Abstract
Purpose
To present a case of acute anterior uveitis with macular edema associated with sildenafil citrate use in an HLA-B27 positive patient.
Observations
A 54-year-old Caucasian male presented at an ophthalmology tertiary center with complaint of pinkish discoloration, irritation, and photophobia in the left eye (OS). He noted that these symptoms appeared one day after using sildenafil for the first time to treat his erectile dysfunction. The patient had no significant ocular history besides refractive surgery in both eyes (OU) and his medical history was insignificant. Best-corrected visual acuity (BCVA) was 20/20 in the right eye (OD) and 20/25 in OS. Slit-lamp-examination (SLE) demonstrated trace cells and 1+ flare in the anterior chamber (AC) in OS and was nonrevealing in AC in OD. Spectral domain optical coherence tomography (SD-OCT) showed parafoveal subretinal hyperreflective deposits in OU. The patient was diagnosed with acute anterior uveitis (AAU) in the left eye and was placed on topical prednisolone acetate.
At 2-week follow-up, the patient reported that his eye symptoms had improved since starting topical steroids but worsened again two days after he had used sildenafil for a second time. In OS, best-corrected visual acuity (BCVA) worsened to 20/40, and SLE revealed 1+ cells and 1+ flare in AC. SD-OCT revealed cystoid macular edema only in OS. Fluorescein angiography showed mild staining around the optic disc and significant macular leakage in OS and minimal macular leakage in OD. Uveitis evaluations revealed that the patient was human leukocyte antigen-27 (HLA-B27) positive. The patient was asked to remain off sildenafil and continue topical prednisolone acetate. At 3-month follow-up, BCVA improved to 20/20 in OS with no evidence of active inflammation.
Conclusions and importance
Sildenafil citrate use might be associated with new onset of intraocular inflammation in predisposed patients. Further studies are necessary to establish this relationship.
Keywords: Sildenafil citrate, Viagra, HLA B27, Macular edema, Acute anterior uveitis, PDE5 inhibitors
1. Introduction
Sildenafil citrate is a phosphodiesterase-5 (PDE5) inhibitor which was approved by the U.S. Food and Drug Administration (FDA) in 1998 for the treatment of erectile dysfunction (ED).1,2 Due to its vasodilatory and smooth muscle relaxing effects, sildenafil was later approved for the treatment of pulmonary arterial hypertension and benign prostatic hyperplasia.3,4 An additional approved indication of PDE5 inhibitors is lower urinary tract symptoms.4 To date, PDE5 inhibitors are researched as potential therapeutics for other diseases, including diabetes mellitus and chronic kidney disease.5
Sildenafil citrate exhibits its vasodilatory effect by competitively inhibiting PDE5, an enzyme found in smooth muscle.1,3 This inhibition prevents the PDE5 catalyzed degradation of cyclic guanosine monophosphate (cGMP) to 5′-GMP, augmenting the vasodilatory effect of nitric oxide (NO).1,3 Overall, PDE5 inhibition induces smooth-muscle relaxation and increases blood flow to various body tissues such as the corpus cavernosum penis, lungs, urethra, and bladder.1,4 Although generally safe, sildenafil can be associated with ocular side effects, including impaired color discrimination and perception, electroretinography changes, and ischemic optic neuropathy.6,7
The most common form of uveitis is anterior uveitis, which accounts for 90% of uveitis cases in primary care settings and 50–60% of uveitis cases in tertiary centers in Western countries.8 Etiologies of anterior uveitis include herpetic, juvenile idiopathic arthritis (JIA), sarcoidosis, Behçet's, human leucocytic antigen B27 (HLA-B27) related, Fuchs, and others.9 HLA-B27 is the most common genetic marker associated with anterior uveitis, with around 50% of sudden onset unilateral recurrent anterior uveitis patients being HLA-B27 positive.10 It is estimated that 38–88% of anterior uveitis cases are idiopathic.8 Macular edema is present in approximately 13% of HLA-B27 related anterior uveitis.11 HLA-B27 is also associated with ankylosing spondylitis (AS), with around 90% of AS patients being HLA-B27 positive.12,13 About 40% of cases with HLA-B27 positive spondylarthritis develop acute anterior uveitis.14 Approximately 84–90% of patients presenting with AAU who are HLA-B27 positive also have ankylosing spondylitis.8
The index report describes a case of an HLA-B27 positive patient with no previous ocular inflammation history who developed acute unilateral uveitis with macular edema following first-time use of sildenafil citrate. To our knowledge, this is the first report of a possible association between PDE5 inhibition and acute anterior uveitis in an HLA-B27 positive patient.
2. Case report
A 54-year-old Caucasian male presented with complaints of redness, photophobia, and blurred vision in the left eye (OS). He reported taking sildenafil citrate for the first time in his life the night before his ocular symptoms started. He awoke with irritation, redness, and photophobia in the left eye, which progressively worsened throughout the day. The patient had an insignificant ocular history except for LASIK in both eyes (OU) thirteen years prior; he had no history of uveitis in either eye. His medical history was unrevealing.
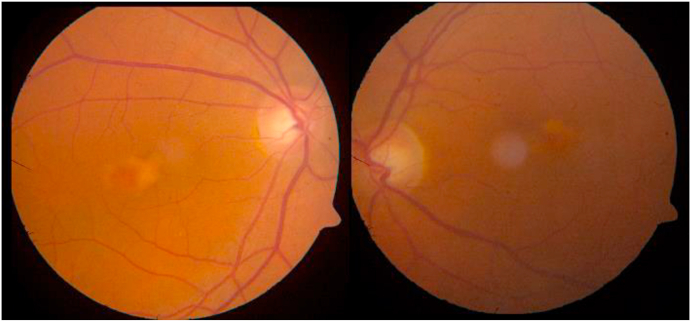
Upon examination, his best corrected visual acuity (BCVA) was 20/20 in the right eye (OD) and 20/25 in OS. IOP was 12 and 10 mmHg in OD and OS, respectively. Mild tenderness in OS was also noted. Slit lamp examination (SLE) was unrevealing in OD but showed signs of iritis in OS, including ciliary injection, few keratic precipitates (KPs), 0.5+ cells, and 1+ flare in the anterior chamber (AC). Dilated fundus examination showed parafoveal yellow-orange subretinal deposits in OU consistent with pattern dystrophy (Fig. 1), while the remaining fundus examination was unrevealing. Spectral domain optical coherence tomography (SD-OCT) confirmed subretinal, parafoveal hyperreflective deposits and no intraretinal or subretinal fluid in OU. The patient was diagnosed with acute anterior uveitis in OS and possible pattern dystrophy in OU. A uveitis workup was ordered, including angiotensin-converting enzyme, lysozyme, syphilis treponemal screening, HLA B27, and chest x-ray. The patient was prescribed hourly prednisolone acetate and cyclopentolate 3 times daily in OS.
Fig. 1.
Color fundus photos (CFP) of left and right eyes showing parafoveal yellow-orange subretinal deposits. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
At 10-day follow up, the patient reported that his symptoms had improved for 1 week but worsened 1 day following repeated sildenafil use. On examination, BCVA was 20/20 in OD and 20/40 in OS, and IOP was 13 and 15 mmHg in OD and OS, respectively. Chest x-ray was non-revealing and laboratory evaluations were within normal limits except for HLA-B27 positivity. SLE was normal in OD and revealed active iritis in OS with 1+ ciliary injection, KPs, 1+ AC cells, and 1+ AC flare. The patient was instructed to continue the eye drops and to not use sildenafil again.
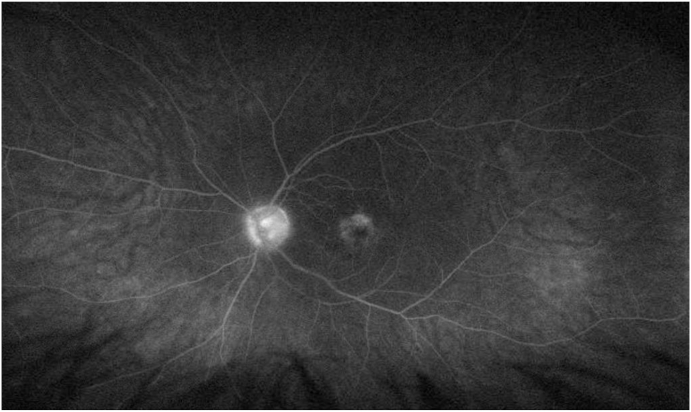
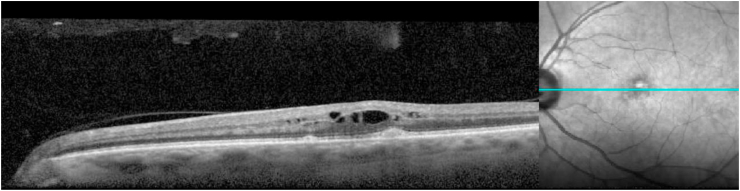
At 1-month follow-up, BCVA decreased in OS to 20/70. SLE showed signs of improvement in OS with quiet conjunctiva, clear cornea, no AC cells, and 0.5+ AC flare. Fluorescein angiography (FA) showed mild and moderate macular leakage in OD and OS, respectively (Fig. 2). SD-OCT showed center involving macular edema in OS, while the subretinal deposits remained unchanged in OU (Fig. 3). The patient was recommended to remain off sildenafil citrate, start ketorolac tromethamine 4 times daily, and taper prednisolone acetate eyedrops in OS. Given the history of occasional back pain and early morning stiffness, the patient had a sacroiliac joint x-ray to screen for ankylosing spondylitis, which was negative, demonstrating that the patient had no HLA-B27 associated ocular or systemic diseases.
Fig. 2.
Late phase fluorescein angiography (FA) of the left eye at 1-month follow up showing moderate peri-foveal and mild optic disc leakage.
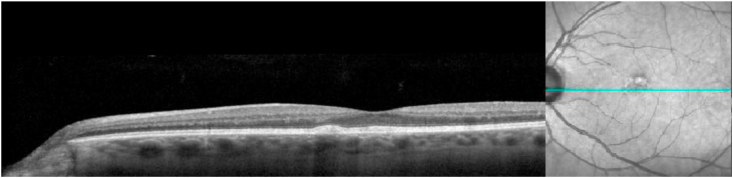
Fig. 3.
Optical coherence tomography (OCT) of the left eye showing sub-RPE parafoveal deposits and intraretinal edema.
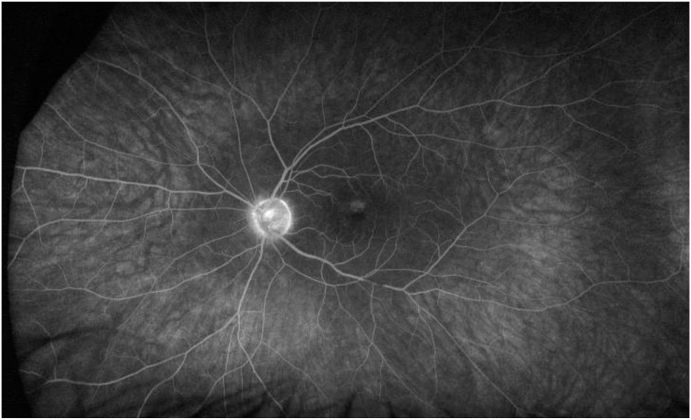
At the 3-month follow-up, BCVA was 20/20 in OS. IOP was 15 mmHg and 20 mmHg in OD and OS, respectively. SLE showed no AC cells and 0.5+ AC flare OS. FA revealed mild macular leakage, which had improved compared with the previous visit in OS (Fig. 4). SD-OCT showed resolution of intraretinal fluid in OS (Fig. 5).
Fig. 4.
Late phase fluorescein angiography (FA) of the left eye at 3-month follow up showing much reduced macular/peri-foveal and optic disc leakage.
Fig. 5.
Optical coherence tomography of the left eye showing resolution of intraretinal edema.
3. Discussion
We have presented a case of a 54-year-old male who had first-time attacks of AAU and development of macular edema following sildenafil citrate use. The differential diagnosis for this age group is broad and includes infectious, autoimmune, cancer-related (least likely), medication-induced, and idiopathic etiologies. Given the patient's age and presentation, syphilis, sarcoidosis, tuberculosis, and HLA-B27 were considered as possible causes of AAU. Syphilis and tuberculosis were excluded by negative syphilis treponemal screening and QuantiFERON tests, respectively. Sarcoidosis was ruled out with normal levels of angiotensin-converting enzyme and lysozyme blood levels. Chest x-ray was normal, which added further evidence against sarcoidosis and tuberculosis. There were no clinical signs of Adamantiades-Behcet's disease or diabetic retinopathy. The only positive test was HLA-B27. Based on this clinical scenario, we propose that the index patient was an already predisposed patient for AAU, but his first-time episodes were only precipitated after sildenafil use.
Sildenafil has been associated with mild ocular side-effects such as small changes in electroretinography readings, color discrimination, and brightness perception.6,7 Visual impairments induced by sildenafil are suspected to result from sildenafil's mild inhibition of phosphodiesterase-6 (PDE6), which is present in photoreceptor cells.15 In several reports, sildenafil has been linked with more serious ocular pathologies such as anterior ischemic optic neuropathy.6,16 In a case reported by Ilhan et al.,17 sildenafil was reported to induce vitreous hemorrhage, hyphema, and macular edema development in a patient with proliferative diabetic retinopathy. Quiram et al.18 reported two cases of serous macular detachments associated with sildenafil use. The FDA announced in July 2005 that men should discontinue PDE5 inhibitors and seek medical care if they experience vision loss.1
Several studies have indicated that PDE5 inhibitors such as sildenafil increase choroidal blood flow (CBF) while having a lesser effect on retinal vasculature.19 Due to vascular similarities between the corpus cavernosum and choroid, this increase in CBF may be attributed to the sildenafil-induced relaxation of choroidal vessel smooth muscle walls.19 Other reports, however, show that sildenafil does not significantly increase choroidal blood flow. Berrones et al.20 used optical coherence tomography-angiography (OCT-A) to monitor ocular vascular changes and reported a significant increase in central choroidal thickness (CCT) and no change in choroidal blood flow in healthy patients one-hour following administration of 50 mg oral sildenafil compared to controls. They also reported a significant increase in outer retina blood flow and no change in retinal capillary density after sildenafil administration.20 Considering the effects of PDE5 inhibitors on ocular blood flow, an increase in CBF after sildenafil administration may have contributed to the development of macular edema in our presented case. Such mechanism, however, is inconclusive and the literature does not consistently show that sildenafil increases CBF.
Different studies have shown an association between ocular inflammation and choroidal thickness. In a study by Gabriel et al.,21 the authors used SD-OCT and OCT-A to demonstrate that during the acute phases of AU, there is increase in choroidal thickness which goes away after the inflammation stops. This increase in thickness can be attributed to an increase in blood flow through the choroid during inflammation.21 Macular edema has also been associated with increase in ocular blood flow in different ocular pathologies. Okamoto et al.22 demonstrated that in patients with macular edema secondary to branch retinal vein occlusion, there is a significant increase in CBF in the affected eye compared to the fellow eye. These patients had a significant reduction in CBF 1-week following intravitreal injection of ranibizumab into affected eye.22 At 1-month and 2-month follow ups, however, there was no significant difference in choroidal blood flow compared to baseline.22 Endo et al. reported that CCT was significantly thickened in patients with diabetic macular edema (DME) as compared to diabetic patients without DME.23
In our case, we propose that sildenafil has precipitated the described first attack of typical acute anterior uveitis in an HLA-B27 positive patient, with no other apparent predisposing factor. The patient had never experienced such an attack before using sildenafil for the first time and the second use of sildenafil was associated with a relapse in inflammation. When sildenafil was stopped, the intraocular inflammation never recurred. According to the Naranjo scale assessing a drug's causality towards inducing an adverse event (AE), sildenafil in this case was rated 4, indicating a “possible” likelihood of the drug causing the adverse reactions described in this case.24 The presumed pattern dystrophy is likely coincidental and did not have any role in the pathogenesis of the inflammatory process.
Işık et al.25 reported recurrent attacks of unilateral posterior uveitis in a patient with Behçet's disease who used sildenafil. The patient had never experienced any ocular inflammation during the first 12 years after being diagnosed with Behçet's. After the patient started using sildenafil, the patient experienced six recurrent attacks of posterior uveitis. The authors did not report any details about the nature of the posterior uveitis, nor gave an account on the follow up of the patient after he stopped using sildenafil.25 Our case is very similar to their report in that first time use of sildenafil has been associated with first time incidence of ocular inflammation in a predisposed patient.
Drug-induced uveitis can occur via two distinct processes: the direct and the indirect mechanisms.26 The direct mechanism involves direct interaction of the drug with intraocular tissues leading to inflammation. The indirect mechanisms include immune cell induction and rupturing of microvasculature, resulting in disruption of the blood ocular barrier.26 Several drugs including MEK inhibitors and tumor necrosis factor-α inhibitors have been implicated in the induction of uveitis.27 Other drugs reported to induce uveitis include metipranolol, sulfonamides, bisphosphonates, cidofovir, triamcinolone acetonide.28
The exact mechanism of sildenafil-induced intraocular inflammation is not clear. Interestingly, sildenafil has been associated with decreased tissue inflammation in both humans and animal models.29 Both the anti-inflammatory property of sildenafil and the extreme rarity of the associated uveitis make it unlikely that ocular inflammation is a result of direct sildenafil-tissue interaction and more of an idiosyncratic property. Another proposed mechanism is that sildenafil has increased the ocular blood flow, which might have accentuated an already present subclinical intraocular inflammation. Such a hypothesis is supported by the fact that sildenafil has only been associated with intraocular inflammation in predisposed patients such as Behçet's and HLA-B27 positive patients.
In our case, FA showed macular leakage OU but OCT only demonstrated macular edema in the left eye. Macular leakage in the right eye without macular edema can be explained by the presence of subclinical inflammation, of which macular leakage was the only indicator. Although uncommon, bilateral simultaneous HLA-B27 related AAU has been reported.30 We also suggest that the possible increase in choroidal blood flow may have contributed to the bilateral macular leakage, which was more accentuated in the left eye due to the active inflammation.
4. Conclusion
Sildenafil citrate use might be associated with new-onset of intraocular inflammation in predisposed patients with HLA-B27 positivity. Further case studies are necessary to establish this relationship.
Patient consent
Written consent from the patient to publish this report was obtained.
Funding
No funding or grant support.
Authorship
All authors attest that they meet the current ICMJE criteria for authorship.
Disclosures
The following authors have no financial disclosures: JR, HG, AA, WM, AM, IK, MZ, BP, QDN.
Declaration of competing interest
We wish to confirm that there are no known conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome.
Acknowledgements
None.
References
- 1.Huang S.A., Lie J.D. Phosphodiesterase-5 (PDE5) inhibitors in the management of erectile dysfunction. P T. Jul 2013;38(7):407–419. [PMC free article] [PubMed] [Google Scholar]
- 2.Goldstein I., Burnett A.L., Rosen R.C., Park P.W., Stecher V.J. The serendipitous story of sildenafil: an unexpected oral therapy for erectile dysfunction. Sex Med Rev. Jan 2019;7(1):115–128. doi: 10.1016/j.sxmr.2018.06.005. [DOI] [PubMed] [Google Scholar]
- 3.Bhogal S., Khraisha O., Al Madani M., Treece J., Baumrucker S.J., Paul T.K. Sildenafil for pulmonary arterial hypertension. Am J Therapeut. Jul/Aug 2019;26(4):e520–e526. doi: 10.1097/MJT.0000000000000766. [DOI] [PubMed] [Google Scholar]
- 4.Andersson K.E. PDE5 inhibitors - pharmacology and clinical applications 20 years after sildenafil discovery. Br J Pharmacol. Jul 2018;175(13):2554–2565. doi: 10.1111/bph.14205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tzoumas N., Farrah T.E., Dhaun N., Webb D.J. Established and emerging therapeutic uses of PDE type 5 inhibitors in cardiovascular disease. Br J Pharmacol. Dec 2020;177(24):5467–5488. doi: 10.1111/bph.14920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Laties A., Zrenner E. Viagra (sildenafil citrate) and ophthalmology. Prog Retin Eye Res. Sep 2002;21(5):485–506. doi: 10.1016/s1350-9462(02)00013-7. [DOI] [PubMed] [Google Scholar]
- 7.Azzouni F., Abu samra K. Are phosphodiesterase type 5 inhibitors associated with vision-threatening adverse events? A critical analysis and review of the literature. J Sex Med. Oct 2011;8(10):2894–2903. doi: 10.1111/j.1743-6109.2011.02382.x. [DOI] [PubMed] [Google Scholar]
- 8.Tsirouki T., Dastiridou A., Symeonidis C. A focus on the epidemiology of uveitis. Ocul Immunol Inflamm. 2018;26(1):2–16. doi: 10.1080/09273948.2016.1196713. [DOI] [PubMed] [Google Scholar]
- 9.Harthan J.S., Opitz D.L., Fromstein S.R., Morettin C.E. Diagnosis and treatment of anterior uveitis: optometric management. Clin Optom. 2016;8:23–35. doi: 10.2147/OPTO.S72079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martin T.M., Rosenbaum J.T. An update on the genetics of HLA B27-associated acute anterior uveitis. Ocul Immunol Inflamm. Apr 2011;19(2):108–114. doi: 10.3109/09273948.2011.559302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Uy H.S., Christen W.G., Foster C.S. HLA-B27-associated uveitis and cystoid macular edema. Ocul Immunol Inflamm. Sep 2001;9(3):177–183. doi: 10.1076/ocii.9.3.177.3963. [DOI] [PubMed] [Google Scholar]
- 12.Sheehan N.J. The ramifications of HLA-B27. J R Soc Med. Jan 2004;97(1):10–14. doi: 10.1258/jrsm.97.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dean L.E., Jones G.T., MacDonald A.G., Downham C., Sturrock R.D., Macfarlane G.J. Global prevalence of ankylosing spondylitis. Rheumatology. Apr 2014;53(4):650–657. doi: 10.1093/rheumatology/ket387. [DOI] [PubMed] [Google Scholar]
- 14.Rademacher J., Poddubnyy D., Pleyer U. Uveitis in spondyloarthritis. Ther Adv Musculoskelet Dis. 2020;12 doi: 10.1177/1759720X20951733. 1759720X20951733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kinoshita J., Iwata N., Shimoda H., Kimotsuki T., Yasuda M. Sildenafil-induced reversible impairment of rod and cone phototransduction in monkeys. Invest Ophthalmol Vis Sci. Jan 8 2015;56(1):664–673. doi: 10.1167/iovs.14-15985. [DOI] [PubMed] [Google Scholar]
- 16.Santaella R.M., Fraunfelder F.W. Ocular adverse effects associated with systemic medications : recognition and management. Drugs. 2007;67(1):75–93. doi: 10.2165/00003495-200767010-00006. [DOI] [PubMed] [Google Scholar]
- 17.Ilhan C., Uzel M.M., Citirik M. Intraocular hemorrhage due to use of sildenafil in a patient with diabetes. Med Hypothesis Discov Innov Ophthalmol. Fall. 2018;7(3):122–125. [PMC free article] [PubMed] [Google Scholar]
- 18.Quiram P., Dumars S., Parwar B., Sarraf D. Viagra-associated serous macular detachment. Graefes Arch Clin Exp Ophthalmol. Apr 2005;243(4):339–344. doi: 10.1007/s00417-004-1099-0. [DOI] [PubMed] [Google Scholar]
- 19.da Cruz N.F.S., Polizelli M.U., Cezar L.M. Effects of phosphodiesterase type 5 inhibitors on choroid and ocular vasculature: a literature review. Int J Retina Vitreous. 2020;6:38. doi: 10.1186/s40942-020-00241-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Berrones D., Salcedo-Villanueva G., Morales-Canton V., Velez-Montoya R. Changes in retinal and choroidal vascular blood flow after oral sildenafil: an optical coherence tomography angiography study. J Ophthalmol. 2017:7174540. doi: 10.1155/2017/7174540. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gabriel M., Kruger R., Shams-Mafi F. Mapping retinal and choroidal thickness in unilateral nongranulomatous acute anterior uveitis using three-dimensional 1060-nm optical coherence tomography. Invest Ophthalmol Vis Sci. Sep 1 2017;58(11):4778–4783. doi: 10.1167/iovs.17-22265. [DOI] [PubMed] [Google Scholar]
- 22.Okamoto M., Yamashita M., Sakamoto T., Ogata N. Choroidal blood flow and thickness as predictors for response to anti-vascular endothelial growth factor therapy in macular edema secondary to branch retinal vein occlusion. Retina. Mar 2018;38(3):550–558. doi: 10.1097/IAE.0000000000001566. [DOI] [PubMed] [Google Scholar]
- 23.Endo H., Kase S., Takahashi M. Relationship between diabetic macular edema and choroidal layer thickness. PLoS One. 2020;15(1) doi: 10.1371/journal.pone.0226630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Naranjo C.A., Busto U., Sellers E.M. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. Aug 1981;30(2):239–245. doi: 10.1038/clpt.1981.154. [DOI] [PubMed] [Google Scholar]
- 25.Isik M., Kilic L., Dogan I. Recurrent uveitis due to sildenafil usage in a patient with Behcet's disease. Rheumatol Int. Mar 2013;33(3):803. doi: 10.1007/s00296-011-2246-7. [DOI] [PubMed] [Google Scholar]
- 26.Agarwal M., Dutta Majumder P., Babu K. Drug-induced uveitis: a review. Indian J Ophthalmol. Sep 2020;68(9):1799–1807. doi: 10.4103/ijo.IJO_816_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moorthy R.S., Moorthy M.S., Cunningham E.T., Jr. Drug-induced uveitis. Curr Opin Ophthalmol. Nov 2018;29(6):588–603. doi: 10.1097/ICU.0000000000000530. [DOI] [PubMed] [Google Scholar]
- 28.London N.J., Garg S.J., Moorthy R.S., Cunningham E.T. Drug-induced uveitis. J Ophthalmic Inflamm Infect. Mar 25 2013;3(1):43. doi: 10.1186/1869-5760-3-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kniotek M., Boguska A. Sildenafil can affect innate and adaptive immune system in both experimental animals and patients. J Immunol Res. 2017;2017:4541958. doi: 10.1155/2017/4541958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Inanc M., Simsek M., Cakar Ozdal M.P. Etiological and clinical characteristics of HLA-B27-associated uveitis in a tertiary referral center. Turk J Ophthalmol. Feb 28 2019;49(1):10–14. doi: 10.4274/tjo.galenos.2018.53896. [DOI] [PMC free article] [PubMed] [Google Scholar]