Abstract
Background
Despite efforts to increase the overall diversity of the medical student body, some medical specialties have a less diverse applicant pool based on both gender and race than would be expected based on medical graduate demographics.
Objectives
To identify whether women and Underrepresented in Medicine (URiM) medical students have baseline differences in their career interests or if their career plans change more during medical school when compared to men and non-URIM students.
Methods
Secondary data analyses of all medical students who applied through ERAS from 2005–2010 was conducted. Binary logistic regression models with the response being a planned career in one of four medical specialties (internal medicine, pediatrics, OB/GYN, and general surgery/surgical specialties) at medical school entry and graduation. Regression models included demographics, student attitudes, debt, academic metrics, and medical school experiences.
Results
Comparatively, women were less likely to be interested in internal medicine and surgery and more interested in pediatrics and OB/GYN at matriculation. URiM students expressed more interest in OB/GYN and surgery when starting medical school. At graduation, women were less likely to plan for internal medicine and surgery and were more interested in pursuing OB/GYN and pediatrics. URiM students were more likely to plan for a career in internal medicine and less likely to choose pediatrics.
Conclusions
From matriculation to graduation, women have relatively stable preferences regarding planned medical specialties. In contrast, URiM students’ specialty plans shifted over time among the four specialties, with variation in preferences occurring between matriculation and graduation.
Introduction
Despite efforts to increase the overall diversity of the medical student body [1–17], some career options [18], such as general surgery [19–23] and the surgical specialties [19, 20, 24–26], obstetrics and gynecology (OB/GYN) [19, 27, 28], pediatrics and its subspecialties [29–31], and emergency medicine (EM) [32–37], have a less diverse applicant pool than would be expected based on medical graduate demographics (by gender, race, or both). These differences have remained largely stable even as women now make up more than 50% of entering medical school classes [38].
Representation matters to patients, not just educators. Physicians treating patients of the same gender [39] or similar racial and ethnic backgrounds may achieve better health outcomes than if these matches are dissimilar [11, 12, 15, 40]. A larger body of evidence reports increased satisfaction from patients with providers from similar backgrounds [41–47] and improved communication with shared-decision making [45, 47–53]. Patient outcome disparities associated with specific racial and ethnic groups in the United States has become more widely reported to the general public during the ongoing COVID pandemic. To ensure equitable care for all patients, now is the time for reevaluating interventions designed to increase physician workforce diversity in all medical specialties.
Many students begin medical school with clear preferences about the specialty area in which they plan to practice [54, 55]. However, as students progress through medical school to graduation the stability of these preferences is less clear [54, 55]. Lifestyle interests, expected income, procedural orientation, societal prestige outside medicine, and the respect of peer physicians within the profession have been correlated with medical specialty selection [56, 57]. Additionally, studies designed to understand how a lack of diversity in the applicant pool persists in EM demonstrated that even when controlling for academic competitiveness, debt, career attitudes and aspirations, women and URiM students had significantly lower interest in that field than their peers [33]. Women were also less likely than men to develop a career interest in EM during medical school and URiM students were less interested in EM at the beginning of medical school and were less likely to maintain or develop an interest in EM compared to their peers [37, 58]. Whereas many academic experiences and opinions may be set prior to medical school, one’s eventual career choice is largely a function of one’s entering career interest and experiences during medical training.
Objectives
To compare specialty choice associated with gender and race by evaluating two potential mechanisms of underrepresentation: under-recruitment of interest (not convincing people previously uninterested to choose a specific specialty) and failure of interest retention (where individuals change their specialty). The latter could be described as either a passive lack of support for career adoption or a more active, intentional “cooling out” of interest (as described in higher education). “Cooling out” is the “redirection” of a learner’s career aspirations by faculty and advisors [59, 60]. The alternative to “cooling out” is a positive recruitment of students to a new career aspiration, in this case a medical specialty. Our study incorporates these ideas into the definition of recruitment and retention, with the understanding that they are likely providing some contribution to the observed effects. We believe this is an important step toward future policy interventions.
Career selection theoretical framework
Concepts from two major applicable theoretical systems, Bounded Rationality Theory (BRT) [61–63] and Bandura’s Theory of Self Efficacy (SE) [64–66], framed this research. Based on BRT, we expect that cognitive limitations and incomplete information availability will drive students to make decisions based on knowable qualities, such as income and specialty competitiveness, instead of acting to maximize their own personal values [61, 62]. SE focuses on one’s belief in his/her ability to influence their cognitive response to adversity and thus persevere toward their goals [64]. Self-efficacy is often enhanced through positive academic experiences and mentorship [64]. Therefore, in addition to individual attitudes previously utilized in career selection studies, an individual’s academic metrics representing likely match competitiveness and a history of positive academic experiences, as well as their level of educational debt are included in the model.
Hypotheses
One: At the onset of medical school, compared to men, women are more interested in fields with more female physician role models [67, 68], (pediatrics and OB/GYN) have less interest in fields where women are underrepresented (surgery), and similar interest to men in fields with more gender parity (internal medicine: IM). Two: URiM students will have similar entering interests compared to their non-URiM peers across the four specialty areas examined. Three: Relative to men, women will exhibit evidence of both under-recruitment and lack of interest retention in medical specialties traditionally dominated by males. Four: URiM medical specialty interest will remain relatively stable from entry of medical school to graduation, but will be consistently lower for specialties that have fewer URiM physicians.
Methods
Participants
The study uses secondary data of 46,776 students who applied for residency using the Electronic Residency Application Service (ERAS) from 2005 through 2010. Nationally representative datasets from the Association of American Medical Colleges (AAMC), including: Matriculating Student Questionnaire (MSQ), Graduation Questionnaire (GQ) administered after the match, AAMC Applicant Matriculant File (AAMF) were matched to the ERAS to create a longitudinal database. The National Board of Medical Examiners (NBME) U.S. Medical Licensing Exam (USMLE) Step 1 and Step 2 CK score data were also included.
Variables and outcomes measured
Predictor variables were selected based on the conceptual framework and the existing literature (Table 1). Students records were only included in the final analysis if they had complete records for all variables included in the final analytical model. No data were imputed. Given the high level of missing data on some of the attitudinal factors recorded on the GQ, a more basic model which only include demographics and USMLE Step Scores was also fitted to provide results with the highest possible number of subjects in addition the model created based on the a priori factors in Table 1. The basic model included total 22,555 subjects. Both models’ results are illustrated in Fig 1 for comparison. The URiM variable represents a binary recoding of a self-reported racial/ethnic identity to be either non-URiM (white or Asian students) or URiM student [69]. Entering career specialty interest was derived from the response to the MSQ item: “What general specialty are you considering?” Graduating career specialty interest was derived from the response to the GQ item: “When thinking about your career, what is your intended area of practice?” Responses were recoded as either “interested in the specialty of study” with all other specialty choices collapsed into “not interested.”
Table 1. Variables.
| Variable Subgroup Names | Variables within Each Subgroup | Measurement Type | Source(s) |
|---|---|---|---|
| Demographics | Gender | Binary | Electronic Residency Application Service (ERAS) |
| Age | Continuous | ||
| URiM Status | Binary | ||
| Entering Attitudes | Opportunity for Authority | Likert-Like Scale | Matriculating Student Questionnaire (MSQ) |
| Opportunity for Patient Contact | |||
| Opportunity for Control | |||
| Opportunity for Decision-Making | |||
| Opportunity for Expertise in Specialized Area | |||
| Opportunity to Make a Difference | |||
| Opportunity for Research | |||
| Chose Medicine to Limit Stress | |||
| Graduation Attitudes | Work-Life Balance | Likert-Like Scale | Graduation Questionnaire (GQ) |
| Specialty Competitiveness | |||
| Specialty Personality | |||
| Specialty Content | |||
| Expected Salary | |||
| Advice from Mentor | |||
| Family Expectations | |||
| Debt Level | |||
| Debt Level | Had Pre-Medical Debt | Continuous | Graduation Questionnaire (GQ) |
| Received Scholarship | |||
| Medical School Debt in $10,000 | |||
| Non-Educational Debt in $10,000 | |||
| Entering GPA | Overall GPA | Continuous | AAMC Applicant Matriculant File (AAMF) |
| Science GPA | |||
| Standardized Tests | MCAT Total | Continuous | AAMC Applicant Matriculant File (AAMF) |
| Step 1 Score | |||
| Step 2 CK Score | U.S. Medical Licensing Exam (USMLE) | ||
| Medical School Activity | Number of Publications | Continuous | Electronic Residency Application Service (ERAS) |
| Research Experience | Continuous | ||
| Awarded AOA prior to application | Binary | ||
| Confidence in Specialty Choice | Likert-Like Scale | ||
| Planned Practice with Underserved Populations | |||
| Binary | |||
| Dependent Variables | Entering Career Interest in IM | Binary | Matriculating Student Questionnaire (MSQ) |
| Planned Career in IM | |||
| Entering Career Interest in Peds | |||
| Planned Career in Peds | |||
| Entering Career Interest in OB/GYN | Graduation Questionnaire (GQ) | ||
| Planned Career in OB/GYN | |||
| Entering Career Interest in Surgery | |||
| Planned Career in Surgery |
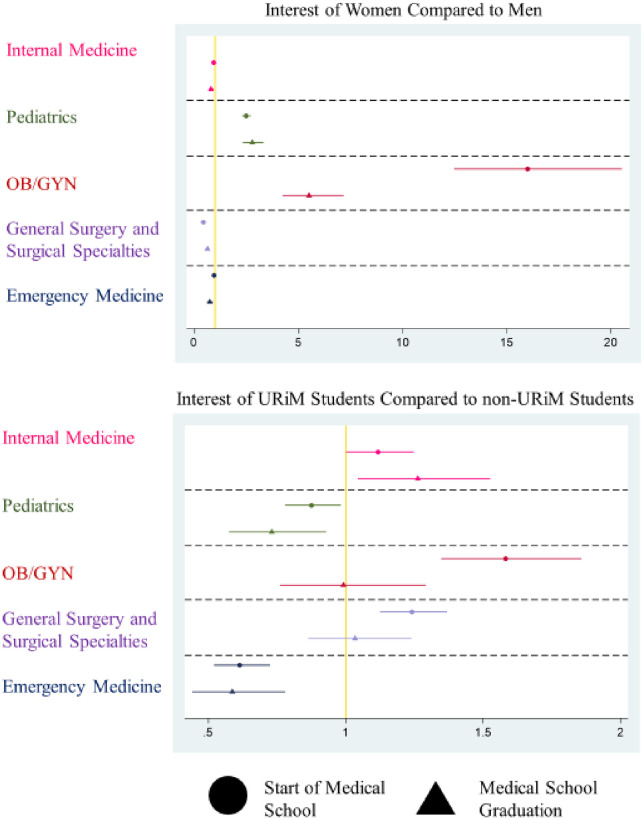
Fig 1. Career interest at onset and graduation.
Plot of Odds Ratios from Two Outcomes (Specialty Interest at the Onset of Medical School and Specialty Interest at the time of Graduation) on a logarithmic scale. X-Axis represents the Odds Ratio of the Outcome in each model for each group. Gold line represents Odds of 1 (no effect). Y-Axis represents the medical specialties investigated. Each point represents the calculated Odds Ratio with the 95% Confidence Interval for each value represented by bars to either side.
Analysis of the outcomes
Eight binary dependent variables were initially examined. Four dependent variables were measures of a plan to enter (or not) a specific career at the beginning of medical school (IM and its specialties, pediatrics and its specialties, OB/GYN, and general surgery and other surgical specialties). These specialties were chosen based on the number of residents in training and because they represented a variety of career options with different patterns of gender and racial representation, including both over and under-representation among the demographic factors included in the study.
The other four dependent variables measured whether the student planned to enter (or not) a specific career (same four specialties) at the time of graduation. Twelve additional models were also fitted by specialty for each of three additional dependent variables: 1) the student planned to enter a specific career (or not) at the time of graduation with the addition of entering interests as a control, 2) a model examining only students who had an entering plan to practice in the same field, and 3) a regression examining only students who did not have an entering plan to practice in the same field. Given the dichotomous nature of all the outcome variables, binary logistic regression was used to fit these models [70] and marginal effects were calculated to provide practical effect size that are easy to interpret. Previously published EM models were included in the figures for further comparison [58].
Institutional Review Board approval was solicited and the study was judged not to require additional regulation or assessment.
Results
At matriculation, female students were less likely than male students to plan to practice in IM (OR 0.94 95% CI 0.88–0.96) or choose a surgical career (OR 0.42 95% CI 0.40–0.44) (Table 2), but had higher odds of choosing a career in pediatrics than their male peers (OR 2.40 95% CI 2.26–2.54) and OB/GYN (OR 15.19 95% CI 12.73–18.11). At graduation women were also less likely than men to plan for a career in IM (OR 0.81 95% CI 0.70–0.93) or a surgical field (OR 0.64 95% CI 0.56–0.73) and more likely to plan to practice in pediatrics (OR 2.79 95% CI 2.33–3.32) and OB/GYN (OR 5.52 95% CI 4.25–7.18) (Table 3). These results translate to women being 3% less probable to choose IM and 7% less probable to choose a surgical career than men. Conversely, women were 9% more probable to choose pediatrics and 10% more probable to choose OB/GYN than men. Comparisons between medical specialties are displayed in Fig 1 with the two GQ outcome models having qualitatively similar patterns.
Table 2. Career interest when entering medical school.
| Internal Medicine (IM) | Pediatrics | OB/GYN | Gen. Surgery and Surgical Specialties | |||||
|---|---|---|---|---|---|---|---|---|
| Odds Ratio | 95% Confidence Interval | Odds Ratio | 95% Confidence Interval | Odds Ratio | 95% Confidence Interval | Odds Ratio | 95% Confidence Interval | |
| Female | 0.94* | 0.883–0.996 | 2.40*** | 2.263–2.549 | 15.19*** | 12.73–18.11 | 0.42*** | 0.400–0.444 |
| (0.029) | (0.073) | (1.366) | (0.011) | |||||
| Age | 1.06*** | 1.049–1.065 | 0.92*** | 0.907–0.927 | 0.99 | 0.974–1.004 | 0.96*** | 0.952–0.969 |
| (0.004) | (0.005) | (0.007) | (0.004) | |||||
| URiM | 1.07 | 0.989–1.157 | 0.92* | 0.847–0.993 | 1.60*** | 1.426–1.794 | 1.25*** | 1.166–1.339 |
| (0.043) | (0.037) | (0.094) | (0.044) | |||||
| GPA | 1.00 | 0.999–1.001 | 1.00* | 0.998–1.000 | 1.00*** | 0.996–0.999 | 1.00*** | 0.997–0.999 |
| (0.001) | (0.001) | (0.001) | (0.000) | |||||
| MCAT | 1.03*** | 1.022–1.037 | 1.01* | 1.000–1.015 | 1.00 | 0.985–1.010 | 1.02*** | 1.011–1.024 |
| (0.004) | (0.004) | (0.006) | (0.003) | |||||
| Work with Underserved | 1.11*** | 1.059–1.155 | 1.04 | 0.999–1.084 | 1.09* | 1.018–1.168 | 0.62*** | 0.601–0.645 |
| (0.024) | (0.022) | (0.038) | (0.011) | |||||
| Opportunity for Authority | 1.07*** | 1.045–1.100 | 0.92*** | 0.900–0.946 | 1.06** | 1.019–1.109 | 1.02 | 0.997–1.041 |
| (0.014) | (0.012) | (0.023) | (0.011) | |||||
| Opportunity for Patient Contact | 1.19*** | 1.147–1.230 | 1.68*** | 1.610–1.749 | 1.29*** | 1.210–1.378 | 0.89*** | 0.866–0.914 |
| (0.021) | (0.035) | (0.043) | (0.012) | |||||
| Opportunity for Control | 0.95*** | 0.916–0.977 | 0.97* | 0.937–0.999 | 0.92** | 0.871–0.973 | 1.05*** | 1.020–1.077 |
| (0.016) | (0.016) | (0.026) | (0.015) | |||||
| Opportunity for Decision-Making | 0.84*** | 0.816–0.858 | 0.87*** | 0.848–0.889 | 0.98 | 0.943–1.021 | 1.03* | 1.003–1.049 |
| (0.011) | (0.011) | (0.020) | (0.012) | |||||
| Opp. for Expert. in Spec. Area | 0.97* | 0.937–0.995 | 0.89*** | 0.861–0.911 | 1.12*** | 1.065–1.172 | 1.32*** | 1.287–1.362 |
| (0.015) | (0.013) | (0.027) | (0.019) | |||||
| Opportunity to Make a Difference | 0.94 | 0.882–1.009 | 1.25*** | 1.139–1.379 | 1.04 | 0.886–1.218 | 0.93* | 0.880–0.988 |
| (0.032) | (0.061) | (0.085) | (0.027) | |||||
| Opportunity for Research | 1.27*** | 1.239–1.299 | 0.96*** | 0.936–0.981 | 0.87*** | 0.836–0.902 | 1.08*** | 1.061–1.104 |
| (0.015) | (0.011) | (0.017) | (0.011) | |||||
| Chose Medicine to Limit Stress | 0.96* | 0.932–0.995 | 1.05** | 1.014–1.079 | 0.99 | 0.943–1.047 | 0.91*** | 0.883–0.931 |
| (0.016) | (0.017) | (0.026) | (0.012) | |||||
| Constant | 0.01*** | 0.00643–0.0209 | 0.27*** | 0.133–0.555 | 0.01*** | 0.00292–0.0256 | 1.80* | 1.041–3.122 |
| (0.003) | (0.099) | (0.005) | (0.505) | |||||
| Observations | 41,047 | 41,047 | 41,047 | 41,047 | 41,047 | 41,047 | 41,047 | 41,047 |
Robust standard errors in parentheses.
*** p<0.001,
** p<0.01,
* p<0.05.
Table 3. Career interest when graduating medical school.
| Internal Medicine (IM) | Pediatrics | OB/GYN | Gen. Surgery and Surgical Specialties | |||||
|---|---|---|---|---|---|---|---|---|
| Odds Ratio | 95% Confidence Interval | Odds Ratio | 95% Confidence Interval | Odds Ratio | 95% Confidence Interval | Odds Ratio | 95% Confidence Interval | |
| Female | 0.81** | 0.697–0.934 | 2.79*** | 2.331–3.329 | 5.52*** | 4.245–7.167 | 0.64*** | 0.561–0.727 |
| (0.060) | (0.253) | (0.737) | (0.042) | |||||
| Age | 0.99 | 0.967–1.018 | 0.91*** | 0.875–0.939 | 0.97 | 0.929–1.008 | 1.00 | 0.975–1.023 |
| (0.013) | (0.016) | (0.020) | (0.012) | |||||
| URiM | 1.26* | 1.044–1.526 | 0.73* | 0.575–0.928 | 0.99 | 0.761–1.292 | 1.03 | 0.863–1.239 |
| (0.122) | (0.089) | (0.134) | (0.095) | |||||
| GPA | 1.00 | 0.997–1.003 | 1.00 | 0.999–1.006 | 1.00 | 0.996–1.004 | 1.00 | 0.997–1.002 |
| (0.001) | (0.002) | (0.002) | (0.001) | |||||
| MCAT | 1.01 | 0.987–1.027 | 1.04** | 1.013–1.061 | 0.97* | 0.943–0.997 | 1.00 | 0.986–1.022 |
| (0.010) | (0.012) | (0.014) | (0.009) | |||||
| USMLE Step 1 | 0.99** | 0.986–0.997 | 0.98*** | 0.973–0.985 | 0.99** | 0.981–0.996 | 1.02*** | 1.017–1.028 |
| (0.003) | (0.003) | (0.004) | (0.003) | |||||
| USMLE Step 2 | 1.01*** | 1.004–1.013 | 1.00 | 0.999–1.010 | 1.00 | 0.995–1.008 | 0.99*** | 0.984–0.993 |
| (0.002) | (0.003) | (0.003) | (0.002) | |||||
| Work with Underserved | 1.01 | 0.919–1.113 | 1.08 | 0.972–1.210 | 1.13 | 0.985–1.298 | 0.86*** | 0.790–0.937 |
| (0.049) | (0.061) | (0.080) | (0.037) | |||||
| Work/Life Balance | 0.89** | 0.835–0.956 | 1.13** | 1.047–1.230 | 0.45*** | 0.411–0.493 | 0.87*** | 0.816–0.927 |
| (0.031) | (0.046) | (0.021) | (0.028) | |||||
| Specialty Personality | 0.77*** | 0.679–0.882 | 0.94 | 0.793–1.118 | 1.20* | 1.008–1.441 | 1.12 | 0.976–1.276 |
| (0.052) | (0.083) | (0.110) | (0.076) | |||||
| Specialty Competitiveness | 0.93 | 0.863–1.006 | 0.59*** | 0.529–0.650 | 1.05 | 0.940–1.166 | 1.17*** | 1.098–1.252 |
| (0.036) | (0.031) | (0.057) | (0.039) | |||||
| Mentor Advice | 1.26*** | 1.174–1.354 | 1.06 | 0.980–1.146 | 1.04 | 0.946–1.132 | 1.01 | 0.946–1.070 |
| (0.046) | (0.042) | (0.047) | (0.032) | |||||
| Medical School Debt | 0.99 | 0.983–1.000 | 0.99 | 0.981–1.001 | 1.02*** | 1.009–1.035 | 1.00 | 0.992–1.007 |
| (0.004) | (0.005) | (0.007) | (0.004) | |||||
| Publications | 0.99 | 0.978–1.007 | 1.00 | 0.980–1.026 | 0.98 | 0.951–1.002 | 1.02*** | 1.009–1.033 |
| (0.007) | (0.012) | (0.013) | (0.006) | |||||
| Research Experiences | 1.05* | 1.008–1.095 | 0.91*** | 0.857–0.956 | 0.99 | 0.931–1.058 | 1.11*** | 1.074–1.153 |
| (0.022) | (0.025) | (0.032) | (0.020) | |||||
| Elected to AOA | 1.00 | 0.814–1.238 | 1.02 | 0.796–1.318 | 1.14 | 0.836–1.566 | 1.11 | 0.928–1.321 |
| (0.107) | (0.132) | (0.183) | (0.100) | |||||
| Confidence in Specialty Choice | 0.60*** | 0.542–0.666 | 0.97 | 0.842–1.127 | 0.95 | 0.805–1.123 | 1.37*** | 1.214–1.554 |
| (0.032) | (0.072) | (0.081) | (0.087) | |||||
| Constant | 0.87 | 0.152–5.005 | 8.32* | 1.012–68.47 | 2.68 | 0.224–32.02 | 0.01*** | 0.00218–0.0522 |
| (0.777) | (8.949) | (3.390) | (0.009) | |||||
| Observations | 6,906 | 6,906 | 6,906 | 6,906 | 6,906 | 6,906 | 6,906 | 6,906 |
Robust standard errors in parentheses.
*** p<0.001,
** p<0.01,
* p<0.05.
At matriculation, URiM students were more likely to plan for a career in OB/GYN (OR 1.60 95% CI 1.43–1.79) or a surgical field (OR 1.34 95% CI 1.25–1.43) than their non-URiM peers (Table 2). Compared to their non-URiM peers, URiM students were less likely to plan for a career in pediatrics (OR 0.92 95% CI 0.85–0.99) but had no significant difference in their reported interest in IM at matriculation. At the time of graduation, URiM students were less likely to plan to enter pediatrics (OR 0.73 95% CI 0.58–0.93) and more likely to report a planned career in IM (OR 1.26 95% CI 1.04–1.53) compared to non-URiM students (Table 3). No differences in the odds of a planned career in OB/GYN or a surgical field were found between URiM students and non-URiM students at graduation. These results translate to URiM students being 3% more probable to choose IM and 3% less probable to choose pediatrics compared to non-URiM students.
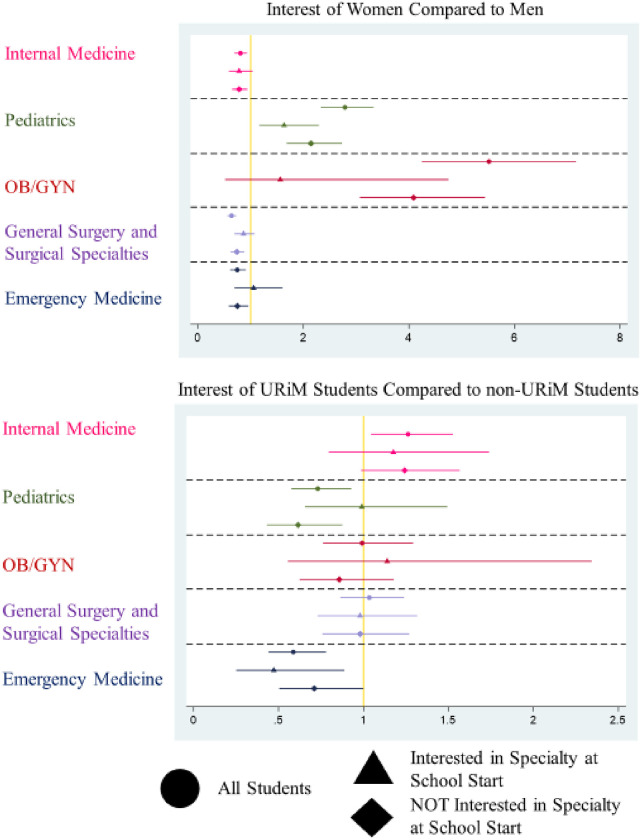
Compared to men, women had significantly lower odds of planning for a career in IM or surgery when controlling for their career plans at the start of medical school (Fig 2). In contrast, women were more likely to plan for a career in pediatrics at the time of graduation, even after controlling for their plans at matriculation. Compared to their male peers, women who reported a plan to enter pediatrics at the start of medical school had higher odds to still plan to enter pediatrics at graduation. Female students had higher odds of a planned career in OB/GYN at graduation, even when initial career interest was controlled for in the model. However, women and men exhibited no significant differences in interest in OB/GYN at the time of graduation when controlling for initial interest.
Fig 2. Graduating interest comparison.
Plot of Odds Ratios from Three Approaches (All Students regardless of entering interest, Only Students Initially Interested in the specialty at the beginning of Medical School, and Only Students NOT Initially Interested in the specialty at the beginning of Medical School) on a logarithmic scale. X-Axis represents the Odds Ratio of the Outcome in each model for each group. Gold line represents Odds of 1 (no effect). Y-Axis represents the medical specialties investigated. Each point represents the calculated Odds Ratio with the 95% Confidence Interval for each value represented by bars to either side.
Compared to their peers, URiM students had significantly higher odds of reporting a planned career in IM at the time of graduation, even after controlling for their entering interest in that field (Fig 2). Conversely, even after controlling for their initial specialty selection, URiM students had significantly lower odds of a final career plan in pediatrics upon graduation. When entering career plans were included in the model, no significant difference between URiM and non-URiM students was evident in the other medical specialties (Fig 2).
Several other academic variables (e.g., grades and test scores) and career attitudinal factors were also statistically significantly related to the outcome variables. Their inclusion in the analysis was based on their theoretical importance in decision-making regarding match competitiveness for individuals and a desire to control for these factors on decision making that may confound the direct effects of gender and URiM status on the outcomes of interest. The relative importance of each of these factors on career planning is outside the focus of this analysis, but those interested can find the results in Tables 2 and 3.
Discussion
The results demonstrate distinctive patterns in medical specialty career plans associated with gender and racial background both in terms of initial career plans at matriculation and the choices made at graduation. Regarding the study hypotheses, while some were supported, the overall patterns were more complex than initially hypothesized. In general, we found that the patterns favoring the proposed under-recruitment mechanism were more often present than those supporting a lack of interest retainment (“cooling out”).
Considering each hypothesis in turn, we found the following. First, specialties with a traditionally higher proportion of female physicians also had higher odds of women initially planning for a career in that field (pediatrics and OB/GYN). Second, two of the four medical specialty groups had statistically different odds of planning to enter a specific specialty for URiM and non-URiM students. Specifically, URiM students had higher odds of reporting a plan to practice in OB/GYN and in a surgical field. This appears to be a new finding as most prior studies did not specifically test correlations with race [71–74]. This may be because prior studies of career plans at matriculation were often smaller in scope [75, 76], older [74, 76–79], and did not include measures of academic competitiveness [71, 79, 80]. Third, changing one’s career path choice appears to be a less common than under-recruitment in terms of explaining preference patterns by gender. Comparatively, women are not being cooled off from a career in fields with relatively fewer female physicians. Instead, it appears a smaller proportionate number of women are becoming interested in those specialties during the course of their medical school careers. Regarding the final hypothesis, URiM student specialty plans were not stable during medical school. Fig 1 indicates where differences in specialty plans between URiM and non-URiM students appear to change between matriculation to medical school and graduation. However, when entering career plans were accounted for, the differences between URiM and non-URiM students’ specialty plans were no longer statistically significant in OB/GYN and surgery (Fig 2). Where changes in planned careers do exist, URiM students have higher odds of choosing IM and lower odds of choosing pediatrics than their peers. In the case of the later, the foremost mechanism we observed was less successful recruitment and not loss of interest by URiM students when compared to their counterparts.
Several limitations of this study must be considered. First, the study uses secondary data and therefore relies on the use of preexisting items which limits the scope of the factors that can be considered. Some variables used are imperfect proxies for underlying constructs, and some factors which could not be considered as they did not exist in the original data. Additionally, privacy policies in place with the primary data holders prohibited the use of some measures, such as the specific medical school attended. Second, the data used is from a period approximately ten years ago and thus the findings may be dated. While this concern cannot be discounted, it is worth noting that applications to each medical specialty have remained largely stable over time as have the relative disparities in representation within each specialty [32, 81]. Where things have changed in the past 5 years, such as decreasing numbers of women applying into EM, this has not resulted in increased representation of women or URiM students. Finally, we were limited to using the eventual specialty of training and not the one in which an applicant may have initially attempted to match. This was as a result of the unwillingness of the National Residency Match Program to share individual level data about applicant match choices, despite requests to gain such access.
In general, this study provides new findings and raises new questions about the underlying mechanisms that result in persistent underrepresentation in some medical specialties. Our results demonstrate that medical specialty choice changes over time and that there are correlations between gender, race, and eventual career aspirations that is missing from the prior empirical work. Differences between specialties, while controlling for academic metrics, suggest that there are structural and cultural effects not currently observed with the data and variables available, and these mechanisms are not currently described in the literature. Our theoretical framework and empirical work provides a road map to better understanding the mechamisms underlying medical choice decisions, yet there remains work to be done.
First, while we attempted to control for some aspects of self-efficacy by including prior academic success, we were unable to account for how prior academic events were interpreted and incorporated into each students self identity. As has been found in work related to persistence through a pre-medical curriculum, men and women may interpret the same grade or test score differently regarding their own underlying abilities [82]. The effect of women perceiving themselves more negatively then men has been shown to be especially true in traditionally male-dominated fields and tasks [83, 84]. Similar mechanisms have been suggested regarding career choice and stereotype threat, sense of belonging, micro-aggressions, and cultural incongruence for both URiM students and women [85–87]. Inaccurate perceptions by students regarding their own ability to succeed in a specific specialty as a result of unwelcoming/non-supportive environments and long term socialization may account for some of the uncontrolled differences observed in our results. Mentorship from physician role models and more transparent peer-to-peer normalization of results may help to ameliorate this effect.
A second potential mechanism derives from our understanding of bounded rationality theory. We used data from only two points in time, the beginning and the end of medical school. BRT suggests decisions such as specialty choice occur over time and are subject to both information limitations and urgency biases. For example, the timing of when students learned about certain specialties and when they were exposed (or not) to physicians from backgrounds similar to theirs is not captured using our design. Studying medical specialty choice in a more granular, and perhaps even prospective manner, that includes sufficient data points for longitudinal modeling could provide a great deal of clarity regarding the decision making process itself in order to inform policy changes in medical education.
Our study suggests that there is no “single solution” to increase the diversity of the physician workforce for all specialties regarding issues of gender or racial underrepresentation. If policy interventions are going to be successful, further study is necessary to describe the mechanisms at work for each individual specialty. We suggest two observed phenomena, loss of interest in a specialty and lower interest generation in a specialty, but understanding the mechanisms operating could be explored either through a qualitative study of students who change their career plans or a quantitative study that uses more detailed temporal data and methods specifically designed to study outcomes that change over time (e.g., fixed effects and/or survival modeling). Our analysis was focused on the four largest specialties in order to establish whether major differences existed between each or if a single pattern could be identified. Future research could focus on those specialties that are considered most competitive or those with the greatest issues regarding representation by using the methods described in this paper.
Conclusions
When compared with their peers, women and URiM students have differences in their planned specialty of practice that can be identified at the start of medical school for some fields. Worsening underrepresentation in some medical specialties is more likely the result of under-recruitment than loss of initial interest. Further study is necessary to establish the complex mechanisms at work that may be driving changes in career interests over time.
Acknowledgments
This material is based upon data provided by the Association of American Medical Colleges (AAMC) and the National Board of Medical Examiners (NBME). The views expressed herein are those of the authors and do not necessarily reflect the positions of the AAMC and the NBME.
Data Availability
Data cannot be shared publicly by the author as it is used under a data usage agreement with the Association of American Medical Colleges (AAMC) and the National Board of Medical Examiners (NBME). Data can be obtained from those organizations through research requests as was done in this case. Data are held by a third party. The authors did not have any special access privileges to the data, and obtained the data in the same way as detailed in their data access guidelines published online. https://www.aamc.org/request-aamc-data https://www.nbme.org/services/data-sharing.
Funding Statement
JB Grant No. EF2016-001 Society for Academic Emergency Medicine Foundation https://www.saem.org/saem-foundation The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Association of American Medical Colleges. Data and Analysis Washington, DC: Association of American Medical Colleges; 2017. [https://www.aamc.org/data. [Google Scholar]
- 2.Razack S, Hodges B, Steinert Y, Maguire M. Seeking inclusion in an exclusive process: discourses of medical school student selection. Med Educ. 2015;49(1):36–47. doi: 10.1111/medu.12547 [DOI] [PubMed] [Google Scholar]
- 3.Puddey IB, Mercer A, Playford DE, Riley GJ. Medical student selection criteria and socio-demographic factors as predictors of ultimately working rurally after graduation. BMC Med Educ. 2015;15:74. doi: 10.1186/s12909-015-0359-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jeffe DB, Andriole DA, Wathington HD, Tai RH. The emerging physician-scientist workforce: demographic, experiential, and attitudinal predictors of MD-PhD program enrollment. Academic medicine: journal of the Association of American Medical Colleges. 2014;89(10):1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reiter HI, Lockyer J, Ziola B, Courneya C-A, Eva K, Alliance CMM-IR. Should efforts in favor of medical student diversity be focused during admissions or farther upstream? Academic Medicine. 2012;87(4):443–8. doi: 10.1097/ACM.0b013e318248f7f3 [DOI] [PubMed] [Google Scholar]
- 6.Nivet MA. Diversity 3.0: A Necessary Systems Upgrade. Academic Medicine. 2011;86(12):1487–9. doi: 10.1097/ACM.0b013e3182351f79 [DOI] [PubMed] [Google Scholar]
- 7.Cantwell B, Canche M, Milem J, Sutton F, editors. Do the data support the discourse? Assessing holistic review as an admissions process to promote diversity at a US medical school. annual meeting of the Association for the Study of Higher Education, Indianapolis; 2010. [Google Scholar]
- 8.Barr DA. Questioning the premedical paradigm: Enhancing diversity in the medical profession a century after the Flexner report: JHU Press; 2010.
- 9.U.S. Department of Health and Human Services. Pipeline Programs to Improve Racial and Ethnic Diverity in the Health Professions: An Inventory of Federal Programs, Assessment of Evaluation Approaches, and Critical Review of the Research Literature. U.S. Department of Health and Human Services Health Resources and Services Administration; 2009. [Google Scholar]
- 10.Saha S, Guiton G, Wimmers PF, Wilkerson L. Student Body Racial and Ethnic Composition and Diversity-Related Outcomes in US Medical Schools. Journal of the American Medical Association. 2008;300(10):1135–45. [DOI] [PubMed] [Google Scholar]
- 11.US Department of Health and Human Services. The Rationale for Diversity in the Health Professions: A Review of the Evidence. US Department of Health and Human Services; 2006. [Google Scholar]
- 12.Baldwin A, Woods K, Simmons MC. Diversity of the allied health workforce: the unmet challenge. J Allied Health. 2006;35(2):116–20. [PubMed] [Google Scholar]
- 13.Sullivan L. Missing Persons: Minorities in Health Professions, A Report of the Sullivan Commission on Diversity in the Healthcare Workforce. W. K. Kellogg Foundation; 2004. [Google Scholar]
- 14.Cohen JJ. The consequences of premature abandonment of affirmative action in medical school admissions. JAMA. 2003;289(9):1143–9. doi: 10.1001/jama.289.9.1143 [DOI] [PubMed] [Google Scholar]
- 15.DeVille K, Kopelman L. Diversity, Trust, and Patient Care: Affirmative Action in Medical Education 25 years After Bakke. Journal of Medicine and Philosophy. 2003;28(4):489–516. [DOI] [PubMed] [Google Scholar]
- 16.Lakhan S. Diversification of U.S. medical schools via affirmative action. BMC Medical Education. 2003;3(6):1–6. doi: 10.1186/1472-6920-3-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Whitla DK, Orfield G, Silen W, Teperow C, Howard C, Reede J. Educational Benefits of Diversity in Medical School: A Survey of Students. Academic Medicine. 2003;78(5):460–6. doi: 10.1097/00001888-200305000-00007 [DOI] [PubMed] [Google Scholar]
- 18.Deville C, Hwang W-T, Burgos R, Chapman CH, Both S, Thomas CR. Diversity in graduate medical education in the United States by race, ethnicity, and sex, 2012. JAMA internal medicine. 2015;175(10):1706–8. doi: 10.1001/jamainternmed.2015.4324 [DOI] [PubMed] [Google Scholar]
- 19.Andriole DA, Jeffe DB, Schechtman KB. Is surgical workforce diversity increasing? Journal of the American College of Surgeons. 2007;204(3):469–77. doi: 10.1016/j.jamcollsurg.2006.12.035 [DOI] [PubMed] [Google Scholar]
- 20.Butler PD, Longaker MT, Britt LD. Major deficit in the number of underrepresented minority academic surgeons persists. Annals of surgery. 2008;248(5):704–9. doi: 10.1097/SLA.0b013e31817f2c30 [DOI] [PubMed] [Google Scholar]
- 21.Ulloa JG, Viramontes O, Ryan G, Wells K, Maggard-Gibbons M, Moreno G. Perceptual and Structural Facilitators and Barriers to Becoming a Surgeon: A Qualitative Study of African-American and Latino Surgeons. Academic medicine: journal of the Association of American Medical Colleges. 2018;93(9):1326. doi: 10.1097/ACM.0000000000002282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Davis G, Allison R. White coats, black specialists? Racial divides in the medical profession. Sociological Spectrum. 2013;33(6):510–33. [Google Scholar]
- 23.Elkbuli A, Narvel RI, Dowd B, McKenney M, Boneva D. Distribution of General Surgery Residencies in the United States and Gender Inequality: Are We There Yet? Journal of Surgical Education. 2019;76(6):1460–8. doi: 10.1016/j.jsurg.2019.05.008 [DOI] [PubMed] [Google Scholar]
- 24.Kane K, Rosero EB, Clagett GP, Adams-Huet B, Timaran CH. Trends in workforce diversity in vascular surgery programs in the United States. Journal of vascular surgery. 2009;49(6):1514–9. doi: 10.1016/j.jvs.2009.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vemulakonda VM, Sorensen MD, Joyner BD. The current state of diversity and multicultural training in urology residency programs. The Journal of urology. 2008;180(2):668–72. doi: 10.1016/j.juro.2008.04.030 [DOI] [PubMed] [Google Scholar]
- 26.Sims HS. More of the Same: Why isn’t otolaryngology becoming more diverse?
- 27.Lett LA, Orji WU, Sebro R. Declining racial and ethnic representation in clinical academic medicine: a longitudinal study of 16 US medical specialties. PLoS One. 2018;13(11):e0207274. doi: 10.1371/journal.pone.0207274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McAlister RP, Andriole DA, Brotherton SE, Jeffe DB. Are entering obstetrics/gynecology residents more similar to the entering primary care or surgery resident workforce? American journal of obstetrics and gynecology. 2007;197(5):536. e1-. e6. doi: 10.1016/j.ajog.2007.07.031 [DOI] [PubMed] [Google Scholar]
- 29.Friedman AL, Workforce AAoPCoP. Enhancing the diversity of the pediatrician workforce. Pediatrics. 2007;119(4):833. doi: 10.1542/peds.2007-0158 [DOI] [PubMed] [Google Scholar]
- 30.Spector ND, Cull W, Daniels SR, Gilhooly J, Hall J, Horn I, et al. Gender and generational influences on the pediatric workforce and practice. Pediatrics. 2014;133(6):1112–21. doi: 10.1542/peds.2013-3016 [DOI] [PubMed] [Google Scholar]
- 31.Jewett EA, Anderson MR, Gilchrist GS. The pediatric subspecialty workforce: public policy and forces for change. Pediatrics. 2005;116(5):1192–202. doi: 10.1542/peds.2004-2339 [DOI] [PubMed] [Google Scholar]
- 32.Association of American Medical Colleges. Table B3. Number of Active Residents, by Type of Medical School, GME Specialty, and Gender: Association of American Medical Colleges; 2016 [https://www.aamc.org/data/448482/b3table.html.
- 33.Burkhardt J, DesJardins S, Gruppen L. Diversity in Emergency Medicine: Are We Supporting a Career Interest in Emergency Medicine for Everyone? Ann Emerg Med. 2019;74(6):742–50. doi: 10.1016/j.annemergmed.2019.04.008 [DOI] [PubMed] [Google Scholar]
- 34.Braddock C 3rd. Strategies to Enhance Diversity in Emergency Medicine: Finding Actionable Solutions. Annals of emergency medicine. 2019;74(6):751. doi: 10.1016/j.annemergmed.2019.08.450 [DOI] [PubMed] [Google Scholar]
- 35.Tunson J, Boatright D, Oberfoell S, Bakes K, Angerhofer C, Lowenstein S, et al. Increasing resident diversity in an emergency medicine residency program: a pilot intervention with three principal strategies. Academic Medicine. 2016;91(7):958–61. doi: 10.1097/ACM.0000000000000957 [DOI] [PubMed] [Google Scholar]
- 36.Landry AM, Stevens J, Kelly SP, Sanchez LD, Fisher J. Under-represented minorities in emergency medicine. The Journal of emergency medicine. 2013;45(1):100–4. doi: 10.1016/j.jemermed.2012.11.064 [DOI] [PubMed] [Google Scholar]
- 37.Burkhardt JC. Meeting the Need for Emergency Medicine Physicians: A National Study of Factors Influencing Medical Specialty Career Choice. Ann Arbor: University of Michigan; 2019. [Google Scholar]
- 38.More Women Than Men Enrolled in U.S. Medical Schools in 2017 [press release]. AAMC News, December 18, 2017 2017.
- 39.Greenwood BN, Carnahan S, Huang L. Patient–physician gender concordance and increased mortality among female heart attack patients. Proceedings of the National Academy of Sciences. 2018:201800097. doi: 10.1073/pnas.1800097115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Geiger HJ. Racial stereotyping and medicine: the need for cultural competence. Cmaj. 2001;164(12):1699–700. [PMC free article] [PubMed] [Google Scholar]
- 41.Cooper LA, Powe NR. Disparities in patient experiences, health care processes, and outcomes: the role of patient-provider racial, ethnic, and language concordance: Commonwealth Fund New York, NY; 2004.
- 42.Doescher MP, Saver BG, Franks P, Fiscella K. Racial and ethnic disparities in perceptions of physician style and trust. 2000. [DOI] [PubMed] [Google Scholar]
- 43.Cooper-Patrick L, Gallo JJ, Gonzales JJ, Vu HT, Powe NR, Nelson C, et al. Race, gender, and partnership in the patient-physician relationship. Jama. 1999;282(6):583–9. doi: 10.1001/jama.282.6.583 [DOI] [PubMed] [Google Scholar]
- 44.David RA, Rhee M. The impact of language as a barrier to effective health care in an underserved urban Hispanic community. Mount Sinai Journal of Medicine. 1998;65:393–7. [PubMed] [Google Scholar]
- 45.Cooper LA, Roter DL, Carson KA, Beach MC, Sabin JA, Greenwald AG, et al. The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. American journal of public health. 2012;102(5):979–87. doi: 10.2105/AJPH.2011.300558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gordon HS, Street RL Jr, Sharf BF, Kelly PA, Souchek J. Racial differences in trust and lung cancer patients’ perceptions of physician communication. Journal of clinical oncology. 2006;24(6):904–9. doi: 10.1200/JCO.2005.03.1955 [DOI] [PubMed] [Google Scholar]
- 47.Penner LA, Dovidio JF, West TV, Gaertner SL, Albrecht TL, Dailey RK, et al. Aversive racism and medical interactions with Black patients: A field study. Journal of experimental social psychology. 2010;46(2):436–40. doi: 10.1016/j.jesp.2009.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kaplan SH, Gandek B, Greenfield S, Rogers W, Ware JE. Patient and visit characteristics related to physicians’ participatory decision-making style: Results from the Medical Outcomes Study. Medical care. 1995:1176–87. doi: 10.1097/00005650-199512000-00002 [DOI] [PubMed] [Google Scholar]
- 49.Johnson RL, Roter D, Powe NR, Cooper LA. Patient race/ethnicity and quality of patient–physician communication during medical visits. American journal of public health. 2004;94(12):2084–90. doi: 10.2105/ajph.94.12.2084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schouten BC, Meeuwesen L. Cultural differences in medical communication: a review of the literature. Patient education and counseling. 2006;64(1–3):21–34. doi: 10.1016/j.pec.2005.11.014 [DOI] [PubMed] [Google Scholar]
- 51.Siminoff LA, Graham GC, Gordon NH. Cancer communication patterns and the influence of patient characteristics: disparities in information-giving and affective behaviors. Patient education and counseling. 2006;62(3):355–60. doi: 10.1016/j.pec.2006.06.011 [DOI] [PubMed] [Google Scholar]
- 52.Gordon HS, Street RL Jr, Sharf BF, Souchek J. Racial differences in doctors’ information‐giving and patients’ participation. Cancer. 2006;107(6):1313–20. doi: 10.1002/cncr.22122 [DOI] [PubMed] [Google Scholar]
- 53.Sabin JA, Greenwald AG. The influence of implicit bias on treatment recommendations for 4 common pediatric conditions: pain, urinary tract infection, attention deficit hyperactivity disorder, and asthma. American journal of public health. 2012;102(5):988–95. doi: 10.2105/AJPH.2011.300621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Carline JD, Greer T. Comparing physicians’ specialty interests upon entering medical school with their eventual practice specialties. Academic Medicine. 1991;66(1):44–6. doi: 10.1097/00001888-199101000-00013 [DOI] [PubMed] [Google Scholar]
- 55.Compton MT, Frank E, Elon L, Carrera J. Changes in US medical students’ specialty interests over the course of medical school. Journal of general internal medicine. 2008;23(7):1095–100. doi: 10.1007/s11606-008-0579-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lieu TA, Schroeder SA, Altman DF. Specialty choices at one medical school: recent trends and analysis of predictive factors. Academic Medicine. 1989;64(10):622–9. [PubMed] [Google Scholar]
- 57.Wright B, Scott I, Woloschuk W, Brenneis F. Career choice of new medical students at three Canadian universities: family medicine versus specialty medicine. Canadian Medical Association Journal. 2004;170(13):1920–4. doi: 10.1503/cmaj.1031111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Burkhardt J, DesJardins S, Gruppen L. Identifying Barriers to a Diverse Emergency Physician Workforce. Ann Emerg Med. 2020; In Press. doi: 10.1016/j.annemergmed.2020.03.002 [DOI] [PubMed] [Google Scholar]
- 59.Clark BR. The “cooling out” function revisited. New directions for community colleges. 1980;1980(32):15–31. [Google Scholar]
- 60.Clark BR. The" cooling-out" function in higher education. American journal of Sociology. 1960;65(6):569–76. [Google Scholar]
- 61.Simon HA. Theories of Bounded Rationality. In: McGuire CB, Radner R, editors. Decision and Organization. 1: North-Holland Publishing Company; 1972. p. 161–76. [Google Scholar]
- 62.Schilirò D. Economic Decisions and Simon’s Notion of Bounded Rationality2018. 64 p.
- 63.Burkhardt JC, Smith-Coggins R, Santen S. Residents values in a rational decision-making model: an interest in academics in emergency medicine. Intern Emerg Med. 2016;11(7):993–7. doi: 10.1007/s11739-016-1408-8 [DOI] [PubMed] [Google Scholar]
- 64.Bandura A. Self-efficacy: Toward a Unifying Theory of Behavioral Change. Psychological Review. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191 [DOI] [PubMed] [Google Scholar]
- 65.Betz N, Hackett G. Applications of Self-Efficacy Theory to Understanding Career Choice Behavior. Journal of Social and Clinical Psychology. 1986;4(8):279–89. [Google Scholar]
- 66.Lent RW, Brown SD, Larkin KC. Self-Efficacy in the Prediction of Academic Performance and Perceived Career Options. Journal of Counseling Psychology. 1986;33(3):265–9. [Google Scholar]
- 67.Basco WT Jr, Reigart JR. When do medical students identify career-influencing physician role models? Academic Medicine. 2001;76(4):380–2. doi: 10.1097/00001888-200104000-00017 [DOI] [PubMed] [Google Scholar]
- 68.Wright S, Wong A, Newill C. The impact of role models on medical students. Journal of General Internal Medicine. 1997;12(1):53–6. doi: 10.1046/j.1525-1497.1997.12109.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Association of American Colleges. Underrepresented in Medicine Definition 2015 [https://www.aamc.org/initiatives/urm/.
- 70.Rodriguez A, Furquim F, DesJardins SL. Categorical and Limited Dependent Variable Modeling in Higher Education. Higher Education: Handbook of Theory and Research: Springer; 2018. p. 295–370. [Google Scholar]
- 71.Scott I, Gowans M, Wright B, Brenneis F. Stability of Medical Student Career Interest: A Prospective Study. Academic Medicine. 2012;87(9):1260–7. doi: 10.1097/ACM.0b013e31826291fa [DOI] [PubMed] [Google Scholar]
- 72.Scott I, Gowans MC, Wright B, Brenneis F. Why medical students switch careers: changing course during the preclinical years of medical school. Canadian Family Physician. 2007;53(1):94–5. [PMC free article] [PubMed] [Google Scholar]
- 73.Scott IM, Wright BJ, Brenneis FR, Gowans MC. Whether or wither some specialties: a survey of Canadian medical student career interest. BMC Medical Education. 2009;9(1):57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kassebaum DG, Szenas PL, Schuchert MK. Determinants of the generalist career intentions of 1995 graduating medical students. Academic medicine: journal of the Association of American Medical Colleges. 1996;71(2):198–209. doi: 10.1097/00001888-199602000-00030 [DOI] [PubMed] [Google Scholar]
- 75.Malhi GS, Parker G, Parker K, Carr V, Kirkby K, Yellowlees P, et al. Attitudes toward psychiatry among students entering medical school. Acta Psychiatrica Scandinavica. 2003;107(6):424–9. doi: 10.1034/j.1600-0447.2003.00050.x [DOI] [PubMed] [Google Scholar]
- 76.Kozar RA, Anderson KD, Escobar-Chaves SL, Thiel MA, Brundage SI. Preclinical students: who are surgeons?1. Journal of Surgical Research. 2004;119(2):113–6. [DOI] [PubMed] [Google Scholar]
- 77.Newton DA, Grayson MS. Trends in Career Choice by US Medical School Graduates. JAMA. 2003;290(9):1179–82. doi: 10.1001/jama.290.9.1179 [DOI] [PubMed] [Google Scholar]
- 78.Kassebaum DG, Szenas PL. Medical students’ career indecision and specialty rejection: roads not taken. Academic medicine: journal of the Association of American Medical Colleges. 1995;70(10):937–43. [DOI] [PubMed] [Google Scholar]
- 79.Carline JD, Greer T. Comparing physicians’ specialty interests upon entering medical school with their eventual practice specialties. Academic medicine: journal of the Association of American Medical Colleges. 1991;66(1):44–6. doi: 10.1097/00001888-199101000-00013 [DOI] [PubMed] [Google Scholar]
- 80.Borges NJ, Navarro AM, G A.: Hoban J.D. How, When, and Why Do Physicians Choose Careers in Academic Medicine? A Literature Review. Academic Medicine. 2010;85(4):680–6. doi: 10.1097/ACM.0b013e3181d29cb9 [DOI] [PubMed] [Google Scholar]
- 81.Association of American Colleges. ERAS Statisitcs: Association of American Medical Colleges; 2020 [https://www.aamc.org/eras-statistics-2019.
- 82.Witherspoon EB, Vincent-Ruz P, Schunn CD. When Making the Grade Isn’t Enough: The Gendered Nature of Premed Science Course Attrition. Educational Researcher. 2019:0013189X19840331. [Google Scholar]
- 83.Beyer S, Bowden EM. Gender differences in seff-perceptions: Convergent evidence from three measures of accuracy and bias. Personality and Social Psychology Bulletin. 1997;23(2):157–72. [Google Scholar]
- 84.Kugler AD, Tinsley CH, Ukhaneva O. Choice of majors: Are women really different from men?: National Bureau of Economic Research; 2017. Report No.: 0898–2937.
- 85.Krupat E, Camargo CA, Strewler GJ, Espinola JA, Fleenor TJ, Dienstag JL. Factors associated with physicians’ choice of a career in research: a retrospective report 15 years after medical school graduation. Advances in Health Sciences Education. 2017;22(1):5–15. doi: 10.1007/s10459-016-9678-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Richards RD. Underrespresentd Minority Medical (URiM) Students: A Social Work Approach to Identifying Factors Affecting Their Experience. 2020-CSU Theses and Dissertations. 2020. [Google Scholar]
- 87.Roberts LW. Belonging, Respectful Inclusion, and Diversity in Medical Education. Academic Medicine. 2020;95(5):661–4. doi: 10.1097/ACM.0000000000003215 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data cannot be shared publicly by the author as it is used under a data usage agreement with the Association of American Medical Colleges (AAMC) and the National Board of Medical Examiners (NBME). Data can be obtained from those organizations through research requests as was done in this case. Data are held by a third party. The authors did not have any special access privileges to the data, and obtained the data in the same way as detailed in their data access guidelines published online. https://www.aamc.org/request-aamc-data https://www.nbme.org/services/data-sharing.