Abstract
Background
Low birth weight (LBW) and fetal growth restriction are associated with the development of cardio-metabolic diseases later in life. A recent Mendelian randomization study concluded that the susceptibility of LBW infants to develop hypertension during adulthood is due to the inheritance of hypertension genes from the mother and not to an unfavorable intrauterine environment. Therein, a negative linear association has been assumed between genetically estimated maternal blood pressure (BP) and birth weight, while the observed relationship between maternal BP and birth weight is substantially different from that assumption. As many hypertension genes are likely involved in vasculature development and function, we hypothesized that BP-increasing genetic variants could affect birth weight by reducing the growth of the placenta, a highly vascular organ, without overtly elevating the maternal BP.
Methods
Using a birth cohort in the Japanese population possessing time-series fetal growth velocity data as a target and a GWAS summary statistics of BioBank Japan as a base data, we performed polygenic score (PGS) analyses for systolic BP (SBP), diastolic BP, mean arterial pressure, and pulse pressure. A causal mediation analysis was performed to assess the meditation effect of placental weight on birth weight reduced by maternal BP-increasing PGS. Maternal genetic risk score constituted of only “vasculature-related” BP single nucleotide polymorphisms (SNPs) was constructed to examine the involvement of vascular genes in the mediation effect of placental weight. We identified gestational week in which maternal SBP-increasing PGS significantly decreased fetal growth velocity.
Results
We observed that maternal SBP-increasing PGS was negatively associated with offspring birth weight. A causal mediation analysis revealed that a large proportion of the total maternal PGS effect on birth weight was mediated by placental weight. The placental mediation effect was remarkable when genetic risk score was constituted of “vasculature-related” BP SNPs. The inverse association between maternal SBP PGS and fetal growth velocity only became apparent in late gestation.
Conclusions
Our study suggests that maternal hypertension genes are strongly associated with placental growth and that fetal growth inhibition is induced through the intrauterine environment established by the placenta.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12916-021-02131-0.
Keywords: Intrauterine programming, Placenta, Blood pressure, Vascular genes, Developmental Origin of Health and Disease (DOHaD)
Background
The increasing prevalence of cardio-metabolic diseases leading to premature death is a raising concern [1]. Although major risk factors are lifestyle factors after birth, epidemiological studies have associated low birth weight (LBW) and/or fetal growth restriction (FGR) with hypertension, cardiovascular diseases, and type 2 diabetes, indicating the existence of prenatal risk factors [2–4]. However, the underlying mechanisms explaining the relationship between LBW/FGR and diseases in adulthood are not fully understood. It is suggested that maternal undernutrition and/or poor placental function could alter long-lasting body function and physiology, predisposing individuals to cardio-metabolic diseases [5, 6]. To analyze the effect of such intrauterine environment on fetal growth, the maternal genotype has been used as a proxy for the intrauterine environment [7, 8]. Maternal genetic factors may influence fetal growth directly through the alleles inherited by the fetus, or indirectly through the intrauterine environment, and this idea has been developed into the Mendelian Randomization (MR) approach in the framework of causal inference [7–10].
Recent MR studies have reported that maternal systolic blood pressure (SBP)-increasing polygenic score (PGS) causes lower birth weight through elevated maternal SBP, independently of direct fetal genetic effects [8, 10]. However, the genetic estimate of the association between maternal SBP and birth weight was in the opposite direction to the observational estimate [8]. In addition, hypertension usually develops in late life. Therefore, it may not be appropriate to apply to pregnant women the estimates of lifelong BP risks in the MR approach. Thus, it remains unclear why higher maternal SBP-increasing PGS results in lower birth weight.
FGR pathophysiology and etiology are complex, but most cases are thought to arise from placental dysfunction [4, 11]. Generally, placental growth precedes fetal growth, with the placental growth rate decreasing from about 30 weeks, and the fetus/placenta growth ratio gradually increasing until 37–38 weeks [12]. Nearly 80% of FGR are late-onset (≥ 32 weeks) [13]. In addition, it has been highlighted that placental weight is an important determinant of fetal growth in the third trimester [14], and birth and placental weight highly correlate [14, 15]. The placenta is a vascular organ, and recent GWAS uncovered numerous BP-associated genes involved in regulating the development and function of the vascular system [16–18]. Therefore, we hypothesized that BP-increasing maternal SNPs influence placental growth, which in turn affects birth weight.
Since the mediating role of the placenta was never been examined, we investigated whether maternal SBP-increasing PGS is inversely associated with placental weight and whether the placental weight mediates the effect of maternal SBP PGS on birth weight. Furthermore, by constructing a genetic BP-increasing risk score composed exclusively of vasculature-related SNPs, we aimed to clarify that the role of placental weight in the effects of vasculature-related BP SNPs on birth weight. We also aimed to confirm by haplotype analysis that maternal transmitted and non-transmitted BP-increasing alleles, but not paternal transmitted alleles, are inversely associated with birth and placental weight. Lowering of birth weight can be caused by deceleration of fetal growth velocity during pregnancy. Motivated to understand the indirect effect of maternal SBP PGS on fetal growth velocity, reflecting the fact that placental growth precedes fetal growth, we aimed to determine that maternal SBP PGS significantly decreases fetal growth velocity at the very end of pregnancy. Thus, our study uncovered that maternal genetic risk of hypertension inhibits fetal growth through the intrauterine environment established by the placenta.
Methods
Study cohorts
The characteristics of the two cohorts analyzed in this study are presented in Additional file 1 : Table S1. More details about the participants of these cohorts have been described previously [19–21]. The study population was comparable with the general Japanese pregnant women on perinatal parameters such as birth weight, maternal age, height, weight, body mass index (BMI), and BP [22, 23]. Chronic hypertension and hypertensive disorder of pregnancy (HDP) were excluded from this study because a previous study has shown that the effect of maternal SBP genetic score on birth weight is the same with and without HDP and hypertension [8]. Also, their frequency was low.
BC-GENIST
Clinical information and genotype data were obtained from the Birth Cohort Gene and ENvironment Interaction Study of Tokyo Medical and Dental University (TMDU) (BC-GENIST) project, which is a prospective mother-offspring cohort designed to evaluate the effects of prenatal environment and genotype on the epigenetic state of mothers and their offspring [19]. During the years 2015–2019, pregnant women in their first trimester were recruited to BC-GENIST at the TMDU hospital in an urban area of Japan, Tokyo (n = 126). All the participants provided written informed consent. Parents/guardians provided consent for their children to participate. Ninety-three mother-child pairs of Japanese ancestry, whose genotype information were available, were included in this study. There was neither HDP nor chronic hypertension.
TMDU pregnant women cohort
Clinical information including maternal BP and birth outcome were obtained from the retrospective cohort of women who gave birth at TMDU Hospital from 2013 to 2017 [20, 21]. The eligible criteria for this study were as follows: Japanese singleton delivery with available placental weight and live birth, without malformation, completing more than 34 weeks of gestation at the time of delivery. Maternal age was above 20 years and existing maternal BP data in two gestational periods (before 20 weeks and from 20 to 34 weeks) were available. In this study, three participants with HDP and nine with chronic hypertension were excluded. BC-GENIST participants were excluded. Total 993 women were eligible for this study. Informed consent was obtained in the form of opt-out on the website of TMDU Life Science and Bioethics Research Center.
This study was approved by the Institutional Review Board of TMDU and was conducted according to the Declaration of Helsinki.
Observational maternal BP and perinatal outcomes
The relationship between observational BP and birth weight was analyzed using the TMDU pregnant women cohort. BP was measured at prenatal check-ups scheduled every 4 weeks until 24 weeks, every 2 weeks between 24 and 36 weeks, and weekly beyond 36 weeks of gestation. Pulse pressure (PP) was calculated by subtracting the diastolic blood pressure (DBP) from the systolic blood pressure (SBP). The PP was divided by three and added to the DBP to calculate the mean arterial pressure (MAP) [24].
Hypertension of pregnancy is classified according to the time of onset, which is also thought to be different in its pathogenesis [25]. Chronic hypertension is defined if hypertension occurs before 20 weeks and early- and late-onset HDP if HDP occurs between 20 and 34 weeks and after 34 weeks, respectively. Therefore, we divided the gestation period into three categories: [1] early, gestational age < 20 weeks [2]; middle, 20 ≤ gestational age < 34 weeks; and [3] late, 34 weeks ≤ gestational age. For each pregnant woman, the mean value of SBP, DBP, MAP, and PP at each period was used for analysis.
Birth weight and placental weight were adjusted for gestational age, fetal sex, and parity using a reference chart [12, 26]. Estimated fetal growth velocity was calculated as described previously [20]. The relatively high frequency of routine ultrasound scans at prenatal checkups in Japan allowed to estimate the weekly values of estimated fetal weight (EFW) by smoothing splines interpolation using a generalized additive model. The weekly fetal growth velocity was computed as the difference between two consecutive weekly EFW values. To compare the genetic effect size across all the phenotypes using the BC-GENIST cohort, we scaled trait to have zero mean and unit variance by Z score transformation.
Genotyping and imputation of target data for polygenic score (PGS) analysis
The DNA was extracted from maternal peripheral blood and cord blood of the BC-GENIST participants using a standard procedure [19]. All samples were genotyped with the Illumina Infinium Asian Screening Array BeadChip by iScan, in accordance with the Illumina protocol, at the Center for Molecular Biology and Genetics/Core-Lab, Graduate School of Regional Innovation Studies, Mie University, Mie, Japan. Genotype calling was performed for all samples as a single project using the Genotyping Module (version 1.9) of the GenomeStudio data analysis software package. The quality control (QC) of participants and genotypes was performed using a standard procedure [27–30]. Briefly, there were no individuals with incorrect sex assignment, excessive heterozygosity, or low call rate (< 98%). There were no incorrect mother-child relationship and cryptic relatedness, as assessed by identity-by-descent (IBD) estimation. Principal component analysis (PCA) anchored with HapMap III reference samples confirmed that all samples taken were from individuals of East Asian descent. At a marker level, SNPs with low call rate (< 95%), low minor allele frequency (MAF; < 0.01), or significant deviation from Hardy-Weinberg equilibrium (p < 1 × 10−5) were excluded. We excluded non-autosomal chromosomes from the analysis.
Following QC procedures, we conducted genome-wide imputation using the 1000 Genome Phase 3 reference panel [31]. SNP alleles were oriented to the forward strand of the GRCh37/hg19 reference sequence of the human genome. Haplotype phasing and imputation were performed in all maternal and fetal samples using Beagle 5.1 software [32, 33]. After the imputation, we excluded variants with the measurement Dosage R-squared (DR2) < 0.7 or those with low MAF (< 0.01). The sample size was 93, which was equivalent to the minimum target sample size for PGS analysis [27].
Construction of individual PGSs
A classic clumping and thresholding method was used to derive individual polygenic scores (PGSs) for the target BC-GENIST participants. As a base data, we used GWAS summary statistics (the normalized effect sizes and p values) for BP phenotypes (SBP, DBP, MAP, and PP) from Japanese individuals (n > 136,000) from the BioBank Japan (BBJ) [34]. We performed QC relevant to base and target data for the PGS calculation [27]. The reported heritability estimates of SBP, DBP, MAP, and PP were 0.0569, 0.04, 0.0496, and 0.0438, respectively [35]. First, a set of independent variants was extracted using linkage disequilibrium (LD) clumping [30] with the following flags: --clump-p1 1 --clump-p2 1 --clump-r2 0.1 --clump-kb 1000. Next, we selected variants meeting the following p value thresholds: 1 × 10−6, 1 × 10−5, 1 × 10−4, and 1 × 10−3. The trait variance explained the derived PGSs by calculating the adjusted R2 attributable to the PGSs was mostly highest at the threshold of 1 × 10−4. We derived PGSs by multiplying the dosage of BP-increasing alleles for each variant by the normalized effect size in the GWAS and summing the scores across all the selected variants unless otherwise indicated. The PGSs were scaled to have zero mean and unit variance by Z score transformation to compare the effect sizes across the investigated phenotypes.
In order to clarify that the placenta specifically mediates the effect of vasculature-related SNPs among BP SNPs, we constructed a genetic BP-increasing risk score limited to vasculature-related SNPs. Previously, a large-scale of GWAS was performed for SBP, DBP, MAP, and PP, respectively [34], but the associated SNPs were highly overlapping across multiple BP phenotypes. Additional file 1-Table S2 shows 41 SNPs associated with SBP, DBP, MAP, and PP with genome-wide significance. As described in “Variant annotation and relevance to the vascular system” section, 41 SNPs were annotated for their relevance to the vasculature. Then, two distinct genetic risk scores were constructed: one from only “vasculature-related” SNPs and the other from “unlikely related” SNPs. Because the effect size of each SNP varies among the four BP phenotypes, alleles with SBP-increasing effect were counted in an unweighted manner. The reported directions of BP-increasing effects of 41 SNPs were mostly concordant for all BP phenotypes. The effect allele (which denotes the BP-increasing allele) of seven PP-associated SNP presented a DBP-decreasing effect (see gray cells in Additional file 1: Table S2). For these seven discordant SNPs, counting SBP-increasing alleles was rational because the direction was the same among PP, SBP, and MAP.
Determination of parental origin and computation of individual haplotype allele counts
For a series of genome-wide significant SNPs associated with any BP phenotypes (p < 5.0 × 10−8) reported by Kanai et al. [34], we estimated mother-offspring allele transmission for each mother-offspring pair after phasing and imputation using Beagle 5.1 software [32, 33]. When either or both mother and fetus were homozygote, the allelic transmission could be unambiguously determined. When both mother and fetus were heterozygote, allelic transmission from mother to child was inferred based on local haplotype sharing, following the method described by Zhang et al. [36]. For each SNP, we calculated three haplotype allele counts: [1] unweighted sum of the number of BP-increasing alleles in maternal transmitted haplotypes, [2] unweighted sum of the number of BP-increasing alleles in maternal non-transmitted haplotypes, and [3] unweighted sum of the number of BP-increasing alleles in paternal transmitted haplotypes.
Variant annotation and relevance to the vascular system
Genome-wide significant SNPs associated with BP phenotypes [34] were annotated with genes using data obtained on 12/18/2020 from multiple bioinformatic tools such as Variant Effect Predictor (VEP, Ensemble release 102) [37], SNPnexus [38], and post-GWAS [39]. We evaluated all SNPs in LD (r2 ≥ 0.8) with each variant for evidence of mediation of expression quantitative trait loci (eQTLs) in all 54 tissues using the GTEx database Release V8, to identify affected genes and tissues. GeneHancer database [40] was also used to identify genes potentially affected by SNPs (Additional file 1: Table S2-3).
For the relevance to the vascular system, we assessed all SNPs in LD (r2 ≥ 0.8) with each variant for evidence of the overlap with ENCODE DNase I regulatory regions and/or Candidate Cis-regulatory elements [38, 41] in blood vessels (umbilical vein endothelial cell [HUVEC]; brain microvascular endothelial cell [HBMEC]; lung microvascular epithelium blood [HMVEC-LBl]; brain vascular smooth muscle cell [HBVSMC]; pulmonary artery fibroblast [HPAF]; aorta fibroblast [AoAF]). The annotated gene relevance to the vasculature (function of the vascular smooth muscle, the vascular endothelial cells, the vascular tone, the vascular assembly, placental vasculature, and HDP; Additional file 1: Table S2-3) was deciphered by a literature review. Among 42 BP-associated SNPs reported [34], rs139293840 (located in RPTOR) was excluded for the analysis, as it is monomorphic in non-Asian population and there was no available GTEx data.
Statistical analyses
R software (version 4.0.3) was used for the statistical analyses. All tests were two-sided. All the variables were scaled by Z score transformation. Associations between PGSs and various phenotypes were examined by regression analysis. For the multiplicity adjustments, Bonferroni-adjusted p value was noted (Additional file 1: Table S4-10). Since only pre-pregnancy BMI (BMI was log-transformed) among several potential BP confounders (including maternal age, smoking status, and the presence or absence of glucose metabolism impairment) was associated with BP phenotypes, birth weight, and placental weight, the pre-pregnancy BMI was used as a confounder. The birth weight and placental weight used in this study were the variables adjusted for fetal sex, parity, and gestational age using a national reference chart.
Global Validation of Linear Model Assumptions (GVLMA) [42] and the Akaike information criterion (AIC) were used to evaluate whether a simple linear or a quadratic model was appropriate to explain the association between observed maternal BP and birth weight.
Since maternal SBP PGS (exposure) and placental weight (mediator), and placental weight (mediator) and offspring birth weight (outcome) were significantly associated, a causal mediation analysis was performed using the R package “mediation (ver.4.5.0)” [43, 44] to assess the meditation effect of placental weight. Pre-pregnancy BMI was a confounder for placental weight (mediator) and birth weight (outcome). The average causal mediation effects (ACME) were estimated to quantify the mediation effect of placental weight on offspring birth weight. Proportion mediated was derived from the ratio between ACME and total effect. We performed additional mediation analyses using SBP PGS constructed with SNPs not associated with type 2 diabetes mellitus (T2D), hemoglobin A1c (HbA1c), and BMI, as the exposure. Sensitivity analysis for sequential ignorability [43, 44] was performed to show the robustness of the mediator effect to the violations of the assumption, that is, the possible existence of unobserved confounders.
Association between haplotype-based BP-increasing allele counts and placental weight was examined by regression analysis using the polygenic allele counts of maternal transmitted, maternal non-transmitted, and paternal transmitted allele, respectively.
To visualize the relationship between BP-increasing PGS and fetal growth velocity, we stratified the participants according to the tertiles of normalized PGS.
A minimum required sample size of 47 for the linear regression was calculated with an alpha value of 0.05, a power of 0.80, and an R2 of 0.15 representing the moderate effect size, using the pwr.f2.test function in the pwr package [45].
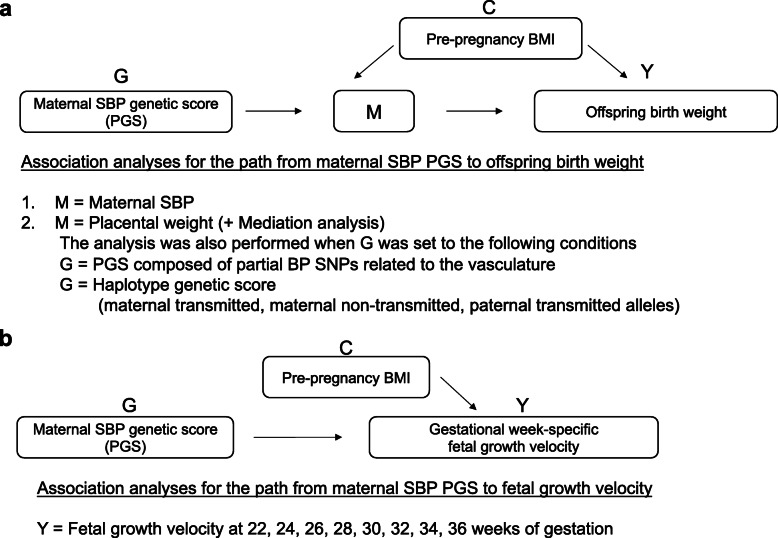
All the associations investigated in this study are schematically represented in Fig. 1.
Fig. 1.
Summary of the associations examined. a Schematic representation of the mediated association between the maternal SBP-increasing genetic score and offspring birth weight, and a summary of association analyses. b Schematic representation of the association between the maternal SBP-increasing genetic score and fetal growth velocity, and a summary of an association analysis. G, genetic score as an exposure; M, mediator as an intermediate phenotype; Y, outcome; C, confounder; PGS, polygenic score; SBP, systolic blood pressure; BMI, body mass index
Results
Study participants
The basic characteristics of the study participants are described in Additional file 1: Table S1, and no differences were observed between the BC-GENIST and the TMDU pregnant women cohorts in terms of maternal characteristics and birth outcomes. Briefly, less than 9% were overweight/obese while more than 17% were underweight (Additional file 1: Table S1). As stated in the “Methods” section, chronic hypertension and HDP were excluded in this study.
Association of BP-PGS with offspring birth weight and placental weight
High maternal PGS for each BP phenotype (SBP, DBP, MAP, or PP; exposure) was negatively associated with birth weight (outcome) (Additional file 1: Tables S4-7). Among four BP phenotypes, SBP-PGS (111 SNPs, GWAS p value threshold = 1.00 × 10−5) was inversely associated with birth weight with the highest significance (estimated regression coefficient [Est.; 95% CI] = − 0.340 [− 0.509, − 0.171], p = 1.29 × 10−4). Although association between maternal SBP-PGS and placental weight (potential mediator) was significant (Est. [95% CI] = − 0.396 [− 0.556, − 0.236], p = 3.98 × 10−6), there was no correlation between SBP-PGS and observational SBP traits (p = 0.736; Additional file 1: Tables S4).
Mediation models of the relationship between maternal SBP-PGS and offspring birth weight
As for potential mediator-outcome association, the linear regression model of birth weight (outcome) on placental weight (potential mediator) was well fitted and the Est. was 0.661 [95% CI 0.50, 0.82] (p value =1.7 × 10−12). In contrast, linear regression models of birth weight on SBP trait were not fitted well (Additional file 2: Figures S1-S3). In addition, placental weight was never negatively associated with BP traits (Additional file 1: Table S8).
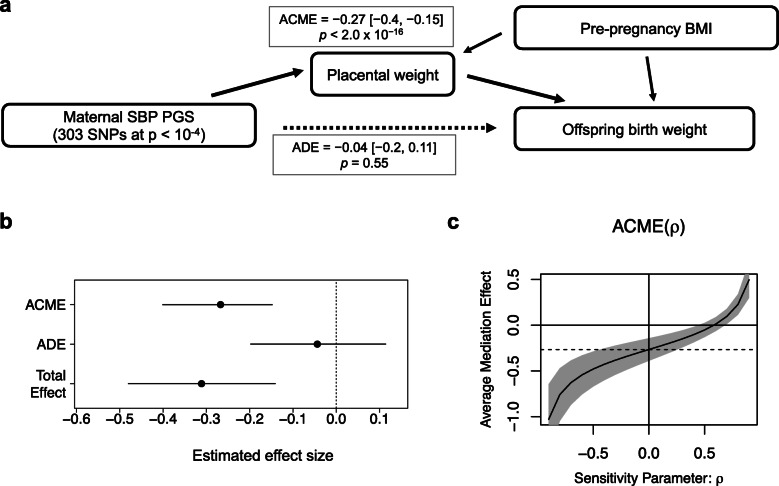
Causal mediation analysis with the quasi-Bayesian Monte Carlo method estimated that 86% of the effect of maternal SBP-increasing PGS on birth weight was mediated by placental weight (Fig. 2a, Additional file 1, Table S9). The average causal mediation effects (ACME) was − 0.27 [95% CI − 0.40, − 0.15] (p value < 2.0 × 10−16) whereas the average direct effects (ADE) was − 0.049 [− 0.21, 0.12] (p value = 0.54; Additional file 1: Table S9 and Figure 2b). Even after excluding pleiotropic SNPs associated with either BMI, T2D, or HbA1c at p value thresholds of 1 × 10−8, 1 × 10−6, or 1 × 10−4, the mediation effect estimates of placental weight were not changed (Additional file 1: Table S9). To assess the extent of estimate robustness to plausible violation of assumption on unmeasured confounder, we performed a sensitivity analysis for sequential ignorability [43, 44] (Fig. 2c). The ACME estimates were not altered much for a wide range of ρ values below 0.6, suggesting that the mediation effects are largely robust to potential violation for sequential ignorability assumption which includes the ignorability assumption of unmeasured variables that confound the relationship between the mediator and the outcome.
Fig. 2.
Causal mediation analysis. a, b Mediation model of the relationship between maternal SBP-increasing PGS (exposure), placental weight (mediator), and birth weight (outcome). Placental weight has a significant average causal mediation effect (ACME) for decreasing birth weight by maternal SBP PGS (effect = − 0.27 [− 0.4, − 0.15], p < 2.0 × 10−16), whereas the average direct effect (ADE) is not significant (effect = − 0.04 [− 0.2, 0.11], p = 0.55). c The sensitivity parameter ρ denotes the correlation coefficient between the residuals of the mediator and outcome regressions [44]. A sensitivity analysis performed by examining how the estimated ACME changes while the value of ρ varies shows that ACME estimates are negative and not altered for a wide range of ρ values below 0.6
Causal mediation analysis for other significantly birth weight-associated PGS, SBP-PGS (111 SNPs, p value thresholds = 1 × 10−5), and PP-PGS (29 SNPs, p value thresholds = 1 × 10−6) estimated that 70% and 72%, respectively, of the effect of maternal BP-increasing PGS on birth weight was mediated by placental weight (Additional file 2: Figure S4).
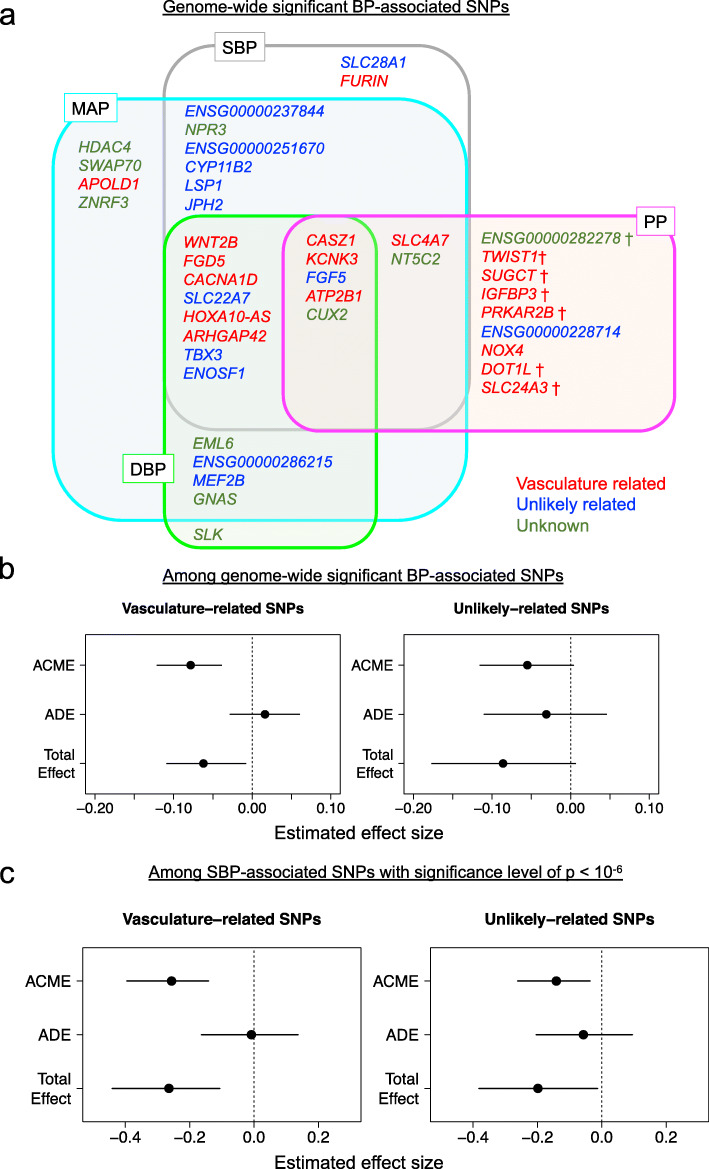
The placenta mediates the effect of vasculature-related BP-increasing SNPs on offspring birth weight
To focus on the relevance to the vasculature, we constructed a maternal genetic risk score limited to vasculature-related SNPs from 41 SNPs associated with SBP, DBP, MAP, and PP identified by Kanai et al. [34] with genome-wide significance (Additional file 1: Table S2 and Fig. 3a). Of the 41 SNPs, 18 were in the “vasculature-related,” 12 in the “unlikely related,” and 11 in the “unknown” classification (Fig. 3a). Whereas “vasculature-related” genetic risk score was inversely associated with birth weight (Est. (change in birth weight z score per allele) = − 0.06 [− 0.12, − 0.01]; p = 2.5 × 10−2) and placental weight (Est. = − 0.11 [− 0.16, − 0.06]; p = 1.7 × 10−5), “unlikely-related” genetic risk score was associated neither with birth weight (p = 0.087), nor with placental weight (p = 0.083). Causal mediation analysis estimated nearly 100% of the effect of “vasculature-related” genetic score on birth weight was mediated by placental weight (Fig. 3b).
Fig. 3.
Placental weight mediates the effects of "vasculature-related" blood pressure SNPs on birth weight. a Venn diagram of 41 genome-wide significant single nucleotide polymorphisms (SNPs) for BP phenotypes. There is a considerable overlap of association across four BP phenotypes, with a consistent direction of the BP increasing effect, except for seven loci that present opposite (BP decreasing) or unclear effect directions for DBP (indicated by †). SNPs are classified into “vasculature-related” (red), “unlikely related” (blue), and “unknown” (green) groups, respectively, as described in the results and Additional File 1: Table S2. b Mediation analysis of the models of either the PGS with vasculature-related BP SNPs (left) and unlikely related BP SNPs (right) as an exposure variable. Maternal PGS of “vasculature-related” SNPs shows a birth weight reducing effect (total effect = − 0.06 [− 0.11, − 0.01], p = 0.032) and placental weight has a significant mediation effect (ACME = − 0.08 [− 0.12, − 0.04], p < 2.0 × 10−16). Maternal PGS of “unlikely-related” SNPs do not significantly reduce birth weight (total effect = − 0.09 [− 0.18, 0.01], p = 0.082). c Mediation analysis of the models of either the SBP-increasing PGS with “vasculature-related” SNPs (left) and with “unlikely related” SNPs (right) as an exposure variable. Of the total effect of “vasculature-related” PGS on birth weight (total effect = − 0.26 [− 0.44, − 0.11], p = 0.002), the mediated effect by placental weight accounts for the most part (ACME = − 0.26 [− 0.40, − 0.14], p < 2.0 × 10−16). Smaller portion (around 69%) of the total effect of “unlikely related” PGS (total effect = − 0.20 [− 0.38, − 0.01], p = 0.034) is mediated by placental weight (ACME = − 0.14 [− 0.26, − 0.04], p = 0.01)
To confirm that the association of “vasculature-related” genetic risk score with placental weight was not due to the larger number of SNPs, we also performed a similar subdivided PGS analysis, using the top 67 SBP-SNPs (SBP association GWAS p value < 1 × 10-6; Additional file 1: Table S3). Of these, 21 were in the “vasculature related,” 30 in the “unlikely related,” and 16 in the “unknown” classification. The “vasculature-related” PGS was more strongly associated with birth weight than the “unlikely related” PGS and was associated with birth weight (Est. (change in birth weight z score per 1 SD increase of PGS) = − 0.26 [− 0.44, − 0.09]; p = 3.6 × 10−3) and placental weight (Est. = − 0.39 [− 0.55, − 0.23]; p = 5.7 × 10−6). Causal mediation analysis estimated 96% of the “vasculature-related” PGS effect was mediated by the placental weight (Fig. 3c).
Haplotype-based genetic score analysis confirmed the role of maternal alleles
To determine the relative contributions of maternal and fetal genotypes to the relationship between BP-increasing alleles and birth weight/placental weight, we estimated mother-offspring allele transmission based on local haplotype sharing [36] for the BP-associated SNPs with genome-wide significance [34] (Fig. 3a). Both the transmitted and non-transmitted maternal haplotype genetic scores (allele counts) were inversely correlated with birth weight (Est. = − 0.07 [− 0.13, − 0.011], p = 2.1 × 10−2; Est. = − 0.092 [− 0.16, − 0.026], p = 6.8 × 10−3, respectively). On the contrary, we did not observe any correlation between paternally inherited haplotype genetic score and birth weight (p = 0.25; Additional file 1: Table S10). Similarly, both transmitted and non-transmitted maternal genetic scores were inversely associated with placental weight (Est. = − 0.14 [− 0.19, − 0.082], p = 2.3 × 10−6; Est. = − 0.094 [− 0.16, − 0.029], p = 4.8 × 10−3, respectively), whereas there was no association with paternally inherited haplotype genetic score (p = 0.25; Additional file 1: Table S10).
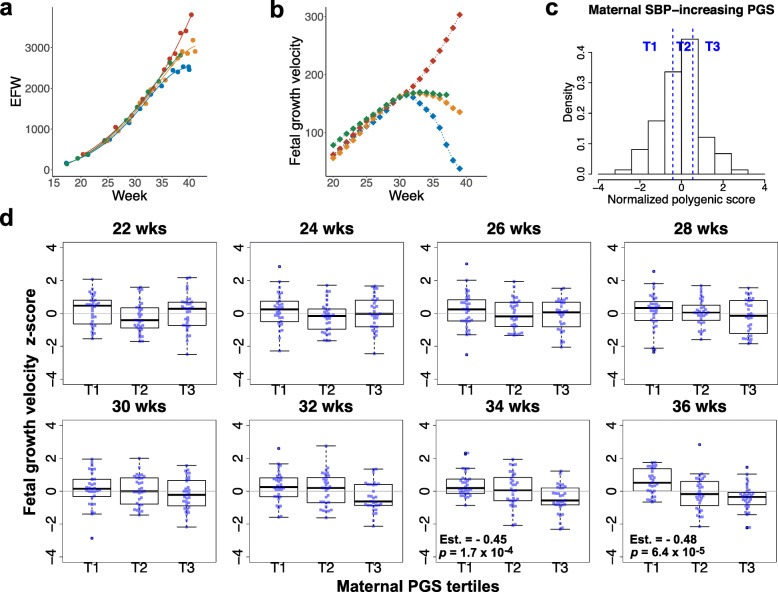
The inverse association between maternal SBP PGS and fetal growth velocity only became apparent in late gestation
We collected longitudinal ultrasound measurements of estimated fetal weight (EFW) and estimated the weekly values of EFW by smoothing splines interpolation (Fig. 4a). We then differentiated them to calculate fetal growth velocity every week (individual changes in EFW per week; Fig. 4b) and normalized them by z score transformation. We stratified the participants according to the tertiles of maternal SBP-increasing PGS consisting of SNPs meeting the p value threshold of 1.0 × 10−4 (Fig. 4c). Linear regression analysis was performed every two weeks from 22 to 36 weeks, and the results showed that the inverse association between maternal SBP-increasing PGS and fetal growth velocity became progressively apparent towards 36 weeks (Fig. 4d).
Fig. 4.
Effects of maternal SBP-increasing PGS on gestational week-specific fetal growth velocity. a Estimation of gestational week-specific estimated fetal weight (EFW) for individual fetus. Longitudinal ultrasound scan data at prenatal checkups are collected for individual fetus (colored circles) and the weekly values (continuous values) of EFW was estimated by smoothing splines interpolation. Data examples for four fetuses are shown (each fetus with a different color). b Gestational week-specific fetal growth velocity was calculated as the difference between two consecutive weekly EFW values. Fetuses are shown the same color as in a. c Distribution of normalized maternal SBP-increasing polygenic score (PGS) constituted of a set of SNPs exceeding a GWAS association p value of 1.0 × 10−4 and the stratification according to the tertiles. d Fetal growth velocity across maternal PGS tertiles. Each subject (n = 93) is shown in the box-and-whisker plots, with the boxes indicating the median and interquartile range and the whiskers denoting the range. Regression coefficient (Est.), standing for the change per strata increase, and p value are shown when p value is below the Bonferroni-corrected threshold for 8 tests (p = 6.3 × 10−3)
Discussion
This is the first study to show that placental weight mediates the effect of maternal SBP-increasing PGS on lowering birth weight. While we found a notable inverse association between maternal genetic score and placental weight, observational BP traits were not associated with BP genetic score. In addition, placental weight well correlated with birth weight, whereas no correlation was observed between observational BP and birth weight. PGS constituted of BP SNPs only related to the vascular system also had a reducing effect on birth weight, and this effect was mediated by the placental weight. Additionally, we put in evidence that both maternal transmitted and non-transmitted alleles of BP-increasing SNPs, but not paternal transmitted alleles, affect birth weight. The association between maternal SBP PGS and deceleration of fetal growth velocity only appeared later in gestation, consistent with a placental mediation of the effect of maternal hypertension genetic risk on birth weight.
Previous MR studies of the European ancestry population have consistently reported an inverse association between maternal SBP-increasing PGS and birth weight [7, 8, 10]. In the present study based on Japanese pregnant women, we replicated this association with linear regression analyses, although SNPs constituting PGS for the Japanese population differed from those for the European population.
Using MR analysis, Tyrrell et al. estimated that every 10 mmHg increase of the maternal SBP is genetically associated with a 208-g decrease in birth weight [8]. However, they observed that a 10-mmHg increase in measured maternal SBP was associated with a 24-g increase in birth weight [8]. That is, the direction of the observed association was opposite to the estimated genetic association. This was inconsistent with the assumption that SBP traits mediate the effect of maternal SBP genetic score on birth weight, but it was thought to be attributed to confounding, such as BMI. Since then, this issue has not been fully explained. Our results indicate that it is unlikely that maternal BP traits mediate the effect of maternal BP PGS on birth weight, even when pre-pregnancy BMI is included as a confounder in the analysis. In contrast, the present study found that maternal SBP increasing genetic score was associated with reducing placental weight, and placental weight correlated with birth weight. A mediation analysis showed that more than 70% of the effect of maternal SBP increasing PGS on birth weight was mediated by placental weight. The results of the mediation analysis were not altered by the exclusion of SNPs associated with BMI, HbA1c, and T2D among the SBP-associated SNPs. Furthermore, the result of our sensitivity analysis for sequential ignorability [43, 44] also showed that even if there were unmeasured confounders, they would not affect the conclusion that the placenta mediates the effect of SBP PGS on birth weight.
Genes associated with hypertension have been identified by recent GWAS [16–18], and beyond genetic variants that work in the kidney and adrenal glands, many SNPs have been shown to be related to vascular function, vascular development, angiogenesis, and remodeling. This prompted us to subdivide BP SNPs into either vasculature-related or unlikely-related groups and examine the association of their genetic scores with birth weight. We observed that the genetic score of SNPs related to the vascular system presented a higher association with birth weight, and this was mostly mediated by placental weight.
To analyze the maternal genetic score as a proxy for the intrauterine environment, Beaumont, Warrington, and their colleague developed a method of analysis that distinguishes it from the effects of genetic factors shared by the fetus [7, 10]. They showed that the effect of the SBP-increasing alleles on lowering birth weight originated from maternal alleles. In the present study, we used a method [36] to calculate genetic scores separately for maternal transmitted, maternal non-transmitted, and paternal transmitted alleles, and confirmed that the effects of BP-increasing alleles on birth weight and placental weight were only observed for maternal alleles. The results are in agreement with previous studies [7, 10].
Fetal growth restriction (FGR) is characterized as a growth deceleration from a certain point in the gestation period, resulting in fetus pathologically small for the gestation period (SGA), which is different from constitutionally SGA [4, 46]. As most FGR are thought to arise from placental dysfunction, which matures in the 3rd trimester and slows down its growth after around 30 weeks, it appears reasonable that nearly 80% of FGR are late-onset (≥ 32 weeks) [13]. When and how the fetal growth velocity changes are important information. We previously calculated the EFW increase per week (differential value) every week, which is called fetal growth velocity, for individual fetuses and analyzed the trajectories of the velocity. We have shown that the heterogeneity of growth velocity trajectories is most pronounced after 30 weeks of gestation [20]. Individual trajectories analysis highlighted the continuity of the degree of growth restriction, and ≥ 10% of the fetuses showed a third-trimester growth deceleration. Considering the time sequence of events, maternal PGS should be associated with fetal growth velocity in late gestation where placental maturation is proceeding. As expected, the inverse association between maternal SBP-increasing PGS and fetal growth velocity became progressively apparent towards 36 weeks. This result, although indirect, further supports a placental mediation of the effects of maternal BP genetic score on birth weight.
The NICHD Fetal Growth Study, which explored the association between maternal SBP (or DBP)-increasing PGS and EFW for each trimester, has been recently reported [47]. A unique feature of the NICHD study is that ethnically different populations (Hispanic, non-Hispanic White, non-Hispanic Black, and Asian) were included in the analysis. The authors referred to the GWAS summary statistics of European ancestry to construct PGS and separately applied it to all distinct target populations. However, it is well known that PGS analyses using the summary statics of ethnically different population from the target population are not reliable [27, 48]. In addition, since the frequency of ultrasound measurements was not very high, the estimation of each individual gestational week-specific EFW might have not been accurate. In our analysis, the study target population was limited to Japanese, and PGS analysis was performed using summary statistics of Japanese GWAS to obtain reliable results. In addition, we were able to collect a much larger number of ultrasound measurements for every fetus so that we could obtain weekly EFW values and their differentiated value, fetal growth velocity [20]. We focused our analysis on the association between the gestational week-specific fetal growth velocity and maternal SBP PGS, and we found that this association only became apparent late in gestation.
Up to now, maternal genetic scores associated with SBP, DBP, BMI, and T2D or birth weight-associated SNPs were used as a proxy for the intrauterine environment to validate Developmental Origin of Health and Disease (DOHaD) hypothesis [7–10]. Recent MR studies have concluded that the intrauterine environment is unlikely to be a major determinant of adverse cardiometabolic outcomes in offspring [10]. However, our study reveals a significant association between placental weight and maternal PGS composed of partial BP SNPs related to the vasculature. This result suggests that it is possible to design a maternal genetic score representing the intrauterine environment much better. A large placental weight GWAS using mother and child genome will be needed to investigate the association between the maternal genetic score related to placental weight and the offspring’s birth weight and cardiometabolic traits in adulthood. Alternatively, since placental function may not necessarily correlate with placental weight, we need to devise a way to evaluate the genetic score that more directly reflects the intrauterine environment. It will also be interesting to see what the impact on the cardiometabolic outcome of the offspring will be in MR approach if maternal BP SNPs are limited to the vasculature and/or placenta-related SNPs. In any case, we think more analyses need to be performed before intrauterine programming is ruled out.
The main strength of our study was using the cohort of mother-offspring pair cohort that contains unique phenotype data for time-series fetal growth velocity and placental weight as well as genotype. In addition, birth weight and placental weight were ideally adjusted for gestational age, fetal sex, and maternal parity to eliminate well-known confounding factors. Pre-pregnancy BMI was also considered as a confounding factor. Using causal mediation analysis, we found for the first time that the effects of maternal SBP PGS on birth weight are mediated by placental weight. However, some limitations should be noted. First, the sample size of the cohort with available genotype was small, around 100, which is the minimum target sample size for PGS analysis [27]. The association between SBP-PGS and placenta was much stronger than the association between typical PGS and the corresponding traits; the variance of placenta trait explained by the PGS, represented by adjusted R2, exceeded 0.2; therefore, we were able to perform statistically reliable association analysis with this sample size. Nevertheless, the results of this study will need to be replicated in another cohort possessing complete data of fetal growth velocity and placental weight. Second, we classified PGSs based on literature and open-source data on gene activities and chromatin status in vascular tissues for the genes affected by SNPs. Although these methods were commonly used in previous studies [16–18], some information is not yet complete and will improve as more data accumulate.
Conclusion
In the present study, we show that maternal hypertension genes are strongly associated with placental growth and that maternal genetic risk of hypertension inhibits fetal growth through the intrauterine environment established by the placenta. Our finding is highly important for the perinatal management of FGR. Given that many FGRs are late-onset and difficult to diagnose [4, 11, 13], maternal SBP-PGS will be useful to the screening for late-onset FGR high-risk groups, regardless of the presence or absence of maternal hypertension. It cannot be dismissed that suboptimal intrauterine environment due to reduced placenta growth could generate future hypertension in LBW offspring. This study reconciles the long-held debate on the prenatal origin of diseases, adverse intrauterine environment or genetic effects, and will contribute to the prevention of hypertension and cardiovascular diseases.
Supplementary Information
Additional file 1: Table S1. Characteristics of participants included in this study. Table S2. Genome-wide significant loci for blood pressure phenotypes and classification based on vasculature relevance. Table S3. Variants constituting SBP-increasing PGS at p value threshold of 1 x 10−6 and classification based on vasculature relevance. Table S4. Linear regression analyses for maternal SBP-increasing PGS predicting various traits including birth weight. Table S5. Linear regression analyses for maternal DBP-increasing PGS predicting various traits including birth weight. Table S6. Linear regression analyses for maternal MAP-increasing PGS predicting various traits including birth weight. Table S7. Linear regression analyses for maternal PP-increasing PGS predicting various traits including birth weight. Table S8. Linear regression analyses for maternal BP traits predicting placental weight. Table S9. Sensitivity analysis for estimates of the causal mediation analyses by excluding pleotropic SNPs from exposure PGS.Table S10. Linear regression analyses for BP-increasing allele predicting birth weight or placental weight.
Additional file 2: Figure S1. Relationship between maternal BP in early gestation and offspring birth weight. Figure S2. Relationship between maternal BP in mid gestation and offspring birth weight. Figure S3. Relationship between maternal BP in late gestation and offspring birth weight. Figure S4. Estimates of mediation analyses with different PGS (exposure variable).
Acknowledgements
We are indebted to the participants of this study. This study was in part based on clinical materials and information from BioBank at the Bioresource Research Center, TMDU. The data used for the analyses described in this manuscript were obtained from the GTEx Portal on 12/18/2020. The GWAS summary statistics were obtained from the BBJ project.
Abbreviations
- ACME
Average causal mediation effects
- ADE
Average direct effects
- AIC
Akaike information criterion
- BBJ
BioBank Japan
- BC-GENIST
Birth Cohort Gene and ENvironment Interaction Study of TMDU
- BP
Blood pressure
- CI
Confidence interval
- DBP
Diastolic blood pressure
- DOHaD
Developmental Origin of Health and Disease
- EFW
Estimated fetal weight
- eQTL
Expression quantitative trait loci
- FGR
Fetal growth restriction
- GVLMA
Global Validation of Linear Model Assumptions
- GWAS
Genome wide association study
- HbA1c
Hemoglobin A1c
- HDP
Hypertensive disorder of pregnancy
- IBD
Identity-by-descent
- LBW
Low birth weight
- LD
Linkage disequilibrium
- MAF
Minor allele frequency
- MAP
Mean arterial pressure
- MR
Mendelian randomization
- PCA
Principal component analysis
- PGS
Polygenic score
- PP
Pulse pressure
- QC
Quality control
- SBP
Systolic blood pressure
- SGA
Small for gestational age
- SNP
Single nucleotide polymorphism
- T2D
Type 2 diabetes mellitus
- TMDU
Tokyo Medical and Dental University
- VEP
Variant Effect Predictor
Authors’ contributions
N.S., A.F, C.I, H.T, I.T, T.A, S.Y., M.O., and N.M. collected the BC-GENIST samples. N.M. collected TMDU pregnant women samples. N.S. contributed to data cleaning, statistical analysis, overall study design, and writing of the manuscript. S.M. and N. M. supervised the study. The authors read and approved the final manuscript.
Funding
This study was partly supported by JSPS KAKENHI Grant Number JP 20 K09594 to N.S.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Our study was approved by the Institutional Review Board of the Medical Research Institute and Faculty of Medicine, TMDU (No. G2000-181, M2017-337), and was conducted according to the Declaration of Helsinki. All the participants of BC-GENIST provided written informed consent. The parents/guardians provided consent for their children to participate. Informed consent of TMDU pregnant women was obtained in the form of opt-out on the website of TMDU Life Science and Bioethics Research Center.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflicts of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.NCD Countdown 2030 collaborators NCD Countdown 2030: worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal target 3.4. Lancet. 2018;392(10152):1072–1088. doi: 10.1016/S0140-6736(18)31992-5. [DOI] [PubMed] [Google Scholar]
- 2.Barker DJ, Hales CN, Fall CH, Osmond C, Phipps K, Clark PM. Type 2 (non-insulin-dependent) diabetes mellitus, hypertension and hyperlipidaemia (syndrome X): relation to reduced fetal growth. Diabetologia. 1993;36(1):62–67. doi: 10.1007/BF00399095. [DOI] [PubMed] [Google Scholar]
- 3.Knop MR, Geng TT, Gorny AW, Ding R, Li C, Ley SH, Huang T. Birth weight and risk of type 2 diabetes mellitus, cardiovascular disease, and hypertension in adults: a meta-analysis of 7 646 267 participants from 135 studies. J Am Heart Assoc. 2018;7(23):e008870. doi: 10.1161/JAHA.118.008870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crispi F, Miranda J, Gratacós E. Long-term cardiovascular consequences of fetal growth restriction: biology, clinical implications, and opportunities for prevention of adult disease. Am J Obstet Gynecol. 2018;218(2S):S869–SS79. doi: 10.1016/j.ajog.2017.12.012. [DOI] [PubMed] [Google Scholar]
- 5.Barker DJ. The origins of the developmental origins theory. J Intern Med. 2007;261(5):412–417. doi: 10.1111/j.1365-2796.2007.01809.x. [DOI] [PubMed] [Google Scholar]
- 6.Hanson MA, Gluckman PD. Early developmental conditioning of later health and disease: physiology or pathophysiology? Physiol Rev. 2014;94(4):1027–1076. doi: 10.1152/physrev.00029.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beaumont RN, Warrington NM, Cavadino A, Tyrrell J, Nodzenski M, Horikoshi M, Geller F, Myhre R, Richmond RC, Paternoster L, Bradfield JP, Kreiner-Møller E, Huikari V, Metrustry S, Lunetta KL, Painter JN, Hottenga JJ, Allard C, Barton SJ, Espinosa A, Marsh JA, Potter C, Zhang G, Ang W, Berry DJ, Bouchard L, Das S, Early Growth Genetics (EGG) Consortium. Hakonarson H, Heikkinen J, Helgeland Ø, Hocher B, Hofman A, Inskip HM, Jones SE, Kogevinas M, Lind PA, Marullo L, Medland SE, Murray A, Murray JC, Njølstad PR, Nohr EA, Reichetzeder C, Ring SM, Ruth KS, Santa-Marina L, Scholtens DM, Sebert S, Sengpiel V, Tuke MA, Vaudel M, Weedon MN, Willemsen G, Wood AR, Yaghootkar H, Muglia LJ, Bartels M, Relton CL, Pennell CE, Chatzi L, Estivill X, Holloway JW, Boomsma DI, Montgomery GW, Murabito JM, Spector TD, Power C, Järvelin MR, Bisgaard H, Grant SFA, Sørensen TIA, Jaddoe VW, Jacobsson B, Melbye M, McCarthy MI, Hattersley AT, Hayes MG, Frayling TM, Hivert MF, Felix JF, Hyppönen E, Lowe WL, Jr, Evans DM, Lawlor DA, Feenstra B, Freathy RM. Genome-wide association study of offspring birth weight in 86 577 women identifies five novel loci and highlights maternal genetic effects that are independent of fetal genetics. Hum Mol Genet. 2018;27(4):742–756. doi: 10.1093/hmg/ddx429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tyrrell J, Richmond RC, Palmer TM, Feenstra B, Rangarajan J, Metrustry S, Cavadino A, Paternoster L, Armstrong LL, de Silva NMG, Wood AR, Horikoshi M, Geller F, Myhre R, Bradfield JP, Kreiner-Møller E, Huikari V, Painter JN, Hottenga JJ, Allard C, Berry DJ, Bouchard L, Das S, Evans DM, Hakonarson H, Hayes MG, Heikkinen J, Hofman A, Knight B, Lind PA, McCarthy MI, McMahon G, Medland SE, Melbye M, Morris AP, Nodzenski M, Reichetzeder C, Ring SM, Sebert S, Sengpiel V, Sørensen TIA, Willemsen G, de Geus EJC, Martin NG, Spector TD, Power C, Järvelin MR, Bisgaard H, Grant SFA, Nohr EA, Jaddoe VW, Jacobsson B, Murray JC, Hocher B, Hattersley AT, Scholtens DM, Davey Smith G, Hivert MF, Felix JF, Hyppönen E, Lowe WL, Jr, Frayling TM, Lawlor DA, Freathy RM, for the Early Growth Genetics (EGG) Consortium Genetic evidence for causal relationships between maternal obesity-related traits and birth weight. JAMA. 2016;315(11):1129–1140. doi: 10.1001/jama.2016.1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Richmond RC, Hemani G, Tilling K, Davey Smith G, Relton CL. Challenges and novel approaches for investigating molecular mediation. Hum Mol Genet. 2016;25(R2):R149–RR56. doi: 10.1093/hmg/ddw197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Warrington NM, Beaumont RN, Horikoshi M, Day FR, Helgeland Ø, Laurin C, et al. Maternal and fetal genetic effects on birth weight and their relevance to cardio-metabolic risk factors. Nat Genet. 2019;51(5):804–814. doi: 10.1038/s41588-019-0403-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nardozza LM, Caetano AC, Zamarian AC, Mazzola JB, Silva CP, Marçal VM, et al. Fetal growth restriction: current knowledge. Arch Gynecol Obstet. 2017;295(5):1061–1077. doi: 10.1007/s00404-017-4341-9. [DOI] [PubMed] [Google Scholar]
- 12.Ogawa M, Matsuda Y, Nakai A, Hayashi M, Sato S, Matsubara S. Standard curves of placental weight and fetal/placental weight ratio in Japanese population: difference according to the delivery mode, fetal sex, or maternal parity. Eur J Obstet Gynecol Reprod Biol. 2016;206:225–231. doi: 10.1016/j.ejogrb.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 13.Malhotra A, Allison BJ, Castillo-Melendez M, Jenkin G, Polglase GR, Miller SL. Neonatal morbidities of fetal growth restriction: pathophysiology and impact. Front Endocrinol (Lausanne) 2019;10:55. doi: 10.3389/fendo.2019.00055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roland MC, Friis CM, Voldner N, Godang K, Bollerslev J, Haugen G, et al. Fetal growth versus birthweight: the role of placenta versus other determinants. PLoS One. 2012;7(6):e39324. doi: 10.1371/journal.pone.0039324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salafia CM, Zhang J, Charles AK, Bresnahan M, Shrout P, Sun W, Maas EM. Placental characteristics and birthweight. Paediatr Perinat Epidemiol. 2008;22(3):229–239. doi: 10.1111/j.1365-3016.2008.00935.x. [DOI] [PubMed] [Google Scholar]
- 16.Evangelou E, Warren HR, Mosen-Ansorena D, Mifsud B, Pazoki R, Gao H, et al. Genetic analysis of over 1 million people identifies 535 new loci associated with blood pressure traits. Nat Genet. 2018;50(10):1412–1425. doi: 10.1038/s41588-018-0205-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Giri A, Hellwege JN, Keaton JM, Park J, Qiu C, Warren HR, et al. Trans-ethnic association study of blood pressure determinants in over 750,000 individuals. Nat Genet. 2019;51(1):51–62. doi: 10.1038/s41588-018-0303-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Warren HR, Evangelou E, Cabrera CP, Gao H, Ren M, Mifsud B, Ntalla I, Surendran P, Liu C, Cook JP, Kraja AT, Drenos F, Loh M, Verweij N, Marten J, Karaman I, Lepe MP, O'Reilly PF, Knight J, Snieder H, Kato N, He J, Tai ES, Said MA, Porteous D, Alver M, Poulter N, Farrall M, Gansevoort RT, Padmanabhan S, Mägi R, Stanton A, Connell J, Bakker SJ, Metspalu A, Shields DC, Thom S, Brown M, Sever P, Esko T, Hayward C, van der Harst P, Saleheen D, Chowdhury R, Chambers JC, Chasman DI, Chakravarti A, Newton-Cheh C, Lindgren CM, Levy D, Kooner JS, Keavney B, Tomaszewski M, Samani NJ, Howson JM, Tobin MD, Munroe PB, Ehret GB, Wain LV, International Consortium of Blood Pressure (ICBP) 1000G Analyses. BIOS Consortium. Lifelines Cohort Study. Understanding Society Scientific group. CHD Exome+ Consortium. ExomeBP Consortium. T2D-GENES Consortium. GoT2DGenes Consortium. Cohorts for Heart and Ageing Research in Genome Epidemiology (CHARGE) BP Exome Consortium. International Genomics of Blood Pressure (iGEN-BP) Consortium. UK Biobank CardioMetabolic Consortium BP working group Genome-wide association analysis identifies novel blood pressure loci and offers biological insights into cardiovascular risk. Nat Genet. 2017;49(3):403–415. doi: 10.1038/ng.3768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pavethynath S, Imai C, Jin X, Hichiwa N, Takimoto H, Okamitsu M, et al. Metabolic and immunological shifts during mid-to-late gestation influence maternal blood methylation of CPT1A and SREBF1. Int J Mol Sci. 2019;20(5):1066. doi: 10.3390/ijms20051066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sato N, Miyasaka N. Heterogeneity in fetal growth velocity. Sci Rep. 2019;9(1):11304. doi: 10.1038/s41598-019-47839-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sato N, Miyasaka N. Stratified analysis of the correlation between gestational weight gain and birth weight for gestational age: a retrospective single-center cohort study in Japan. BMC Pregnancy Childbirth. 2019;19(1):402. doi: 10.1186/s12884-019-2563-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morisaki N, Nagata C, Yasuo S, Morokuma S, Kato K, Sanefuji M, Shibata E, Tsuji M, Senju A, Kawamoto T, Ohga S, Kusuhara K, Japan Environment and Children’s Study Group Optimal protein intake during pregnancy for reducing the risk of fetal growth restriction: the Japan Environment and Children's Study. Br J Nutr. 2018;120(12):1432–1440. doi: 10.1017/S000711451800291X. [DOI] [PubMed] [Google Scholar]
- 23.Watanabe N, Bokuda K, Fujiwara T, Suzuki T, Mito A, Morimoto S, Jwa SC, Egawa M, Arai Y, Suzuki F, Sago H, Ichihara A. Soluble (pro)renin receptor and blood pressure during pregnancy: a prospective cohort study. Hypertension. 2012;60(5):1250–1256. doi: 10.1161/HYPERTENSIONAHA.112.197418. [DOI] [PubMed] [Google Scholar]
- 24.DeMers D, Wachs D. Physiology, mean arterial pressure. In StatPearls. Treasure Island (FL): StatPearls Publishing; 2021. https://www.ncbi.nlm.nih.gov/books/NBK538226/ [PubMed]
- 25.Brown MA, Magee LA, Kenny LC, Karumanchi SA, McCarthy FP, Saito S, Hall DR, Warren CE, Adoyi G, Ishaku S, International Society for the Study of Hypertension in Pregnancy (ISSHP) Hypertensive disorders of pregnancy: ISSHP Classification, Diagnosis, and Management Recommendations for International Practice. Hypertension. 2018;72(1):24–43. doi: 10.1161/HYPERTENSIONAHA.117.10803. [DOI] [PubMed] [Google Scholar]
- 26.Itabashi K, Miura F, Uehara R, Nakamura Y. New Japanese neonatal anthropometric charts for gestational age at birth. Pediatr Int. 2014;56(5):702–708. doi: 10.1111/ped.12331. [DOI] [PubMed] [Google Scholar]
- 27.Choi SW, Mak TS, O'Reilly PF. Tutorial: a guide to performing polygenic risk score analyses. Nat Protoc. 2020;15(9):2759–2772. doi: 10.1038/s41596-020-0353-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Anderson CA, Pettersson FH, Clarke GM, Cardon LR, Morris AP, Zondervan KT. Data quality control in genetic case-control association studies. Nat Protoc. 2010;5(9):1564–1573. doi: 10.1038/nprot.2010.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira M, Bender D, Maller J, Sklar P, de Bakker P, Daly MJ, Sham PC. PLINK: A Tool Set for Whole-Genome and Population-Based Linkage Analyses. 2007. [DOI] [PMC free article] [PubMed]
- 30.Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira MA, Bender D, et al. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet. 2007;81(3):559–575. doi: 10.1086/519795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sudmant PH, Rausch T, Gardner EJ, Handsaker RE, Abyzov A, Huddleston J, Zhang Y, Ye K, Jun G, Hsi-Yang Fritz M, Konkel MK, Malhotra A, Stütz AM, Shi X, Paolo Casale F, Chen J, Hormozdiari F, Dayama G, Chen K, Malig M, Chaisson MJP, Walter K, Meiers S, Kashin S, Garrison E, Auton A, Lam HYK, Jasmine Mu X, Alkan C, Antaki D, Bae T, Cerveira E, Chines P, Chong Z, Clarke L, Dal E, Ding L, Emery S, Fan X, Gujral M, Kahveci F, Kidd JM, Kong Y, Lameijer EW, McCarthy S, Flicek P, Gibbs RA, Marth G, Mason CE, Menelaou A, Muzny DM, Nelson BJ, Noor A, Parrish NF, Pendleton M, Quitadamo A, Raeder B, Schadt EE, Romanovitch M, Schlattl A, Sebra R, Shabalin AA, Untergasser A, Walker JA, Wang M, Yu F, Zhang C, Zhang J, Zheng-Bradley X, Zhou W, Zichner T, Sebat J, Batzer MA, McCarroll SA, The 1000 Genomes Project Consortium. Mills RE, Gerstein MB, Bashir A, Stegle O, Devine SE, Lee C, Eichler EE, Korbel JO. An integrated map of structural variation in 2,504 human genomes. Nature. 2015;526(7571):75–81. doi: 10.1038/nature15394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Browning SR, Browning BL. Rapid and accurate haplotype phasing and missing-data inference for whole-genome association studies by use of localized haplotype clustering. Am J Hum Genet. 2007;81(5):1084–1097. doi: 10.1086/521987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Browning BL, Zhou Y, Browning SR. A one-penny imputed genome from next-generation reference panels. Am J Hum Genet. 2018;103(3):338–348. doi: 10.1016/j.ajhg.2018.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kanai M, Akiyama M, Takahashi A, Matoba N, Momozawa Y, Ikeda M, Iwata N, Ikegawa S, Hirata M, Matsuda K, Kubo M, Okada Y, Kamatani Y. Genetic analysis of quantitative traits in the Japanese population links cell types to complex human diseases. Nat Genet. 2018;50(3):390–400. doi: 10.1038/s41588-018-0047-6. [DOI] [PubMed] [Google Scholar]
- 35.Sakaue S, Kanai M, Karjalainen J, Akiyama M, Kurki M, Matoba N, et al. Trans-biobank analysis with 676,000 individuals elucidates the association of polygenic risk scores of complex traits with human lifespan. Nat Med. 2020;26(4):542–548. doi: 10.1038/s41591-020-0785-8. [DOI] [PubMed] [Google Scholar]
- 36.Zhang G, Bacelis J, Lengyel C, Teramo K, Hallman M, Helgeland Ø, Johansson S, Myhre R, Sengpiel V, Njølstad PR, Jacobsson B, Muglia L. Assessing the causal relationship of maternal height on birth size and gestational age at birth: a Mendelian randomization analysis. PLoS Med. 2015;12(8):e1001865. doi: 10.1371/journal.pmed.1001865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McLaren W, Gil L, Hunt SE, Riat HS, Ritchie GR, Thormann A, et al. The Ensembl variant effect predictor. Genome Biol. 2016;17(1):122. doi: 10.1186/s13059-016-0974-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Oscanoa J, Sivapalan L, Gadaleta E, Dayem Ullah AZ, Lemoine NR, Chelala C. SNPnexus: a web server for functional annotation of human genome sequence variation (2020 update) Nucleic Acids Res. 2020;48(W1):W185–WW92. doi: 10.1093/nar/gkaa420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Peat G, Jones W, Nuhn M, Marugán JC, Newell W, Dunham I, Zerbino D. The open targets post-GWAS analysis pipeline. Bioinformatics. 2020;36(9):2936–2937. doi: 10.1093/bioinformatics/btaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fishilevich S, Nudel R, Rappaport N, Hadar R, Plaschkes I, Iny Stein T, et al. GeneHancer: genome-wide integration of enhancers and target genes in GeneCards. Database (Oxford) 2017;2017:bax028. doi: 10.1093/database/bax028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Thurman RE, Rynes E, Humbert R, Vierstra J, Maurano MT, Haugen E, Sheffield NC, Stergachis AB, Wang H, Vernot B, Garg K, John S, Sandstrom R, Bates D, Boatman L, Canfield TK, Diegel M, Dunn D, Ebersol AK, Frum T, Giste E, Johnson AK, Johnson EM, Kutyavin T, Lajoie B, Lee BK, Lee K, London D, Lotakis D, Neph S, Neri F, Nguyen ED, Qu H, Reynolds AP, Roach V, Safi A, Sanchez ME, Sanyal A, Shafer A, Simon JM, Song L, Vong S, Weaver M, Yan Y, Zhang Z, Zhang Z, Lenhard B, Tewari M, Dorschner MO, Hansen RS, Navas PA, Stamatoyannopoulos G, Iyer VR, Lieb JD, Sunyaev SR, Akey JM, Sabo PJ, Kaul R, Furey TS, Dekker J, Crawford GE, Stamatoyannopoulos JA. The accessible chromatin landscape of the human genome. Nature. 2012;489(7414):75–82. doi: 10.1038/nature11232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Peña EA, Slate EH. Global validation of linear model assumptions. J Am Stat Assoc. 2006;101(473):341–354. doi: 10.1198/016214505000000637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tingley D, Yamamoto T, Hirose K, Keele L, Imai K. Mediation: R package for causal mediation analysis . Journal of Statistical Software, 2014.
- 44.Imai K, Keele L, Tingley D. A general approach to causal mediation analysis. Psychol Methods. 2010;15(4):309–334. doi: 10.1037/a0020761. [DOI] [PubMed] [Google Scholar]
- 45.Cohen J. Statistical power analysis for the behavioral science. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 46.Gordijn SJ, Beune IM, Thilaganathan B, Papageorghiou A, Baschat AA, Baker PN, Silver RM, Wynia K, Ganzevoort W. Consensus definition of fetal growth restriction: a Delphi procedure. Ultrasound Obstet Gynecol. 2016;48(3):333–339. doi: 10.1002/uog.15884. [DOI] [PubMed] [Google Scholar]
- 47.Workalemahu T, Rahman ML, Ouidir M, Wu J, Zhang C, Tekola-Ayele F. Associations of maternal blood pressure-raising polygenic risk scores with fetal weight. J Hum Hypertens. 2021. 10.1038/s41371-021-00483-x. [DOI] [PMC free article] [PubMed]
- 48.Martin AR, Kanai M, Kamatani Y, Okada Y, Neale BM, Daly MJ. Clinical use of current polygenic risk scores may exacerbate health disparities. Nat Genet. 2019;51(4):584–591. doi: 10.1038/s41588-019-0379-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Characteristics of participants included in this study. Table S2. Genome-wide significant loci for blood pressure phenotypes and classification based on vasculature relevance. Table S3. Variants constituting SBP-increasing PGS at p value threshold of 1 x 10−6 and classification based on vasculature relevance. Table S4. Linear regression analyses for maternal SBP-increasing PGS predicting various traits including birth weight. Table S5. Linear regression analyses for maternal DBP-increasing PGS predicting various traits including birth weight. Table S6. Linear regression analyses for maternal MAP-increasing PGS predicting various traits including birth weight. Table S7. Linear regression analyses for maternal PP-increasing PGS predicting various traits including birth weight. Table S8. Linear regression analyses for maternal BP traits predicting placental weight. Table S9. Sensitivity analysis for estimates of the causal mediation analyses by excluding pleotropic SNPs from exposure PGS.Table S10. Linear regression analyses for BP-increasing allele predicting birth weight or placental weight.
Additional file 2: Figure S1. Relationship between maternal BP in early gestation and offspring birth weight. Figure S2. Relationship between maternal BP in mid gestation and offspring birth weight. Figure S3. Relationship between maternal BP in late gestation and offspring birth weight. Figure S4. Estimates of mediation analyses with different PGS (exposure variable).
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.