]
- 77.Ortega G, Rodriguez JA, Maurer LR, et al. Telemedicine, COVID-19, and disparities: Policy implications. Health Policy Technol 2020;9(3):368–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Brewer LC, Kaihoi B, Schaepe K, et al. Patient-perceived acceptability of a virtual world-based cardiac rehabilitation program. Digit Health 2017;3:2055207617705548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wongvibulsin S, Habeos EE, Huynh PP, et al. Digital Health Interventions for Cardiac Rehabilitation: Systematic Literature Review. J Med Internet Res 2021;23(2):e18773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hutchinson K. Community-Based Cardiac Rehabilitation: A YMCA Model. ACSM’s Health & Fit J 2006;10(6):21–27. [Google Scholar]
- 81.Brewer LC, Hayes SN, Jenkins SM, et al. Improving Cardiovascular Health Among African-Americans Through Mobile Health: the FAITH! App Pilot Study. J Gen Intern Med 2019;34(8):1376–1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Brewer LC, Hayes SN, Caron AR, et al. Promoting cardiovascular health and wellness among African-Americans: Community participatory approach to design an innovative mobile-health intervention. PLoS One 2019;14(8):e0218724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Takeshita J, Wang S, Loren AW, et al. Association of Racial/Ethnic and Gender Concordance Between Patients and Physicians With Patient Experience Ratings. JAMA Netw Open 2020;3(11):e2024583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Midence L, Mola A, Terzic CM, Thomas RJ, Grace SL. Ethnocultural Diversity in Cardiac Rehabilitation. J Cardiopulm Rehabil Prev 2014;34(6):437–444. [DOI] [PubMed] [Google Scholar]
- 85.McGregor B, Belton A, Henry TL, Wrenn G, Holden KB. Improving Behavioral Health Equity through Cultural Competence Training of Health Care Providers. Ethn Dis 2019;29(Suppl 2):359–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Qt Capers, Johnson A, Berlacher K, Douglas PS. The Urgent and Ongoing Need for Diversity, Inclusion, and Equity in the Cardiology Workforce in the United States. J Am Heart Assoc 2021;10(6):e018893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Peeler Katherine, Peeler Crandall, Betancourt Joseph, et al. Equity Metrics Should Be An Essential Component Of Hospital Rankings. Health Affairs Blog, March 19, 2021. 2021. [Google Scholar]
- 88.Brewer LC, Fortuna KL, Jones C, et al. Back to the Future: Achieving Health Equity Through Health Informatics and Digital Health. JMIR Mhealth Uhealth 2020;8(1):e14512. [DOI] [PMC free article] [PubMed] [Google Scholar]


