Abstract
Background:
The interscalene brachial plexus block (ISB) is a commonly used nerve block technique for postoperative analgesia in patients undergoing shoulder arthroscopy surgery; however, it is associated with potentially serious complications. The use of suprascapular nerve block (SSNB) and axillary Nerve Block (ANB) has been reported as an alternative nerve block with fewer reported side effects for shoulder arthroscopy. This review aimed to compare the impact of SSNB and ANB with ISB during shoulder arthroscopy surgery.
Methods:
A meta-analysis was conducted to identify relevant randomized or quasirandomized controlled trials involving SSNB and ISB during shoulder arthroscopy surgery. We searched Web of Science, PubMed, Embase, Cochrane Controlled Trials Register, Cochrane Library, Highwire, CNKI, and Wanfang database from 2010 through August 2021.
Results:
We identified 641 patients assessed in 10 randomized or quasirandomized controlled trials. Compared with the ISB group, the SSNB+ANB group had higher visual analog scale or numerical rating scale in PACU (P = .03), 4 hour (P = .001),6 hour after the operation (P = .002), and lower incidence of complications such as Numb/Tingling (P = .001), Weakness (P <.00001), Horner syndrome (P = .001) and Subjective dyspnea (P = .002). No significant difference was found for visual analog scale or numerical rating scale 8 hour (P = .71),12 hour (P = .17), 16 hour (P = .38),1day after operation (P = .11), patient satisfaction (P = .38) and incidence of complications such as hoarseness (P = .07) and nausea/vomiting (P = .41) between 2 groups.
Conclusion:
Our high-level evidence has established SSNB+ ANB as an effective and safe analgesic technique and a clinically attractive alternative to interscalene block during arthroscopic shoulder surgery, especially for severe chronic obstructive pulmonary disease, obstructive sleep apnea, and morbid obesity. Given our meta-analysis's relevant possible biases, we required more adequately powered and better-designed randomized controlled trial studies with long-term follow-up to reach a firmer conclusion.
Keywords: arthroscopy, axillary, interscalene, nerve block, regional, shoulder, suprascapular
1. Introduction
There is a high incidence reaching up to 45%; of severe intraoperative and postoperative pain associated with arthroscopic shoulder surgery, which is often significant enough to interfere with initial recovery and rehabilitation.[1] Various peripheral nerve blocks have been used to reduce intraoperative anesthetic requirements to improve rapid recovery and reduce postoperative pain.[2,3] Of all blocks, Interscalene brachial plexus block (ISB) is the most frequently used block, as it provides adequate postoperative analgesia for 6 to 12 hours.[4] However, ISB has the potential for some complications. The most common of these complications is phrenic nerve palsy ISB which can result in diaphragmatic paralysis.[5,6] Less common complications included respiratory distress, weakness of the arm, hoarseness of voice, Horner's syndrome and brachial plexus neuropathy.[7–9] Therefore, ISB is contraindicated in patients with contralateral phrenic nerve palsy, severe preexisting respiratory insufficiency due to chronic obstructive pulmonary disease, restrictive pulmonary disease, bronchial asthma, and high body mass index.[6,10]
Recently, the Combined suprascapular nerve block and axillary nerve block (SSNB+ANB) was proposed to provide anesthesia and postoperative analgesia for shoulder surgery as a safe alternative to ISB.[1] ISB provides anesthesia for the shoulder joint by blocking C5 and C6 nerve roots, and most of the nerve supply from C5 and C6 nerve roots are also carried by suprascapular and the axillary nerves. These two peripheral nerves are responsible for the majority of the sensory innervation of the shoulder.
But there is still a conflicting view in the literature regarding the effect of combined blockade of SSNB and ANB compared with ISB. The purpose of our meta-analysis was to compare the analgesic efficacy of the SSNB+ANB and ISB, which was measured in terms of the visual analog scale (VAS) score or numerical rating scale (NRS) in the first 24 h after surgery and incidence of complications. The secondary aims were to study patient satisfaction scores.
2. Methods
The current meta-analysis was registered on PROSPERO (International prospective register of systematic reviews) and the registration number was CRD42020210385. This meta-analysis was performed using a predetermined protocol following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement to assess the results’ quality to make sure our meta-analysis's results reliable and veritable.
2.1. Search strategy
Web of Science, PubMed, Embase, Cochrane Controlled Trials Register, Cochrane Library, Highwire, CNKI, and Wanfang database were searched from 2010 through August 2021. The keywords used were “ nerve block,” “ regional,” “ suprascapular,” “ interscalene,” “axillary,” ”shoulder,” ”arthroscopic in conjunction with Boolean operators “AND” or “OR.” We used Review Manager Software for MAC to perform the meta-analysis.
2.2. Inclusion criteria
Studies were eligible if 1. The intervention was patients undergoing shoulder arthroscopic surgery with SSNB+ANB; 2. The comparator was patients undergoing shoulder arthroscopic surgery with ISB 3. The design of the study was a randomized controlled trials (RCTs) or quasirandomized controlled trials.; 4. The studies were required to contain at least one clinical outcome data; The exclusion criteria were as follows: studies with insufficient clinical outcome data.
2.3. Data extraction process
Two reviewers (C.J.S and H.D.Y) used a standardized form to extract data. A third reviewer (X.L.J.) was used to resolve disagreements in eligibility, data extraction, or quality assessment. Extracted data included the primary data based on the following: first author, year of publication, participants, age, gender, body mass index, follow up, type of surgery, Localization method, analgesia Used in nerve block, Analgesia Used in PACU, Analgesia Used in the ward.
2.4. Assessment of studies
We assessed the studies’ methodological quality following the Cochrane Handbook's instructions for Systematic Reviews of Interventions.
2.5. Ethical consideration
The adverse effects of the intervention were identified for inclusion in the study and reported as a composite outcome. All included studies had appropriate ethical approval.
2.6. Statistical analysis
RevMan software (version 5.3; The Cochrane Collaboration) was used for the analysis. We used a random-effects model for all analyses, as clinical heterogeneity was assumed to exist because of differences in standardization in anesthetic, nerve block techniques, diversity of shoulder surgeries performed, and the timing of assessment across studies.
Data were summarized as the ratio of relative risk (patient satisfaction, complications including the rate of Numb/Tingling, weakness, horner syndrome, subjective dyspnea, hoarseness, Nausea/vomiting. or the difference between means (VAS or NRS and patient satisfaction). Studies that did not have standard deviations were calculated from p values, confidence intervals, or standard errors. The results were considered as a statistically significant difference when P values were less than .05.
3. Results
The literature search identified 386 citations. Of these, we removed 305 duplicates. After reviewing the 81 remaining articles’ titles and abstracts, we excluded 61 papers according to the inclusion and exclusion criteria; 20 full texts were retrieved. Because some articles didn’t compare the SSBN+ANB with Block ISB, we excluded eight studies. Finally, we identified 641 patients assessed in 10 articles[10–19] (Fig. 1). Study baseline characteristics and general intervention information are summarized in Tables 1 and 2.
Figure 1.
The search results and selection procedure. The literature search identified 386 citations. Of these, we removed 305 duplicates. After reviewing the 81 remaining articles’ titles and abstracts, we excluded 61 papers according to the inclusion and exclusion criteria; 20 full texts were retrieved. Because some articles didn’t compare the SSBN+ANB with Block ISB, we excluded ten studies. Finally, we identified 641 patients assessed in 10 articles.
Table 1.
Characteristics of included studies and patients.
| Sample sizes, n | Age, yr, Mean | %Female | BMI,kg/m2 | ||||
| Study | Country | (SSNB/ISB) | Follow-up | Surgery | |||
| Dhir 2016 | Canada | 29/30 | 46.5/51.3 | 24.1/13.3 | 29/28.9 | 7 d | Shoulder arthroscopy |
| Lee 2012 | South Korea | 18/26 | 54/57 | 44.4/57.7 | 23.62/24.92 | 24 h | Arthroscopic rotator cuff |
| Li 2020 | China | 40/40 | 51.1/53 | 57.5/52.5 | 22.81/23.39 | 24 h | Arthroscopic rotator cuff |
| Luo 2019 | China | 20/20 | 48.6/49.6 | 45/55 | 24.84/23.91 | 72 h | Shoulder arthroscopy |
| Neuts 2018 | Belgium | 48/50 | 51/54 | 62.5/44 | 26/26 | 24 h | Shoulder arthroscopy |
| Pani 2019 | India | 35/37 | 37.1/37.7 | 17.1/21.6 | 26.027/25.083 | 24 h | Shoulder arthroscopy |
| Pitombo 2013 | Brazil | 34/34 | 52.2/55 | 52.9/61.8 | 26.79/27.95 | 24 h | Shoulder arthroscopy |
| Saini 2021 | India | 35/35 | 26.97/27.29 | 11.5/14.3 | 24.99/24.03 | 24 h | Arthroscopic Bankart repair |
| Waleed 2016 | Egypt | 30/30 | 28.6/27.4 | 33.3/36.7 | 24.32/24.65 | 24 h | Shoulder arthroscopy |
| Zanfaly 2015 | Egypt | 25/25 | 43.5/44.6 | 36/44 | NA | 24 h | Shoulder arthroscopy |
AXB = axillary nerves block, BMI = body mass index. ISB = interscalene block, SSNB = suprascapular nerve block.
The detailed baseline characteristics information including country, number of participants, age, gender, BMI, follow-up time and type of surgery.
Table 2.
Details of the nerve blocks and anesthesia used.
| Study | Localization method | Analgesia used in SSNB + AXB | Analgesia used in ISB | Analgesia used in PACU | Analgesia used in ward |
| Dhir 2016 | Ultrasound and nerve stimulator guided | 15 mL of 0.5% ropivacaine + 15 mL of 0.5% ropivacaine | 20 mL of 0.5% ropivacaine. | Ketorolac, acetaminophen | NA |
| Lee 2012 | Ultrasound and nerve stimulator guided | 2% mepivacaine 10 ml and 0.75% ropivacaine 20 ml | 2% mepivacaine 5 ml and 0.75% ropivacaine 10 ml | NA | NA |
| Li 2020 | Ultrasound guided | 10 mL of 0.5% ropivacaine + 10 mL of 0.5% ropivacaine | 20 mL of 0.5% ropivacaine. | flurbiprofen axetil IV (50mg) was used as rescue analgesia when VAS > 4 | flurbiprofen axetil IV (50mg) was used as rescue analgesia when VAS > 4 |
| Luo 2019 | Ultrasound guided | 15 mL of 0.25% ropivacaine + 5 mL of 0.25% ropivacaine | 20 mL of 0.25% ropivacaine. | NA | NA |
| Neuts 2018 | Ultrasound guided | 10 mL of 0.75% ropivacaine + 10 mL of 0.75% ropivacaine | 20 mL of 0.75% ropivacaine | intravenous paracetamol (15 mg/kg 4 times a day), ketorolac (0.5 mg/kg 3 times a day), and PCIA with piritramide (bolus dose = 2 mg and lockout inter- val = 12 min). | NA |
| Pani 2019 | Ultrasound and nerve stimulator guided | 10 mL of 0.75% ropivacaine + 10 mL of 0.75% ropivacaine | 10 mL of 0.75% ropivacaine | Paracetamol IV (1 gm) was used as rescue analgesia when VAS > 4 | Paracetamol IV (1 gm) was used as rescue analgesia when VAS > 4 |
| Pitombo 2013 | Ultrasound and nerve stimulator guided | 15 mL of 0.33% levobupivacaine with epinephrine 1:200,000 + 15 mL of 0.33% levobupivacaine with epinephrine 1:200,000 | 30 mL of 0.33% levobupivacaine with epinephrine 1:200,000 | In case of moderate (> 3 ≤ 6) or severe (> 7) pain, single-dose intravenous morphine (0.04 mg/kg) | NA |
| Saini 2021 | Ultrasound and nerve stimulator guided | 10 mL of 0.5% ropivacaine+10 mL of 0.5% ropivacaine | 10 mL of 0.5% ropivacaine | paracetamol 1 g IV was administered on demand or if VAS was ≥ 4 | paracetamol 1 g IV was administered on demand or if VAS was ≥ 4 |
| Waleed 2016 | Ultrasound guided | 10 ml of 0.25% levobupivacaine/10 ml of 0.25% levobupivacaine | 20 ml of 0.25% levobupivacaine | NA | NA |
| Zanfaly 2015 | Ultrasound and nerve stimulator guided | 7–10 ml of 0.5% bupivacaine + 7–10 ml of 0.5% bupivacaine | 25–30 ml 0.5% bupivacaine | diclofenac natrium (voltaren) IM, every 8 h, If VAS >3 morphine 0.1 mg/kg IM | NA |
ACU = postanesthesia care unit, AXB = axillary nerves block, IM = intramuscular, ISB = interscalene block, IV = intravenous, NRS = numerical rating scale, SSNB = suprascapular nerve block, US = ultrasound, VAS = visual analog scale.
Details of the nerve blocks and anesthesia used to include localization method, analgesia, used in nerve block, analgesia used in PACU and analgesia used in ward.
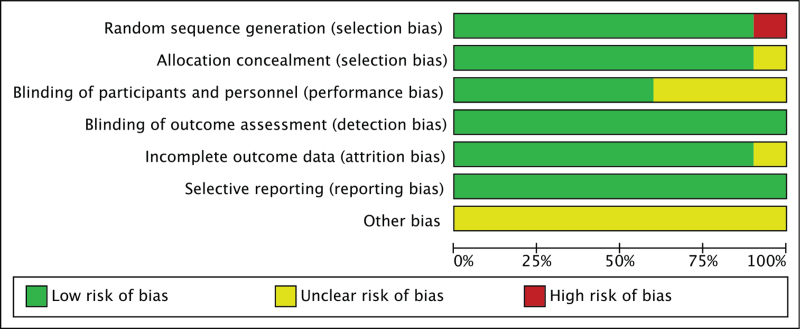
The risk of bias summary and bias graph for RCTs is shown in Figures 2 and 3. Nine studies adequately described the correct randomization. Nine studies demonstrated sufficient allocation concealment. Six studies described the blinding of participants and personnel. All ten articles described the blinding of outcome assessment and avoided selective reporting. Nine articles retained complete outcome data. We rated as unclear risk of other bias because we can’t ignore other potential dangers of biases. As a result, the risk of bias is low or moderate in most of the articles reviewed. (Fig. 2).
Figure 2.
Risk of bias summary for included studies. ? = bias unknown. + = no bias, - = bias. Nine studies adequately described the correct randomization. Nine studies demonstrated sufficient allocation concealment. Six studies described the blinding of participants and personnel. All ten articles described the blinding of outcome assessment and avoided selective reporting. Nine articles retained complete outcome data. We rated as unclear risk of other bias because we can’t ignore other potential dangers of biases. As a result, the risk of bias is low or moderate in most of the articles reviewed.
Figure 3.
The risk of bias graph. The overall quality of the included studies was considered adequate
3.1. VAS or NRS
The pooled results showed that ISB group had lower VAS or NRS in PACU (MD = 1.38, 95% confidence intervals [CI] [0.16,2.60], P = .03 Fig. 4),4 hour after operation (MD = 1.78, 95% CI [0.72,2.85], P = .001 Fig. 4). and 6 hour after operation (MD = 1.08, 95% CI [0.40, 1.76], P = .002 Fig. 4). No significant difference was found for VAS or NRS 8 hour after operation (MD = 0.3, 95% CI [-1.28,1.88], P = .71 Fig. 4), 12 hours (MD = -0.51, 95% CI [-1.23,0.21], P = .17 Fig. 4), 16 hour (MD = -0.75, 95% CI [-2.4,0.91], P = .38 Fig. 4) and 1day after operation (MD = -0.5, 95% CI [-1.13,0.12], P = .11 Fig. 4) between 2 groups.
Figure 4.
A forest plot diagram showing VAS or NRS The pooled results showed that ISB group had lower VAS or NRS in PACU (MD = 1.38, 95% CI [0.16,2.60], P = .03),4 h after operation (MD = 1.78, 95% CI [0.72,2.85], P = .001). and 6 h after operation (MD = 1.08, 95% CI [0.40, 1.76], P = .002). No significant difference was found for VAS or NRS 8 h after operation(MD = 0.3, 95% CI [-1.28,1.88], P = .71),12 h (MD = -0.51, 95% CI [-1.23,0.21], P = .17), 16 h (MD = -0.75, 95% CI [-2.4,0.91], P = .38)and 1d after operation((MD = -0.5, 95% CI [-1.13,0.12], P = .11) between two groups.
3.2. Block related complications
The pooled data showed that SSNB+ ANB group had lower incidence of Numb/Tingling (relative risk [RR] = 0.29, 95% CI [0.13,0.61], P = .001 Fig. 5),Weakness (RR = 0.11, 95% CI [0.05,0.24], P <.0001 Fig. 5), Horner syndrome (RR = 0.09, 95% CI [0.02,0.37], P = .001 Fig. 5) and Subjective dyspnea (RR = 0.19, 95% CI [0.07,0.55], P = .002 Fig. 5) No significant difference was found for Hoarseness (RR = 0.26, 95% CI [0.06,1.12], P = .07 Fig. 5), and nausea/vomiting (RR = 0.8, 95% CI [0.47,1.36], P = .41 Fig. 5).
Figure 5.
A forest plot diagram showing Block related complications. The pooled data showed that SSNB+ ANB group had lower incidence of numb/tingling (RR = 0.29, 95% CI [0.13,0.61], P = .001), weakness (RR = 0.11, 95% CI [0.05,0.24], P <.0001), Horner syndrome (RR = 0.09, 95% CI [0.02,0.37], P = .001) and Subjective dyspnea (RR = 0.19, 95% CI [0.07,0.55], P = .002). No significant difference was found for Hoarseness (RR = 0.26, 95% CI [0.06,1.12], P = .07), and nausea/vomiting (RR = 0.8, 95% CI [0.47,1.36], P = .41).
3.3. Patient satisfaction
We didn’t find any significant difference for patient satisfaction (MD = 0.31, 95% CI [-0.38,0.99], P = .38 Fig. 6).
Figure 6.
A forest plot diagram showing patient satisfaction. We didn’t find any significant difference for patient satisfaction MD = 0.31, 95% CI [-0.38,0.99], P = .38).
4. Discussion
Our study is the first meta-analysis to identify relevant randomized controlled trials or quasirandomized controlled trials involving SSNB+ANB and ISB during arthroscopic shoulder surgery. The postoperative pain at the individual time points suggested that SSNB+ANB may provide inferior pain control limited to the PACU stay, 4 hours and 6 hours after the operation. However, SSNB+ANB was not different from ISB for providing postoperative pain control at other time points for the first 24 hours after surgery. Furthermore, SSBNB+ANB was associated with a lower incidence of numb/tingling, weakness, horner syndrome, and subjective dyspnea. The remaining analgesic outcome results, such as patient satisfaction and other nerve block complications, including Hoarseness and nausea/vomiting, were consistently not different between the 2 groups.
In our study, SSNB+ANB provided inadequate analgesia to ISB in the immediate postoperative period at PACU,4 hours, and 6 hours. The analgesic difference between the two groups gradually decreased as the blocks wore off, and pain scores became comparable during the 12 hours,16 hours, and 1day after surgery between SSNB+ANB and ISB groups. There are several reasons for increased pain in the SSNB+ANB group in the immediate postoperative period. First, irrigation fluid from the arthroscopic procedure may take up to 12 hours to be absorbed; Second, capsular overdistension may contribute to the increased pain in the SSNB+ANB group. Third, the subscapular muscles, the acromioclavicular articulation, and the anterior portion of the glenohumeral articular capsule are not supplied by the SSNB+ANB technique. Fourth, The suprascapular nerve's superior articular branch may leave the nerve before entering the suprascapular fossa.[20]
In our meta-analysis, the incidence of numb/tingling, weakness, Horner syndrome, and subjective dyspnea was higher and statistically significant in the ISB group compared with the SSNB + ANB group. Interscalene block causes a motor blockade of muscles supplied by the brachial plexus, resulting in weakness extending to the forearm and hand. The radial, median, musculocutaneous, and ulnar nerves receive contributions from C7-T1 nerve roots. As the ISB technique is most often done at the level of C5-C6, the ISB may spare the lower segments (C7-T1) of the brachial plexus,[21] so the patients may be present with numb or tingling. Urmey et al. reported all patients undergoing ISB had the complication of phrenic nerve block, which may be due to the unpredictable local anesthetic spread to adjacent structures like neural structures or the stellate ganglion.[22] The patients may present with Horner syndrome and Subjective dyspnea.
The present study showed a good patient satisfaction level in both the SSNB+ANB group and the ISB group. Motor blockade associated with an SSNB and AXNB is confined to the deltoid, supraspinatus, infraspinatus, and teres minor muscles (posterior rotator cuff). The outer pectoral girdle muscles such as latissimus dorsi and pectoral are preserved and those of the hand, forearm, and upper arm. Thus, in addition to provide analgesia, the SSNB +ANB technique provides potential conservation of the patient's functional capacity to improve patient satisfaction.
Management of arthroscopic shoulder surgery pain is often accomplished by using opioids; however, their use is often associated with side effects such as vomiting, nausea, dysphoria, respiratory depression, and hormonal effects.[23,24]
Our findings may have an impact on clinical practice. The minor analgesic advantages of ISB compared with the SSNB+ANB seem to be transient and limited to the immediate postoperative period (before 6 hours after the operation). In contrast, the risk of block-related complications associated with ISB may outweigh its benefits in specific settings or patient populations, especially when SSNB can offer a safe and effective alternative in patients with the severe chronic obstructive pulmonary disease,[7,25] obstructive sleep apnea,[26] contralateral phrenic nerve and morbid obesity.[27] Our findings established the SSNB+ANB's clinical benefits as an attractive, effective treatment for postoperative pain in patients undergoing arthroscopic shoulder surgery.
4.1. Limitations
Our meta-analysis has limitations that should be acknowledged. First, heterogeneity was found across the included studies in terms of standardization in nerve block techniques, the dose of anesthetic, type of shoulder surgeries performed as well as the timing of assessment, which precluded the pooling of many of outcomes. Second, some studies included in this review had smaller sample sizes, which may decrease the strength of their effect and limit external validity. Third, we didn’t evaluate the total opioid consumption because it's hard to calculate the total opioid consumption in these studies. Another bias inherent to the present study relates to the inability to blind the operator to the block technique being performed because of the interventions’ nature.
5. Conclusion
ISB seems to offer analgesic advantages that are transient and limited to 6 hours after the operation. SSNB +ANB is not different from ISB concerning postoperative pain severity between 6 hours to the first 24 hours postoperation. Furthermore, SSNB + ANB does appear to reduce the risk of numb/tingling, weakness, Horner syndrome, and Subjective dyspnea. Our high-level evidence has established SSNB + ANB as an effective and safe analgesic technique and a clinically attractive alternative to ISB during arthroscopic shoulder surgery, especially for patients of severe chronic obstructive pulmonary disease, obstructive sleep apnea, contralateral phrenic nerve, and morbid obesity. Given our meta-analysis's relevant possible biases, we required more adequately powered and better-designed RCT studies with long-term follow-up to reach a firmer conclusion.
Author contributions
Conceptualization: Changjiao Sun, Xu Cai.
Data curation: Peng Yu.
Funding acquisition: Changjiao Sun.
Investigation: Xiaolin Ji, Xu Cai, Huadong Yang.
Methodology: Huadong Yang.
Project administration: Xiaolin Ji.
Resources: Xiaofei Zhang.
Software: Xiaofei Zhang.
Supervision: Changjiao Sun, Xiaolin Ji, Xu Cai, Huadong Yang.
Validation: Xiaofei Zhang.
Visualization: Huadong Yang.
Writing – original draft: Changjiao Sun.
Writing – review & editing: Changjiao Sun.
Footnotes
Abbreviations: ANB = Axillary Nerve Block, CI = confidence interval, ISB = interscalene block, NRS = numerical rating scale, RCTs = randomized controlled trials, RR = relative risk, SSNB = Suprascapular nerve block, VAS = visual analog scale.
How to cite this article: Sun C, Zhang X, Ji X, Yu P, Yang H, Cai X. Suprascapular nerve block and axillary nerve block versus interscalene nerve block for arthroscopic shoulder surgery: a meta-analysis of randomized controlled trials. Medicine. 2021;100:44(e27661).
XC and HY contributed equally to this work.
Ethics approval and consent to participate was not applicable.
Consent for publication was not applicable.
The authors have no funding and conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Checcucci G, Allegra A, Bigazzi P, Gianesello L, Ceruso M, Gritti G. A new technique for regional anesthesia for arthroscopic shoulder surgery based on a suprascapular nerve block and an axillary nerve block: an evaluation of the first results. Arthroscopy 2008;24:689–96. [DOI] [PubMed] [Google Scholar]
- [2].Borgeat A, Ekatodramis G. Anaesthesia for shoulder surgery. Best Pract Res Clin Anaesthesiol 2002;16:211–25. [DOI] [PubMed] [Google Scholar]
- [3].Ritchie ED, Tong D, Chung F, Norris AM, Miniaci A, Vairavanathan SD. Suprascapular nerve block for postoperative pain relief in arthroscopic shoulder surgery: a new modality? Anesth Analg 1997;84:1306–12. [DOI] [PubMed] [Google Scholar]
- [4].Abdallah FW, Halpern SH, Aoyama K, Brull R. Will the real benefits of single-shot interscalene block please stand up? A systematic review and meta-analysis. Anesth Analg 2015;120:1114–29. [DOI] [PubMed] [Google Scholar]
- [5].Verelst P, van Zundert A. Respiratory impact of analgesic strategies for shoulder surgery. Reg Anesth Pain Med 2013;38:50–3. [DOI] [PubMed] [Google Scholar]
- [6].Bergmann L, Martini S, Kesselmeier M, et al. Phrenic nerve block caused by interscalene brachial plexus block: breathing effects of different sites of injection. BMC Anesthesiol 2016;16:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Urmey WF, McDonald M. Hemidiaphragmatic paresis during interscalene brachial plexus block: effects on pulmonary function and chest wall mechanics. Anesth Analg 1992;74:352–7. [DOI] [PubMed] [Google Scholar]
- [8].Passannante AN. Spinal anesthesia and permanent neurologic deficit after interscalene block. Anesth Analg 1996;82:873–4. [DOI] [PubMed] [Google Scholar]
- [9].Borgeat A, Ekatodramis G, Kalberer F, Benz C. Acute and nonacute complications associated with interscalene block and shoulder surgery: a prospective study. Anesthesiology 2001;95:875–80. [DOI] [PubMed] [Google Scholar]
- [10].Yiping L, Yisheng H, Baolin Z, Yijian C, Wen Z. Application of ultrasound-guided suprascapular nerve combined with axillary nerve block for analgesia after shoulder arthroscopy. J Gannan University 2020;40:786–9. [Google Scholar]
- [11].Saini S, Rao SM, Agrawal N, Gupta A. Comparison of analgesic efficacy of shoulder block versus interscalene block for postoperative analgesia in arthroscopic shoulder surgeries: a randomised trial. Indian J Anaesth 2021;65:451–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Dhir S, Sondekoppam RV, Sharma R, Ganapathy S, Athwal GS. A comparison of combined suprascapular and axillary nerve blocks to interscalene nerve block for analgesia in arthroscopic shoulder surgery: an equivalence study. Reg Anesth Pain Med 2016;41:564–71. [DOI] [PubMed] [Google Scholar]
- [13].Lee SM, Park SE, Nam YS, et al. Analgesic effectiveness of nerve block in shoulder arthroscopy: comparison between interscalene, suprascapular and axillary nerve blocks. Knee Surg Sports Traumatol Arthrosc 2012;20:2573–8. [DOI] [PubMed] [Google Scholar]
- [14].Qianqian L. The effect of ultrasound-guided suprascapular nerve combined axillary nerve block on analgesia after shoulder arthroscopy [Master]. China Medical University; Feb 2019:29. [Google Scholar]
- [15].Neuts A, Stessel B, Wouters PF, et al. Selective suprascapular and axillary nerve block versus interscalene plexus block for pain control after arthroscopic shoulder surgery: a noninferiority randomized parallel-controlled clinical trial. Reg Anesth Pain Med 2018;43:738–44. [DOI] [PubMed] [Google Scholar]
- [16].Pani N, Routray SS, Pani S, Mallik S, Pattnaik S, Pradhan A. Post-operative analgesia for shoulder arthroscopic surgeries: a comparison between inter-scalene block and shoulder block. Indian J Anaesth 2019;63:382–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Pitombo PF, Meira Barros R, Matos MA, Pinheiro Módolo NS. Selective suprascapular and axillary nerve block provides adequate analgesia and minimal motor block. Comparison with interscalene block. Braz J Anesthesiol 2013;63:45–51. [DOI] [PubMed] [Google Scholar]
- [18].Waleed A. Postoperative analgesia for arthroscopic shoulder surgery: comparison between ultrasound-guided interscalene block and combined suprascapular and axillary nerve blocks. Ain-Shams J Anaesthesiol 2016;9:536–41. [Google Scholar]
- [19].Zanfaly HE, Aly AA. Shoulder block versus interscalene block for postoperative pain relief after shoulder arthroscopy. Ain-Shams J Anesth 2016;9:296–303. [Google Scholar]
- [20].Vorster W, Lange CP, Briët RJ, et al. The sensory branch distribution of the suprascapular nerve: an anatomic study. J Shoulder Elbow Surg 2008;17:500–2. [DOI] [PubMed] [Google Scholar]
- [21].Neal JM, Gerancher JC, Hebl JR, et al. Upper extremity regional anesthesia: essentials of our current understanding, 2008. Reg Anesth Pain Med 2009;34:134–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Urmey WF, Gloeggler PJ. Pulmonary function changes during interscalene brachial plexus block: effects of decreasing local anesthetic injection volume. Reg Anesth 1993;18:244–9. [PubMed] [Google Scholar]
- [23].Manchikanti L, Fellows B, Ailinani H, Pampati V. Therapeutic use, abuse, and nonmedical use of opioids: a ten-year perspective. Pain Physician 2010;13:401–35. [PubMed] [Google Scholar]
- [24].Seyfried O, Hester J. Opioids and endocrine dysfunction. Br J Pain 2012;6:17–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Urmey WF, Talts KH, Sharrock NE. One hundred percent incidence of hemidiaphragmatic paresis associated with interscalene brachial plexus anesthesia as diagnosed by ultrasonography. Anesth Analg 1991;72:498–503. [DOI] [PubMed] [Google Scholar]
- [26].D’Apuzzo MR, Browne JA. Obstructive sleep apnea as a risk factor for postoperative complications after revision joint arthroplasty. J Arthroplasty 2012;27: (8 Suppl): 95–8. [DOI] [PubMed] [Google Scholar]
- [27].Griffin JW, Novicoff WM, Browne JA, Brockmeier SF. Morbid obesity in total shoulder arthroplasty: risk, outcomes, and cost analysis. J Shoulder Elbow Surg 2014;23:1444–8. [DOI] [PubMed] [Google Scholar]