Abstract
The causal mechanisms and treatment for the negative symptoms and cognitive dysfunction in schizophrenia are the main issues attracting the attention of psychiatrists over the last decade. The first part of this review summarizes the pathogenesis of schizophrenia, especially the negative symptoms and cognitive dysfunction from the perspectives of genetics and epigenetics. The second part describes the novel medications and several advanced physical therapies (e.g., transcranial magnetic stimulation and transcranial direct current stimulation) for the negative symptoms and cognitive dysfunction that will optimize the therapeutic strategy for patients with schizophrenia in future.
Keywords: Schizophrenia, Genetics, Epigenetics, Negative symptoms, Cognitive dysfunction, Physical therapy
Introduction
Schizophrenia is a group of major mental spectrum disorders of unknown etiology, with a lifetime prevalence of approximately 1% in the world population [1]. The main clinical manifestations include positive symptoms (delusions, hallucinations, and disorganized speech), negative symptoms (diminished emotional expression or avolition), and cognitive dysfunction (deficits in attention, working memory, and executive function). In the late stages, the long-lasting negative symptoms and cognitive dysfunction deprive patients of independent lives and impose great economic burdens on families and society [2].
Negative symptoms are prevalent in patients with schizophrenia as nearly 60% of outpatients present them throughout the disease process [3–7]. Furthermore, patients with prominent negative symptoms (i.e., with greater severity than the co-occurring positive symptoms) account for 40% of schizophrenia outpatients, of whom 19% do not even present prominent positive symptoms [8]. Besides, negative symptoms tend to last for a long time and worsen with time. This is because, firstly, 73% of patients with negative symptoms present with asociality and trait anhedonia in their early childhood/adolescence, before the onset of schizophrenia [9–12]; and secondly, a greater percentage of patients exhibit more stable deficits (from 67% to 80%) as schizophrenia progresses [13]. In general, negative symptoms are linked with poor functional outcomes and a heavy economic burden of patients with schizophrenia [14].
Patients with schizophrenia who present cognitive impairments account for 98.1% [15], and on average their cognitive performance is 1–2 standard deviations below controls [16, 17]. The cognitive dysfunction occurs nearly one decade earlier than the first onset of psychosis and worsens with progression of the disease [18]. Thus, the early cognitive decline is acknowledged as a hallmark feature of schizophrenia, and schizophrenia may be a cognitive illness [19, 20]. Furthermore, cognitive dysfunction is treated as one of the strongest predictors of functional recovery from schizophrenia. Because it had direct effects on patients’ quality of life, the efficacy of psychosocial rehabilitation programs, and employment retention [21–23].
The General Mechanisms Underlying Negative Symptoms and Cognitive Dysfunction
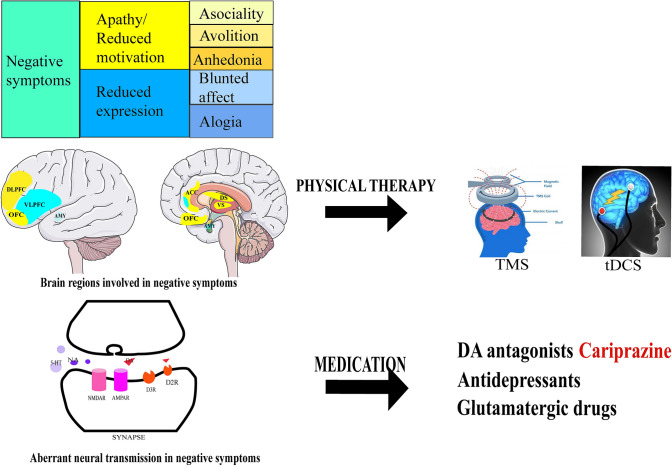
The conceptualization of negative symptoms has developed a lot to understand its mechanisms [24]. There are generally two dimensions in negative symptoms including five domains: (1) the reduced expression dimension, including blunted affect and alogia; (2) the reduced motivation dimension (also named apathy dimension), including asociality, avolition, and anhedonia [14]. However, the neurobiology of negative symptoms remains mysterious. The general mechanisms are associated with deficits in dopamine transmission in mesocortical pathways and deficits in other neurotransmitter systems such as serotonergic, noradrenergic, and glutamatergic transmission [14]. Of note, dopamine D3 receptors play a critical role in regulating negative symptoms. The D3 receptors, localized in the prefrontal cortex and the nucleus accumbens, which control reward and motivation [25], regulate glutamatergic circuits connecting the prefrontal cortex to subcortical areas [26, 27].
A meta-analysis of functional brain imaging studies reported that the ventral striatum hypoactivation during reward anticipation plays a central role in the negative symptoms of schizophrenia [28]. Different neural networks are involved in the different dimensions of negative symptoms (Fig. 1) [29]. For example, prefrontal-striatal networks (the ventral and dorsal striatum, ventromedial prefrontal cortex/orbito-frontal cortex, dorsolateral prefrontal cortex (DLPFC), and anterior cingulate cortex) play critical roles in the apathy dimension [29]. Other brain regions such as the rostral anterior cingulate cortex, amygdala, and basal ganglia are involved in the pathophysiology of the reduced expression dimension [29].
Fig. 1.
The pathophysiology and treatment of negative symptoms. The negative symptoms have two dimensions, apathy/reduced motivation and reduced expression. The apathy dimension (yellow) contains the asociality, avolition, and anhedonia domains, and the reduced expression dimension (blue) contains the blunted affect and alogia domains. The brain regions involved in the apathy dimension (yellow) include the anterior cingulate cortex (ACC), dorsal striatum (DS), dorsolateral prefrontal cortex (DLPFC), orbito-frontal cortex (OFC), and ventral striatum (VS). The brain regions involved in the reduced expression dimension (blue) include the ventrolateral prefrontal cortex (VLPFC) and amygdala (AMY). Physical therapy such as transcranial magnetic stimulation (TMS) and transcranial direct current stimulation (tDCS) may target these brain regions and improve negative symptoms. The abnormal synaptic transmission underlying the negative symptoms include dopaminergic, glutamatergic, and serotonergic transmission. The corresponding medications include dopamine antagonists, antidepressants, and glutamatergic drugs.
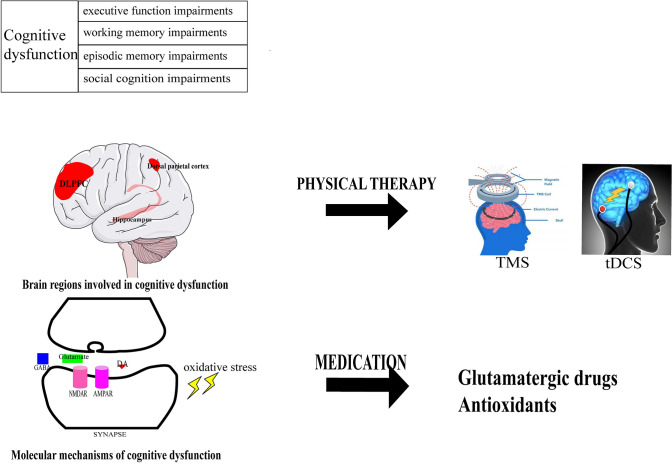
Cognition includes eight domains: (1) attention/vigilance, (2) cognitive control/executive function, (3) reasoning/problem-solving, (4) social cognition, (5) speed of processing, (6) verbal learning, (7) visual learning, and (8) working memory [30, 31]. Among these, impairments in learning and memory, working memory, attention, problem solving, processing speed, and social cognition are prominent in schizophrenia [32, 33].The brain regions involved in cognition are the hippocampus, basal ganglia, DLPFC, and dorsal parietal cortex [34] (Fig. 2). Abnormalities in the cortico-cerebellar-striatal-thalamic loop, and task-positive and task-negative cortical networks have been identified in the functional connectivity analysis of resting-state functional magnetic resonance imaging in schizophrenia [35]. Of note, the impairments in context processing, working memory, and episodic memory are associated with impaired function of the DLPFC in schizophrenia [36]. Besides, episodic memory deficits have been highlighted in the cognitive dysfunction of schizophrenia as they are controlled by the DLPFC in the frontal and medial temporal lobe network [36]. Presynaptic and postsynaptic signaling has different effects on cognition, as the synthesis of presynaptic components is associated with memory, while postsynaptic signaling is associated with working memory [37]. The dysregulation of transmitters is involved in the cognitive dysfunction of schizophrenia as well. For example, the aberrant glutamatergic pathway might affect executive functioning, especially in cognitive flexibility and learning potential, [37] and an aberrant central muscarinic system (especially M1 and M4 receptors) has been described in regions linked to cognitive function [38].
Fig. 2.
The pathophysiology and treatments of cognitive dysfunction. The cognitive dysfunction in schizophrenia is characterized by impairments of executive function, working memory, episodic memory, and social cognition. The brain regions involved in cognitive dysfunction include the hippocampus, dorsolateral prefrontal cortex (DLPFC), and dorsal parietal cortex. Physical therapy such as TMS and tDCS may target these brain regions and improve cognitive dysfunction in schizophrenia. The molecular mechanisms involved in cognitive dysfunction include abnormal glutamatergic transmission and oxidative stress. The corresponding medications include glutamatergic drugs and antioxidants.
Some associations between negative symptoms and cognitive symptoms have been found in schizophrenia. Conceptually, negative symptoms have some overlaps with cognitive dysfunction in schizophrenia [14]. For example, executive function in cognition affects goal-directed behavior, which contributes to avolition. The diminished verbal fluency and social cognition have some overlaps with alogia and asociality [24]. In addition to the overlapping concepts, cognitive impairment and negative symptoms have some mechanisms in common. For example, they may share the mechanism of aberrant interhemispheric connections (especially in the pallidum), as revealed in the fMRI of resting-state functional connectivity in first-episode schizophrenia patients [39]. Among molecular mechanisms, some glutamatergic variants influence both negative symptoms and cognitive dysfunction in the prediction analysis of groups at clinical high risk [40]. Besides, neuroinflammation and oxidative stress also play important roles in the pathogenesis of these two symptoms. Aberrant inflammatory status has been identified in patients with schizophrenia, and is associated with the severity of negative symptoms and cognitive dysfunction [41, 42]. Increased inflammatory processes such as microglial activation and elevated cytokine levels might have disruptive effects on neurogenesis and synaptic signaling [43]. In terms of oxidative stress, parvalbumin interneurons are vulnerable to oxidative stress, and the disruption of cortical and hippocampal parvalbumin interneurons may play key roles in the pathology of negative symptoms and cognitive dysfunction [44]. Plasma markers of oxidative stress (e.g., glutathione/GSH) interact with brain-derived neurotrophic factor and then impair cognition by affecting executive dysfunction in schizophrenia [45].
Genetic Mechanisms of Negative Symptoms and Cognitive Dysfunction
As the neurodevelopmental model of schizophrenia has been proposed and refined with evidence from genetics and epigenetics, the mechanisms underlying negative symptoms and cognitive dysfunction have also been revealed by novel evidence from these fields. Multiple kinds of common variation [e.g., single nucleotide polymorphisms (SNPs)] and rare variation [e.g., copy number variants (CNVs) [46], loss-of-function variants [47, 48], and ultra-rare variants [49]] have been identified in schizophrenia. In general, SNPs are the primary common genetic variants with small effects while rare variants (including CNVs) generally have large effects [49]. For SNPs, common variant associations with the onset and treatment of schizophrenia have been identified in genome-wide association studies (GWASs) [50, 51]. In terms of rare variation, several CNV loci associated with the risk of schizophrenia and the medication response have been identified in GWASs [52–54].
The etiologies of negative symptoms have been associated with differential “modifier loci” in GWASs of schizophrenia [55]. In a meta-analysis of GWASs of Irish cases [55], SNPs in several genes (related to neuron projection and postsynaptic membrane) and several pathways (related to axon guidance, Netrin-1 signaling, and long-term depression) were demonstrated in negative symptoms [55]. Five SNPs (three SNPs in the BCL9 gene and two in C9orf5) have robust associations with negative symptoms [56]. Besides, variation in other genes such as DRD2, which encodes the dopamine receptor DR2 [57], a FOXO6 risk allele [58], and the catechol-O-methyltransferase (COMT) gene [59] are associated with the severity of negative symptom in patients with schizophrenia.
In the genetic mechanisms of cognitive dysfunction, several common and rare variations play important parts as well. SNPs of the psychosis susceptibility gene ZNF804A pathway are associated with IQ, memory, and social cognition in schizophrenia [60, 61]. Some CNVs such as the chromosome 15q11.2 deletion between breakpoints 1 and 2 diminish several cognitive traits and subsequently cause dyslexia and dyscalculia [62]. In addition to reports of several SNPs and CNVs in cognitive dysfunction, researchers have found that cognition and schizophrenia share some genetic bases [63], and several genetic loci jointly affect the risk of schizophrenia and cognitive traits (verbal-numerical reasoning, reaction time, and general cognitive function) [64]. Besides, there are negative correlations between genomic risk/polygenetic risk scores [65] for schizophrenia and cognitive traits such as general cognitive function [66] and IQ [67]. But this correlation is complicated and controversial as another two studies denied any association between polygenetic risk scores for schizophrenia and cognitive phenotypes [68, 69].
Epigenetic Mechanisms of Negative Symptoms and Cognitive Dysfunction
Epigenetics refers to heritable phenotype changes without alterations in the DNA sequence. Much genetic risk cannot be explained at the DNA level and may be associated with epigenetic mechanisms in schizophrenia as well as its negative symptoms and cognitive dysfunction [1, 70].
First, schizophrenia is associated with DNA methylation changes at sites such as CpGs. Different brain regions may have different DNA methylation signatures in schizophrenia [71, 72], and a 4-fold enrichment is exhibited in schizophrenia risk loci among DNA methylation quantitative trait loci in the developing brain [73, 74]. In the negative symptoms, changes in DNA methylation in the oxytocin receptor gene are associated with the functional connectivity of the striatal-amygdala network underlying anhedonia-asociality in resting-state functional magnetic resonance imaging [75]. Patients with primary and enduring negative symptoms have lower DNA methylation in exons 4 and 5 of the matrix metalloproteinase 9 gene than other patients [76]. In cognitive dysfunction, CpG site methylation plays a key role in central nervous system differentiation as well as synaptic plasticity, learning, and memory [77]. Besides, hypomethylation of the GRIN2B promoter associated with cognitive dysfunction has been identified in early-onset schizophrenia versus controls [78]. In the DLPFC region associated with cognition, two expression and two methylation modules have been identified in schizophrenia [79]. Second, the spatial organization of genome architecture is critical in neurodevelopment as well as cognition in schizophrenia [80–82]. Schahram et al. found that the spatial organization of the genome architecture affects genes associated with the susceptibility to schizophrenia during the differentiation of neural progenitor cells, and these genes might affect risk variants at the transcriptome and proteome levels [83]. Third, some non-coding RNAs (e.g., long non-coding RNAs) are associated with the negative symptoms and cognitive performance [84] in schizophrenia [85].
The interactions among environmental risk factors, genetic mechanisms, and epigenetic mechanisms are: common genetic variations increase individuals’ susceptibility to environmental risk factors [86]; and environmental risk factors in early development alter the epigenetic regulation in schizophrenia [87–90]. The epigenetic mechanisms of negative symptoms and cognitive dysfunction are affected by environmental risk factors in schizophrenia. Patients with the COMT Val(158) Met polymorphism might have more severe negative symptoms if they suffer from emotional neglect [91]. Early-life diet can regulate learning and memory processes associated with schizophrenia via epigenetic mechanisms [92].
Treatment of Negative Symptoms and Cognitive Dysfunction
Nowadays, antipsychotics are still the main treatment for schizophrenia [93]. The application of first-generation antipsychotics (FGAs/typical antipsychotics) is limited by their adverse effects on the motor system (e.g., adverse extrapyramidal effects) and the cardiovascular system. With the advent of second-generation antipsychotics (SGAs/atypical antipsychotics), the incidence of the side-effects noted above is lower but the incidence of severe metabolic disorders is higher [94]. Antipsychotics have a robust effectiveness in the treatment of acute schizophrenia, as 2/3 patients show significant improvement in positive symptoms [95, 96]. In the treatment of stable schizophrenia, continuous administration of antipsychotics is vital for recovery and the prevention of relapse [97–99]. However, the efficacy of SGAs is no better than FGAs for the negative symptoms and cognitive dysfunction in stable schizophrenia [100]. A meta-analysis of 168 randomized placebo-controlled trials denied clinically significant improvements of negative symptoms with current medications [100]. With regard to cognitive dysfunction, longitudinal evidence indicated that the mild improvements in general cognition disappear after the first two months of treatment and few effective drugs have been reported to have long-term cognitive improvements [101].
Pharmacological Treatments for Negative Symptoms
The heterogeneity of negative symptoms in pathophysiology is universally acknowledged. Negative symptoms are classified as primary or secondary [102]. Primary negative symptoms are intrinsic to the disease, while secondary negative symptoms result from known factors including positive symptoms, affective symptoms, antipsychotic-associated extrapyramidal symptoms (EPSs) and sedation, social deprivation, and substance abuse [102]. Schizophrenia with primary negative symptoms accounts for 15%–25% in patients with schizophrenia [103]. Primary and enduring negative symptoms have been defined as deficit symptoms in schizophrenia [103]. However, psychiatrists find it rather difficult to differentiate primary from secondary negative symptoms in clinical practice [104]. The term “predominant negative symptoms” is frequently used instead, as it is easy to classify according to the scale scores [105]. To our knowledge, effective pharmacological treatments for primary negative symptoms are still rare, while secondary negative symptoms seem to have more available treatments such as clozapine [106]. However, proposals for clinical management of the negative symptoms have been improved with the development of new dopamine antagonists such as cariprazine [107]. Cariprazine is proposed as a first-line treatment for patients with predominant negative symptoms, and low-dose amisulpride is an alternative when cariprazine is ineffective [107]. In general, pharmacological treatments for negative symptoms include dopamine antagonists (cariprazine and low-dose amisulpride) as monotherapy, with serotoninergic or noradrenergic and glutamatergic drugs as adjunctive therapy (Table 1).
Table 1.
Medications for negative symptoms in schizophrenia.
| Molecular target | Example compound | Clinical evidence |
|---|---|---|
| Dopamine antagonists | Amisulpride (low dose), monotherapy | Improvements in negative symptoms with improvements in depressive symptoms |
| Cariprazine, monotherapy | Improvements in predominant negative symptoms | |
| lisdexamfetamine dimesylate, add-on therapy | Improvements in predominant negative symptoms | |
| Serotoninergic and noradrenergic drugs | SSRIs , TCAs, etc. add-on therapy | Improvements of negative symptoms with improvements in depressive symptoms |
| Glutamate agonists | Glycine, glycine transporter-1 inhibitors, D-serine , D-amino acid oxidase (DAAO) inhibitors, D-cycloserine (DCS) add-on therapy | Small to moderate effects |
| Sigma-2 antagonist and 5-HT2A antagonist | Roluperidone (MIN-101) monotherapy | Positive results |
| Other targets | Minocycline, add-on therapy | Positive results |
Dopamine Antagonists as Monotherapy
As noted above, deficits in dopamine transmission in mesocortical pathways are the universally accepted mechanisms for the negative symptoms. New dopamine antagonists with preferential selectivity for D3 receptors (such as low-dose amisulpride and cariprazine) have potential to relieve predominantly negative symptoms in schizophrenia.
Low-Dose Amisulpride (50–300 mg/day)
Amisulpride is a second-generation antipsychotic of the benzamide class with high affinity for dopamine D2 and D3 receptors. Amisulpride was revealed as the only antipsychotic effective in the treatment of predominant negative symptoms [108]. In the last century, low-dose amisulpride (50–300 mg/day) was highlighted for significantly reducing the scores on the Scale for the Assessment of Negative Symptoms (SANS) in the placebo-controlled studies [109–112]. Low-dose amisulpride remarkably improves predominant negative symptoms, especially avolition, attentional impairment, and retardation [112], and it is suspected to relieve non-persistent negative symptoms in medium-term treatment [109, 113]. Recently, a Chinese study reported that amisulpride (average 623.9 mg/day) reduces Positive and Negative Syndrome Scale (PANSS) negative symptom scores from baseline to week 8 with a 45.2% average reduction in Chinese patients with predominantly negative symptoms [114]. All of these studies excluded the effects of amisulpride on negative symptoms secondary to the positive symptoms and EPS by comparing the simultaneous changes in these two symptoms [113]. However, the improvement in negative symptoms is accompanied by improvements in depressive symptoms [113]. Thus, its effects on negative symptoms secondary to depression were not excluded and thus confused its effects on primary negative symptoms. Besides, its marked efficacy has only been revealed in studies by comparison with placebo [109–111], and merely a trend in favor of amisulpride has been reported when compared with other antipsychotics [115].
Cariprazine
Cariprazine is a dopamine D3 and D2 receptor partial agonist that preferentially binds to D3 receptors and a partial agonist of the serotonin 5-HT1A receptor. In 2014, the efficacy of cariprazine in the acute exacerbation of schizophrenia was explored for the first time. A meta-analysis in 2018 summarized 4 randomized controlled trials on the efficacy and safety of cariprazine in the acute exacerbation of schizophrenia [116–119]. Cariprazine seems to have equal effects on positive and negative symptoms compared with placebo (PANSS total scores, standardized mean difference (SMD) = −0.37; PANSS positive, SMD = −0.32; PANSS negative, SMD = −0.32) [120]. Cariprazine has broad-spectrum effects in acute schizophrenia, improving all 5 PANSS factor domains [121]. Although cariprazine has a higher incidence of treatment-emergent events and akathisia versus placebo [120], long-term administration (up to 9 mg/day) has been reported to be reported generally safe and well-tolerated by patients [122]. Only small changes in metabolic parameters and a decrease in prolactin level have been reported in cariprazine treatment compared with placebo [118, 123].
Despite its application in acute schizophrenia, cariprazine has been characterized as effective for predominant negative symptoms under the condition that the secondary negative symptoms are well-controlled [124, 125]. A rigorously-designed study published in Lancet compared the efficacy of cariprazine with risperidone monotherapy and found that cariprazine has advantages over risperidone in improving predominant negative symptoms as well as community functioning [125]. Cariprazine was reported to take effect at week 14 and continued to improve symptoms at the week 26 endpoint [125]. The secondary negative symptoms were well-controlled in this study, as no significant changes in positive symptoms, EPS, or depressive symptoms were detectable in the cariprazine and risperidone groups [125, 126]. However, this study had some limitations, such as the lack of a placebo control group. Another group conducted post hoc analyses of individual PANSS items and PANSS-derived factors. They found that cariprazine is superior to risperidone in most PANSS Negative Subscale items and across all PANSS-derived factors, which means that cariprazine has broad-spectrum efficacy for predominant negative symptoms [126].
Other Dopaminergic Drugs
Other preferential D3 receptor antagonists such as F17464 and ABT-925 have reached clinical study phase. Only F17464 exhibits a good efficacy in acute schizophrenia [27, 127], but without special effects on negative symptoms.
Asenapine, an agent binding to dopamine, serotonin, noradrenaline, and histamine receptors, is more effective than risperidone and haloperidol on negative symptoms [128, 129]. But it fails to outperform olanzapine in patients with persistent negative symptoms [130, 131].
Dopamine agonists (such as methylphenidate, amphetamine, and lisdexamfetamine) may improve the negative symptoms in patients with schizophrenia. A meta-analysis in 2019 on pro-dopaminergic drugs including armodafinil, L-dopa, and pramipexole found that they do not significantly improve negative symptoms [132]. However, adjunctive lisdexamfetamine dimesylate therapy improved predominant negative symptoms in outpatients with schizophrenia without positive symptom worsening [133]. Besides, the D1 dopamine agonist dihydrexidine (DAR-0100) failed to elicit significant improvements in cognitive dysfunction [134].
Serotoninergic and Noradrenergic Drugs (Antidepressants) as Adjunctive Therapy
Since abnormal serotoninergic or noradrenergic transmission plays an important role in negative symptoms, adjunctive antidepressants can improve these symptoms and general functioning in patients with schizophrenia. A meta-analysis in 2010 that included SSRIs, mirtazapine, reboxetine, mianserin, trazodone, and ritanserin confirmed the moderate effects of antidepressants in improving negative symptoms in chronic schizophrenia (SMD = –0.48) [135]. Another meta-analysis in 2016 found that antidepressants have small positive effects on both depressive symptoms (SMD = –0.25) and negative symptoms (SMD = –0.30) [136]. In the analysis of subgroups, the authors found that antidepressants have larger effects on predominant negative symptoms (SMD = –0.58) [136]. Antidepressants (MAOs, NDRIs, NRIs, SNRIs, SSRIs, TCAs and TeCAs, and SSRIs and TCAs) have been reported to be more efficacious on negative symptoms compared with placebo [136]. Among individual drugs, selegiline, duloxetine, citalopram, fluvoxamine, and mirtazapine have been reported to benefit the negative symptoms in schizophrenia [136]. In addition, a meta-analysis on adjunctive antidepressants in stable antipsychotic treatment reported that these drugs have small-to-medium effects on negative symptoms [137]. Of note, their beneficial effects on negative symptoms seem to be limited to the augmentation of first-generation antipsychotics [137]. The immune mechanisms underlying SSRI augmentation have been revealed with a decrease in C-reactive protein and interleukin-6 levels [138]. However, the effects of adjunctive antidepressants in schizophrenia cannot rule out the improvement of negative symptoms secondary to depression. When patients with depression are excluded, antidepressants such as fluoxetine fail to present positive results in primary and enduring negative symptoms [139].
Roluperidone (MIN-101), an antagonist of both sigma-2 and 5-HT2A receptors, is a serotoninergic drug rarely used as monotherapy for schizophrenia [140]. The efficacy of both doses (32 and 64 mg) of roluperidone monotherapy on negative symptoms was confirmed in patients with stable positive symptoms [141]. The post hoc analysis for this trial showed that roluperidone works on the two domains, reduced experience and reduced expression, among the negative symptoms [142]. Roluperidone may also improve personal and social adjustments in patients with stable positive symptoms and concurrent clinically significant negative symptoms [143]. In these studies, the effects of positive symptoms were controlled as no significant differences were found between roluperidone and placebo [141]. However, other compounding factors in secondary negative symptoms have not yet been taken into consideration. Besides, roluperidone monotherapy improves cognitive dysfunction in stable schizophrenia as well [144].
Glutamatergic Drugs as Adjunctive Therapy
Abnormal glutamate signaling in the pathology of schizophrenia includes hypofunction of NMDA receptors in GABAergic interneurons and hyperglutamatergic signaling in excitatory pyramidal neurons in cortex [145, 146]. Thus, the therapeutic strategy is to augment NMDA receptor function; this includes agents targeting NMDA receptors and AMPA receptors, positive allosteric modulators of metabotropic glutamate receptors, and antioxidants [147]. Agents targeting GluN1 (a subunit of NMDA receptors) include glycine and glycine transporter-1 inhibitors, D-serine and D-amino-acid oxidase inhibitors, D-cycloserine (DCS), and KAT inhibitors [148, 149]. Adjunctive glutamatergic drugs have small to moderate effects on the negative symptoms in patients with schizophrenia. A meta-analysis including DCS and D-serine in 2013 reported a moderate effect-size improvement (SMD = 0.62). Besides, a meta-analysis that included D-serine, sarcosine, NAC, DCS, and glycine in 2011 and another that included glycine, D-serine, DCS, and sarcosine in 2010 both reported a small effect-size (2013: SMD = –0.27; 2010: SMD = 0.38) [150–152]. However, the effects of glutamatergic drugs on negative symptoms were not classified into primary or secondary negative symptoms. Although their spontaneous effects on positive symptoms are relatively small compared with negative symptoms, studies on their effects on predominant negative symptoms with well-controlled secondary negative symptoms are clearly warranted [150–152]. In terms of cognitive dysfunction, some cognitive domains such as working memory can be improved by glutamatergic drugs [153], and some glycine transporter-1 inhibitors, BI-425809, and cannabidiol are still being further explored for cognitive improvements [154].
Other Drugs and Dietary Supplements
Minocycline, a second-generation tetracycline, can serve as adjunctive therapy for the negative symptoms via reducing pro-inflammatory cytokines [155]. The early research on minocycline focused on its effects in the early phase of schizophrenia and reported some positive results [156–158]. However, a recent study denied its effects in first-episode psychosis as no progressive inflammatory process underpins the negative symptoms [159]. The administration of minocycline with risperidone demonstrated its efficacy on the negative symptoms in stable schizophrenia, which are positively co-related with the dose of minocycline [155, 160].
Sulforaphane, a natural compound extracted from the seeds and sprouts of cruciferous plants, can protect brain cells from inflammation and oxidative stress [161]. The protective mechanisms of sulforaphane are related to kelch-like ECH-associated protein 1 and the transcription factor NF-E2-related factor 2 [162, 163]. Two studies have been published on the efficacy of sulforaphane associated with schizophrenia [164, 165]. One reported that sulforaphane-rich broccoli sprout extract (30 mg/day) improves cognitive dysfunction in patients with schizophrenia [164], and the other focused on the increased brain GSH level after the administration of sulforaphane for 7 days [165].
Since reduced blood omega-3 fatty-acids are associated with cognitive dysfunction, their administration may improve this symptom cluster [166]. Besides, omega-3 fatty-acids might have better efficacy when administered at the early stages of schizophrenia [167]. Of note, they also have beneficial effects on metabolic syndrome, such as reducing the triglyceride levels in patients with schizophrenia [168]. However, more clinical studies and meta-analyses are needed, as some trials reported that they are not efficacious on cognitive dysfunction [169]. The pharmacological entities for cognitive dysfunction described above are listed in Table 2.
Table 2.
Medications for cognitive dysfunction in schizophrenia.
| Molecular target | Example compound | Clinical evidence |
|---|---|---|
| D1 Dopamine agonists | Dihydrexidine (DAR-0100), monotherapy | Negative proof-of-concept trial |
| Glutamate agonists | Glycine, glycine transporter-1 inhibitors, D-serine , D-amino acid oxidase (DAAO) inhibitors, D-cycloserine (DCS) add-on therapy | Improvement in working memory domain; mixed results. |
| Sigma-2 antagonist and 5-HT2A antagonist | Roluperidone (MIN-101), monotherapy | Positive results |
| Antioxidants | Sulforaphane, omega-3 fatty acids add-on therapy | Mixed results |
Physical Therapy for Negative Symptoms and Cognitive Dysfunction
Since cortical excitation/inhibition imbalance plays a vital role in negative symptoms and cognitive dysfunction, physical therapy may directly reverse the aberrant neural activity and cortical excitability in schizophrenia. Physical therapy for schizophrenia (especially treatment-resistant schizophrenia) includes transcranial magnetic stimulation (TMS), transcranial direct-current stimulation (tDCS), and modified electroconvulsive therapy (mECT) [170]. Compared with TMS and tDCS, mECT serves as an add-on therapy, mainly for refractory schizophrenia with little marked advance in the last decade [171, 172]. Thus, we discuss TMS and DCS below, and these two invasive forms of stimulation in the frontal cortex exhibit great potential, especially for negative symptoms [173].
Transcranial Magnetic Stimulation
TMS can probe the functioning of the neural networks and neurotransmitter systems associated with the negative symptoms and cognitive dysfunction in schizophrenia [174]. Deep repetitive TMS applied to the prefrontal cortex (PFC) is a common, long-accepted therapy for treatment-resistant depression [175]. Currently, this strategy is recognized as an adjunctive therapy for the negative symptoms and cognitive dysfunction in schizophrenia, especially for negative symptoms [174, 176, 177]. The first study of TMS in schizophrenia found that 20 daily H1-coil deep TMS treatments (20 Hz, 120% motor threshold) significantly reduce the negative symptoms versus baseline via assessing with the SANS [178]. However, the active and sham stimulation groups did not differ at the endpoint [178]. High-frequency (18 Hz) bilateral deep stimulation applied over the lateral PFC using the Brainsway H-2 coil has been reported to have good efficacy for negative symptoms [179]. This study excluded the effects of depression as no differences were detected in patients with or without depression [179]. Cerebellar vermal magnetic stimulation significantly improves the negative symptoms and depressive symptoms compared with sham stimulation [180]. In some studies, TMS was applied to the DLPFC to demonstrate its effects on negative symptoms. Bilateral 10-Hz stimulation of the DLPFC for 3 weeks reduced scores measured in the SANS [181]. However, repetitive TMS to the left DLPFC affects the positive and total psychotic symptoms rather than negative symptoms in patients with predominant negative symptoms [182].
In the treatment of cognitive dysfunction, improvements in working memory have been reported with high-frequency repetitive TMS over the left PFC [183]. In addition, 10-Hz rTMS stimulation of the PFC significantly improves facial affect recognition, which plays a critical role in social cognition [184]. However, some studies reported negative results. For example, 10-Hz repetitive TMS applied to the left DLPFC for 3 weeks did not improve any of the cognitive domains in schizophrenia patients with predominant negative symptoms [185]. Although some remarkable findings have been reported with TMS, a review reported insufficient evidence to support or refute the use of TMS in schizophrenia [176, 186], as its overall beneficial effects on negative and cognitive symptoms may be inconsistent and small in schizophrenia [174, 187, 188].
Transcranial Direct Current Stimulation
tDCS is a potential treatment for negative symptoms [189–192] and cognitive dysfunction [193, 194] in schizophrenia. Its primary effects on neurons are to shift the resting membrane potential towards depolarization or hyperpolarization [195]. In contrast to TMS, tDCS works on active neurons and cannot activate neurons in the resting state [195].
Leandro et al. found that patients receiving active tDCS show a marked reduction of negative symptoms versus controls, and the active group had higher response rates (40%) for negative symptoms versus the sham group (4%) (P < 0.001) [192]. Moreover, tDCS can help outpatients to improve adherence [196, 197]. The application of tDCS to the prefrontal cortex during task training may have surprisingly beneficial effects on behavioral performance [198].
In terms of cognitive dysfunction, tDCS targeting the DLPFC can improve several domains of cognition. Anodal stimulation improves attention and working memory, while cathodal stimulation improves cognitive ability and memory [194]. Of note, the working memory and overall cognition scores of patients improve over time after stimulation [193]. Besides, the mechanisms of its pro-cognitive effects have been explored via functional MRI [199].
In treatment-resistant schizophrenia, tDCS-clozapine combination might be an effective intervention in clozapine-refractory patients [195]. Fronto-temporal transcranial tDCS improved the awareness of illness and positive symptoms but not auditory verbal hallucinations [200]. Furthermore, add-on tDCS demonstrated efficacy on auditory hallucinations in hospitalized patients with ultra-treatment-resistant schizophrenia [190]. In all, the overall effects on both symptoms failed to elicit positive results, but the high stimulation frequency, twice daily subgroup showed improved negative symptoms (SMD = –0.31) in the latest meta-analysis of tDCS [201].
Psychosocial Treatments
Psychosocial treatments for schizophrenia include individual psychological, psychoeducational, and family interventions [14, 29]. Among them, social skill training (SST) plays a critical role in improving the negative symptoms. SST has been demonstrated to have significant efficacy for negative symptoms compared with active controls, treatment-as-usual, and waiting list controls in two meta-analyses [202, 203]. Of note, the efficacy of SST on negative symptoms is comparable with other interventions, including medications [203]. However, more rigorously-designed studies on SST are needed to promote its application in psychological intervention [204]. In addition to SST, cognitive remediation had small to moderate beneficial effects on negative symptoms, but robust effects on cognitive dysfunction in a network meta-analysis [205, 206]. Meditation-based mind-body therapies had small to moderate efficacy on negative symptoms compared to treatment-as-usual or non-specific control interventions [207].
Conclusions
Schizophrenia is a polygenic disease of unknown etiology. With advances in sequencing and detection technology, genetic and epigenetic analyses can promote our comprehension of the pathogenesis of schizophrenia as well as the mechanisms underlying the negative symptoms and cognitive dysfunction in schizophrenia. Currently, the treatments of negative symptoms and cognitive dysfunction play key roles in the full recovery of patients with schizophrenia. The prospects for predominant negative symptoms are good, with the advent of new D3-selective dopamine antagonists such as cariprazine. Besides, some physical therapies have the potential to improve negative symptoms and cognitive dysfunction as well. Compared with other reviews on the negative symptoms [29, 104] or cognitive dysfunction in schizophrenia [154], in this review we report new advances in physical therapy as well as genetic and epigenetic mechanisms underlying these two symptoms.
However, further exploration is still required for curing the negative symptoms and cognitive dysfunction in schizophrenia. The potential reasons for the unsatisfactory therapeutic effects of novel medications on these two symptoms might be due to their multiple domains, and the complicated mechanisms underlying each domain. Exploration of these mechanisms and treatments according to domain criteria (Research Domain Criteria, above) is anticipated. Besides, clinical studies should distinguish the heterogeneity of negative symptoms when assessing the real efficacy of novel drugs.
Acknowledgements
This review was supported by the National Key R&D Program of China (2016YFC1306900), the National Natural Science Foundation of China (81622018) and an Innovation Driven Project of Central South University (2020CX018).
Conflict of interest
The authors claim that there are no conflicts of interest.
Footnotes
Qiongqiong Wu and Xiaoyi Wang have contributed equally to this work.
Contributor Information
Jing-Ping Zhao, Email: zhaojingping@csu.edu.cn.
Ren-Rong Wu, Email: wurenrong@csu.edu.cn.
References
- 1.Owen MJ, Sawa A, Mortensen PB. Schizophrenia. Lancet. 2016;388:86–97. doi: 10.1016/S0140-6736(15)01121-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rund BR, Barder HE, Evensen J, Haahr U, ten Velden Hegelstad W, Joa I, et al. Neurocognition and duration of psychosis: A 10-year follow-up of first-episode patients. Schizophr Bull. 2016;42:87–95. doi: 10.1093/schbul/sbv083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sicras-Mainar A, Maurino J, Ruiz-Beato E, Navarro-Artieda R. Impact of negative symptoms on healthcare resource utilization and associated costs in adult outpatients with schizophrenia: A population-based study. BMC Psychiatry. 2014;14:225. doi: 10.1186/s12888-014-0225-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bobes J, Arango C, Garcia-Garcia M, Rejas J, CLAMORS Study Collaborative Group. Prevalence of negative symptoms in outpatients with schizophrenia spectrum disorders treated with antipsychotics in routine clinical practice: Findings from the CLAMORS study. J Clin Psychiatry 2010, 71: 280–286. [DOI] [PubMed]
- 5.Mäkinen J, Miettunen J, Isohanni M, Koponen H. Negative symptoms in schizophrenia: A review. Nord J Psychiatry. 2008;62:334–341. doi: 10.1080/08039480801959307. [DOI] [PubMed] [Google Scholar]
- 6.Evensen J, Røssberg JI, Barder H, Haahr U, Hegelstad WT, Joa I, et al. Flat affect and social functioning: A 10 year follow-up study of first episode psychosis patients. Schizophr Res. 2012;139:99–104. doi: 10.1016/j.schres.2012.04.019. [DOI] [PubMed] [Google Scholar]
- 7.Austin SF, Mors O, Budtz-Jørgensen E, Secher RG, Hjorthøj CR, Bertelsen M, et al. Long-term trajectories of positive and negative symptoms in first episode psychosis: A 10year follow-up study in the OPUS cohort. Schizophr Res. 2015;168:84–91. doi: 10.1016/j.schres.2015.07.021. [DOI] [PubMed] [Google Scholar]
- 8.Rabinowitz J, Berardo CG, Bugarski-Kirola D, Marder S. Association of prominent positive and prominent negative symptoms and functional health, well-being, healthcare-related quality of life and family burden: A CATIE analysis. Schizophr Res. 2013;150:339–342. doi: 10.1016/j.schres.2013.07.014. [DOI] [PubMed] [Google Scholar]
- 9.Tarbox SI, Pogue-Geile MF. Development of social functioning in preschizophrenia children and adolescents: A systematic review. Psychol Bull. 2008;134:561–583. doi: 10.1037/0033-2909.34.4.561. [DOI] [PubMed] [Google Scholar]
- 10.Kwapil TR. Social anhedonia as a predictor of the development of schizophrenia-spectrum disorders. J Abnorm Psychol. 1998;107:558–565. doi: 10.1037/0021-843X.107.4.558. [DOI] [PubMed] [Google Scholar]
- 11.Matheson SL, Vijayan H, Dickson H, Shepherd AM, Carr VJ, Laurens KR. Systematic meta-analysis of childhood social withdrawal in schizophrenia, and comparison with data from at-risk children aged 9–14 years. J Psychiatr Res. 2013;47:1061–1068. doi: 10.1016/j.jpsychires.2013.03.013. [DOI] [PubMed] [Google Scholar]
- 12.Piskulic D, Addington J, Cadenhead KS, Cannon TD, Cornblatt BA, Heinssen R, et al. Negative symptoms in individuals at clinical high risk of psychosis. Psychiatry Res. 2012;196:220–224. doi: 10.1016/j.psychres.2012.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Savill M, Banks C, Khanom H, Priebe S. Do negative symptoms of schizophrenia change over time? A meta-analysis of longitudinal data. Psychol Med. 2015;45:1613–1627. doi: 10.1017/S0033291714002712. [DOI] [PubMed] [Google Scholar]
- 14.Galderisi S, Mucci A, Buchanan RW, Arango C. Negative symptoms of schizophrenia: New developments and unanswered research questions. Lancet Psychiatry. 2018;5:664–677. doi: 10.1016/S2215-0366(18)30050-6. [DOI] [PubMed] [Google Scholar]
- 15.Keefe RS, Eesley CE, Poe MP. Defining a cognitive function decrement in schizophrenia. Biol Psychiatry. 2005;57:688–691. doi: 10.1016/j.biopsych.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 16.Bora E, Yücel M, Pantelis C. Cognitive impairment in schizophrenia and affective psychoses: Implications for DSM-V criteria and beyond. Schizophr Bull. 2010;36:36–42. doi: 10.1093/schbul/sbp094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Keefe RS, Fenton WS. How should DSM-V criteria for schizophrenia include cognitive impairment? Schizophr Bull. 2007;33:912–920. doi: 10.1093/schbul/sbm046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kahn RS, Sommer IE. The neurobiology and treatment of first-episode schizophrenia. Mol Psychiatry. 2015;20:84–97. doi: 10.1038/mp.2014.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kahn RS, Keefe RS. Schizophrenia is a cognitive illness: Time for a change in focus. JAMA Psychiatry. 2013;70:1107–1112. doi: 10.1001/jamapsychiatry.2013.155. [DOI] [PubMed] [Google Scholar]
- 20.van Oel CJ, Sitskoorn MM, Cremer MP, Kahn RS. School performance as a premorbid marker for schizophrenia: A twin study. Schizophr Bull. 2002;28:401–414. doi: 10.1093/oxfordjournals.schbul.a006949. [DOI] [PubMed] [Google Scholar]
- 21.Bowie CR, Reichenberg A, Patterson TL, Heaton RK, Harvey PD. Determinants of real-world functional performance in schizophrenia subjects: Correlations with cognition, functional capacity, and symptoms. Am J Psychiatry. 2006;163:418–425. doi: 10.1176/appi.ajp.163.3.418. [DOI] [PubMed] [Google Scholar]
- 22.Green MF, Kern RS, Braff DL, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: Are we measuring the “right stuff” ? Schizophr Bull. 2000;26:119–136. doi: 10.1093/oxfordjournals.schbul.a033430. [DOI] [PubMed] [Google Scholar]
- 23.Kurtz MM, Wexler BE, Fujimoto M, Shagan DS, Seltzer JC. Symptoms versus neurocognition as predictors of change in life skills in schizophrenia after outpatient rehabilitation. Schizophr Res. 2008;102:303–311. doi: 10.1016/j.schres.2008.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marder SR, Galderisi S. The current conceptualization of negative symptoms in schizophrenia. World Psychiatry. 2017;16:14–24. doi: 10.1002/wps.20385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lacroix LP, Hows ME, Shah AJ, Hagan JJ, Heidbreder CA. Selective antagonism at dopamine D3 receptors enhances monoaminergic and cholinergic neurotransmission in the rat anterior cingulate cortex. Neuropsychopharmacology. 2003;28:839–849. doi: 10.1038/sj.npp.1300114. [DOI] [PubMed] [Google Scholar]
- 26.Sokoloff P, Le Foll B. The dopamine D3 receptor, a quarter century later. Eur J Neurosci. 2017;45:2–19. doi: 10.1111/ejn.13390. [DOI] [PubMed] [Google Scholar]
- 27.Cosi C, Martel JC, Auclair AL, Collo G, Cavalleri L, Heusler P, et al. Pharmacology profile of F17464, a dopamine D3 receptor preferential antagonist. Eur J Pharmacol 2021, 890: 173635. [DOI] [PubMed]
- 28.Radua J, Schmidt A, Borgwardt S, Heinz A, Schlagenhauf F, McGuire P, et al. Ventral striatal activation during reward processing in psychosis: A neurofunctional meta-analysis. JAMA Psychiatry. 2015;72:1243–1251. doi: 10.1001/jamapsychiatry.2015.2196. [DOI] [PubMed] [Google Scholar]
- 29.Bègue I, Kaiser S, Kirschner M. Pathophysiology of negative symptom dimensions of schizophrenia - Current developments and implications for treatment. Neurosci Biobehav Rev. 2020;116:74–88. doi: 10.1016/j.neubiorev.2020.06.004. [DOI] [PubMed] [Google Scholar]
- 30.Barch DM, Ceaser A. Cognition in schizophrenia: Core psychological and neural mechanisms. Trends Cogn Sci. 2012;16:27–34. doi: 10.1016/j.tics.2011.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kimoto S, Makinodan M, Kishimoto T. Neurobiology and treatment of social cognition in schizophrenia: Bridging the bed-bench gap. Neurobiol Dis 2019, 131: 104315. [DOI] [PubMed]
- 32.Lencz T, Smith CW, McLaughlin D, Auther A, Nakayama E, Hovey L, et al. Generalized and specific neurocognitive deficits in prodromal schizophrenia. Biol Psychiatry. 2006;59:863–871. doi: 10.1016/j.biopsych.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 33.Wood SJ, Pantelis C, Velakoulis D, Yücel M, Fornito A, McGorry PD. Progressive changes in the development toward schizophrenia: Studies in subjects at increased symptomatic risk. Schizophr Bull (Bp) 2008;34:322–329. doi: 10.1093/schbul/sbm149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Robison AJ, Thakkar KN, Diwadkar VA. Cognition and reward circuits in schizophrenia: Synergistic, not separate. Biol Psychiatry. 2020;87:204–214. doi: 10.1016/j.biopsych.2019.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sheffield JM, Barch DM. Cognition and resting-state functional connectivity in schizophrenia. Neurosci Biobehav Rev. 2016;61:108–120. doi: 10.1016/j.neubiorev.2015.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guo JY, Ragland JD, Carter CS. Memory and cognition in schizophrenia. Mol Psychiatry. 2019;24:633–642. doi: 10.1038/s41380-018-0231-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Thomas EHX, Bozaoglu K, Rossell SL, Gurvich C. The influence of the glutamatergic system on cognition in schizophrenia: A systematic review. Neurosci Biobehav Rev. 2017;77:369–387. doi: 10.1016/j.neubiorev.2017.04.005. [DOI] [PubMed] [Google Scholar]
- 38.Carruthers SP, Gurvich CT, Rossell SL. The muscarinic system, cognition and schizophrenia. Neurosci Biobehav Rev. 2015;55:393–402. doi: 10.1016/j.neubiorev.2015.05.011. [DOI] [PubMed] [Google Scholar]
- 39.Mwansisya TE, Wang Z, Tao HJ, Zhang HR, Hu AM, Guo SX, et al. The diminished interhemispheric connectivity correlates with negative symptoms and cognitive impairment in first-episode schizophrenia. Schizophr Res. 2013;150:144–150. doi: 10.1016/j.schres.2013.07.018. [DOI] [PubMed] [Google Scholar]
- 40.Jagannath V, Theodoridou A, Gerstenberg M, Franscini M, Heekeren K, Correll CU, et al. Prediction analysis for transition to schizophrenia in individuals at clinical high risk for psychosis: The relationship of DAO, DAOA, and NRG1 variants with negative symptoms and cognitive deficits. Front Psychiatry. 2017;8:292. doi: 10.3389/fpsyt.2017.00292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.García-Bueno B, Bioque M, Mac-Dowell KS, Barcones MF, Martínez-Cengotitabengoa M, Pina-Camacho L, et al. Pro-/anti-inflammatory dysregulation in patients with first episode of psychosis: Toward an integrative inflammatory hypothesis of schizophrenia. Schizophr Bull. 2014;40:376–387. doi: 10.1093/schbul/sbt001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Goldsmith DR, Rapaport MH, Miller BJ. A meta-analysis of blood cytokine network alterations in psychiatric patients: Comparisons between schizophrenia, bipolar disorder and depression. Mol Psychiatry. 2016;21:1696–1709. doi: 10.1038/mp.2016.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fourrier C, Singhal G, Baune BT. Neuroinflammation and cognition across psychiatric conditions. CNS Spectr. 2019;24:4–15. doi: 10.1017/S1092852918001499. [DOI] [PubMed] [Google Scholar]
- 44.Barron H, Hafizi S, Andreazza AC, Mizrahi R. Neuroinflammation and oxidative stress in psychosis and psychosis risk. Int J Mol Sci. 2017;18:E651. doi: 10.3390/ijms18030651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wei C, Sun Y, Chen N, Chen S, Xiu M, Zhang X. Interaction of oxidative stress and BDNF on executive dysfunction in patients with chronic schizophrenia. Psychoneuroendocrinology 2020, 111: 104473. [DOI] [PubMed]
- 46.Marshall CR, Howrigan DP, Merico D, Thiruvahindrapuram B, Wu W, Greer DS, et al. Contribution of copy number variants to schizophrenia from a genome-wide study of 41, 321 subjects. Nat Genet. 2017;49:27–35. doi: 10.1038/ng.3725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Singh T, Kurki MI, Curtis D, Purcell SM, Crooks L, McRae J, et al. Rare loss-of-function variants in SETD1A are associated with schizophrenia and developmental disorders. Nat Neurosci. 2016;19:571–577. doi: 10.1038/nn.4267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Singh T, Walters JTR, Johnstone M, Curtis D, Suvisaari J, Torniainen M, et al. The contribution of rare variants to risk of schizophrenia in individuals with and without intellectual disability. Nat Genet. 2017;49:1167–1173. doi: 10.1038/ng.3903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Genovese G, Fromer M, Stahl EA, Ruderfer DM, Chambert K, Landén M, et al. Increased burden of ultra-rare protein-altering variants among 4, 877 individuals with schizophrenia. Nat Neurosci. 2016;19:1433–1441. doi: 10.1038/nn.4402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schizophrenia Working Group of the Psychiatric Genomics Consortium Biological insights from 108 schizophrenia-associated genetic loci. Nature. 2014;511:421–427. doi: 10.1038/nature13595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhao LS, Wang HJ, Zhang YM, Wei JX, Ni PY, Ren HY, et al. Interaction between variations in dopamine D2 and serotonin 2A receptor is associated with short-term response to antipsychotics in schizophrenia. Neurosci Bull. 2019;35:1102–1105. doi: 10.1007/s12264-019-00432-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Malhotra D, Sebat J. CNVs: harbingers of a rare variant revolution in psychiatric genetics. Cell. 2012;148:1223–1241. doi: 10.1016/j.cell.2012.02.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rees E, Walters JT, Chambert KD, O'Dushlaine C, Szatkiewicz J, Richards AL, et al. CNV analysis in a large schizophrenia sample implicates deletions at 16p12.1 and SLC1A1 and duplications at 1p36.33 and CGNL1. Hum Mol Genet 2014, 23: 1669–1676. [DOI] [PMC free article] [PubMed]
- 54.Wang Q, ManWu H, Yue WH, Yan H, Zhang YM, Tan LW, et al. Effect of damaging rare mutations in synapse-related gene sets on response to short-term antipsychotic medication in Chinese patients with schizophrenia: A randomized clinical trial. JAMA Psychiatry. 2018;75:1261–1269. doi: 10.1001/jamapsychiatry.2018.3039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Edwards AC, Bigdeli TB, Docherty AR, Bacanu S, Lee D, de Candia TR, et al. Meta-analysis of positive and negative symptoms reveals schizophrenia modifier genes. Schizophr Bull. 2016;42:279–287. doi: 10.1093/schbul/sbv119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Xu C, Aragam N, Li X, Villla EC, Wang L, Briones D, et al. BCL9 and C9orf5 are associated with negative symptoms in schizophrenia: Meta-analysis of two genome-wide association studies. PLoS One. 2013;8:e51674. doi: 10.1371/journal.pone.0051674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Alfimova MV, Kondratyev NV, Tomyshev AS, Lebedeva IS, Lezheiko TV, Kaleda VG, et al. Effects of a GWAS-supported schizophrenia variant in the DRD2 locus on disease risk, anhedonia, and prefrontal cortical thickness. J Mol Neurosci. 2019;68:658–666. doi: 10.1007/s12031-019-01324-w. [DOI] [PubMed] [Google Scholar]
- 58.Shenker JJ, Sengupta SM, Joober R, Malla A, Chakravarty MM, Lepage M. Bipolar disorder risk gene FOXO6 modulates negative symptoms in schizophrenia: A neuroimaging genetics study. J Psychiatry Neurosci. 2017;42:172–180. doi: 10.1503/jpn.150332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wang Y, Fang Y, Shen Y, Xu Q. Analysis of association between the catechol-O-methyltransferase (COMT) gene and negative symptoms in chronic schizophrenia. Psychiatry Res. 2010;179:147–150. doi: 10.1016/j.psychres.2009.03.029. [DOI] [PubMed] [Google Scholar]
- 60.Nicodemus KK, Hargreaves A, Morris D, Anney R, Schizophrenia Psychiatric Genome-wide Association Study (GWAS) Consortium, Wellcome Trust Case Control Consortium, et al. Variability in working memory performance explained by epistasis vs polygenic scores in the ZNF804A pathway. JAMA Psychiatry 2014, 71: 778–785. [DOI] [PMC free article] [PubMed]
- 61.Walters JT, Corvin A, Owen MJ, Williams H, Dragovic M, Quinn EM, et al. Psychosis susceptibility gene ZNF804A and cognitive performance in schizophrenia. Arch Gen Psychiatry. 2010;67:692–700. doi: 10.1001/archgenpsychiatry.2010.81. [DOI] [PubMed] [Google Scholar]
- 62.Stefansson H, Meyer-Lindenberg A, Steinberg S, Magnusdottir B, Morgen K, Arnarsdottir S, et al. CNVs conferring risk of autism or schizophrenia affect cognition in controls. Nature. 2014;505:361–366. doi: 10.1038/nature12818. [DOI] [PubMed] [Google Scholar]
- 63.Smeland OB, Andreassen OA. How can genetics help understand the relationship between cognitive dysfunction and schizophrenia? Scand J Psychol. 2018;59:26–31. doi: 10.1111/sjop.12407. [DOI] [PubMed] [Google Scholar]
- 64.Smeland OB, Frei O, Kauppi K, Hill WD, Li W, Wang Y, et al. Identification of genetic loci jointly influencing schizophrenia risk and the cognitive traits of verbal-numerical reasoning, reaction time, and general cognitive function. JAMA Psychiatry. 2017;74:1065–1075. doi: 10.1001/jamapsychiatry.2017.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mallet J, Le Strat Y, Dubertret C, Gorwood P. Polygenic risk scores shed light on the relationship between schizophrenia and cognitive functioning: Review and meta-analysis. J Clin Med. 2020;9:E341. doi: 10.3390/jcm9020341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Davies G, Armstrong N, Bis JC, Bressler J, Chouraki V, Giddaluru S, et al. Genetic contributions to variation in general cognitive function: A meta-analysis of genome-wide association studies in the CHARGE consortium (N = 53949) Mol Psychiatry. 2015;20:183–192. doi: 10.1038/mp.2014.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sniekers S, Stringer S, Watanabe K, Jansen PR, Coleman JRI, Krapohl E, et al. Genome-wide association meta-analysis of 78, 308 individuals identifies new loci and genes influencing human intelligence. Nat Genet. 2017;49:1107–1112. doi: 10.1038/ng.3869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Richards AL, Pardiñas AF, Frizzati A, Tansey KE, Lynham AJ, Holmans P, et al. The relationship between polygenic risk scores and cognition in schizophrenia. Schizophr Bull (Bp) 2020;46:336–344. doi: 10.1093/schbul/sbz061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Engen MJ, Lyngstad SH, Ueland T, Simonsen CE, Vaskinn A, Smeland O, et al. Polygenic scores for schizophrenia and general cognitive ability: Associations with six cognitive domains, premorbid intelligence, and cognitive composite score in individuals with a psychotic disorder and in healthy controls. Transl Psychiatry. 2020;10:416. doi: 10.1038/s41398-020-01094-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Birnbaum R, Weinberger DR. Genetic insights into the neurodevelopmental origins of schizophrenia. Nat Rev Neurosci. 2017;18:727–740. doi: 10.1038/nrn.2017.125. [DOI] [PubMed] [Google Scholar]
- 71.Hoffmann A, Ziller M, Spengler D. The future is the past: Methylation QTLs in schizophrenia. Genes (Basel) 2016;7:E104. doi: 10.3390/genes7120104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Liu JY, Chen JY, Ehrlich S, Walton E, White T, Perrone-Bizzozero N, et al. Methylation patterns in whole blood correlate with symptoms in schizophrenia patients. Schizophr Bull. 2014;40:769–776. doi: 10.1093/schbul/sbt080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hannon E, Spiers H, Viana J, Pidsley R, Burrage J, Murphy TM, et al. Methylation QTLs in the developing brain and their enrichment in schizophrenia risk loci. Nat Neurosci. 2016;19:48–54. doi: 10.1038/nn.4182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jaffe AE, Gao Y, Deep-Soboslay A, Tao R, Hyde TM, Weinberger DR, et al. Mapping DNA methylation across development, genotype and schizophrenia in the human frontal cortex. Nat Neurosci. 2016;19:40–47. doi: 10.1038/nn.4181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bang MJ, Kang JI, Kim SJ, Park JY, Kim KR, Lee SY, et al. Reduced DNA methylation of the oxytocin receptor gene is associated with anhedonia-asociality in women with recent-onset schizophrenia and ultra-high risk for psychosis. Schizophr Bull. 2019;45:1279–1290. doi: 10.1093/schbul/sbz016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gao J, Yi HW, Tang XW, Feng XT, Yu M, Sha WW, et al. Corrigendum: DNA methylation and gene expression of matrix metalloproteinase 9 gene in deficit and non-deficit schizophrenia. Front Genet. 2020;11:823. doi: 10.3389/fgene.2020.00823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Grayson DR, Guidotti A. The dynamics of DNA methylation in schizophrenia and related psychiatric disorders. Neuropsychopharmacology. 2013;38:138–166. doi: 10.1038/npp.2012.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Fachim HA, Loureiro CM, Corsi-Zuelli F, Shuhama R, Louzada-Junior P, Menezes PR, et al. GRIN2B promoter methylation deficits in early-onset schizophrenia and its association with cognitive function. Epigenomics. 2019;11:401–410. doi: 10.2217/epi-2018-0127. [DOI] [PubMed] [Google Scholar]
- 79.Lin DD, Chen JY, Duan KK, Perrone-Bizzozero N, Sui J, Calhoun V, et al. Network modules linking expression and methylation in prefrontal cortex of schizophrenia. Epigenetics 2020: 1–18. [DOI] [PMC free article] [PubMed]
- 80.Rajarajan P, Gil SE, Brennand KJ, Akbarian S. Spatial genome organization and cognition. Nat Rev Neurosci. 2016;17:681–691. doi: 10.1038/nrn.2016.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Fujita Y, Yamashita T. Spatial organization of genome architecture in neuronal development and disease. Neurochem Int. 2018;119:49–56. doi: 10.1016/j.neuint.2017.06.014. [DOI] [PubMed] [Google Scholar]
- 82.Rajarajan P, Borrman T, Liao W, Espeso-Gil S, Chandrasekaran S, Jiang Y, et al. Spatial genome exploration in the context of cognitive and neurological disease. Curr Opin Neurobiol. 2019;59:112–119. doi: 10.1016/j.conb.2019.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Rajarajan P, Borrman T, Liao W, Schrode N, Flaherty E, Casiño C, et al. Neuron-specific signatures in the chromosomal connectome associated with schizophrenia risk. Science 2018, 362: eaat4311. [DOI] [PMC free article] [PubMed]
- 84.Butler AA, Webb WM, Lubin FD. Regulatory RNAs and control of epigenetic mechanisms: Expectations for cognition and cognitive dysfunction. Epigenomics. 2016;8:135–151. doi: 10.2217/epi.15.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gibbons A, Udawela M, Dean B. Non-coding RNA as novel players in the pathophysiology of schizophrenia. Noncoding RNA. 2018;4:E11. doi: 10.3390/ncrna4020011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.van Os J, Rutten BP, Poulton R. Gene-environment interactions in schizophrenia: Review of epidemiological findings and future directions. Schizophr Bull. 2008;34:1066–1082. doi: 10.1093/schbul/sbn117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Insel TR. Rethinking schizophrenia. Nature. 2010;468:187–193. doi: 10.1038/nature09552. [DOI] [PubMed] [Google Scholar]
- 88.Cannon TD. How schizophrenia develops: Cognitive and brain mechanisms underlying onset of psychosis. Trends Cogn Sci. 2015;19:744–756. doi: 10.1016/j.tics.2015.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Green MF, Horan WP, Lee J. Social cognition in schizophrenia. Nat Rev Neurosci. 2015;16:620–631. doi: 10.1038/nrn4005. [DOI] [PubMed] [Google Scholar]
- 90.Malkki H. Altered epigenetic regulation in early development associated with schizophrenia. Nat Rev Neurol. 2016;12:1. doi: 10.1038/nrneurol.2015.239. [DOI] [PubMed] [Google Scholar]
- 91.Green MJ, Chia TY, Cairns MJ, Wu JQ, Tooney PA, Scott RJ, et al. Catechol-O-methyltransferase (COMT) genotype moderates the effects of childhood trauma on cognition and symptoms in schizophrenia. J Psychiatr Res. 2014;49:43–50. doi: 10.1016/j.jpsychires.2013.10.018. [DOI] [PubMed] [Google Scholar]
- 92.Moody L, Chen H, Pan YX. Early-life nutritional programming of cognition-the fundamental role of epigenetic mechanisms in mediating the relation between early-life environment and learning and memory process. Adv Nutr. 2017;8:337–350. doi: 10.3945/an.116.014209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Haddad PM, Correll CU. The acute efficacy of antipsychotics in schizophrenia: A review of recent meta-analyses. Ther Adv Psychopharmacol. 2018;8:303–318. doi: 10.1177/2045125318781475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Winkelbeiner S, Leucht S, Kane JM, Homan P, Homan P. Evaluation of differences in individual treatment response in schizophrenia spectrum disorders: A meta-analysis. JAMA Psychiatry. 2019;76:1063–1073. doi: 10.1001/jamapsychiatry.2019.1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Leucht S, Cipriani A, Spineli L, Mavridis D, Orey D, Richter F, et al. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: A multiple-treatments meta-analysis. Lancet. 2013;382:951–962. doi: 10.1016/S0140-6736(13)60733-3. [DOI] [PubMed] [Google Scholar]
- 96.Leucht S, Leucht C, Huhn M, Chaimani A, Mavridis D, Helfer B, et al. Sixty years of placebo-controlled antipsychotic drug trials in acute schizophrenia: Systematic review, Bayesian meta-analysis, and meta-regression of efficacy predictors. Am J Psychiatry. 2017;174:927–942. doi: 10.1176/appi.ajp.2017.16121358. [DOI] [PubMed] [Google Scholar]
- 97.Zipursky RB, Agid O. Recovery, not progressive deterioration, should be the expectation in schizophrenia. World Psychiatry. 2015;14:94–96. doi: 10.1002/wps.20194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.McEvoy JP, Lieberman JA, Stroup TS, Davis SM, Meltzer HY, Rosenheck RA, et al. Effectiveness of clozapine versus olanzapine, quetiapine, and risperidone in patients with chronic schizophrenia who did not respond to prior atypical antipsychotic treatment. Am J Psychiatry. 2006;163:600–610. doi: 10.1176/ajp.2006.163.4.600. [DOI] [PubMed] [Google Scholar]
- 99.Volavka J, Czobor P, Sheitman B, Lindenmayer JP, Citrome L, McEvoy JP, et al. Clozapine, olanzapine, risperidone, and haloperidol in the treatment of patients with chronic schizophrenia and schizoaffective disorder. Am J Psychiatry. 2002;159:255–262. doi: 10.1176/appi.ajp.159.2.255. [DOI] [PubMed] [Google Scholar]
- 100.Fusar-Poli P, Papanastasiou E, Stahl D, Rocchetti M, Carpenter W, Shergill S, et al. Treatments of negative symptoms in schizophrenia: Meta-analysis of 168 randomized placebo-controlled trials. Schizophr Bull. 2015;41:892–899. doi: 10.1093/schbul/sbu170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Keefe RS, Buchanan RW, Marder SR, Schooler NR, Dugar A, Zivkov M, et al. Clinical trials of potential cognitive-enhancing drugs in schizophrenia: What have we learned so far? Schizophr Bull. 2013;39:417–435. doi: 10.1093/schbul/sbr153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Kirschner M, Aleman A, Kaiser S. Secondary negative symptoms - A review of mechanisms, assessment and treatment. Schizophr Res. 2017;186:29–38. doi: 10.1016/j.schres.2016.05.003. [DOI] [PubMed] [Google Scholar]
- 103.Mucci A, Merlotti E, Üçok A, Aleman A, Galderisi S. Primary and persistent negative symptoms: Concepts, assessments and neurobiological bases. Schizophr Res. 2017;186:19–28. doi: 10.1016/j.schres.2016.05.014. [DOI] [PubMed] [Google Scholar]
- 104.Correll CU, Schooler NR. Negative symptoms in schizophrenia: A review and clinical guide for recognition, assessment, and treatment. Neuropsychiatr Dis Treat. 2020;16:519–534. doi: 10.2147/NDT.S225643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Stauffer VL, Song G, Kinon BJ, Ascher-Svanum H, Chen L, Feldman PD, et al. Responses to antipsychotic therapy among patients with schizophrenia or schizoaffective disorder and either predominant or prominent negative symptoms. Schizophr Res. 2012;134:195–201. doi: 10.1016/j.schres.2011.09.028. [DOI] [PubMed] [Google Scholar]
- 106.Arango C, Garibaldi G, Marder SR. Pharmacological approaches to treating negative symptoms: A review of clinical trials. Schizophr Res. 2013;150:346–352. doi: 10.1016/j.schres.2013.07.026. [DOI] [PubMed] [Google Scholar]
- 107.Cerveri G, Gesi C, Mencacci C. Pharmacological treatment of negative symptoms in schizophrenia: Update and proposal of a clinical algorithm. Neuropsychiatr Dis Treat. 2019;15:1525–1535. doi: 10.2147/NDT.S201726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Krause M, Zhu YK, Huhn M, Schneider-Thoma J, Bighelli I, Nikolakopoulou A, et al. Antipsychotic drugs for patients with schizophrenia and predominant or prominent negative symptoms: A systematic review and meta-analysis. Eur Arch Psychiatry Clin Neurosci. 2018;268:625–639. doi: 10.1007/s00406-018-0869-3. [DOI] [PubMed] [Google Scholar]
- 109.Loo H, Poirier-Littre MF, Theron M, Rein W, Fleurot O. Amisulpride versus placebo in the medium-term treatment of the negative symptoms of schizophrenia. Br J Psychiatry. 1997;170:18–22. doi: 10.1192/bjp.170.1.18. [DOI] [PubMed] [Google Scholar]
- 110.Danion JM, Rein W, Fleurot O. Improvement of schizophrenic patients with primary negative symptoms treated with amisulpride. Amisulpride Study Group. Am J Psychiatry. 1999;156:610–616. doi: 10.1176/ajp.156.4.610. [DOI] [PubMed] [Google Scholar]
- 111.Boyer P, Lecrubier Y, Puech AJ, Dewailly J, Aubin F. Treatment of negative symptoms in schizophrenia with amisulpride. Br J Psychiatry. 1995;166:68–72. doi: 10.1192/bjp.166.1.68. [DOI] [PubMed] [Google Scholar]
- 112.Paillère-Martinot ML, Lecrubier Y, Martinot JL, Aubin F. Improvement of some schizophrenic deficit symptoms with low doses of amisulpride. Am J Psychiatry. 1995;152:130–134. doi: 10.1176/ajp.152.1.130. [DOI] [PubMed] [Google Scholar]
- 113.Storosum JG, Elferink AJ, van Zwieten BJ, van Strik R, Hoogendijk WJ, Broekmans AW. Amisulpride: is there a treatment for negative symptoms in schizophrenia patients? Schizophr Bull. 2002;28:193–201. doi: 10.1093/oxfordjournals.schbul.a006931. [DOI] [PubMed] [Google Scholar]
- 114.Liang Y, Yu X. Effectiveness of amisulpride in Chinese patients with predominantly negative symptoms of schizophrenia: A subanalysis of the ESCAPE study. Neuropsychiatr Dis Treat. 2017;13:1703–1712. doi: 10.2147/NDT.S140905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Leucht S, Pitschel-Walz G, Engel RR, Kissling W. Amisulpride, an unusual “atypical” antipsychotic: A meta-analysis of randomized controlled trials. Am J Psychiatry. 2002;159:180–190. doi: 10.1176/appi.ajp.159.2.180. [DOI] [PubMed] [Google Scholar]
- 116.Durgam S, Starace A, Li DY, Migliore R, Ruth A, Németh G, et al. An evaluation of the safety and efficacy of cariprazine in patients with acute exacerbation of schizophrenia: A phase II, randomized clinical trial. Schizophr Res. 2014;152:450–457. doi: 10.1016/j.schres.2013.11.041. [DOI] [PubMed] [Google Scholar]
- 117.Durgam S, Cutler AJ, Lu KF, Migliore R, Ruth A, Laszlovszky I, et al. Cariprazine in acute exacerbation of schizophrenia: A fixed-dose, phase 3, randomized, double-blind, placebo- and active-controlled trial. J Clin Psychiatry. 2015;76:e1574–e1582. doi: 10.4088/JCP.15m09997. [DOI] [PubMed] [Google Scholar]
- 118.Kane JM, Zukin S, Wang Y, Lu KF, Ruth A, Nagy K, et al. Efficacy and safety of cariprazine in acute exacerbation of schizophrenia: Results from an international, phase III clinical trial. J Clin Psychopharmacol. 2015;35:367–373. doi: 10.1097/JCP.0000000000000346. [DOI] [PubMed] [Google Scholar]
- 119.Durgam S, Litman RE, Papadakis K, Li DY, Németh G, Laszlovszky I. Cariprazine in the treatment of schizophrenia: A proof-of-concept trial. Int Clin Psychopharmacol. 2016;31:61–68. doi: 10.1097/YIC.0000000000000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Zhao MJ, Qin B, Wang JB, Zhang YP, Zhao JT, Mao YG, et al. Efficacy and acceptability of cariprazine in acute exacerbation of schizophrenia: Meta-analysis of randomized placebo-controlled trials. J Clin Psychopharmacol. 2018;38:55–59. doi: 10.1097/JCP.0000000000000834. [DOI] [PubMed] [Google Scholar]
- 121.Marder S, Fleischhacker WW, Earley W, Lu KF, Zhong Y, Németh G, et al. Efficacy of cariprazine across symptom domains in patients with acute exacerbation of schizophrenia: Pooled analyses from 3 phase II/III studies. Eur Neuropsychopharmacol. 2019;29:127–136. doi: 10.1016/j.euroneuro.2018.10.008. [DOI] [PubMed] [Google Scholar]
- 122.Cutler AJ, Durgam S, Wang Y, Migliore R, Lu KF, Laszlovszky I, et al. Evaluation of the long-term safety and tolerability of cariprazine in patients with schizophrenia: Results from a 1-year open-label study. CNS Spectr. 2018;23:39–50. doi: 10.1017/S1092852917000220. [DOI] [PubMed] [Google Scholar]
- 123.Earley W, Durgam S, Lu KF, Laszlovszky I, Debelle M, Kane JM. Safety and tolerability of cariprazine in patients with acute exacerbation of schizophrenia: A pooled analysis of four phase II/III randomized, double-blind, placebo-controlled studies. Int Clin Psychopharmacol. 2017;32:319–328. doi: 10.1097/YIC.0000000000000187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Leucht S, Davis JM. Schizophrenia, primary negative symptoms, and soft outcomes in psychiatry. Lancet. 2017;389:1077–1078. doi: 10.1016/S0140-6736(17)30181-2. [DOI] [PubMed] [Google Scholar]
- 125.Németh G, Laszlovszky I, Czobor P, Szalai E, Szatmári B, Harsányi J, et al. Cariprazine versus risperidone monotherapy for treatment of predominant negative symptoms in patients with schizophrenia: A randomised, double-blind, controlled trial. Lancet. 2017;389:1103–1113. doi: 10.1016/S0140-6736(17)30060-0. [DOI] [PubMed] [Google Scholar]
- 126.Fleischhacker W, Galderisi S, Laszlovszky I, Szatmári B, Barabássy Á, Acsai K, et al. The efficacy of cariprazine in negative symptoms of schizophrenia: Post hoc analyses of PANSS individual items and PANSS-derived factors. Eur Psychiatry. 2019;58:1–9. doi: 10.1016/j.eurpsy.2019.01.015. [DOI] [PubMed] [Google Scholar]
- 127.Bitter I, Lieberman JA, Gaudoux F, Sokoloff P, Groc M, Chavda R, et al. Randomized, double-blind, placebo-controlled study of F17464, a preferential D3 antagonist, in the treatment of acute exacerbation of schizophrenia. Neuropsychopharmacology. 2019;44:1917–1924. doi: 10.1038/s41386-019-0355-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Potkin SG, Cohen M, Panagides J. Efficacy and tolerability of asenapine in acute schizophrenia: A placebo- and risperidone-controlled trial. J Clin Psychiatry. 2007;68:1492–1500. doi: 10.4088/JCP.v68n1004. [DOI] [PubMed] [Google Scholar]
- 129.Kane JM, Cohen M, Zhao J, Alphs L, Panagides J. Efficacy and safety of asenapine in a placebo- and haloperidol-controlled trial in patients with acute exacerbation of schizophrenia. J Clin Psychopharmacol. 2010;30:106–115. doi: 10.1097/JCP.0b013e3181d35d6b. [DOI] [PubMed] [Google Scholar]
- 130.Buchanan RW, Panagides J, Zhao J, Phiri P, den Hollander W, Ha X, et al. Asenapine versus olanzapine in people with persistent negative symptoms of schizophrenia. J Clin Psychopharmacol. 2012;32:36–45. doi: 10.1097/JCP.0b013e31823f880a. [DOI] [PubMed] [Google Scholar]
- 131.Potkin SG, Phiri P, Szegedi A, Zhao J, Alphs L, Cazorla P. Long-term effects of asenapine or olanzapine in patients with persistent negative symptoms of schizophrenia: A pooled analysis. Schizophr Res. 2013;150:442–449. doi: 10.1016/j.schres.2013.08.024. [DOI] [PubMed] [Google Scholar]
- 132.Sabe M, Kirschner M, Kaiser S. Prodopaminergic drugs for treating the negative symptoms of schizophrenia: Systematic review and meta-analysis of randomized controlled trials. J Clin Psychopharmacol. 2019;39:658–664. doi: 10.1097/JCP.0000000000001124. [DOI] [PubMed] [Google Scholar]
- 133.Lasser RA, Dirks B, Nasrallah H, Kirsch C, Gao J, Pucci ML, et al. Adjunctive lisdexamfetamine dimesylate therapy in adult outpatients with predominant negative symptoms of schizophrenia: Open-label and randomized-withdrawal phases. Neuropsychopharmacology. 2013;38:2140–2149. doi: 10.1038/npp.2013.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Girgis RR, van Snellenberg JX, Glass A, Kegeles LS, Thompson JL, Wall M, et al. A proof-of-concept, randomized controlled trial of DAR-0100A, a dopamine-1 receptor agonist, for cognitive enhancement in schizophrenia. J Psychopharmacol. 2016;30:428–435. doi: 10.1177/0269881116636120. [DOI] [PubMed] [Google Scholar]
- 135.Singh SP, Singh V, Kar N, Chan K. Efficacy of antidepressants in treating the negative symptoms of chronic schizophrenia: Meta-analysis. Br J Psychiatry. 2010;197:174–179. doi: 10.1192/bjp.bp.109.067710. [DOI] [PubMed] [Google Scholar]
- 136.Helfer B, Samara MT, Huhn M, Klupp E, Leucht C, Zhu YK, et al. Efficacy and safety of antidepressants added to antipsychotics for schizophrenia: A systematic review and meta-analysis. Am J Psychiatry. 2016;173:876–886. doi: 10.1176/appi.ajp.2016.15081035. [DOI] [PubMed] [Google Scholar]
- 137.Galling B, Vernon JA, Pagsberg AK, Wadhwa A, Grudnikoff E, Seidman AJ, et al. Efficacy and safety of antidepressant augmentation of continued antipsychotic treatment in patients with schizophrenia. Acta Psychiatr Scand. 2018;137:187–205. doi: 10.1111/acps.12854. [DOI] [PubMed] [Google Scholar]
- 138.Ding N, Li ZQ, Liu ZX. Escitalopram augmentation improves negative symptoms of treatment resistant schizophrenia patients - A randomized controlled trial. Neurosci Lett. 2018;681:68–72. doi: 10.1016/j.neulet.2018.05.030. [DOI] [PubMed] [Google Scholar]
- 139.Arango C, Kirkpatrick B, Buchanan RW. Fluoxetine as an adjunct to conventional antipsychotic treatment of schizophrenia patients with residual symptoms. J Nerv Ment Dis. 2000;188:50–53. doi: 10.1097/00005053-200001000-00010. [DOI] [PubMed] [Google Scholar]
- 140.Jones MT, Strassnig MT, Harvey PD. Emerging 5-HT receptor antagonists for the treatment of Schizophrenia. Expert Opin Emerg Drugs. 2020;25:189–200. doi: 10.1080/14728214.2020.1773792. [DOI] [PubMed] [Google Scholar]
- 141.Davidson M, Saoud J, Staner C, Noel N, Luthringer E, Werner S, et al. Efficacy and safety of MIN-101: A 12-week randomized, double-blind, placebo-controlled trial of a new drug in development for the treatment of negative symptoms in schizophrenia. Am J Psychiatry. 2017;174:1195–1202. doi: 10.1176/appi.ajp.2017.17010122. [DOI] [PubMed] [Google Scholar]
- 142.Harvey PD, Saoud JB, Luthringer R, Moroz S, Blazhevych Y, Stefanescu C, et al. Effects of Roluperidone (MIN-101) on two dimensions of the negative symptoms factor score: Reduced emotional experience and reduced emotional expression. Schizophr Res. 2020;215:352–356. doi: 10.1016/j.schres.2019.08.029. [DOI] [PubMed] [Google Scholar]
- 143.Rabinowitz J, Badescu S, Palamarchuk P, Filyk V, Voloshchuk A, Rud V, et al. Personal and social adjustment effects of roluperidone in patients with schizophrenia and negative symptoms: Results from an exploratory outcome of a randomized placebo-controlled trial. Schizophr Res. 2019;211:103–104. doi: 10.1016/j.schres.2019.07.029. [DOI] [PubMed] [Google Scholar]
- 144.Keefe RSE, Harvey PD, Khan A, Saoud JB, Staner C, Davidson M, et al. Cognitive effects of MIN-101 in patients with schizophrenia and negative symptoms: Results from a randomized controlled trial. J Clin Psychiatry 2018, 79: 17m11753. [DOI] [PubMed]
- 145.Belforte JE, Zsiros V, Sklar ER, Jiang ZH, Yu G, Li YQ, et al. Postnatal NMDA receptor ablation in corticolimbic interneurons confers schizophrenia-like phenotypes. Nat Neurosci. 2010;13:76–83. doi: 10.1038/nn.2447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Hardingham GE, Do KQ. Linking early-life NMDAR hypofunction and oxidative stress in schizophrenia pathogenesis. Nat Rev Neurosci. 2016;17:125–134. doi: 10.1038/nrn.2015.19. [DOI] [PubMed] [Google Scholar]
- 147.Field JR, Walker AG, Conn PJ. Targeting glutamate synapses in schizophrenia. Trends Mol Med. 2011;17:689–698. doi: 10.1016/j.molmed.2011.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Uno Yota, Coyle Joseph T.. Glutamate hypothesis in schizophrenia. Psychiatry Clin Neurosci 2019, 73: 204–215. [DOI] [PubMed]
- 149.Balu DT, Coyle JT. The NMDA receptor ‘Glycine modulatory site’ in schizophrenia: D-serine, Glycine, and beyond. Curr Opin Pharmacol. 2015;20:109–115. doi: 10.1016/j.coph.2014.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Tsai GE, Lin PY. Strategies to enhance N-methyl-D-aspartate receptor-mediated neurotransmission in schizophrenia, a critical review and meta-analysis. Curr Pharm Des. 2010;16:522–537. doi: 10.2174/138161210790361452. [DOI] [PubMed] [Google Scholar]
- 151.Singh SP, Singh V. Meta-analysis of the efficacy of adjunctive NMDA receptor modulators in chronic schizophrenia. CNS Drugs. 2011;25:859–885. doi: 10.2165/11586650-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 152.Matsuda Y, Kishi T, Iwata N. Efficacy and safety of NMDA receptor antagonists augmentation therapy for schizophrenia: An updated meta-analysis of randomized placebo-controlled trials. J Psychiatr Res. 2013;47:2018–2020. doi: 10.1016/j.jpsychires.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 153.Chang CH, Lane HY, Tseng PT, Chen SJ, Liu CY, Lin CH. Effect of N-methyl-D-aspartate-receptor-enhancing agents on cognition in patients with schizophrenia: A systematic review and meta-analysis of double-blind randomised controlled trials. J Psychopharmacol. 2019;33:436–448. doi: 10.1177/0269881118822157. [DOI] [PubMed] [Google Scholar]
- 154.Krogmann A, Peters L, von Hardenberg L, Bödeker K, Nöhles VB, Correll CU. Keeping up with the therapeutic advances in schizophrenia: A review of novel and emerging pharmacological entities. CNS Spectr. 2019;24:38–69. doi: 10.1017/S109285291900124X. [DOI] [PubMed] [Google Scholar]
- 155.Zhang LL, Zheng HB, Wu RR, Zhu FR, Kosten TR, Zhang XY, et al. Minocycline adjunctive treatment to risperidone for negative symptoms in schizophrenia: Association with pro-inflammatory cytokine levels. Prog Neuropsychopharmacol Biol Psychiatry. 2018;85:69–76. doi: 10.1016/j.pnpbp.2018.04.004. [DOI] [PubMed] [Google Scholar]
- 156.Liu F, Guo XF, Wu RR, Ou JJ, Zheng YJ, Zhang BK, et al. Minocycline supplementation for treatment of negative symptoms in early-phase schizophrenia: A double blind, randomized, controlled trial. Schizophr Res. 2014;153:169–176. doi: 10.1016/j.schres.2014.01.011. [DOI] [PubMed] [Google Scholar]
- 157.Chaudhry IB, Hallak J, Husain N, Minhas F, Stirling J, Richardson P, et al. Minocycline benefits negative symptoms in early schizophrenia: A randomised double-blind placebo-controlled clinical trial in patients on standard treatment. J Psychopharmacol. 2012;26:1185–1193. doi: 10.1177/0269881112444941. [DOI] [PubMed] [Google Scholar]
- 158.Levkovitz Y, Mendlovich S, Riwkes S, Braw Y, Levkovitch-Verbin H, Gal G, et al. A double-blind, randomized study of minocycline for the treatment of negative and cognitive symptoms in early-phase schizophrenia. J Clin Psychiatry. 2010;71:138–149. doi: 10.4088/JCP.08m04666yel. [DOI] [PubMed] [Google Scholar]
- 159.Deakin B, Suckling J, Barnes TRE, Byrne K, Chaudhry IB, Dazzan P, et al. The benefit of minocycline on negative symptoms of schizophrenia in patients with recent-onset psychosis (BeneMin): A randomised, double-blind, placebo-controlled trial. Lancet Psychiatry. 2018;5:885–894. doi: 10.1016/S2215-0366(18)30345-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Khodaie-Ardakani MR, Mirshafiee O, Farokhnia M, Tajdini M, Hosseini SM, Modabbernia A, et al. Minocycline add-on to risperidone for treatment of negative symptoms in patients with stable schizophrenia: Randomized double-blind placebo-controlled study. Psychiatry Res. 2014;215:540–546. doi: 10.1016/j.psychres.2013.12.051. [DOI] [PubMed] [Google Scholar]
- 161.Fahey JW, Talalay P. Antioxidant functions of sulforaphane: A potent inducer of Phase II detoxication enzymes. Food Chem Toxicol. 1999;37:973–979. doi: 10.1016/S0278-6915(99)00082-4. [DOI] [PubMed] [Google Scholar]
- 162.Cardozo LF, Pedruzzi LM, Stenvinkel P, Stockler-Pinto MB, Daleprane JB, Leite M, Jr, et al. Nutritional strategies to modulate inflammation and oxidative stress pathways via activation of the master antioxidant switch Nrf2. Biochimie. 2013;95:1525–1533. doi: 10.1016/j.biochi.2013.04.012. [DOI] [PubMed] [Google Scholar]
- 163.Keum YS. Regulation of the Keap1/Nrf2 system by chemopreventive sulforaphane: Implications of posttranslational modifications. Ann N Y Acad Sci. 2011;1229:184–189. doi: 10.1111/j.1749-6632.2011.06092.x. [DOI] [PubMed] [Google Scholar]
- 164.Shiina A, Kanahara N, Sasaki T, Oda Y, Hashimoto T, Hasegawa T, et al. An open study of sulforaphane-rich broccoli sprout extract in patients with schizophrenia. Clin Psychopharmacol Neurosci. 2015;13:62–67. doi: 10.9758/cpn.2015.13.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Sedlak TW, Nucifora LG, Koga M, Shaffer LS, Higgs C, Tanaka T, et al. Sulforaphane augments glutathione and influences brain metabolites in human subjects: A clinical pilot study. Mol Neuropsychiatry. 2018;3:214–222. doi: 10.1159/000487639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Satogami K, Takahashi S, Yamada S, Ukai S, Shinosaki K. Omega-3 fatty acids related to cognitive impairment in patients with schizophrenia. Schizophr Res Cogn. 2017;9:8–12. doi: 10.1016/j.scog.2017.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Chen AT, Chibnall JT, Nasrallah HA. A meta-analysis of placebo-controlled trials of Omega-3 fatty acid augmentation in schizophrenia: Possible stage-specific effects. Ann Clin Psychiatry. 2015;27:289–296. [PubMed] [Google Scholar]
- 168.Xu FK, Fan WX, Wang WP, Tang W, Yang FY, Zhang Y, et al. Effects of Omega-3 fatty acids on metabolic syndrome in patients with schizophrenia: A 12-week randomized placebo-controlled trial. Psychopharmacology (Berl) 2019;236:1273–1279. doi: 10.1007/s00213-018-5136-9. [DOI] [PubMed] [Google Scholar]
- 169.Fenton WS, Dickerson F, Boronow J, Hibbeln JR, Knable M. A placebo-controlled trial of Omega-3 fatty acid (ethyl eicosapentaenoic acid) supplementation for residual symptoms and cognitive impairment in schizophrenia. Am J Psychiatry. 2001;158:2071–2074. doi: 10.1176/appi.ajp.158.12.2071. [DOI] [PubMed] [Google Scholar]
- 170.Nieuwdorp W, Koops S, Somers M, Sommer IE. Transcranial magnetic stimulation, transcranial direct current stimulation and electroconvulsive therapy for medication-resistant psychosis of schizophrenia. Curr Opin Psychiatry. 2015;28:222–228. doi: 10.1097/YCO.0000000000000156. [DOI] [PubMed] [Google Scholar]
- 171.Petrides G, Malur C, Braga RJ, Bailine SH, Schooler NR, Malhotra AK, et al. Electroconvulsive therapy augmentation in clozapine-resistant schizophrenia: A prospective, randomized study. Am J Psychiatry. 2015;172:52–58. doi: 10.1176/appi.ajp.2014.13060787. [DOI] [PubMed] [Google Scholar]
- 172.Wang WZ, Pu CC, Jiang JL, Cao XY, Wang JJ, Zhao M, et al. Efficacy and safety of treating patients with refractory schizophrenia with antipsychotic medication and adjunctive electroconvulsive therapy: A systematic review and meta-analysis. Shanghai Arch Psychiatry. 2015;27:206–219. doi: 10.11919/j.issn.1002-0829.215093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Aleman A, Enriquez-Geppert S, Knegtering H, Dlabac-de Lange JJ. Moderate effects of noninvasive brain stimulation of the frontal cortex for improving negative symptoms in schizophrenia: Meta-analysis of controlled trials. Neurosci Biobehav Rev. 2018;89:111–118. doi: 10.1016/j.neubiorev.2018.02.009. [DOI] [PubMed] [Google Scholar]
- 174.Mehta UM, Naik SS, Thanki MV, Thirthalli J. Investigational and therapeutic applications of transcranial magnetic stimulation in schizophrenia. Curr Psychiatry Rep. 2019;21:89. doi: 10.1007/s11920-019-1076-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Tendler A, Roth Y, Barnea-Ygael N, Zangen A. How to use the H1 deep transcranial magnetic stimulation coil for conditions other than depression. J Vis Exp. 2017 doi: 10.3791/55100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Dougall N, Maayan N, Soares-Weiser K, McDermott LM, McIntosh A. Transcranial magnetic stimulation for schizophrenia. Schizophr Bull. 2015;41:1220–1222. doi: 10.1093/schbul/sbv121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Levkovitz Y, Rabany L, Harel EV, Zangen A. Deep transcranial magnetic stimulation add-on for treatment of negative symptoms and cognitive deficits of schizophrenia: A feasibility study. Int J Neuropsychopharmacol. 2011;14:991–996. doi: 10.1017/S1461145711000642. [DOI] [PubMed] [Google Scholar]
- 178.Rabany L, Deutsch L, Levkovitz Y. Double-blind, randomized sham controlled study of deep-TMS add-on treatment for negative symptoms and cognitive deficits in schizophrenia. J Psychopharmacol. 2014;28:686–690. doi: 10.1177/0269881114533600. [DOI] [PubMed] [Google Scholar]
- 179.Linsambarth S, Jeria A, Avirame K, Todder D, Riquelme R, Stehberg J. Deep transcranial magnetic stimulation for the treatment of negative symptoms in schizophrenia: Beyond an antidepressant effect. J ECT. 2019;35:e46–e54. doi: 10.1097/YCT.0000000000000592. [DOI] [PubMed] [Google Scholar]
- 180.Garg S, Sinha VK, Tikka SK, Mishra P, Goyal N. The efficacy of cerebellar vermal deep high frequency (Theta range) repetitive transcranial magnetic stimulation (rTMS) in schizophrenia: A randomized rater blind-sham controlled study. Psychiatry Res. 2016;243:413–420. doi: 10.1016/j.psychres.2016.07.023. [DOI] [PubMed] [Google Scholar]
- 181.Dlabac-de Lange JJ, Bais L, van Es FD, Visser BG, Reinink E, Bakker B, et al. Efficacy of bilateral repetitive transcranial magnetic stimulation for negative symptoms of schizophrenia: Results of a multicenter double-blind randomized controlled trial. Psychol Med. 2015;45:1263–1275. doi: 10.1017/S0033291714002360. [DOI] [PubMed] [Google Scholar]
- 182.Wagner E, Wobrock T, Kunze B, Langguth B, Landgrebe M, Eichhammer P, et al. Efficacy of high-frequency repetitive transcranial magnetic stimulation in schizophrenia patients with treatment-resistant negative symptoms treated with clozapine. Schizophr Res. 2019;208:370–376. doi: 10.1016/j.schres.2019.01.021. [DOI] [PubMed] [Google Scholar]
- 183.Prikryl R, Mikl M, Prikrylova Kucerová H, Ustohal L, Kasparek T, Marecek R, et al. Does repetitive transcranial magnetic stimulation have a positive effect on working memory and neuronal activation in treatment of negative symptoms of schizophrenia? Neuro Endocrinol Lett. 2012;33:90–97. [PubMed] [Google Scholar]
- 184.Wölwer W, Lowe A, Brinkmeyer J, Streit M, Habakuck M, Agelink MW, et al. Repetitive transcranial magnetic stimulation (rTMS) improves facial affect recognition in schizophrenia. Brain Stimul. 2014;7:559–563. doi: 10.1016/j.brs.2014.04.011. [DOI] [PubMed] [Google Scholar]
- 185.Hasan A, Guse B, Cordes J, Wölwer W, Winterer G, Gaebel W, et al. Cognitive effects of high-frequency rTMS in schizophrenia patients with predominant negative symptoms: Results from a multicenter randomized sham-controlled trial. Schizophr Bull. 2016;42:608–618. doi: 10.1093/schbul/sbv142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Dougall N, Maayan N, Soares-Weiser K, McDermott LM, McIntosh A. Transcranial magnetic stimulation (TMS) for schizophrenia. Cochrane Database Syst Rev 2015: CD006081. [DOI] [PMC free article] [PubMed]
- 187.Mogg A, Purvis R, Eranti S, Contell F, Taylor JP, Nicholson T, et al. Repetitive transcranial magnetic stimulation for negative symptoms of schizophrenia: A randomized controlled pilot study. Schizophr Res. 2007;93:221–228. doi: 10.1016/j.schres.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 188.Wobrock T, Guse B, Cordes J, Wölwer W, Winterer G, Gaebel W, et al. Left prefrontal high-frequency repetitive transcranial magnetic stimulation for the treatment of schizophrenia with predominant negative symptoms: A sham-controlled, randomized multicenter trial. Biol Psychiatry. 2015;77:979–988. doi: 10.1016/j.biopsych.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 189.Koutsouleris N, Wobrock T, Guse B, Langguth B, Landgrebe M, Eichhammer P, et al. Predicting response to repetitive transcranial magnetic stimulation in patients with schizophrenia using structural magnetic resonance imaging: A multisite machine learning analysis. Schizophr Bull. 2018;44:1021–1034. doi: 10.1093/schbul/sbx114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Lindenmayer JP, Kulsa MKC, Sultana T, Kaur A, Yang R, Ljuri I, et al. Transcranial direct-current stimulation in ultra-treatment-resistant schizophrenia. Brain Stimul. 2019;12:54–61. doi: 10.1016/j.brs.2018.10.002. [DOI] [PubMed] [Google Scholar]
- 191.Sathappan AV, Luber BM, Lisanby SH. The Dynamic Duo: Combining noninvasive brain stimulation with cognitive interventions. Prog Neuropsychopharmacol Biol Psychiatry. 2019;89:347–360. doi: 10.1016/j.pnpbp.2018.10.006. [DOI] [PubMed] [Google Scholar]
- 192.Valiengo LDCL, Goerigk S, Gordon PC, Padberg F, Serpa MH, Koebe S, et al. Efficacy and safety of transcranial direct current stimulation for treating negative symptoms in schizophrenia: A randomized clinical trial. JAMA Psychiatry. 2020;77:121–129. doi: 10.1001/jamapsychiatry.2019.3199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Jeon DW, Jung DU, Kim SJ, Shim JC, Moon JJ, Seo YS, et al. Adjunct transcranial direct current stimulation improves cognitive function in patients with schizophrenia: A double-blind 12-week study. Schizophr Res. 2018;197:378–385. doi: 10.1016/j.schres.2017.12.009. [DOI] [PubMed] [Google Scholar]
- 194.Mervis JE, Capizzi RJ, Boroda E, MacDonald AW., 3rd Transcranial direct current stimulation over the dorsolateral prefrontal cortex in schizophrenia: A quantitative review of cognitive outcomes. Front Hum Neurosci. 2017;11:44. doi: 10.3389/fnhum.2017.00044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Lefaucheur JP, Antal A, Ayache SS, Benninger DH, Brunelin J, Cogiamanian F, et al. Evidence-based guidelines on the therapeutic use of transcranial direct current stimulation (tDCS) Clin Neurophysiol. 2017;128:56–92. doi: 10.1016/j.clinph.2016.10.087. [DOI] [PubMed] [Google Scholar]
- 196.Gandal MJ, Zhang P, Hadjimichael E, Walker RL, Chen C, Liu S, et al. Transcriptome-wide isoform-level dysregulation in ASD, schizophrenia, and bipolar disorder. Science 2018, 362: eaat8127. [DOI] [PMC free article] [PubMed]
- 197.Palm U, Kumpf U, Behler N, Wulf L, Kirsch B, Wörsching J, et al. Home use, remotely supervised, and remotely controlled transcranial direct current stimulation: A systematic review of the available evidence. Neuromodulation. 2018;21:323–333. doi: 10.1111/ner.12686. [DOI] [PubMed] [Google Scholar]
- 198.Chase HW, Boudewyn MA, Carter CS, Phillips ML. Transcranial direct current stimulation: A roadmap for research, from mechanism of action to clinical implementation. Mol Psychiatry. 2020;25:397–407. doi: 10.1038/s41380-019-0499-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Orlov ND, O'Daly O, Tracy DK, Daniju Y, Hodsoll J, Valdearenas L, et al. Stimulating thought: A functional MRI study of transcranial direct current stimulation in schizophrenia. Brain. 2017;140:2490–2497. doi: 10.1093/brain/awx170. [DOI] [PubMed] [Google Scholar]
- 200.Chang CC, Tzeng NS, Chao CY, Yeh CB, Chang HA. The effects of add-on Fronto-temporal transcranial direct current stimulation (tDCS) on auditory verbal hallucinations, other psychopathological symptoms, and insight in schizophrenia: A randomized, double-blind, sham-controlled trial. Int J Neuropsychopharmacol. 2018;21:979–987. doi: 10.1093/ijnp/pyy074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Yu L, Fang X, Chen Y, Wang Y, Wang D, Zhang C. Efficacy of transcranial direct current stimulation in ameliorating negative symptoms and cognitive impairments in schizophrenia: A systematic review and meta-analysis. Schizophr Res. 2020;224:2–10. doi: 10.1016/j.schres.2020.10.006. [DOI] [PubMed] [Google Scholar]
- 202.Turner DT, van der Gaag M, Karyotaki E, Cuijpers P. Psychological interventions for psychosis: A meta-analysis of comparative outcome studies. Am J Psychiatry. 2014;171:523–538. doi: 10.1176/appi.ajp.2013.13081159. [DOI] [PubMed] [Google Scholar]
- 203.Turner DT, McGlanaghy E, Cuijpers P, van der Gaag M, Karyotaki E, MacBeth A. A meta-analysis of social skills training and related interventions for psychosis. Schizophr Bull. 2021;44:475–491. doi: 10.1093/schbul/sbx146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Granholm E, Harvey PD. Social skills training for negative symptoms of schizophrenia. Schizophr Bull. 2018;44:472–474. doi: 10.1093/schbul/sbx184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Nijman SA, Veling W, van der Stouwe ECD, Pijnenborg GHM. Social cognition training for people with a psychotic disorder: A network meta-analysis. Schizophr Bull 2020: sbaa023. [DOI] [PMC free article] [PubMed]
- 206.Cella M, Preti A, Edwards C, Dow T, Wykes T. Cognitive remediation for negative symptoms of schizophrenia: A network meta-analysis. Clin Psychol Rev. 2017;52:43–51. doi: 10.1016/j.cpr.2016.11.009. [DOI] [PubMed] [Google Scholar]
- 207.Sabe M, Sentissi O, Kaiser S. Meditation-based mind-body therapies for negative symptoms of schizophrenia: Systematic review of randomized controlled trials and meta-analysis. Schizophr Res. 2019;212:15–25. doi: 10.1016/j.schres.2019.07.030. [DOI] [PubMed] [Google Scholar]