Abstract
Plain community people (Amish and Mennonites) have increased risk of having recessive genetic disorders. This study was designed to assess the rate of referral of Plain people to genetic services at UPMC Children’s Hospital of Pittsburgh. Medical records of Plain patients from a 1-year time period were reviewed. Data collected included demographic information, clinical presentation, referral for genetic services, and diagnosis. Of the 303 patients, 102 (33.7%) had a clinical presentation suggestive of a genetic disorder, yet only 32 of those 102 patients (31.4%) had been evaluated by the division of Medical Genetics. These data indicate that less than half of Plain patients with a clinical presentation suggestive of a genetic disorder had been referred to the division of Medical Genetics for a formal evaluation. Now that under-referral of Plain patients has been confirmed, providers can be educated in order to increase referrals for genetic services and facilitate positive healthcare outcomes for the Plain Community.
Keywords: Amish, genetic testing, genetics services, Mennonites, plain community, referral practices
1 |. INTRODUCTION/BACKGROUND
The Plain Community collectively refers to the Amish, Mennonites, and Hutterites, all of whom are descendants of Anabaptists from central Europe, and who immigrated to North America in the 18th century because of religious persecution. The Plain Communities have increased rates of recessive genetic disorders as a result of limited allelic diversity in their communities; this is due to the bottleneck effect related to their migration to North America, and subsequent expression of founder mutations (Strauss & Puffenberger, 2009). Each Plain Community has a similar genetic background, but as a result of their cultural isolation, communities within the same geographic area have a specific pattern of genetic disorders that differ from other communities throughout the United States due to genetic drift (Morton et al., 2003). Today, most Plain Community members reside in socially isolated groups with little genetic inflow; the largest populations are located in Pennsylvania, Ohio, and Indiana. About half of the genetic diseases seen in the Plain Community can cause major disability, such as maple syrup urine disease (MSUD) and glutaric aciduria type 1 (GA1), yet many of these diseases are also treatable with proper intervention (Strauss et al., 2012). In Lancaster County, eastern Pennsylvania, high rates of GA1 are seen in the Amish population. As a result of the development of a screening test and special formula for infants with the disease, there has been a significant decrease in morbidity and mortality from GA1 in the Lancaster County Amish population, highlighting the importance of early detection and management of genetic disorders (Morton et al., 1991; Strauss et al., 2012). Western Pennsylvania Plain Communities are among the least studied Plain Community populations in the US (Morton et al., 2003). Despite the high density of Plain Community people in Western Pennsylvania, they have limited access to subspecialty health care, increasing their risk for suffering from unidentified and potentially treatable genetic disorders. Lack of referral of Plain Community patients who present with characteristics suggestive of a genetic disorder is concerning since early diagnosis, management, and treatment can prevent severe disabilities and excess future medical costs (Morton et al., 2003). The present study was designed to assess the rate of referral of Plain people to genetic services at UPMC Children’s Hospital of Pittsburgh using a comprehensive sampling method to ascertain all Plain Community patients seen at UPMC Children’s Hospital of Pittsburgh over a one-year time period. In order to further examine the rate of referral for patients presenting with clinical characteristics indicative of a potential genetic disorder, a chart review was designed to gather data about the Plain people seen at UPMC Children’s Hospital and its associated clinics.
2 |. METHODS
2.1 |. Study design and setting
This study involved review of medical records of Plain patients seen either as an inpatient at UPMC Children’s Hospital of Pittsburgh or in one of the UPMC outpatient clinics between July 1, 2016, and June 30, 2017. This study was approved by the University of Pittsburgh Medical Center QI project approval process (QI project # 1,148).
2.2 |. Identification of plain patients
In order to have the most comprehensive data set possible, Plain patients seen during this time period were identified using hospital billing records. Identification of patients by their ethnicity or religion in the electronic medical record was considered, but this would have excluded a large number of patients due to a lack of self-identification or input of the information by hospital staff. Even if Plain patients did not have Amish/Mennonite contracts (see discussion of insurance types below), their general demographic information, including Amish/Mennonite background, is included within billing and finance information since these patients, if not on contract, will interface with the finance system to arrange for payment plans. All Plain patients with documents from their visits in the UPMC electronic medical record seen during this time period were included in the study.
2.3 |. Data collection
Data collected from patient charts included demographic information, clinical characteristics, initial division visit, referral for genetic services, and final diagnosis. Clinical information collected from patient charts was predetermined using the Plain people genetic database (Payne et al., 2011). This database lists all of the genetic disorders seen across various Plain Communities, along with the associated clinical symptoms, expected laboratory results and specific mutations. Examples of clinical data collected included, but were not limited to, dysmorphic features, physical examination findings, laboratory results, imaging studies, and genetic testing done (Table S1).
2.4 |. Primary outcome and hypothesis
The primary outcome measure was to determine the percentage of patients from the Plain Community with clinical features suggestive of a genetic disorder that was referred for genetic services. Examples of these features included dysmorphic features, multiple congenital anomalies, and metabolic acidosis in light of abnormal metabolic genetic testing. We hypothesized that less than half of the Plain Community patients seen at UPMC Children’s Hospital of Pittsburgh or its associated outpatient clinics, who had clinical characteristics suggestive of an underlying genetic disorder were referred to genetic services and have a confirmed genetic diagnosis.
2.5 |. Analysis
Analysis included descriptive statistics on demographic information and the percentage of patients with a clinical presentation suggestive of a genetic disorder, as well as those who were referred for genetic services and those with a confirmed genetic diagnosis.
3 |. RESULTS
3.1 |. Demographic Information
A total of 303 patient medical records were examined. 166 (54.8%) patients were male and the average patient age was 7.41 years (±8.0 years) during the 2016–2017 timeframe. Patients lived in the following states: Pennsylvania (84.5%), Ohio (10.9%), New York (3.6%), Illinois (0.3%), Kentucky (0.3%), and Maryland (0.3%). Almost half of the patients seen (49.2%) lived in counties in northwestern Pennsylvania (Figure 1). In patient charts, there are sections for identifying a patient’s ethnicity/religion and race, where a patient can be listed as a member of the Amish or Mennonite community. Patients were correctly identified as members of one of the previously listed Plain Communities in their electronic medical record only 57.1% of the time as compared to all being identified as members of one of these groups in billing records. When data were collected from charts in the summer of 2019, 4 patients (1.3%) were listed as deceased. The average age of these patients at the time of their death was 12.75 years (±5.68 years). Cause of death of these patients was related to various genetic disorders: respiratory failure secondary to cystic fibrosis, multi-organ failure following a bone marrow transplant for reticular dysgenesis, complications related to Rett Syndrome, and complications related to undiagnosed progressive spastic quadriplegia, the last of whom was never seen by medical genetics.
FIGURE 1.
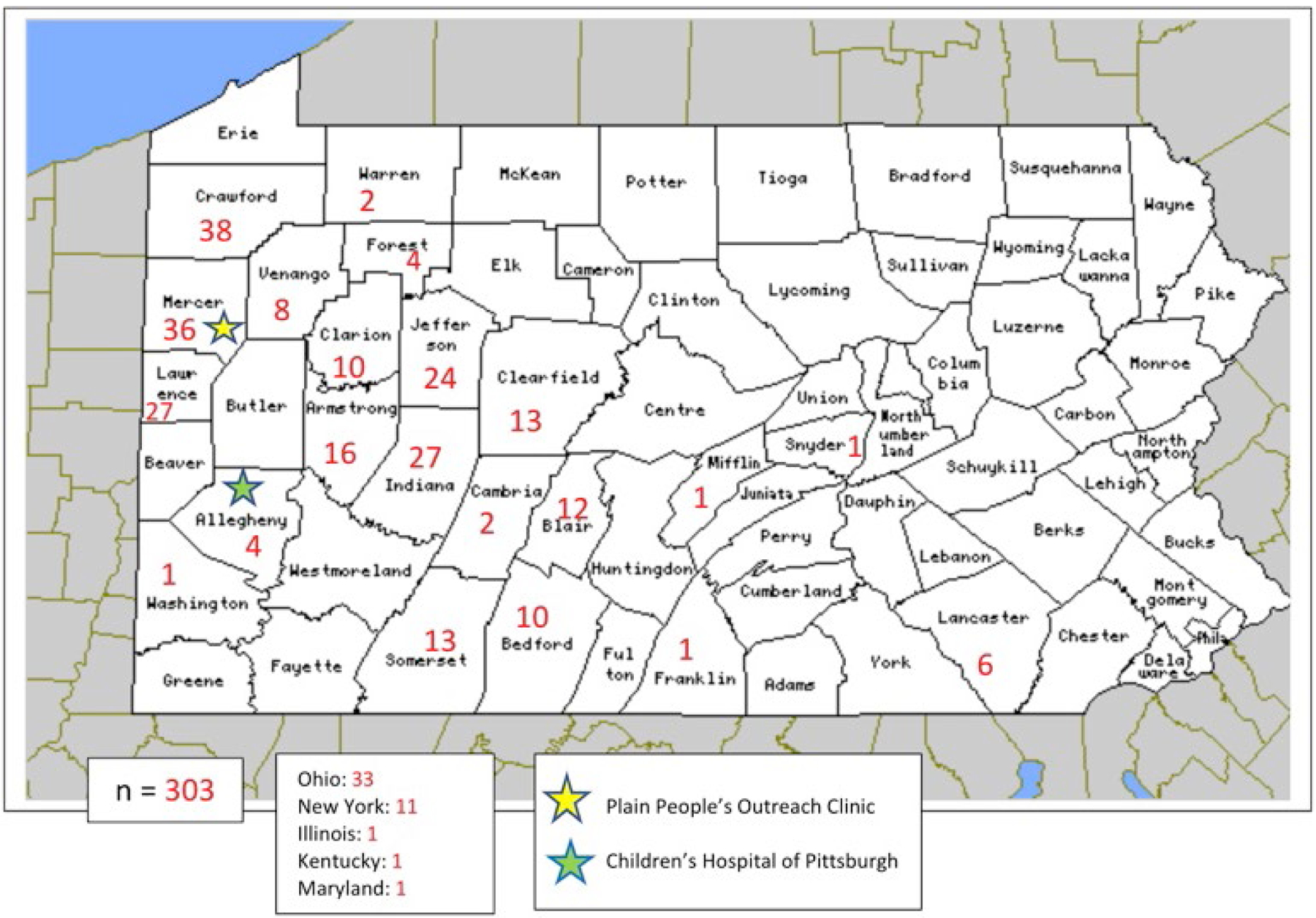
Residence of plain community patients seen at UPMC children’s hospital of Pittsburgh or its outreach clinic. residence of plain community patients by Pennsylvania county is depicted in the figure. 49.2% of patients reside in Northwestern Pennsylvania counties, near the location of the UPMC medical genetics outreach clinic in mercer county. few patients seen were from states other than Pennsylvania
3.2 |. Breakdown of medical insurance types
Types of medical insurance for these patients were also examined. The most common types of insurance, accounting for 95.05% of patients, were Amish Contract (77.56%), Mennonite Population Full Coverage (5.94%), UPMC for You (Medicaid) (3.96%), Self-Pay (3.96%), and Gateway HMO (Medicaid) (3.63%) (Figure S1). Within the UPMC system, elders from Amish and Mennonite church districts can negotiate with the UPMC health system to pay a reduced rate for care due to limited income of the church district members. This typically results in a discount to about 20% of billable costs; these are referred to as the Amish Contract and Mennonite Population Full Coverage programs. Further, both Amish and Mennonite communities may be self-insured, with families contributing to a community fund that provides financial assistance to members experiencing unanticipated or substantial medical expenses (Rohrer & Dundes, 2016).
3.3 |. Initial clinical presentation in 2016–2017
The five most common divisions that patients initially visited in the 2016–2017 timespan were Emergency room (51.8%), Cardiology (7.6%), Transplant (4.6%), Gastroenterology (4.3%), and Orthopedics (3.6%) (Table 1). The five most common types of complaints that patients presented with were General Medical (30.7%), Trauma (17.2%), Cardiac (9.6%), Gastrointestinal (7.3%), and Metabolic (4.6%) (Table 1). General medical complaints encompassed various illnesses such as the common cold, influenza, pneumonia, allergic reactions, and rashes. Metabolic complaints included lactic acidosis, hyper-ammonemia, abnormal acylcarnitine profile, urine organic acids or plasma amino acids, and others.
TABLE 1.
Most common initial department visits and chief complaints of plain people seen at UPMC children’s hospital of Pittsburgh or its outreach clinic
| Initial department visit | Initial chief complaint | ||
|---|---|---|---|
| Emergency | 157 (51.8%) | General Medical | 93 (30.7%) |
| Cardiology | 23 (7.6%) | Trauma | 52 (17.2%) |
| Transplant | 14 (4.6%) | Cardiac | 29 (9.6%) |
| Gastroenterology | 13 (4.3%) | Gastrointestinal | 22 (7.3%) |
| Orthopedics | 11 (3.6%) | Metabolic | 14 (4.6%) |
| Neurology | 9 (3.0%) | Urologic | 13 (4.3%) |
| ENT | 8 (2.6%) | Neurologic | 12 (4.0%) |
| The top 7 departments are listed, accounting for 77.5% of patients (n = 303). | The top 7 types of complaints are listed, accounting for 77.7% of patients (n = 303). | ||
3.4 |. Rates of referral to genetic services
Of the 303 patients, a total of 102 (33.7%) had a clinical presentation suggestive of a genetic disorder based on the predetermined information obtained from their chart. Of those 102 patients, 48 (47.1%) had a genetic diagnosis listed in their chart, while only 32 (31.4%) of the 102 patients suspected to have a genetic disorder had been evaluated by the Genetics division at CHP (Figure S2). The remaining 16 of the 48 patients who had a genetic diagnosis listed in their chart but were not evaluated by the Genetics division at CHP received that diagnosis at healthcare systems outside of UPMC. Therefore, 54 (52.9%) of the 102 patients with a suspected genetic disorder were not seen by Genetics at UPMC or elsewhere.
4 |. DISCUSSION
This examination of Plain Community patients seen during a one-year time period at UPMC Children’s Hospital of Pittsburgh showed that approximately one third of them had a clinical presentation suggestive of a genetic disorder. Half of those patients who presented with a suspected genetic disorder had a genetic diagnosis listed on their chart, yet only one third of them had been evaluated by genetic services at the UPMC Children’s Hospital of Pittsburgh. Upon closer examination of this discrepancy, those patients who had a genetic diagnosis listed, but had not been evaluated by genetic services within the UPMC system, were seen by genetic services at an outside institution or other Plain community clinics. The remaining two thirds of patients with a confirmed or suspected genetic diagnosis did not receive genetic services at UPMC. These data indicate that over half of Plain Community patients with a clinical presentation suggestive of a genetic disorder were not seen by the division of Medical Genetics for a formal evaluation.
Prior to this study, the goal of the division of Medical Genetics was to increase accessibility to health care for the Plain Community of Western Pennsylvania. Initial outreach by the Division of Medical Genetics focused specifically on members of the Plain Community. Members of the Division of Medical Genetics participated in Community Health fairs and published notices in local Plain Community newspapers including The Sugar Creek Budget and Die Botschaft. In 2015, a UPMC Children’s Hospital of Pittsburgh Plain Communities Outreach Clinic was established in Hermitage, Mercer County, Pennsylvania, close to the highest population concentration of Plain Community members in Western Pennsylvania, in order to limit travel expenses for these families and provide the care they need closer to their homes. This also led to the establishment of the Plain Communities Translational Medicine program at UPMC Children’s Hospital of Pittsburgh. In June 2015, a letter was sent to all established patients and families to let them know of clinic developments, and recipients were encouraged to share this information with their neighbors and family members. Following this, outreach was next aimed at local clinicians. This included a Grand Rounds lecture at the site of the Outreach Clinic in Hermitage, Pennsylvania in 2015, a letter of introduction sent to all UPMC health network primary care providers in the region, and development of a brochure to be placed in local physicians’ offices. An article was published in the Allegheny County Medical Bulletin in March of 2016 reviewing the development of the programs and services. County health department staff and other support services were made aware of the new resources. During this time, the Pennsylvania State Newborn Screening Program also found that there was under-utilization of newborn screening for critical congenital heart defects among providers who had limited access to pulse-oximeters. In early 2018, members of the division of Medical Genetics, collaborating with colleagues in Cardiology and at the state newborn screening program, worked to provide oximeters (supported by the state and by Masimo, a global medical technology company that focuses on noninvasive patient monitoring technologies) and education for these providers, many of whom provide home birth services for the Plain Communities.
This study was designed to collect baseline data on of the rate of referral of Plain patients to Genetic Services within the UPMC system. Future comparisons will be possible to evaluate the effectiveness of further educational efforts and public announcements about services the division of Medical Genetics offers. Now that under-referral of Plain Community patients for genetic services has been confirmed, providers will continue to be educated on the issue as a whole and on the importance of referral of patients with clinical findings suggestive of genetic disorders to genetic services. Information about the Plain Communities Outreach Program was presented in a Pediatric Grand Rounds at UPMC Children’s Hospital of Pittsburgh prior to this Quality Improvement study following the initial observations of novel genetic disorders in the Plain community in Western Pennsylvania that were not seen in other Plain communities. Attendees at this program included staff attendings and trainee physicians in the Department of Pediatrics and other subspecialty divisions within this large academic medical facility. Topics included an overview of rare disorders in the Plain Community population, opportunities for discounted clinical genetic testing, and the research program that constituted an undiagnosed disease program for the local Plain Community, definition of founder mutations in the community and population genetics. Additional efforts after completion of this Quality Improvement study were aimed at educating other healthcare providers; these included presentations of the results in the 2nd Annual University of Pittsburgh Genetics Retreat and in the University of Pittsburgh Medical School Dean’s Summer Research Program (DSPR), both in 2019. This allowed using an in-house web-based publication to highlight the study. Furthermore, information from this study has allowed us to approach providers at the UPMC Children’s Hospital of Pittsburgh to encourage referrals of Plain Community patients for genetic services, in order to provide patients with more comprehensive care and to ultimately improve health outcomes for Plain people in Western Pennsylvania. Patients can be referred to Genetic Services at the UPMC Children’s Hospital of Pittsburgh, or the Medical Genetics outreach clinic in northwestern Pennsylvania where nearly half of the Plain people that were seen at the UPMC Children’s Hospital of Pittsburgh reside. Alternate educational modalities and needs will be evaluated to assure comprehensive referral of these patients. Results from this study were also presented at the American College of Medical Genetics meeting (ACMG) in 2020, which could encourage other institutions to conduct their own Quality Improvement studies to assess referral of Plain patients for genetic services.
Some limitations of the present study are due to the nature of a chart review. Patient charts were not always completed by the medical service that initially evaluated the patient; this was dependent on the patient’s presenting findings, the urgency of their condition, and the divisions where they were seen. Furthermore, physician reasoning behind why some patients were not referred to genetic services is not included in patient charts. Possible explanations for why there was a lack of referral of Plain patients include physician bias, such as providers assuming that patients would not want to be seen by or could not afford to be seen by genetic services, or that providers did not realize the patients could benefit from the referral to genetics. In total, one chart did note that genetic services had been consulted, but the family declined the evaluation. If this occurred with other patients, the declination was not noted in their charts. In addition, while the majority of patients presented to the Emergency department, physician practice in that area focuses on immediate needs and defers referral to subspecialty providers. A more complete ascertainment of referrals from both in- and out-patient service providers for Plain patients might have allowed for a more complete estimate of referral rates. Lastly, this work is limited to one-year period which might differ compared with other years; however, the difference would likely not be substantial.
Access to genetic services by members of the Plain Community is essential in order to improve health outcomes for this population, as rates of certain recessive genetic disorders are higher in the Plain Community than in the general population (Payne et al., 2011). Early detection of genetic disorders is important in order to prevent or reduce disease sequalae; in Plain patients with propionic acidemia, for example, early detection has been associated with improved neurological outcomes (Scott Schwoerer et al., 2018; Strauss et al., 2012). Some genetic disorders seen in the Plain Community can be detected by newborn screening, but not all Plain patients utilize newborn screening; in Wisconsin, one study found that less than half of Amish households who responded to a survey sent by the researchers had each of their children receive newborn screening, citing lack of access to testing as the most common reason (Sieren et al., 2016). Without universal access to newborn screening, as well as decreased sensitivity in screening for certain genetic disorders due to the presence of milder mutations in this population, referral to genetic services when patients present with symptoms suggestive of a genetic disorder is crucial.
This study addresses many aspects of genetic counselor practice-based competencies as well as components of the National Society of Genetic Counselors (NSGC) Code of Ethics (Doyle et al., 2013; National Society of Genetic, 2018). Activities detailed in this project address many of the competencies that were updated by the Accreditation Council for Genetic Counseling in 2019 and that are expected from a genetic counselor provider. Some of these competencies that are relevant here and are sought when working with the Plain community include integrating specific psychosocial needs to promote client well-being, engaging in a relationship-building with client/community, adapting genetic counseling skills in a culturally responsive, and respectful manner as well as advocating for individuals, families, and communities. In addition to this, adherence to and application of the NSCG Code of Ethics should be sought in these activities, particularly the following aspects of the Code including providing genetic counseling services to their clients regardless of their clients’ abilities, age, culture, religion, ethnicity and respect clients’ beliefs, inclinations, circumstances, feelings, family relationships, sexual orientation, religion, gender identity, and cultural traditions and also, sharing knowledge and providing mentorship and guidance for the professional development of genetic counselors, employees, trainees, and colleagues. At UPMC CHP, the Plain Community Outreach Program is coordinated by and was co-developed by an advanced-practice genetic counselor (CWV). The initial goals of the program included development of a service delivery model that respects the cultural preferences of the community, advocates for the unique needs of the community, and promotes equal access to genetic services in the relatively underserved part of the western Pennsylvania population. Some progress has been made on these goals, but this study illuminates the continuing need to focus on the first principles of equity and advocacy, to inform colleagues about the needs of the community and of the availability of a variety of services, many which can be at no or reduced cost because of the existence of the Outreach Program. Focus on early referral and diagnosis to prevent sequelae from undiagnosed conditions that are amenable to management involves education of families and providers, genetic counseling, informed decision-making by families, diagnostic testing and interpretation, and implementation of customized treatment programs for these patients. Genetic counselors fulfill key roles in each step of this process.
4.1 |. Future goals
Given the findings of this study, plans are underway to continue educational programs to all patient-facing providers, especially those who work directly with the Plain Community, This includes presentations on newborn screening and ‘red flags for referral to genetics’ for lay and licensed midwives and primary care providers, continued education of trainees within divisions most likely to have appropriate patients for referral, and maintaining our visibility within the hospital and outpatient clinic settings at CHP. These efforts should include prospective data collection on frequency and types of referrals and on acceptance and follow through on the appointments related to these referrals. A survey of the Western PA Plain community regarding understanding of and attitudes about genetic evaluation may also provide critical information about how to continuously improve programs.
5 |. CONCLUSIONS
This study demonstrated a clear under-referral of Plain Community patients to genetic services at the UMPC Children’s Hospital of Pittsburgh when referral was warranted based on patients’ clinical presentations. Until the reason(s) behind under-referral is understood, it is essential to educate healthcare providers on the benefit of genetic services for Plain Community patients through a variety of modalities such as grand rounds and institutional newsletters. Medical systems that work with underserved communities, such as the Plain Community, should assess their referral practices to ensure that patients who present with characteristics warranting further evaluation are able to receive it.
Supplementary Material
What is known about this topic
Although most of the research on the Plain Community focuses on genetic disorders prevalent among this population, little is known about the specific referral rates of Plain patients to genetic services when they present to healthcare providers outside of clinics established for and dedicated to the care of members of these communities. To the authors’ knowledge, there are no published studies on referral rates of Plain patients to genetic services.
What this paper adds to the topic
This paper looks at specific rates of referral of Plain patients, primarily from Western Pennsylvania and adjacent state regions, to genetic services when they have characteristics suggestive of a genetic disorder. As noted above, there are no known similar publications, and thus, this paper opens the door to education and discussion with colleagues in Genetics and a broad range of sub-specialties about referral, when indicated, to allow for equitable access to genetic services.
ACKNOWLEDGEMENTS
This work was conducted as part of medical training to fulfill the requirements of doing research or quality improvement studies during medical school at the University of Pittsburgh School of Medicine.
Funding information
The authors did not receive any financial support or grant for this research/quality improvement study.
Footnotes
CONFLICT OF INTEREST
All of the authors declare that they have no conflict of interest.
HUMAN STUDIES AND INFORMED CONSENT
This study was submitted as a quality improvement (QI) project per institutional guidelines and received approval by UPMC (Project ID number 1,148). No informed consent was required from subjects as data were anonymously extracted from the UPMC electronic medical records system. All procedures followed were in accordance with the US Federal Policy for the Protection of Human Subjects.
ANIMAL STUDIES
No non-human animal studies were carried out by the authors for this article.
SUPPORTING INFORMATION
Additional supporting information may be found online in the Supporting Information section.
DATA AVAILABILITY STATEMENT
Data from this study are not publicly available.
REFERENCES
- Doyle DL, Awwad RI, Austin JC, Baty BJ, Bergner AL, Brewster SJ, Erby LA, Franklin CR, Greb AE, Grubs RE, Hooker GW, Noblin SJ, Ormond KE, Palmer CG, Petty EM, Singletary CN, Thomas MJ, Toriello H, Walton CS, & Uhlmann WR (2013). Review and update of the genetic counseling practice based competencies by a task force of the accreditation council for genetic counseling. Journal of Genetic Counseling, 25(5), 868–879. 10.1007/s10897-016-9984-3 [DOI] [PubMed] [Google Scholar]
- Morton DH, Bennett MJ, Seargeant LE, Nichter CA, & Kelley RI (1991). Glutaric aciduria type I: A common cause of episodic encephalopathy and spastic paralysis in the Amish of Lancaster county, Pennsylvania. American Journal of Medical Genetics, 41(1), 89–95. 10.1002/ajmg.1320410122 [DOI] [PubMed] [Google Scholar]
- Morton DH, Morton CS, Strauss KA, Robinson DL, Puffenberger EG, Hendrickson C, & Kelley RI (2003). Pediatric medicine and the genetic disorders of the Amish and Mennonite people of Pennsylvania. American Journal of Medical Genetics Part C: Seminars in Medical Genetics, 121C(1), 5–17. 10.1002/ajmg.c.20002 [DOI] [PubMed] [Google Scholar]
- National Society of Genetic Counselors. (2018). National Society of Genetic Counselors Code of Ethics. Journal of Genetic Counseling, 27(1), 6–8. 10.1007/s10897-017-0166-8 [DOI] [PubMed] [Google Scholar]
- Payne M, Rupar CA, Siu GM, & Siu VM (2011). Amish, mennonite, and hutterite genetic disorder database. Paediatrics & Child Health, 16(3), e23–e24. 10.1093/pch/16.3.e23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohrer K, & Dundes L (2016). Sharing the load: Amish healthcare financing. Healthcare (Basel), 4(4), 10.3390/healthcare4040092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott Schwoerer J, Clowes Candadai S, & Held PK (2018). Long-term outcomes in Amish patients diagnosed with propionic acidemia. Molecular Genetics and Metabolism Reports, 16, 36–38. 10.1016/j.ymgmr.2018.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sieren S, Grow M, GoodSmith M, Spicer G, Deline J, Zhao Q, Lindstrom MJ, Harris AB, Rohan AM, & Seroogy CM (2016). Cross-sectional survey on newborn screening in Wisconsin Amish and Mennonite communities. Journal of Community Health, 41(2), 282–288. 10.1007/s10900-015-0094-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss KA, & Puffenberger EG (2009). Genetics, medicine, and the Plain people. Annual Review of Genomics and Human Genetics, 10, 513–536. 10.1146/annurev-genom-082908-150040 [DOI] [PubMed] [Google Scholar]
- Strauss KA, Puffenberger EG, & Morton DH (2012). One community’s effort to control genetic disease. American Journal of Public Health, 102(7), 1300–1306. 10.2105/AJPH.2011.300569 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data from this study are not publicly available.


