Abstract
Purpose
Dry eye is a multifactorial ocular surface disease (DED) characterized by a loss of tear film homeostasis, which is widely associated with alterations in mental health. Problematic internet use (PIU) is defined as the feeling of concern about using this tool irresistibly, for longer periods than usual, accompanied by anguish that results from not doing so without reaching mania or hypomania behaviors. Both PIU and DED present a theoretical link; however, there are no published studies that report its relationship with problematic internet use. Therefore, this study aims to determine the association between PIU and symptomatic DED in Peruvian medical students.
Patients and Methods
Analytical cross-sectional study that included human medical students from Peru. For the measurement of main variables, the Ocular Surface Disease Index (OSDI) and the Internet Addiction Test (IAT) were used. To study their relationship, the Poisson regression analysis was used, we consider a p-value <0.05 as significant.
Results
Data from 844 medical students were analyzed, 35.7% male and 64.3% female, with an average age of 21.8 ± 3.3 years. Likewise, the prevalence of symptomatic DED was 70.9%, and the internet’s controlled use was 85.3%. In the analysis adjusted for symptomatic DED, the men showed significant differences in the controlled use of the internet (p <0.003), of which those who had PIU, 50% had severe symptomatic DED, as well as 80% of those addicted to the internet. The adjusted model showed that the PIU increases the prevalence of symptomatic DED in men (PR = 1.17, 95% CI: 1.06–1.29); however, in women, no association was found between both variables.
Conclusion
PIU and symptomatic DED showed a significant association in male medical students from Peru.
Keywords: mental health, screen time, psychological stresses, ocular surface
Introduction
Dry eye is a multifactorial disease of the ocular surface characterized by a loss of tear film homeostasis. Besides, it is accompanied by ocular symptoms, in which instability, hyperosmolarity of the tear film, inflammation, damage to the ocular surface, and neurosensory abnormalities play an etiological role.1 The symptoms described by the patient are the basis for the diagnosis of dry eye.2 Prevalence rates vary about the place, in Asian countries, they are 50%, and in Europe 6%.3 In Latin America there are few studies, one of them being in Chile where 81%,4 was reported and in Brazil 34.4%,5 however, in Peru, it has not been investigated.
Around the world, there are more than 7 billion people who are Internet users.6 This tool has both benefits and harms, one of them being Problematic Internet Use, defined as the concern to use this tool irresistibly for longer periods than usual, as well as the presence of anguish that results from not doing it without arriving at behaviors of mania or hypomania.7 The university population is one of the most susceptible to presenting PIU,8 which have prevalence rates that differ according to place, being in Spain 6%, China 8.4%, Colombia 12%, and in Peru 68.4%.9–12
Additionally, people with PIU have emotional dysregulation, lack of confidence, and social support.13 These alterations generate a state of psychological stress that through the release of inflammatory cytokines such as IL-1β, IL-6 and IL-8 generate the instability of the tear film, as well as the suppression of tear production, generating dry eye disease.14,15 The aforementioned would indicate the association between these variables, however, as far as we know, there are no investigations that report this relationship. In addition, considering that due to the COVID-19 pandemic, we remain in social isolation, which generates an active use of the internet, which generates the predisposition to develop our study variables.16 Therefore, our objective is to determine the association between PIU and symptomatic DED in medical students from Peru.
Materials and Methods
General Characteristics of the Study
This cross-sectional analytical study collected data from 1203 Peruvian medical students, belonging to the 38 faculties of human medicine affiliated to the Peruvian Student Medical Society (SOCIMEP). The sending of the questionnaires began the 7th of December and ended 12th of February, 2021. The type of sampling carried out was non-probabilistic for convenience. Students over 18 years of age were included and excluded those with Sjögren’s syndrome, refractive surgery procedures, glaucoma, uncorrected ametropia, use of contact lenses, active ocular surface disease, previous psychiatric illnesses, or who had this previous diagnosis.
Before the execution of the study, we had the approval of the Research Ethics Committee of the Universidad Peruana Union (Number 2020-CEUPeU-00029). Student participation was voluntary, manifested in the informed consent on the page before the data collection instrument.
Data Collection Instrument
The data were collected in a self-administered questionnaire through the Google Forms platform. As DED is a predominantly symptomatic pathology, the Ocular Surface Disease Index (OSDI) was used to determine the presence of symptomatic DED, which consists of 12 items divided into three dimensions: consequences of Internet use, cognitive-emotional, and time control; measured by Likert scale from 0 to 4 points. It has a Cronbach’s alpha of 0.91. Symptomatic DED was considered a score greater than or equal to 13 points, the degree being mild from 13 to 22 points, moderate from 23 to 32 points, and severe from 33 to 100 points.4 As for the PIU, it was evaluated through the Internet Addiction Test (IAT), which consists of 20 items, and has values from 0 to 5 on a Likert scale, with a Cronbach’s alpha of 0.77. To determine the presence of PIU, a score greater than or equal to 50 is required, and for internet addiction (IA) a score greater than or equal to 80.11
Other characteristics of the students that were recorded in the instrument were demographic data (age and sex), frequency of smoking or alcohol intake (every day, week, month, or year), variables to add with the development of symptoms, including screen exposure time per day, intermittent Internet rest (time elapsed from the start of Internet use to the first rest of Internet use), use of blue-light blocking spectacle lenses, use of screen light filter, display brightness (dull, very dull, bright, very bright), screen viewing distance (eye-screen distance in centimeters), room lighting (dark, low light, illuminated, very illuminated), most used device (phone, PC or laptop, tablet, television),17 and the practice of 20-20-20 rule (every 20 minutes, a 20-second break is taken, focusing with the eyes on an object at least 20 feet away).18
Data Analysis
The statistical analysis was carried out using the programming language R version 4.0.2. (R Foundation for Statistical Computing, Vienna, Austria; http://www.R-project.org). The variables were distributed in graphs and tables with absolute and relative frequencies (%) for categorical variables, and means and standard deviation (±SD) for numerical variables. For comparative analysis of symptomatic DED and non-symptomatic DED groups by sex, Mann Whitney U or Chi-square test depending on the distribution of the variables. Finally, to determine the association of PIU to symptomatic DED, Poisson regression models were performed with robust variance in the overall population and stratified by sex. The first model was unadjusted, and the second model considering the adjusted by potential confounders. In all regressions calculated the prevalence ratios (PR) with their 95% confidence intervals (CI95%). A p<0.05 (α =0.05) was considered statistically significant.
Results
General Characteristics of the Participants
A sample of 1203 medical students was obtained, which after applying the exclusion criteria left 844, of which 301 (35.7%) were male and 543 (64.3%) were female, with an average age of 21.8 ± 3.3 years. Some characteristics of this population reveal an important frequency of unsuitable habits to visual health, as >6 hours connect to the internet (66.7%), not use blue-light blocking spectacle lenses (48.7%), set brilliant screen (41%), and maintain <40 cm of distance to the screen (56.9%), some of these variables presented significantly statistical differences by sex. On the other hand, the prevalence of symptomatic DED was 70.9% and uncontrolled use of the internet was 14.7% in medical students without significant differences by sex (Table 1).
Table 1.
General Characteristics of Population of Study
| Variables | Overall | Men | Women | p |
|---|---|---|---|---|
| (n=844) | (n=301) | (n=543) | ||
| Age (years) | 21.8 ± 3.3 | 22.2 ± 4.0 | 21.6 ± 2.9 | 0.005 |
| Frequency of alcohol intake | ||||
| Each year | 63 (7.46%) | 26 (8.64%) | 37 (6.81%) | 0.002 |
| Each month | 99 (11.7%) | 47 (15.6%) | 52 (9.58%) | |
| Every week | 69 (8.18%) | 29 (9.63%) | 40 (7.37%) | |
| No alcohol consumption | 613 (72.6%) | 199 (66.1%) | 414 (76.2%) | |
| Frequency of smoking | ||||
| Each month | 25 (2.96%) | 12 (3.99%) | 13 (2.39%) | 0.056 |
| Every week | 6 (0.71%) | 5 (1.66%) | 1 (0.18%) | |
| Every day | 1 (0.12%) | 0 (0.00%) | 1 (0.18%) | |
| Non-smoker | 812 (96.2%) | 284 (94.4%) | 528 (97.2%) | |
| Screen exposure time per day | ||||
| <3 h | 17 (2.0) | 10 (3.3) | 7 (1.3) | 0.022 |
| 3–6 h | 264 (31.3) | 105 (34.9) | 159 (29.3) | |
| >6 h | 563 (66.7) | 186 (61.8) | 377 (69.4) | |
| Intermittent Internet rest | ||||
| <3h | 535 (63.4%) | 201 (66.8%) | 334 (61.5%) | 0.197 |
| 3–5h | 111 (13.2%) | 38 (12.6%) | 73 (13.4%) | |
| >5h | 19 (2.25%) | 6 (1.99%) | 13 (2.39%) | |
| No rest | 179 (21.2%) | 56 (18.6%) | 123 (22.7%) | |
| Use of blue-light blocking spectacle lenses | ||||
| Yes | 433 (51.3) | 140 (46.5) | 293 (54.0) | 0.045 |
| No | 411 (48.7) | 161 (53.5) | 250 (46.0) | |
| Use of screen light filter | ||||
| Yes | 275 (32.6) | 107 (35.5) | 168 (30.9) | 0.196 |
| No | 569 (67.4) | 194 (64.5) | 375 (69.1) | |
| Display brightness | ||||
| Dull | 67 (7.9) | 18 (6.0) | 49 (9.0) | 0.068 |
| Very dull | 391 (46.3) | 130 (43.2) | 261 (48.1) | |
| Bright | 346 (41.0) | 134 (44.5) | 212 (39.0) | |
| Very bright | 40 (4.7) | 19 (6.3) | 21 (3.9) | |
| Display viewing distance | ||||
| < 40 cm | 480 (56.9) | 134 (44.5) | 346 (63.7) | <0.001 |
| 40–76 cm | 343 (40.6) | 159 (52.8) | 184 (33.9) | |
| >76 cm | 21 (2.5) | 8 (2.7) | 13 (2.4) | |
| Room lighting | ||||
| Dark | 17 (2.0) | 5 (1.7) | 12 (2.2) | 0.24 |
| Low light | 176 (20.9) | 71 (23.6) | 105 (19.3) | |
| Illuminated | 537 (63.6) | 192 (63.8) | 345 (63.5) | |
| Very illuminated | 114 (13.5) | 33 (11.0) | 81 (14.9) | |
| Most used device | ||||
| Phone | 446 (52.8%) | 154 (51.2%) | 292 (53.8%) | 0.832 |
| PC or laptop | 387 (45.9%) | 143 (47.5%) | 244 (44.9%) | |
| Tablet | 10 (1.18%) | 4 (1.33%) | 6 (1.10%) | |
| Television | 1 (0.12%) | 0 (0.00%) | 1 (0.18%) | |
| PIU | ||||
| Controlled | 720 (85.3) | 248 (82.4) | 472 (86.9) | 0.093 |
| Uncontrolled | 124 (14.7) | 53 (17.6) | 71 (13.1) | |
| SDED | ||||
| Yes | 598 (70.9) | 201 (66.8) | 397 (73.1) | 0.063 |
| No | 246 (29.1) | 100 (33.2) | 146 (26.9) |
Note: Data shown as mean ± SD or absolute frequency (%).
Abbreviations: PIU, problematic internet use; SDED, symptomatic dry eye disease.
Characteristics of Participants by Dry Eye Disease
The study population was stratified into symptomatic DED and non-symptomatic DED groups by sex. When comparing the characteristics of symptomatic DED and non-symptomatic DED groups, we found that some variables in men as use of blue-light blocking spectacle lenses, the use of light screen filter, display brightness, and the severity of PIU presented significant differences in symptomatic DED and non-symptomatic DED groups. However, all variables compared in women did not present significantly statistical differences in symptomatic DED and non-symptomatic DED groups (Table 2). To understand this result, we focus on the distribution of symptomatic DED and PIU.
Table 2.
Characteristics of the Population by Symptomatic Dry Eye Disease and Sex
| Variables | Men | Women | ||||
|---|---|---|---|---|---|---|
| Non-SDED (n=100) | SDED | p | No-SDED (n=146) | SDED | p | |
| (n=201) | (n=397) | |||||
| Age (years) | 22.0 ± 3.7 | 22.3 ± 4.1 | 0.617 | 21.3 ± 2.6 | 21.6 ± 3.0 | 0.242 |
| Frequency of alcohol intake | ||||||
| Each year | 10 (38.5%) | 16 (61.5%) | 0.506 | 8 (21.6%) | 29 (78.4%) | 0.733 |
| Each month | 12 (25.5%) | 35 (74.5%) | 15 (28.8%) | 37 (71.2%) | ||
| Every week | 8 (27.6%) | 21 (72.4%) | 13 (32.5%) | 27 (67.5%) | ||
| No alcohol consumption | 70 (35.2%) | 129 (64.8%) | 110 (26.6%) | 304 (73.4%) | ||
| Frequency of smoking | ||||||
| Each month | 4 (33.3%) | 8 (66.7%) | 0.485 | 3 (23.1%) | 10 (76.9%) | 0.573 |
| Every week | 3 (60.0%) | 2 (40.0%) | 0 (0.00%) | 1 (100%) | ||
| Every day | 0 (0.00%) | 0 (0.00%) | 1 (100%) | 0 (0.00%) | ||
| Non-smoker | 93 (32.7%) | 191 (67.3%) | 142 (26.9%) | 386 (73.1%) | ||
| Screen exposure time per day | ||||||
| <3 h | 4 (40.0) | 6 (60.0) | 0.895 | 2 (28.6) | 5 (71.4) | 0.655 |
| 3–6 h | 35 (33.3) | 70 (66.7) | 47 (29.6) | 112 (70.4) | ||
| >6 h | 61 (32.8) | 125 (67.2) | 97 (25.7) | 280 (74.3) | ||
| Intermittent Internet rest | ||||||
| <3h | 71 (35.3%) | 130 (64.7%) | 0.076 | 92 (27.5%) | 242 (72.5%) | 0.987 |
| 3–5h | 16 (42.1%) | 22 (57.9%) | 19 (26.0%) | 54 (74.0%) | ||
| >5h | 2 (33.3%) | 4 (66.7%) | 3 (23.1%) | 10 (76.9%) | ||
| No rest | 11 (19.6%) | 45 (80.4%) | 32 (26.0%) | 91 (74.0%) | ||
| Use of blue-light blocking spectacle lenses | ||||||
| Yes | 35 (25.0) | 105 (75.0) | 0.007 | 69 (23.5) | 224 (76.5) | 0.072 |
| No | 65 (40.4) | 96 (59.6) | 77 (30.8) | 173 (69.2) | ||
| Use of screen light filter | ||||||
| Yes | 45 (42.1) | 62 (57.9) | 0.022 | 49 (29.2) | 119 (70.8) | 0.486 |
| No | 55 (28.4) | 139 (71.6) | 97 (25.9) | 278 (74.1) | ||
| Display brightness | ||||||
| Dull | 9 (50.0) | 9 (50.0) | 0.025 | 15 (30.6) | 34 (69.4) | 0.103 |
| Very dull | 50 (38.5) | 80 (61.5) | 81 (31.0) | 180 (69.0) | ||
| Bright | 39 (29.1) | 95 (70.9) | 46 (21.7) | 166 (78.3) | ||
| Very bright | 2 (10.5) | 17 (89.5) | 4 (19.0) | 17 (81.0) | ||
| Display viewing distance | ||||||
| < 40 cm | 46 (34.3) | 88 (65.7) | 0.518 | 85 (24.6) | 261 (75.4) | 0.222 |
| 40–76 cm | 50 (31.4) | 109 (68.6) | 56 (30.4) | 128 (69.6) | ||
| >76 cm | 4 (50.0) | 4 (50.0) | 5 (38.5) | 8 (61.5) | ||
| Room lighting | ||||||
| Dark | 1 (20.0) | 4 (80.0) | 0.231 | 2 (16.7) | 10 (83.3) | 0.79 |
| Low light | 25 (35.2) | 46 (64.8) | 26 (24.8) | 79 (75.2) | ||
| Illuminated | 68 (35.4) | 124 (64.6) | 95 (27.5) | 250 (72.5) | ||
| Very illuminated | 6 (18.2) | 27 (81.8) | 23 (28.4) | 58 (71.6) | ||
| Most used device: | ||||||
| Phone | 53 (34.4%) | 101 (65.6%) | 0.886 | 90 (30.8%) | 202 (69.2%) | 0.082 |
| PC or laptop | 46 (32.2%) | 97 (67.8%) | 54 (22.1%) | 190 (77.9%) | ||
| Tablet | 1 (25.0%) | 3 (75.0%) | 2 (33.3%) | 4 (66.7%) | ||
| Television | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | 1 (100%) | ||
| PIU | ||||||
| Controlled | 92 (37.1) | 156 (62.9) | 0.003 | 132 (28.0) | 340 (72.0) | 0.188 |
| Uncontrolled | 8 (15.1) | 45 (84.9) | 14 (19.7) | 57 (80.3) | ||
Note: Data shown as mean ± SD or absolute frequency (%).
Abbreviations: PIU, problematic internet use; SDED, symptomatic dry eye disease.
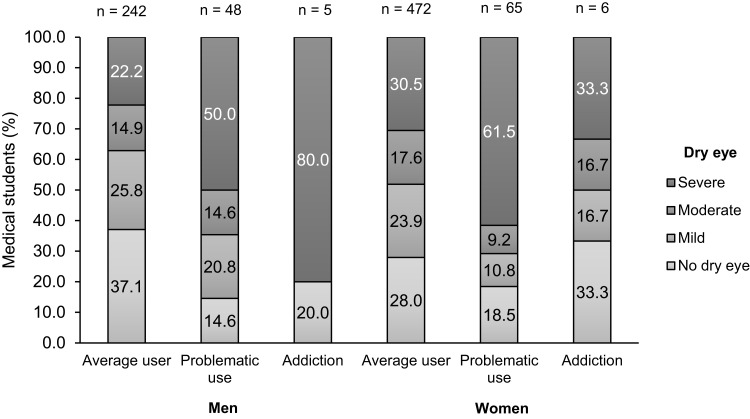
Symptomatic DED and PIU severity groups showed different distribution patterns in both sexes. In men, more severity of PIU (addiction) presented a high frequency of severe symptomatic DED (80%). However, in women paradoxically the more severe class of PIU (addiction) presented the same frequency of severe symptomatic DED as the lowest severity class of PIU (average user) (Figure 1). These differences must take account in future research.
Figure 1.
Percentage of symptomatic DED by degree of intensity in people with and without PIU or IA.
Association of Internet Use and Dry Eye Disease
To determine the association between PIU and symptomatic DED, Poisson regression models were performed (Table 3). The non-adjusted models showed that in the overall population (PR = 1.19, 95% CI: 1.08–1.31) and men (PR = 1.35, 95% CI: 1.16–1.57) increase 19% and 35% respectively, the prevalence of symptomatic DED in uncontrolled use of internet compared to controlled use of the internet. In the same way, the adjusted models presented a significant association of PIU to symptomatic DED in the overall population (PR = 1.17, 95% CI: 1.06–1.29) and men (PR = 1.27, 95% CI: 1.09–1.49). The regression models in women no-showed the association of PIU to symptomatic DED in the bivariate or multivariable analysis. Men with uncontrolled use of the internet in this study have more probability of symptomatic DED.
Table 3.
Poisson Regression Models of Problematic Use of Internet and Symptomatic Dry Eye Disease in Medical Students
| Symptomatic DED | PR | (CI95%) | p-value |
|---|---|---|---|
| Overall | |||
| Model 1a | 1.19 | (1.08–1.31) | 0.000* |
| Model 2b | 1.17 | (1.06–1.29) | 0.002* |
| Men | |||
| Model 1a | 1.35 | (1.16–1.57) | 0.000* |
| Model 2c | 1.27 | (1.09–1.49) | 0.002* |
| Women | |||
| Model 1a | 1.11 | (0.98–1.27) | 0.098 |
| Model 2c | 1.12 | (0.99–1.28) | 0.081 |
Notes: aNon-adjusted. bAdjusted by sex, age, frequency of smoking and alcohol intake, intermittent Internet rest, screen time per day. cAdjusted by age, frequency of smoking and alcohol intake, intermittent Internet rest, screen time per day. *p<0.05, statistically significant.
Discussion
Symptoms of DED affect tens of millions of people around the world.3 One of the causes being the excessive use of screens and the internet, which have been very pronounced in university students.19
In this population of Peruvian medical students, we found a 70.9% prevalence of symptomatic DED, compared to a study in Brazil, where only 34.4% of the students suffered from it.5 This notorious difference may be due to the social confinement resulting from the COVID-19 pandemic, and the migration from university education to digital remote teaching, which has generated greater exposure to the use of the internet.20
On the other hand, the prevalence of PIU in students was similar to a study carried out in Colombia where 12% had problems with the use of the internet,11 while a study in Spain found a prevalence of 6.04%.9 These findings are attributed to unlimited access to devices without adequate control for the student’s own needs.
We also observed in this study that most of the students remained in front of a screen for more than six hours a day. Similar results were obtained in Turkish University students, who spent more than four hours a day in front of a screen.21 Despite these results, in the associative analysis, screen exposure time per day was not associated with symptomatic DED. This is striking since most of them did not practice the 20-20-20 rule, and it would be theoretically expected that students would present DED as a consequence of this.18 This is a finding that contradicts the literature which should be studied in future research focused on this population.22
Regarding the frequency of smoking or alcohol intake had no relation with symptomatic DED, similar to an investigation which was conducted on African medical students.23 However, other studies considered both as risk factors because they provoke tear film instability.24,25 The difference could be because, in our study, most of the medical students do not drink alcohol or drink it infrequently; a previous study reported that these harmful habits are not usually very prevalent in medical students.25 Despite this, remains to be clarified which could be the physiopathology mechanism involved.
Concerning room illumination, there was no association with symptomatic DED. The aforementioned contrasts with other studies which reported that a bad illumination has a relation with the apparition of symptomatology compatible with DED.26 This is probably due to a factor that influences independently of illumination, the activity of using video terminal screens.27
Besides, the use of blue-light blocking spectacle lenses, the screen light filter, and the diminution of bright were associated with symptomatic DED in men. From them, the blue light has been associated with corneal damage and consequently with the apparition of dry eye.27 To find in our study a high prevalence of symptomatic DED in men who use blue-light blocking spectacle lenses, make us think that glasses protection is not effective to prevent DED,28 or these glasses, in reality, had no protection for blue light. However, for a better understanding, it needs to be investigated in future work.
The most relevant finding of the study was that PIU was associated with symptomatic DED in male medical students. Similarly, men who had PIU had a higher percentage of symptomatic DED, finding severity in those who manifested a picture greater than PIU (IA). Currently, these results differ from the majority of mental health research related to DED with both emotionally and psychiatric area, which has reported associations and higher prevalence predominantly in women as a result of hormonal imbalance.29–31 In addition, the use of the internet by women is more focused on social networks, unlike men who use video games as social support.9,32 The aforementioned can trigger depression and anxiety that leads to psychological stress, which suppresses the production of the lacrimal gland leads to DED, and manifests itself symptomatically.14,33,34 However, more research is required to determine the factors that influence this association.
This study has some limitations, among them virtually sending the self-reported questionnaire did not allow the physical evaluation of complementary tests such as the Schirmer test strips, the measurement of the tear film break time, and blinking. In addition, anxiety, depression, sleep patterns, and others related to the activities carried out during the Internet use were not considered; on the other hand, the causality of the variables studied was not evaluated. Within the strengths, to our knowledge, this is the first multicenter study carried out in medical students of all years of studies and different regions of Peru (coast, mountains, and jungle). In addition, the analysis performed for the study variables was adjusted for potential confounders.
The Internet has become the most popular medium used by the population, studies show that the percentage of students using the Internet has increased significantly,35 and point out that Internet access is closely related to problematic use, affecting the correct development of daily life by reducing study time and/or obligations.36,37 In addition, visual conditions have acquired critical importance for health, demonstrating the PIU to have a great impact on medical students, being influential in the generation of symptomatic DED. Currently, due to the aforementioned, PIU has become a public health problem, which if left untreated can generate symptomatic DED. Therefore, it deserves institutional policy implementations that incorporate strategies to promote mental health, as well as ocular health, focused on education of good visual habits and self-control, to improve the correct functioning and tear stability concerning the ocular surface, which will consequently prevent symptomatic DED.
Conclusion
In conclusion, although women are physiologically predisposed to symptomatic DED, our results show a significant association with PIU only in male medical students due to their tendency to PIU. The relationship is probably mediated by inflammatory mechanisms induced by psychological stress shared by the main variables. In contrast to the literature, screen exposure time per day was not associated with symptomatic DED, even though most did not practice the 20-20-20 rule. Result contradicting the literature, which should be studied in this population for future research. There are still factors to be studied, but due to these results, we emphasize that strategies of good visual habits and self-control of Internet use should be promoted in students.
Acknowledgments
We thank the scientific societies of each Peruvian university associated with SOCIMEP for their support in distributing the surveys to the students, as well as our future colleagues who voluntarily filled out the instrument, thus contributing to the development of this work. We also thank Dr. Marco Galarza Pérez for his support in the orientation and correction of the article.
Funding Statement
There is no funding to report.
Data Sharing Statement
The original data used to support the findings of this study are available from the corresponding authors upon request.
Ethical Statement
All procedures were performed in accordance with the 1964 Helsinki declaration and its later amendments.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
- 1.Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15(3):276–283. doi: 10.1016/j.jtos.2017.05.008 [DOI] [PubMed] [Google Scholar]
- 2.Williamson JF, Huynh K, Weaver MA, Davis RM. Perceptions of dry eye disease management in current clinical practice. Eye Contact Lens. 2014;40(2):111–115. doi: 10.1097/icl.0000000000000020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stapleton F, Alves M, Bunya VY, et al. TFOS DEWS II epidemiology report. Ocul Surf. 2017;15(3):334–365. doi: 10.1016/j.jtos.2017.05.003 [DOI] [PubMed] [Google Scholar]
- 4.Traipe L, Gauro F, Goya MC, et al. Adaptación cultural y validación del cuestionario Ocular Surface Disease Index en una población chilena [Validation of the Ocular Surface Disease Index Questionnaire for Chilean patients]. Revista médica de Chile. 2020;148(2):187–195. Spanish. doi: 10.4067/s0034-98872020000200187 [DOI] [PubMed] [Google Scholar]
- 5.Yang I, Sacho IBI, Lopes GA, et al. Dry eye prevalence and main risk factors among undergraduate students in Brazil. Invest Ophthalmol Vis Sci. 2020;61(7):329. [Google Scholar]
- 6.Internet World Stats. Internet user distribution in the world; 2021. Available from: https://www.internetworldstats.com/stats.htm. Accessed October 21, 2021.
- 7.Shapira NA, Lessig MC, Goldsmith TD, et al. Problematic internet use: proposed classification and diagnostic criteria. Depress Anxiety. 2003;17(4):207–216. doi: 10.1002/da.10094 [DOI] [PubMed] [Google Scholar]
- 8.Aznar Díaz I, Kopecký K, Romero Rodríguez JM, Cáceres Reche MP, Trujillo Torres JM. Pathologies associated with Problematic Internet Use. A systematic review and meta-analysis in WoS and Scopus. Investigación bibliotecológica. 2020;34(82):229–253. doi: 10.22201/iibi.24488321xe.2020.82.58118 [DOI] [Google Scholar]
- 9.Fernández-Villa T, Ojeda JA, Gómez AA, et al. Uso problemático de internet en estudiantes universitarios: factores asociados y diferencias de género [Problematic Internet Use in University Students: associated factors and differences of gender]. Adicciones. 2015;27(4):265–275. Spanish. doi: 10.20882/adicciones.751 [DOI] [PubMed] [Google Scholar]
- 10.Vázquez-Chacón M, Cabrejos-Llontop S, Yrigoin-Pérez Y, Robles-Alfaro R, Toro-Huamanchumo CJ. Adicción a internet y calidad de sueño en estudiantes de medicina de una Universidad peruana, 2016 [Internet addiction and sleep quality in medical students from a Peruvian university, 2016]. Revista Habanera de Ciencias Médicas. 2019;18(5):817–830. Spanish. [Google Scholar]
- 11.Puerta-Cortés DX, Carbonell X. Uso problemático de Internet en una muestra de estudiantes universitarios colombianos [Problematic Internet use in a sample of Colombian university students]. Avances en psicología latinoamericana. 2013;31(3):620–631. Spanish. [Google Scholar]
- 12.Li L, Xu DD, Chai JX, et al. Prevalence of Internet addiction disorder in Chinese university students: a comprehensive meta-analysis of observational studies. J Behav Addict. 2018;7(3):610–623. doi: 10.1556/2006.7.2018.53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gioia F, Rega V, Boursier V. Problematic internet use and emotional dysregulation among young people: a literature review. Clin Neuropsychiatry. 2021;18(1). doi: 10.36131/cnfioritieditore20210104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nepp J. [Psychosomatic aspects of dry eye syndrome] Psychosomatische Aspekte beim trockenen Auge. Ophthalmologe. 2016;113(2):111–119. doi: 10.1007/s00347-015-0187-3 [DOI] [PubMed] [Google Scholar]
- 15.Shields GS, Kuchenbecker SY, Pressman SD, Sumida KD, Slavich GM. Better cognitive control of emotional information is associated with reduced pro-inflammatory cytokine reactivity to emotional stress. Stress. 2016;19(1):63–68. doi: 10.3109/10253890.2015.1121983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Awan HA, Aamir A, Diwan MN, et al. Internet and pornography use duriNG the COVID-19 pandemic: presumed impact and what can be done. Front Psychiatry. 2021;12:623508. doi: 10.3389/fpsyt.2021.623508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Al Tawil L, Aldokhayel S, Zeitouni L, Qadoumi T, Hussein S, Ahamed SS. Prevalence of self-reported computer vision syndrome symptoms and its associated factors among university students. Eur J Ophthalmol. 2020;30(1):189–195. doi: 10.1177/1120672118815110 [DOI] [PubMed] [Google Scholar]
- 18.Boulet C. The ‘20/20/20 rule’–When good intentions and axiomatic habit displace best practices. Canadian J Optometry. 2016;78(4):6. doi: 10.15353/cjo.78.448 [DOI] [Google Scholar]
- 19.Carbonell X, Chamarro A, Oberst U, Rodrigo B, Prades M. Problematic use of the internet and smartphones in university students: 2006–2017. Int J Environ Res Public Health. 2018;15(3):475. doi: 10.3390/ijerph15030475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pandey SK, Sharma V. Mask-associated dry eye disease and dry eye due to prolonged screen time: are we heading towards a new dry eye epidemic during the COVID-19 era? Indian J Ophthalmol. 2021;69(2):448–449. doi: 10.4103/ijo.IJO_3250_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aygar H, Goktas S, Zencirci SA, Alaiye M, Onsuz MF, Metintas S. Association between fear of missing out in social media and problematic internet use in university students. Dusunen Adam. 2019;32(4):302–308. [Google Scholar]
- 22.Mehra D, Galor A. Digital screen use and dry eye: a review. Asia Pac J Ophthalmol. 2020;9(6):491–497. doi: 10.1097/apo.0000000000000328 [DOI] [PubMed] [Google Scholar]
- 23.Asiedu K, Kyei S, Boampong F, Ocansey S. Symptomatic dry eye and its associated factors: a study of university undergraduate students in Ghana. Eye Contact Lens. 2017;43(4):262–266. doi: 10.1097/icl.0000000000000256 [DOI] [PubMed] [Google Scholar]
- 24.You YS, Qu NB, Yu XN. Alcohol consumption and dry eye syndrome: a Meta-analysis. Int J Ophthalmol. 2016;9(10):1487–1492. doi: 10.18240/ijo.2016.10.20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mohidin N, Jaafar AB. Effect of smoking on tear stability and corneal surface. J Curr Ophthalmol. 2020;32(3):232–237. doi: 10.4103/joco.Joco_70_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vicente-Herrero M, de la Torre MR-I, Terradillos-García M, González ÁL. Síndrome del ojo seco. Factores de riesgo laboral, valoración y prevención [Dry eye syndrome. Occupational risk factors, valuation and prevention]. SEMERGEN-Medicina de Familia. 2014;40(2):97–103. Spanish. doi: 10.1016/j.semerg.2013.05.003 [DOI] [PubMed] [Google Scholar]
- 27.Kowalska M, Zejda JE, Bugajska J, Braczkowska B, Brozek G, Malińska M. [Eye symptoms in office employees working at computer stations] Dolegliwości ze strony narzadu wzroku u pracowników biurowych zatrudnionych na komputerowych stanowiskach pracy. Med Pr. 2011;62(1):1–8. [PubMed] [Google Scholar]
- 28.Lawrenson JG, Hull CC, Downie LE. The effect of blue-light blocking spectacle lenses on visual performance, macular health and the sleep-wake cycle: a systematic review of the literature. Ophthalmic Physiol Opt. 2017;37(6):644–654. doi: 10.1111/opo.12406 [DOI] [PubMed] [Google Scholar]
- 29.Hyon JY, Yang HK, Han SB. Dry eye symptoms may have association with psychological stress in medical students. Eye Contact Lens. 2019;45(5):310–314. doi: 10.1097/icl.0000000000000567 [DOI] [PubMed] [Google Scholar]
- 30.Matossian C, McDonald M, Donaldson KE, Nichols KK, MacIver S, Gupta PK. Dry eye disease: consideration for women’s health. J Women's Health. 2019;28(4):502–514. doi: 10.1089/jwh.2018.7041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liang CY, Cheang WM, Wang CY, et al. The association of dry eye syndrome and psychiatric disorders: a nationwide population-based cohort study. BMC Ophthalmol. 2020;20(1):123. doi: 10.1186/s12886-020-01395-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Arthanari S, Khalique N, Ansari MA, Faizi N. Prevalence & determinants of Internet Addiction among Indian adolescents. Indian J Community Health. 2017;29(1):54. [Google Scholar]
- 33.Tsumura H, Kanda H, Sugaya N, Tsuboi S, Fukuda M, Takahashi K. Problematic internet use and its relationship with psychological distress, insomnia, and alcoholism among schoolteachers in Japan. Cyberpsychol Behav Soc Netw. 2018;21(12):788–796. doi: 10.1089/cyber.2018.0233 [DOI] [Google Scholar]
- 34.Maia BR, Marques M, Pereira AT, Macedo A. Internet use patterns and the relation between generalized problematic internet use and psychological distress in Portuguese university students. Revista De Psicopatologia y Psicologia Clinica. 2020;25(1):31–39. doi: 10.5944/rppc.25324 [DOI] [Google Scholar]
- 35.Odell PM, Korgen KO, Schumacher P, Delucchi M. Internet use among female and male college students. Cyber Psychol Behav. 2000;3(5):855–862. doi: 10.1089/10949310050191836 [DOI] [Google Scholar]
- 36.Acier D, Kern L. Problematic internet use: perceptions of addiction counsellors. Comput Educ. 2011;56(4):983–989. doi: 10.1016/j.compedu.2010.11.016 [DOI] [Google Scholar]
- 37.Castellana Rosell M, Sánchez-Carbonell X, Graner Jordana C, Beranuy Fargues M. El adolescente ante las tecnologías de la información y la comunicación: internet, móvil y videojuegos [The adolescent before information and communication technologies: Internet, mobile and video games]. Pap Psicol. 2007;3:196–204. Spanish. [Google Scholar]