Dear Editor, We report three patients with refractory DM and calcinosis who were part of an open-label clinical trial [Study of Tofacitinib in Refractory Dermatomyositis (STIR)] [1] who also had improvement in their calcinosis that coincided with improvement on muscle MRI after 3 months of treatment.
Minimum Cutaneous Dermatomyositis Disease Area and Severity Index (CDASI) of >5 and/or Manual Muscle Testing-8 (MMT-8) <142 was required to enrol in the study. This study was approved by the Johns Hopkins Institutional Review Board and each patient gave written informed consent.
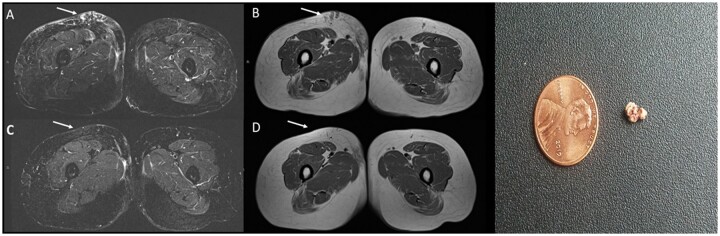
Patient 1 is a 50-year-old female with a history of NXP-2 positive refractory DM for 14 years prior to enrolment in the STIR study. Her initial presentation was manifested by proximal muscle weakness and dysphagia and classic rash including Gottron’s papules and V-neck sign. She developed calcinosis of the left calf within 3 months of the onset of her DM, which progressed to include her thighs. While she had improvement in her muscle disease with immunosuppression, her continued skin disease activity prompted entry into the STIR study. There was an improvement in her skin disease with tofacitinib (see CDASI scores in Supplementary Table S1, available at Rheumatology online). Her muscle strength was full power at entry into the study. On imaging, there was elevated signal of the intramuscular and subcutaneous reticular areas on baseline bilateral thigh muscle MRI. After 3 months of treatment, the patient noticed an improvement in her calcinosis in the calf and thighs, which was also confirmed on muscle MRI (Fig. 1A–D).
Fig. 1.
Patient 1 – a 50-year-old woman with dermatomyositis and calcinosis
Axial STIR (A) and T1-weighted images (B) through the bilateral thighs using myositis protocol performed at baseline reveal bilateral asymmetric right greater than left lower extremity skin thickening and reticular elevated STIR signal and confluent T1-hypointense signal in the right anteromedial thigh to the greatest extent (arrows). Note the close proximity of signal abnormality in the right anterior thigh to the skin surface. Superficial calcific masses can ulcerate and extrude calcium as seen in this patient. Axial STIR (C) and T1-weighted images (D) through the bilateral thighs using myositis protocol performed 3 months after treatment reveal decrease in subcutaneous signal abnormalities in both legs (arrows). Photograph (E) demonstrates the extruded calcium deposit from patient 1’s leg after treatment with tofacitinib.
Patient 2 is a 55-year-old female with TIF-1 γ positive refractory DM for 5 years prior to enrolment in the STIR study. Her initial presentation was manifested by proximal weakness and classic DM skin rashes (i.e. heliotrope rash and Gottron’s papules); ∼1 year after the onset of her DM she started to develop calcinosis in the abdomen and lower back. The prior immunosuppression treated her muscle disease but due to continued skin disease activity she was enrolled into the STIR study. She was also found to have calcinosis in her abdomen, lower back, neck and arm at the baseline visit. After 3 months of treatment, her CDASI improved to 2, and it was also noted that the small calcium deposits in the right arm had dissolved and calcinosis in the lower back was less painful. Decreased reticular signal was also observed in the thigh subcutaneous tissues on thigh muscle MRI at 3 months after treatment when compared with baseline images (Supplementary Fig. S1, available at Rheumatology online). In addition, right hip radiographs revealed decreased conspicuity and density of subcutaneous calcifications.
Patient 3 is a 35-year-old female with a history of NXP-2 positive refractory DM for 10 years prior to enrolment in the STIR study. Her initial presentation was manifested by proximal muscle weakness, and classic rash including Gottron’s papules and shawl sign. Within months after the rash, she also developed what she called ‘soft bumps’ in her arms and upper thighs. Due to continued active skin disease not responsive to immunosuppression, she was enrolled into the STIR study. She was also noted to have calcinosis in her arms, leg, abdomen, upper back and thighs. After 3 months of treatment, in addition to improvement in skin activity, it was noted that she had a decrease in the smaller calcium deposits in conjunction with a subjective ‘softening’ of the larger deposits in the arms and thighs. This also corresponded to decreased reticular signal on STIR sequences as well as T1-weighted sequences on muscle MRI (Supplementary Fig. S2, available at Rheumatology online).
In our case series of three patients, tofacitinib, a pan-JAK inhibitor, was correlated with clinical improvement in the treatment of DM cutaneous and muscle symptoms, as well as improvement in calcinosis. While the mechanism of calcinosis is not fully understood, there are hypotheses that dysregulated mitochondrial calcium storage and release mediated by the STAT 3 pathway may be contributing to the pathogenesis [2, 3]. Therefore, by using a pan-JAK inhibitor, not only are proinflammatory cytokines being inhibited, but the STAT 3 pathway inhibition may improve calcium regulation and contribute to the improvement in calcinosis.
On radiography [4, 5], calcinosis can manifest as sheet-like plaques or nodules within the skin, subcutaneous tissues, fascia or muscle, classically located along the extremities and buttocks, as evident in the radiographs for patient 2 in our series. On MRI, calcinosis follows a similar distribution exhibiting hypointense or dark signals on all sequences. There are two previous case reports of tofacitinib improving calcinosis in adult and juvenile DM [6]. Our case series further supports their findings and contributes to the plausibility that JAK inhibitors may have a direct effect on the pathophysiology of calcinosis.
In conclusion, our series highlights that JAK inhibitors may be an attractive therapeutic agent to be considered early in DM patients who may be at high risk for calcinosis.
Rheumatology key message
Tofacitinib, a pan-JAK inhibitor, demonstrated improvement of calcinosis in refractory dermatomyositis
Funding: J.J.P. and L.C.S. were supported in part by Pfizer Inc. This study was also supported in part by the NIH to J.J.P. K23AR0739.
Disclosures statement: J.J.P. and L.C.S. received research support from Pfizer Inc. M.S. and S.A. do not have any conflicts of interest.
Data availability statement
Data from this clinical trial can be made available upon request.
Supplementary data
Supplementary data are available at Rheumatology online.
Supplementary Material
References
- 1. Paik JJ, Casciola-Rosen L, Shin JY. et al. Study of Tofacitinib In Refractory Dermatomyositis (STIR): an open label pilot study of ten patients. Arthritis Rheumatol 2021;73:858–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Weinel S, Callen JP.. Calcinosis cutis complicating adult-onset dermatomyositis. Arch Dermatol 2004;140:365–6. [DOI] [PubMed] [Google Scholar]
- 3. Duvvuri B, Pachman L, Moore R, Doty S, Lood C.. Mitochondrial ROS as a regulator of calcinosis in juvenile dermatomyositis [abstract]. Arthritis Rheumatol 2020;72(Suppl 10). https://acrabstracts.org/abstract/mitochondrial-ros-as-a-regulator-of-calcinosis-in-juvenile-dermatomyositis/ (2 February 2021, date last accessed). [Google Scholar]
- 4. Blane CE, White SJ, Braunstein EM, Bowyer SL, Sullivan DB.. Patterns of calcification in childhood dermatomyositis. Am J Roentgenol 1984;142:397–400. [DOI] [PubMed] [Google Scholar]
- 5. Bowyer SL, Blane CE, Sullivan DB, Cassidy JT.. Childhood dermatomyositis: factors predicting functional outcome and development of dystrophic calcification. J Pediatr 1983;103:882–8. [DOI] [PubMed] [Google Scholar]
- 6. Sabbagh S, Almeida de Jesus A, Hwang S. et al. Treatment of anti-MDA5 autoantibody-positive juvenile dermatomyositis using tofacitinib. Brain J Neurol 2019;142:e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data from this clinical trial can be made available upon request.