Key Points
Question
Do patients who fulfill 5 criteria 2 or 3 days after laparoscopic colorectal surgery (a C-reactive protein level <150 mg/dL on the day of discharge, a return of bowel function, tolerance of a diet, pain less than 5 of 10 on a visual analog scale, and being afebrile during the entire stay) have a lower risk of developing an anastomotic leak and can therefore be discharged early?
Findings
This cohort study included 287 adults. Two of 15 anastomotic leaks occurred in patients that fulfilled the criteria vs 13 of 15 in patients who did not, a significant difference.
Meaning
These 5 criteria could determine who is eligible for early discharge after laparoscopic colorectal surgery.
This cohort study observes 287 patients after colorectal surgery to determine if a set of 5 criteria could help differentiate those who are unlikely to develop an anastomotic leak and can therefore be discharged on postoperative day 2 or 3.
Abstract
Importance
Early discharge after colorectal surgery has been advocated. However, there is little research evaluating clinical and/or laboratory criteria to determine who can be safely discharged early.
Objective
To evaluate the diagnostic performance of a C-reactive protein (CRP) level combined with 4 clinical criteria in ruling out an anastomotic leak and therefore allowing an early discharge on postoperative day 2 or 3.
Design, Setting, and Participants
This prospective, single-center cohort study was performed between February 2012 and July 2017. All consecutive adult patients undergoing laparoscopic colorectal surgery were included. All patients were followed up for 30 days postoperatively. Data analysis was performed in May 2021.
Exposures
Whether the 5 discharge criteria were fulfilled on postoperative day 3 (or day 2 for patients discharged on day 2). Fulfillment was defined as a CRP level less than 150 mg/dL on the day of discharge, a return of bowel function, tolerance of a diet, pain less than 5 of 10 on a visual analog scale, and being afebrile during the entire stay.
Main Outcomes and Measures
The primary outcome measurement was the diagnostic performance of the 5 discharge criteria in anticipating anastomotic leak development. The diagnostic performance of CRP level alone and 4 clinical criteria alone was also evaluated. Secondary measures were anastomotic leaks and mortality rates up to postoperative day 30. A discharge was successful if the patient left the hospital on postoperative day 2 or 3 without any complications or readmissions.
Results
A total of 287 patients were included (median [IQR] age, 58 [20] years; 141 men [49%] and 146 women [51%]). Mortality was 0%. There were 17 anastomotic leaks, of which 2 were on day 1 and were excluded. A total of 128 patients fulfilled all criteria, and 125 did not, including 34 for whom data were missing. Two leaks occurred in patients who had fulfilled all criteria vs 13 leaks in patients who did not (hazard ratio, 0.15 [95% CI, 0.03-0.69]; P = .01). Seventy-six of 128 patients (59.4%) were discharged successfully by postoperative day 3. The negative predictive value in ruling out an anastomotic leak was at least 96.9% for CRP alone (96.9% [95% CI, 93.3%-98.8%]), the 4 clinical criteria (98.4% [95% CI, 95.3%-99.7%]), and all 5 criteria combined (98.4% [95% CI, 94.5%-99.8%]). False-negative rates were 40% (95% CI, 16.3%-67.7%) for CRP level alone, 20% (95% CI, 4.3%-48.1%) for the other 4 criteria, and 13.3% (95% CI, 0%-40.5%) for all 5 criteria.
Conclusions and Relevance
These 5 criteria have a high negative predictive value and the lowest false-negative rate, indicating they have the potential to allow for safe early discharge after laparoscopic colorectal surgery.
Introduction
Enhanced recovery programs (ERP) have improved perioperative care and accelerated postoperative recovery following colorectal surgery.1,2,3,4,5,6 Several studies have confirmed the safety of an early discharge, as early as postoperative day (POD) 3.4,7 Despite this possibility, there is a paucity of criteria that can safely determine which patient can be discharged by POD 3. This lack of discharge criteria may lead to unnecessarily longer hospital stays. The most feared and serious complications following colorectal surgery are anastomotic leaks (ALs). To safely discharge a patient, the physician must be confident that the probability of developing an AL after discharge is almost zero. Levels of C-reactive protein (CRP) on POD 3 have been shown to have a good negative predictive value (NPV) for ALs.8,9
The diagnostic accuracy of CRP level could improve with the addition of more information. A recent study10 attempted to determine if the performance of CRP level in diagnosing ALs could improve by adding procalcitonin levels and clinical markers (Dutch Leakage Score). However, procalcitonin levels are more expensive and not as readily available as CRP levels,11 and the Dutch Leakage Score includes too many elements to be practical in everyday use. A simpler and practical method is therefore necessary.
The goal of this study was to evaluate the feasibility and safety of an early discharge within 3 days, following an ERP after laparoscopic colorectal surgery, provided that patients met 5 simple criteria: a CRP level less than 150 mg/dL (to convert to milligrams per liter, multiply by 10), an absence of fever during the entire hospital stay (temperature <38 °C), a return of bowel function (flatus with or without stool), adequate pain control with oral analgesics (pain less than 5 of 10 on a 10-point visual analog scale), and tolerance of a solid diet.
Methods
Study Design
This prospective, noninterventional study was performed in a single colorectal surgery department (Lyon Sud University Hospital, Lyon, France). By French law, given its noninterventional nature, the study was exempt from an ethics review and patient consent procedures.
Participants
All adult patients undergoing laparoscopic colorectal surgery between February 2012 and July 2017 were included. We chose laparoscopic procedures because they are becoming the standard of care for elective colorectal procedures. Also, CRP level thresholds in detecting AL differ between open and laparoscopic approaches.12 All patients were included in this ERP. Exclusion criteria were conversion to an open procedure, creation of a stoma during the same procedure, and another major procedure being performed simultaneously (eg, liver resection).
Perioperative Protocol
Preoperatively
Carbohydrate drinks were recommended up until 2 hours before surgery.13 The standard of care in France during the study period was to not perform a bowel preparation.14
Intraoperatively
Patients did not undergo routine urinary catheter placement. Patients did not undergo routine placement of intra-abdominal drains by the end of the procedure.15 Intravenous fluids were restricted to 3 mL/kg/h of crystalloid. An opioid-sparing protocol was implemented to prevent postoperative ileus.16
Postoperatively
Patients were allowed to take liquids by mouth once they awoke from anesthesia. A diet was advanced as tolerated, and maintenance intravenous fluids were discontinued on POD 1, unless the patient developed an ileus. The patients would ambulate on POD 0 and have daily physical therapy sessions.
Laboratory measurements were collected on PODs 1 and 3. If the patient was going to be discharged on POD 2, a blood test would be performed on POD 2. Any additional blood tests were performed as deemed necessary by the surgeon.
Pain was treated with intravenous analgesics until POD 1, followed by oral analgesics. Whenever possible, opioids were avoided. Routine imaging was not performed prior to discharge. Patients could be discharged on POD 3 (or POD 2 if the patient was doing exceptionally well) if all of the following 5 conditions were met: a CRP level less than 150 mg/dL,9 an absence of fever during the entire hospital stay (temperature <38 °C), a return of bowel function (flatus with or without stool), adequate pain control with oral analgesics (pain less than 5 on a 10-point visual analog scale) with 1 g of scheduled paracetamol every 6 hours and 50 mg of tramadol every 6 hours as needed, and tolerance of a solid diet. Postoperative visits took place 15 and 30 days after discharge.
Variables
The following variables were recorded for each patient. Preoperatively, age, sex, body mass index (calculated as weight in kilograms divided by height in meters squared), American Society of Anesthesiologists score, and operative indication were recorded. Intraoperatively, the type of procedure, operative time, and placement of an intra-abdominal drain were recorded. Postoperatively, the CRP levels on PODs 1 and 3 (or POD 2, if the patient was discharged on POD 2), vital signs and pain on a visual analog scale daily per the nursing protocol, the return of bowel function, food tolerance, and the day of discharge were recorded. The day of diagnosis of an AL and its management, other complications, the Clavien-Dindo classification of complications, readmission, and mortality were recorded until POD 30.
Outcomes
The primary outcome of the study was the diagnostic performance of the 5 criteria in ruling out an AL. An AL was defined as an AL, perianastomotic fluid collection, or perianastomotic air-fluid levels seen on computed tomography scan. Secondary outcomes were the rate of successful discharge, uncomplicated discharge, postoperative complications (including ALs), readmissions, and death in the group that fulfilled the 5 criteria vs the group that did not and the diagnostic performance of the 5 criteria in prognosticating a successful discharge or an uncomplicated discharge and ruling out all complications combined, readmission, and death. A successful discharge was defined as a discharge on POD 2 or 3 without readmission or complications up until POD 30. An uncomplicated discharge was defined as discharge on any POD without readmission or complications up until POD 30. We were also interested in the diagnostic performance of the 4 criteria without a CRP level and a CRP level alone. Finally, we recorded the reason why patients who fulfilled the 5 criteria were not discharged on POD 3.
Statistical Analysis
For the diagnostic performance of the 5 criteria, the 4 criteria, or CRP level alone on AL, complications, readmissions, successful discharge, and uncomplicated discharge, the following were calculated: NPV for negative outcomes and positive predictive values (PPVs) for positive outcomes. Specifically, for ALs, we also calculated sensitivity and the false-negative rate. Exact binomial 95% CIs for all measures were calculated.
For comparisons between patients who fulfilled the 5 criteria vs those who did not and those with missing data, we did not assume any underlying distribution and treated all continuous data as nonparametric; the Kruskal-Wallis rank sum test was used for independent observations. For categorical variables, we used Fisher exact tests. For time-to-event data (time to diagnosis of AL), hazard ratios with their corresponding 95% CIs were calculated after evaluating if a multivariate Cox proportional hazards model was appropriate according to Schoenfeld residuals. Variables were included in the model if they were significant on univariate analysis. A Kaplan-Meier graph was produced as well. The ALs that developed on POD 1 were excluded from the analysis, since the leak developed before the patient could be evaluated for discharge.
All analyses were carried out with R version 4.0.5 (R Project for Statistical Computing). A P < .05 was considered statistically significant. Data analysis was performed in May 2021.
Results
A total of 287 patients underwent laparoscopic colorectal surgery between February 2012 and July 2017. The median (IQR) length of stay was 4 (2) days. Of these, 128 patients fulfilled the 5 criteria, 125 did not, and 34 had missing data with regards to the 5 criteria, not allowing classification. All of the 34 patients specifically lacked CRP measurements. One also lacked a pain evaluation at discharge. Of note, a total of 45 CRP levels were missing for the entire cohort. However, 11 patients could be classified as not fulfilling the criteria by the remaining 4 variables.
Demographic Data
The overall median age was 58 (range, 17-90) years. Overall median operating time was 192 (range, 64-435) minutes. An abdominal drain was placed in 39 of 287 patients (13.6%) in whom the operating surgeon deemed that there was a risk of postoperative bleeding. The most common operative indication was diverticulitis (139 of 287 [48.4%]), followed by cancer (83 of 287 [28.9%]), terminal ileitis in patients with Crohn disease (34 of 287 [11.8%]), and polyps with dysplasia or the inability to remove them entirely endoscopically (21 of 287 [7.3%]). Table 1 presents the breakdown according to how the criteria were fulfilled. Groups were similar for all variables.
Table 1. Patient Characteristics According to 5 Criteria Fulfillment Status.
| Variable | 5 Criteria, No. (%) | P value | ||
|---|---|---|---|---|
| Fulfilled (n = 128) | Not fulfilled (n = 125) | Missing (n = 34) | ||
| Age, median (IQR), y | 59 (49-66) | 56 (45-68) | 58 (50-64) | .75 |
| Sex | ||||
| Male | 69 (54) | 53 (42) | 19 (56) | .13 |
| Female | 59 (46) | 72 (58) | 15 (44) | |
| BMI, median (IQR) | 24.3 (22.0-27.3) | 24.7 (22.4-28.4) | 25.2 (22.6-28.0) | .33 |
| American Society of Anesthesiologists category | ||||
| 1 | 69 (54) | 54 (43) | 23 (68) | .12 |
| 2 | 53 (41) | 62 (50) | 10 (29) | |
| 3 | 6 (4.7) | 9 (7.2) | 1 (2.9) | |
| Indication | ||||
| Adenocarcinoma | 37 (29) | 35 (28) | 11 (32) | .18 |
| Crohn disease | 10 (7.8) | 23 (18) | 1 (2.9) | |
| Diverticulitis | 69 (54) | 52 (42) | 18 (53) | |
| Polyp | 8 (6.2) | 10 (8.0) | 3 (8.8) | |
| Other | 4 (3.1) | 5 (4.0) | 1 (2.9) | |
| Type of surgery | ||||
| Ileocecal resection | 13 (10) | 22 (18) | 1 (2.9) | .10 |
| Right hemicolectomy | 16 (12) | 24 (19) | 7 (21) | |
| Splenic flexure resection | 1 (0.8) | 4 (3.2) | 1 (2.9) | |
| Left hemicolectomy | 6 (4.7) | 10 (8.0) | 2 (5.9) | |
| Sigmoidectomy | 80 (62) | 57 (46) | 20 (59) | |
| Hartmann reversal | 2 (1.6) | 0 (0) | 1 (2.9) | |
| High anterior resection | 8 (6.2) | 5 (4.0) | 2 (5.9) | |
| Subtotal colectomy | 2 (1.6) | 3 (2.4) | 0 (0) | |
| Operative time, median (IQR), min | 198 (156-240) | 180 (137-240) | 188 (149-244) | .28 |
| Intraoperative drain | 18 (14) | 19 (15) | 2 (5.9) | .40 |
Abbreviation: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared).
Outcomes
Details on Patient Discharge
Of the 128 patients who fulfilled the 5 criteria, 76 (59.4%) were discharged by POD 3. The remaining 52 (40.6%) were discharged at later dates. The reasons for delayed discharge are shown in Table 2. The most common cause was patient delay (ie, the patient did not feel comfortable being discharged on the day chosen by the surgeon) or physician delay (ie, even though a patient fulfilled the 5 criteria, the physician felt that the patient could more appropriately leave after POD 3), occurring in 33 of 52 patients (64%).
Table 2. Reasons Why Patients Who Fulfilled the Criteria Were Not Discharged on Postoperative Day 3.
| Reason | No. (%) |
|---|---|
| Patient or physician delaya | 33 (63) |
| Drain still in place | 9 (17) |
| Bleeding per rectum | 4 (8) |
| Urinary catheter removed on postoperative day 3 | 1 (2) |
| Restarted vitamin K anticoagulant use | 1 (2) |
| Intravenous antibiotics for preoperative infection | 1 (2) |
| Altered mental status (self-resolving) | 1 (2) |
| Waiting for skilled nursing facility | 1 (2) |
| Monitoring for Crohn disease in a patient receiving corticosteroids | 1 (2) |
Patient delay means that the patient did not feel comfortable being discharged on the day chosen by the surgeon and would therefore stay longer. Physician delay means that even though a patient would fulfill the 5 criteria, the physician felt that the patient was more appropriate to leave after postoperative day 3.
Of the 125 patients who did not fulfill the 5 criteria, 32 of 125 (25.6%) were discharged by POD 3. The specific reasons why the criteria were not fulfilled in those patients are presented in eFigure 1 in the Supplement. None of these patients developed an AL later.
Diagnostic Performance of the Criteria in Ruling Out Negative Outcomes and Anticipating Positive Outcomes
The NPV of fulfilling the 5 criteria in ruling out ALs was 98.4% (95% CI, 94.5%-99.8%), and the PPV for a successful discharge was 78.9% (95% CI, 70.6%-85.7%). The false-negative rate of the 5 criteria vs ALs was 13.3% (95% CI, 0%-40.5%). These data were calculated on 253 patients.
Table 3 shows the NPVs and PPVs for the remaining outcomes of interest as well as the diagnostic performance of the 4 clinical criteria, without taking into account CRP levels (calculated on 286 patients) and CRP levels alone (calculated on 242 patients). The false-negative rate increased as we removed information, from 13.3% (95% CI, 0%-40.5%) for the 5 criteria, to 20% (95% CI, 4.3%-48.1%) for the 4 criteria, to 40% (95% CI, 16.3%-67.7%) for the CRP level alone.
Table 3. Metrics for Positive and Negative Outcomes.
| Outcome | % (95% CI) | ||
|---|---|---|---|
| 5 Criteria | 4 Criteria | C-reactive protein level alone | |
| Sensitivity | |||
| AL | 86.7 (59.5-98.3) | 80.0 (51.9-95.7) | 60.0 (32.3-83.7) |
| False-negative rate | |||
| AL | 13.3 (0-40.5) | 20.0 (4.3-48.1) | 40.0 (16.3-67.7) |
| Negative predictive value | |||
| AL | 98.4 (94.5-99.8) | 98.4 (95.3-99.7) | 96.9 (93.3-98.8) |
| All complications | 79.7 (71.7-86.3) | 76.5 (69.7-82.4) | 74.5 (67.7-80.5) |
| Readmission | 92.2 (86.1-96.2) | 91.3 (86.2-94.9) | 93.8 (89.3-96.7) |
| Positive predictive value | |||
| Successful discharge | 78.9 (70.6-85.7) | 78.2 (68.9-85.8) | 87.5 (74.8-95.3) |
| Uncomplicated discharge | 78.9 (70.6-85.7) | 78.2 (68.9-85.8) | 87.5 (74.8-95.3) |
Abbreviation: AL, anastomotic leak.
Anastomotic Leaks, Complications, Reinterventions, Readmissions, and Mortality
Eighty-three of 287 patients (28.9%) developed a complication (Table 4). Most had complications of Clavien-Dindo grade I (25 of 83 [30%]) or grade II (42 of 83 [51%]). The most common grade I complication was bleeding per rectum (15 of 25 [60%]). The most common grade II complication was ileus (12 of 42 [29%]). Two of 83 (2%) developed a grade IIIa complication and 14 of 83 (17%) developed a grade IIIb complication.
Table 4. Patient Outcomes According to 5 Criteria Fulfillment Status.
| Variable | 5 Criteria status, No. (%) | P value | ||
|---|---|---|---|---|
| Fulfilled (n = 128) | Not fulfilled (n = 125) | Missing (n = 34) | ||
| Complications | 26 (20) | 50 (40) | 7 (21) | .001 |
| Clavien-Dindo level | ||||
| I | 12 (46) | 10 (20) | 3 (43) | .21 |
| II | 11 (42) | 27 (54) | 4 (57) | |
| IIIa | 0 (0) | 2 (4.0) | 0 | |
| IIIb | 3 (12) | 11 (22) | 0 | |
| Anastomotic leak | 2 (1.6) | 15 (12) | 0 | <.001 |
| Readmission | 10 (7.8) | 6 (4.8) | 4 (12) | .29 |
| Successful discharge | 66 (52) | 26 (21) | 25 (74) | <.001 |
| No complication or readmission | 102 (80) | 75 (60) | 27 (79) | .001 |
| Length of stay, median (IQR), d | 3 (1) | 5 (4) | 3.00 (0) | <.001 |
| Day of discharge | ||||
| 2 | 8 (6.2) | 4 (3.2) | 7 (21) | <.001 |
| 3 | 68 (53) | 28 (22) | 24 (71) | |
| ≥4 | 52 (41) | 93 (74) | 3 (8.8) | |
Abbreviation: AL, anastomotic leak.
The most common grade IIIa and IIIb complication was ALs. These occurred in 17 of 287 patients (5.9%) overall. Of the 17 patients who developed an AL, 10 (59%) had Clavien-Dindo IIIb ALs, 1 (6%) had a Clavien-Dindo IIIa AL, and 6 (35%) had Clavien-Dindo II ALs. No one died.
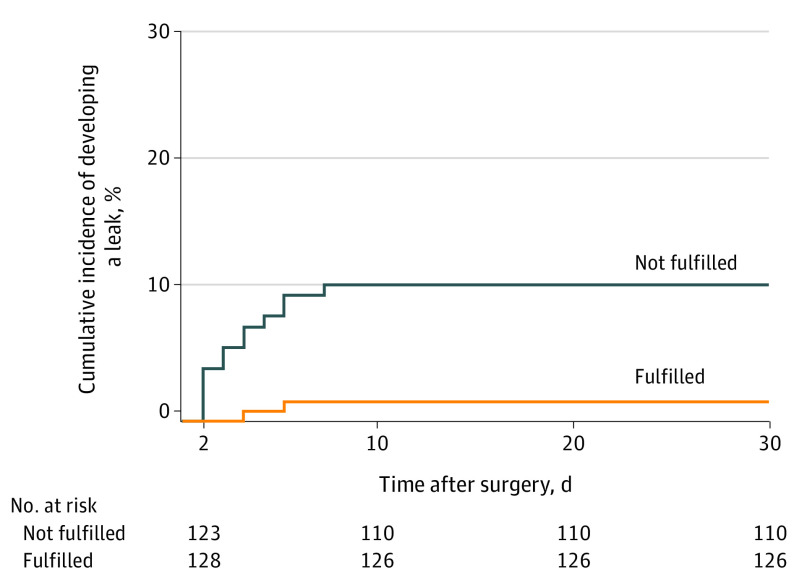
Of the 128 patients who fulfilled the 5 criteria, 2 developed an AL, vs 13 patients who developed ALs among those who did not fulfill the criteria (hazard ratio, 0.15 [95% CI, 0.03-0.69]; P = .01 on the multivariate Cox analysis). A Kaplan-Meier graph comparing the cumulative incidence of AL in the patients that fulfilled the 5 criteria vs those that did not is seen in the Figure. Of note, in the univariate analysis (but not in the multivariate analysis), body mass index was significantly different between the patients who developed a leak vs those who did not (χ2 = 4.765; P = .03 by Kruskal-Wallis rank sum test). The specific way in which the criteria were not fulfilled in all patients who developed an AL is presented in eFigure 2 in the Supplement.
Figure. Cumulative Incidence of Anastomotic Leaks in Patients Who Fulfilled 5 Criteria vs Those Who Did Not.
Of note, there were 2 anastomotic leaks that occurred on postoperative day 1 and were not taken into account (since the criteria are evaluated on postoperative day 2 or 3). Data were censored at 30 days of follow-up since surgery.
The other Clavien-Dindo grade IIIa complication was in a patient with an abdominal wall hematoma that was drained radiologically. The remaining Clavien-Dindo grade IIIb complications were in 1 patient who underwent an abscess incision and drainage under general anesthesia, 2 patients who underwent laparoscopy for hemoperitoneum evacuation, and 1 patient who underwent endoscopic treatment of a bleeding gastric ulcer.
Sixteen of 287 (5.6%) needed reintervention for the following reasons: 13 of 16 (81%) needed surgery: 10 of 13 for an AL, 2 of 13 for hemoperitoneum evacuation, and 1 of 13 for abscess drainage. Two of 16 (13%) required interventional radiology drainage: 1 for an AL and 1 for an abdominal wall hematoma. Finally, 1 patient required endoscopic treatment for a bleeding gastric ulcer.
Twenty of 287 (7.9%) required readmission. The most common cause was bleeding per rectum (5 of 20 [25%]). Only 2 required blood transfusion; the rest were admitted for observation but did not require any intervention. Two of 20 (10%) developed an AL (and both fulfilled the 5 criteria). Readmission rates were not different between the patients who fulfilled the 5 criteria vs those who did not (Table 4). Among those discharged on POD 3 or earlier, 9 of 139 (6.5%) required readmission compared with 11 of 148 (7.4%) discharged after POD 3. Mortality at POD 30 was 0% for all groups.
Discussion
This study showed that the combination of 4 simple clinical criteria and CRP levels can possibly allow for a safe early discharge after laparoscopic colorectal surgery. By these criteria, only 2 patients had their ALs missed.
This is also the first study, to our knowledge, to compare the false-negative rates of CRP levels alone, 4 clinical criteria, and their combination. Studies evaluating ways to anticipate ALs put the most weight on a high NPV17 or high accuracy.18 We also obtained very high NPVs (>97%). However, it must be noted that the NPV depends on the prevalence of ALs. A low prevalence will always lead to a high NPV, even if the test does not perform as well as desired.
In the specific case of ALs, the most important metric is neither the NPV nor accuracy. What is important is the absolute number or ratio of patients who were thought to be unlikely to develop an AL who went on to develop an AL (ie, the false-negative rate). This can be seen immediately from our comparative table between CRP levels, the 4 clinical criteria, and all 5 criteria (Table 4). All 3 have an NPV that is greater than 97%. However, the false-negative rates are very different. As more information is removed, more patients are missed. Even though the 95% CIs overlap, the difference between the point estimates is large. Furthermore, compared with NPV values, the false-negative rate does not depend on prevalence but is instead a number intrinsic to the test.
The fact that the false-negative rate decreases as more information is supplied points to the direction that is necessary to improve discharge criteria. In our cohort, only 2 patients developed a leak despite meeting the 5 criteria. One was receiving steroids for Crohn disease during the perioperative period and had a repeated ileocolic resection. Steroids can reduce inflammation (and specifically CRP levels19) and decrease postoperative pain.20 Even though he fulfilled all 5 criteria on POD 3, he remained hospitalized for 1 more day; because he was doing very well, we discharged him on POD 4. He was readmitted on POD 6 for an AL and was managed conservatively. We believe that these discharge criteria are probably not applicable for patients receiving steroids.
The second patient developed tachycardia with a persistent heart rate greater than 120 beats per minute after the second day. He was discharged on POD 3 while perfectly well from a clinical standpoint. He was readmitted the following day for peritonitis and underwent a Hartmann procedure. It seems that, just as in bariatric surgery, tachycardia may be an early sign of AL or peritonitis.21
Another important point in our method is that we excluded patients who developed a leak on POD 1, since our discharge criteria should be applied on patients who have not yet developed an AL. Indeed, in previous studies,10 this possibly trivial point is not clarified. However, in everyday practice, we would not apply a score to anticipate something that has already happened. If this point is not clarified, the applicability of a study’s conclusion could be compromised.
An important point is the use of a single CRP cutoff value for 2 different PODs. Even though the cutoff values are different (POD 2: 180 mg/dL; POD 3, 150 mg/dL9,18), we decided to use a single value to facilitate applicability in the clinical setting. Also, by choosing the lower value, the test’s sensitivity increased.
Several studies have already shown that the length of stay following colorectal surgery can decrease by implementing ERPs.6 Despite multiple studies, the mean length of stay is more than 5 days.5,22,23 Even though the cause of delayed discharge is not always clear, one of the reasons leading to extended stays could be the surgeon’s fear of missing a developing leak if the patient is discharged too early. In this cohort, none of the patients discharged on POD 2 and only 2 patients discharged on POD 3 developed an AL, showing that a discharge by POD 3 is not necessarily too early. Furthermore, 9 of 139 patients (6.5%) discharged on PODs 2 or 3 required readmission, compared with 11 of 148 patients (7.4%) discharged after POD 3. This shows that discharging patients earlier does not necessarily increase readmission rates.
Previous studies have shown a reduction in the rate of postoperative complications and length of stay when using ERPs.24 In our study, 83 of 287 patients (28.9%) developed postoperative complications, which is a rate similar to other studies.24,25
Finally, when looking at successful discharge, fewer than half of the patients (40.8%) had their cases defined as a success (discharge at POD 3 without complications or readmission). The median length of stay was 4 days. This result is partly explained by the proportion of patients who fulfilled all 5 criteria but were not discharged (n = 52), mainly because of patient or surgeon reluctance for a discharge on POD 3.
Limitations
Our study has the following limitations. First, a considerable portion of CRP levels was missing (45 of 287 [11.8%]). Nevertheless, we were able to classify 11 of them as not fulfilling the criteria based on the other 4 variables. At the time, our postoperative protocol was not automated, leading to missed laboratory values. Despite this, the diagnostic performance of the 5 criteria was able to be calculated on approximately 90% of the cohort and that of the 4 criteria on the entire cohort. More importantly, of the 34 patients who we were not able to classify, none developed an AL. Second, our cohort is heterogeneous. Table 1 shows that both malignant and benign pathology results are included in the analysis, and different types of surgery were performed. However, the partition between the 3 groups in Table 1 does not appear extremely different, and for that reason, we believe that this heterogeneity does not invalidate our conclusions. Furthermore, it seems possible that the criteria may be applicable in multiple settings exactly because of this heterogeneity.
Conclusions
Our study shows that a patient fulfilling our 5 criteria on PODs 2 or 3 has a low probability of developing an AL. This potentially allows for an early safe discharge.
eFigure 1. A heatmap demonstrating how each one of the 5 different criteria was fulfilled or not in patients that left on POD#3 despite not fulfilling all 5 criteria simultaneously.
eFigure 2. A heatmap demonstrating how each one of the 5 different criteria was fulfilled or not in patients that developed an anastomotic leak.
References
- 1.Bagnall NM, Malietzis G, Kennedy RH, Athanasiou T, Faiz O, Darzi A. A systematic review of enhanced recovery care after colorectal surgery in elderly patients. Colorectal Dis. 2014;16(12):947-956. doi: 10.1111/codi.12718 [DOI] [PubMed] [Google Scholar]
- 2.Esteban F, Cerdan FJ, Garcia-Alonso M, et al. A multicentre comparison of a fast track or conventional postoperative protocol following laparoscopic or open elective surgery for colorectal cancer surgery. Colorectal Dis. 2014;16(2):134-140. doi: 10.1111/codi.12472 [DOI] [PubMed] [Google Scholar]
- 3.Forsmo HM, Pfeffer F, Rasdal A, et al. Compliance with enhanced recovery after surgery criteria and preoperative and postoperative counselling reduces length of hospital stay in colorectal surgery: results of a randomized controlled trial. Colorectal Dis. 2016;18(6):603-611. doi: 10.1111/codi.13253 [DOI] [PubMed] [Google Scholar]
- 4.Gash KJ, Greenslade GL, Dixon AR. Enhanced recovery after laparoscopic colorectal resection with primary anastomosis: accelerated discharge is safe and does not give rise to increased readmission rates. Colorectal Dis. 2012;14(10):1287-1290. doi: 10.1111/j.1463-1318.2012.02969.x [DOI] [PubMed] [Google Scholar]
- 5.Kennedy RH, Francis EA, Wharton R, et al. Multicenter randomized controlled trial of conventional versus laparoscopic surgery for colorectal cancer within an enhanced recovery programme: EnROL. J Clin Oncol. 2014;32(17):1804-1811. doi: 10.1200/JCO.2013.54.3694 [DOI] [PubMed] [Google Scholar]
- 6.Zhuang C-L, Huang D-D, Chen F-F, et al. Laparoscopic versus open colorectal surgery within enhanced recovery after surgery programs. Surg Endosc. 2015;29(8):2091-2100. doi: 10.1007/s00464-014-3922-y [DOI] [PubMed] [Google Scholar]
- 7.Couch DG, Luther A, Farid S, Kang P. Response to Gash et al. Colorectal Dis. 2013;15(6):758. doi: 10.1111/codi.12184 [DOI] [PubMed] [Google Scholar]
- 8.Giaccaglia V, Salvi PF, Antonelli MS, et al. Procalcitonin reveals early dehiscence in colorectal surgery. Ann Surg. 2016;263(5):967-972. doi: 10.1097/SLA.0000000000001365 [DOI] [PubMed] [Google Scholar]
- 9.Ortega-Deballon P, Radais F, Facy O, et al. C-reactive protein is an early predictor of septic complications after elective colorectal surgery. World J Surg. 2010;34(4):808-814. doi: 10.1007/s00268-009-0367-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Italian ColoRectal Anastomotic Leakage (iCral) Study Group . Anastomotic leakage after elective colorectal surgery. BJS Open. 2020;4(3):499-507. doi: 10.1002/bjs5.50269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cousin F, Ortega-Deballon P, Bourredjem A, Doussot A, Giaccaglia V, Fournel I. Diagnostic accuracy of procalcitonin and C-reactive protein for the early diagnosis of intra-abdominal infection after elective colorectal surgery. Ann Surg. 2016;264(2):252-256. doi: 10.1097/SLA.0000000000001545 [DOI] [PubMed] [Google Scholar]
- 12.Paradis T, Zorigtbaatar A, Trepanier M, et al. Meta-analysis of the diagnostic accuracy of C-reactive protein for infectious complications in laparoscopic versus open colorectal surgery. J Gastrointest Surg. 2020;24(6):1392-1401. doi: 10.1007/s11605-020-04599-2 [DOI] [PubMed] [Google Scholar]
- 13.Lidder P, Thomas S, Fleming S, Hosie K, Shaw S, Lewis S. A randomized placebo controlled trial of preoperative carbohydrate drinks and early postoperative nutritional supplement drinks in colorectal surgery. Colorectal Dis. 2013;15(6):737-745. doi: 10.1111/codi.12130 [DOI] [PubMed] [Google Scholar]
- 14.Bretagnol F, Panis Y, Rullier E, et al. ; French Research Group of Rectal Cancer Surgery (GRECCAR) . Rectal cancer surgery with or without bowel preparation. Ann Surg. 2010;252(5):863-868. doi: 10.1097/SLA.0b013e3181fd8ea9 [DOI] [PubMed] [Google Scholar]
- 15.Prudhomme M, Alline M, Chauvat J, Fabbro-Perray P, Ripoche J, Bertrand MM; French Research Group of Rectal Cancer Surgery (GRECCAR) . Primary prevention of peristomial hernias via parietal prostheses. Dig Liver Dis. 2016;48(7):812-816. doi: 10.1016/j.dld.2016.03.020 [DOI] [PubMed] [Google Scholar]
- 16.Baucom RB, Phillips SE, Ehrenfeld JM, et al. Association of perioperative hypothermia during colectomy with surgical site infection. JAMA Surg. 2015;150(6):570-575. doi: 10.1001/jamasurg.2015.77 [DOI] [PubMed] [Google Scholar]
- 17.Singh PP, Zeng ISL, Srinivasa S, Lemanu DP, Connolly AB, Hill AG. Systematic review and meta-analysis of use of serum C-reactive protein levels to predict anastomotic leak after colorectal surgery. Br J Surg. 2014;101(4):339-346. doi: 10.1002/bjs.9354 [DOI] [PubMed] [Google Scholar]
- 18.Yeung DE, Peterknecht E, Hajibandeh S, Hajibandeh S, Torrance AW. C-reactive protein can predict anastomotic leak in colorectal surgery. Int J Colorectal Dis. 2021;36(6):1147-1162. doi: 10.1007/s00384-021-03854-5 [DOI] [PubMed] [Google Scholar]
- 19.Tarp S, Bartels EM, Bliddal H, et al. Effect of nonsteroidal antiinflammatory drugs on the C-reactive protein level in rheumatoid arthritis. Arthritis Rheum. 2012;64(11):3511-3521. doi: 10.1002/art.34644 [DOI] [PubMed] [Google Scholar]
- 20.Gupta A, Bah M. NSAIDs in the treatment of postoperative pain. Curr Pain Headache Rep. 2016;20(11):62. doi: 10.1007/s11916-016-0591-7 [DOI] [PubMed] [Google Scholar]
- 21.Montravers P, Augustin P, Zappella N, et al. Diagnosis and management of the postoperative surgical and medical complications of bariatric surgery. Anaesth Crit Care Pain Med. 2015;34(1):45-52. doi: 10.1016/j.accpm.2014.06.002 [DOI] [PubMed] [Google Scholar]
- 22.ERAS Compliance Group . The impact of enhanced recovery protocol compliance on elective colorectal cancer resection. Ann Surg. 2015;261(6):1153-1159. doi: 10.1097/SLA.0000000000001029 [DOI] [PubMed] [Google Scholar]
- 23.Healthcare Quality Improvement Project . National bowel cancer audit report 2017. Published December 14, 2017. Accessed October 1, 2021. https://www.hqip.org.uk/resource/national-bowel-cancer-audit-annual-report-2017/#.YVcmU5rMI2w.
- 25.Christensen HK, Thaysen HV, Rodt SÅ, Carlsson P, Laurberg S. Short hospital stay and low complication rate are possible with a fully implemented fast-track model after elective colonic surgery. Eur Surg Res. 2011;46(3):156-161. doi: 10.1159/000324406 [DOI] [PubMed] [Google Scholar]
- 26.Arezzo A, Bini R, Lo Secco G, Verra M, Passera R. The role of stents in the management of colorectal complications. Surg Endosc. 2017;31(7):2720-2730. doi: 10.1007/s00464-016-5315-x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. A heatmap demonstrating how each one of the 5 different criteria was fulfilled or not in patients that left on POD#3 despite not fulfilling all 5 criteria simultaneously.
eFigure 2. A heatmap demonstrating how each one of the 5 different criteria was fulfilled or not in patients that developed an anastomotic leak.