Abstract
Background:
Cancer-related fatigue (CRF) is one of the most common adverse events of anticancer therapies, with an incidence of up to 90%, which seriously affects the quality of life in cancer patients. Complementary and alternative therapies for CRF include acupuncture, Chinese herbal medicine, Tai Chi, Qigong, and massage therapy. Several studies have shown that traditional Chinese medicine (TCM) exercise therapies, such as Tai Chi, Ba Duan Jin, the classics of tendon changing, Six Healing Sounds, and Wu Qin Xi, can improve CRF, anxiety symptoms, and sleep quality in cancer patients. However, their specific efficacy and which TCM exercise therapy is the best remain controversial. In this study, we assess and compare the effects of different TCM exercise therapies on CRF, anxiety, and sleep quality in cancer patients by network meta-analysis (NMA).
Methods:
Randomized controlled trials reporting TCM exercise therapies for CRF, anxiety and sleep quality in cancer patients published before October 2021 will be searched in the PubMed, Web of Science, Scopus, Cochrane Library, Embase, China Scientific Journal Database, China National Knowledge Infrastructure, Chinese Biomedical Literature Database, and Wanfang Data. Two researchers will be independently responsible for literature screening, data extraction and assessment of their quality. Standard pair-wise and NMA will be performed to compare the efficacy of different TCM exercise therapies on CRF, anxiety and sleep quality in cancer patients using Stata 14.0 software.
Results:
The results of this meta-analysis will be submitted to a peer-reviewed journal for publication.
Conclusions:
This NMA will contribute to identify the optimal TCM exercise therapy for CRF and provide evidence-based bias for clinical decision-making.
Ethics and dissemination:
Ethical approval was not required for this study. The systematic review will be published in a peer-reviewed journal, presented at conferences, and shared on social media platforms.
OSF REGISTRATION NUMBER:
DOI 10.17605/OSF.IO/MJ8DA.
Keywords: anxiety, cancer, cancer-related fatigue, network meta-analysis, protocol, sleep, traditional Chinese medicine exercise
1. Introduction
The American Association for Cancer Research in 2019 proposed that massive cancer research has driven a substantial progress with continuously decreased cancer-related death and increased survival rate.[1] At present, quality of life and cancer-related symptoms in cancer patients have been well concerned.[2] Cancer-related fatigue (CRF) is one of the most common and distressing symptoms in anticancer therapy, which is also the most prominent residual or persistent symptom in cancer survivors.[3–5] The National Comprehensive Cancer Network defines CRF as a distressing, persistent, and subjective feeling of somatic, emotional, or cognitive fatigue or exhaustion that is inconsistent with recent activity levels, but related to the tumor or treatment of the tumor, and interferes with daily functioning.[6] Clinical manifestations of CRF include weakness, cognitive impairment, drowsiness, mood disturbances, and low energy.[7] Unlike the typical fatigue experienced by most people in the normal daily life, CRF cannot be relieved by rest or sleep.[8]
Up to 90% of cancer patients receiving antineoplastic therapy experience fatigue, and 27% to 82% of them remain fatigued after treatment.[9] The high incidence and chronicity of CRF can seriously affect patient care and quality of life.[10] The Guidelines for the Management of Cancer-Caused Fatigue published by the National Comprehensive Cancer Network recommend exercise therapy to manage fatigue symptoms in cancer patients.[11]
Traditional Chinese medicine (TCM) exercise therapy has been inherited and reformed with time, which is based on the holistic view of human life, and integrates TCM health preservation and care. The acceptable efficacy of TCM exercise therapy on strengthening the body and preventing diseases has been validated.[12] In recent years, TCM exercise therapy has exerted a significant role in CRF treatment, which has been widely and flexibly used in clinical practice, and served as an important tool for effective prevention of CRF.[13–17]
Valid evidences have confirmed the efficacy of multiple TCM exercise therapies on CRF in cancer patients.[18–21] However, it is unclear which one is optimal. In addition, different TCM exercise therapies have their own advantages and disadvantages. To our knowledge, a network meta-analysis (NMA) on comparing the effects of different TCM exercise therapies on CRF, anxiety, and sleep quality in cancer patients has not been reported. To promote the rational use of TCM exercise therapy and provide evidence-based basis, this study will conduct a NMA for analyzing randomized controlled trials (RCTs) reporting TCM exercise therapies on interfering CRF, anxiety and sleep quality in cancer patients.
2. Methods
2.1. Study registration
The protocol of this review was registered in OSF (OSF registration number: DOI 10.17605/OSF.IO/MJ8DA). This protocol was designed according to the guideline of Preferred Reporting Items for Systematic Review and Meta-analysis Protocols.[22] The findings of this study will be reported in line with the guideline of Preferred Reporting Items for Systematic Reviews and Network Meta-analysis.[23]
2.2. Inclusion criteria for study selection
2.2.1. Types of studies
RCTs reporting the efficacy of TCM exercise therapies on CRF, anxiety, and sleep quality in cancer patients.
2.2.2. Types of participants
The diagnosis of cancer was confirmed by pathological or cytological examination, and CRF was diagnosed based on the diagnostic criteria.[24] There will be no restriction on the gender, region, or race of participants.
2.2.3. Types of interventions
In the experimental group, patients will be treated with TCM exercise therapies, such as Tai Chi, Ba Duan Jin, the classics of tendon changing, Six Healing Sounds, and Wu Qin Xi; while those in the control group will receive standard management without exercise interventions.
2.2.4. Types of outcome indexes
-
i)
CRF: Pipers’ Fatigue Scale, Multidimensional Fatigue Symptom Inventory, and Cancer Fatigue Scale scores;
-
ii)
Anxiety: Self-rating Anxiety Scale and Hamilton Anxiety Scale scores;
-
iii)
Sleep: Pittsburgh sleep quality index.
2.3. Exclusion criteria
-
1)
Non-RCTs;
-
2)
Editorials, letters, reviews, etc;
-
3)
Duplicate publications;
-
4)
Absence of complete data or full-text.
2.4. Data sources
RCTs reporting TCM exercise therapies for CRF, anxiety, and sleep quality in cancer patients published before October 2021 will be systematically searched in the PubMed, Web of Science, Scopus, Cochrane Library, Embase, China Scientific Journal Database, China National Knowledge Infrastructure, Chinese Biomedical Literature Database, and Wanfang. Searching strategy in the Pubmed was depicted in Table 1. The appropriate combination of MeSH terms, free words, and keywords will be searched in online databases.
Table 1.
Search strategy in PubMed database.
| Number | Search terms |
| #1 | Neoplasms[MeSH] |
| #2 | Cancer[Title/Abstract] |
| #3 | Tumors[Title/Abstract] |
| #4 | Benign neoplasms[Title/Abstract] |
| #5 | Neoplasia[Title/Abstract] |
| #6 | Neoplasm[Title/Abstract] |
| #7 | Neoplasms, benign[Title/Abstract] |
| #8 | Benign neoplasm[Title/Abstract] |
| #9 | Cancers[Title/Abstract] |
| #10 | Neoplasm, benign[Title/Abstract] |
| #11 | Tumor[Title/Abstract] |
| #12 | OR/1 to 11 |
| #13 | Exercise therapy[MeSH] |
| #14 | Therapy, exercise[Title/Abstract] |
| #15 | Exercise therapies[Title/Abstract] |
| #16 | Therapies, exercise[Title/Abstract] |
| #17 | Tai Ji[MeSH] |
| #18 | T’ai Chi[Title/Abstract] |
| #19 | Tai Chi[Title/Abstract] |
| #20 | Tai Ji Quan[Title/Abstract] |
| #21 | Tai-ji[Title/Abstract] |
| #22 | Taiji[Title/Abstract] |
| #23 | Taijiquan[Title/Abstract] |
| #24 | Tai Chi Chuan[Title/Abstract] |
| #25 | Chi, Tai[Title/Abstract] |
| #26 | Ji Quan, Tai[Title/Abstract] |
| #27 | Quan, Tai Ji[Title/Abstract] |
| #28 | Traditional Chinese medicine exercise therapy[Title/Abstract] |
| #29 | Ba Duan Jin[Title/Abstract] |
| #30 | Classics of tendon changing[Title/Abstract] |
| #31 | Six Healing Sounds[Title/Abstract] |
| #32 | Wu Qin Xi[Title/Abstract] |
| #33 | Qi Gong[Title/Abstract] |
| #34 | Liu Zi Jue[Title/Abstract] |
| #35 | OR/13-34 |
| #36 | Randomized controlled trials as topic[MeSH] |
| #37 | Clinical trials, randomized[Title/Abstract] |
| #38 | Controlled clinical trials, randomized[Title/Abstract] |
| #39 | Trials, randomized clinical[Title/Abstract] |
| #40 | Random∗[Title/Abstract] |
| #41 | OR/36 to 40 |
| #42 | #12 AND #35 AND #41 |
2.5. Data collection and analysis
2.5.1. Data extraction and management
EndNote X9 software will be used to exclude duplicate title information, merge the same literatures from different databases, create a database involving eligible RCTs and downloads their full text. Data extraction will be carried out independently by 2 researchers and cross-checked for review using a predeveloped form.
The following data will be extracted: basic information, including the first author, journal and year of publication, and title; RCT information in experimental and control group, including case number of each group and total number, age, intervention, duration of treatment, and outcome indicators; quality evaluation of the included literature; and outcome indicators.
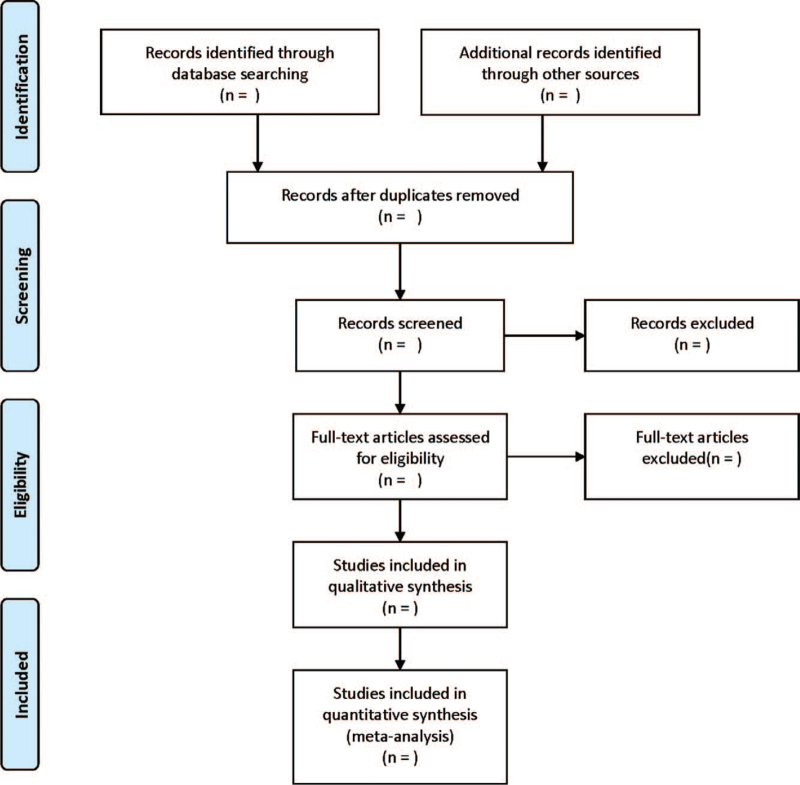
The flow chart for literature screening was presented in Figure 1.
Figure 1.
Flow diagram of study selection process.
2.5.2. Assessment of risk of bias
The methodological quality of included RCTs will be evaluated according to the Cochrane Risk of Bias Assessment Tool.[25] The evaluation indicators will include the randomization method, allocation concealment, blinding, completeness of outcome data, selective reporting, number of dislodged cases, follow-up, and other biases. Each item will be subdivided into high risk, low risk, and uncertain risk. Based on the description of the above aspects by the included RCTs, 3 investigators will be responsible for determining and evaluating the methodological quality.
2.5.3. Measures of therapeutic effect
The effect size of continuous variable data will be calculated with the standardized mean difference and corresponding 95% confidence intervals (CIs).
2.5.4. Management of missing data
In case of any missing data in relevant study, the original data will be requested by E-mail; otherwise, they will be excluded from this study.
2.5.5. Assessment of heterogeneity and data synthesis
STATA 14.0 software (STATA Corporation, College Station, TX) will be used to perform the pairwise meta-analysis and NMA. Chi-square test will be performed to measure the heterogeneity among the direct comparison results, and I2 will be conducted to measure the heterogeneity. If there is no heterogeneity (I2 < 50%, P > .1), a fixed-effects model will be adopted in the meta-analysis; otherwise, a random-effects model will be adopted.[26] The STATA 14 software will be used to draw a network diagram to visually present the comparisons between all therapies.
The inconsistency factor and corresponding 95% CI will be calculated to evaluate the consistency of each closed loop. The value of 95% CI of the inconsistency factor value at 0 will indicate the consistency between direct and indirect comparative evidence, as well as the closure loop; otherwise, the closure loop will be considered inconsistency. After comparing multiple exercise interventions, the pooled surface under the cumulative ranking curve will be calculated for each intervention, and they will be ranked according to surface under the cumulative ranking curve.
2.5.6. Assessment of reporting biases
Comparison-adjusted funnel plots will be plotted to analyze the existence of publication bias if 10 or more pieces of literature are included in this meta-analysis.[27]
2.5.7. Subgroup analysis
Subgroup analysis will be performed based on the timing of the intervention.
2.5.8. Sensitivity analysis
Sensitivity analysis will be performed by a one-by-one elimination method to verify the robustness of the results.
2.5.9. Grading the quality of evidence
The evidence quality will be independently evaluated by 2 reviewers using the Grading of Recommendations Assessment, Development and Evaluation, which classifies the quality of evidence as high, medium, low, and very low.[28]
2.5.10. Ethics and dissemination
The contents of this paper do not involve moral approval or ethical review and will be presented in print or at relevant conferences.
3. Discussion
CRF is a persistent, subjective exertional feeling in physiological, emotional or cognitive aspects related to tumor or tumor treatment, which is characterized by rapid development, heavy degree, high energy consumption and long duration, etc.[29,30] It is a common clinical symptom in cancer patients, with an incidence rate as high as 96.5% and a degree of moderate to severe, which seriously affects patients’ quality of life.[31] TCM exercise therapies are functional in strengthening the body and relaxing the mind, which is of significance in promoting cancer recovery. However, their specific efficacy on CRF, anxiety and sleep quality in cancer patients has not been compared. NMA is able to quantify and analyze different interventions for treating the same disease, while ranking all intervention strategies to determine the best intervention. This study will summarize and rank the effects of different TCM exercise therapies on CRF, anxiety, and sleep quality in cancer patients by comparing them through NMA, thus providing a reference for determining the optimal one.
Author contributions
Conceptualization: Xianfeng Du, Lihao Jiang.
Data curation: Lihao Jiang.
Funding acquisition: Xianfeng Du.
Investigation: Ju Ouyang.
Methodology: Ju Ouyang.
Project administration: Xianfeng Du.
Supervision: Xianfeng Du.
Validation: Ju Ouyang.
Visualization: Ju Ouyang.
Writing – original draft: Xianfeng Du, Lihao Jiang.
Writing – review & editing: Xianfeng Du, Lihao Jiang.
Footnotes
Abbreviations: CIs = confidence intervals, CRF = cancer-related fatigue, NMA = network meta-analysis, RCTs = randomized controlled trials, TCM = traditional Chinese medicine.
How to cite this article: Jiang L, Ouyang J, Du X. Effects of traditional Chinese medicine exercise therapy on cancer-related fatigue, anxiety and sleep quality in cancer patients: a protocol for systematic review and network meta-analysis. Medicine. 2021;100:44(e27681).
This work is supported by the Dazu Science and Technology Bureau (DZKJ, 2021ACC1008).
Patient consent is not required.
Ethics is not required.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Sengupta R, Honey K. AACR cancer progress report 2019: transforming lives through innovative cancer science. Clin Cancer Res 2019;25:5431. [DOI] [PubMed] [Google Scholar]
- [2].Travier N, Velthuis MJ, Steins Bisschop CN, et al. Effects of an 18-week exercise programme started early during breast cancer treatment: a randomised controlled trial. BMC Med 2015;13:121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Bower JE. Cancer-related fatigue–mechanisms, risk factors, and treatments. Nat Rev Clin Oncol 2014;11:597–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Al-Majid S, Wilson LD, Rakovski C, Coburn JW. Effects of exercise on biobehavioral outcomes of fatigue during cancer treatment: results of a feasibility study. Biol Res Nurs 2015;17:40–8. [DOI] [PubMed] [Google Scholar]
- [5].Garland SN, Roscoe JA, Heckler CE, et al. Effects of armodafinil and cognitive behavior therapy for insomnia on sleep continuity and daytime sleepiness in cancer survivors. Sleep Med 2016;20:18–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Bower JE, Bak K, Berger A, et al. Screening, assessment, and management of fatigue in adult survivors of cancer: an American Society of Clinical oncology clinical practice guideline adaptation. J Clin Oncol 2014;32:1840–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Pearson EJM, Morris ME, McKinstry CE. Cancer related fatigue: implementing guidelines for optimal management. BMC Health Serv Res 2017;17:496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Pearson EJ, Morris ME, McKinstry CE. Cancer-related fatigue: appraising evidence-based guidelines for screening, assessment and management. Support Care Cancer 2016;24:3935–42. [DOI] [PubMed] [Google Scholar]
- [9].Wu HS, Harden JK. Symptom burden and quality of life in survivorship: a review of the literature. Cancer Nurs 2015;38:E29–54. [DOI] [PubMed] [Google Scholar]
- [10].Ebede CC, Jang Y, Escalante CP. Cancer-related fatigue in cancer survivorship. Med Clin North Am 2017;101:1085–97. [DOI] [PubMed] [Google Scholar]
- [11].Mock V, Atkinson A, Barsevick A, et al. NCCN practice guidelines for cancer-related fatigue. Oncology (Williston Park, NY) 2000;14:151–61. [PubMed] [Google Scholar]
- [12].Yu Y. network meta-analysis of four kinds of traditional Chinese fitness exercises in the treatment of osteoporosis in the elderly. China Sport Sci Technol 2020;56:37–43. [Google Scholar]
- [13].Zhang LL, Wang SZ, Chen HL, Yuan AZ. Tai Chi exercise for cancer-related fatigue in patients with lung cancer undergoing chemotherapy: a randomized controlled trial. J Pain Symptom Manage 2016;51:504–11. [DOI] [PubMed] [Google Scholar]
- [14].Burschka JM, Keune PM, Oy UH, Oschmann P, Kuhn P. Mindfulness-based interventions in multiple sclerosis: beneficial effects of Tai Chi on balance, coordination, fatigue and depression. BMC Neurol 2014;14:165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Lu Y, Qu HQ, Chen FY, et al. Effect of Baduanjin Qigong exercise on cancer-related fatigue in patients with colorectal cancer undergoing chemotherapy: a randomized controlled trial. Oncol Res Treat 2019;42:431–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Zhou W, Wan YH, Chen Q, Qiu YR, Luo XM. Effects of Tai Chi exercise on cancer-related fatigue in patients with nasopharyngeal carcinoma undergoing chemoradiotherapy: a randomized controlled trial. J Pain Symptom Manage 2018;55:737–44. [DOI] [PubMed] [Google Scholar]
- [17].Xiu M. Study on influence of Baduanjin exercise on cancer chemotherapy patients with cancer-related fatigue. Chin Gen Pract Nurs 2015;13:3012–4. [Google Scholar]
- [18].Larkey LK, Roe DJ, Weihs KL, et al. Randomized controlled trial of Qigong/Tai Chi easy on cancer-related fatigue in breast cancer survivors. Ann Behav Med 2015;49:165–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].McQuade JL, Prinsloo S, Chang DZ, et al. Qigong/tai chi for sleep and fatigue in prostate cancer patients undergoing radiotherapy: a randomized controlled trial. Psycho Oncol 2017;26:1936–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Huang Y, Wang C, Qiu L, Shang L. Influence of eight-section brocade on the quality of life of chemotherapy patients after breast cancer radical mastectomy. Int J Nurs Stud 2017;92:1591–4. [Google Scholar]
- [21].Ying W, Min QW, Lei T, Na ZX, Li L, Jing L. The health effects of Baduanjin exercise (a type of Qigong exercise) in breast cancer survivors: a randomized, controlled, single-blinded trial. Eur J Oncol Nurs 2019;39:90–7. [DOI] [PubMed] [Google Scholar]
- [22].Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ (Clin Res ed) 2015;350:g7647. [DOI] [PubMed] [Google Scholar]
- [23].Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med 2015;162:777–84. [DOI] [PubMed] [Google Scholar]
- [24].Portenoy RK, Itri LM. Cancer-related fatigue: guidelines for evaluation and management. Oncologist 1999;4:01–10. [PubMed] [Google Scholar]
- [25].Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ (Clin Res ed) 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].von Hippel PT. The heterogeneity statistic I(2) can be biased in small meta-analyses. BMC Med Res Methodol 2015;15:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Contour-enhanced meta-analysis funnel plots help distinguish publication bias from other causes of asymmetry. J Clin Epidemiol 2008;61:991–6. [DOI] [PubMed] [Google Scholar]
- [28].Xiao Z, Wang C, Zhou M, et al. Clinical efficacy and safety of Aidi injection plus paclitaxel-based chemotherapy for advanced non-small cell lung cancer: a meta-analysis of 31 randomized controlled trials following the PRISMA guidelines. J Ethnopharmacol 2019;228:110–22. [DOI] [PubMed] [Google Scholar]
- [29].Wang XS, Zhao F, Fisch MJ, et al. Prevalence and characteristics of moderate to severe fatigue: a multicenter study in cancer patients and survivors. Cancer 2014;120:425–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Muthanna FMS, Karuppannan M, Hassan BAR, Mohammed AH. Impact of fatigue on quality of life among breast cancer patients receiving chemotherapy. Osong Public Health Res Perspect 2021;12:115–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Xu H, Jiang L, Yin Z, Jin Y, Li P, Tu H. Investigation on cancer-related fatigue of lung cancer patients receiving chemotherapy. Chin J Nurs 2010;45:332–5. [Google Scholar]