Highlights
-
•
There is a pressing need to create a holistic and respectful culture of care for children with FND and their families.
-
•
An outdated culture of care for children with FND lingers across many health systems.
-
•
The outdated culture imposes iatrogenic stigma on children and families.
-
•
Structural, educational, and process interventions can be used to promote change.
-
•
Essential changes include adoption of FND-informed beliefs, attitudes, and referral/treatment processes by professionals.
Keywords: Functional neurological disorder (FND), Functional seizures, Stigma, Children and adolescents, Cultural change, Clinical ethics
Abstract
As members of a multidisciplinary team of professionals who treat children and adolescents with functional neurological (conversion) disorder (FND), we highlight the pressing need to develop an FND-informed culture of care that takes into account recent advances in our understanding of this group of patients. Stories of clinical encounters in health care settings from around the world—told by children and adolescents with FND, their parents, and health professionals—portray an outdated culture of care characterized by iatrogenic stigma, erosion of empathy and compassion within the clinician-patient relationship, and a lack of understanding of FND and its complex neurobiology. After a brief exploration of the outdated culture, we share our counterstories: how we and our colleagues have worked, and continue to work, to create an FND-informed culture in the health systems where we practice. We discuss the therapeutic use of child-friendly language. We also discuss a range of structural, educational, and process interventions that can be used to promote FND-informed beliefs and attitudes, FND-informed clinician-patient encounters, and FND-informed referral processes, treatment pathways, and therapeutic interventions.
1. Introduction
In this article we use clinical vignettes—derived from our own work as members of a multidisciplinary team of professionals, and also from that of colleagues—to illustrate the experiences and perceptions of children (including adolescents), their parents, medical trainees, nurses, and senior clinicians when children present with functional neurological disorder (FND) (including functional seizures). We refer to these vignettes as stories in order to emphasize their narrative dimension and human context. Stories provide a window into the experiences of patients and families, the beliefs and attitudes of clinicians, and the complexities of clinical health care [1], [2]. We use them here to bring into focus the challenges of working with children and adolescents experiencing FND, to illustrate how cultures of care can be detrimental for patients with FND, and to highlight the pressing need to change the culture of care.
Our initial set of stories (below) provides a powerful account of an outdated culture characterized by stigma, erosion of empathy and compassion within the clinician-patient relationship, and a lack of understanding of FND and its complex neurobiology [3], [4], [5], [6]. After that brief exploration of the outdated culture, we use some of our own stories and counterstories [1], [2] to communicate how we and our colleagues have worked, and continue to work, to create a FND-informed culture in the health systems where we practice. Notably, this approach to FND is, in effect, an application of the holistic, biopsychosocial model of illness. This model of illness takes into account “the social, psychological, and behavioral dimensions of illness” (p 129) [7]. Importantly, the model is consistent with contemporary research findings that suggest complex interactions between biological (e.g., genetics, epigenetics, aberrant neural network function), psychological (e.g., attention, expectations, maladaptive coping strategies), and social (e.g., adversity and the experience-dependent neuroplastic consequences of adversity) factors in the neurobiology of FND [8], [9], [10].
While the stories—and our examination of the culture of care—come from pediatric clinical practice, we are aware that similar issues arise in working with adults [9], [11], [12], [13], [14]. In this context, it is likely that the issues and ideas examined in this article have important implications for clinicians treating adults with FND across a range of adult health care systems.
Throughout the manuscript we use the pronoun she because in the civilian pediatric setting, more girls than boys present with FND. During wartime or in the context of the military action, the situation is reversed [15].
2. The outdated culture: Stories
2.1. Stories capturing the child or family’s perspective
Communicating the Misguided Belief That the Child Is Faking Her Symptoms
When I was having a [functional] seizure on the way to the hospital in the ambulance, the ambulance man [paramedic] yelled at me, “Just stop this nonsense. I know you’re putting it on! Snap out of it!”
A Clinician’s Failure to Give and Explain the diagnosis
The neurologist did not give me a diagnosis. Instead, he suggested that my mother organize an appointment to see Dr. X. When we rang to make the appointment, we realized that Dr. X was a psychologist. It was then that I realized that the neurologist thought that it was all in my head.
A Dismissive Bedside Manner
The doctor took my history and completed a physical examination. Then, turning away from me, he said to his team, “This is conversion and not neurologic,” after which he simply walked out of the room. That was the end of the consultation.
Disrespect Expressed Publicly and Overheard by the Family
After the ER doctor checked my daughter, I could hear him talking to other doctors outside our room. They were giggling. They tried to make it quiet, but I could tell it was about my daughter. She couldn’t walk, and they were laughing at her.
2.2. Stories capturing the clinician’s perspective
The Misguided Belief That the Child Is Faking Her Symptoms
A teenage girl was brought to our emergency room experiencing events that were suspicious for functional seizures. After watching her for 30 seconds, the attending lifted the girl’s arm above her face and dropped it. Seeing that she diverted her arm, thus not hitting her face, the attending announced to the room, “OK, honey, you can stop now,” and walked out of the room.
Clinician’s Reluctance to Convey a Diagnosis That the Clinician Believes to Be Unwelcome
In the rounding room, my supervising pediatricians spoke about the FND diagnosis with certainty. They were unambiguous in the diagnosis and were clear about their plan. At the patient’s bedside, their demeanor changed, either to be apologetic (e.g., “Life has many mysteries, and your disorder just isn’t well understood”) or to be confrontational (and in language that sometimes belied the doctor’s discomfort: e.g., “Your symptoms are a consequence of something bad, even if you haven’t figured yourself out enough yet to know what that is”). Physicians who commonly approached their work with compassion and confidence were transformed into lesser versions of their clinical selves.
Clinician Conviction That Functional Aphonia Always Represents Unspoken Issues Related to Early Sexual Abuse
A speech pathologist refused to offer therapy to an adolescent with functional loss of voice until she attended intensive psychotherapy with a mental health practitioner. The therapist held the firm belief that all children who present with functional aphonia have been sexually abused, even if they have never reported it or had no recollection of such an incident. The parents felt deeply affronted by the pressure put on their daughter to admit to some form of sexual abuse and the underlying suggestion that the father may have been involved.
Inaction Due to an Ingrained Belief That No Treatment Is Possible
As a resident, I met a patient who was effectively mute due to a serious functional stutter. When I discussed her with my attending, he told me, “Patients like her are unfixable. It’s sad, it really is. But there’s not much we can do.” He spent roughly 90 seconds with her. Before leaving he announced that I would tell her the plan. But we had no plan. The plan was, in effect, “Tell her what she has and then tell her goodbye.”
The Belief That Patients with FND Are Not Deserving of Health Care Resources
More times than I can count, I have heard physicians and nurses state that a child with FND was taking a bed that should go instead to a patient with “real” symptoms.
Some of my colleagues (in physiotherapy) see my work with these patients as “not real physio.”
Disrespect and Disconnection Expressed Publicly Via Laughter, Jokes, and Negative Comments
A grand rounds speaker showed videos of patients with epilepsy and contrasted them with patients with functional seizures. One of the patients with functional seizures fell out of bed—head first—and the room roared with laughter. A physician seated behind me muttered, “These patients will do anything to sell their episodes.”
The Clinician’s Feeling Helpless or Inadequate
I think physicians resent patients who have problems they don’t know how to fix. And FND is a big black box. I think physicians may feel they do not have time or bandwidth to help individuals with FND because they feel unsupported, have limited resources, or are working in an institution with no experts in FND across disciplines.
I think there’s both the stigma that “it isn’t really a neurological problem” and, frankly, a self-protective response to the helplessness we can feel in the face of FND. When I was training, the emergency room wanted to admit a patient to us who couldn’t walk (due to FND). I pushed back, rationalizing, “This is not our problem. This is not really a neurological problem.”
A neurological colleague felt affronted when a child’s seizures, which we had treated as epilepsy, turned out to be functional—as if the child had knowingly pulled the wool over his eyes. It was easier to feel angry with the child than to manage his own feelings.
Over time, I have actually become pretty good at diagnosing FND. The problem is that I still have no skills or abilities or resources to manage some of the issues and stressors that the patients tell me about. I feel helpless. That is my fear and peril when I find FND.
3. Understanding the outdated culture
The above stories paint a picture of the outdated culture, created largely by the medical profession in reaction to a clinical problem—FND—that did not fit neatly into the traditional orientation of medical education and clinical practice toward organ systems, recognizable lesions, and structural defects [16], [17]. The strong emotional responses embedded in the stories are palpable. Clinicians working in the outdated culture experience a complex mixture of feelings1 when faced with the problem of FND: a sense of helplessness; feeling out of their depth; feeling threatened, overwhelmed, or fearful; feeling irritated, angry, affronted, or duped. In turn, the child (including adolescent) and her family respond to the clinical encounter by feeling offended, dismissed or discounted, helpless, and angry. In general, the child and family have not previously heard of FND, and their responses to the illness are shaped by the clinicians who undertake the assessment and treatment process. In the outdated culture, the child and family came to the clinical encounter seeking medical help and expecting an empathic response—but they often left the encounter distressed, angry, and stigmatized.
Text Box 1: The meaning of stigma
| Stigma refers to negative stereotyping, “a mark of disgrace associated with a particular circumstance, quality, or person” (Oxford English Dictionary). Iatrogenic stigma—a subset of public stigma [12], [13], [20] —is the stigma imposed on the child and family during the child’s journey through the health care system. |
In human interactions, “Emotions are closely and intimately related to action by way of their nature as motivational states” (p 159) [21]. Put simply, human emotions guide behavior and decision making, and play a vital role in communication with others [18], [19]. Children are no exception. They are often skilled communicators who have, among other things, spent their very early years mastering nonverbal modes of communication. They continue to use, and to rely on, these same modes of communication well after they start using language. In the stories presented above, the clinicians’ underlying emotions—alongside their attitudes and beliefs, including the “disease prestige rank” they allot to the illness [17]—are enacted and transmitted to the child not just by the choice of language, but via facial expression, body posture, mannerisms, tone of voice, and behavior [22], [23]. The child and family pick up the clinician’s verbal and nonverbal communication, and are either soothed, encouraged, and contained by it (positive communication) or distressed, discouraged, and hurt by it (negative communication). In the former scenario the clinician mitigates potential stigma, whereas in the latter scenario, the clinician imposes or reinforces stigma on the child and her family (see Text Box 1). In this way the clinician plays a pivotal role in the child’s experience of her illness and shapes the role that stigma plays—or does not play—in that experience.
The culture of care we saw in the opening stories is confronting and difficult to face. But as James Baldwin, the writer and social critic, noted in “As Much Truth as One Can Bear” (an essay recently brought to light in a 2021 Lancet Psychiatry article, “Stigma in Practice,” [24]),
“Not everything that is faced can be changed, but nothing can be changed until it is faced.” [25]
From the perspective of our multidisciplinary group of professionals, the most pressing issue in the field of pediatric FND is to bring about change in the culture and to develop an FND-informed culture of care so that it reflects current neuroscience research and consciously addresses past prejudices. Pervasive stigma is also a problem in relation to adult patients with FND [9], [11], [12], [13], [14]. Without cultural change, the clinical treatment of FND cannot progress, and patients will continue to receive a different standard—a lower standard—of care. Until the clinicians and institutions directly tied into patient care embrace these new understandings of FND, the beliefs and attitudes at other system levels (policy, resource allocation, payment and billing systems, and research funding, as well as the beliefs and attitudes of the person on the street) cannot and will not change. The beliefs and attitudes of clinicians—including the family doctor, ambulance paramedic, emergency room nurse or doctor, pediatrician, medical student, and clinicians working in psychological services—represent a nodal point for intervention and achieving change.
4. Using language that does not offend
The use of child-friendly language—coupled with appropriate caregiving behavior and nonverbal communication—is the cornerstone of pediatric practice. The influential pediatrician and therapist, Donald Winnicott, used the term holding environment to refer to the creation of a therapeutic environment in the treatment setting that enables the child to feel emotionally supported, thereby enabling further “emotional growth in which the character builds up positively” (p 209) [26].
In the field of FND, creation of the holding environment includes a deliberate effort by the clinician to use language therapeutically—in a way that strengthens the therapeutic relationship, that enables the child to both understand and accept the FND diagnosis and accompanying formulation and treatment plan, and that steers the child toward health-promoting thoughts, actions, and outcomes [27]. While the academic task of reaching agreement about terminology is still ongoing [28], [29], children with FND have given clear feedback—both via research [30] and in the clinical setting [23], [31]—about terminology that they find offensive and unhelpful (see Text Box 2). When clinicians use offensive terminology, the child experiences distress, anger, shame, powerlessness, and so on. The clinician thereby activates negative processes that rupture the therapeutic relationship—the trust bestowed on the clinician by the child—and that steer the child toward illness-promoting thoughts, actions, and outcomes. It is therefore not surprising that the child, along with the family, may become defensive and invest significant energy in resisting the offensive diagnosis, formulation, and treatment plan, and in communicating a desire to withdraw from the relationship with the offending clinician.
Text Box 2: Language that children find offensive
| Term | Example of use | Reason why the child finds the term offensive | Alternate language options |
|---|---|---|---|
| Psycho (prefix) | Psychogenic, as in psychogenic non-epileptic seizures, psychogenic tremor, and so on | In everyday slang, psycho means crazy or mentally ill, and the child interprets the clinicians to be telling her that she is crazy or mentally ill. | Non-epileptic seizures (without the “psychogenic” prefix) Functional seizures Functional tremor |
| Pseudo (prefix) | Pseudoseizures | The child may interpret the clinician’s use of pseudo as communicating that her that her seizures are “fake” and that she is “faking” the seizures. | Functional seizures Non-epileptic seizures (without the “psychogenic” prefix) |
| Behavioral | The FND symptom is described as being “behavioral” | In everyday slang, behavioral means naughty or bad behavior, and the child interprets the clinician as telling her that she is naughty or bad or that she is doing it on purpose. | The symptom can be described as functional: reflecting dysregulation within the nervous system—rather than a problem with structure—and requiring mind–body interventions that restore regulation and normal function. The symptom can be described as functional: reflecting activation of the stress-system and disruption of normal motor function, as a result of physical, emotional, or cognitive stress* (see explanation given in text). |
| Psychological | The FND symptom is described as “psychological” | The child may interpret that the clinician as telling her that her symptoms are “all in the mind” or “all in the head” and that she is making them up. | The symptom can be described as functional: reflecting dysregulation within the nervous system—rather than a problem with structure—and requiring mind–body interventions that restore regulation and normal function. The symptom can be described as functional: reflecting activation of the stress-system and disruption of normal motor function, as a result of physical, emotional, or cognitive stress* (see explanation given in text). |
* It is very important that the clinicians highlight that when he/she uses the term stress he/she is referring to both physical and psychological factors. Physical stress commonly includes illness (e.g. viral illness), injury (e.g. fall), or medical procedures: all of which can activate the brain-body stress system(s). Emotional stress commonly includes difficulties with friends, academic stress, stress in the home setting due to conflict or other issues, and uncommonly various forms of maltreatment: all of which can activate the brain-body stress system(s). Cognitive stress involves thoughts, images, emotions, and memories, that function to activate the brain-body stress system(s) in a top-down manner.
By contrast, an FND-informed conversation using language that is therapeutic communicates both knowledge and respect and strengthens the child’s sense of being understood and emotionally supported.
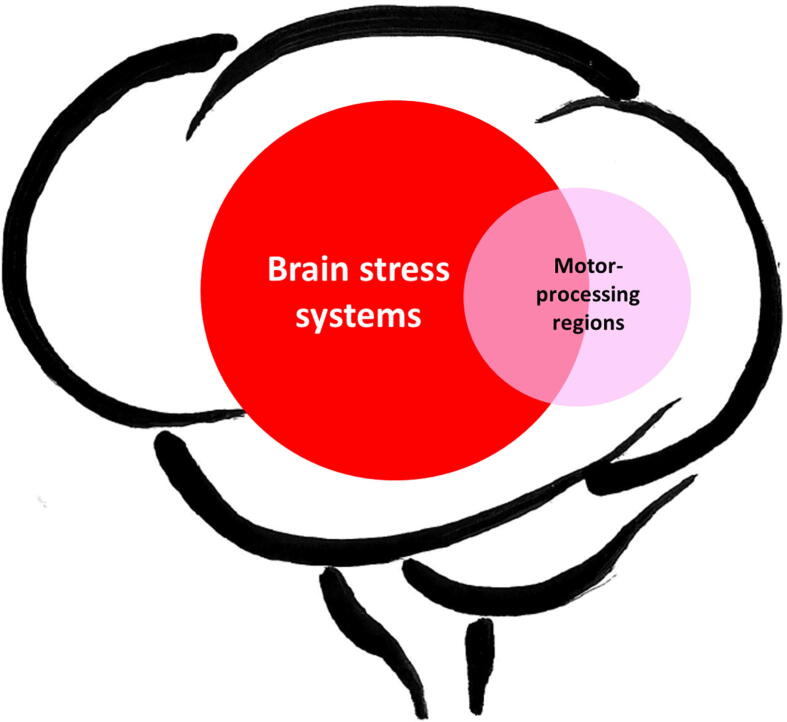
[Said to the child with leg weakness and her family] Thank you for giving me such a comprehensive account of your story [= developmental history]. I know the neurology doctor gave you an explanation of FND, but I think that this is a good time to go through it one more time. Here is a picture showing you what happens (see Fig. 1). It is a simple summary of the emerging neuroscience research. The red ball represents the brain stress systems—the parts of the brain that activate with stress. When the red ball becomes too big and too strong it can disrupt motor function (depicted by the pink ball). In your case the horrible bullying at school, the loss of your best friend, the worry thoughts about your mum’s health, and the feelings of anger and sense of rejection that you have experienced in your relationship with your dad, have all been activating the red ball.2 The fall you had last week was the last straw. The fall activated the red ball even more and triggered the FND illness. To help you get back to health, we will need to do physiotherapy to help get your legs going again [point to the pink ball], and we need to do some mind–body work to help you manage the stress from the bullying, to help you manage the worry thoughts about your mum, and to help you and your dad repair your relationship. And we shall also need to talk to your school to make sure that they put a stop to the bullying. All of this together will help your stress system settle down—the red ball to get smaller—and will help your symptoms go away. Does that make sense to you?
Fig. 1.
The visual metaphor used in the explanation to the child. ©Kasia Kozlowska 2017 (for other metaphors see Kozlowska and colleagues, 2020) [23].
The collaborative process of co-constructing a formulation—based on the developmental history given by the family and child—helps to build a strong therapeutic relationship and enables the child and family to accept the diagnosis and to be active in developing a treatment plan based on the co-constructed formulation [32], [33]. For a more detailed account of the diagnostic process (including history taking, giving the diagnosis, and explaining the diagnosis), as well as the biopsychosocial assessment and formulation co-constructed with children with FND and their families, see Kozlowska and Mohammad (forthcoming 2021) [34].
5. The referral process: educational and structural interventions to promote change
One barrier to effective treatment is that many referrals for FND treatment come without an official diagnosis. Consequently, before embarking on any intervention, the clinician has no choice but to track down the referring pediatrician to discuss the diagnosis, to clarify which symptoms the provider considers to be functional, and to clarify what—if anything—the child and the family have been told about the name and etiology of their illness. In each of our respective health care systems, we, the multidisciplinary team of authors, have addressed this issue—the inadequate referral process from the pediatrician to psychological services—by implementing a variety of educational and structural interventions (see below).
5.1. Educating the referring pediatrician
When working with pediatricians (or physicians3) who are not locked into the outdated culture, who are keen to work in a collaborative way, but who have not quite mastered the challenges of providing accurate, direct diagnoses to children and their families, it is helpful to provide education and training regarding the benefits of making the FND diagnosis and explaining it to the patient and family. Educational interventions can include any of the following: the observation of, and comments on, particular clinician-child encounters; training sessions that model clinical skills; grand rounds presentations; didactic sessions and resources for trainees; updates about research findings and etiological models; and pediatric rotations within psychological services [8], as well as efforts to conduct research using multidisciplinary teams (see Text Box 3). Continuous and far-reaching educational initiatives that both educate and empower clinicians (and patients) will facilitate cultural change across time and across generations of clinicians [35]. Pediatricians will become skilled at providing and explaining positive diagnoses of FND and at organizing treatment interventions that include the necessary referrals to psychological services, physiotherapy, occupational therapy, speech therapy, and so on.
In Text Box 3 we summarize a broad range of educational interventions that can be implemented across clinical fields to increase understanding of FND and to change beliefs and attitudes within the broader health care system.
Text Box 3: Educational Interventions That Can Be Implemented Across Clinical Fields to Increase Understanding of FND and Respect for Patients (Child and Adult) Who Suffer from This Complex Disorder
| Educational Modality | Intervention Description |
|---|---|
| Health care training program curricula (e.g., nursing, paramedics, medicine, psychology, physical therapy, occupational therapy, speech therapy) | Lectures on functional somatic symptoms—including FND—need to be included in all curricula to signal that functional presentations are common within the health care system and represent a substantial proportion of practitioner workload. |
| Postgraduate student rotations (e.g., nursing, paramedics, medicine, psychology, physical therapy, occupational therapy, speech therapy) | Inclusion of functional disorders—including FND—in clinical discussions pertaining to assessment, differential diagnosis, and treatment of patients. Provision of educational materials when patients with functional disorders present (e.g., Functional Somatic Symptoms in Children and Adolescents [23], when working in the pediatric setting). |
| Hospital-based continuing education programs | Grand rounds and inbuilt continuing educational programs (in the emergency department, neurology, pain team, consultation-liaison team, physiotherapy, occupational therapy, speech therapy, and wards that manage patients with FND) all present ongoing educational activities. |
| Conference-level education | The Functional Neurological Disorder Society (FNDS, https://www.fndsociety.org) has set up bi-yearly conferences to promote education. Neurology, neuroscience, psychiatry, psychology, occupational therapy, speech therapy, nursing, and paramedic conferences provide other venues for conference-level education. Conference-level education should also include all medical subspecialties. For example, gastroenterologists, respiratory physicians, and otolaryngologists all see patients with functional communication, swallowing, cough, and related disorders. |
| Peer-reviewed literature | A concerted effort has been made to publish clinical neurology handbooks [36], consensus criteria, expert opinion articles, updates on etiology, assessment, and treatment of FND subtypes [23], [37], [38], [39], [40], and articles describing the clinical assessment process [41], [42]. |
| Use of video teaching resources within all levels of education | Video teaching resources can be helpful in teaching about patterns of presentation, the neurology examination, and interviewing skills. |
| Supervision of clinicians/provision of second opinions | Supervision of clinicians, discussion of cases, and provision of second-opinion consultations for difficult cases via a variety of modalities (face to face or via telephone, telehealth, site visits, or ambulant teams). |
| Miscellaneous resources that clinicians from all fields can use for patients | FND website written for patients by neurologist Jon Stone: https://www.neurosymptoms.org Educational resources available via the Functional Neurological Disorder Society (FNDS): https://www.fndsociety.org American Epilepsy Society Task Force Handout on PNES for Mental Health Professionals: http://www.aesnet.org/docs/default-source/pdfs-clinical/5-pnes-for-mental-health-profs-final.pdf?sfvrsn=d8f1bbf5_2 A comic book—“Not There: A Story of Functional Neurological Disorders”—written for young adults [51]. |
| Resources pertaining to costs of FND for use in education and lobbying of administrators, government bodies, and insurance companies | FND as a common disorder (approximately 16% of neurology outpatient visits and up to 23% of patients in epilepsy clinics) [43], [44]. FND and other presentations with functional somatic symptoms are both common and costly [45], [46], [47]. Investment in recently developed treatment interventions (including those for functional seizures) is worthwhile because the interventions have good outcomes [48], [49], [50]. Insurance providers do cover health care costs associated with FND [52]. |
5.2. Structural interventions that support an adequate referral process
When pediatricians are anxious about providing FND diagnoses to their patients—for example, the pediatricians perceive themselves as not having the necessary skill set or are locked into the outdated culture—structural interventions within the medical system may help to ensure that pediatricians make the requisite FND diagnoses. Within some health care systems, it may be possible for clinicians working in psychological services to collaborate with their information technology (IT) departments to develop a referral pathway in the electronic medical record (EMR) requiring the referring pediatrician to enter a specific diagnosis of FND in order to trigger treatment by psychological services or allied health professionals [53].4 Additionally, if a referring pediatrician continues to struggle with the task of explaining the diagnosis, the EMR can—once the diagnosis has been entered—automatically send a video or information sheets explaining the FND diagnosis and treatment process through the patient portal. Likewise, if the child is in hospital at the time, the EMR can prompt the pediatrician or nurse to play the video for the child and family prior to discharge. The FND treatment team can also use the EMR system to request the referring pediatrician to make referrals to physical, occupational, or speech therapy, if deemed necessary.
For referrals to psychological services from outside the health care system—where an EMR pathway may not be an option—developing a referral form that needs to be completed by the referring pediatrician (or intake officer) can be helpful. Required criteria for referral to the treatment team may include the following: confirmation that the pediatrician has formally made a diagnosis of FND (or other functional disorder) and has communicated the diagnosis to the child and the family; information pertaining to the child and family’s acceptance of the diagnosis; a description of the symptoms that are considered functional; documentation of diagnostic testing (e.g., EEG, EMG, or MRI, as appropriate), and clarification of the child’s general medical status (including a list of symptoms that are due to any comorbid medical diagnosis).
5.3. Broader educational initiatives
Students learning the clinical sciences are tomorrow’s physicians, psychologists, and allied health professionals. In this context education about FND—and other functional disorders—needs to be integrated into professional health education curricula (e.g., medicine, nursing, psychology, other allied health professions) and also into postgraduate and continuing medical/health education programs (see also Text Box 3).
6. Brain, mind, and body: Reconceptualizing FND
Fragmentation of the health care system into services that treat the body and services that treat the mind—a reflection, in contemporary medicine, of Descartes’ mind–body dualism—has been one of the main barriers to effective treatment of pediatric FND. What this means in daily clinical practice, at least within the outdated culture, is that children with FND have fallen between the cracks. Pediatricians have commonly perceived FND as a psychological disorder (disorder of the mind) that, for lack of a physical or medical basis, needs to be treated by clinicians working in psychological services. And when referred, in turn, to psychological services, the child has typically failed to meet the intake criteria—because the presenting symptoms are physical rather than psychological. In this way, many children and families have been left in a treatment limbo, with neither the pediatrician nor the clinician working in psychological services being willing to “own” the problem and to “take on” the child’s clinical care. In the subsections that follow, we try to highlight some nodal points for bringing about cultural change, enabling us to move past this ongoing dilemma in addressing the needs of patients with FND.
6.1. A change in thinking: FND as a disorder of brain, mind, and body
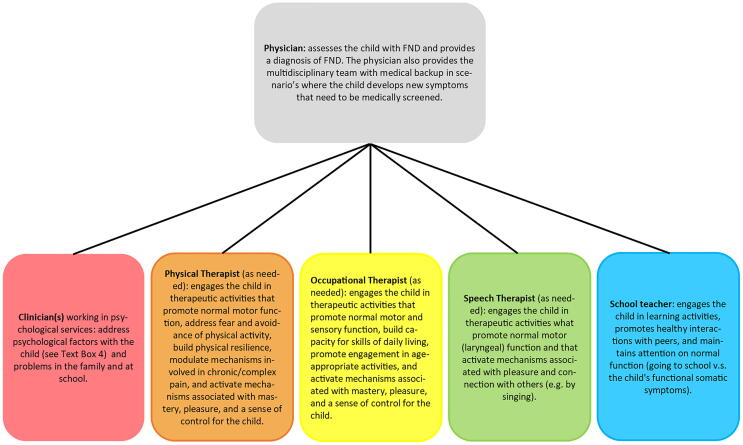
A change in thinking and in how FND is conceptualized by clinicians across all disciplines—by the paramedic, nurse, pediatrician, psychiatrist, psychologist, physiotherapist, occupational therapist, and speech therapist—is key to changing the treatment culture. Innovative teaching efforts based on contemporary research may facilitate this change in thinking. For example, the emerging picture from neuroscience research is that FND is a neuropsychiatric (mind–body) condition that involves complex interactions between brain, mind, body, and context—the lived experience of the child and the family. FND reflects the activation of brain regions that underpin salience detection, arousal, pain, and emotional states [3], [5], [54], [55]. These regions, collectively referred to as the brain’s stress system or emotion-processing regions, are commonly activated in the context of stress (the psychological-arousal component of FND). And because these emotion-processing regions are over-active and over-dominant, they over-connect with motor- and sensory-processing regions and disrupt motor and sensory function (the physical, motor-sensory component of FND) [3], [5], [54], [55]. Given that FND thus involves both psychological and physical components, treatment needs to address both dimensions. Psychologically oriented interventions target emotional, cognitive, interpersonal, and physiological regulation processes, all of which function to activate the brain’s stress systems, and to trigger and maintain symptoms. Physical therapy interventions—when required (see Fig. 2)—target motor and sensory processes and the focus of attention, with the aim of reestablishing normal motor and sensory function.5
Fig. 2.
This figure represents the multidisciplinary team. A physician, clinicians from psychological services, and staff from the child’s school are included on every team. A physical therapist, occupational therapist, speech therapist, and other allied health professionals (e.g., art, music, and recreational therapists) join the team as required. ©Kasia Kozlowska 2021.
The implication for clinical practice is that the diverse range of clinicians caring for children with FND—including pediatricians, nurses, and clinicians working in psychological services, along with physical, occupational, and speech therapists—need to see FND as a part of their professional mandate. And each of them needs to see themselves, in the context of a multidisciplinary intervention, as being responsible for managing one component of that intervention (see Fig. 2).
6.2. Understanding the somatic narrative: the language of the body
Understanding the somatic narrative—the language of the body and the story it is telling about what is happening to the child—is crucial to understanding and treating pediatric FND. For these children, the somatic narrative potentially includes the following neurophysiological processes and any associated symptoms: activation or dysregulation of the stress system (e.g., upregulation of the autonomic nervous system and increases in cortical arousal) [49], [54], [55], [56]; changes in homeostatic setpoints (e.g., lowering of pain thresholds and changes in regulation of PCO2 secondary to hyperventilation) [57], [58], [59]; activation of the body’s protective (alarm) systems (e.g., pain and fatigue) that signal a need for protective action [60], [61]; and changes in neural networks (see previous subsection). The narrative also includes the positive signs (e.g., entrainment of tremor or incongruity and reversibility of voice or other motor symptoms) that distinguish functional neurological symptoms from other neurological conditions [37], [38] and that reflect the disruption within and between neural networks controlling emotion processing and motor and sensory processing (see previous subsection). In sum, the somatic narrative provides the pediatrician with valuable information about changes in the child’s body function in response to stress, threat, or danger, whether actual or perceived.
Unfortunately, with the advent of scientific medicine and a reliance on technology, pediatricians came to focus exclusively on the signs and symptoms that mark organic disease. Teaching about the somatic narrative—including the “rule-in” signs and symptoms for functional somatic disorders—largely disappeared from medical textbooks, medical and psychiatric curricula, and formal and bedside teaching [62], [63]. As a consequence, many children are diagnosed with FND long after their bodies began signaling, in many different ways, the emerging neurophysiological dysregulation. Because the symptoms had not been heeded in earlier visits to the doctor, a functional diagnosis has not been made; the connection between the emerging symptoms and the challenges in the child’s life had not been recognized; the window for early treatment had been lost; and the progressive dysregulation within body systems ultimately resulted in FND [64].6
7. The treatment process: educational and structural interventions to overcome mind–body dualism
7.1. Designing joint services: psychology within the neurology service
In many cases, children with FND initially present to the emergency room followed by review by the neurology department and potentially its specialized services or clinics (e.g., epilepsy services, movement disorder clinics, or tic clinics). From that starting point, the child and family would be well (and efficiently) served if multidisciplinary, FND-informed psychological and allied health services were embedded within the neurology department. Embedded care has multiple advantages. It can increase acceptance of the FND diagnosis by the child and family, limit the experience of being dismissed or discharged into an uncertain treatment future, and facilitate access to clinicians familiar with FND treatment. Once the right resources are in place, collaboration among clinicians is easier to promote and maintain, and hospital administrators are more likely to recognize the efficiency and resulting cost savings of embedded practice. These collaborations can serve, in turn, as models for standard practice or for structuring clinical care pathways, potentially leading, more broadly, to programs with improved diagnostic accuracy and better treatment outcomes [49].
7.2. Partnerships among disciplines
Another structural intervention—one that needs to be supported by administrators and budget allocation—is to establish and maintain partnerships among disciplines where the ownership of children presenting with FND is a joint endeavor. The partnership may be cemented within a clinic—involving medical specialties, psychological services, and allied health—or it may exist in the form of a virtual clinic, where the partnerships are maintained without the clinic frame. Strong interdisciplinary partnerships among disciplines strengthen numerous objectives. They (1) greatly enhance the health system’s ability to take on, treat, and manage children with FND and also, importantly, to manage children with chronic symptoms and severe comorbidity; (2) enable individual clinicians to feel supported in their confidence to attempt treating difficult cases; (3) provide a space for various specialties to consult, educate, and advise each other, and (4) enable the specialists involved to share problem-solving responsibility while navigating diagnostic and treatment hurdles and the ethical challenges encountered at various junctures in the assessment and treatment process.
8. Reframing the clinical intervention I: Psychological services
Clinicians who work in psychological services can contribute to the change in culture—and can help to ensure that children with FND receive appropriate treatment—in four important ways.
8.1. Core responsibilities as including children with FND
In many settings, intake criteria for psychological services are operationalized along dualistic lines. Children with anxiety, depression, suicidal ideation, risk of self-harm, psychosis, and other mood disorders are included, but children with FND and those with other functional somatic disorders are excluded—a key barrier to effective treatment. As a first step, clinicians can work on revising clinical guidelines and intake criteria to ensure that FND is included as a core concern for psychological services and part of their professional mandate. Revised intake criteria may also need include a broader construction of risk beyond the risk of harm to self and others (in connection with psychological disorder), and to include risks associated with physical disability and school absenteeism (as the sequelae of functional somatic symptoms). After all, in both scenarios the child’s developmental trajectory is derailed, and long-term health and social outcomes are adversely affected [65].
8.2. Going beyond the psychological construct
As a second step, because the somatic narrative is, in effect, the language through which the body speaks, it becomes the language in which children who present with FND—and other somatic symptoms—speak to their clinicians: “Here is my body, speaking.” Clinicians, including those working in psychological services, need to understand this language and to respect its centrality in treating patients with FND (see above). And they need to understand how these narratives can be integrated into a biopsychosocial (systems) framework that takes into account the body, emotions, cognition, and events in the family and school, along with the ongoing interactions between them. This change in perspective is important because most children with FND do not relate well to psychological constructs as such, and they have low levels of insight into psychological functioning [66], [67]. For example, on face-to-face clinical assessment, the child with FND with comorbid anxiety or depression7 will typically smile and deny the symptoms of anxiety, depression, and psychological distress. The child may answer in the negative when asked (using a psychological construct) if she has ever experienced a panic attack, but she may answer in the affirmative when asked (using body-based language to explore the patient’s somatic narrative) whether she has ever experienced her heart pounding, feeling sweaty, butterflies in her stomach, nausea, or wanting to vomit—the physical symptoms of a panic attack. Or alternatively, a child may deny feeling depressed—she does not have the subjective experience of feeling depressed—but when her mood is tracked on a 0–10 Likert scale, she may report that it has dropped from an 8/10 to 4/10 in the context of bullying at school.
Likewise, self-report and parent-report questionnaire measures looking at the full range of psychological disorders—which are typically designed using psychological constructs—typically yield negative findings: the child does not meet the questionnaire’s clinical cutoffs for a psychiatric disorder [66], [67]. Therefore, to work with children with FND, clinicians may need to use language and visual tools that resonate with the child and that help the child communicate her actual subjective experience in response to life challenges. For the same reasons, the screening tools themselves need to incorporate body-centered framing—rather than exclusively psychological constructs [66].
8.3. Understanding the role of illness-promoting psychological processes in FND
As a third step, it is important that clinicians recognize that illness-promoting psychological processes are common in patients with FND. In the pediatric setting, an emerging body of work assessing psychological and interpersonal functioning has identified maladaptive patterns in the interpersonal, emotional, and cognitive domains. Assessments of attachment classify children with FND (vs. healthy controls) into at-risk patterns of attachment with high rates of unresolved loss and trauma [68], indicating a long-standing history of relational stress. Personality testing using the Millon Adolescent Clinical Inventory shows high levels of psychic tension, anxiety, depressive affect, and maladaptive personality traits (reflecting maladaptive patterns of coping) [49], [67]. And on the clinical level, effective treatment programs involve a psychological component that targets illness-promoting psychological processes [23], [48], [49], [67]. Such illness-promoting psychological processes include recurring cognitions, emotions, and memories that activate the brain’s stress systems through appraisal-based, top-down pathways [69] (see Text Box 3). What we see here is that the human mind can generate or maintain cognitions, emotions, and memories that can, in and of themselves, function as cognitive stressors. These psychological processes are important to recognize because they can not only compromise the child’s ability to engage in treatment, but distort their expectations of the treatment outcomes (and the outcome itself) and cut off support from family and other social systems that could help sustain the treatment process.
Text Box 4: Illness-Promoting Psychological Processes That Are a Common Target of Psychological Treatment Interventions When Working with Children with FND and Their Families © Kasia Kozlowska and Blanche Savage 2021
| Psychological process | Explanation/example of the psychological process |
|---|---|
| Attentional processes | |
| Attention to symptoms | Attention to symptoms—by the child or the parents—worsens FND symptoms and amplifies subjective pain. |
| Cognitive processes and expectations | |
| Catastrophic* symptom expectations | Thoughts about the symptom lead to a catastrophic outcome. For example, in response to a muscle spasm and a new pattern of pain in the back—in a boy with motor weakness in the legs and left arm—thinking over and over again, “What is wrong now? How bad is it going to get?” coupled with a visual image of his body being completely paralyzed. |
| Low sense of control (predictability) over symptoms | Thoughts—coupled with feelings of helplessness— that highlight the child perceived lack of control. For example, “It just happens out of the blue.” |
| Negative expectations pertaining to treatment interventions | Negative expectations (nocebo effect) are set up in the context of catastrophic symptom expectations and thoughts/feelings associated with a low sense of control. Negative expectations can undermine the efficacy of strategies that the child needs to learn to manage the symptoms. |
| Low sense of control (and predictability) with regard to events or expectations in the home or school setting | Thoughts that underline the child perceived lack of control. For example, “It’s too hard. I can’t do it. I hate school. They all think I am stupid.”—coupled with feelings of helplessness. |
| Catastrophic thinking (pertaining to self, symptoms excluded) | If I don’t get everything right now (in the upcoming test), I’ll never be able to become a surgeon. |
| Catastrophic thinking (pertaining to non-self) | For example, ruminating thoughts about the ecological stress that the earth is under, as in ”When the glacier melts, we shall have no water, and we shall all die.” |
| Perfectionistic thinking | For example, “I did not reply to my brother’s text because I could not get my text right.” Or “I only got 98% in the math exam” (associated with a feeling of disappointment and sadness). |
| Self-critical rumination** | Beating oneself up over what one could or should have done. For example, when a child with FND says, “I haven’t tried hard enough. It is my fault I am in hospital. I should have tried harder and done better.” Or “The money my parents are spending on my treatment means my family is missing out.” |
| Obsessive thinking | Unable to switch thought processes away from a certain idea or worry. For example, an adolescent girl with FND was obsessed with the accuracy of her diagnosis. Each morning at ward rounds she grilled her team about her diagnosis, including the pros and cons of formally including other diagnoses on her chart: fibromyalgia; postural orthostatic tachycardia syndrome; complex/chronic pain; irritable bowel syndrome; and so on. |
| An exclusively negative focus regarding the future, coupled with the inability to be in the present and to celebrate progress in the here and now | For example, an adolescent girl who had presented with leg paralysis, cognitive impairment, and functional seizures complained that everything was getting worse, that her occasional drop attacks made life impossible. She forgot to mention—or celebrate—that she was now dancing around the house and that her cognitive capacities had returned. |
| Pushing difficult thoughts out of mind (cognition avoidance) | Attempting to manage worries and difficult thoughts—and the associated emotions—by pushing them out of mind. For example, an adolescent girl did not tick the questionnaire item pertaining to family conflict. When asked why, she explained that her father—with whom she was in sharp conflict—was no longer part of her family. |
| Feeling-related processes (especially emotions that are unacceptable to the self or in the family system) | |
| Feeling overly responsible | For example, feeling compelled to act as a confidant and mediator in the school setting to settle distress felt by others or to sort out disputes between friends. Or taking responsibility to keep younger siblings safe while an older sibling is out of control or while parents engage in conflict. |
| Feeling worried | For example, chronic worries about schoolwork, friendships, or parental well-being. |
| Feeling sad | For example, experiencing sadness or a low mood but not being able to admit and share these feelings with attachment figures. |
| Feeling anger | For example, experiencing anger but not being able to admit and share feelings of anger. |
| Feeling guilt | For example, feeling guilt about asking for help or for taking up a hospital bed, or about feeling sad or worried. |
| Feeling helpless/hopeless about the situation | For example, “Nothing will work. No point trying.” —and so on. |
| Pushing difficult feelings out of mind (feeling avoidance) | For example (and most commonly), pushing anger out of mind. |
| Feeling-related processes (feeling homeostatic emotions) | |
| Disconnecting and the inability to track body states (homeostatic emotions) | Inability to track any change in body state marking increased arousal or distress (e.g., respiratory rate, butterflies in the stomach, changes in tension). For example, an adolescent with leg weakness and panic attacks repetitively stated that she loved school and that school was not stressful despite a relapse of symptoms every time reintegration to school was attempted. |
| Attachment-related processes and behavioral processes | |
| Fear and avoidance of activities | For example, avoidance of exercise because it exacerbates pain and can trigger autonomic system activation (such as a panic attack). |
| Being unable to tell parents that not all is well. | For example, not being able to tell parents about feelings of sadness or anger, or about the experience of being worried, overwhelmed. |
| Not telling parents about what is happening to the child to protect (not burden) parents. | For example, not telling parents about bullying, and trying to manage it all by oneself (but being unable to) in an effort to protect parents from becoming too stressed. |
| No being able to ask for help. | For example, from the teacher, thereby perpetuating problems at school. |
| Amplify signals of distress to activate caregiving behavior from parents (others) | For example, a boy with an abnormal gait coupled with back pain who signals his distress via loud, lingering wails as he laboriously makes his way to hospital school room. |
| Unresolved loss, unresolved trauma, and unresolved bad experiences | |
| Intrusive thoughts/memories of the adverse event | For example, FND symptoms triggered on the anniversary of a parent’s death or past hospitalization, or when memories of an unresolved trauma are brought to mind in some other way. |
* To catastrophize means to “imagine the worst possible outcome of an action or event: to think about a situation or event as being a catastrophe or having a potentially catastrophic outcome” (Merriam-Webster’s Online Dictionary).
** Rumination (as a medical term) involves “obsessive thinking about an idea, situation, or choice, especially when it interferes with normal mental functioning[,] specifically: a focusing of one’s attention on negative or distressing thoughts or feelings” (Merriam-Webster’s Online Dictionary).
8.4. The biopsychosocial framework
As a fourth step it is important to acknowledge that addressing a broad range of psychosocial problems—including problems at home or at school—comes within the mandate of clinicians working in psychological services. For example, given that problems at school are a common source of stress for children with FND, a holistic, biopsychosocial evaluation of the child and family needs to carefully explore the role of such problems in the child’s presentation. Common difficulties include the following: cognitive difficulties; specific learning problems; feeling unable to cope; working too hard in the context of high expectations; social problems with peers; bullying; and school absenteeism (see Asadi-Pooya et al. [2021] for review) [14]. A biopsychosocial perspective is crucial because problems at school are affected by a variety of interrelated factors: personality; cognitive ability; expectations (others’ or one’s own); anxiety and other emotional problems; use of coping strategies; family function; social functioning more generally; and parents’ responses to their child’s complaints [14], [23], [70].
The outcome of the evaluation is a biopsychosocial (systems) formulation that will then be used to put together a treatment program addressing the specific needs of each particular child and family [23], [67]. While this way of working has been described in many different ways over the last few decades—including adaptive, appropriate, customized, holistic, patient-centered, personalized, targeted, or whole-person—clinicians who work in child and adolescent psychological services have long been using biopsychosocial formulations to inform treatment. And in the particular context of helping children with FND, clinicians need to develop and maintain expertise in constructing such biopsychosocial formulations and in case-managing children whose histories include multiple precipitating, perpetuating, and maintaining factors and whose treatment involves multiple components and multiple clinicians (in addition to themselves).
9. Reframing the clinical intervention II: Physical, occupational, and speech therapy
9.1. Psychologically informed physical and occupational therapy for children with FND
Physiotherapy is a core element of the treatment program for children with FND who present with motor symptoms or with deconditioning in the context of inactivity due to pain or functional seizures (see Text Box 5). Physiotherapy is also useful in treating chronic complex pain and in improving physical self-regulation. Because FND symptoms and complex/chronic pain are amplified by attention, standard musculoskeletal approaches to physiotherapy—where the focus of attention is specifically on the problem area—can make FND symptoms worse. In addition, the children’s presentations are complicated by psychological factors, including fear and avoidance of physical activities, that may affect their capacity to engage in the physiotherapy process. In this context, physiotherapy with children with FND requires a psychologically informed approach [71]. Such an approach prioritizes the establishment of a therapeutic relationship, creation of a safe space for physiotherapy, and a therapeutic process that fosters mastery, pleasure, and a sense of control for the child. The goals need to be achievable [71], [72], and the process needs to maintain an external focus—that is, on the outcome of the action and not on the action itself (e.g., “How high can you reach on the wall?” rather than “Straighten your back!”). That is, psychologically informed physiotherapy prioritizes indirect approaches that move the focus of attention away from symptoms and that emphasize the completion of tasks and activities that engage the sick or compromised body part indirectly [71], [73]. Occupational therapy with the child follows the same principles, and because it includes activities of daily living (e.g., cooking), occupational therapy also broadens the range of normative activities that can be offered as part of the child’s treatment program.
Text Box 5: The Role of Physical Therapy in the Treatment of FND—Including Functional Seizures—and Comorbid Conditions
Physical therapy—followed by a regular exercise program once formal physical therapy is terminated—with children with FND is useful for the following reasons:
|
9.2. Psychologically informed speech therapy for children with FND
The speech pathologist has a pivotal role to play in the diagnosis and treatment of functional voice disorders—in particular, when the child presents with functional aphonia (loss of voice), functional dysphonia (most commonly in adolescents with features of inappropriately high-pitched falsetto or unstable voice), anxious concerns about swallowing, choking phobias, or chronic symptoms of “habit,” “tic,” or “barking” cough [38], [78], [79], [80]. A biopsychosocial approach—if possible, in collaboration with the other members of a multidisciplinary team when possible—is important. The functional symptoms are distressing and disabling for the child. For example, having no voice at all can make it difficult for children to engage with others, to express themselves, and to talk about feelings, and for adolescents with dysphonia, hearing themselves talk with an unstable and unnaturally high-pitched falsetto voice can be very embarrassing and inhibiting. If the symptoms become protracted, they will have a significant impact not only on parents, siblings, and family life, but on school attendance and friendships.
The speech pathologist prioritizes the establishment of a therapeutic relationship and the creation of a therapeutic space in which treatment can take place. The assessment process itself involves a detailed psychosocial history and a formal oromotor/speech assessment (including elicitation of positive signs) [38], [79], [80]. In the process, the speech pathologist also creates a safe space for the child. She invites children to convey, in whatever way they can, any changes they have noticed in their speech, voice, swallowing, or cough; the circumstances that they recall being associated with the onset of their difficulties; and if they are able to talk about it, their current attitudes and beliefs about the nature of their difficulties and how this is affecting them now.
An 11-year-old girl choked painfully on a fish bone, which was followed by a terrifying episode of coughing and dry retching. Despite the fish bone being coughed out, and with no tissue damage to the throat, several weeks later she still felt “really scared” about eating, chewing, and swallowing, and believed all foods and beverages to be potentially painful or dangerous. Her parents reported that previously happy family mealtimes had become fraught events: the girl was fearful in anticipation of choking; her eating behaviors focused on nibbling tiny amounts of food; and the parents were distressed by their daughter’s weight loss and compromised nutrition.
Early intervention is important because it can facilitate a rapid resolution of symptoms. The speech pathologist engages the child in pleasant and collaborative tasks and activities—parallel play, artwork, music, or singing—to facilitate automatic patterns of sounds, words, and movement. It is in the context of “make believe” or creative endeavors that the child can be encouraged to make early vocal and preverbal sounds or exaggerated animal noises. And through this joint play with the child, the therapist can help shape the child’s vocalizations into the long-familiar, automatic utterances involved in such things as counting and nursery rhymes—which can then be gradually transitioned into easy, relaxed verbal exchanges. The preverbal noises and automatic utterances are typically less threatening because they free the child from needing to formulate thoughts and ideas in complex language. Playful interactions and vocalizations obviate/counteract the activation of the brain stress systems that triggered the symptoms in the first place (as described in subsections above). This approach can also potentially distract the child’s attention away from the child’s particular symptoms, potentially triggering normal phonation, albeit inadvertently.
A five-year-old girl presented with a functional aphonia after being involved in a car accident one month prior. Her mother, who was driving, was seriously injured at the time and was unable to respond to her daughter’s crying and her calling out to the mother from the back seat. After the police and ambulance personnel extracted the girl from the wreckage, she was unable to speak using her regular voice, though she could whisper softly. Therapy activities involved gently connecting with the child in a way that placed no pressure on her to talk about the emotionally stressful accident. Together the child and therapist created a playful drama with hand puppets, encouraging the characters to make playful sounds and humorous animal noises as they interacted with one another. When this was happening easily and spontaneously, the sounds were extended into singing musical notes and then phrases, eventually ending in shared laughter at the antics of their puppet people. These non-threatening activities helped this little girl “to find her voice” again, which then enabled her to talk about the overwhelming fears that her mother may have died in those moments when she could not hear her mother’s voice.
Through such interventions, and with time, the child regains voluntary control over the initiation and maintenance of voice and movements. The speech pathologist then supports the child (and family) to generalize these gains beyond the clinical setting into the wider social context. For instance, when a young girl has overcome her fears of choking during swallowing, it can be effective to invite a close friend into a therapy session, and to chat together while sharing an informal snack and drink. Similarly, some adolescents with dysphonia (e.g., falsetto voice) feel extremely self-conscious about their new age-appropriate deeper voice, which may be a full octave below their previous voice. This sudden change can be confronting to their personal identity and sense of self. Here it will add to a boy’s confidence if he can pick out a friend with whom he feels “safe” and invite the friend into a session.
The speech pathologist also helps to create the space needed for conversation and ongoing therapeutic work. This part of the intervention—conducted by either the speech pathologist or, especially later, another therapist—addresses the psychosocial issues identified by the child or parents as predisposing or precipitating factors. It also aims to identify other factors that are operating to maintain the child’s symptom patterns. In this latter context, it may be important to address any unrealistic expectations, attitudes, and beliefs that the child or family may have about their various symptoms or what is maintaining them. Notably, it is often only after normal voice has been restored that the child may use the therapeutic space to talk about sensitive issues—which then enables a more effective, stable resolution to be achieved [80].
10. Limitations
The authors of this manuscript all work in, and come from, English-speaking countries (Australia, Canada, and the United States) or from Europe (Norway). In this context some of our suggestions pertaining to language may not be accurate for other cultures and countries. For example, we are aware that in some Spanish-speaking countries, there are psychological descriptors—e.g., “ataque de nervios”—that can be applied to functional seizures that are well conceptualized and well accepted in the community [81].
We are also aware that the countries that we work in are relatively highly resourced in comparison to some other countries. In this context, some of the interventions that we have described and implemented in our own settings—for example, those involving the information technology department (IT) or the management of referrals to psychological services—may not be attainable elsewhere. Potential barriers include the following: complications pertaining to catchment areas; limitations due to medical insurance; extensive waiting lists; insufficient psychological resources/professionals; resistance on the part of professionals working in psychological services who are not informed about FND; and so on.
The issue of funding in health care systems is an important one, and we were only able to touch upon it briefly (see Text Box 3). Change within medical systems—including the development of an FND-informed culture of care—is dependent on funding and on investment of both institutions and providers. In turn, funding issues are best discussed when there is clear evidence available pertaining to the costs of not treating (the cost of chronicity) and the near- and long-term cost savings associated with best-practice treatment interventions. Evidence regarding both of these factors is beginning to emerge, and more studies undertaking financial analyses and looking at treatment outcomes will facilitate the education and lobbying of health institutions and government bodies.
Finally, as members of a multidisciplinary team of professionals who treat children and adolescents, we have focused our analysis and discussion on pediatric practice. We are aware, however, that the same issues apply to adult practice, and we hope that adult clinicians will apply some of the thoughts and ideas presented in this article to their own clinical practice.
Conclusion
There is a pressing need to change the culture of care for children and adolescents with FND. In this article we have described an outdated medical culture built on the traditional dualistic understanding of illness—reflecting, centuries later, Descartes’ mind–body dualism. We have used stories of clinical encounters in health care settings from around the world—told by children and adolescents with FND, their parents, and health professionals—to look at the problem head-on. The stories illustrate the way in which the outdated culture permeates the attitudes of clinicians across all levels of the health system, how it shapes the way that the health care system is organized—physical locations, referral and intake routines, treatment, health care financing, and so on—and how it causes harm to children with FND and their families. And because health systems are embedded in the broader society, the outdated culture has also permeated the attitudes of the general population, the doctors and leaders of hospital departments and outpatient clinics, leaders and staff at universities, and politicians with a special interest in health care [9].
Given that the outdated culture is sustained and perpetuated by physicians and other health professionals, the process of change needs to begin with these very health professionals—that is, from within the health care system itself. But today, we have a medical community in which two subcultures, the outdated one and the FND-informed one, exist side by side. Many clinicians maintain an allegiance to the old culture, and still others have a foot in each culture and find their balance shifting uncomfortably, and ineffectively, from one foot to the other. The process of building an FND-informed culture, though surely in motion, still has a long way to go.
Health care professionals are now moving ahead—inexorably but slowly—as more and more is known about functional disorders, and as more and more information about FND shifts down through the various layers of clinical medicine. Perhaps because FND in pediatric populations has yet to become chronic and is therefore more approachable and treatable, pediatricians have arguably been especially likely to see FND presentations in a new light. The last few decades have seen major advances, as discussed throughout this article, in our understanding of FND onset, etiology, and treatment. Imaging-based studies identifying clear structural, metabolic and fMRI correlates in FND have helped, as have preliminary, but testable, new models (e.g., mammalian threat responses, stress-system activation, integrated cognitive theory) linking FND presentation and course with central and peripheral nervous system findings [23], [82], [83]. Development of new tools and examination strategies yielding positive diagnostic signs for functional symptoms (e.g., gait, weakness, sensory disturbances) have also increased clinicians’ confidence in the capacity to discriminate FND from organic illness. And as new medical residents and trainees in fields outside neurology encounter the clinical milieu, the awareness of FND signs and diagnostic criteria, as well as the capacity to treat and manage FND, is beginning to permeate beyond the field of neurology and into pediatrics, psychiatry, psychology, and other fields.
The field of FND is ripe for change. For the sake of our patients, we hope that this article helps to move that process ahead.
Ethical statement
No patients or volunteers were involved in this opinion piece.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors would like to acknowledge Blanche Savage for her contribution to Text box 3 and Gretel Butler, Helen Dawson, and Nicola Gray for their ideas and enthusiasm when the ideas for this paper were taking shape. We also thank Maryllor De for her assistance with Figure 2.
Footnotes
Feeling an emotion refers to the subjective perception of that emotion (bottom-up process involving subjective experience of body state, including homeostatic emotions) or to the anticipation of that emotion (top-down process involving the human capacity to use the mind to create images [18], [19].
There is no one pattern of presentation. Pediatric research studies suggest that stress system activation—and the emergence of FND symptoms—can occur in the context of physical stress (illness, minor injury, or medical procedure), emotional stress (family conflict, bullying etc), illness promoting psychological processes that function as a top-down stressor (see also Text Box 3), and a neurophysiological system that is more susceptible to stress (due to genetic, epigenetic, or priming mechanisms), or a combination of factors.
The term physician can be used to cover the broad range of medical professionals who refer to pediatric psychological pediatric services: pediatricians (including pediatric neurologists), adult physicians (including adult neurologists), and primary care physicians.
A similar EMR system for an epilepsy clinic pathways—which includes coding for functional seizures by neurologists—has been described by Buchhalter and colleagues (2021) [53].
Physical therapy itself needs to be psychologically informed. See Gray and colleagues (2020) [71].
References
- 1.Delgado R. Storytelling for oppositionists and others: A plea for narrative. Mich Law Rev. 1989;87(8):2411–2441. [Google Scholar]
- 2.Scher S., Kozlowska K., editors. Rethinking Health Care Ethics. Springer Singapore; Singapore: 2018. [PubMed] [Google Scholar]
- 3.Voon V., Brezing C., Gallea C., Ameli R., Roelofs K., LaFrance W.C. Emotional stimuli and motor conversion disorder. Brain. 2010;133(5):1526–1536. doi: 10.1093/brain/awq054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fobian A.D., Elliott L. A review of functional neurological symptom disorder etiology and the integrated etiological summary model. J Psychiatry Neurosci. 2018;43(5) doi: 10.1503/jpn.170190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pick S., Goldstein L.H., Perez D.L., Nicholson T.R. Emotional processing in functional neurological disorder: a review, biopsychosocial model and research agenda. J Neurol Neurosurg Psychiatry. 2019;90(6):704–711. doi: 10.1136/jnnp-2018-319201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Keynejad R.C., Frodl T., Kanaan R., Pariante C., Reuber M., Nicholson T.R. Stress and functional neurological disorders: mechanistic insights. J Neurol Neurosurg Psychiatry. 2019;90(7):813–821. doi: 10.1136/jnnp-2018-318297. [DOI] [PubMed] [Google Scholar]
- 7.Engel G. The need for a new medical model: A challenge for biomedicine. Science. 1977;196(4286):129–136. doi: 10.1126/science.847460. [DOI] [PubMed] [Google Scholar]
- 8.Begue I., Nicholson T.R., Kozlowska K., LaFrance W.C., Levenson J.L., Rapaport M.H. Psychiatry's modern role in functional neurological disorder: Join the renaissance. Psychol Med. 2021:1–3. doi: 10.1017/S0033291721002038. [DOI] [PubMed] [Google Scholar]
- 9.Perez D.L., Edwards M.J., Nielsen G., Kozlowska K., Hallett M., LaFrance, Jr W.C. Decade of progress in motor functional neurological disorder: Continuing the momentum. J Neurol Neurosurg Psychiatry. 2021;92(6):668–677. doi: 10.1136/jnnp-2020-323953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Perez D.L., Nicholson T.R., Asadi-Pooya A.A., Bègue I., Butler M., Carson A.J. Neuroimaging in functional neurological disorder: State of the field and research agenda. Neuroimage Clin. 2021;30:102623. doi: 10.1016/j.nicl.2021.102623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baker J. Psychogenic dysphonia: peeling back the layers. J Voice. 1998;12(4):527–535. doi: 10.1016/s0892-1997(98)80061-1. [DOI] [PubMed] [Google Scholar]
- 12.Rommelfanger K.S., Factor S.A., LaRoche S., Rosen P., Young R., Rapaport M.H. Disentangling stigma from functional neurological disorders: Conference report and roadmap for the future. Front Neurol. 2017;8:106. doi: 10.3389/fneur.2017.00106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.MacDuffie KE, Grubbs L, Best T, LaRoche S, Mildon B, Myers L, et al. Stigma and functional neurological disorder: a research agenda targeting the clinical encounter. CNS Spectr 2020:Dec 3, p. 1–6. [DOI] [PubMed]
- 14.Asadi-Pooya A.A., Brigo F., Kozlowska K., Perez D.L., Pretorius C., Sawchuk T. Social aspects of life in patients with functional seizures: Closing the gap in the biopsychosocial formulation. Epilepsy Behav. 2021;117:107903. doi: 10.1016/j.yebeh.2021.107903. [DOI] [PubMed] [Google Scholar]
- 15.Shephard B. Harvard University Press; Cambridge, MA: 2001. A war of nerves: Soldiers and psychiatrists in the twentieth century. [Google Scholar]
- 16.Flexner A. Carnegie Foundation for the Advancement of Teaching; New York: 1910. Medical Education in the United States and Canada: a report to the Carnegie Foundation for the Advancement of Teaching. [PMC free article] [PubMed] [Google Scholar]
- 17.Album D., Johannessen L.E.F., Rasmussen E.B. Stability and change in disease prestige: A comparative analysis of three surveys spanning a quarter of a century. Soc Sci Med. 2017;180:45–51. doi: 10.1016/j.socscimed.2017.03.020. [DOI] [PubMed] [Google Scholar]
- 18.Damasio A.R. Harcourt Brace; New York: 1999. The feeling of what happens: Body and emotion in the making of consciousness. [Google Scholar]
- 19.Lowe R., Ziemke T. The feeling of action tendencies: On the emotional regulation of goal-directed behavior. Front Psychol. 2011;2:346. doi: 10.3389/fpsyg.2011.00346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Corrigan P.W. Lessons learned from unintended consequences about erasing the stigma of mental illness. World Psychiatry. 2016;15(1):67–73. doi: 10.1002/wps.20295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Frijda N.H. In: Feelings and emotions. Manstead A.S.R., Frijda N., Fischer A., editors. Cambridge University Press; Cambridge: 2004. Emotions and action; pp. 158–173. [Google Scholar]
- 22.Monzoni C.M., Duncan R., Grünewald R., Reuber M. How do neurologists discuss functional symptoms with their patients: a conversation analytic study. J Psychosom Res. 2011;71(6):377–383. doi: 10.1016/j.jpsychores.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 23.Kozlowska K., Scher S., Helgeland H. Palgrave Macmillan; London: 2020. Functional somatic symptoms in children and adolescents: the stress-system approach to assessment and treatment. [Google Scholar]
- 24.Minnis H. Stigma in practice. Lancet Psychiatry. 2021;8(6):466–468. doi: 10.1016/S2215-0366(21)00116-4. [DOI] [PubMed] [Google Scholar]
- 25.Baldwin J. As much truth as one can bear. NY Times. 1962 Jan 14. [Google Scholar]
- 26.Winnicott D.W. Hogarth; London: 1965. The maturational processes and the facilitating environment: Studies in the theory of emotional development. [Google Scholar]
- 27.Erickson M.H., Rossi E.L., editors. The nature of hypnosis and suggestion. Irvington; New York: 1980. [Google Scholar]
- 28.Tolchin B., Perez D.L., Szaflarski J.P., Baslet G., Doss J., Buchhalter J. What's in a name? Epilepsy Behav. 2020;112:107364. doi: 10.1016/j.yebeh.2020.107364. [DOI] [PubMed] [Google Scholar]
- 29.Wardrope A, Dworetzky B, Barkley G, Baslet G, Buchhalter J, Doss J, et al. How to do things with words: two seminars on the naming of functional (psychogenic, non-epileptic, dissociative, conversion, . . .) seizures. Seizure (in press). [DOI] [PMC free article] [PubMed]
- 30.Karterud H.N., Risør M.B., Haavet O.R. The impact of conveying the diagnosis when using a biopsychosocial approach: A qualitative study among adolescents and young adults with NES (non-epileptic seizures) Seizure. 2015;24:107–113. doi: 10.1016/j.seizure.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 31.Kozlowska K. A paediatric point of view: What to say and what not to say when talking to children with non-epileptic seizures. American Epilepsy Society’s Functional Neurological Disorders webinar series. Boston, MA. 2020; Dec 3.
- 32.Winters N.C., Hanson G., Stoyanova V. The case formulation in child and adolescent psychiatry. Child Adolesc Psychiatr Clin N Am. 2007;16(1):111–132. doi: 10.1016/j.chc.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 33.Henderson S., Martin A. In: IACAPAP e-Textbook of child and adolescent mental health. Rey J.M., editor. International Association for Child and Adolescent Psychiatry and Allied Professions; Geneva: 2014. Case formulation and integration of information in child and adolescent mental health. [Google Scholar]
- 34.Kozlowska K, Mohammad S. Functional neurological disorder in children and adolescents: Assessment and treatment. In: Sivaswamy L, Kamat D, editors. Symptom based approach to pediatric neurology. Springer Nature: New York; 2021 (forthcoming).
- 35.Kuhn T.S. University of Chicago Press; Chicago: 1962. The structure of scientific revolutions. [Google Scholar]
- 36.Hallett M, Stone J, Carson A, editors. Functional neurologic disorders. Handbook of Clinical Neurology, 3rd series, volume 139. Amsterdam: Elsevier Health Sciences; 2016.
- 37.Perez D.L., Aybek S., Popkirov S., Kozlowska K., Stephen C.D., Anderson J. A review and expert opinion on the neuropsychiatric assessment of motor functional neurological disorders. J Neuropsychiatry Clin Neurosci. 2021;33(1):14–26. doi: 10.1176/appi.neuropsych.19120357. [DOI] [PubMed] [Google Scholar]
- 38.Baker J., Barnett C., Cavalli L., Dietrich M., Dixon L., Duffy J.R. Management of functional communication, swallowing, cough and related disorders: consensus recommendations for speech and language therapy. J Neurol Neurosurg Psychiatry. 2021;92(10):1112–1125. doi: 10.1136/jnnp-2021-326767. [DOI] [PubMed] [Google Scholar]
- 39.Myers L, Korman GP, Sarudiansky M, Baslet G. Using evidence-based psychotherapy to tailor treatment for patients with FND. Epilepsy Behav Rep (in press). [DOI] [PMC free article] [PubMed]
- 40.Williams S.E., Zahka N.E. Guilford; New York: 2017. Treating somatic symptoms in children and adolescents. [Google Scholar]
- 41.Stone J. Functional neurological disorders: the neurological assessment as treatment. Neurophysiol Clin. 2014;44(4):363–373. doi: 10.1016/j.neucli.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 42.Carson A., Lehn A., Ludwig L., Stone J. Explaining functional disorders in the neurology clinic: A photo story. Pract Neurol. 2016;16(1):56–61. doi: 10.1136/practneurol-2015-001242. [DOI] [PubMed] [Google Scholar]
- 43.Stone J., Carson A., Duncan R., Roberts R., Warlow C., Hibberd C. Who is referred to neurology clinics?–the diagnoses made in 3781 new patients. Clin Neurol Neurosurg. 2010;112(9):747–751. doi: 10.1016/j.clineuro.2010.05.011. [DOI] [PubMed] [Google Scholar]
- 44.Kutluay E., Selwa L., Minecan D., Edwards J., Beydoun A. Nonepileptic paroxysmal events in a pediatric population. Epilepsy Behav. 2010;17(2):272–275. doi: 10.1016/j.yebeh.2009.12.020. [DOI] [PubMed] [Google Scholar]
- 45.Watson C., Sivaswamy L., Agarwal R., Du W., Agarwal R. Functional neurologic symptom disorder in children: Clinical features, diagnostic investigations, and outcomes at a tertiary care children's hospital. J Child Neurol. 2019;34(6):325–331. doi: 10.1177/0883073819830193. [DOI] [PubMed] [Google Scholar]
- 46.Wiggins A., Court A., Sawyer S.M. Somatic symptom and related disorders in a tertiary paediatric hospital: prevalence, reach and complexity. Eur J Pediatr. 2021;180(4):1267–1275. doi: 10.1007/s00431-020-03867-2. [DOI] [PubMed] [Google Scholar]
- 47.Rinaldi M., Ilzarbe D., Kyriakopoulos M. Hospital admission for severe pediatric dissociative disorder. J Nerv Ment Dis. 2019;207(5):406–409. doi: 10.1097/NMD.0000000000000980. [DOI] [PubMed] [Google Scholar]
- 48.Fobian A.D., Long D.M., Szaflarski J.P. Retraining and control therapy for pediatric psychogenic non-epileptic seizures. Ann Clin Transl Neurol. 2020;7(8):1410–1419. doi: 10.1002/acn3.51138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sawchuk T., Buchhalter J., Senft B. Psychogenic nonepileptic seizures in children—prospective validation of a clinical care pathway & risk factors for treatment outcome. Epilepsy Behav. 2020;105 doi: 10.1016/j.yebeh.2020.106971. [DOI] [PubMed] [Google Scholar]
- 50.Kozlowska K., Gray N., Scher S., Savage B. Psychologically informed physiotherapy as part of a multidisciplinary rehabilitation program for children and adolescents with functional neurological disorder: Physical and mental health outcomes. J Paediatr Child Health. 2021;57(1):73–79. doi: 10.1111/jpc.15122. [DOI] [PubMed] [Google Scholar]
- 51.Inglis G., Cramb I. Edinburgh and Lothians Health Foundation; Edinburgh: 2021. Not there: A story of functional neurological disorders. https://www.neurosymptoms.org/en_US/fnd-videos/not-there/ [Google Scholar]
- 52.Herbert LD, Kim R, Hassan AAO, Wilkinson-Smith A, Waugh JL. When neurologists diagnose functional neurological disorder, why don’t they code for it? CNS Spectr (in press). [DOI] [PMC free article] [PubMed]
- 53.Buchhalter J.R., Scantlebury M.H., D’Alfonso S., Appendino J.P., Bello Espinosa L., Brooks B.L. Creation and implementation of an electronic health record note for quality improvement in pediatric epilepsy: Practical considerations and lessons learned. Epilepsia Open. 2021;6(2):345–358. doi: 10.1002/epi4.12480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Radmanesh M., Jalili M., Kozlowska K. Activation of functional brain networks in children and adolescents with psychogenic non-epileptic seizures. Front Hum Neurosci. 2020;14:339. doi: 10.3389/fnhum.2020.00339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Braun M, Sawchuk T, Simpkins A, Heer N, Johnson J, Esser M, et al. Quantitative EEG during hyperventilation as a biomarker for pediatric psychogenic non-epileptic seizures (PNES). Poster session presented at the annual meeting of the American Epilepsy Society. Chicago, IL. 2021.
- 56.Kozlowska K, Palmer DM, Brown KJ, McLean L, Scher S, Gevirtz R, et al. Reduction of autonomic regulation in children and adolescents with conversion disorders. Psychosom Med 2015;77(4):356–70. [DOI] [PubMed]
- 57.Kovacic K., Kolacz J., Lewis G.F., Porges S.W. Impaired vagal efficiency predicts auricular neurostimulation response in adolescent functional abdominal pain disorders. Am J Gastroenterol. 2020;115(9):1534–1538. doi: 10.14309/ajg.0000000000000753. [DOI] [PubMed] [Google Scholar]
- 58.Chapman C.R., Tuckett R.P., Song C.W. Pain and stress in a systems perspective: reciprocal neural, endocrine, and immune interactions. J Pain. 2008;9(2):122–145. doi: 10.1016/j.jpain.2007.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kozlowska K., Rampersad R., Cruz C., Shah U., Chudleigh C., Soe S. The respiratory control of carbon dioxide in children and adolescents referred for treatment of psychogenic non-epileptic seizures. Eur Child Adolesc Psychiatry. 2017;26(10):1207–1217. doi: 10.1007/s00787-017-0976-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Moseley G.L., Butler D.S. Fifteen years of explaining pain: The past, present, and future. J Pain. 2015;16(9):807–813. doi: 10.1016/j.jpain.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 61.Norheim K.B., Jonsson G., Omdal R. Biological mechanisms of chronic fatigue. Rheumatology (Oxford) 2011;50(6):1009–1018. doi: 10.1093/rheumatology/keq454. [DOI] [PubMed] [Google Scholar]
- 62.Stone J., Hewett R., Carson A., Warlow C., Sharpe M. The ‘disappearance’ of hysteria: Historical mystery or illusion? J R Soc Med. 2008;101(1):12–18. doi: 10.1258/jrsm.2007.070129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fend M., Williams L., Carson A.J., Stone J. The arc de siecle: Functional neurological disorder during the ‘forgotten’ years of the 20th century. Brain. 2020;143(4):1278–1284. doi: 10.1093/brain/awaa037. [DOI] [PubMed] [Google Scholar]
- 64.Kozlowska K. Management considerations for pediatric FND In: LaFaver K, Maurer C, Perez DL, Nicholson TRJ, editors. Functional movement disorders: An interdisciplinary case-based approach. Springer (forthcoming 2021).
- 65.Allison M.A., Attisha E. The link between school attendance and good health. Pediatrics. 2019;143(2):e20183648. doi: 10.1542/peds.2018-3648. [DOI] [PubMed] [Google Scholar]
- 66.Kozlowska K., Cruz C., Davies F., Brown K.J., Palmer D.M., McLean L. The utility (or not) of self-report instruments in family assessment for child and adolescent conversion disorders? Aust N Z J Fam Ther. 2016;37(4):480–499. [Google Scholar]
- 67.Sawchuk T., Buchhalter J. Psychogenic nonepileptic seizures in children - Psychological presentation, treatment, and short-term outcomes. Epilepsy Behav. 2015;52(Pt A):49–56. doi: 10.1016/j.yebeh.2015.08.032. [DOI] [PubMed] [Google Scholar]
- 68.Kozlowska K., Scher S., Williams L.M. Patterns of emotional-cognitive functioning in pediatric conversion patients: Implications for the conceptualization of conversion disorders. Psychosom Med. 2011;73(9):775–788. doi: 10.1097/PSY.0b013e3182361e12. [DOI] [PubMed] [Google Scholar]
- 69.Gianaros PJ, Wager TD. Brain-body pathways linking psychological stress and physical health. Curr Dir Psychol Sci 2015;24(4):313–21. [DOI] [PMC free article] [PubMed]
- 70.Garralda M.E., Rask C.U. In: Rutter’s child and adolescent psychiatry. 6th edition. Thapar A., Pine D.S., Leckman J.F., Scott S., Snowling M.J., Taylor E., editors. Wiley; Chichester, West Sussex: 2015. Somatoform and related disorders; pp. 1035–1054. [Google Scholar]
- 71.Gray N., Savage B., Scher S., Kozlowska K. Psychologically informed physical therapy for children and adolescents with functional neurological symptoms: The wellness approach. J Neuropsychiatry Clin Neurosci. 2020;32(4):389–395. doi: 10.1176/appi.neuropsych.19120355. [DOI] [PubMed] [Google Scholar]
- 72.Butz C., Iske C., Truba N., Trott K. Treatment of functional gait abnormality in a rehabilitation setting: emphasizing the physical interventions for treating the whole child. Innov Clin Neurosci. 2019;16(7–8):18–21. [PMC free article] [PubMed] [Google Scholar]
- 73.Nielsen G., Stone J., Matthews A., Brown M., Sparkes C., Farmer R. Physiotherapy for functional motor disorders: A consensus recommendation. J Neurol Neurosurg Psychiatry. 2015;86(10):1113–1119. doi: 10.1136/jnnp-2014-309255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Greenwood B.N., Fleshner M. Exercise, stress resistance, and central serotonergic systems. Exerc Sport Sci Rev. 2011;39(3):140–149. doi: 10.1097/JES.0b013e31821f7e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Leung A., Gregory N.S., Allen L.A., Sluka K.A. Regular physical activity prevents chronic pain by altering resident muscle macrophage phenotype and increasing interleukin-10 in mice. Pain. 2016;157(1):70–79. doi: 10.1097/j.pain.0000000000000312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lloyd B.A., Hake H.S., Ishiwata T., Farmer C.E., Loetz E.C., Fleshner M. Exercise increases mTOR signaling in brain regions involved in cognition and emotional behavior. Behav Brain Res. 2017;323:56–67. doi: 10.1016/j.bbr.2017.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Monda V., Villano I., Messina A., Valenzano A., Esposito T., Moscatelli F. Exercise modifies the gut microbiota with positive health effects. Oxid Med Cell Longev. 2017;2017:1–8. doi: 10.1155/2017/3831972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Butcher P., Elias A., Cavalli L. 1. Aufl. ed. Wiley; New York: 2007. Understanding and treating psychogenic voice disorder: A CBT framework. [Google Scholar]
- 79.Baker J. In: Hallet M., Stone J., Carson A., editors. volume 139. Elsevier Health Sciences; Amsterdam: 2016. Functional voice disorders: Clinical presentations and differential diagnosis; pp. 389–406. (Handbook of Clinical Neurology, 3rd series). [DOI] [PubMed] [Google Scholar]
- 80.Baker J. Compton; Oxford: 2017. Psychosocial perspectives on the management of voice disorders: Implications for patients and clients, options and strategies for clinicians. [Google Scholar]
- 81.Liebowitz M.R., Salman E., Jusino C.M., Garfinkel R., Street L., Cardenas D.L. Ataque de nervios and panic disorder. Am J Psychiatry. 1994;151(6):871–875. doi: 10.1176/ajp.151.6.871. [DOI] [PubMed] [Google Scholar]
- 82.Kozlowska K., Walker P., McLean L., Carrive P. Fear and the defense cascade: Clinical implications and management. Harv Rev Psychiatry. 2015;23(4):263–287. doi: 10.1097/HRP.0000000000000065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Brown R.J., Reuber M. Towards an integrative theory of psychogenic non-epileptic seizures (PNES) Clin Psychol Rev. 2016;47:55–70. doi: 10.1016/j.cpr.2016.06.003. [DOI] [PubMed] [Google Scholar]