Abstract
Background
As India is fighting against the second wave of COVID-19, Healthcare professionals are the front-line warriors on that battlefield which puts them under psychological pressure, this systematic review aims to critically look into and amalgamate the evidence on impact of COVID-19 on psychological health of healthcare professionals in India and to seek the attention of policymakers.
Methods
A systematic literature search was performed using the following databases PubMed, SCOPUS, Web of Science, Cochrane Library, ScienceDirect. Additionally, random search in Google, Google Scholar and ResearchGate was also performed until February 2021. The methodological quality of studies was assessed using Downs and Black for reporting quality. Meta-analysis was performed using revMAN. The review protocol is registered in PROSPERO and is available online.
Result
Prevalence of depression was found to be present in 41.90% of 5796 participants in five studies (95% Confidence Interval [CI]: 29.17 to 54.64), and prevalence of anxiety was found to be 42.87% common in 10 studies with a total sample size of 3059 people (95% Confidence Interval [CI]: 30.26 to 55.49), Stress was found to be prevalent (58.04%) in 12 studies with 4209 participants, (95% CI: 44.81–71.28), Prevalence of sleeping problem in 3 studies with 416 participants recorded a prevalence rate of 31.94 (95% CI: 21.38–42.49)
Conclusion
The COVID-19 pandemic has had a significant impact on people's mental and physical health, particularly among health-care workers. Authorities should develop programmes to help health-care workers improve their mental health.
Keywords: COVID-19, Mental health, Anxiety, Stress, Depression, India
1. Introduction
In December 2019, in a city of China called Wuhan has reported an outbreak of pneumonia caused by severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2). The clinical characteristics of the disease is unpredictable as it varies from person to person. It differs from asymptomatic to mild symptom and to severe case like pneumonia.1 , 2 On March 11, 2020 WHO (World Health Organisation) issued a statement that COVID-19 as a global pandemic because of the exponential spreading of COVID-19 disease and increased death rate.3 COVID-19 (Coronavirus disease) was declared as PHEIC (Public Health Emergency of International Concern) for those countries who have poor health infrastructure, as alert for emerging infectious disease.4 On 30 January 2020 India reported first case of COVID-19 in the state Kerala. Since then till now our health care workers struggle to provide better treatment and care.5 , 6
In the battle against COVID-19 health care workers are the first line workers, as they are involved in the treatment and all other patient related work which put them under pressure. Long duty hours without sufficient rest, heavy work load, shortage of Personal Protective Equipment's and the high spread of infection accounts for severe stress anxiety and psychological distress creating a negative impact on mental health of health care workers.7 The health care population was concerned about the contagious infection, as there was high chance of them to get infected since they are more exposed to the traumatic or stressful situation, which created an adverse effect on their mental health outcome.8,9 According to WHO, 21,89,46836 confirmed cases and 45,39,723 confirmed deaths of COVID-19 were reported across the globe on 3rd September 2021.10 In India, so far 32,90,3289 confirmed cases of COVID-19 were reported, with 43,98,95 confirmed deaths.11 Isolation, contact restrictions, and economic shutdown have all had a significant impact on the mental environment in the countries affected. Despite the fact that the current crisis may provide opportunity for personal growth and family bonding, many negatives outweigh these advantages. Anxiety, a lack of peer contact, and fewer opportunity to manage stress are all major problems. Aside from concerns and misgivings over COVID-19, the global economic situation has deteriorated, with high and rising unemployment rates. The current situation has a particularly negative impact on children, adolescents, and their families. Kindergartens and schools have been shuttered, social interactions have been severely restricted, and out-of-home leisure activities have been cancelled. Parents are encouraged to assist their children with home-schooling while working from home.12 , 13
The increasing number of cases, overload of work, depleting personal care equipment's and all other stressful situations together contributed to the burden of health care workers. They are worried about their family and friends, because of the high chance of them giving infection to their loved ones. All these thoughts add a huge impact on their mental health leading to a situation of stress, anxiety and depression symptoms. This could lead to long term impact on their psychological health.14 India is the second largest populated country in the world and, so it is critical to have access the mental health of Indian health care workers. Even though there are some studies already done on the topic but there is no review on this topic, for overall conclusion. Hence, we decided to conduct this systematic review on depression and anxiety associated with COVID- 19 pandemic among healthcare professionals in India.
2. Methods
Initially, all synonyms, search terms and entry terms resembling to the population (healthcare workers), condition (COVID-19), outcome (psychological stress, anxiety, depression other mental health data, were collected from various sources such as Pub Med (Medical subject heading [MeSH] Terms), ClinicalTrials.gov and the previous systematic reviews. The following electronic databases were searched, MEDLINE (PubMed), the Cochrane Library, Scopus, and Web of Science. Article language were limited to English. Bibliography of all the included studies and a random search in Google, Google Scholar and Research Gate were performed to find any other relevant studies.
2.1. Inclusion and exclusion criteria
Studies which are published in English which is of full text and conducted in India were included. Studies published in non-English language and that were conducted outside India was excluded.
2.2. Study selection
Every article was screened by reading title and abstract to find if the article meets the criteria for inclusion. All duplicates were removed and Screening of articles was performed to find out whether articles pass the inclusion criteria under the types of studies, participants, interventions, settings, and outcomes. First and second authors separately screened title of all studies, if the title did not mention about country, population and intervention then abstract screening was done if the abstract did not mention then full text screening was done on the time of first pass only, as it is anyway required to read the full article for the screening. If an article was excluded, the reason was noted, the third author screened all the selected studies. Total of 23 studies were included for quality evaluation.
2.3. Quality evaluation
Risk of bias/methodological quality was checked differently by first and second authors and reviewed by a third author using the following tools: Downs and Black checklist for observational studies was used to assess the methodological quality. It contains 27 questions which has to be graded as “Yes”, “No” and “Unable to determine” as per the available information. Previously, studies have used a modified version by simplification of the power question and awarding only 1 point if a study had adequate power to recognize a clinically significant effect, where the probability value for difference being due to chance is <5%, if a study did not mention statistical power, it was deemed either “no” or “unable to determine” and given a score of 0. There are 5 sections which includes the study quality (10 items), external validity (3 items), study bias (7 items), confounding and selection bias (6 items), and power (1 item). Each question if answered “yes” gets a score of 1, except for the 5th question which can get a score of 2 if answered “yes”.15
2.4. Data extraction
Data retrieval was performed on a pilot-tested standardized form on Microsoft Excel by first author and reviewed by second and a third author. We extracted data according to authors, year of publication, country of study, pandemic, design and method, participants, mental health issues, context, to extract information about the interventions used to address stress, anxiety and mental health), and key result. A narrative summary and tables (Table no-1) were used to summarize the characteristics and results of included studies.
2.5. Statistical analysis
RevMan 5.3 was used for 5 meta-analyses. The number of events and total number of participants were used for prevalence outcome and results were presented in terms of prevalence rate with 95% confidence interval (CI), whereas mean with standard deviation (SD) were used for continuous outcomes and results were presented as mean along with 95% CI. We used the fixed effect model in case of non-significant heterogeneity (I2<50; P > 0.1), whereas a random effect model was employed in this study in case of substantial heterogeneity (I2>50%; P < 0.10)16 We could not perform subgroup analysis due to insufficient data, though it was planned. Sensitivity analysis was not performed as the effect size was in percentage along with 95% confidence interval.
Funnel plot was used for the visual inspection of publication bias. It is a form of scatter plot with a single point for each study, in which X-axis denoting the prevalence rate and the Y-axis representing the study precision, commonly standard error.
3. Result
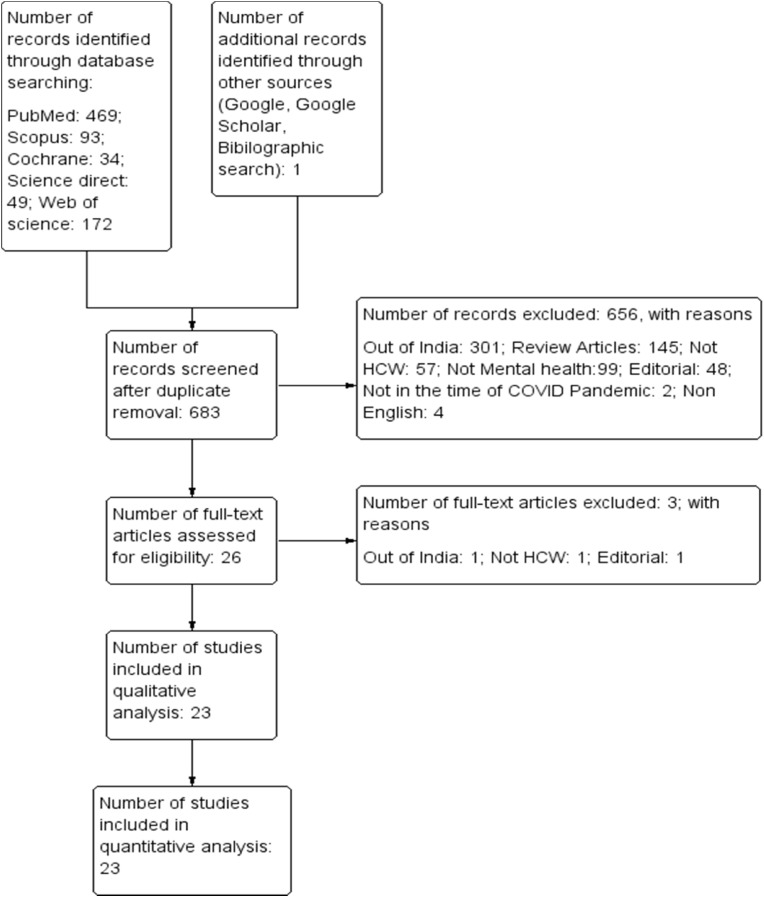
After eliminating 135 duplicates from 818 studies, the remaining 638 studies were screened for the title, abstract, and full text out of which 654 were omitted due to irrelevant content. 26 articles with full text were screened and 3 omitted as it was not fulfilling the criteria. This review included 23 full-text articles, as shown in detail in the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow-chart in Fig. 1 . Details and characteristics of these articles are also provided in Table 1 .
Fig. 1.
The PRISMA Flow diagram for study selection.
Table 1.
Characteristics of the included studies.
| Author & Year | Study Design | Type of Questionnaire used/Measures | Type of Participants (%) | City/state of study | Depression% | Anxiety% | Stress% | Result/conclusion |
|---|---|---|---|---|---|---|---|---|
| Rehman U et al., 202117 | Online survey n = 403 | Family Affluence Scale Response Accuracy Scale Depression Anxiety Stress Scale |
Students (34.4%) Teachers (12.6%) Researchers (7.6%) Mental health professionals (8.4%) Health professionals (Doctors and Nurses) (8.1%) Corporate job workers (8.6%) |
Not mentioned | NA | NA | NA | Among various professional's health care professionals were found to have more depression, anxiety and stress. |
| George C.E et al., 202018 | Mixed methods survey n = 87 | Mixed methods research with a quantitative (QUAN)design Paradigm nested in the primary qualitative (QUAL) design |
Doctors (31.3%) Nurses (21.9%) Allied health Professionals (15.6%) Field staff (21.9%) Others (9.3%) |
Bangalore | NA | 73.4% | 62.5% | Fear of getting infection to their family, fear of death, and exhaustion were the main reason for stress among HCW |
| Shetty A et al., 202019 | Questionnaire-based online survey n = 405 | Validated questionnaire (seventeen questions divided into two sections first regarding the demographic data of the dentists and the second comprised of questions that aimed to assess anxiety levels and attitudes toward COVID-19 and the subsequent infection control practices in dentistry.) | Dentists | Not mentioned | NA | NA | NA | Age of the dental clinicians was found to be a positive factor and directly proportional to a high anxiety score. The response scores of anxieties in this study indicate greater psychological pressure on the dentists due to uncertainty of progression of the pandemic |
| Suryavanshi N et al., 202020 | Structured online survey n = 197 | Patient Health Questionnaire (PHQ‐9) Generalized Anxiety Disorder (GAD‐7) questionnaire ne‐item quality of life (QoL‐1) visual analogue scale multiple‐choice question by Shwu‐Hua Lee in Taiwan during the SARS outbreak |
Para clinical (13%) Resident/intern (29%) Nurse (24%) Physician (34%) |
Maharashtra | 22% | 29% | NA | Most of the HCW reported of having high anxiety, depression, and low quality of life (QOL). Work stress was found to be a factor for increased anxiety, depression, and low QOL. |
| Sil A et al., 202021 | Cross-sectional study n = 41 | Patient Health Questionnaire (PHQ‐9) Perceived Stress Scale(PSS) |
Dermatologists | Not mentioned | 26.82% | NA | 29.2% | Long working time and lack of proper rest due to posting in COVID-positive ward shows a high prevalence of stress among HCW. those who were away from family also showed similar result. |
| Saraswathi I et al., 202022 | Prospective longitudinal study n = 217 | Depression Anxiety Stress Scale 21 Items (DASS21) Pittsburgh Sleep Quality Index self-administered questionnaire |
Undergraduate medical students | Not mentioned | 35.5% | 33.2% | 24.9% | Because of the CoV-19 outbreak and quarantine, stress and anxiety levels shown to be increased in HCW, and depression symptoms remained unaltered |
| Das A et al., 202023 | A cross-sectional, observational study n = 422 | Patient Health Questionnaire (PHQ‐9) Perceived Stress Scale (PSS) |
Doctors | North: New Delhi; West: Nagpur, Maharashtra; and South: Thiruvananthapuram, Kerala East: Kolkata, West Bengal; |
63.5% | NA | 45% | Long working hours and staying away from families reported to have a significant role in high-stress levels. Unmarried doctors showed high stress levels. |
| Dhingra V et al., 202024 | n = 231 | Psychological Well Being (PWB) Scale PSS Subjective Happiness Scale. |
Physicians (44.1%) Nurses (35%) Paramedical staff (20.7%) |
Northern India | NA | NA | NA | The findings show that perceived stress has a considerable impact on psychological well-being, with subjective happiness serving as a mediating factor. Physicians' and health-care employees' psychological well-being is completely mediated by subjective happiness. |
| Sharma R et al., 202025 | Questionnaire-based observational cross-sectional study n = 200 | 21-item depression anxiety stress scale (DASS scale) | HCWs working in a tertiary care unit | Not mentioned | 72% | 85% | 82% | HCW shows high DASS score than administrative staff. Staying away from family, and children, and fear of transition of infection to family members contributed to factors that increased the DASS score. |
| Bansal A et al., 202026 n = 112 | Cross-sectional study | Screening Questionnaire for Disaster Mental Health | HCW (Faculty, postgraduate students, nursing, and paramedical staff) | Jaipur | 94.6% | NA | 94.6% | Front line health care workers in the hospital at the time of COVID-19 showed post-traumatic stress disorder and depression. |
| Bajaj J et al., 202027 | Cross-sectional survey n = 51 | 26-item self-administered Questionnaire | All level doctors of all specialties in Mumbai | Mumbai | NA | NA | NA | Medical doctors interfering with CoV-19 confirmed patients are at high risk of getting infected and that caused a major impact on the physical and psychological health of medical doctors |
| Gupta S et al., 202028 | Cross sectional survey n = 749 | Hospital anxiety and depression scale (HADS) | Doctors at Armed Forces across India | Not mentioned | 28.2% | 35.2% | NA | Anxiety and depression symptoms were increased among armed forces doctors at the time of CoV-19. The risk factors were young age group, non-clinical specialities, female gender, and having doctoral degree |
| Chatterjee S.S et al., 202029 | Cross-sectional, observational study n = 152 | Semi-structured pro forma, Depression, Anxiety, and Stress Scale-21. (DASS)-21 | Doctors in West Bengal | West Bengal. | 34.9% | 39.5% | 32.9% | Duty time, using personal protective instruments and altruistic coping are factors that contributed to increase level of stress anxiety, and depression. |
| Sahu D et al., 202030 | Online anonymous survey n = 611 | The survey consisted of 3 mandated demographic questions and 10 other optional question | Orthopaedic surgeons | Not mentioned | NA | NA | 63% | Among orthopaedic surgeons, the young age group showed more stressed out because of imbalance in life and uncertainty on returning to work. |
| Nair A.K.R et al., 202031 | Online survey n = 586 | COVID-19 Peri-traumatic Distress Index and Perceived stress scale | Indian endodontists | Not mentioned | NA | NA | 80% | In the time of COVID-19 related lockdown 1-in- 2 endodontists had distressed and 4-in-5 had perceived stress. Among them, female endodontists had more perceived stress than males. |
| Grover R et al., 202032 | Cross-sectional survey | DASS −21 questionnaire n = 144 | Ophthalmologists in India | Not mentioned | 53% | 52% | 14% | All of the ophthalmologists (64.2%) suffered from mental health problems. Among them, 52.7 had depression and anxiety and 14% had stress. Above 40 years old with more than 10 of experience showed high stress. |
| Nathiya D et al., 202133 | Descriptive quantitative cross-sectional, web-based study n = 418 | Impact of event scale-revised Connor-Davidson resilience scale The professional quality of life Feelings of health care worker during COVID-19 outbreak was assessed by the adapted questionnaire by Cai H et al. in a Chinese study |
Healthcare workers from different departments of hospital | Not mentioned | NA | NA | NA | Female nurses and doctors employed in the emergency division were reported to have high risk of psychological distress. |
| Khanna RC et al., 202034 | Online survey | PHQ-9 n = 2355 | Ophthalmologists | Karnataka, Kerala, Maharashtra, Tamil Nadu, Telangana, Uttar Pradesh, West Bengal, Andhra Pradesh, Delhi, Gujarat. | 32.6% | NA | NA | Ophthalmologists of younger age, female and those who not practice shows significantly high depression. |
| Nanjundaswamy MH et al., 202035 | Survey n = 106 | Questionnaire on stress and anxiety during CoV-19 pandemic | Junior and senior psychiatry resident doctors | South India | NA | 35% | NA | Among psychiatry trainees, 29% reported afraid to go home and 13% feared of stigma, 35% had anxiety, loneliness, and sadness |
| Podder I et al., 202036 | Web‐based cross‐sectional study n = 384 | Stress assessment (Perceived Stress Scale (PSS-10) | Dermatologists (37.5%) and other physicians (62.5%) | Across Eastern India | NA | NA | 85.9% | Perceived stress was higher in non-dermatologists than dermatologists. Also, high perceived stress was seen in females and unmarried doctors. Fear of getting the infection, fear of transferring the infection to family and co-workers, and lack of protective instruments were the cause of increased stress |
| Mishra S et al., 202037 | Cross-sectional online questionnaire-based survey n = 1253 | PSS | Dentists | Chhattisgarh | NA | NA | 79.24% | Among dental professionals the PSS score were increased during CoV-19 pandemic. The main risk factor identified was they can't touch their family members because of the prolonged working hours |
| Pandey U et al., 202038 | Cross-sectional survey n = 83 | Depression—PHQ-9 Anxiety GAD-7 scale |
Medical students and junior doctors of the Obstetrics and Gynaecology department | Varanasi | 7.3% | 9.8% | NA | Female gender reported high anxiety and depression than male. Direct contact with Cov-19 patient not affected doctors psychologically |
| Gupta S et al., 202039 | Prospective study n = 1124 | Questions about the COVID-19 pandemic Hospital Anxiety and Depression Scale |
Doctors (0.8%) Nurses (18.4%) Paramedics (12%) Administrators (2.04%) Supporting staff members (0.88%) |
Not mentioned | 31.4% | 37.2% | NA | Prevalence of anxiety and depression was reported as 37.2% and 31.4% respectively. Following were reported as risk factors of anxiety female, age group between 20 and 35 years, unmarried. Risk factors of depression were age group and employment at primary care hospital. |
3.1. Risk of bias in included studies
The Risk of bias assessment was performed using Downs and Black checklist. Downs and Black checklist were used to assess the quality of original or primary source research article. A total of five sections of questions are included. 1.Reporting 2. External validity 3. Internal validity-bias 4. Internal validity – confounding 5. Power. Out of 27 questions, 16 Questions were only eligible for our study as few questions were not relevant for the studies included in our review; hence the total score was 17. Out of that 2 (8%) studies scored 16 point, 6 (26%) studies scored 15 points, 4 (17.3%) studies scored 14 points, 3 (13%) studies scored 13 points, 1 (4.3%) study scored 12 point, 3 (13%) studies scored 11 points, 1 (4.3%) study scored 10 points, and 1 (4.3%) study scored 6 points (Table 2 ).
Table 2.
Downs and blacks checklist.
| Studies | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | 26 | 27 | TS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rehman U et al., 2021 | 1 | 1 | 1 | NA | 2 | 1 | 1 | NA | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | NA | 1 | NA | 1 | NA | NA | NA | 0 | NA | 1 | 0 | 15 |
| George C.E et al., 2020 | 1 | 1 | 1 | NA | 2 | 1 | 0 | NA | 0 | 0 | 0 | 1 | NA | NA | NA | 1 | NA | 1 | NA | 1 | NA | NA | NA | 0 | NA | 1 | 0 | 11 |
| Shetty A et al., 2020 | 1 | 1 | 1 | NA | 2 | 0 | 1 | NA | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | NA | 1 | NA | 1 | NA | NA | NA | 0 | NA | 1 | 1 | 15 |
| Suryavanshi N et al., 2020 | 1 | 1 | 1 | NA | 2 | 1 | 1 | NA | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | NA | 1 | NA | 1 | NA | NA | NA | 0 | NA | 1 | 0 | 15 |
| Sil A. et al., 2020 | 0 | 1 | 1 | NA | 2 | 1 | 1 | NA | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | NA | 1 | NA | 1 | NA | NA | NA | 0 | NA | 1 | 0 | 13 |
| Saraswathi I. et al., 2020 | 1 | 1 | 1 | NA | 2 | 1 | 1 | NA | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | NA | 1 | NA | 1 | NA | NA | NA | 0 | NA | 1 | 0 | 15 |
| Dhingra V | 1 | 1 | 1 | NA | 2 | 1 | 1 | NA | 0 | 1 | 0 | 0 | NA | NA | NA | 1 | NA | 1 | NA | 1 | NA | NA | NA | 0 | NA | 0 | 0 | 11 |
| Sharma R et al. | 1 | 1 | 1 | NA | 0 | 1 | 0 | NA | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | NA | 1 | NA | 1 | NA | NA | NA | 0 | NA | 1 | 0 | 12 |
| Bansal A et al. | 1 | 1 | 1 | NA | 0 | 0 | 0 | NA | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | NA | 1 | NA | 1 | NA | NA | NA | 0 | NA | 1 | 0 | 11 |
| Bajaj J et al. | 1 | 1 | 1 | NA | 2 | 0 | 0 | NA | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | NA | 1 | NA | 1 | NA | NA | NA | 0 | NA | 1 | 0 | 13 |
| Gupta S et al. | 1 | 1 | 1 | NA | 2 | 1 | 1 | NA | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | NA | 1 | NA | 1 | NA | NA | NA | 0 | NA | 1 | 1 | 16 |
| Chatterjee S.S et al. | 1 | 1 | 1 | NA | 2 | 1 | 1 | NA | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | NA | 1 | NA | 1 | NA | NA | NA | 0 | NA | 1 | 0 | 14 |
| Sahu D et al. | 1 | 0 | 1 | NA | 0 | 1 | 0 | NA | 1 | 1 | 1 | 0 | NA | NA | NA | 1 | NA | 1 | N1 | 1 | NA | NA | NA | 0 | NA | 1 | 0 | 10 |
| Nair A.K.R et al. | 1 | 1 | 1 | NA | 2 | 1 | 1 | NA | 1 | 0 | 1 | 1 | NA | NA | NA | 1 | NA | 1 | NA | 1 | NA | NA | NA | 0 | NA | 1 | 0 | 14 |
| Grover R et al. | 1 | 1 | 1 | NA | 2 | 1 | 1 | NA | 1 | 0 | 1 | 1 | NA | NA | NA | 1 | NA | 1 | NA | 1 | NA | NA | NA | 0 | NA | 1 | 0 | 14 |
| Nathiya D et al. | 1 | 1 | 1 | NA | 2 | 1 | 1 | NA | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | NA | 1 | NA | 1 | NA | NA | NA | 0 | NA | 1 | 0 | 15 |
| Khanna RC et al. | 1 | 1 | 1 | NA | 2 | 1 | 0 | NA | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | NA | 1 | NA | 1 | NA | NA | NA | 0 | NA | 0 | 0 | 13 |
| Nanjundaswamy MH et al. | 1 | 0 | 1 | NA | 0 | 0 | 0 | NA | 0 | 0 | 1 | 1 | NA | NA | NA | 1 | NA | 1 | NA | 0 | NA | NA | NA | 0 | NA | 0 | 0 | 6 |
| Podder I et al. | 1 | 1 | 1 | NA | 2 | 1 | 1 | NA | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | NA | 1 | NA | 1 | NA | NA | NA | 0 | NA | 0 | 0 | 14 |
| Mishra S et al. | 1 | 1 | 1 | NA | 2 | 1 | 1 | NA | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | NA | 1 | NA | 1 | NA | NA | NA | 0 | NA | 1 | 1 | 16 |
| Pandey U et al. | 1 | 1 | 1 | NA | 2 | 1 | 0 | NA | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | NA | 1 | NA | 0 | NA | NA | NA | 0 | NA | 0 | 0 | 12 |
| Gupta S., Prasad A.S et al. | 1 | 1 | 1 | NA | 2 | 1 | 0 | NA | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | NA | 1 | NA | 1 | NA | NA | NA | 0 | NA | 1 | 1 | 15 |
Score 16 point – 2 studies, score 15 points – 6 studies, score 14 points- 4 studies, score 13 points- 3 studies Score 12 points- 1 study, score 11 points- 3 studies, score 10 points- 1 study, Score 6 points- 1 study.
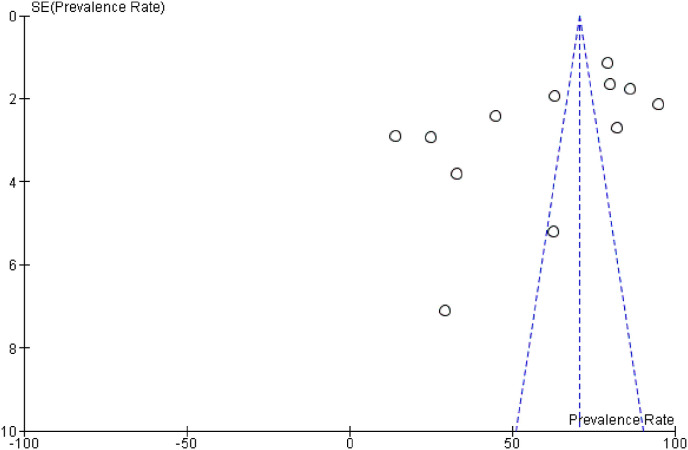
3.2. Investigating heterogeneity and publication bias
To investigate the heterogeneity of the studies, the I2 (%) indices for the prevalence of stress (I2: 99%), anxiety (I2: 98%), depression (I2: 99. %), Worry (I2:93%), Sleeping problem (I2:81%) and Fear (I2:94%) were obtained. Due to the high heterogeneity in the studies, the random effects model was used in the analysis of findings. Visual inspection of the funnel plots revealed an obvious asymmetry, which indicates that there is a chance of publication bias in the included studies (Fig. 2 ).
Fig. 2.
Funnel plot for publication bias.
3.3. Meta-analysis
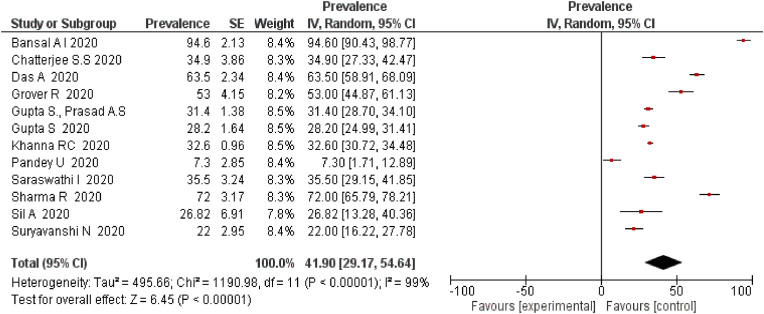
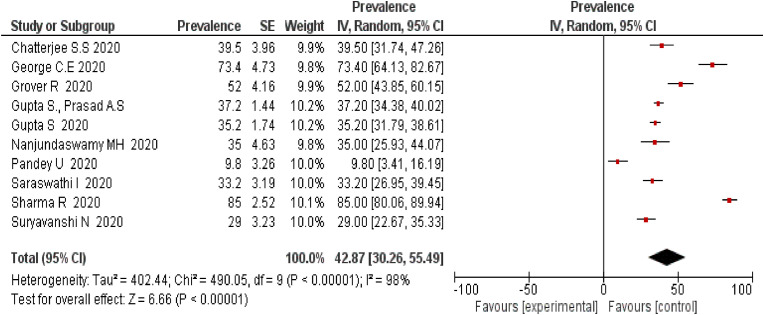
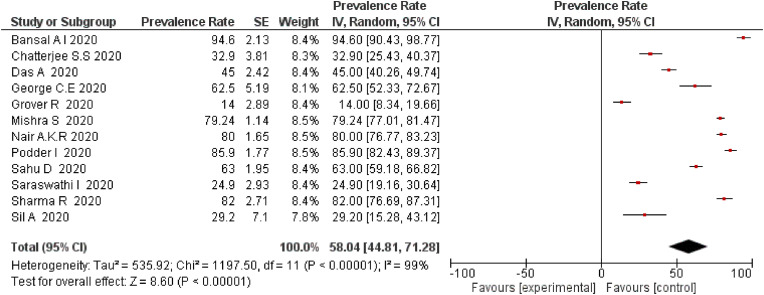
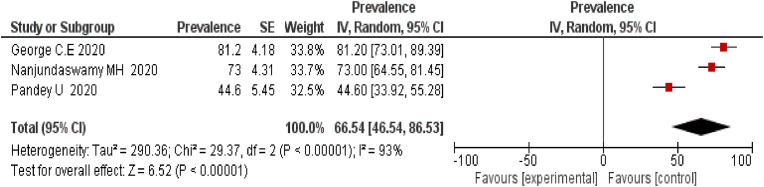
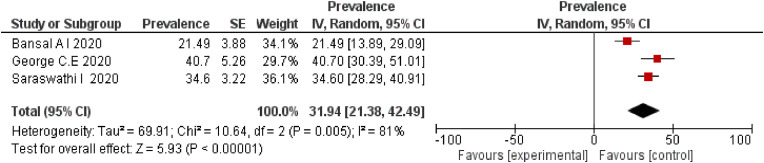
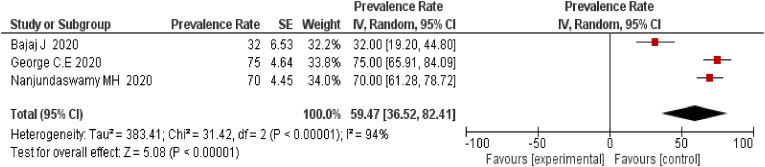
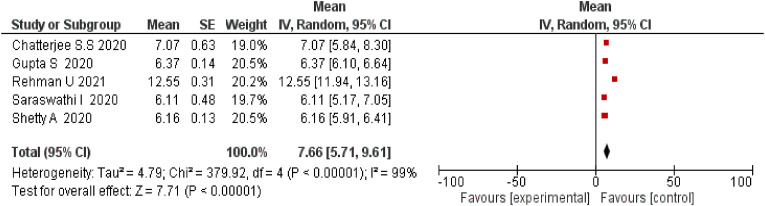
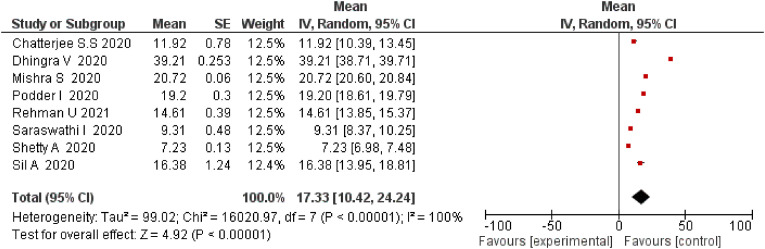
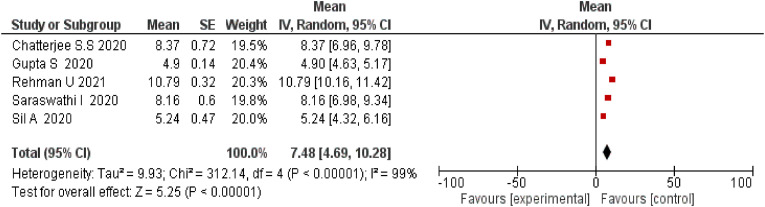
Prevalence of depression among 5796 participants in 5 studies was 41.90% (95% Confidence Interval [CI]: 29.17 to 54.64)(Fig. 3 ), Prevalence of anxiety in 10 studies with sample size of 3059 was 42.87% (95% Confidence Interval [CI]: 30.26 to 55.49)(Fig. 4 ), Prevalence of stress in 12 studies with 4209 participants recorded a prevalence rate of 58.04 (95% CI: 44.81–71.28)(Fig. 5 ), Prevalence of worry in 3 studies with 276 participants demonstrated a prevalence rate of 66.54 (95% CI: 46.54–86.53)(Fig. 6 ), Prevalence of sleeping problem in 3 studies with 416 participants recorded a prevalence rate of 31.94 (95% CI: 21.38–42.49)(Fig. 7 ), Prevalence of fear in 3 studies with 244 participants recorded a prevalence rate of 59.47 (95% CI: 36.52–82.41)(Fig. 8 ). 5 studies with 1926 participants reported that the overall mean score for anxiety was found to be 7.66 (95% CI: 5.71–9.61) (Fig. 9 ), 8 studies with 3086 participants reported that the overall mean score for stress was found to be 17.33 (95% CI: 10.42–24.24) (Fig. 10 ), 5 studies with 1562 participants reported that the overall mean score for depression was found to be 7.48 (95% Confidence Interval: 4.69–10.28) (Fig. 11 ).
Fig. 3.
Prevalence rate of depression among HCW during COVID-19.
Fig. 4.
Prevalence rate of anxiety among HCW during COVID-19.
Fig. 5.
Prevalence rate of stress among HCW during COVID-19.
Fig. 6.
Prevalence rate of worry among HCW during COVID-19.
Fig. 7.
Prevalence rate of sleeping problems among HCW during COVID-19.
Fig. 8.
Prevalence rate of fear among HCW during COVID-19.
Fig. 9.
The level of anxiety among HCW during COVID-19.
Fig. 10.
The level of stress among HCW during COVID-19.
Fig. 11.
The level of depression among HCW during COVID-19.
4. Discussion
COVID-19 pandemic has become a serious problem of mental anguish in healthcare workers (HCW). HCW are suffering from stress, depression, anxiety, insomnia due to the Cov-19 pandemic.40 , 41 Gender, age, place of work, profession, department of work are associated with the increased anxiety, stress and insomnia in Health Care Workers at the time of COVID-19 is an independent risk factor for getting stress among HCW.40 Extended working hours, emergency calls, a quarantine, and separation from friends due to professional commitments puts HCW under extreme stress, anxiety, and frustration. They are more worried for their thoughts as like, they might transfer infection to their loved ones and others.42 After checking the article by standardise and random search we understand, this is the first review which reviewing of depression and anxiety associated with COVID-19 pandemic among healthcare professionals in India.
When compared to exiting systematic review and meta-analysis, 13 studies with 33,062 participants found 23.2% pooled anxiety in 12 studies, and 22.8% pooled depression in 10 studies.43 In our study pooled prevalence of anxiety was 42.87% in 10 studies and pooled prevalence of depression was 41.9% in 12 studies.
A study done by Gonzalo Salazar de Pablo et al.44 found HCW has gone through on 43.7% fear, 37.9% insomnia, 34.4% burnout, 37.8% psychological distress, 29.0% anxiety, 26.3% depressive symptoms. In our study we could find HCW has gone through 66.54% worry, 31.94% sleep problems, 59.47% fear.
In this review, we could find that the health care workers are going through serious mental health care problems. There are so many confounding factors found in health care sectors and within HCWs, that include HCWs have a high chance of getting the infection so also spreading infection, HCW have cared about their family and friend, so they are worried about spreading the infection to them.18 , 25 , 36
COVID-19 pandemic stuck the normal flow of health care sectors, because of the sudden outbreak had lack of protective instruments, HCW worked over time and they are forced to work in COVID-19 ward these factors influenced HCW to tend to fall on depression and anxiety.17 , 21 , 23 , 29
HCW working with COVID-19 patients despite they have worn protective instruments they should go to quarantine. Which puts them through mental health problems like depression anxiety, and stress.22 COVID-19 outbreak affected more on females, young and unmarried HCW. These factors show direct relation on high depression and stress level.33 , 28 , 34 , 31 , 30 , 19 , 23 , 38 ,and 39
The inherent heterogeneity across research is a fundamental disadvantage that should be considered. This is the first comprehensive study and meta-analysis of the pooled prevalence of depression and anxiety among HCW in India during the COVID-19 outbreak that we are aware of. Despite the fact that multiple research used the same tests, different assessment scales and cut-offs were used for population screening. Another drawback is that while numerous studies were conducted in the same region/country, they may have included the same population.
5. Conclusion
The mental health problems among HCW during the COVID-19 were ranged from 30% to 60%. There should be a better plan to mitigate the impact of COVID-19 on HCW and appropriate counselling should be provided to overcome the mental health issues among HCW. More interventions need to be implemented which can tackle the mental health problem among HCW. The government should give psychological assistance, cut working hours, and hire more people, as well as provide free medical care if necessary. All of these resources can help health-care employees deal with mental health issues. The findings of this study can be used to quantify staff support needs and to inform tiered and personalised treatments that improve resilience and reduce susceptibility in pandemic situations.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors report no conflicts of interest.
Acknowledgement
Authors would like to thank Mr. Muhammed Rasheed, Research Scholar, Manipal College of Pharmaceutical Sciences, Manipal Academy of Higher Education for the support and help provided.
References
- 1.Mahalmani V.M., Mahendru D., Semwal A., et al. COVID-19 pandemic: a review based on current evidence. Indian journal of pharmacology. 2020 Mar;52(2):117. doi: 10.4103/ijp.IJP_310_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou P., Yang X.L., Wang X.G., et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. nature. 2020 Mar;579(7798):270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cucinotta D., Vanelli M. WHO declares COVID-19 a pandemic. Acta Bio Medica: Atenei Parmensis. 2020;91(1):157. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jee Y. WHO international health regulations emergency committee for the COVID-19 outbreak. Epidemiology and health. 2020:42. doi: 10.4178/epih.e2020013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kakar A., Nundy S. COVID-19 in India. Journal of the Royal Society of Medicine. 2020 Jun;113(6):232–233. doi: 10.1177/0141076820927668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martin AL, Natalia ES, Ana MA. The SARS-CoV-2 coronavirus and the COVID-19 outbreak. International braz j urol: official journal of the Brazilian Society of Urology.;46. [DOI] [PMC free article] [PubMed]
- 7.Evanoff B.A., Strickland J.R., Dale A.M., et al. Work-Related and personal factors associated with mental well-being during the COVID-19 response: survey of health care and other workers. Journal of medical Internet research. 2020;22(8) doi: 10.2196/21366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bohlken J., Schömig F., Lemke M.R., Pumberger M., Riedel-Heller S.G. COVID-19 pandemic: stress experience of healthcare workers-a short current review. Psychiatrische Praxis. 2020 Apr 27;47(4):190–197. doi: 10.1055/a-1159-5551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rossi R., Socci V., Pacitti F., et al. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA network open. 2020 May 1;3(5) doi: 10.1001/jamanetworkopen.2020.10185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WHO 2021 6 September. 2021. https://covid19.who.int/
- 11.WHO 2021 6 September. 2021. https://covid19.who.int/region/searo/country/in
- 12.Fegert J.M., Vitiello B., Plener P.L., Clemens V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child and adolescent psychiatry and mental health. 2020 Dec;14 doi: 10.1186/s13034-020-00329-3. 1-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.OECD 2021 31 March 2020 OECD policy responses to coronavirus (COVID-19) COVID-19: protecting people and societies. https://www.oecd.org/coronavirus/policy-responses/covid-19-protecting-people-and-societies-e5c9de1a/#biblio-d1e2308
- 14.Lai J., Ma S., Wang Y., et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA network open. 2020 Mar 2;3(3) doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Downs S.H., Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. Journal of Epidemiology & Community Health. 1998 Jun 1;52(6):377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Review Manager (RevMan) The Nordic Cochrane Centre, The Cochrane Collaboration; Copenhagen: 2014. [Computer Program]. Version 5.3. [Google Scholar]
- 17.Rehman U., Shahnawaz M.G., Khan N.H., et al. Depression, anxiety and stress among Indians in times of Covid-19 lockdown. Community mental health journal. 2021 Jan;57(1):42–48. doi: 10.1007/s10597-020-00664-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.George C.E., Inbaraj L.R., Rajukutty S., de Witte L.P. Challenges, experience and coping of health professionals in delivering healthcare in an urban slum in India during the first 40 days of COVID-19 crisis: a mixed method study. BMJ open. 2020 Nov 1;10(11) doi: 10.1136/bmjopen-2020-042171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shetty A., Bhat R., Shetty P., Hegde M.N., Nayak U.K., D’souza N. The psychological impact of the COVID-19 pandemic on dental healthcare professionals. Journal of International Oral Health. 2020 Nov 1;12(8):98. [Google Scholar]
- 20.Suryavanshi N., Kadam A., Dhumal G., et al. Mental health and quality of life among healthcare professionals during the COVID‐19 pandemic in India. Brain and behavior. 2020 Nov;10(11) doi: 10.1002/brb3.1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sil A., Das A., Jaiswal S., et al. Mental health assessment of frontline COVID‐19 dermatologists: a Pan‐Indian multicentric cross‐sectional study. Dermatologic Therapy. 2020 Jun 22 doi: 10.1111/dth.13884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Saraswathi I., Saikarthik J., Kumar K.S., Srinivasan K.M., Ardhanaari M., Gunapriya R. Impact of COVID-19 outbreak on the mental health status of undergraduate medical students in a COVID-19 treating medical college: a prospective longitudinal study. PeerJ. 2020 Oct 16;8 doi: 10.7717/peerj.10164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Das A., Sil A., Jaiswal S., et al. A study to evaluate depression and perceived stress among frontline Indian doctors combating the COVID-19 pandemic. The primary care companion for CNS disorders. 2020 Oct 8;22(5) doi: 10.4088/PCC.20m02716. [DOI] [PubMed] [Google Scholar]
- 24.Dhingra V, Dhingra M. Effect of perceived stress on psychological well-being of health care workers during COVID 19: mediating role of subjective happiness. European Journal of Molecular & Clinical Medicine.;7(02):2020.
- 25.Sharma R., Saxena A., Magoon R., Jain M.K. A cross-sectional analysis of prevalence and factors related to depression, anxiety, and stress in health care workers amidst the COVID-19 pandemic. Indian Journal of Anaesthesia. 2020 Sep;64(Suppl 4):S242. doi: 10.4103/ija.IJA_987_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bansal A., Jain S., Sharma L., Kumar M., Sharma A. A cross-sectional study to assess the psychosocial impact of COVID-19 pandemic on health-care workers at a tertiary care hospital in India. International Journal of Academic Medicine. 2020 Jul 1;6(3):197. [Google Scholar]
- 27.Bajaj J.S., Solanki S.L. Study of risk factors and psychological impact in physicians diagnosed with COVID-19: an online, postexposure, cross-sectional survey. Journal of Anaesthesiology Clinical Pharmacology. 2020 Jul 1;36(3):345. doi: 10.4103/joacp.JOACP_417_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gupta S., Kohli K., Padmakumari P., et al. Psychological health among armed forces doctors during COVID-19 pandemic in India. Indian Journal of Psychological Medicine. 2020 Jul;42(4):374–378. doi: 10.1177/0253717620934037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chatterjee S.S., Bhattacharyya R., Bhattacharyya S., Gupta S., Das S., Banerjee B.B. Attitude, practice, behavior, and mental health impact of COVID-19 on doctors. Indian Journal of Psychiatry. 2020 May;62(3):257. doi: 10.4103/psychiatry.IndianJPsychiatry_333_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sahu D., Agrawal T., Rathod V., Bagaria V. Impact of COVID 19 lockdown on orthopaedic surgeons in India: a survey. Journal of clinical orthopaedics and trauma. 2020 May 1;11:S283–S290. doi: 10.1016/j.jcot.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ramachandran Nair A.K., Savrimalai Karumaran C., Kattula D., Thavarajah R., Arunachalam Mohandoss A. Stress levels of Indian endodontists during COVID-19 pandemic. Rev. cuba. estomatol. 2020:e3445. [Google Scholar]
- 32.Grover R., Dua P., Juneja S., Chauhan L., Agarwal P., Khurana A. “Depression, anxiety and stress” in a cohort of registered practicing ophthalmic surgeons, post lockdown during COVID-19 pandemic in India. Ophthalmic Epidemiology. 2020 Nov 14:1–8. doi: 10.1080/09286586.2020.1846757. [DOI] [PubMed] [Google Scholar]
- 33.Nathiya D, Suman S, Singh P, Raj P, Tomar BS. WITHDRAWN: Mental Health Outcome and Professional Quality of Life Among Healthcare Worker during COVID-19 Pandemic: A (FRONTLINE-COVID) Survey. InAnnales Médico-Psychologiques, Revue Psychiatrique 2021 Jan 6. Elsevier Masson. [DOI] [PMC free article] [PubMed]
- 34.Khanna R.C., Honavar S.G., Metla A.L., Bhattacharya A., Maulik P.K. Psychological impact of COVID-19 on ophthalmologists-in-training and practising ophthalmologists in India. Indian journal of ophthalmology. 2020 Jun;68(6):994. doi: 10.4103/ijo.IJO_1458_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nanjundaswamy M.H., Pathak H., Chaturvedi S.K. Perceived stress and anxiety during COVID-19 among psychiatry trainees. Asian journal of psychiatry. 2020 Dec;54:102282. doi: 10.1016/j.ajp.2020.102282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Podder I., Agarwal K., Datta S. Comparative analysis of perceived stress in dermatologists and other physicians during national lock‐down and COVID‐19 pandemic with exploration of possible risk factors: a web‐based cross‐sectional study from Eastern India. Dermatologic Therapy. 2020 Jul;33(4) doi: 10.1111/dth.13788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mishra S., Singh S., Tiwari V., Vanza B., Khare N., Bharadwaj P. Assessment of level of perceived stress and sources of stress among dental professionals before and during the COVID-19 outbreak. Journal of International Society of Preventive & Community Dentistry. 2020 Nov;10(6):794. doi: 10.4103/jispcd.JISPCD_340_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pandey U., Corbett G., Mohan S., et al. Anxiety, depression and behavioural changes in junior doctors and medical students associated with the coronavirus pandemic: a cross-sectional survey. The Journal of Obstetrics and Gynecology of India. 2021 Feb;71(1):33–37. doi: 10.1007/s13224-020-01366-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gupta S., Prasad A.S., Dixit P.K., Padmakumari P., Gupta S., Abhisheka K. Survey of prevalence of anxiety and depressive symptoms among 1124 healthcare workers during the coronavirus disease 2019 pandemic across India. Medical Journal Armed Forces India. 2020 Sep 1 doi: 10.1016/j.mjafi.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Spoorthy M.S., Pratapa S.K., Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic-A review. Asian journal of psychiatry. 2020;51:102119. doi: 10.1016/j.ajp.2020.102119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Collins R. COVID-19: nurses have responded, now it is time to support them as we move forward. Healthcare management forum. 2020;33(5):190–194. doi: 10.1177/0840470420953297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Khanagar S.B., Al-Ehaideb A., Vishwanathaiah S., Maganur P.C., Varadarajan S., Patil S. Depression, anxiety, and psychological distress among health-care providers during the outbreak of the life-threatening coronavirus disease (COVID-19) J Contemp Dent Pract. 2020;21:471–472. [PubMed] [Google Scholar]
- 43.Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. 2020 May 8. Prevalence of Depression, Anxiety, and Insomnia Among Healthcare Workers during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Brain, Behavior, and Immunity. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.de Pablo G.S., Serrano J.V., Catalan A., et al. Impact of coronavirus syndromes on physical and mental health of health care workers: systematic review and meta-analysis. Journal of affective disorders. 2020 Jun 25 doi: 10.1016/j.jad.2020.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]