Abstract
Objective:
The aim of this study was to obtain a comprehensive analysis of the physical workload of clinical staff in long-term care facilities, before and after a safe resident handling program (SRHP).
Background:
Ergonomic exposures of health care workers include manual handling of patients and many non-neutral postures. A comprehensive assessment requires the integration of loads from these varied exposures into a single metric.
Method:
The Postures, Activities, Tools, and Handling observational protocol, customized for health care, was used for direct observations of ergonomic exposures in clinical jobs at 12 nursing homes before the SRHP and 3, 12, 24, and 36 months afterward. Average compressive forces on the spine were estimated for observed combinations of body postures and manual handling and then weighted by frequencies of observed time for the combination. These values were summed to obtain a biomechanical index for nursing assistants and nurses across observation periods.
Results:
The physical workload index (PWI) was much higher for nursing assistants than for nurses and decreased more after 3 years (−24% versus −2.5%). Specifically during resident handling, the PWI for nursing assistants decreased by 41% of baseline value.
Conclusion:
Spinal loading was higher for nursing assistants than for nurses in long-term care centers. Both job groups experienced reductions in physical loading from the SRHP, especially the nursing assistants and especially while resident handling.
Application:
The PWI facilitates a comprehensive investigation of physical loading from both manual handling and non-neutral postures. It can be used in any work setting to identify high-risk tasks and determine whether reductions in one exposure are offset by increases in another.
Keywords: intervention effectiveness, ergonomic tools and methods, health care ergonomics
INTRODUCTION
Manual resident handling (RH) performed by health care workers leads to load on the lumbar spine and has been associated with musculoskeletal disorders, especially those affecting the low back. According to the Centers for Disease Control and Prevention’s National Nursing Home Survey of 2004–2005, back injuries were the second leading injury to nursing assistants (NAs) (Jones, Dwyer, Bercovitz, & Strahan 2009). NAs perform the majority of direct care in nursing homes, and their physical exposures often far exceed those of registered nurses (RNs) and licensed practical nurses (LPNs) (Boyer, 2008).
A 1998 review of 42 studies on low-back pain among nursing jobs reported relationships between low-back pain and physical stressors, such as lifts, transfers, “save-the-patient” situations, awkward work postures, static standing, and working as an NA as opposed to an RN (Lagerström, Hansson, & Hagberg, 1998). A major finding was that in nursing homes, NAs had a higher prevalence of work-related low-back problems than did nurses and that higher levels of physical exposure likely played a role.
Because of the varied tasks and exposures involved in patient care, all of which may contribute to spinal loading, it is not sufficient to compare one exposure at a time when contrasting job groups or settings or evaluating interventions. Biomechanical modeling can be a valuable tool for combining multiple exposures into a common metric, such as lumbar spine compressive forces. Low-back modeling in laboratory settings has been used to describe exposures of health care workers in patient care tasks, with and without the use of handling equipment (Garg, 1992; Garg & Owen, 1992; Marras, Davis, Kirking, & Granata, 1999; Skotte, Essendrop, Hansen, & Schibye, 2002; Zhuang, Stobbe, Hsiao, Collins, & Hobbs, 1999).
A German study of nursing home workers described an index of physical workload (Klimmer, Kylian, Hollmann, & Schmidt, 1998). A total of 610 nursing home employees (nursing, psychosocial care, and housekeeping) estimated frequencies of postures and MH activities using a 5-point Likert-type scale (never to very often). A biomechanical model of lumbar loading on the L5/S1 motion segment (Jager, Luttmann, & Lauring, 1991) was used to develop weighting factors for 15 combinations of postures and MH. The weights were computed as the difference between L5/S1 compression in the specified posture/activity and a reference value (compression with trunk upright and hands empty). Weighted frequencies were combined for an overall lumbar load estimate within each job group.
In this study and a follow-up of 455 of the original employees (Hollmann, Klimmer, Schmidt, & Kylian, 1999), nursing staff had the highest physical workload compared to other occupations. Further, the index values were associated with musculoskeletal symptoms (Hollmann et al., 1999; Klimmer et al., 1998, 2005).
Hollmann et al. (1999) recommended further testing of the index using physical workload data from observational methods, and authors of a comment on the study suggested that “these approaches, based on self-reported data, can only yield rather crude estimates of biomechanical load” (Burdorf & van der Beek, 1999, p. 82).
In the present study, a large nursing home corporation instituted a safe resident handling program (SRHP) in 2004. Previous evaluation showed that clinical staff spent less time in patient handling and in non-neutral postures after the SRHP began (Kurowski, Boyer, Fulmer, Gore, & Punnett, 2012). The next goal was to evaluate the change in combined exposures, using biomechanical modeling to compute a physical workload index (PWI). The index was analogous to that of Klimmer et al. (1998) and Hollmann et al. (1999), but the frequencies of ergonomic exposures were derived not from self-report by workers but from direct observations collected using the Postures, Activities, Tools, and Handling (PATH) method (Buchholz, Paquet, Punnett, Lee, & Moir, 1996). The PWI was used to describe biomechanical load for NAs and nurses separately, both before and after initiation of the SRHP.
METHOD
Background to the Intervention
Process
The SRHP was implemented by a third-party firm that provided protocols for selection and use of mechanical RH devices. Equipment was purchased by the company for each facility to accommodate the needs of the individual residents in each center. In each center, nurses assessed residents’ needs for safe patient handling with plans to reassess upon admission, readmission, following significant health changes, and in quarterly reviews. Assessments indicated types of equipment residents required, and stickers applied to their nameplates also indicated the number of staff required for RH.
Representatives of the third-party firm also provided training on equipment use and maintenance. The trainers visited facilities to conduct orientations with department heads and nurses. Follow-up visits were made to emphasize training and policies and to evaluate staff competency after 2, 4, 10, 20, 30, 40, and 50 weeks.
Study Design
In 2006, at the initiation of this prospective study, six centers were identified for baseline ergonomic observations. Follow-up data were also collected at 3-month, 12-month, and 24-month follow-up periods at five of these centers. Two more facilities were recruited 1 year after they had implemented the SRHP, so 12-month and 24-month data were collected. Additionally, 36-month data were collected at five centers where the SRHP had begun before initiation of this study. Thus the observations were made at different but overlapping sets of centers at each time point.
Ergonomic Exposure Assessment
As described elsewhere (Kurowski et al., 2012), the PATH method (Buchholz et al., 1996) was adapted to record frequencies of ergonomic exposures, including health care–specific activities (e.g., RH) and tools (e.g., RH devices). PATH is a direct observation method for analyzing nonroutine work, in which multiple ergonomic exposures are recorded in categorical form for a single moment in time, followed by a fixed time interval (in this case, 60 s). The data are expressed as the percentages of observations (work time) in which employees are exposed to each posture or activity.
Categorical items recorded included trunk, leg, and arm postures; manual handling (MH); RH; and task information. Handling categories were less than 4.55 kg, 4.55 to 22.68 kg, and greater than 22.68 kg. Tasks (direct care, medical care, administrative, and other care) were mutually exclusive. RH was coded when employees were repositioning, transferring, transporting, or assisting with ambulation. Repositioning occurred when a resident (or body part) was moved from one area to another on the same surface (e.g., boosting up in bed). Transfers occurred when moving a resident from one surface to another (e.g., bed to wheelchair). Transporting involved moving a resident from one place to another by use of equipment (e.g., wheelchair). Assisting with ambulation involved helping ambulatory residents walk.
RH: Task versus activity.
Resident handling is captured in two ways in the PATH data, both as an option for direct care task and as a separate variable called RH activity, which captures information about the type of handling occurring (reposition, transfer, transport, or ambulation assist). Most observations associated with an RH activity are also coded as the direct care task of RH. However, there are some occasions on which another task may be coded, even though an RH activity is occurring. Some exam-ples of this situation include repositioning a resident’s leg while performing wound care (a medical care task) or repositioning while changing sheets in an occupied bed (housekeeping, an other care task).
Data collection procedures.
Twelve observers were trained to collect PATH data on personal digital assistants with stylus-based touch screens, using InspectWrite™ software, from Penfact Inc. (Boston, MA).
New observers were required to demonstrate 80% agreement (Kappa coefficient > 0.6) with more experienced observers. Nine of the 18 collected variables were used in the biomechanical modeling reported in this study (trunk angle, leg action, arm angle, weight in hands, RH type, and task type). For these variables, among 11 pairs of observers, percentage agreement ranged from 80% to 100%, and kappa statistics ranged from 0.63 to 0.96. Interrater reliability (IRR) was generally higher for the leg action, weight in hands, RH type, medical tasks, and administrative tasks.
The PATH data collection protocol involved observation of clinical employees in sessions lasting from 1 to 8 hr. All data were collected on the first shift (7:00 a.m. to 3:00 p.m.). Individual workers were selected by convenience from members of the clinical staff and were followed exclusively for the observation period. Because NAs performed most of the RH in these workplaces and were the primary focus of the SRHP, they were preferentially recruited for observations. LPNs and RNs performed RH activities for less than 3% of the collected observations at baseline (Kurowski et al., 2012). Whenever possible, follow-up observations were completed with the same individuals who had previously volunteered. The University of Massachusetts Lowell Institutional Review Board reviewed and approved all procedures.
Data management and analysis.
Exposure data were downloaded, cleaned, and documented in a standardized format. Frequencies of PATH variables were computed using SAS 9.2.
Distribution of Tasks by Job Group
Because exposures can vary substantially among tasks (Kurowski et al., 2012), the frequencies of observed tasks were calculated for each job group for each survey occasion. Tasks were categorized as direct care (e.g., RH, bathe, dress, toilet, feed), medical (e.g., give meds, med prep/mix, wound care, vital signs), administrative (e.g., computer, paper, phone, meet/train), and other (e.g., food prep/deliver, housekeeping, retrieve/replace equipment, universal precaution).
PWI
As described in the following steps, the PWI for each job was a weighted sum of average L5/S1 compressive forces resulting from 17 combinations of postures and MH actions. Each of the 17 terms in the index consisted of the frequency of the posture/action in that job (converted to a relative score) multiplied by its weighting factor, obtained from the biomechanical modeling. The calculations were done in Microsoft Excel.
The PWI was calculated for NAs both overall and only for the RH observations. The data for LPNs and RNs were pooled to create an overall PWI for nurses.
The equation used for calculating the PWI was as follows:
where S = frequency score, W = weighting factor, Ti = trunk postures, Aj = arm postures, Lk = leg postures, Wul = weight in hands with upright trunk, and Wim = weight in hands with inclined trunk.
The trunk, arm, and leg postures and MH weights were categorized as observed in PATH (Tables 1, 2, 3, and 4). For PWI calculations, weights carried (Table 4) were subdivided into MH with an upright trunk (Wu1 − Wu3) and weights carried with an inclined trunk (Wi1 − Wi3).
TABLE 1:
Trunk Postures
| Model Input |
Postures From Postures, Activities, Tools, and Handling Method |
|---|---|
| T1 | Neutral (trunk flexed <20°) |
| T2 | Moderate flexion (trunk flexed ≥20° to <45°) |
| T3 | Severe flexion (trunk flexed ≥45°) |
| T4 | Lateral bent/twisted–neutral (trunk flexed <20°) |
| T5 | Lateral bent/twisted–flexed (trunk flexed ≥20°) |
TABLE 2:
Arm Postures
| Model Input |
Postures From Postures, Activities, Tools, and Handling Method |
|---|---|
| A1 | Both arms <60° |
| A2 | 1 arm raised ≥60° |
| A3 | 2 arms raised ≥60° |
TABLE 3:
Leg Postures
| Model Input |
Postures From Postures, Activities, Tools, and Handling Method |
|---|---|
| L1 | Sitting |
| L2 | Standing |
| L3 | Shallow squat (knees bent >35° to <80°) |
| L4 | Kneeling (one or both knees) |
| L5 | Walking |
| L6 | Deep squat (knees bent ≥80°) |
| L7 | Lunge (1 knee bent >35°) |
TABLE 4:
Manual Handling Actions
| Model Input |
Manual Handling From Postures, Activities, Tools, and Handling Method |
|---|---|
| Wu 1 /Wi 1 | <4.55 kg |
| Wu 1 /Wi 2 | ≥4.55 to ≤22.68 kg |
| Wu 1 /Wi 3 | >22.68 kg |
Frequency scores.
The observed frequencies of the postures and weights carried were converted from raw percentages of time to a score ranging from 0 to 1. For example, moderate trunk flexion (T2) was observed 15.49% of the time at baseline for NAs, which was converted to the frequency score of 0.1549.
Weighting factors.
The University of Michigan’s Three Dimensional Static Strength Prediction Program (3DSSPP) was utilized to estimate compressive forces on the L5/S1 motion segment in each posture/MH action, assuming a female with a height of 1.62 m and a weight of 72.71 kg.
The body segments were positioned at the midpoint of the range for each posture referenced in the PATH template. For example, T2 is defined as 20° to 45°, so an angle of 32.5° of forward flexion was used. Upper endpoints for severe flexion (T3) and lateral bent/twist flexed (T5) are not specified in the PATH template, and in some instances, observers witnessed extreme forward flexion (up to 120°). Thus the T3 midpoint was calculated on the basis of the range of 45° to 120°. Loads were assumed to be handled equally bilaterally.
Several postures included multiple possibilities for observational classification, including lateral bent or twisted–neutral (T4), lateral bent or twisted–flexed (T5), and kneeling (one or both knees) (L4). In these cases, each possibility for a posture classification was entered into the 3DSSPP, and their resulting compressive forces on L5/S1 were averaged.
Neutral standing (L2) and sitting (L1) were included in the 3DSSPP’s preset postures feature. For walking (L5), hip and knee flexion-extension angles were determined by consulting literature on human gait analysis (Kadaba et al., 1989). Interpolated hip and knee angles representing 20%, 40%, 60%, 80%, and 100% of the gait cycle were input into the 3DSSPP, and the resulting compressive forces were averaged.
The weight category less than 4.55 kg included a large portion of observations in which 0-kg loads were handled. To consider the percentage of time when no load was handled, PATH tasks were stratified by job group, and observations in which less than 4.55 kg was handled were identified. The frequency of observations with no load handled was much higher for nurses than for NAs, overall and during RH (mean 89.6% vs. 47.3% vs. 2.4%). For NAs, no load was handled more frequently when the trunk was upright compared to flexed (mean 47.3% vs. 20.4%).
Compressive forces on L5/S1 for the Wu1 and Wi1 inputs were calculated for neutral and flexed trunks with no load handled and with a 2.28-kg load handled (the midpoint of 0 to 4.55 kg). The forces were then weighted according to the percentage of observations in which no load was handled.
Following the design of the existing index, four postures (neutral trunk, standing, sitting, and both arms below 60°) with the lowest compressive forces on L5/S1 were omitted. Postures retained in the index were T2 through T5, A2 through A3, and L3 through L7. Weighted compressive forces were converted to kiloNewtons (kN) for index inputs.
Standard compressive force.
The loads for posture/MH combinations were standardized relative to a reference value. This value was computed, from the same model, for neutral standing (T1) with arms at the sides (A1) and no load handled (Wu1). The weighting factors used in the PWI were the difference between this reference value (0.24 kN compressive force on L5/S1) and the modeled compressive forces for each posture/action.
Calculation of equation inputs.
A sample calculation for the postural input of moderate flexion (T2) for NAs at baseline is as follows:
where W = weighting factor and S = frequency score.
RESULTS
Demographics
For all time periods, the observed population predominantly consisted of female NAs (Table 5).
TABLE 5.
Population Demographics
| Variable | Baseline | 3 Months | 12 Months | 24 Months | 36 Months |
|---|---|---|---|---|---|
| Number of centers | 7 | 6 | 7 | 7 | 5 |
| Number of observed workers | |||||
| Nursing assistant | 51 | 49 | 75 | 55 | 45 |
| Nurse | 12 | 8 | 18 | 10 | 1 |
| Number of observation periods | |||||
| Nursing assistant | 58 | 55 | 100 | 88 | 57 |
| Nurse | 13 | 8 | 23 | 14 | 1 |
| Number of observation moments (minutes) | |||||
| Nursing assistant | 11,408 | 8,474 | 17,738 | 21,141 | 17,365 |
| Nursing assistant (resident handling) | 1,473 | 1,252 | 1,604 | 1,823 | 1,933 |
| Nurse | 1,160 | 1,846 | 2,841 | 2,624 | 178 |
| Sex (% female) | |||||
| Nursing assistant | 75% | 84% | 94% | 94% | 93% |
| Nurse | 100% | 88% | 96% | 100% | 100% |
| Mean tenure (years) | |||||
| Nursing assistant | 4.75 | 4.24 | 4.00 | 4.45 | 4.50 |
| Nurse | 6.44 | 4.22 | 6.11 | 3.03 | 4.00 |
Distribution of Tasks by Job Group
The frequencies of observed tasks varied substantially between nurses and nursing assistants (Figure 1). On average, nurses performed much less direct care than NAs (12.7% vs. 46.0%). Administrative tasks (45.3%) and medical tasks (31%) represented the majority of nurses’ work time.
Figure 1.
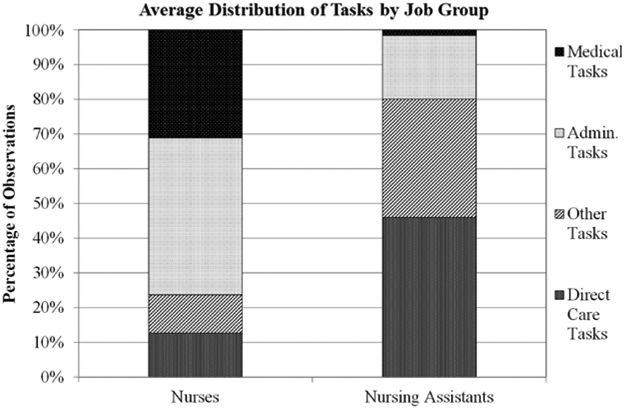
Frequency of task by job group. Five-year average percentage of observations in 15 nursing homes, 2006–2010.
These proportions were virtually identical within each job group across the five survey occasions. Among the direct care observations, NAs were most likely to be performing bathe/groom (11.7%), RH (7.6%), and dress/undress (7.3%), while nurses were most likely to perform resident family counseling (7.4%).
Frequency Scores
Observed frequencies of trunk, arm, and leg postures and MH activities were converted to frequency scores for the PWI and are listed in the appendix. Over 3 years, NAs worked more frequently in neutral trunk postures and with both arms below 60° compared to baseline measurements. They walked more than they stood still and handled lighter loads more frequently and heavier loads less frequently than at baseline (Kurowski et al., 2012). The exposures of nurses did not change as much across time periods.
Weighting Factors
Compressive forces on L5/S1 and the resulting weighting factors for each postural and MH input in the index were computed using the 3DSSPP (Tables 6, 7, 8, 9, and 10).
TABLE 6:
Compressive Forces on L5/S1 and Weighting Factors Resulting From Trunk Postures
| Input | Trunk Angle | Definition | Midpoint Angle |
Average Compressive Force on L5/S1 (kN) |
Weighting Factor |
|---|---|---|---|---|---|
| T2 | Moderate flexion | 20°–45° | 32.5° | 1.41 | 1.16 |
| T3 | Severe flexion | >45° | 82.5°a | 1.98 | 1.73 |
| T4 | Lateral bent/twist–neutral | 20° bent or 45° twist | 10°b | 0.64d | 0.40 |
| T5 | Lateral bent/twist–flexed | >20° flexed and 20° bent or 45° twist |
70°c | 1.96d | 1.72 |
Midpoint between 45° and 120°.
Neutral flexion midpoint between 0° and 20°.
Midpoint between 20° and 120°.
Compressive forces were averaged for lateral bent posture and twist posture.
TABLE 7:
Compressive Forces on L5/S1 and Weighting Factors Resulting From Arm Postures
| Input | Arm Angle | Definition | Midpoint Angle |
Average Compressive Force on L5/S1 (kN) |
Weighting Factor |
|---|---|---|---|---|---|
| A2 | 1 arm >60° | >60° | 120°a | .40 | .16 |
| A3 | 2 arms >60° | >60° | 120°a | .56 | .31 |
Midpoint between 60° and 180°.
TABLE 8:
Compressive Forces on L5/S1 and Weighting Factors Resulting From Leg Postures
| Input | Leg Action | Definition | Midpoint or Interpolated Angles |
Average Compressive Force on L5/S1 (kN) |
Weighting Factor |
|---|---|---|---|---|---|
| L3 | Shallow squat | 35°–80° | 57.5° | .26 | .01 |
| L4 | Kneeling | 1 knee | −90° (upper leg), 0° (lower leg)a | .27d | .03 |
| 2 knees | |||||
| L5 | Walking/running | 20% gait cycle | 17° (hip), 14° (knee)b | .31d | .07 |
| 40% gait cycle | −6° (hip), 5° (knee)b | ||||
| 60% gait cycle | −4° (hip), 39° (knee)b | ||||
| 80% gait cycle | 27° (hip), 36° (knee)b | ||||
| 100% gait cycle | 31° (hip), 5° (knee)b | ||||
| L6 | Deep squat | > 80° | 85°c | .36 | .11 |
| L7 | Lunge | 35°–90° | 67.5° | .25 | .004 |
Input angles for knee on ground.
Hip and knee angles interpolated from Kadaba et al. (1989).
Midpoint between 80° and 90°.
Compressive forces were averaged for individual kneeling and walking/running postures.
TABLE 9:
Compressive Forces on L5/S1 and Weighting Factors Resulting From Lifting Loads With an Upright Trunk
| Input | Weight in Hands With Upright Trunk |
Definition | Midpoint Weight |
Average Compressive Force on L5/S1 (kN) |
Weighting Factor |
|---|---|---|---|---|---|
| Wu 1 | Less than 4.55 kg | 0–4.55 kg | 2.28 kg (1.14 kg/hand) | 0.66 (handling 0 kg); 0.71 (handling 2.28 kg) | BL–24 months: 0.44; 36 months: 0.43a BL–36 months: 0.46b BL–36 months: 0.42c |
| Wu 2 | 4.55 to 22.68 kg | 4.55–22.68 kg | 13.62 kg (6.81 kg/hand) | 0.93 | 0.69 |
| Wu 3 | Greater than 22.68 kg | 22.68–68.04 kg | 45.36 kg (22.68 kg/hand) | 1.57 | 1.33 |
Note. BL = baseline.
Weighting factors for five time points for nursing assistants (NAs; incorporates frequency of handling 0 vs. 2.28 kg).
Weighting factor for five time points for NAs while resident handling (incorporates frequency of handling 0 vs. 2.28 kg).
Weighting factor for five time points for nurses (incorporates frequency of handling 0 vs. 2.28 kg).
TABLE 10:
Compressive Forces on L5/S1 and Weighting Factors Resulting From Lifting Loads With a Flexed Trunk
| Input | Weight in Hands With Inclined Trunk |
Definition | Midpoint Weight |
Average Compressive Force on L5/S1 (kN) |
Weighting Factor |
|---|---|---|---|---|---|
| Wi 1 | Less than 4.55 kg | Moderate flexiona Severe flexionb Lateral bent flexedc Lateral twist flexedc |
>2.28 kg (1.14 kg/hand) | >1.78 (handling 0 kg); 2.07 (handling 2.28 kg) | BL: 1.75; 3–24 months: 1.77; 36 months: 1.75d BL: 1.81; 3 months: 1.79; 12–24 months: 1.81; 36 months: 1.82e BL: 1.56; 3 months: 1.62; 12–36 months: 1.60f |
| Wi 2 | 4.55 to 22.68 kg | Moderate flexiona Severe flexionb Lateral bent flexedc Lateral twist flexedc |
13.62 kg (6.81 kg/hand) | 2.60 | 2.36 |
| Wi 3 | Greater than 22.68 kg | Moderate flexiona Severe flexionb Lateral bent flexedc Lateral twist flexedc |
45.36 kg (22.68 kg/hand) | 4.26 | 4.01 |
Note. BL = baseline.
Flexion midpoint is 32.5°.
Flexion midpoint is 82.5°.
Flexion midpoint is 70°.
Weighting factors for five time points for nursing assistants (NAs; incorporates frequency of handling 0 vs. 2.28 kg).
Weighting factors for five time points for NAs while resident handling (incorporates frequency of handling 0 vs. 2.28 kg).
Weighting factors for five time points for nurses (incorporates frequency of handling 0 vs. 2.28 kg).
Multiple weighting factors were listed for the representative time periods in Table 9 due to differing proportions of tasks in which each job group was handling 0 kg and 2.28 kg.
Similar to Wu1, different weighting factors for Wi1 were listed for the representative time periods for each job group in Table 10 to consider handling 0 kg or 2.28 kg.
PWI
At each survey occasion, the NAs had PWI values of about 30% to 40% higher than those for nurses (Figure 2). For the RH observations, the PWI was almost twice as high as the overall workload value in each survey until the last, when the downward trend became steeper. By the end of the 36-month follow-up, the index had decreased by 24.2% for NAs, by 40.9% for NAs while RH, and by only 2.5% for nurses.
Figure 2.
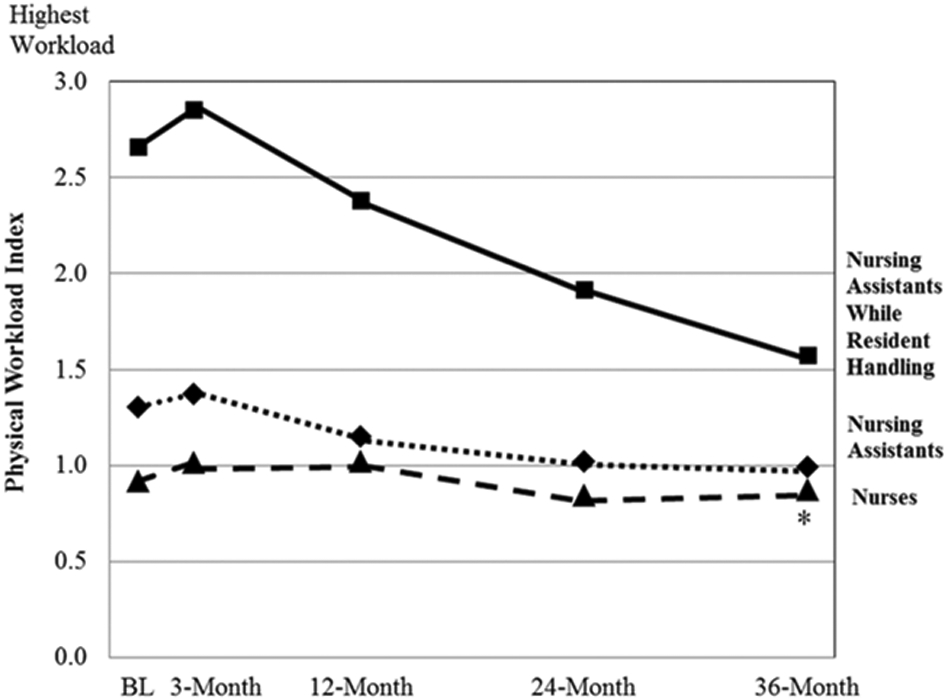
Physical workload index for nurses, nursing assistants, and nursing assistants while resident handling. Thirty-six-month data point for nurses is based on only one observation period.
DISCUSSION
In this large observational study of nursing home staff, NAs had a substantially higher physical workload than nurses. The apparent effect of the SRHP was to decrease the workload of NAs markedly, especially while RH, across a 3-year follow-up period.
The original index (Hollmann et al., 1999) was developed to differentiate between job titles based on self-reported workload. Although the job categories in this study are different, the resulting index did differentiate between NAs and nurses on the basis of their observed physical workload. When reviewing the distribution of observed tasks among job groups, we found evidence that nurses perform less physically strenuous tasks than NAs, like medical and administrative tasks. Even when observed performing direct care, we found that nurses were usually counseling residents and families, a task that is not typically associated with physical exposures. On the other hand, when NAs were performing direct care, they were usually handling residents, helping them to bathe and groom and to dress and undress. NAs’ tasks are more likely to be associated with strenuous postures and handling heavy loads. Task frequencies did not vary much over time, so the reductions in PWI reflect decreases in lumbar loading associated with these tasks. Additionally, the longitudinally stable nature of the task frequencies indicates a robust work sampling process.
The slight PWI increases at 3 months for each job group followed from slight increases in both body postures and weight in hands (MH actions). The increases may have been due to the SRHP implementation process and associated learning curve. After adopting new equipment, it is possible that in the first 3 months, NAs were working in more strenuous postures because they had not yet mastered equipment-use procedures.
The longitudinal decrease in NAs’ PWI is likely attributable to gradual acceptance of the SRHP, resulting in less strenuous RH methods. The use of equipment for RH at 3 months did not change from baseline (10% of RH observations). Equipment use then increased steadily over time (Kurowski et al., 2012). Increased equipment use to alleviate physical exposures associated with manual RH would logically influence loads handled and strenuous postures, therefore reducing NAs’ PWI.
Using RH equipment has been shown to reduce compressive forces on the lumbar spine in laboratory studies. Static biomechanical evaluations of manual transferring tasks and mechanical transfer devices showed reduced compressive forces on L5/S1 when using mechanical devices (Garg, 1992; Garg & Owen, 1992). Zhuang et al. (1999) investigated the effects of transfer methods and resident weight using a three-dimensional biomechanical model; lifting devices significantly reduced low-back compressive forces for nine NAs. A biomechanical assessment, with ground and hand reaction forces as input variables in a linked-segment model, showed higher compressive forces on the lumbar spine in manual versus mechanically assisted patient handling (OHSAH, 2006).
Output from the PATH method is in the form of relative frequencies of observed posture and activity categories. The method has been criticized for lack of detail (Takala et al., 2010) and lack of a summary score for multilevel modeling (Janowitz et al., 2006). By pairing frequencies of PATH exposures with biomechanical modeling of the lumbar spine to calculate the PWI, the type of output score that could be useful to musculoskeletal researchers is now available.
Limitations and Strengths of This Study
When biomechanical models have been used to evaluate health care work, inputs are typically collected from controlled laboratory studies with cooperative “patients,” which may not represent real working situations, thus underestimating the physical stress on the body. Prior uses of the PWI (Hollmann et al., 1999; Janowitz et al., 2006; Klimmer et al., 1998, 2005; Nabe-Nielson, Fallentin, Christensen, Jensen, & Diderichsen, 2008) involved self-reported frequencies of postures and MH. Janowitz et al. (2006) modified the index as part of an ergonomics assessment tool for hospitals, and Nabe-Nielsen et al. (2008) used the index in a hospital questionnaire comparing self-reported measures of work demands. In contrast, our study involved observational postural and MH data collected at work sites, which was more objective than self-reported information.
The exposure frequencies were obtained by fixed-interval sampling during multiple hours per day. Clinical work lacks short, repetitive work cycles, making the alternative of continuous observation inefficient, burdensome, and fatiguing for the observers and PATH (or any other sampling protocol) a more useful method for exposure assessment. PATH has been validated relative to direct instrumentation (Paquet, Punnett, & Buchholz, 2001) and has good IRR, conditional upon sufficient observer training (Park et al., 2009). Weight in hands is difficult to observe visually. We used very broad categories, based on a prior observational study of health care workers (Park et al., 2009), which sacrificed precision in favor of between-category accuracy.
However, there are some limitations to the methods used in this study. Our method of fixed interval sampling resulted in missing some occurrences of heavy loading during RH activities. We also did not observe every moment of work performed while on site; we did not seek every event, only a sample. As long as they are not in synch with the work process, a large number of observations will generate a statistically valid estimate of the frequency of that activity, so whether RH activities were observed few or many times will correspond to their actual occurrence. The RH events we observed were used to compute the proportion of work time they represent. As long as they were an unbiased sample, and the total work time was accurately recorded, we have generated an unbiased estimate of the frequency of RH events.
The biomechanical model is a static one and does not involve estimating contributions attributable to any dynamic activities, such as accelerations necessary to move a person who cannot physically assist with a transfer. When working with the 3DSSPP, we made assumptions regarding inputs for body postures, weight in hands, and anthropometry. For example, when computing the compressive forces for the arm posture 1 arm >60°, we input trunk posture as neutral and leg postures as straight at all joints. It is likely that in real work situations, an NA would be working in more severe trunk and leg postures while lifting an arm, so compressive forces attributable to additional posture combinations were not accounted for in this study. However, these assumptions would have underestimated compressive force on the lumbar spine, on all survey occasions, and for all job categories; thus they are not likely to have biased any of the comparisons shown here. Anthropometry for a 50th-percentile female was used for computations, so index results may be different for males. Because the observed populations of both nurses and NAs were primarily female, this assumption was justifiable.
Midpoints of body angles and weights were used in the 3DSSPP to calculate compressive forces on L5/S1 for posture and MH combinations. If possible, the most appropriate inputs for the 3DSSPP would be median joint angles and loads for each combination. However, this type of information cannot be determined from PATH data. Monte Carlo simulation or bootstrapping techniques utilized in other studies (Tak, 2005; Yuan, 2006) could be used to estimate distributions (and medians could then be calculated) for postures and loads for each combination.
Median values of actual trunk postures within categories may be lower than the midpoints of those categories, which were used for calculating PWI. Because moment arms about the trunk increase as flexion increases to 90°, using midpoints for severe flexion and lateral bent/twist–flexed that are close to 90° may therefore somewhat overestimate the weighting factors for these categories. Since midpoint values were held constant across five time periods and across job titles, any resulting error would likely cancel out, avoiding bias in comparison of survey periods or job groups.
The manner in which the categories for weight in hands were defined in the PATH template made visual judgment of handled loads easier for observers to categorize from visual observation. However, 4.55 to 22.68 kg and greater than 22.68 kg are very wide intervals. If there were reductions in weight within categories, the loss of sensitivity to actual changes in loads handled would have led to underestimating the reduction in mechanical loading.
Although the PWI provides an overall estimate of exposure and a useful output score for PATH data, it does not specify whether that exposure is related to lower frequencies of high biomechanical loading or higher frequencies of lower biomechanical loading. In the future, individual inputs could be examined to identify which frequencies of posture combinations contribute most to the overall exposure of each job group.
At the 36-month follow-up, only one nurse was observed, resulting in a smaller sample size than the other periods. With more data for this time point, the resulting index may have been different. However, nurses spend considerably less time handling residents; therefore it is unlikely that the SRHP would have much impact on the physical workload of nurses, and it is doubtful that the PWI for the 36-month follow-up would change much.
CONCLUSIONS AND RECOMMENDATIONS
The method used in this study demonstrated differences in physical exposures between clinical job titles and also across time periods, indicating benefits resulting from the SRHP for both NAs and nurses. There are many potential applications for the PWI in the scope of this study. Variability between individuals could be examined using actual anthropometric measurements and frequencies of postures and MH activities. The index could also be used to further explore direct care tasks to confirm the highest-risk tasks for health care workers, so further interventions could be considered. Additionally, further examination of the PWI could provide insight into threshold levels of physical exposures for job safety. In the future, pairing PATH frequencies and biomechanical modeling of the lumbar spine could also be applied to other industries to better understand physical exposures in the workplace.
KEY POINTS.
A physical workload index (PWI) was computed for nurses and nursing assistants (overall and while resident handling only) to evaluate the effects of a safe resident handling program (SRHP).
The PWI was calculated using frequencies of observational data regarding postures and manual handling and their resulting compressive forces on L5/S1.
The PWI for nursing assistants was 30% higher than that of nurses preintervention, and after 36 months, nursing assistants’ PWI was only 12% higher than that of nurses.
The PWI decreased by 24% for nursing assistants, by 41% for nursing assistants while resident handling, and by 2.5% for nurses 36 months after the SRHP began.
Future applications of the PWI include identifying high-risk tasks so further interventions could be considered and examining potential threshold levels of physical exposures for reducing the occurrence of musculoskeletal disorders.
ACKNOWLEDGMENTS
This study was supported by Grant No. U19-OH008857 from the U.S. National Institute of Occupational Safety and Health (NIOSH). The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official views of NIOSH. We thank Donna LaBombard and Deborah Slack-Katz for assistance with entry into the study sites and Susan Yuhas, Suzanne Nobrega, and Lindsay Casavant for liaising with centers. Jon Boyer, Scott Fulmer, Jamie Tessler, Kendra Kincaid, Sam Agyem-Bediako, Brad Schugardt, XiaoLu Jing, Narendra Vaidya, Michelle LaBoda, Alex Neusner, and Priyadarshini Dasgupta assisted with Postures, Activities, Tools, and Handling observations.
Biography
Alicia Kurowski is a postdoctoral research fellow in the Work Environment Department at the University of Massachusetts Lowell. She received an ScD in occupational ergonomics in 2011 from the University of Massachusetts Lowell.
Bryan Buchholz is a professor in the Work Environment Department and Biomedical Engineering and Biotechnology Program at the University of Massachusetts Lowell. He received a PhD in bioengineering in 1989 from the University of Michigan.
ProCare Research Team is affiliated with the Center for the Promotion of Health in the New England Workplace, University of Massachusetts Lowell, and University of Connecticut, Storrs.
Laura Punnett is a professor in the Work Environment Department at the University of Massachusetts Lowell. She received an ScD in occupational health and epidemiology in 1985 from the Harvard School of Public Health.
APPENDIX FREQUENCY SCORES FOR THE PHYSICAL WORKLOAD INDEX
Frequency Scores of Postures and Manual Handling for Nursing Assistants
| Nursing Assistants | ||||||
|---|---|---|---|---|---|---|
| Index Inputs | Baseline | 3 Months | 12 Months | 24 Months | 36 Months | |
| T2 | Moderate flexion | .155 | .141 | .154 | .129 | .081 |
| T3 | Severe flexion | .069 | .072 | .048 | .035 | .071 |
| T4 | Lateral bent/twist–neutral | .069 | .070 | .041 | .035 | .017 |
| T5 | Lateral bent/twist–flexed | .045 | .062 | .027 | .022 | .023 |
| A2 | 1 arm >60° | .190 | .192 | .137 | .130 | .083 |
| A3 | Both arms >60° | .133 | .159 | .113 | .086 | .060 |
| L3 | Shallow squat | .003 | .004 | .004 | .005 | .002 |
| L4 | Kneeling (one or both) | .002 | .003 | .001 | .001 | .003 |
| L5 | Walking | .237 | .290 | .234 | .256 | .287 |
| L6 | Deep squat | .010 | .007 | .007 | .006 | .009 |
| L7 | Lunge | .001 | .002 | .004 | .003 | .001 |
| Wu 1 | <4.55 kg (upright) | .633 | .624 | .703 | .752 | .770 |
| Wu 2 | 4.55–22.68 kg (upright) | .025 | .028 | .025 | .025 | .035 |
| Wu 3 | >22.68 kg (upright) | .002 | .001 | .001 | .001 | .003 |
| Wi 1 | <4.55 kg (inclined) | .216 | .202 | .194 | .160 | .157 |
| Wi 2 | 4.55–22.68 kg (inclined) | .042 | .057 | .031 | .025 | .016 |
| Wi 3 | >22.68 kg (inclined) | .010 | .016 | .003 | .002 | .001 |
Frequency Scores of Postures and Manual Handling for Nursing Assistants While Resident Handling
| Nursing Assistants (Resident Handling) |
||||||
|---|---|---|---|---|---|---|
| Index Inputs | Baseline | 3 Months | 12 Months | 24 Months | 36 Months | |
| T2 | Moderate flexion | .303 | .309 | .366 | .288 | .150 |
| T3 | Severe flexion | .181 | .177 | .124 | .084 | .111 |
| T4 | Lateral bent/twist–neutral | .078 | .074 | .045 | .040 | .019 |
| T5 | Lateral bent/twist–flexed | .126 | .164 | .065 | .041 | .050 |
| A2 | 1 arm >60° | .333 | .344 | .225 | .188 | .115 |
| A3 | Both arms >60° | .286 | .338 | .347 | .275 | .139 |
| L3 | Shallow squat | .013 | .011 | .008 | .011 | .006 |
| L4 | Kneeling (one or both) | .005 | .010 | .002 | .003 | .004 |
| L5 | Walking | .147 | .142 | .196 | .296 | .349 |
| L6 | Deep squat | .019 | .021 | .015 | .008 | .007 |
| L7 | Lunge | .003 | .002 | .006 | .004 | .005 |
| Wu 1 | <4.55 kg (upright) | .184 | .186 | .242 | .362 | .427 |
| Wu 2 | 4.55–22.68 kg (upright) | .110 | .079 | .144 | .171 | .227 |
| Wu 3 | >22.68 kg (upright) | .014 | .007 | .011 | .011 | .015 |
| Wi 1 | <4.55 kg (inclined) | .267 | .242 | .239 | .159 | .175 |
| Wi 2 | 4.55–22.68 kg (inclined) | .270 | .306 | .283 | .237 | .123 |
| Wi 3 | >22.68 kg (inclined) | .073 | .101 | .032 | .017 | .012 |
Frequency Scores of Postures and Manual Handling for Nurses
| Nurses |
||||||
|---|---|---|---|---|---|---|
| Index Inputs | Baseline | 3 Months | 12 Months | 24 Months | 36 Months | |
| T2 | Moderate flexion | .091 | .107 | .118 | .101 | .073 |
| T3 | Severe flexion | .048 | .035 | .043 | .019 | .068 |
| T4 | Lateral bent/twist–neutral | .048 | .069 | .045 | .032 | .028 |
| T5 | Lateral bent/twist–flexed | .019 | .030 | .025 | .007 | .006 |
| A2 | 1 arm >60° | .135 | .184 | .165 | .139 | .096 |
| A3 | Both arms >60° | .051 | .121 | .096 | .073 | .051 |
| L3 | Shallow squat | .002 | .001 | .004 | .004 | .000 |
| L4 | Kneeling (one or both) | .000 | .001 | .001 | .002 | .000 |
| L5 | Walking | .169 | .167 | .129 | .143 | .096 |
| L6 | Deep squat | .009 | .002 | .008 | .005 | .000 |
| L7 | Lunge | .000 | .000 | .004 | .002 | .000 |
| Wu 1 | <4.55 kg (upright) | .778 | .748 | .754 | .829 | .814 |
| Wu 2 | 4.55–22.68 kg (upright) | .014 | .010 | .014 | .010 | .006 |
| Wu 3 | >22.68 kg (upright) | .002 | .001 | .000 | .001 | .006 |
| Wi 1 | <4.55 kg (inclined) | .148 | .148 | .172 | .122 | .135 |
| Wi 2 | 4.55–22.68 kg (inclined) | .007 | .018 | .013 | .005 | .011 |
| Wi 3 | >22.68 kg (inclined) | .002 | .006 | .000 | .000 | .000 |
REFERENCES
- Boyer J (2008). Ergonomic exposures, socioeconomic status and musculoskeletal disorder risk among healthcare workers (Doctoral dissertation). Retrieved from ProQuest Dissertations & Theses database. (UMI No. 3326513) [Google Scholar]
- Buchholz B, Paquet V, Punnett L, Lee D, & Moir S (1996). PATH: A work sampling-based approach to ergonomic job analysis for construction and other non-repetitive work. Applied Ergonomics, 2, 177–187. [DOI] [PubMed] [Google Scholar]
- Burdorf A, & van der Beek AJ (1999). In musculoskeletal epidemiology are we asking the unanswerable in questionnaires on physical load? (Editorial). Scandinavian Journal of Work Environment and Health, 25, 81–83. [DOI] [PubMed] [Google Scholar]
- Garg A (1992). Occupational biomechanics and low-back pain. Occupational Medicine: State of the Art Review, 7, 609–628. [PubMed] [Google Scholar]
- Garg A, & Owen B (1992). Reducing back stress to nursing personnel: An ergonomic intervention in a nursing home. Ergonomics, 35, 1353–1375. [DOI] [PubMed] [Google Scholar]
- Hollmann S, Klimmer F, Schmidt KH, & Kylian H (1999). Validation of a questionnaire for assessing physical work load. Scandinavian Journal of Work Environment and Health, 25, 105–114. [DOI] [PubMed] [Google Scholar]
- Jager M, Luttmann A, & Lauring W (1991). Lumbar load during one-handed bricklaying. International Journal of Industrial Ergonomics, 8, 261–277. [Google Scholar]
- Janowitz IL, Gillen M, Ryan G, Rempel D, Trupin L, Swig L, Mullen K, Rugulies R, & Blanc PD (2006). Measuring the physical demands of work in hospital settings: Design and implementation of an ergonomics assessment. Applied Ergonomics, 37, 641–658. [DOI] [PubMed] [Google Scholar]
- Jones AL, Dwyer LL, Bercovitz AR, & Strahan GW (2009). The National Nursing Home Survey: 2004 overview (Vital and Health Statistics Series 13, No. 167). Atlanta, GA: National Center for Health Statistics. [PubMed] [Google Scholar]
- Kadaba MP, Ramakrishnan HK, Wooten J, Gainey G, Gorton G, & Cochran GVB (1989). Repeatability of kinematic, kinetic, and electromyographic data in normal adult gait. Journal of Orthopaedic Research, 7, 849–860. [DOI] [PubMed] [Google Scholar]
- Klimmer F, Kylian H, Hollmann S, & Schmidt KH (1998). Ein screening-verfahren zur beurteiluug kijlperlicher belastnng bei der arbeit [Screening method for the analysis of physical load during professional work]. Z Arbeitswiss, 52, 73–81. [Google Scholar]
- Klimmer F, Kylian H, Schmidt KH, Jordan C, Luttmann A, & Jäger M (2005). Musculoskeletal stress and strain of big samples with different workload: Comparison of methods. Z Arbeitswiss, 59, 1–12. [Google Scholar]
- Kurowski A, Boyer J, Fulmer S, Gore R, & Punnett L (2012). Changes in ergonomic exposures of nursing assistants after the introduction of a safe resident handling program in nursing homes. International Journal of Industrial Ergonomics, 42, 525–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lagerström M, Hansson T, & Hagberg M (1998). Work-related low-back problems in nursing. Scandinavian Journal of Work Environment Health, 24, 449–464. [DOI] [PubMed] [Google Scholar]
- Marras WS, Davis KG, Kirking BC, & Granata KP (1999). Spine loading and trunk kinematics during team lifting. Ergonomics, 42, 1258–1273. [DOI] [PubMed] [Google Scholar]
- Nabe-Nielsen K, Fallentin N, Christensen KB, Jensen JN, & Diderichsen F (2008). Comparison of two self-reported measures of physical work demands in hospital personnel: A cross-sectional study. BMC Musculoskeletal Disorders, 9, 61–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OHSAH. (2006). Development of a method for quantifying biomechanical risk factors associated with manual and mechanically assisted patient handling. Retrieved from http://www.ohsah.bc.ca/media/91-ES-AssistedPatientHandling.pdf
- Paquet V, Punnett L, & Buchholz B (2001). Validity of fixed-interval observations for postural assessment in construction work. Applied Ergonomics, 32, 215–224. [DOI] [PubMed] [Google Scholar]
- Park JK, Boyer J, Tessler J, Casey J, Schemm L, Gore R, & Punnett L (2009). Inter-rater reliability of PATH observations for assessment of ergonomic risk factors in hospital work. Ergonomics, 52, 820–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skotte JH, Essendrop M, Hansen AF, & Schibye B (2002). A dynamic 3D biomechanical evaluation of the load on the low back during different patient-handling tasks. Journal of Biomechanics, 35, 1357–1366. [DOI] [PubMed] [Google Scholar]
- Tak SW (2005). Variability in mechanical exposures in the construction industry (Doctoral dissertation). Retrieved from ProQuest Dissertations & Theses database. (UMI No. 3161158) [Google Scholar]
- Takala E-P, Pehkonen I, Forsman M, Hansson G-A, Mathiassen SE, Neumann WP, Sjøgaard G, Veiersted KB, Westgaard RH, & Winkel J (2010). Systematic evaluation of observational methods assessing biomechanical exposures at work. Scandinavian Journal of Work, Environment and Health, 36, 3–24. [DOI] [PubMed] [Google Scholar]
- Yuan L (2006). Biomechanical analysis of the physical loads on the low back and shoulder during drywall installation(Doctoral dissertation). Retrieved from ProQuest Dissertations & Theses database. (UMI No. 3239306) [Google Scholar]
- Zhuang Z, Stobbe TJ, Hsiao H, Collins JW, & Hobbs GR (1999). Biomechanical evaluation of assistive devices for transferring residents. Applied Ergonomics, 30, 285–294. [DOI] [PubMed] [Google Scholar]


