Abstract
Background
Successful outcomes in total hip arthroplasty (THA) rely in part on accurate component positioning, which may be optimized through the use of computer navigation and robot-assistance. Therefore, we queried a large national database to characterize national trends in technology-assisted THA utilization, determine whether these technologies were associated with increased hospital charges, and identify demographic factors associated with technology-assisted THA.
Methods
Using the Nationwide Inpatient Sample database, patients that underwent conventional THA, computer-navigated THA, and robot-assisted THA from 2005 to 2018 were identified. Patient and hospital demographics, charge data, and payer characteristics were collected. Temporal trends in utilization were reported. Univariate analyses were performed to compare differences between groups with multiple logistic regression analysis to account for confounders.
Results
In total, 3,428,208 patients undergoing THA from 2005 to 2018 were identified, of which 63,136 (1.8%) used computer navigation and 32,660 (1.0%) used robot-assistance. National utilization of computer navigation in THA increased from 0.1% to 1.9% between 2005 and 2018, while utilization of robot-assisted THA increased from <0.1% to 2.1% from 2008 to 2018. On multivariate analysis, technology-assisted THA was most commonly performed in urban hospitals in the Northeastern United States. Median hospital charges were increased for technology-assisted THAs relative to conventional THAs ($66,089 ± $254 vs $55,418 ± $43).
Conclusions
Computer navigation and robot-assistance in THA demonstrated a consistent increase in utilization during the period examined, representing 4.0% of THAs performed in 2018. Patient and hospital characteristics including risk of mortality, geographic region, and teaching status were associated with increased utilization. Utilization of computer navigation was associated with increased hospital charges.
Keywords: Robotics, Technology, Navigation, Total hip arthroplasty, THA
Introduction
Total hip arthroplasty (THA) is a common and highly successful intervention for patients with degenerative hip disease. However, complications including dislocation, leg length discrepancy, periprosthetic joint infection, aseptic loosening, and periprosthetic fracture persist [[1], [2], [3], [4], [5]]. One critical element to mitigate the risk of complications and improve the long-term outcomes of THA is accurate component positioning. The development and expansion of computer navigation and robot-assisted THA has presented surgeons with the opportunity to improve both the precision and accuracy of component positioning during THA [[6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19]]. However, the true clinical impact of these technological advancements on patient-reported outcomes, decreased complication rates, and decreased revision rates after THA remains unknown [12,15,[20], [21], [22]].
In 2004, updates to the International Classification of Diseases, Ninth Revision (ICD-9) procedure codes introduced a code for computer-assisted surgery (00.3), followed by the creation of a robot-assisted surgery (17.4) code in 2008. Boylan et al. presented the utilization trends of technology-assisted THA (TA-THA) in New York using the New York Statewide Planning and Research Cooperative System (SPARCS) database [23]. This study demonstrated yearly increases in the use of TA-THA from 2008 to 2015; however, their data were limited to one state. Another retrospective study by Hsiue et al. used the National Inpatient Sample (NIS) database and found that the utilization of TA-THA increased from 2005 to 2014, reaching 3% of THAs performed in 2014 [24]. However, despite growing interest in these technologies, no study to our knowledge has investigated the utilization of these technologies after 2014.
Therefore, the purpose of this study was to characterize national trends in the utilization of computer navigation and robot-assistance in THA from 2005 to 2018, determine if the use of these technologies was associated with increased hospital charges, and identify patient and hospital factors associated with the utilization of TA-THA.
Material and methods
Data collection
A retrospective cohort study of all patients who underwent a primary THA from 2005 to 2018 was performed, using the Nationwide Inpatient Sample (NIS) database for patient identification. The NIS is the largest publicly available, national, all-payer hospital inpatient care database within the United States (U.S.). This database was developed as part of the Healthcare Cost and Utilization Project, is sponsored by the Agency for Healthcare Research and Quality, and represents an approximate 20% sampling of all hospital discharges [23]. The present study was exempt from institutional review board review in accordance with the Health Insurance Portability and Accountability Act as the NIS database provides no protected health information.
Variables
Patients of all ages who underwent primary THA from 2005 to 2018 were included in this study, identified using the ICD-9 procedure code 81.51 (THA) and ICD-10 procedure codes 0SR90 and 0SR9B. A subset of patients for whom computer-assistance was used during THA was identified using procedure modifier codes 00.3 (ICD-9) and 8E0YXB (ICD-10). ICD-9 codes used to identify the use of computer-assistance included (Supplemental Table 1) computer-assisted surgery with computed tomography/computed tomography angiography (00.31), computer-assisted surgery with magnetic resonance/magnetic resonance angiography (00.32), computer-assisted surgery with fluoroscopy (00.33), imageless computer-assisted surgery (00.34), computer-assisted surgery with multiple data sets (00.35), and/or other computer-assisted surgery (00.39). ICD-10 computer-assisted surgery codes included (Supplemental Table 2) computer-assisted procedure of lower extremity (8E0YXBZ), computer-assisted procedure of lower extremity with CT (8E0YXBG), computer-assisted procedure of lower extremity with MRI (8E0YXBH), and computer-assisted procedure of lower extremity with fluoroscopy (8E0YXBF).
Patients undergoing robot-assisted surgery were identified using the ICD-9 procedure modifier codes for open robot-assisted procedure (17.41) and other unspecified robot-assisted procedure (17.49), as well as the ICD-10 procedure modifier codes for robot-assisted procedure of lower extremity (8E0YXCZ) and robot-assisted procedure of lower extremity, open approach (8E0Y0CZ).
Patient demographics, including age, gender, race, primary health insurance, and risk mortality (minor, moderate, major, and extreme likelihood of dying), were recorded and analyzed. In addition, hospital characteristics such as hospital location, teaching status (rural, urban nonteaching, urban teaching), geographic region (Northeast, Midwest, South, West), bed size, median household income by quartile, and median hospital charges (adjusted for inflation to 2018 USD) were analyzed [25]. Importantly, hospital charge data provided within the NIS database indicates the billable amount for hospital services rendered, but does not directly represent the payment received by hospitals for those services.
Statistical analysis
Descriptive statistics were used to characterize temporal trends in utilization of TA-THA and are reported as means, standard deviations, and percentages where appropriate. Differences between the computer-navigation, robot-assistance, and conventional THA cohorts were assessed via univariate analyses. Pearson's chi-squared test was used for categorical variables, and Student’s t-test was used for continuous variables where appropriate. Then, a multivariate model was generated using variables identified from the univariate analysis with a P value ≤ .1. Finally, multiple logistic regression analysis was used to identify independent predictors for the use of computer navigation or robot-assistance in THA in 2018, while controlling for comorbidities and accounting for potential confounders. All statistical analyses were performed using STATA (version 13.0; StataCorp LP, College Station, TX).
Results
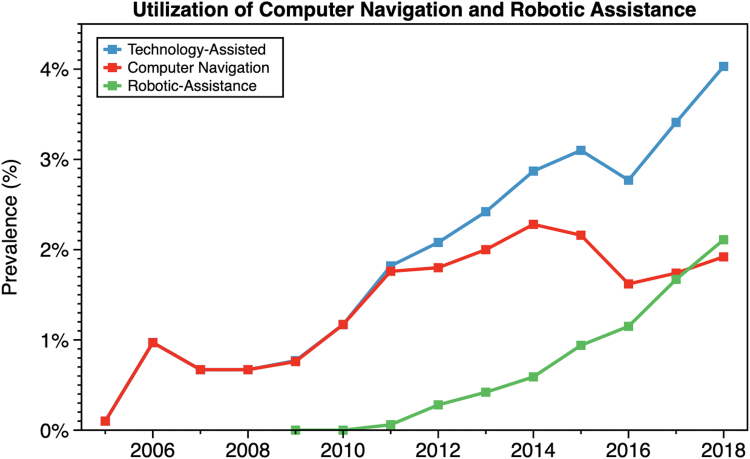
In total, 3,428,208 patients who received a THA from 2005 to 2018 were identified, of which 63,136 (1.8%) used computer navigation and 32,660 (1.0%) used robotic assistance (Table 1). The utilization of computer navigation in THA increased from 0.1% in 2005 to 1.9% in 2018, while the prevalence of robot-assisted THA increased from <0.1% in 2008 to 2.1% in 2018 (Fig. 1). Overall, the utilization of TA-THA increased yearly throughout the study period, peaking in 2018 at 4.0% of all THAs analyzed in the final year of study.
Table 1.
Comparison of patient demographics and hospital characteristics between conventional and technology-assisted (computer navigation and robot-assistance) total hip arthroplasty (THA) groups.
| Variable | Conventional |
Technology-assisted |
P value | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
| 3,332,412 | 97.2% | 95,796 | 2.8% | ||
| Computer navigation | 63,136 | 1.8% | |||
| Robot-assistance | 32,660 | 1.0% | |||
| Age (y), mean ± SD | 65.4 + 0.0 | 65.0 + 0.1 | <.0001 | ||
| Gender (%) | |||||
| Female | 1,678,488 | 44.0% | 45,064 | 44.2% | .495 |
| Male | 2,140,597 | 56.1% | 56,891 | 55.8% | |
| Race (%) | |||||
| White | 2,869,382 | 86.1% | 83,240 | 86.9% | <.0001 |
| Black | 242,620 | 7.3% | 5801 | 6.1% | |
| Hispanic | 114,282 | 3.4% | 3716 | 3.9% | |
| Asian or Pacific Islander | 29,983 | 0.9% | 938 | 1.0% | |
| Native American | 10,816 | 0.3% | 464 | 0.5% | |
| Other | 464 | 0.5% | 10,816 | 0.3% | |
| Primary payment (%) | |||||
| Medicare | 2,052,109 | 53.7% | 52,915 | 52.0% | <.0001 |
| Medicaid | 1528 | 4.0% | 3689 | 3.6% | |
| Private | 1,484,123 | 38.9% | 42,238 | 41.5% | |
| Self-pay | 29,967 | 0.8% | 508 | 0.5% | |
| No charge | 4802 | 0.1% | 85 | 0.1% | |
| Other payment | 95,267 | 2.5% | 4802 | 0.1% | |
| Median household income | |||||
| 0-25th Percentile | 693,642 | 19.7% | 17,383 | 17.4% | <.0001 |
| 25-50th Percentile | 900,655 | 25.5% | 24,625 | 24.6% | |
| 50-75th Percentile | 942,565 | 26.7% | 26,467 | 26.5% | |
| 75-100th Percentile | 989,375 | 28.1% | 31,512 | 31.5% | |
| Hospital location/teaching status | <.0001 | ||||
| Rural | 368,000 | 9.6% | 5766 | 5.7% | |
| Urban, nonteaching | 1,439,794 | 37.7% | 36,334 | 35.6% | |
| Urban, teaching | 2,008,351 | 52.6% | 59,902 | 58.7% | |
| Hospital bed size | |||||
| Small | 800,892 | 21.0% | 31,122 | 30.5% | <.0001 |
| Medium | 989,437 | 25.9% | 26,245 | 25.7% | |
| Large | 2,025,817 | 53.1% | 44,636 | 43.8% | |
| Region of hospital | <.0001 | ||||
| Northeast | 763,790 | 20.0% | 22,955 | 22.5% | |
| Midwest | 1,007,975 | 26.4% | 15,350 | 15.1% | |
| South | 1,270,426 | 33.2% | 34,672 | 34.0% | |
| West | 783,656 | 20.5% | 29,043 | 28.5% | |
| Total hospital charge ($USD), median ± SD | $55,418 ± $43 | $66,089 ± $254 | .2472 | ||
Statistically significant (P < .05) values are depicted in bold.
Figure 1.
The percentage of total hip arthroplasties using computer navigation or robot-assistance from 2005 to 2018. The technology-assisted trendline is the sum of the computer navigation and robot-assisted trendlines.
Univariate results
The conventional THA and TA-THA cohorts had many similar patient characteristics. The average patient age in both groups was approximately 65 years, and both groups were predominantly male (conventional: 56.1%, technology-assisted: 55.8%) and White (conventional: 86.1%, technology-assisted: 86.9%) (Table 1). Medicare was the primary payer in approximately 53% of patients in both cohorts. Overall, THA was performed least frequently for patients in the lowest household income quartile in both the conventional (19.7%) and TA-THA (17.4%) cohorts.
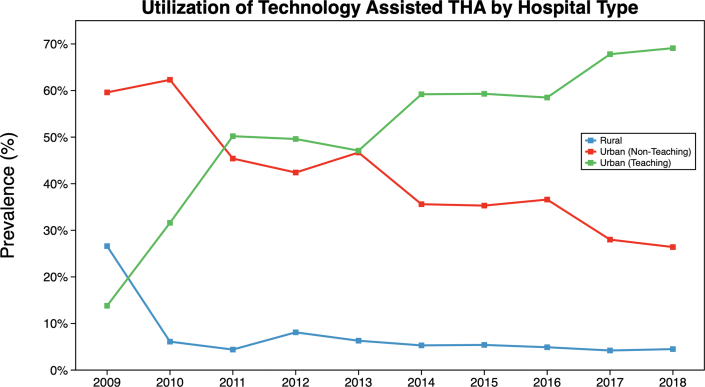
Univariate analysis of hospital factors revealed differences between the conventional and technology-assisted cohorts. By geographic region, the largest number of THAs during the study period were performed in the South (conventional: 33.2%, technology-assisted: 34.0%). Although hospitals in the West accounted for only 20.5% of conventional THAs, these hospitals accounted for 28.5% of technology-assisted surgeries. In contrast, the Midwest accounted for 26.4% of conventional THAs, but only 15.1% of technology-assisted procedures (Table 1). The utilization of TA-THA was largely driven by urban teaching hospitals, accounting for 13.8% of the TA-THAs in 2009 and increasing to 69.1% in 2018 (Fig. 2). Overall, urban teaching hospitals accounted for 58.7% of all TA-THAs performed across the entire study period.
Figure 2.
Utilization of technology-assisted THAs by hospital location and teaching status from 2009 to 2018. The increased utilization of these technologies has been spearheaded by urban teaching institutions which accounted for 69.1% of technology-assisted THAs in 2018.
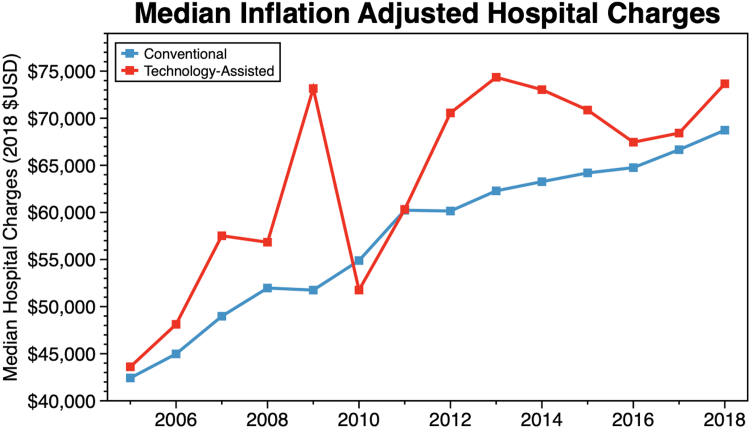
During the study period, the median hospital charge was significantly increased for patients receiving TA-THA compared to patients receiving conventional THA ($70,711 ± $272 vs $59,294 ± $46). Median hospital charges for TA-THA and conventional THA were similar in 2005 ($43,609 ± $2614 vs $42,424 ± $114, respectively) but have since increased for both cohorts. However, charges for TA-THA have increased at a faster rate. In 2018, the average hospital charge for conventional THA was $68,733 ± $162, compared to $73,659 ± $710 for TA-THA (Fig. 3).
Figure 3.
The median hospital charges (inflation-adjusted to 2018 $USD) for total hip arthroplasty performed by conventional or technology-assisted techniques from 2005 to 2018.
Multivariate results
To determine independent predictors for the use of computer navigation or robot-assistance in THA, multivariate analyses were conducted for the year 2018. No significant differences were identified between White, Black, Hispanic, Asian, or Native American patients with regard to the use of computer navigation in THA (P > .05) (Table 2). Patients in the upper quartile of household income (Relative risk [RR] 1.51, 95% confidence interval [CI] 1.29-1.76, P < .01) were more likely to undergo a computer-navigated surgery relative to those in the lowest quartile of household income, as were patients undergoing THA at urban teaching (RR 1.54, 95% CI 1.20-1.99, P < .01) and nonteaching (RR 1.36, 95% CI 1.04-1.77, P = .03) hospitals when compared to rural hospitals. In contrast, patients with higher risk mortality (ie, “extreme likelihood of dying”) had a decreased likelihood of undergoing computer-navigated THA (RR 0.24, 95% CI 0.09-0.64, P < .01) relative to those with lower risk of mortality (ie, “minor likelihood of dying”) (Table 2). Relative to the Northeast, computer-navigated THA was least likely to be performed in the Midwest (RR 0.27, 95% CI 0.23-0.33, P < .01) and the South (RR 0.58, 95% CI 0.51-0.66, P < .01). Finally, computer-navigated THA was less likely to be performed at hospitals with larger bed sizes (RR 0.53, 95% CI 0.48-0.59, P < .01) relative to hospitals with smaller bed sizes (Table 2).
Table 2.
Independent factors associated with the utilization of computer navigation during total hip arthroplasty (THA) in 2018 on multivariate analysis.
| Variable | Relative risk | Confidence interval | P value |
|---|---|---|---|
| Age | 1.00 | 1.00-1.01 | .20 |
| Female gender (reference: male) | 1.08 | 0.98-1.19 | .10 |
| Risk mortality (reference: minor likelihood of dying) | |||
| Moderate likelihood of dying | 0.78 | 0.68-0.90 | <.01 |
| Major likelihood of dying | 0.43 | 0.30-0.61 | <.01 |
| Extreme likelihood of dying | 0.24 | 0.09-0.64 | <.01 |
| Race (reference: White) | |||
| Black | 0.97 | 0.80-1.19 | .78 |
| Hispanic | 0.98 | 0.78-1.23 | .85 |
| Asian or Pacific Islander | 1.01 | 0.68-1.52 | .94 |
| Native American | 1.77 | 0.90-3.46 | .10 |
| Other | 0.96 | 0.68-1.36 | .83 |
| Primary payment (reference: Medicare) | |||
| Medicaid | 1.05 | 0.82-1.35 | .68 |
| Private | 1.10 | 0.97-1.25 | .13 |
| Self-pay | 0.69 | 0.34-1.39 | .30 |
| Median household income (reference: 1st quartile) | |||
| 25-50th Percentile | 1.14 | 0.97-1.34 | .10 |
| 50-75th Percentile | 0.96 | 0.81-1.13 | .62 |
| 75-100th Percentile | 1.51 | 1.29-1.76 | <.01 |
| Hospital location/teaching status (reference: rural) | |||
| Urban, nonteaching | 1.36 | 1.04-1.77 | .03 |
| Urban, teaching | 1.54 | 1.20-1.99 | <.01 |
| Hospital bed size (reference: small) | |||
| Medium | 0.58 | 0.52-0.65 | <.01 |
| Large | 0.53 | 0.48-0.59 | <.01 |
| Hospital region (reference: Northeast) | |||
| Midwest | 0.27 | 0.23-0.33 | <.01 |
| South | 0.58 | 0.51-0.66 | <.01 |
| West | 1.02 | 0.90-1.15 | .74 |
Statistically significant (P < .05) values are depicted in bold.
Similarly, multivariate analyses were conducted for robot-assisted THA in the year 2018 (Table 3). Hispanic patients were less likely to undergo robot-assisted THA than White patients (RR 0.71, 95% CI 0.55-0.91, P = .01) in 2018. Furthermore, patients with Medicaid as their primary health insurance (RR 0.74, 95% CI 0.58-0.95, P = .02) and patients without external health insurance (RR 0.34, 95% CI 0.14-0.82, P = .02) were less likely to undergo robot-assisted THA relative to patients covered by Medicare. However, median household income was not a predictor of the use of robot-assistance during THA (P > .05) (Table 3).
Table 3.
Independent factors associated with robot-assisted total hip arthroplasty (THA) utilization in 2018 on multivariate analysis.
| Variable | Relative risk | Confidence interval | P value |
|---|---|---|---|
| Age | 0.99 | 0.99-1.00 | <.01 |
| Female gender (reference: male) | 1.05 | 0.96-1.15 | .31 |
| Risk mortality (reference: minor likelihood of dying) | |||
| Moderate likelihood of dying | 0.84 | 0.74-0.96 | .01 |
| Major likelihood of dying | 0.57 | 0.42-0.78 | <.01 |
| Extreme likelihood of dying | 0.59 | 0.32-1.11 | .10 |
| Race (reference: White) | |||
| Black | 0.85 | 0.70-1.01 | .07 |
| Hispanic | 0.71 | 0.55-0.91 | .01 |
| Asian or Pacific Islander | 0.76 | 0.45-1.27 | .30 |
| Native American | 2.67 | 1.58-4.53 | <.01 |
| Other | 0.70 | 0.49-1.02 | .06 |
| Primary payment (reference: Medicare) | |||
| Medicaid | 0.74 | 0.58-0.95 | .02 |
| Private | 1.09 | 0.97-1.23 | .14 |
| Self-pay | 0.34 | 0.14-0.82 | .02 |
| Median household income (reference: 1st quartile) | |||
| 25-50th Percentile | 0.88 | 0.77-1.02 | .09 |
| 50-75th Percentile | 0.98 | 0.86-1.13 | .81 |
| 75-100th Percentile | 0.95 | 0.83-1.10 | .50 |
| Hospital location/teaching status (reference: rural) | |||
| Urban, nonteaching | 1.87 | 1.49-2.37 | <.01 |
| Urban, teaching | 1.38 | 1.10-1.73 | .01 |
| Hospital bed size (reference: small) | |||
| Medium | 0.82 | 0.74-0.91 | <.01 |
| Large | 0.54 | 0.48-0.60 | <.01 |
| Hospital region (reference: Northeast) | |||
| Midwest | 0.39 | 0.34-0.44 | <.01 |
| South | 0.56 | 0.50-0.63 | <.01 |
| West | 0.50 | 0.44-0.57 | <.01 |
Statistically significant (P < .05) values are depicted in bold.
On multivariate analysis, urban hospitals, both teaching (RR 1.38, 95% CI 1.10-1.73, P = .01) and nonteaching (RR 1.87, 95% CI 1.49-2.37, P < .01), were more likely to use robot-assistance in THA relative to rural hospitals (Table 3). Mirroring trends in the utilization of computer-navigated THA, robot-assisted THA was most likely to be performed in the Northeast, with all other regions demonstrating decreased utilization of robot-assistance, most notably the Midwest (RR 0.39, 95% CI 0.34-0.44, P < .01) (Table 3).
Regression analysis was performed to identify drivers of high cost in 2018 (defined as hospital charges ≥90th percentile), representing charges greater than $120,099 for our data set (Table 4). Hospital charges were more likely to be high for patients with higher risk mortality (ie, “extreme likelihood of dying”) relative to patients with low risk of mortality (ie, “minor likelihood of dying”) (RR 21.63, 95% CI 18.68-25.05), as well as when Medicaid was the primary payer compared to Medicare (RR 1.14, 95% CI 1.03-1.26, P = .02) (Table 4). Costs were also greater for urban hospitals, both teaching (RR 3.07, 95% CI 2.69-3.51, P < .01) and nonteaching (RR 3.18, 95% CI 2.77-3.65, P < .01), relative to rural hospitals. Hospital charges were also more likely to be high in the West (RR 2.66, 95% CI 2.49-2.86, P < .01) and less likely to be high in the Midwest (RR 0.62, 95% CI 0.57-0.68, P < .01), when compared to the Northeast. Finally, the utilization of computer navigation during THA was associated with increased hospital charges (RR 2.11, 95% CI 1.86-2.39, P < .01). However, the utilization of robot-assistance was not statistically significantly associated with increased hospital charges (RR 0.93, 95% CI 0.80-1.10, P = .40) (Table 4).
Table 4.
Independent factors associated with high hospital charges for patients undergoing total hip arthroplasty (THA) in 2018 on multivariate analysis.
| Variable | Relative risk | Confidence interval | P value |
|---|---|---|---|
| Age | 0.98 | 0.98-0.99 | <.01 |
| Female gender (reference: male) | 1.02 | 0.97-1.07 | .40 |
| Risk mortality (reference: minor likelihood of dying) | |||
| Moderate likelihood of dying | 1.88 | 1.77-1.99 | <.01 |
| Major likelihood of dying | 4.95 | 4.56-5.37 | <.01 |
| Extreme likelihood of dying | 21.63 | 18.68-25.05 | <.01 |
| Race (reference: White) | |||
| Black | 1.17 | 1.08-1.27 | <.01 |
| Hispanic | 1.61 | 1.47-1.76 | <.01 |
| Asian or Pacific Islander | 1.28 | 1.06-1.53 | .01 |
| Native American | 0.43 | 0.25-0.72 | <.01 |
| Other | 2.10 | 1.84-2.40 | <.01 |
| Primary payment (reference: Medicare) | |||
| Medicaid | 1.14 | 1.03-1.26 | .02 |
| Private | 0.77 | 0.72-0.81 | <.01 |
| Self-Pay | 0.83 | 0.65-1.06 | .14 |
| Median household income (reference: 1st quartile) | |||
| 25-50th Percentile | 0.92 | 0.86-0.98 | .02 |
| 50-75th Percentile | 0.81 | 0.76-0.87 | <.01 |
| 75-100th Percentile | 1.00 | 0.94-1.07 | .97 |
| Hospital location/teaching status (reference: rural) | |||
| Urban, nonteaching | 3.18 | 2.77-3.65 | <.01 |
| Urban, teaching | 3.07 | 2.69-3.51 | <.01 |
| Hospital bed size (reference: small) | |||
| Medium | 1.45 | 1.37-1.54 | <.01 |
| Large | 1.22 | 1.16-1.29 | <.01 |
| Hospital region (reference: Northeast) | |||
| Midwest | 0.62 | 0.57-0.68 | <.01 |
| South | 1.64 | 1.53-1.76 | <.01 |
| West | 2.66 | 2.49-2.86 | <.01 |
| Computer navigation | 2.11 | 1.86-2.39 | <.01 |
| Robotic assistance | 0.93 | 0.80-1.10 | .40 |
High cost was defined as hospital charges in the 90th percentile and above, equaling charges greater than $120,099 for our data set.
Statistically significant (P < .05) values are depicted in bold.
Discussion
Computer navigation and robot-assistance in THA demonstrated a consistent increase in utilization during the period examined, accounting for 4.0% of all THAs analyzed in 2018. The highest number of THAs overall were performed in urban, academic hospitals on White, male patients with Medicare insurance. On multivariate analysis, patients with lower risk of mortality, with higher median household income, and seeking care from urban hospital centers in the Northeastern and Western US were more likely to undergo computer-navigated THA in 2018, irrespective of race/ethnicity or primary health insurance. Robot-assisted surgery is newer and less common, accounting for only 1.0% of primary THAs analyzed in the study period. Increased utilization of robot-assistance in THA was observed for both academic and nonacademic urban hospitals and for hospitals in the Northeastern US, irrespective of median household income. However, Hispanic patients, patients paying out of pocket, and patients covered by Medicaid were less likely to undergo robot-assisted THA. Interestingly, the use of computer navigation was associated with increased hospital charges, while utilization of robot-assistance in THA was not associated with significantly increased cost.
Using a New York database, Boylan et al. similarly demonstrated yearly increases in utilization of technology assistance in THA, reaching approximately 5% of primary THAs performed [23]. A recent study by Hsiue et al. used the NIS to demonstrate a similar increase in utilization of TA-THA from 2005 to 2014 [24]. In contrast to the present study, which demonstrated that urban hospitals were more likely to use robot-assistance during THA, Hsiue et al. found no relationship between hospital type and likelihood of undergoing a TA-THA. We attribute this discrepancy to differences in statistical methodology, as the authors of that study did not perform multivariate adjustments when calculating odds ratios. In addition, Hsiue et al. were unable to perform individual analyses investigating the use of computer navigation and robot-assistance during THA, as they elected to combine these ICD-9 codes into one group [24]. The present study is in agreement with these two studies, as we identified increased utilization of these technologies over the study period. However, unlike these other studies, the present study provides increased granularity by reporting the results of separate multivariate analyses for the utilization of both computer navigation and robot-assistance during THA.
The mean hospital cost of THA has increased by 49.8% in the past 15 years [26]. Our study demonstrates an approximately 20% increase in median hospital charges for TA-THA compared to conventional THA. On multivariate analysis, the use of computer navigation was associated with high hospital charges. Furthermore, high hospital charges were independently associated with large, urban hospitals in the Southern and Western US. Although the utilization of technological assistance for THA remains relatively low currently, the trend of increasing utilization demonstrated in the present study suggests that the use of these technologies may contribute to rising health-care costs in the future.
Although the importance of optimal component positioning for successful outcomes after THA is well-understood, multiple studies have demonstrated poor reliability and reproducibility with conventional techniques. In a study of 500 consecutive primary THAs performed by eight trained orthopedic surgeons, 19.8% of cups were oriented outside the Lewinnek safe zone for inclination, and 11.2% were oriented outside the anteversion safe zone [27]. Similarly, in an analysis of 1823 hips, Callanan et al. found that only 50% of THAs were in the presumed safe zone for both inclination and abduction [28]. Positioning was subject to patients' BMI, surgical approach, and surgeon experience. Of 40 patients studied, 55% had hip center of rotation, and 47% had femoral offset restored within 5 mm from anatomic [9].
Several studies have demonstrated improvements in component accuracy and precision with TA-THA when compared to conventional techniques [[6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19]]. As assessed on postoperative CT scans, computer navigation provided predictable and reproducible cup anteversion and inclination within 5°, while surgeons using conventional techniques in the same study were within 11° to 14°, depending on surgeons' experience [6]. Honl et al. similarly demonstrated decreased acetabular component variability with computer navigation [10].
While previous studies have demonstrated that the use of technological assistance during THA may reliably improve objective markers such as component positioning, the clinical significance of these findings remains a subject of ongoing debate. In an early study by Nakamura et al., robot-assisted THA improved clinical outcome scores at early two- and 3-year follow-up visits compared to conventional THA; however, scores were not significantly different at 5-year follow-up [29]. In a single-surgeon study, Brown et al. found no clinical difference in postoperative Harris Hip Score or leg length discrepancy between computer navigated and conventional THA, while procedure time nearly doubled with computer assistance [30]. Bukowski et al. demonstrated improved mean modified Harris Hip Score and University of California Los Angeles activity score at minimum 1-year follow-up, with no changes in Western Ontario and McMaster or Short-Form 12 Health Survey scores [21]. In that study, the use of robotic assistance only increased operative time by an average of 9 minutes, although operative time increases are subject to variability in surgeon experience and the specific computer or robotic system used [8,[31], [32], [33]]. Overall, these studies demonstrate the need for long-term follow-up studies. A consensus regarding conventional outcome measures is yet to be reached, and it remains to be seen if functional or patient-measured outcomes are significantly improved to justify the increased intraoperative time and operative costs.
As common with database studies, our study has several limitations, most notably reliance on accurate coding. The novelty of the two new series of ICD-9 codes and ICD-10 codes may have led to underreporting due to a lack of familiarity with the new coding system. Therefore, utilization may be underrepresented in this database. However, as the use of technological assistance is associated with higher hospital charges, hospitals are incentivized to accurately code these procedures when performed. The NIS database has been shown previously to provide reliable patient demographic data, while neither underestimating inpatient complications nor patient comorbidities played a significant role in this study [34,35]. Another inherent limitation of our study is the lack of outpatient data, which was not feasible using the inpatient NIS database.
Strengths of our study include the large sample size, geographic and socioeconomic diversity of populations, and inclusion of multiple payer types, leading to generalizable results. To our knowledge, this is the second study in the literature to present national trends of TA-THA [24]. The present study expands on a previous analysis by Hsiue et al. using the NIS database by expanding the study period to 2005-2018 and incorporates ICD-10 procedure codes specific for the use of computer navigation and robotic assistance. This enables a novel sub-analysis of the modern utilization trends of these technological modalities during THA that has not previously been performed.
Conclusions
The present study demonstrates increasing nationwide adoption of computer navigation and robot-assisted THA surgery from 2005 to 2018. Patients with lower risk of mortality and higher household income were more likely to undergo computer-navigated THA. Urban hospitals, both teaching and nonteaching, have more readily adopted the use of both computer navigation and robot-assistance during THA. As technology-assisted surgery continues to be integrated into total joint arthroplasty, continued studies are needed to determine their clinical value.
Footnotes
One or more of the authors of this paper have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field whichmay be perceived to have potential conflict of interest with this work. For full disclosure statements refer to https://doi.org/10.1016/j.artd.2021.08.020.
Declaration of interests: The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: D. A. Oakes is a paid consultant for DePuy, A Johnson & Johnson Company, and LimaCorporate. N. D. Heckmann is a paid consultant for Intellijoint Surgical and MicroPort Orthopedics; has stock or stock options in Intellijoint Surgical; and is a board member in American Academy of Orthopaedic Surgeons (AAOS).
Appendix
Supplemental Table 1.
| ICD-9 procedure modifier codes | |
|---|---|
| Computer-assisted | |
| 00.31 | Computer-assisted surgery with computed tomography/ computed tomography angiography |
| 00.32 | Computer-assisted surgery with MR/MRA |
| 00.33 | Computer-assisted surgery with fluoroscopy |
| 00.34 | Imageless computer-assisted surgery |
| 00.35 | Computer-assisted surgery with multiple data sets |
| 00.39 | Other computer-assisted surgery |
| Robot-assisted | |
| 17.41 | Open robot-assisted procedure |
| 17.49 | Other unspecified robot-assisted procedure |
Supplemental Table 2.
| ICD-10 procedure modifier codes | |
|---|---|
| Computer-assisted | |
| 8E0YXBZ | Computer-assisted procedure of lower extremity |
| 8E0YXBG | Computer-assisted procedure of lower extremity, with CT |
| 8E0YXBH | Computer-assisted procedure of lower extremity, with MRI |
| 8E0YXBF | Computer-assisted procedure of lower extremity, with fluoroscopy |
| Robot-assisted | |
| 8E0YXCZ | Robot-assisted procedure of lower extremity |
| 8E0Y0CZ | Robot-assisted procedure of lower extremity, open approach |
Supplementary data
References
- 1.Lombardi A.V., Berend K.R., Mallory T.H., Skeels M.D., Adams J.B. Survivorship of 2000 tapered titanium porous plasma-sprayed femoral components. Clin Orthop Relat Res. 2009;467:146. doi: 10.1007/s11999-008-0568-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kroell A., Beaulé P., Krismer M., Behensky H., Stoeckl B., Biedermann R. Aseptic stem loosening in primary THA: migration analysis of cemented and cementless fixation. Int Orthop. 2009;33:1501. doi: 10.1007/s00264-008-0701-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee Y.-K., Yoo J.J., Koo K.-H., Yoon K.S., Kim H.J. Metal neck and liner impingement in ceramic bearing total hip arthroplasty. J Orthop Res. 2011;29:218. doi: 10.1002/jor.21246. [DOI] [PubMed] [Google Scholar]
- 4.Kennedy J.G., Rogers W.B., Soffe K.E., Sullivan R.J., Griffen D.G., Sheehan L.J. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplasty. 1998;13:530. doi: 10.1016/s0883-5403(98)90052-3. [DOI] [PubMed] [Google Scholar]
- 5.Delaunay C., Hamadouche M., Girard J., Duhamel A., SoFCOT Group What are the causes for failures of primary hip arthroplasties in France? Clin Orthop Relat Res. 2013;471:3863. doi: 10.1007/s11999-013-2935-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dorr L.D., Malik A., Wan Z., Long W.T., Harris M. Precision and bias of imageless computer navigation and surgeon estimates for acetabular component position. Clin Orthop Relat Res. 2007;465:92. doi: 10.1097/BLO.0b013e3181560c51. [DOI] [PubMed] [Google Scholar]
- 7.Dorr L.D., Wan Z., Malik A., Zhu J., Dastane M., Deshmane P. A comparison of surgeon estimation and computed tomographic measurement of femoral component anteversion in cementless total hip arthroplasty. J Bone Joint Surg Am. 2009;91:2598. doi: 10.2106/JBJS.H.01225. [DOI] [PubMed] [Google Scholar]
- 8.Li Y.-L., Jia J., Wu Q., Ning G.-Z., Wu Q.-L., Feng S.-Q. Evidence-based computer-navigated total hip arthroplasty: an updated analysis of randomized controlled trials. Eur J Orthop Surg Traumatol. 2014;24:531. doi: 10.1007/s00590-013-1222-1. [DOI] [PubMed] [Google Scholar]
- 9.Bjarnason J.A., Reikeras O. Changes of center of rotation and femoral offset in total hip arthroplasty. Ann Transl Med. 2015;3:355. doi: 10.3978/j.issn.2305-5839.2015.12.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Honl M., Schwieger K., Salineros M., Jacobs J., Morlock M., Wimmer M. Orientation of the acetabular component. A comparison of five navigation systems with conventional surgical technique. J Bone Joint Surg Br. 2006;88:1401. doi: 10.1302/0301-620X.88B10.17587. [DOI] [PubMed] [Google Scholar]
- 11.Dastane M., Dorr L.D., Tarwala R., Wan Z. Hip offset in total hip arthroplasty: quantitative measurement with navigation. Clin Orthop Relat Res. 2011;469:429. doi: 10.1007/s11999-010-1554-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nawabi D.H., Conditt M.A., Ranawat A.S. Haptically guided robotic technology in total hip arthroplasty: a cadaveric investigation. Proc Inst Mech Eng H. 2013;227:302. doi: 10.1177/0954411912468540. [DOI] [PubMed] [Google Scholar]
- 13.Kanawade V., Dorr L.D., Banks S.A., Zhang Z., Wan Z. Precision of robotic guided instrumentation for acetabular component positioning. J Arthroplasty. 2015;30:392. doi: 10.1016/j.arth.2014.10.021. [DOI] [PubMed] [Google Scholar]
- 14.Domb B.G., El Bitar Y.F., Sadik A.Y., Stake C.E., Botser I.B. Comparison of robotic-assisted and conventional acetabular cup placement in THA: a Matched-pair controlled study. Clin Orthop Relat Res. 2014;472:329. doi: 10.1007/s11999-013-3253-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bargar W.L., Bauer A., Börner M. Primary and revision total hip replacement using the Robodoc (R) system. Clin Orthop Relat Res. 1998;354:82. doi: 10.1097/00003086-199809000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Redmond J.M., Gupta A., Hammarstedt J.E., Petrakos A.E., Finch N.A., Domb B.G. The learning curve associated with robotic-assisted total hip arthroplasty. J Arthroplasty. 2015;30:50. doi: 10.1016/j.arth.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 17.Xu K., Li Y.-M., Zhang H.-F., Wang C.-G., Xu Y.-Q., Li Z.-J. Computer navigation in total hip arthroplasty: a meta-analysis of randomized controlled trials. Int J Surg. 2014;12:528. doi: 10.1016/j.ijsu.2014.02.014. [DOI] [PubMed] [Google Scholar]
- 18.Lass R., Kubista B., Olischar B., Frantal S., Windhager R., Giurea A. Total hip arthroplasty using imageless computer-assisted hip navigation: a prospective randomized study. J Arthroplasty. 2014;29:786. doi: 10.1016/j.arth.2013.08.020. [DOI] [PubMed] [Google Scholar]
- 19.Deep K., Shankar S., Mahendra A. Computer assisted navigation in total knee and hip arthroplasty. SICOT J. 2017;3:50. doi: 10.1051/sicotj/2017034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aoude A.A., Aldebeyan S.A., Nooh A., Weber M.H., Tanzer M. Thirty-day complications of conventional and computer-assisted total knee and total hip arthroplasty: analysis of 103,855 patients in the American College of Surgeons National Surgical Quality Improvement Program database. J Arthroplasty. 2016;31:1674. doi: 10.1016/j.arth.2016.01.042. [DOI] [PubMed] [Google Scholar]
- 21.Bukowski B.R., Anderson P., Khlopas A., Chughtai M., Mont M.A., Illgen R.L., 2nd Improved functional outcomes with robotic compared with manual total hip arthroplasty. Surg Technol Int. 2016;29:303. [PubMed] [Google Scholar]
- 22.Ogawa K., Kabata T., Maeda T., Kajino Y., Tsuchiya H. Accurate leg length measurement in total hip arthroplasty: a comparison of computer navigation and a Simple manual measurement Device. Clin Orthop Surg. 2014;6:153. doi: 10.4055/cios.2014.6.2.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Boylan M., Suchman K., Vigdorchik J., Slover J., Bosco J. Technology-assisted hip and knee arthroplasties: an analysis of utilization trends. J Arthroplasty. 2018;33:1019. doi: 10.1016/j.arth.2017.11.033. [DOI] [PubMed] [Google Scholar]
- 24.Hsiue P.P., Chen C.J., Villalpando C., Ponzio D., Khoshbin A., Stavrakis A.I. Trends and patient factors associated with technology-assisted total hip arthroplasty in the United States from 2005 to 2014. Arthroplast Today. 2020;6:112. doi: 10.1016/j.artd.2019.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.CPI Inflation Calculator. https://data.bls.gov/cgi-bin/cpicalc.pl
- 26.Molloy I.B., Martin B.I., Moschetti W.E., Jevsevar D.S. Effects of the length of stay on the cost of total knee and total hip arthroplasty from 2002 to 2013. J Bone Joint Surg. 2017;99:402. doi: 10.2106/JBJS.16.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rittmeister M., Callitsis C. Factors influencing cup orientation in 500 consecutive total hip Replacements. Clin Orthop Relat Res. 2006;445:192. doi: 10.1097/01.blo.0000194669.77849.3c. [DOI] [PubMed] [Google Scholar]
- 28.Callanan M.C., Jarrett B., Bragdon C.R. The John Charnley Award: risk factors for cup malpositioning: quality improvement through a joint registry at a tertiary hospital. Clin Orthop Relat Res. 2011;469:319. doi: 10.1007/s11999-010-1487-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nakamura N., Sugano N., Nishii T., Kakimoto A., Miki H. A comparison between robotic-assisted and manual implantation of cementless total hip arthroplasty. Clin Orthop Relat Res. 2010;468:1072. doi: 10.1007/s11999-009-1158-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brown M.L., Reed J.D., Drinkwater C.J. Imageless computer-assisted versus conventional total hip arthroplasty: one surgeon’s initial experience. J Arthroplasty. 2014;29:1015. doi: 10.1016/j.arth.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 31.Lim S.-J., Kim S.-M., Lim B.-H., Moon Y.-W., Park Y.-S. Comparison of manual rasping and robotic milling for short metaphyseal-fitting stem implantation in total hip arthroplasty: a cadaveric study. Computer Aided Surg. 2013;18:33. doi: 10.3109/10929088.2012.744430. [DOI] [PubMed] [Google Scholar]
- 32.Nishihara S., Sugano N., Nishii T., Miki H., Nakamura N., Yoshikawa H. Comparison between hand rasping and robotic milling for stem implantation in cementless total hip arthroplasty. J Arthroplasty. 2006;21:957. doi: 10.1016/j.arth.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 33.Schulz A.P., Seide K., Queitsch C. Results of total hip replacement using the Robodoc surgical assistant system: clinical outcome and evaluation of complications for 97 procedures. Int J Med Robot. 2007;3:301. doi: 10.1002/rcs.161. [DOI] [PubMed] [Google Scholar]
- 34.Bohl D.D., Basques B.A., Golinvaux N.S., Baumgaertner M.R., Grauer J.N. Nationwide Inpatient Sample and National Surgical Quality Improvement Program give different results in hip fracture studies. Clin Orthop Relat Res. 2014;472:1672. doi: 10.1007/s11999-014-3559-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bohl D.D., Russo G.S., Basques B.A. Variations in data collection methods between national databases affect study results: a comparison of the nationwide inpatient sample and national surgical quality improvement program databases for lumbar spine fusion procedures. J Bone Joint Surg. 2014;96:e193. doi: 10.2106/JBJS.M.01490. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.