Abstract
Hip resection arthroplasty is a useful procedure for the management of complex hip problems and in patients with high surgical and anesthetic risk factors. Unilateral procedures performed for failed total hip arthroplasty have been shown to be successful for pain relief with acceptable functional outcomes; however, to our knowledge, no research exists on simultaneous bilateral hip resection arthroplasty for femoral head osteonecrosis. We present two cases of single-stage bilateral hip resection arthroplasty performed under singular anesthetic procedures for femoral head osteonecrosis. The patients were each able to stand for transfers postoperatively and had no deterioration in pain or function. These two cases demonstrate that satisfactory pain control with preservation of function may be achievable with bilateral hip resection arthroplasty procedures in patients who are not a candidate for more advanced reconstructive procedures.
Keywords: Bilateral hip resection arthroplasty, Girdlestone procedure, Femoral head osteonecrosis, Hip avascular necrosis
Introduction
Hip resection arthroplasty (HRA) has existed for over a century and was first described by Gathorne Girdlestone in the 1920s for management of chronic tuberculosis infection of the hip [1]. Today, HRA is commonly performed as a salvage procedure, especially for failed total hip arthroplasty (THA) cases that are unfit for revision [2,3]. However, some surgeons consider the procedure to be more than a salvage option and indicated for hip problems in patients with high surgical risk factors [4,5]. There have been many studies looking at unilateral HRA after an infected hip prosthetic joint infection, reporting overall success with significant pain relief and good functional outcome [3,[5], [6], [7], [8], [9]]. There are only a few published studies looking at bilateral HRA, but these studies did not specify whether the bilateral procedures were performed simultaneously or if they were limited to salvage, as opposed to primary situations [[10], [11], [12]]. To our knowledge, there has been no published literature describing bilateral HRA performed simultaneously in a single anesthetic event. We present two cases of different patients undergoing simultaneous bilateral HRA for femoral head osteonecrosis. Local institutional review board reviewed and approved this current case series. Both patients gave their informed consent to be included in this study.
Case histories
Case 1
A 57-year-old male presented for evaluation and management of bilateral femoral head osteonecrosis. The patient reported severe hip pain and was wheelchair-dependent, only able to bear weight on his legs to transfer with two-person assist. He was on chronic hydromorphone, morphine, pregabalin, and cannabinoids for pain control. He had been on prednisone for approximately 10 years for an undifferentiated connective tissue disorder, which caused nodular swelling and superficial blisters. He had numerous hospitalizations for renal failure and chronic wound methicillin-resistant Staphylococcus aureus infection in his lower extremities with a history of hospitalization for bacteremia and sepsis three times in the previous year. Anteroposterior (AP) pelvis demonstrated flattening of bilateral femoral heads (Fig. 1), with confirmation of aseptic necrosis on magnetic resonance imaging (MRI) (Fig. 2). Both hips were considered high grade in the Kerboul classification because of the combined necrotic angle over 200 degrees on the AP and lateral radiographs. Given the patient’s complex medical condition, low functional demand, and significant risk factors for arthroplasty surgery and anesthesia, the patient elected to undergo HRA for pain relief. The patient consented for a simultaneous procedure because of the benefit of needing only one surgery, hospitalization, and rehabilitation period.
Figure 1.
Preoperative radiograph of the AP pelvis demonstrates bilateral femoral head deformity with flattening and subchondral sclerosis. There are severe degenerative changes including narrowed joint space and acetabular sclerosis and subchondral cysts.
Figure 2.
Preoperative T2 coronal (a), T1 coronal (b), and T1 axial (c) MRI scans demonstrating signal changes at the weight-bearing portions of the femoral heads consistent with necrotic tissues. T2 MRI showed high signal intensity consistent with edema around the area of necrotic tissues.
Given that this case was a primary surgery with no previous hip procedures, a modified Smith-Peterson anterior supine intermuscular approach was selected for each hip to allow for simple supine positioning, simultaneous draping of both surgical sites, and allow for use of fluoroscopy for accurate bone cuts. A low femoral neck cut was performed along the intertrochanteric line (Fig. 3) to prevent calcar impingement on the lateral acetabular sourcil. The position of the osteotome was verified under fluoroscopy before making the final cut with a sagittal saw. Once the head and neck were removed (Fig. 4), the posterior capsule was excised off the proximal femur and approximated to the anterior capsule to cover the acetabulum, preventing migration of the proximal femur into the acetabulum. The surgical wound was then closed in layers. Postoperatively, the patient was recommended to weight-bear as tolerated on bilateral lower extremities for transfer only; otherwise, he was to remain non-weightbearing for 6 weeks. He reported immediate improvement in groin pain after surgery and was satisfied with the early surgical outcome. He was able to put full weight on both legs with a front-wheeled walker to transfer on postoperative day one. Before discharge, the patient was able to transfer with minimal hip pain and manage his own toileting and basic hygiene. His postoperative films are shown in Figure 5 at 3 weeks. At his 1-year follow-up, the patient was able to ambulate 30 feet, and he stated his goals from the procedure had been met and exceeded. His Western Ontario and McMaster Universities Arthritis Index (WOMAC) score was 74 on 2-year follow-up.
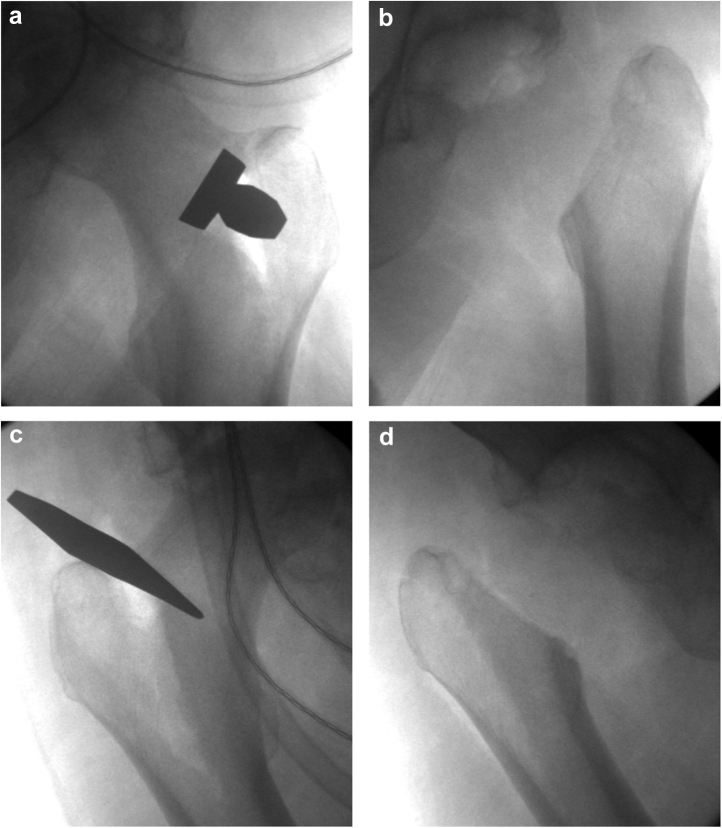
Figure 3.
Intraoperative fluoro of bilateral hips before (a, c) and after (b, d) femoral neck cuts. The “a” and “c” also show the location and orientation of the osteotome to be low on the neck and parallel to the intertrochanteric line.
Figure 4.
Intraoperative clinical photos of right (a) and left (b) femoral heads and necks showing delamination of the cartilage with exposed, collapsed subchondral bone.
Figure 5.
Postoperative, non-weight-bearing AP pelvis radiograph showing superior migration of bilateral femurs without direct contact to the acetabula.
Case 2
A 67-year-old female presented with bilateral hip pain due to femoral head osteonecrosis. Her medical history was significant for chronic obstructive pulmonary disease, hepatitis C, drug abuse, depression, anxiety, homelessness, and obesity. The right side was related to treatment from acute hip joint septic arthritis treated 8 months previously. The left side was related to a posttraumatic setting, 4-year status after cephalomedullary nailing for an intertrochanteric femur fracture with screw cutout. Both acetabula were noted to have destructive changes along with the bilateral femoral head avascular necrosis. She was predominantly bedbound, and she had turned to elicit narcotics for pain control. AP pelvis radiographs demonstrated bilateral femoral head avascular necrosis with the presence of antibiotic beads and a cephalomedullary nail in the right and left hips, respectively (Fig. 6). Both hips were also considered high grade based on the Kerboul classification.
Figure 6.
AP pelvis of case 2 demonstrating destructive, end-stage, bilateral femoral avascular necrosis with complete collapse, destructive erosive changes of the dome of both acetabulum with significant superior and lateral migration of the femoral heads. Antibiotic beads are present in the right hip along with a short cephalomedullary nail in the left hip.
For this particular case, a posterior approach for the right hip was performed to use the patient’s previous surgical scar for better preservation of muscular anatomy. This also allowed for removal of the posteriorly placed antibiotic beads and the ability to extend the incision to a Kocher-Langenbeck approach given the high hip center on the ilium with posteriorly subluxed hip joint. Antibiotic beads were removed, and the femoral neck was cut with a sagittal saw. The patient was then transferred to the opposite side and reprepped. The left hip was then performed in a similar fashion to the right side with another posterior approach to allow for utilization of previous scars, access to the ilium and posteriorly subluxed head with a Kocher-Langenbeck approach, and to provide ease of hardware extraction. The prior hardware was removed without complication. The patient was made non-weightbearing on bilateral lower extremities except for transfers. At 1-week and 4-week follow-up visits, the patient noted improvement in bilateral hip pain and spasm, without any notable wound issues. Postoperative radiographs are depicted in Figure 7. The patient’s next follow-up was at 9 months after several missed appointments, and she was able to ambulate two steps with a walker, no worsening pain or spasms and well-healed incisions. The patient’s WOMAC score was 63 on 18-month follow-up, with no deterioration in function from prior evaluation.
Figure 7.
Postoperative non-weight-bearing AP pelvis of case 2 after bilateral Girdlestone procedure, demonstrating superior femoral migration without direct bony contact to the acetabulum.
Discussion
Osteonecrosis of the femoral head may lead to progressive deformity of the femoral head and destruction of the hip joint [13]. The pathogenesis of osteonecrosis is not fully understood; however, multiple comorbid risk factors have been found to be associated with osteonecrosis [14,15]. Diagnosis and classification are based on radiographs and MRI, with MRI being the most sensitive and specific [16]. Treatment is based on age and imaging findings. Early onset osteonecrosis with no head collapse may be treated with pharmacologic agents such as enoxaparin or alendronate [[17], [18], [19]]. Surgical treatment may be categorized into head-preserving procedures or arthroplasty. Head-preserving procedures such as core decompression and vascularized bone grafting may be considered in precollapse phases or young patients with early-stage osteonecrosis [14]. For patients younger than 60 years with subchondral collapse but no flattening of the femoral head, resurfacing arthroplasty may be considered to preserve bone stock [20]. In older patients with collapsed femoral heads and advanced degeneration, THA has been shown to be a reliable option with satisfactory outcomes [[21], [22], [23], [24], [25]]. Although indications are rare, HRA is also a viable option for femoral head osteonecrosis, especially in patients with high surgical and anesthetic risk factors [6,9,[26], [27], [28]].
Before HRA, the patients in this case series had difficulty with transferring, sitting, and performing hygiene due to severe hip pain. Our primary goal was to alleviate pain, and the secondary goal was to maintain or improve function. Although previous studies have demonstrated poor functional outcomes in patients who underwent HRA [10,12,29], especially bilateral procedures [10,12], a more recent review by Lee et al. [30] showed good functional outcomes. In that review, the author found that 89% of 711 hips had much less pain or were pain-free postoperatively, and 90% maintained walking ability when HRA was performed for a variety of hip problems. The majority of literature surrounding Girdlestone procedures involves a history of failed primary THA. A case report of a staged bilateral HRA for a patient with osteopetrosis and no primary joint arthroplasty was recently published, and the patient was found to have improved functional outcomes, range of motion, and basic hygiene [31]. Similarly, for our two patients without a history of primary joint arthroplasty, we were able to successfully obtain pain relief while maintaining their ability to transfer, sit, and perform personal hygiene. Longer follow-up is required to determine if functional ability will continue to improve over time.
Summary
This case series demonstrates that simultaneous bilateral primary HRA may be a viable management option for femoral head osteonecrosis in functionally low-demand patients with high surgical and anesthetic risk. Adequate pain relief can be achieved safely in these rare patient presentations, although further investigation is needed on functional outcomes. In addition, total cost of care should be evaluated in future studies comparing resection arthroplasty vs total joint arthroplasty and management of its expected complications vs no surgery and the expected sequelae seen with immobility.
Informed patient consent
The authors declare that informed patient consent was taken from all the patients.
Footnotes
No author associated with this paper has disclosed any potential or pertinent conflicts which may be perceived to have impending conflict with this work. For full disclosure statements refer to https://doi.org/10.1016/j.artd.2021.09.008.
Declaration of interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this article.
Supplementary data
References
- 1.GR G. Operative treatment in tuberculosis of the larger joints. Br Med J. 1929;2(3585):529. doi: 10.1136/bmj.2.3585.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Laat E.A., van der List J.J., van Horn J.R., Slooff T.J. Girdlestone's pseudarthrosis after removal of a total hip prosthesis; a retrospective study of 40 patients. Acta Orthop Belg. 1991;57(2):109. [PubMed] [Google Scholar]
- 3.Lee J.M. The current concepts of total hip arthroplasty. Hip Pelvis. 2016;28(4):191. doi: 10.5371/hp.2016.28.4.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Parr P.L., Croft C., Enneking W.F. Resection of the head and neck of the femur with and without angulation osteotomy. A follow-up study of thirty-eight patients. J Bone Joint Surg Am. 1971;53(5):935. [PubMed] [Google Scholar]
- 5.Gołda W., Pawelec A., Walczak J. Clinical results evaluation of the Girdlestone's procedure after hip arthrography. Ortop Traumatol Rehabil. 2001;3(1):68. [PubMed] [Google Scholar]
- 6.Sharma H., De Leeuw J., Rowley D.I. Girdlestone resection arthroplasty following failed surgical procedures. Int Orthop. 2005;29(2):92. doi: 10.1007/s00264-004-0633-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sharma H., Kakar R. Outcome of Girdlestone's resection arthroplasty following complications of proximal femoral fractures. Acta Orthop Belg. 2006;72(5):555. [PubMed] [Google Scholar]
- 8.Castellanos J., Flores X., Llusà M., Chiriboga C., Navarro A. The Girdlestone pseudarthrosis in the treatment of infected hip replacements. Int Orthop. 1998;22(3):178. doi: 10.1007/s002640050236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Basu I., Howes M., Jowett C., Levack B. Girdlestones excision arthroplasty: current update. Int J Surg. 2011;9(4):310. doi: 10.1016/j.ijsu.2011.01.012. [DOI] [PubMed] [Google Scholar]
- 10.Haw C.S., Gray D.H. Excision arthroplasty of the hip. J Bone Joint Surg Br. 1976;58(1):44. doi: 10.1302/0301-620X.58B1.1270495. [DOI] [PubMed] [Google Scholar]
- 11.Schröder J., Saris D., Besselaar P.P., Marti R.K. Comparison of the results of the Girdlestone pseudarthrosis with reimplantation of a total hip replacement. Int Orthop. 1998;22(4):215. doi: 10.1007/s002640050245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Müller R.T., Schlegel K.F., Konermann H. Long-term results of the Girdlestone hip. Arch Orthop Trauma Surg. 1989;108(6):359. doi: 10.1007/BF00932446. [DOI] [PubMed] [Google Scholar]
- 13.Ha Y.C., Jung W.H., Kim J.R., Seong N.H., Kim S.Y., Koo K.H. Prediction of collapse in femoral head osteonecrosis: a modified Kerboul method with use of magnetic resonance images. J Bone Joint Surg Am. 2006;88(Suppl 3):35. doi: 10.2106/JBJS.F.00535. [DOI] [PubMed] [Google Scholar]
- 14.Zalavras C.G., Lieberman J.R. Osteonecrosis of the femoral head: evaluation and treatment. J Am Acad Orthop Surg. 2014;22(7):455. doi: 10.5435/JAAOS-22-07-455. [DOI] [PubMed] [Google Scholar]
- 15.Heimann W.G., Freiberger R.H. Avascular necrosis of the femoral and humeral heads after high-dosage corticosteroid therapy. N Engl J Med. 1960;263:672. doi: 10.1056/NEJM196010062631404. [DOI] [PubMed] [Google Scholar]
- 16.Lieberman J.R., Berry D.J., Mont M.A. Osteonecrosis of the hip: management in the 21st century. Instr Course Lect. 2003;52:337. [PubMed] [Google Scholar]
- 17.Lai K.A., Shen W.J., Yang C.Y., Shao C.J., Hsu J.T., Lin R.M. The use of alendronate to prevent early collapse of the femoral head in patients with nontraumatic osteonecrosis. A randomized clinical study. J Bone Joint Surg Am. 2005;87(10):2155. doi: 10.2106/JBJS.D.02959. [DOI] [PubMed] [Google Scholar]
- 18.Glueck C.J., Freiberg R.A., Sieve L., Wang P. Enoxaparin prevents progression of stages I and II osteonecrosis of the hip. Clin Orthop Relat Res. 2005;(435):164. doi: 10.1097/01.blo.0000157539.67567.03. [DOI] [PubMed] [Google Scholar]
- 19.Luo R.B., Lin T., Zhong H.M., Yan S.G., Wang J.A. Evidence for using alendronate to treat adult avascular necrosis of the femoral head: a systematic review. Med Sci Monit. 2014;20:2439. doi: 10.12659/MSM.891123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pyda M., Koczy B., Widuchowski W. Hip resurfacing arthroplasty in treatment of avascular necrosis of the femoral head. Med Sci Monit. 2015;21:304. doi: 10.12659/MSM.891031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim S.M., Lim S.J., Moon Y.W., Kim Y.T., Ko K.R., Park Y.S. Cementless modular total hip arthroplasty in patients younger than fifty with femoral head osteonecrosis: minimum fifteen-year follow-up. J Arthroplasty. 2013;28(3):504. doi: 10.1016/j.arth.2012.08.005. [DOI] [PubMed] [Google Scholar]
- 22.Bedard N.A., Callaghan J.J., Liu S.S., Greiner J.J., Klaassen A.L., Johnston R.C. Cementless THA for the treatment of osteonecrosis at 10-year follow-up: have we improved compared to cemented THA? J Arthroplasty. 2013;28(7):1192. doi: 10.1016/j.arth.2012.09.008. [DOI] [PubMed] [Google Scholar]
- 23.Issa K., Naziri Q., Maheshwari A.V., Rasquinha V.J., Delanois R.E., Mont M.A. Excellent results and minimal complications of total hip arthroplasty in sickle cell hemoglobinopathy at mid-term follow-up using cementless prosthetic components. J Arthroplasty. 2013;28(9):1693. doi: 10.1016/j.arth.2013.03.017. [DOI] [PubMed] [Google Scholar]
- 24.Kim Y.H., Kim J.S., Park J.W., Joo J.H. Contemporary total hip arthroplasty with and without cement in patients with osteonecrosis of the femoral head: a concise follow-up, at an average of seventeen years, of a previous report. J Bone Joint Surg Am. 2011;93(19):1806. doi: 10.2106/JBJS.J.01312. [DOI] [PubMed] [Google Scholar]
- 25.Marker D.R., Seyler T.M., Jinnah R.H., Delanois R.E., Ulrich S.D., Mont M.A. Femoral neck fractures after metal-on-metal total hip resurfacing: a prospective cohort study. J Arthroplasty. 2007;22(7 Suppl 3):66. doi: 10.1016/j.arth.2007.05.017. [DOI] [PubMed] [Google Scholar]
- 26.Sharma S., Gopalakrishnan L., Yadav S.S. Girdlestone arthroplasty. Int Surg. 1982;67(4 Suppl):547. [PubMed] [Google Scholar]
- 27.Cordero-Ampuero J. Girdlestone procedure: when and why. Hip Int. 2012;22(Suppl 8):S36. doi: 10.5301/HIP.2012.9568. [DOI] [PubMed] [Google Scholar]
- 28.Maguire N., Robertson B., Henman P. Girdlestone procedure for avascular necrosis of the hip in an intravenous drug user. J Surg Case Rep. 2014;2014(8):rju039. doi: 10.1093/jscr/rju039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McElwaine J.P., Colville J. Excision arthroplasty for infected total hip replacements. J Bone Joint Surg Br. 1984;66(2):168. doi: 10.1302/0301-620X.66B2.6707049. [DOI] [PubMed] [Google Scholar]
- 30.Lee S.Y., Jeon D.G., Cho W.H., Song W.S., Kong C.B. Comparison of pasteurized autograft-prosthesis composite reconstruction and resection hip arthroplasty for periacetabular tumors. Clin Orthop Surg. 2017;9(3):374–385. doi: 10.4055/cios.2017.9.3.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Agrawal A., Maniar A., Maniar R. Bilateral Girdlestone procedure as a treatment modality in a case of complicated adult-onset osteopetrosis: a case report. JBJS Case Connect. 2019;9(4):e0179. doi: 10.2106/JBJS.CC.18.00179. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.