Abstract
The International Centre for Diarrhoeal Disease Research, Bangladesh, is a major center for research into diarrheal diseases. The center treats more than 100,000 patients a year. To obtain useful information representative of all patients, a surveillance system in which a 4% systematic sample of all patients is studied in detail, including etiological agents of diarrhea, was installed in October 1979. The first paper on etiology for the surveillance patients was published in 1982, which identified a potential enteric pathogen in 66% of patients. In subsequent years, several new agents of diarrhea have been identified. To assess the importance of a broader spectrum of diarrheal agents including the ones identified relatively recently, we studied 814 children with diarrhea. The children were up to 5 years of age and were part of the surveillance system. They were matched with an equal number of community controls without diarrhea. The study was conducted from February 1993 to June 1994. A potential enteric pathogen was isolated from 74.8% of diarrheal children and 43.9% of control children (P = 0.0001). Even though the first study was not a case-control study, it identified rotavirus, Campylobacter jejuni, enterotoxigenic Escherichia coli, Shigella spp., and Vibrio cholerae O1 as major pathogens. The present study identified these pathogens as being significantly associated with diarrhea. In addition, the study also identified six additional agents, including enteropathogenic E. coli, Aeromonas spp., V. cholerae O139, enterotoxigenic Bacteroides fragilis, Clostridium difficile, and Cryptosporidium parvum, as being significantly associated with diarrhea. Plesiomonas shigelloides, Salmonella spp., diffusely adherent E. coli, enteroaggregative E. coli, Entamoeba histolytica, and Giardia lamblia were not significantly associated with diarrhea. Enteroinvasive E. coli, enterohemorrhagic E. coli, and Cyclospora cayetanensis were not detected in any of the children. The major burden of diseases due to most pathogens occurred in the first year of life. As in the previous study, seasonal patterns were seen for diarrhea associated with rotavirus, V. cholerae, and enterotoxigenic E. coli, and infections with multiple pathogens were common. With a few exceptions, these findings are in agreement with those from other developing countries. This knowledge of a broader spectrum of etiological agents of diarrhea in the surveillance patients will help us plan studies into various aspects of diarrheal diseases in this population.
The International Centre for Diarrhoeal Disease Research, Bangladesh (ICDDR,B), located in Dhaka, Bangladesh, is the only international health research institution situated in the developing world. Apart from studying other health-related problems, it primarily conducts research into the etiology, pathogenesis, treatment, and prevention of diarrheal diseases. The center treats more than 100,000 patients a year, and this number is increasing year after year. Although these patients provide valuable materials for research on diarrheal diseases, it is very expensive to gather useful data from all patients because of their great numbers. However, to cull important information which is representative of all patients treated, the center instituted a surveillance system in which every 25th patient (4% sample) is studied in detail, including culturing of stool for important diarrheal pathogens. This surveillance system was established in October 1979, and the first report on the etiological agents of diarrhea in the surveillance patients was published in 1982 (45). Nearly 17 years have passed since publication of that report, and during this period, many new agents of diarrhea have been identified. The center has undertaken some studies on the etiological roles of some new pathogens during this period (1, 39, 40), but a comprehensive study in which all pathogens were sought in a single study has never been undertaken. The objective of the present study was to investigate the etiological roles of a broad array of pathogens including the ones discovered relatively recently.
MATERIALS AND METHODS
Patients.
Children who were up to 5 years of age, who had acute diarrhea (defined as three or more stools a day), and who were seen at the Clinical Research and Service Center of ICDDR,B, from February 1993 to June 1994 were studied. These children were part of the routine surveillance patients (every 25th patient is included in the diarrhea surveillance system) (45). Although this constituted a large sample size for the study period, our objective was to survey pathogens in all surveillance children. The patients were first seen in a triage area, and those requiring further care were admitted to the hospital ward. A physician performed a physical examination and assessed the patient's dehydration status as none, mild, moderate, or severe according to clinical signs (49). A health assistant administered to an adult guardian a questionnaire regarding demographic background, medical history, and previous treatment. A stool specimen collected immediately after admission was used for etiological studies.
Control children.
Controls were healthy children from the same neighborhood as the patients. After leaving the household of a patient in the community, a health worker tossed a pencil onto the street and then walked in the direction in which the sharpened end of the pencil pointed. After passing the first 10 houses, the health worker located the first house with an age-matched control and collected for the control the same information except the physical findings that had been collected for the patients. Control children had not taken antibiotics during the previous 2 weeks. Stool samples were collected from controls within 2 weeks of collection of a sample from patients and were transported in refrigerated boxes to the laboratory within a few hours of collection.
The nutritional statuses of both diarrheal children and control children were expressed by Z scores for weight for age (undernutrition), height for age (stunting), and weight for height (wasting) as described previously (14).
Microbiology.
Stool samples were cultured for bacterial pathogens as described before (1, 40). The samples were plated on MacConkey agar (MA), Salmonella-Shigella agar (SSA), taurocholate-tellurite-gelatin agar (TTGA), Campy-BAP, and Bacteroides fragilis bile-esculin agar (BBE). The specimens were also enriched in selenite F broth and bile peptone broth and were subcultured onto SSA from the former and onto TTGA from the latter. MA and SSA were used for isolation of Escherichia coli, Salmonella spp., and Shigella spp., TTGA was used for isolation of Vibrio cholerae, Campy-BAP was used for isolation of Campylobacter jejuni, and BBE was used for isolation of B. fragilis. All microbiological media or their ingredients were either Difco products (Becton Dickinson Microbiology Systems, Sparks, Md.) or BBL products (Becton Dickinson and Company, Cockeysville, Md.). Enterotoxin production by B. fragilis was assayed by testing culture filtrate from heart infusion broth for morphological changes on the HT 29/C1 human colonic cell line (40). Stool was assayed for Clostridium difficile toxin by a standard tissue culture technique with Vero cells (33). The specificity of the cytopathic effect was verified by neutralization with Clostridium sordelli antitoxin (Wellcome Research Laboratories, Beckenham, United Kingdom). Different categories of diarrheagenic E. coli, enterotoxigenic E. coli (ETEC), enteropathogenic E. coli (EPEC), enteroinvasive E. coli (EIEC), enterohemorrhagic E. coli (EHEC), enteroaggregative E. coli (EAEC), and diffusely adherent E. coli (DAEC), were detected by hybridization of three E. coli colonies from each patient with specific DNA probes (1, 35). E. coli strains positive for hybridization with EPEC adherence factor (EAF) probe and/or the E. coli attachment and effacement gene (eae) probe were identified as EPEC (1, 35). Giardia lamblia and Entamoeba histolytica were detected by direct microscopy of a saline preparation of the specimen. Cryptosporidium parvum and Cyclospora cayetanensis were detected with a modified acid-fast stain (27). Rotavirus was detected by an enzyme-linked immunosorbent assay (47).
Chi-square and Fisher's exact tests were used to compare differences between the groups. A P value of ≤0.05 was considered significant.
RESULTS
A total of 814 children with diarrhea (age, up to 5 years) and an equal number of matched healthy children from the community were enrolled in the study during a 17-month period from February 1993 to June 1994. The number of children in the different age categories is shown in Table 1. Among the case children, the male-to-female ratio was 1:0.7, and among the control children, it was 1:1. Even though malnutrition was common, the nutritional statuses of both diarrheal children and control children were comparable (Table 2).
TABLE 1.
Age strata of 814 children with diarrhea and 814 control children without diarrhea
| Age (mo) | No. (%) of diarrheal children | No. (%) of control children |
|---|---|---|
| 0–12 | 476 (58.5) | 411 (50.5) |
| 13–24 | 193 (23.7) | 234 (28.7) |
| 25–36 | 72 (8.8) | 96 (11.8) |
| 37–48 | 56 (6.9) | 54 (6.6) |
| 49–60 | 17 (2.1) | 19 (2.3) |
TABLE 2.
Nutritional status of 814 children with diarrhea and 814 matched control children without diarrhea
| Parameter (in ≤−2.0 Z score)a | % with a Z score of ≤−2
|
P value | |
|---|---|---|---|
| Diarrheal children | Control children | ||
| Wt for age | 56.0 | 51.4 | 0.20 |
| Ht for age | 45.2 | 42.4 | 0.32 |
| Wt for ht | 22.0 | 18.9 | 0.24 |
Indicates poor nutritional status.
A potential enteric pathogen was isolated from 609 children with diarrhea (74.8%) and 357 controls without diarrhea (43.9%) (P = 0.0001). The rates of isolation of different enteric organisms are shown in Table 3. The organisms that were significantly associated with diarrhea overall were rotavirus, C. jejuni, ETEC, EPEC, Aeromonas spp., Shigella spp., V. cholerae O1, V. cholerae O139, enterotoxigenic B. fragilis (ETBF), C. difficile, and C. parvum EAEC and DAEC were not significantly associated with diarrhea; the latter was isolated from a significantly higher proportion of control children than diarrheal children. Salmonella spp., Plesiomonas shigelloides, G. lamblia, and E. histolytica were isolated from a small number of children and were not associated with diarrhea. G. lamblia was present in a significantly higher proportion of control children than diarrheal children. EIEC, EHEC, and C. cayetanensis were not isolated from any children with or without diarrhea.
TABLE 3.
Major enteric pathogens isolated from 814 children with diarrhea and 814 matched children without diarrhea
| Organism | Age group (mo) | No. (%) of infected children
|
P value | Organism | Age group (mo) | No. (%) of infected children
|
P value | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Diarrheal | Control | Diarrheal | Control | |||||||
| Rotavirus | 0–12 | 118 (24.8) | 6 (1.5) | 0.0001 | ||||||
| 13–24 | 34 (17.6) | 6 (2.6) | 0.0001 | |||||||
| 25–36 | 7 (9.7) | 0 (0.0) | 0.002 | |||||||
| 37–48 | 4 (7.1) | 0 (0.0) | 0.11 | |||||||
| 49–60 | 2 (11.8) | 0 (0.0) | 0.22 | |||||||
| All | 165 (20.3) | 12 (1.5) | 0.0001 | |||||||
| C. jejuni | 0–12 | 84 (17.7) | 54 (13.1) | 0.06 | ||||||
| 13–24 | 31 (16.1) | 31 (13.3) | 0.41 | |||||||
| 25–36 | 11 (15.3) | 10 (10.4) | 0.35 | |||||||
| 37–48 | 10 (17.9) | 6 (11.1) | 0.32 | |||||||
| 49–60 | 6 (35.3) | 2 (10.5) | 0.11 | |||||||
| All | 142 (17.4) | 103 (12.7) | 0.007 | |||||||
| ETEC | 0–12 | 83 (17.4) | 30 (7.3) | 0.0001 | ||||||
| 13–24 | 34 (17.6) | 30 (12.8) | 0.16 | |||||||
| 25–36 | 11 (15.3) | 9 (9.4) | 0.24 | |||||||
| 37–48 | 8 (14.3) | 2 (3.7) | 0.09 | |||||||
| 49–60 | 1 (5.9) | 1 (5.3) | 1.00 | |||||||
| All | 137 (16.8) | 72 (8.8) | 0.0001 | |||||||
| EPEC | 0–12 | 76 (16.0) | 32 (7.8) | 0.0002 | ||||||
| 13–24 | 16 (18.3) | 9 (3.9) | 0.052 | |||||||
| 25–36 | 5 (7.0) | 2 (2.1) | 0.12 | |||||||
| 37–48 | 2 (3.6) | 1 (1.9) | 1.00 | |||||||
| 49–60 | 0 (0.0) | 0 (0.0) | 0 | |||||||
| All | 99 (12.2) | 44 (5.4) | 0.0001 | |||||||
| Aeromonas spp. | 0–12 | 46 (9.7) | 19 (4.6) | 0.004 | ||||||
| 13–24 | 25 (13.0) | 9 (3.9) | 0.0005 | |||||||
| 25–36 | 11 (15.3) | 7 (7.3) | 0.098 | |||||||
| 37–48 | 15 (26.8) | 3 (5.6) | 0.003 | |||||||
| 49–60 | 2 (11.8) | 1 (5.3) | 0.59 | |||||||
| All | 99 (12.2) | 39 (4.8) | 0.0001 | |||||||
| Shigella spp. | 0–12 | 28 (5.9) | 6 (1.5) | 0.0006 | ||||||
| 13–24 | 26 (13.5) | 9 (3.9) | 0.0006 | |||||||
| 25–36 | 11 (15.3) | 7 (7.3) | 0.097 | |||||||
| 37–48 | 7 (12.5) | 2 (3.7) | 0.16 | |||||||
| 49–60 | 3 (17.7) | 0 (0.0) | 0.095 | |||||||
| All | 75 (9.2) | 24 (3.0) | 0.0001 | |||||||
| V. cholerae O1 | 0–12 | 16 (3.4) | 1 (0.2) | 0.0007 | ||||||
| 13–24 | 7 (3.6) | 0 (0.0) | 0.004 | |||||||
| 25–36 | 6 (8.3) | 0 (0.0) | 0.005 | |
| 37–48 | 7 (12.5) | 0 (0.0) | 0.013 | |
| 49–60 | 1 (5.9) | 0 (0.0) | 0.47 | |
| All | 37 (4.5) | 1 (0.1) | 0.0001 | |
| V. cholerae O139 | 0–12 | 8 (1.7) | 2 (0.5) | 0.12 |
| 13–24 | 7 (3.6) | 0 (0.0) | 0.004 | |
| 25–36 | 9 (12.5) | 0 (0.0) | 0.0003 | |
| 37–48 | 8 (14.3) | 0 (0.0) | 0.006 | |
| 49–60 | 2 (11.8) | 0 (0.0) | 0.22 | |
| All | 34 (4.5) | 2 (0.2) | 0.0001 | |
| ETBF | 0–12 | 16 (3.4) | 7 (1.7) | 0.13 |
| 13–24 | 6 (3.1) | 4 (1.7) | 0.36 | |
| 25–36 | 2 (2.9) | 1 (1.1) | 0.58 | |
| 37–48 | 2 (3.8) | 0 (0.0) | 0.57 | |
| 49–60 | 2 (11.8) | 0 (0.0) | 0.22 | |
| All | 28 (3.5) | 12 (1.5) | 0.01 | |
| C. difficile | All | 13 (1.6) | 4 (0.5) | 0.02 |
| C. parvum | All | 11 (1.4) | 3 (0.4) | 0.03 |
| Salmonella spp. | All | 15 (1.8) | 10 (1.2) | 0.31 |
| P. shigelloides | All | 8 (1.0) | 10 (1.2) | 0.64 |
| G. lambliaa | All | 7 (0.8) | 23 (2.9) | 0.003 |
| E. histolytica | All | 5 (0.6) | 1 (0.1) | 0.21 |
| EAEC | 0–12 | 54 (11.3) | 39 (9.5) | 0.37 |
| 13–24 | 18 (9.3) | 15 (6.4) | 0.26 | |
| 25–36 | 3 (4.2) | 3 (3.1) | 1.00 | |
| 37–48 | 2 (3.6) | 0 (0.0) | 0.5 | |
| 49–60 | 0 (0.0) | 0 (0.0) | 0 | |
| All | 77 (9.5) | 57 (7.0) | 0.07 | |
| DAECa | 0–12 | 19 (4.0) | 35 (8.5) | 0.008 |
| 13–24 | 11 (5.7) | 19 (8.1) | 0.33 | |
| 25–36 | 2 (2.8) | 5 (5.2) | 0.77 | |
| 37–48 | 7 (12.5) | 3 (5.6) | 0.32 | |
| 49–60 | 1 (5.9) | 0 (0.0) | 0.47 | |
| All | 40 (4.9) | 62 (7.6) | 0.02 |
These organisms were isolated from significantly higher proportions of control children than diarrheal children.
Analysis of data according to age strata showed a significant association with diarrhea for all pathogens in the first year of life except for C. jejuni, V. cholerae O139, and ETBF, which had an overall association with diarrhea. In addition, rotavirus, Aeromonas spp., Shigella spp., and V. cholerae O1 were associated with diarrhea beyond the first year of life. V. cholerae O139 was also associated with diarrhea beyond the first year of life (Table 3). Because in the older age group, the numbers were small and one would not expect to see statistically significant differences, analysis was repeated by pooling the data for children ages 25 to 60 months for selected pathogens (Table 4). The differences in the isolation rates between case patients and control subjects remained significant for rotavirus, Aeromonas spp., Shigella spp., and V. cholerae O1 and O139 but lost significance for ETEC, EPEC, and ETBF. However, the isolation rates remained insignificant for EAEC and DAEC.
TABLE 4.
Comparison of isolation of selected enteric pathogens from 145 children with diarrhea and 169 controls who were between 25 and 60 months old
| Organism | No. (%) of infected children
|
P value | |
|---|---|---|---|
| Diarrheal | Control | ||
| Rotavirus | 13 (9.0) | 0 (0.0) | 0.0002 |
| C. jejuni | 27 (18.6) | 18 (10.7) | 0.065 |
| ETEC | 20 (13.8) | 12 (7.1) | 0.077 |
| EPEC | 7 (4.8) | 3 (1.8) | 0.196 |
| Aeromonas spp. | 28 (19.3) | 11 (6.5) | 0.001 |
| Shigella spp. | 21 (14.5) | 9 (5.3) | 0.010 |
| V. cholerae O1 | 14 (9.7) | 0 (0.0) | 0.0001 |
| V. cholerae O139 | 19 (13.1) | 0 (0.0) | 0.0001 |
| ETBF | 6 (4.1) | 1 (0.6) | 0.052 |
| EAEC | 5 (3.5) | 3 (1.8) | 0.478 |
| DAEC | 10 (6.9) | 8 (4.7) | 0.563 |
Among ETEC, heat-stable toxin (ST)-only producing strains and both ST- and heat-labile toxin (LT)-producing strains were significantly associated with diarrhea. Among EPEC, strains positive with the EAF probe and the eae probe and those positive with the eae probe but negative with the EAF probe were detected. The former were significantly associated with diarrhea, but the latter were not (Table 5).
TABLE 5.
Types of ETEC and EPEC isolated from children with diarrhea and controls
| Organism | No. (%) of infected children
|
P value | |
|---|---|---|---|
| Diarrheal (n = 814) | Control (n = 814) | ||
| ETEC positive for: | |||
| LT only | 37 (4.6) | 41 (5.0) | 0.64 |
| ST only | 68 (8.4) | 18 (2.2) | 0.0001 |
| LT and ST | 32 (3.9) | 13 (1.6) | 0.004 |
| EPEC positive with: | |||
| eae probe only | 20 (2.5) | 22 (2.7) | 0.75 |
| EAF and eae probes | 79 (9.7) | 22 (2.7) | 0.001 |
Among children with diarrhea, 321 (39.4%) had infections with two or more pathogens, and among control children, 121 (14.9%) had mixed infections (P = 0.0001). The data on infections with single organisms and coinfection with different numbers of pathogens are shown in Table 6. A greater number of children with diarrhea than control children had coinfections with different numbers of pathogens. For pathogens significantly associated with diarrhea, mixed infections involving two or more pathogens were seen in 48 to 74% of the children with diarrhea, but no predominant mixed infections were evident (Table 7).
TABLE 6.
Infection with single and mixed pathogens in children with diarrhea and controls
| No. of infecting pathogens | No. (%) of infected children
|
P value | |
|---|---|---|---|
| Diarrheal (n = 814) | Control (n = 814) | ||
| 1 | 288 (35.6) | 236 (29.0) | 0.007 |
| 2 | 212 (26.2) | 105 (12.9) | 0.0001 |
| 3 | 96 (11.9) | 10 (1.2) | 0.0001 |
| 4 | 9 (1.1) | 1 (0.1) | 0.026 |
| 5 | 4 (0.5) | 5 (0.6) | 1.00 |
TABLE 7.
Occurrence of mixed infections with enteric pathogens significantly associated with diarrhea
| Pathogen | No. of patients positive | No. (%) with mixed infection | No. (%) with mixed infection with:
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rotavirus | C. jejuni | ETEC | EPEC | Aeromonas spp. | Shigella spp. | V. cholerae O1 | V. cholerae O139 | ETBF | C. difficile | C. parvum | |||
| Rotavirus | 165 | 83 (50.3) | NAa | 25 (15.2) | 28 (17.0) | 16 (9.7) | 15 (9.1) | 2 (1.2) | 6 (3.6) | 3 (1.8) | 1 (0.6) | 2 (1.2) | 0 (0.0) |
| C. jejuni | 142 | 96 (67.6) | 25 (17.6) | NA | 27 (19.0) | 20 (14.1) | 19 (13.4) | 12 (8.5) | 7 (4.9) | 4 (2.8) | 4 (2.8) | 1 (0.7) | 4 (2.8) |
| ETEC | 137 | 75 (54.8) | 28 (20.4) | 27 (19.0) | NA | 6 (4.4) | 16 (11.7) | 6 (4.4) | 7 (5.1) | 4 (2.9) | 1 (0.7) | 1 (0.7) | 3 (2.2) |
| EPEC | 99 | 53 (53.5) | 16 (16.2) | 20 (20.2) | 6 (6.1) | NA | 7 (7.1) | 7 (7.1) | 4 (4.0) | 3 (3.0) | 4 (4.0) | 1 (1.0) | 0 (0.0) |
| Aeromonas spp. | 99 | 58 (58.6) | 15 (15.2) | 20 (20.2) | 16 (16.2) | 7 (7.1) | NA | 8 (8.1) | 2 (2.0) | 5 (5.1) | 1 (1.0) | 1 (1.0) | 1 (1.0) |
| Shigella spp. | 75 | 36 (48.0) | 2 (2.7) | 11 (14.7) | 6 (8.0) | 7 (9.3) | 8 (10.7) | NA | 0 (0.0) | 3 (4.0) | 5 (6.7) | 1 (1.3) | 0 (0.0) |
| V. cholerae O1 | 37 | 21 (56.8) | 6 (16.2) | 7 (18.9) | 8 (21.6) | 4 (10.8) | 2 (5.4) | 0 (0.0) | NA | 0 (0.0) | 1 (2.7) | 0 (0.0) | 2 (5.4) |
| V. cholerae O139 | 34 | 21 (61.8) | 3 (8.8) | 4 (11.8) | 4 (11.8) | 3 (8.8) | 4 (11.8) | 3 (8.8) | 0 (0.0) | 0 (0.0) | 2 (5.9) | 0 (0.0) | 1 (2.9) |
| ETBF | 28 | 17 (60.7) | 1 (3.6) | 4 (14.3) | 1 (3.6) | 4 (14.3) | 1 (3.6) | 5 (17.9) | 1 (3.6) | 2 (7.1) | NA | 0 (0.0) | 0 (0.0) |
| C. difficile | 13 | 7 (53.9) | 2 (18.2) | 1 (9.1) | 1 (9.1) | 1 (9.1) | 1 (9.1) | 1 (9.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| C. parvum | 11 | 8 (72.7) | 0 (0.0) | 4 (30.8) | 3 (23.1) | 0 (0.0) | 1 (7.7) | 0 (0.0) | 2 (15.4) | 1 (7.7) | 0 (0.0) | 0 (0.0) | NA |
NA, not applicable.
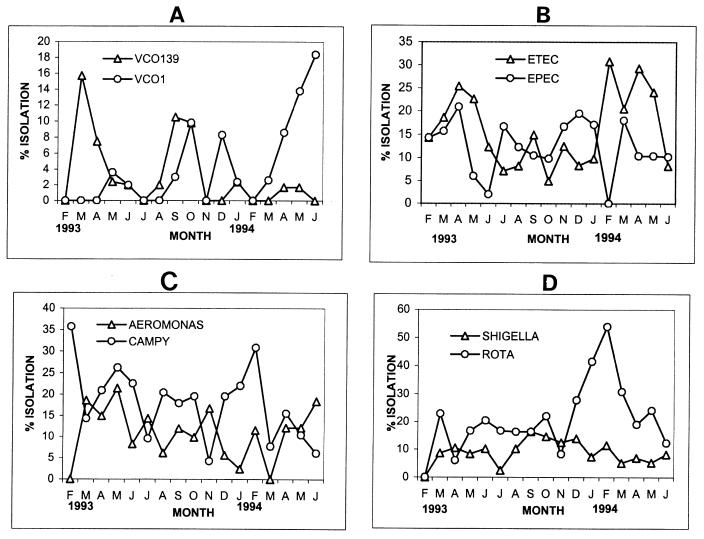
The seasonalities of infection were analyzed for selected enteric pathogens. In Bangladesh, the months from December to February are cooler winter months, the months from March to May are hot, dry, spring months, and the months from June to November are hot, wet, monsoon rain months. Peak V. cholerae O139 infections occurred in March and April 1993 and then in August and October 1994. A high prevalence of infection due to V. cholerae O1 was seen in the months of September, October, and December in 1993 and then from April to June 1994 (Fig. 1A).
FIG. 1.
Monthly isolation rates of V. cholerae O1 (VCO1) and V. cholerae O139 (VCO139) (A), ETEC and EPEC (B), Aeromonas spp. (Aeromonas) and C. jejuni (CAMPY) (C), and Shigella spp. and rotavirus (ROTA) (D).
ETEC infections were present throughout the year, but then peaked from February to May. There did not appear to be a seasonality for EPEC infections (Fig. 1B).
Infections due to C. jejuni and Aeromonas spp. were fairly frequent throughout the year, with no seasonality (Fig. 1C).
Infections with Shigella spp. were prevalent throughout the year, with no particular seasonal pattern. Rotavirus infections peaked in the winter months of December to March (Fig. 1D).
DISCUSSION
In the first surveillance study of diarrheal patients from Dhaka published in 1982, which included both children and adults, eight diarrheal pathogens (Salmonella spp., Shigella spp., V. cholerae O1, C. jejuni, ETEC, rotavirus, E. histolytica, and G. lamblia) were sought, and a recognized pathogen was isolated from 66% of patients (45). In the present study, an additional 12 pathogens (V. cholerae O139, Aeromonas spp., P. shigelloides, C. parvum, C. cayetanensis, C. difficile, EPEC, DAEC, EAEC, EHEC, EIEC, and ETBF) were sought and a potential pathogen was isolated from 74.8% of patients. Many of these additional pathogens were recognized as causative agents of diarrhea relatively recently. Also, the present study differs from the previous study, in that we have included only children up to 5 years of age and community controls, whereas there were no controls in the previous study. Because of the inclusion of controls, it was possible to find an epidemiological association with diarrhea for the pathogens studied. Thus, rotavirus, C. jejuni, ETEC, EPEC, Aeromonas spp., V. cholerae O1 and O139, ETBF, C. difficile, and C. parvum were significantly associated with diarrhea. In a previous study in our center (1), EHEC was detected in only a negligible number of children without diarrhea, and EIEC was not detected in either diarrheal children or control children. Again as in a previous study (1), DAEC and EAEC were not associated with diarrhea in the present study.
There are conflicting reports on the association of EAEC with acute diarrhea (1, 5, 15, 32, 48). However, many reports (5, 13, 17), including our previous study (4), suggested that they are associated with persistent diarrhea. EAEC also causes outbreaks of diarrhea (43) and growth retardation in children (44). There are also conflicting reports on the association of DAEC with diarrhea. Several studies have not found an association with diarrhea (1, 15, 29), while others have found an association with acute and persistent diarrhea (3, 21, 25, 31). It is likely that EAEC and DAEC may represent heterogeneous groups of organisms, and certain subgroups within these categories may be pathogenic.
As reported previously (38, 45), the rates of detection of Salmonella spp., P. shigelloides, E. histolytica, and G. lamblia have been low in the present study. The other pathogens sought in the study were significantly associated with diarrhea, and for most pathogens the major burden of disease occurred in the first year of life. However, age stratification did not show any association with diarrhea for any particular age group for ETBF, although there was an overall association with diarrhea for this organism. Analysis of data for all patients >25 months of age also did not show a significant difference between patients and controls. Further analysis of data for all patients >12 months of age also did not show a significant difference between patients and controls (12 of 338 [3.6%] for patients versus 5 of 403 [1.2%] for controls >12 months of age [P = 0.065]). These data are in contrast to the data from a previous study with the same population (40). In the previous study, among children >12 months of age, ETBF was significantly associated with diarrhea. Moreover, age stratification also showed a significant association between ETBF and diarrhea for different age strata beyond the first year of life. The differences between the two studies may be related to the culture technique and the control populations. In the previous study, in the beginning of the study PINN (polymyxin B, irgasan, nalidixic acid, novobiocin) medium, a more inhibitory medium, was used for isolation of B. fragilis, and in the latter part of the study, BBE, a less inhibitory medium, was used for isolation of B. fragilis. However, in the present study, BBE was used throughout the study. In the previous study, the controls were nondiarrheal children seen at the hospital for other infections. However, in the present study, they were nondiarrheal children from the community.
Also, in our study Aeromonas spp. were significantly associated with diarrhea. However, the role of Aeromonas spp. as significant diarrheal disease agents is controversial. These organisms have been epidemiologically linked to acute diarrhea in some controlled studies (9, 36) but not in others (20, 37). Oral challenge studies with Aeromonas spp. have failed to show significant diarrhea in adult volunteers, even though the challenge strains have been shown to produce numerous potential virulence factors (34). No well-described epidemiologically linked outbreaks of diarrheal disease attributed to Aeromonas spp. have ever been reported. Nevertheless, several case reports support a role for Aeromonas spp. in diarrheal disease. Diarrheal diseases in these individuals were associated with excretion of Aeromonas organisms, with pure or predominant growth of Aeromonas spp. on culture, a serological response to the organisms, and resolution of symptoms and pathology with the disappearance of the organisms from the stool (26).
The causative role of P. shigelloides in diarrheal diseases is not firmly established. A previous case-control study has not shown that it has an association with diarrhea (37), although there are several case reports of diarrhea and several outbreaks of diarrhea linked to P. shigelloides (7). However, the pathogenic mechanism of diarrhea has not been established, and volunteers fed with the organism did not develop diarrhea (22). The low prevalence of P. shigelloides in our study is comparable to that seen in other studies from neighboring countries (12, 16).
C. difficile is the major cause of antibiotic-associated diarrhea and pseudomembranous colitis. Its role in sporadic diarrhea in children is controversial. While some controlled studies have shown an association with diarrhea (30), others have not (11, 41). In the present study, even though it was significantly associated with diarrhea, it was detected in only a small proportion of patients and controls.
As reported previously (1, 45, 47), cholera, ETEC diarrhea, and rotavirus diarrhea had seasonal peaks, with cholera peaking in the hot, dry spring months and again in the hot, wet months of August to October, ETEC diarrhea peaking in the spring months, and rotavirus diarrhea peaking in the winter months. In 1993, in the initial stages of the outbreak of cholera due to V. cholerae O139, V. cholerae O1 was temporarily suppressed, but in 1994 and in subsequent years, it reemerged as the predominant pathogen causing cholera (18). As found previously in our study (1) and studies elsewhere (5, 30, 41), among ETEC, ST only-producing and both ST- and LT-producing strains were associated with diarrhea, and among EPEC, both EAF probe-positive (corresponding to localized adherence) and eae probe-positive (corresponding to the presence of the attachment and effacement gene) strains were associated with diarrhea.
As in past studies (19, 45), another observation from the present study was that infection with multiple pathogens was very common. This is a reflection of environmental contamination, but it makes it difficult to identify which pathogen is the causative agent of diarrhea. It may also be that multiple pathogens act synergistically to produce diarrhea.
Among bacterial pathogens, Yersina spp. were not sought in the present study. However, a previous study found that these pathogens are extremely rare in this population (10). Also, some viral agents of diarrhea were not sought in this study. A previous study has found serological evidence of Norwalk virus infection in up to 80% of children in Bangladesh (6). Also, in previous studies, enteric adenoviruses and astroviruses were detected in a small proportion of children with acute diarrhea in this population (28, 46), although the latter was found in a higher proportion of children with persistent diarrhea (46).
Among the parasitic agents of diarrhea, C. cayetanensis, a newly discovered agent, was not detected in any children. Initial studies indicated that it causes diarrhea mainly in immunocompromised patients and prolonged diarrhea in expatriate populations in certain developing countries including Nepal (42). However, a subsequent study in Nepal suggested that it also causes diarrhea among the indigenous children (23). In a previous study in Bangladesh, it was detected in some patients with prolonged diarrhea (2).
Thus, the present study in Bangladesh found that, like studies conducted in other developing countries, the major pathogens of childhood diarrhea are rotavirus, C. jejuni, ETEC, EPEC, Shigella spp., and V. cholerae. Other similarities include the low prevalence or absence of infections due to Salmonella spp., P. shigelloides, G. lamblia, E. histolytica, EIEC, and EHEC; a lack of association with diarrhea for EAEC and DAEC; a high prevalence of mixed infections; and a high rate of asymptomatic carriage of pathogens by controls (8, 16, 24). However, in contrast to a study in neighboring Nepal, we did not detect C. cayetanensis in our children (23), and contrary to the finding in Thailand, we found an association with diarrhea for Aeromonas spp. (16, 37).
In comparison to the first surveillance study (45), the present study has identified additional pathogens that are significantly associated with diarrhea and has placed them in context with traditional pathogens of diarrhea. This new knowledge on the etiology of diarrhea in the surveillance patients will help us plan studies into various aspects of diarrheal diseases in this population.
ACKNOWLEDGMENTS
This research was funded by the ICDDR,B Centre for Health and Population Research, which is supported by countries and agencies which share its concern for the health problems of developing countries. Current donors that provide unrestricted support include the aid agencies of the governments of Australia, Bangladesh, Belgium, Canada, Saudi Arabia, Sri Lanka, Sweden, Switzerland, the United Kingdom, and the United States; international organizations that provide support include the United Nations Children's Fund (UNICEF).
We thank M. A. Malek for help with the data analysis and Khairun Nessa and Mohammed Atiqullah for secretarial assistance.
REFERENCES
- 1.Albert M J, Faruque S M, Faruque A S G, Neogi P K B, Ansaruzzaman M, Bhuiyan N A, Alam K, Akbar M S. Controlled study of Escherichia coli diarrheal infections in Bangladeshi children. J Clin Microbiol. 1995;33:973–977. doi: 10.1128/jcm.33.4.973-977.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Albert M J, Kabir I, Azim T, Hossain A, Ansaruzzaman M, Unicomb L. Diarrhea associated with Cyclospora sp. in Bangladesh. Diagn Microbiol Infect Dis. 1994;19:47–49. doi: 10.1016/0732-8893(94)90050-7. [DOI] [PubMed] [Google Scholar]
- 3.Baqui A, Sack R B, Black R E, Haider K, Hossain A, Alim A R M A, Yunus M, Chowdhury H R, Siddique A K. Enteropathogens associated with acute and persistent diarrhea in Bangladeshi children <5 years of age. J Infect Dis. 1992;166:792–796. doi: 10.1093/infdis/166.4.792. [DOI] [PubMed] [Google Scholar]
- 4.Bardhan P K, Albert M J, Alam N H, Faruque S M, Neogi P K B, Mahalanabis D. Small bowel and fecal microbiology in children suffering from persistent diarrhea in Bangladesh. J Ped Gastroenterol Nutr. 1998;26:9–15. doi: 10.1097/00005176-199801000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Bhan M K, Raj P, Levine M M, Kaper J B, Bhandari N, Srivastava R, Kumar R, Sazawal S. Enteroaggregative Escherichia coli associated with persistent diarrhea in a cohort of rural children in India. J Infect Dis. 1989;159:1061–1064. doi: 10.1093/infdis/159.6.1061. [DOI] [PubMed] [Google Scholar]
- 6.Black R E, Greenberg H B, Kapikian A Z, Brown K H, Becker S. Acquisition of serum antibody to Norwalk virus and rotavirus and relation to diarrhea in a longitudinal study of young children in rural Bangladesh. J Infect Dis. 1982;145:483–489. doi: 10.1093/infdis/145.4.483. [DOI] [PubMed] [Google Scholar]
- 7.Brenden R A, Miller M A, Janda J M. Clinical disease spectrum and pathogenic factors associated with Plesiomonas shigelloides infections in humans. Rev Infect Dis. 1988;10:303–316. doi: 10.1093/clinids/10.2.303. [DOI] [PubMed] [Google Scholar]
- 8.Brown J E, Echeverria P, Taylor D N, Seriwatana J, Vanapruks V, Lexomboon U, Neill R J, Newland J W. Determination by DNA hybridization of Shiga-like toxin producing Escherichia coli in children with diarrhea in Thailand. J Clin Microbiol. 1989;27:291–294. doi: 10.1128/jcm.27.2.291-294.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burke V, Gracey M, Robinson J, Peck D, Beaman J, Bundell C. The microbiology of childhood gastroenteritis: Aeromonas species and other infective agents. J Infect Dis. 1983;148:68–74. doi: 10.1093/infdis/148.1.68. [DOI] [PubMed] [Google Scholar]
- 10.Carniel E, Butler T, Hossain S, Alam N H, Mazigh D. Infrequent detection of Yersinia enterocolitica in childhood diarrhea in Bangladesh. Am J Trop Med Hyg. 1986;35:370–371. doi: 10.4269/ajtmh.1986.35.370. [DOI] [PubMed] [Google Scholar]
- 11.Cerquetti M, Luzzi I, Caprioli A, Sebastianelli A, Mastrantonio P. Role of Clostridium difficile in childhood diarrhea. Pediatr Infect Dis J. 1995;14:598–603. doi: 10.1097/00006454-199507000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Chatkaeomorakot A, Echeverria P, Taylor D N, Bettelheim K A, Blacklow N R, Sethabutr O, Seriwatana J, Kaper J. HeLa cell-adherent Escherichia coli in children with diarrhea in Thailand. J Infect Dis. 1987;156:669–672. doi: 10.1093/infdis/156.4.669. [DOI] [PubMed] [Google Scholar]
- 13.Cravioto A, Tello A, Navarro A, Ruiz J, Villarfan H, Uribe F, Eslava C. Association of Escherichia coli HEp-2 adherence patterns with type and duration of diarrhea. Lancet. 1991;337:262–264. doi: 10.1016/0140-6736(91)90868-p. [DOI] [PubMed] [Google Scholar]
- 14.Dewan N, Faruque A S G, Fuchs G J. Nutritional status and diarrhoeal pathogen in hospitalized children in Bangladesh. Acta Paediatr. 1998;87:627–630. doi: 10.1080/080352598750014012. [DOI] [PubMed] [Google Scholar]
- 15.Echeverria P, Serichantalerg S, Changchavalit S, Baudry B, Levine M M, Orskov F, Orskov I. Tissue culture adherent Escherichia coli in infantile diarrhea. J Infect Dis. 1992;165:141–143. doi: 10.1093/infdis/165.1.141. [DOI] [PubMed] [Google Scholar]
- 16.Echeverria P, Taylor D N, Lexomboon U, Bhaibulaya M, Blacklow N R, Tamura K, Sakazaki R. Case-control study of endemic diarrheal disease in Thai children. J Infect Dis. 1989;159:543–548. doi: 10.1093/infdis/159.3.543. [DOI] [PubMed] [Google Scholar]
- 17.Fang G D, Lima A A M, Martins C V, Nataro J P, Guerrant R L. Etiology and epidemiology of persistent diarrhea in northeastern Brazil: a hospital-based, prospective, case-control study. J Pediatr Gastroenterol Nutr. 1995;21:137–144. doi: 10.1097/00005176-199508000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Faruque A S G, Fuchs G J, Albert M J. Changing epidemiology of cholera due to Vibrio cholerae O1 and O139 Bengal in Dhaka, Bangladesh. Epidemiol Infect. 1996;116:275–278. doi: 10.1017/s0950268800052572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Faruque A S G, Mahalanabis D, Islam A, Hoque S S. Severity of cholera during concurrent infections with other enteric pathogens. J Diarrheal Dis Res. 1994;12:214–218. [PubMed] [Google Scholar]
- 20.Figura N, Marri L, Verdiani S, Ceccherini C, Barberi A. Prevalence, species differentiation, and toxicity of Aeromonas strains in cases of childhood gastroenteritis and in controls. J Clin Microbiol. 1981;23:595–599. doi: 10.1128/jcm.23.3.595-599.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Giron J A, Jones T, Millan-Velasco F, Castro-Munoz E, Zarate L, Fry J, Frankel G, Moseley S L, Baudry B, Kaper J B, Schoolnik G K, Riley L W. Diffuse-adhering Escherichia coli (DAEC) as a putative cause of diarrhea in Mayan children in Mexico. J Infect Dis. 1991;163:507–513. doi: 10.1093/infdis/163.3.507. [DOI] [PubMed] [Google Scholar]
- 22.Herrington D A, Tzipori S, Robins-Browne R M, Tall B D, Levine M M. In vitro and in vivo pathogenicity of Plesiomonas shigelloides. Infect Immun. 1987;55:979–985. doi: 10.1128/iai.55.4.979-985.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hoge C W, Echeverria P, Rajah R, Jacobs J, Malthouse S, Chapman E, Jimenez L M, Shlim D R. Prevalence of Cyclospora species and other enteric pathogens among children less than 5 years of age in Nepal. J Clin Microbiol. 1995;33:3058–3060. doi: 10.1128/jcm.33.11.3058-3060.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Huilan S, Zhen L G, Mathan M M, Mathew M M, Olarte J, Espejo R, Maung K, Ghafoor M A, Khan M A, Sami Z, Sutton R G. Etiology of acute diarrhoea among children in developing countries: a multicentre study in five countries. Bull W H O. 1991;69:549–555. [PMC free article] [PubMed] [Google Scholar]
- 25.Jallat C, Livrelli V, Darfeuille-Michaud A, Rich C, Joly B. Escherichia coli strains involved in diarrhea in France: high prevalence and heterogeneity of diffusely adhering strains. J Clin Microbiol. 1993;31:2031–2037. doi: 10.1128/jcm.31.8.2031-2037.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Janda J M, Abbott S L. Evolving concepts regarding the genus Aeromonas: an expanding panorama of species, disease presentations, and unanswered questions. Clin Infect Dis. 1998;27:332–344. doi: 10.1086/514652. [DOI] [PubMed] [Google Scholar]
- 27.Janoff E N, Barthreller L. Cryptosporidium species, a protean protozoan. J Clin Microbiol. 1987;25:967–975. doi: 10.1128/jcm.25.6.967-975.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jarecki-Khan J, Tzipori S R, Unicomb L E. Enteric adenovirus infection among infants with diarrhea in rural Bangladesh. J Clin Microbiol. 1993;31:484–489. doi: 10.1128/jcm.31.3.484-489.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kang G, Mathan M M, Mathan V I. Evaluation of a simplified HEp-2 cell adherence assay for Escherichia coli isolated from south Indian children with acute diarrhea and controls. J Clin Microbiol. 1995;33:2204–2205. doi: 10.1128/jcm.33.8.2204-2205.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim K-H, Suh I-S, Kim J M, Kim C W, Cho Y-J. Etiology of childhood diarrhea in Korea. J Clin Microbiol. 1989;27:1192–1196. doi: 10.1128/jcm.27.6.1192-1196.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Levine M M, Ferrechio C, Prado V, Cayazzo M, Abrego P, Martinez J, Maggi L, Baldini M M, Martin W, Maneval D, Kay B, Guers L, Lior H, Wasserman S S, Nataro J P. Epidemiologic studies of Escherichia coli diarrheal infections in a low socioeconomic level peri-urban community in Santiago, Chile. Am J Epidemiol. 1993;138:849–869. doi: 10.1093/oxfordjournals.aje.a116788. [DOI] [PubMed] [Google Scholar]
- 32.Levine M M, Prado V, Robins-Browne R, Lior H, Kaper J B, Moseley S L, Gicquelais K, Nataro J P, Vial P, Tall B. Use of DNA probes and HEp-2 cell adherence assay to detect diarrheagenic Escherichia coli. J Infect Dis. 1988;158:224–228. doi: 10.1093/infdis/158.1.224. [DOI] [PubMed] [Google Scholar]
- 33.Maniar A C, Williams T V, Hammond G W. Detection of Clostridium difficile toxins in various tissue culture monolayers. J Clin Microbiol. 1987;25:1999–2000. doi: 10.1128/jcm.25.10.1999-2000.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Morgan D R, Johnson P C, DuPont H L, Satterwhite T K, Wood L V. Lack of correlation between known virulence properties of Aeromonas hydrophila and enteropathogenicity of humans. Infect Immun. 1985;50:62–65. doi: 10.1128/iai.50.1.62-65.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nataro P, Kaper J B. Diarrhoeagenic Escherichia coli. Clin Microbiol Rev. 1998;11:142–201. doi: 10.1128/cmr.11.1.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pazzaglia G, Sack R B, Salazar E, Yi A, Chea E, Leon-Barua R, Guerrero C E, Palomino J. High frequency of coinfecting enteropathogens in Aeromonas-associated diarrhea of hospitalized Peruvian infants. J Clin Microbiol. 1991;26:1151–1156. doi: 10.1128/jcm.29.6.1151-1156.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pitarangsi C, Echeverria P, Whitmore R, Tirapat C, Formal S, Dammin G J, Tingtalapong M. Enteropathogenicity of Aeromonas hydrophila and Plesiomonas shigelloides: prevalence among individuals with and without diarrhea in Thailand. Infect Immun. 1982;35:666–673. doi: 10.1128/iai.35.2.666-673.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rahim Z, Ali A, Kay A B. Prevalence of Plesiomonas shigelloides among diarrhea patients in Bangladesh. Eur J Epidemiol. 1992;8:753–756. doi: 10.1007/BF00145397. [DOI] [PubMed] [Google Scholar]
- 39.Rahman M, Shahid N S, Rahman H, Sack D A, Rahman N, Hossain S. Cryptosporidiosis: a cause of diarrhea in Bangladesh. Am J Trop Med Hyg. 1990;42:127–130. doi: 10.4269/ajtmh.1990.42.127. [DOI] [PubMed] [Google Scholar]
- 40.Sack R B, Albert M J, Alam K, Neogi P K B, Akbar M S. Isolation of enterotoxigenic Bacteroides fragilis from Bangladeshi children with diarrhea: a controlled study. J Clin Microbiol. 1994;32:960–963. doi: 10.1128/jcm.32.4.960-963.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Santosham M, Sack R B, Reid R, Black R, Croll J, Yolken R, Aurelian L, Wolff M, Chan E, Garrett S, Froehlich J. Diarrheal diseases in the White Mountain Apaches: epidemiologic studies. J Diarrheal Dis Res. 1995;13:18–28. [PubMed] [Google Scholar]
- 42.Shlim D R, Cohen M T, Eaton M, Ramachandran R, Long E G, Ungar B L P. An alga-like organism associated with an outbreak of prolonged diarrhea among foreigners in Nepal. Am J Trop Med Hyg. 1991;45:383–389. doi: 10.4269/ajtmh.1991.45.383. [DOI] [PubMed] [Google Scholar]
- 43.Smith H R, Scotland S M, Willshaw G A, Rowe B, Cravioto A, Eslava C. Isolates of Escherichia coli O44:H18 of diverse origin are enteroaggregative. J Infect Dis. 1994;170:1610–1613. doi: 10.1093/infdis/170.6.1610. [DOI] [PubMed] [Google Scholar]
- 44.Steiner T S, Lima A A M, Nataro J P, Guerrant R L. Enteroaggregative Escherichia coli produce intestinal inflammation and growth impairment and cause interleukin-8 release from intestinal epithelial cells. J Infect Dis. 1998;177:88–96. doi: 10.1086/513809. [DOI] [PubMed] [Google Scholar]
- 45.Stoll B J, Glass R I, Huq M I, Khan M U, Holt J E, Banu H. Surveillance of patients attending a diarrheal disease hospital in Bangladesh. Br Med J. 1982;285:1185–1188. doi: 10.1136/bmj.285.6349.1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Unicomb L, Banu N N, Azim T, Islam A, Bardhan P K, Faruque A S G, Hall A, Moe C L, Noel J S, Monroe S S, Albert M J, Glass R I. Astrovirus infection in association with acute, persistent and nosocomial diarrhea in Bangladesh. Pediatr Infect Dis J. 1998;17:611–614. doi: 10.1097/00006454-199807000-00007. [DOI] [PubMed] [Google Scholar]
- 47.Unicomb L E, Bingnan F, Rahim Z, Banu N N, Golmes J G, Podder G, Munshi M H, Tzipori S R. A one year survey of rotavirus strains from three locations in Bangladesh. Arch Virol. 1993;132:201–208. doi: 10.1007/BF01309854. [DOI] [PubMed] [Google Scholar]
- 48.Vial P A, Robins-Browne R, Lior H, Prado V, Kaper J B, Nataro J P, Maneval D, Elsayed A, Levine M M. Characterization of enteroadherent-aggregative Escherichia coli, a putative agent of diarrheal disease. J Infect Dis. 1988;158:70–79. doi: 10.1093/infdis/158.1.70. [DOI] [PubMed] [Google Scholar]
- 49.World Health Organization. A manual for the treatment of diarrhea. Geneva, Switzerland: World Health Organization; 1990. pp. 6–7. [Google Scholar]