Abstract
Background:
Controversy exists regarding the use of titanium and stainless steel implants in fracture surgery. To our knowledge, no recent, comprehensive review on this topic has been reported.
Purpose:
To perform a systematic review of the evidence in the current literature comparing differences between titanium and stainless steel implants for fracture fixation.
Methods:
A systematic review of original research articles was performed through the PubMed database using PRISMA guidelines. Inclusion criteria were English-language studies comparing titanium and stainless steel implants in orthopaedic surgery, and outcome data were extracted.
Results:
The search returned 938 studies, with 37 studies meeting our criteria. There were 12 clinical research articles performed using human subjects, 11 animal studies, and 14 biomechanical studies. Clinical studies of the distal femur showed the stainless steel cohorts had significantly decreased callus formation and an increased odds radio (OR 6.3, 2.7-15.1; P < .001) of nonunion when compared with the titanium plate cohorts. In the distal radius, 3 clinical trials showed no implant failures in either group, and no difference in incidence of plate removal, or functional outcome. Three clinical studies showed a slightly increased odds ratio of locking screw breakage with stainless steel intramedullary nails compared with titanium intramedullary nails (OR 1.52, CI 1.1-2.13).
Conclusion:
Stainless steel implants have equal or superior biomechanical properties when compared with titanium implants. However, there is clinical evidence that titanium plates have a lower rate of failure and fewer complications than similar stainless steel implants in some situations. Although our review supports the use of titanium implants in these clinical scenarios, we emphasize that further prospective, comparative clinical studies are required before the conclusions can be made.
Keywords: clinical evidence, fracture fixation, stainless steel, titanium
1. Introduction
The use of metal implants for fracture fixation has allowed providers to maintain anatomic alignment and begin earlier rehabilitation, enhancing functional outcome. Early problems encountered with metal implants included corrosion, insufficient material strength, and breakage. This led investigators to develop new implants with characteristics that could withstand the physical and physiological stresses of internal fixation of fractures.
A desirable implant must have the following characteristics: ductility, strength, stiffness, and biocompatibility. Titanium and stainless steel implants differ in each of these categories, theoretically making them more desirable for different functions or in different anatomic locations. Ductile materials are capable of extreme plastic deformation and energy absorption before fracture. Once implanted, materials are subjected to cyclic forces applied in the axial, flexural, or torsional direction, causing material fatigue. This may cause failure of the implant at loads considerably lower than the tensile or yield strengths of the material under static load.
Stainless steel alloys are significantly stiffer than bone and have traditionally proven to be durable enough to allow healing.[1] In addition, stainless steel is relatively inexpensive and biologically well tolerated, much in part to the smooth surface from electropolishing.[2] It also has the advantage of being ductile enough to allow contouring of the plate without fracture. Electro-polished stainless steel overall has an excellent clinical track record in most fracture types and anatomic locations; however, questions have arisen regarding whether it may be too stiff to allow for fracture healing in some anatomic locations or fracture types, such as the distal femur.[3,4]
Titanium, on the other hand, more closely matches the modulus of elasticity of bone. This flexibility may be more conducive to fracture healing in areas where more strain is required for a healing response to develop. Additionally, titanium alloy is more resistant to cyclic load and notch sensitivity.[5] Titanium has a good clinical track record when used in internal fixation devices for fractures. Previous issues of “cold-welding” of screws to plates when commercially pure titanium was used have been essentially eliminated with the introduction of titanium alloys.[5] The use of titanium has been limited by regional surgeon preference and increased cost compared with electro-polished stainless steel, although these barriers are decreasing.
Comparing the advantages and disadvantages of the mechanical properties of each metal does not lead to an obvious conclusion about which is better for fracture fixation. It may be that neither metal is universally superior to the other, but that each has properties that may make it superior to the other in specific anatomic locations. In addition, the strength and durability of the construct also depends significantly on the number, type (i.e., locking versus nonlocking, uni- versus bi-cortical), and composition/position of the screws used. The purpose of this review, recognizing the limited quality of the available literature, is to summarize studies directly comparing stainless steel and titanium implants in specific regions of the body to determine which metal, if either, performs best in that anatomic region.
2. Methods
Ethics approval was not required for this review.
A systematic review of original research articles was performed through the PubMed database for the years 1970 to 2019 inclusive. PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines were followed. The search term was designed to include all articles comparing titanium and stainless steel implants in orthopaedic surgery. Only studies investigating plate and screw or intramedullary nail fixation were included. Levels of evidence I through IV were included in the study. Articles not available in the English language were excluded. Human, animal, and biomechanical studies were included. In vivo and in vitro studies were included and no discretion was made with regard to outcome.
Exclusion criteria for the study were all studies not relating to orthopaedic surgery, such as dental, orthodontic, and neurosurgical studies. Non-English language studies, surgical technique articles, letters to the editor, systematic reviews, meta-analyses, duplicate subject populations, case studies, and expert reviews were not included in the study. Orthopaedic surgery subspecialties of arthroplasty, spine, and pediatrics were excluded.
Both electronic and print published articles were accepted for inclusion. Meeting abstracts and proceedings were not included. Inclusion and exclusion criteria were determined by the title and abstract. If there was uncertainty of whether the article met inclusion criteria, the full article was reviewed to determine if it should be included.
Outcome data, such as union rate, complications, evidence of biological reaction, and other relevant information, were extracted from included investigations and described qualitatively. Due to the heterogeneity of the studies, quantitative analysis of data from studies was not performed, and no specific statistical analyses were performed of the data from the studies.
3. Results
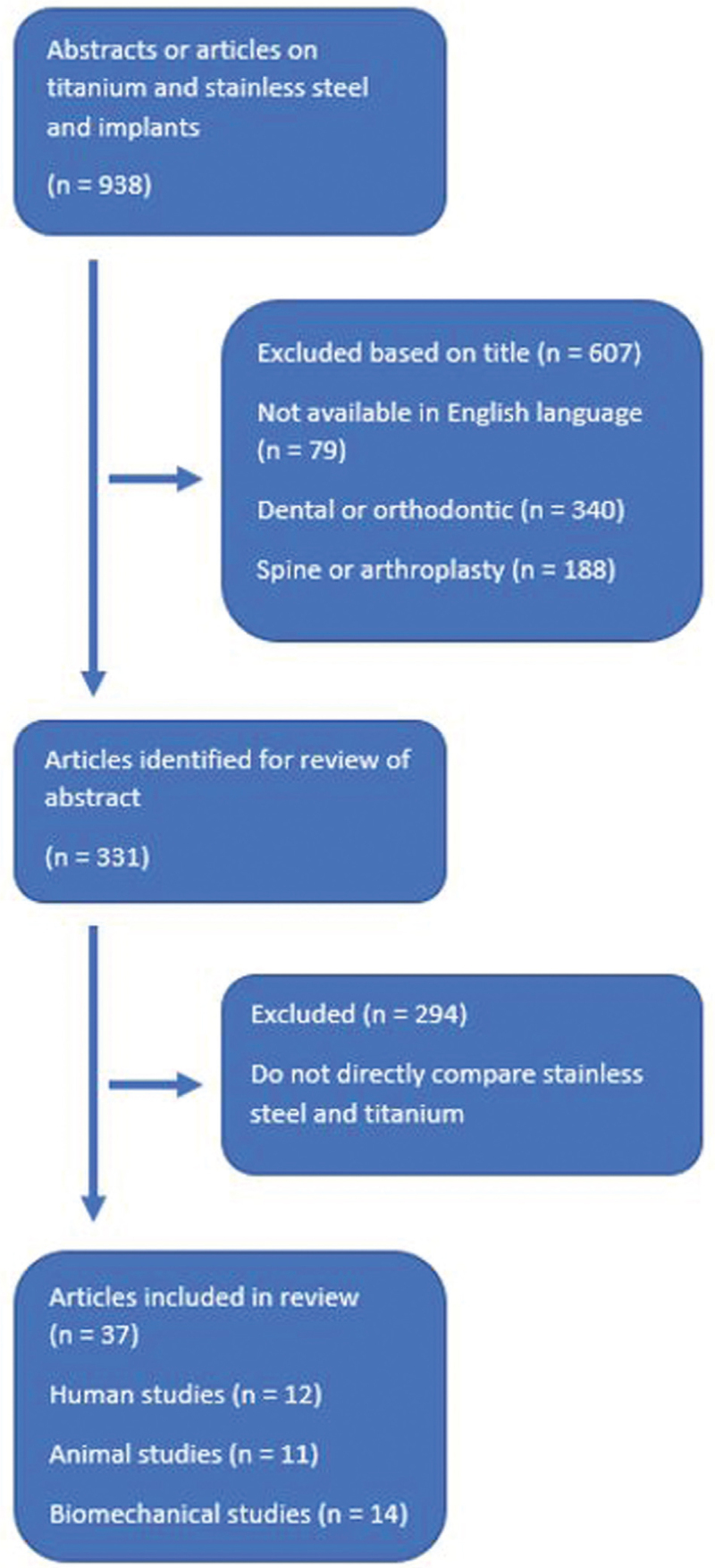
The search identified 938 studies, with 37 studies meeting inclusion and exclusion criteria (Fig. 1). Seventy-nine studies were not available in the English language. Of the remaining 859 studies, 340 did not include orthopaedic surgery implants. Of the remaining 519 studies, 188 were implants used in spine or arthroplasty. Three hundred thirty-one articles remained, of which 294 studies did not directly compare titanium to stainless steel. This left 37 articles to be accepted into the study (femur-14, radius/hand-9, tibia-8, foot/ankle-5, clavicle-1).
Figure 1.
Schematic of studies included in this review.
3.1. Clavicle
There were no clinical or animal studies done comparing titanium to stainless steel fracture fixation.
Biomechanical: Goswami et al[6] compared paired cadaver specimens to test plate strength across artificially created clavicle osteotomies. Each construct was tested on a material testing apparatus with regard to axial tension and compression and torsional strength in compression and tension.[6] They showed that there was no difference between a precontoured titanium plate and a 3.5 mm stainless steel low-contact dynamic compression plate when tested in axial tension, axial compression, torsional tension, and torsional compression.
3.2. Radius
A total of 9 studies focused on the radius, with 6 specifically investigating distal radius fixation. Three of the studies were clinical studies with a total of 134 patients. There were also 2 cadaver studies and 2 animal studies.
Biomechanical: The majority of studies focused on mechanical measures including strength to failure and plate stiffness. Interestingly, increased implant stiffness did not necessarily lead to increased construct strength. Jain et al[7] compared strength and deformation when plating dog radii with and without bone defects spanned by titanium or stainless steel plates. They found similar torsional and bending stiffness when no bone defect was present. When a gap was presents, stainless steel resisted bending more than titanium, but overall strength to failure was not different.[7]
Animal: Several studies have investigated the effect of plate material on the adjacent soft tissues. In a study by Sinicropi et al[8], 18 dogs had distal radius fracture repairs using titanium or stainless steel plates. At 4 months, histological analysis of tendons showed a higher amount of inflammation in the titanium group than in the stainless steel group.[8] Two other studies, 1 in dogs and 1 in rabbits, found no difference in the effect of plate material on tendon inflammation over a similar time frame.[9,10] Unfortunately, there are no human clinical trials specifically evaluating the differences of the effect of plate composition on tendon inflammation and function. Additionally, the animal studies were performed using dorsal plating where an increased incidence of soft-tissue irritation is well recognized: studies are limited evaluating the effect of plate material on soft tissue and tendon irritation using the more common volar plating technique.
Clinical: When fixing distal radius fractures in cadaver specimens with fixed angle stainless steel or titanium plates, stiffness and load to failure were similar between the 2 groups; however, the titanium plates were found to have greater translational and rotational displacement than the stainless steel plates.[11] In another biomechanical study using cadavers, no difference was found in fracture displacement after cyclic loading.[12] Despite the variation seen in biomechanical studies, the clinical studies had no evidence of mechanical failure or nonunion/malunion.[13–15] Plate failure or breakage in distal radial fracture fixation is exceedingly rare, with no instances of this complication in the multiple series reviewed.
When comparing complications after distal radial fracture fixation, the most common complications were soft tissue in nature, including tenosynovitis or tendon rupture, complex regional pain syndrome, and carpal tunnel syndrome. In a randomized trial comparing titanium and stainless steel plating of distal radius fractures, Shakir et al[14] compared the incidence of complications and reoperations 5 years after fixation. In their series of 63 patients, 7 total plates were removed (11%). Four of the plates were titanium and 3 were stainless steel. A significant difference was not detected in rate of plate removal based on metal, nor was there a difference in the soft-tissue complication rates between the 2 groups.[14] Rozental et al[13] also did not detect a significant difference based on plate composition in complication or plate removal in a retrospective review of distal radius fractures.
Three studies examined clinical outcome, including range of motion and functional outcome measures, following plate fixation of distal radial fractures. Souer et al[15] conducted a retrospective analysis of 24 patients treated for distal radius fractures with either a titanium or stainless steel volar locking plate. They recorded functional and patient-reported outcomes at 6, 12, and 24 months of follow-up. No significant difference in wrist function was found in patients of either group. There was no significant difference detected in range of motion, grip strength, pain, Disabilities of the Arm, Hand, and Shoulder score, and Gartland and Werley score.[15] Similar results were found in the Rozental study with no significant difference in Disabilities of the Arm, Hand, and Shoulder score and Gartland and Werley scoring systems.[13]
3.3. Hand
There were no comparative animal or clinical studies in the hand.
Biomechanical: Damron et al[16] examined fixation of proximal phalanx fractures in a cadaveric hand model. They created an osteotomy in the diaphysis of a proximal phalanx and fixed it with either a titanium or stainless steel implant. In this study, titanium plated phalanges were the stiffest construct and absorbed more load to failure than the phalanges plated with stainless steel implants.
3.4. Femur
Studies examining the femur were generally divided into proximal femur/femoral neck fixation, diaphyseal fixation, and supracondylar fixation. Three studies were clinical in nature, 3 were animal studies, and 8 were biomechanical studies.
Biomechanical: Two biomechanical studies were conducted looking at proximal femur fixation. Gok et al[17] conducted a finite element analysis comparing different types of cannulated screws and the forces they experienced during physiologic loading. They concluded that titanium was advantageous compared with stainless steel because it created minimum stress at the upper and lower proximity of the fracture line.[17] Another finite element analysis was performed by Taheri et al.[18] They concluded that a sliding hip screw (SHS) generated greater stresses within the implanted femur compared with the intact femur. The stainless steel SHS was subjected to greater stresses than the titanium SHS, suggesting that if the goal was to minimize stress, titanium may be a superior material for this type of implant.
Several investigations were performed regarding intramedullary (IM) fixation of femoral shaft fractures and properties of the IM nail and interlocking screws. Gabarre et al[19] performed 2 finite element analyses looking at nail material, fracture gap size, and screw configuration. In both of their analyses, they showed higher mobility when using titanium, with increased motion at the fracture site, creating higher rates of strain at the fracture site compared with the stainless steel nail.[19,20] They also did a clinical follow-up of patients undergoing fixation of femoral shaft fractures with intramedullary nails, but made no mention of nail material.[19] Chantarapanich also studied interlocking screws, and compared bending strength of titanium and stainless steel.[21] The titanium screws had a significantly lower bending resistance at 1413 N compared with stainless steel screws at 2071 N. Based on their results, they recommend stainless steel interlocking screws if maintenance of reduction is dependent on interlocking screws maintaining their integrity.[22]
Beingessner and Kandemir looked at the difference in plate stiffness between stainless steel and titanium in sawbones models of distal femoral fractures. They found no difference in deformation of the plate[23] or mode of failure.[24] Both studies showed some increased stiffness in the stainless steel plate constructs compared with the titanium plate constructs, but the authors felt the differences were small and should not be used in decision making regarding the choice of implant material.
Animal: Uhthoff looked at biomechanical characteristics of bone after plating in animal models. In this study, plates were applied to Beagle femurs with and without osteotomies. Plates were removed at different time points before the animals were sacrificed and bones removed. Radiographic and histologic studies of the bones were performed. Under both plates, bone thickness decreased, but titanium plates had less reduction in cortical thickness (6% vs 19%), less bone loss (3.7 vs 11.0%), and a greater increase in cortical thickness 16 weeks after removal of the plate (69% vs 30%) compared with their stainless steel counterparts. These differences were statistically significant.[25] In the second study, osteotomized femorae that were plated had marked periosteal callus and ill-defined margins of cortices, with decreased density when examined histologically. In the titanium group at 32 weeks following removal of the plate, the bone returned to normal shape and thickness faster and to a greater degree than the stainless steel plated bones.[26] Seligson et al[27] also looked at the strength of the bone in an animal osteotomy model and confirmed that strength of the bone after removal was higher for titanium plated bones than the stainless steel plated bones.
Clinical: Lujan et al[3] performed a retrospective cohort study of 64 distal femur fractures fixed with periarticular locking plates. Custom computer software was used to look at the development and extent of the callus formation on plain radiographs. Their hypothesis was that titanium would allow for more interfragmentary strain and better callus formation. Their results showed titanium plated fractures had 76% more callus at week 6 postoperatively and 71% more at week 12 compared with stainless steel plated fractures. At the final evaluation of the study at week 24 postoperatively, deficient callus formation was present in 26% of titanium plate constructs and 49% of stainless steel constructs.
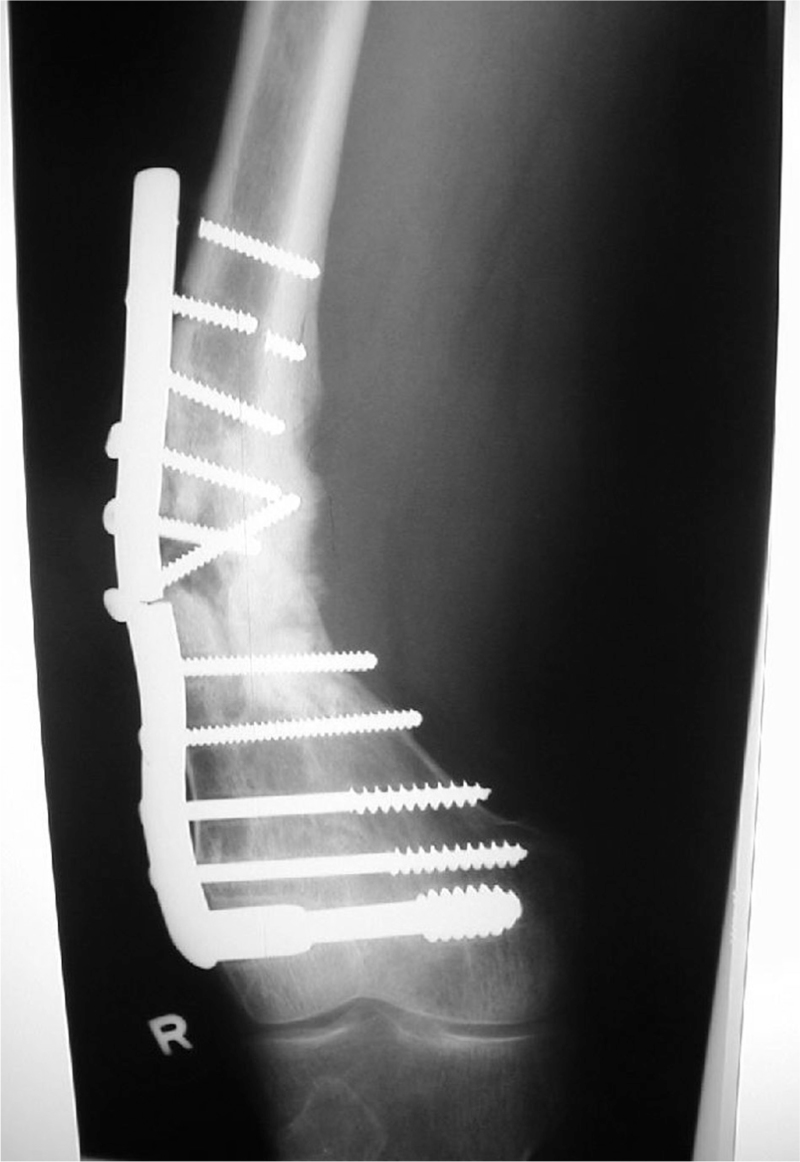
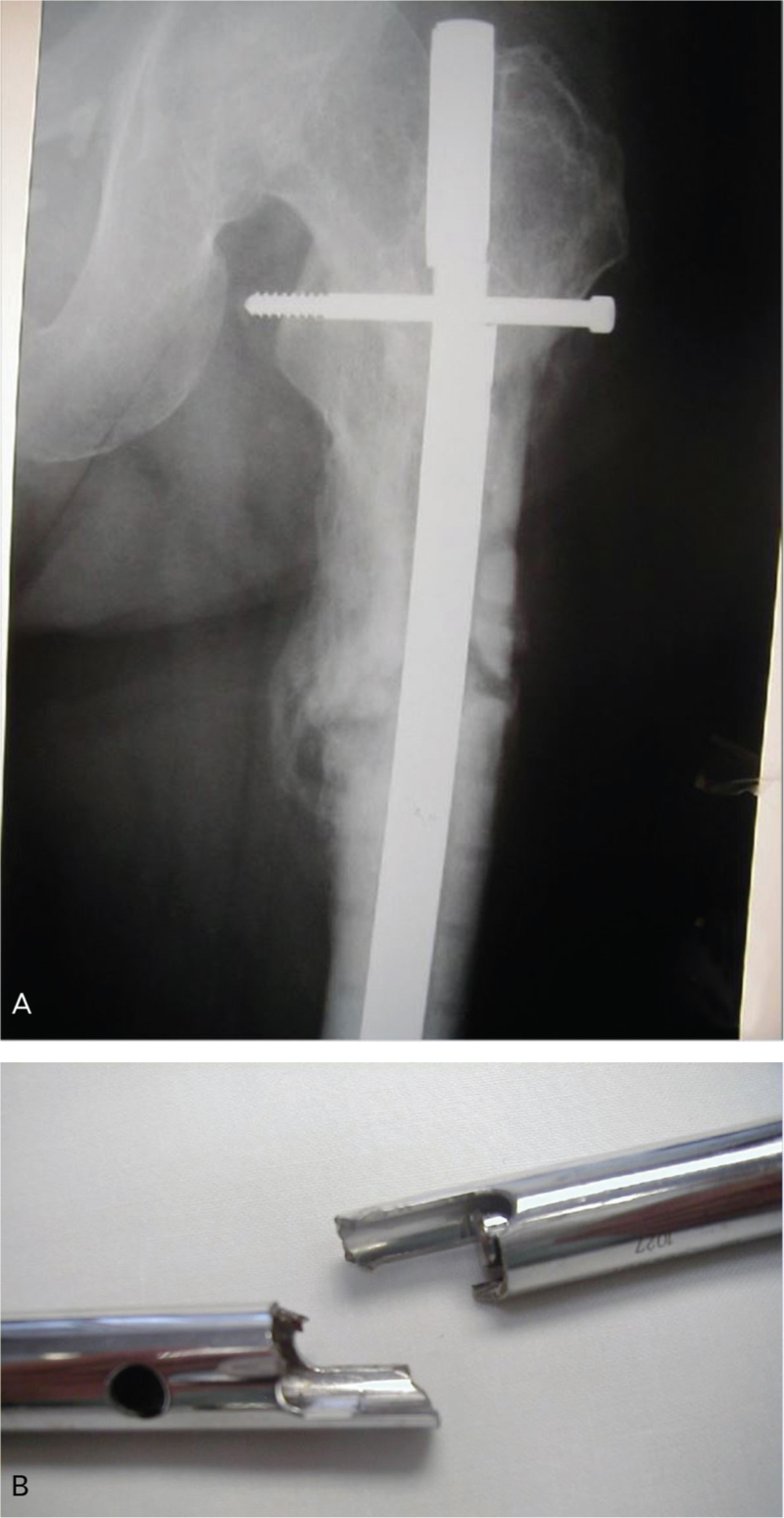
Rodriguez et al[28] published a large retrospective review of 283 patients who had undergone lateral locked plating for distal femur fractures, 28 of which were performed for nonunion. The authors used multivariable analysis to identify independent risk factors for nonunion. The odds ratio of nonunion for stainless steel was 6.3 with CI 2.7-15.1 (P < .001) compared with titanium plates (Figs. 2 and 3). Other significant factors identified were infection, open fracture, and obesity.[28]
Figure 2.
Fatigue failure of a stainless steel implant used for fixation of a comminuted distal femoral fracture in a 34-year-old male, 12 months postoperatively, with varus deformity and shortening.
Figure 3.
(A) A stainless steel antegrade femoral nail with fatigue failure of the nail through the proximal locking hole. (B) A close-up photograph of the fatigue failure of the nail.
The only clinical study regarding intramedullary fixation of femoral shaft fractures examined the rate of removal of hardware for pain or discomfort. Forty-five patients met inclusion criteria including 23 with a titanium nail and 22 with a stainless steel nail. In this series, the titanium nails tended to have more interlocking screws and took more operative time to be removed. However, there was no difference in time for nail removal when the number of interlocking screws was controlled for. Heterotopic ossification was present in both populations without a significant difference between groups.[29]
3.5. Tibia
Titanium and stainless steel have inherently different properties that may make them advantageous for achieving different outcomes in fracture fixation of the tibia. Several clinical studies have investigated the differences and similarities in devices made with these materials. There were no biomechanical or animal studies.
Clinical: In a large multicenter Study to Prospectively Evaluate Reamed Intramedullary Nails in Patients with Tibial Fractures, Schemitsch et al[30] looked at factors associated with increased risk of negative outcomes. With regard to intramedullary nail material, nails composed of stainless steel had increased overall risk of complication (primarily locking screw breakage) when compared with titanium (OR 1.52, CI 1.1-2.13). Of note, autodynamization (i.e., breakage of locking screws) of stainless steel nails was 10.1% compared with 2.3% with titanium nails, a statistically significant and clinically relevant difference. The investigators considered screw breakage as a “negative event” that could cause retained screws, temporary pain, or complicate revision surgery. When the investigators controlled for the autodynamization, stainless steel no longer was statistically significant as a predictor of complication (i.e., the majority of the additional complications seen in the stainless steel group were locking screw breakages).[30]
In cases of infection or hardware failure, surgical intervention is typically indicated. Similarly, elective nail removal for symptomatic hardware irritation is also recommended in certain situations. While in North America asymptomatic hardware is typically left in situ, in many countries routine removal of fracture implants is performed. In a retrospective study comparing 62 patients who underwent removal of an implanted tibial IM nail for hardware irritation (24 stainless steel and 38 titanium), the titanium nail group had 9 complications in 38 patients (24%) versus 3 in 24 patients (3%) in the stainless steel group (P = .44). The complications were predominantly screw breakages.[31] Operating time and the amount of intraoperative bleeding were significantly higher in the titanium group than the stainless steel group, which the authors postulated was due to greater bone contact and bone integration as suggested in previous animal studies.[31,32] This led to the authors of the study recommending against removal of titanium nails in asymptomatic patients.
Prior studies assessing the outcome associated with the removal of early titanium implants and designs described a high rate of complications such as cold-welding, screw breakage, and thread stripping.[33] More recent advances in both implant design and titanium alloy composition have minimized these complications and vastly improved the handling qualities of titanium implants during both insertion and removal (Fig. 4A and B).
Figure 4.
(A) A long titanium precontoured distal humeral plate was used to repair a complex distal humeral fracture in an 18-year-old male patient. (B) Due to local soft-tissue irritation and the patient's request, hardware removal was performed. The procedure was uncomplicated and took only 35 minutes. Modern titanium alloys have much better handling characteristics than older implants and cold-welding, screw breakage, and screw stripping are infrequent.
When comparing overall treatment outcomes, a study comprised of 256 cases of tibial shaft fractures showed no significant differences between groups treated by fixation with either titanium or stainless steel dynamic compression plates. Both groups had full return of function and adjacent joint movement in greater than 90% of cases with no significant differences between groups. Refracture occurred in both groups, but subsequent injury after fracture had a high rate of healing.[34]
3.6. Ankle
Biomechanical: One ankle study described a cadaveric model which compared 16 cadavers with syndesmosis injury fixed with either titanium or stainless steel screws, using 3 or 4 cortices. The specimens were subjected to a predetermined number of cycles simulating the weight bearing that would occur until healing in a typical clinical case. There was no incidence of hardware failure (including screw breakage) and no differences in syndesmotic widening attributable to screw material.[35]
Clinical: Ozkaya et al[36] reviewed metaphyseal distal tibia fractures fixed with distal locking plates. There was no significant difference in union or maintenance of reduction between groups treated with stainless steel versus titanium plates. Clinical outcomes measured with the American Orthopaedic Foot & Ankle Society (AOFAS) score were not different between groups. They concluded that similar results may be obtained by use of stainless steel or titanium plates.[36]
3.7. Foot
Three of 4 studies identified in the foot were comparative clinical studies, and 1 was biomechanical.
Biomechanical: Reese and DeVries both looked at fixation material in fractures of the base of the fifth meta-tarsal (Jones fractures). In a biomechanical study, Reese et al[37] found stainless steel screws were more resistant to fatigue than titanium screws.
Clinical: DeVries et al[38] examined outcomes of patients treated with cannulated screws for Jones fractures: 37 were treated with titanium screws and 16 with stainless steel screws. Radiographs were taken immediately post-operatively and 1, 2 , 4, and 6 weeks postoperatively. There was a longer time to union in the stainless steel screw group, although the complication rate was not statistically significantly different between the titanium and stainless steel groups. In the titanium group, there was one asymptomatic nonunion which did not go on to revision. In the stainless steel group, there were 2 nonunions that were scheduled to undergo revision surgery. There was no hardware failure or breakage in either group. Three titanium screws and no stainless steel screws were removed later secondary to hardware pain.[38]
Hunt et al[39] reported a large retrospective review investigating plate characteristics to outcomes in the fusion of metatarsophalangeal joint with either locking titanium plates versus nonlocking or conventional stainless steel screw constructs. They found a higher nonunion rate in the locked titanium plates, but it is unknown whether these differences are attributable to the plate composition or plate design. It is possible that the stiffer locking titanium construct performed less well due to the biomechanical characteristics of the locking construct in this setting as opposed to the nature of the material in the plate.[39]
4. Discussion
A number of comparative studies were identified in this systematic review, ranging from basic science studies to randomized clinical trials. There were a large number of comparative studies involving the distal radius, but none of them showed evidence of clinical superiority of 1 implant material over another. In plating of the distal femur or IM nailing of the tibial shaft, the results of the reviewed studies indicated potential advantages of titanium over stainless steel. In the other anatomic regions surveyed, the heterogeneity and lack of high-quality comparative studies made it difficult to determine which, if either, implant material was superior.
As has been noted before, different implant metallurgy may have advantages that make it more conducive to fracture healing and less prone to complications depending on the region involved. In distal radius fractures, the complication rate is low and nonunion is uncommon which makes it difficult to find a difference based on plate material. No clear difference in clinical or functional outcomes was shown in any of the studies. It is possible that these studies were underpowered (too few patients to demonstrate a small but true difference, a type II or beta-error), or that no real difference exists.
In the distal femur, basic science studies revealed an increase in callus formation in the titanium plate group compared with the stainless steel plate group, and less stress shielding in the titanium plate versus steel plate group.[25,26] This was consistent with a clinical study showing more callus formation in the titanium plate group.[3] The largest clinical study examining complications in this scenario found an increase in nonunion with stainless steel plate fixation versus titanium plates.[28] These results may be due to the beneficial effects of higher, but controlled, inter-fragmentary strain at the fracture site consistent with the more flexible nature of titanium.[40,41]
In the tibia group, biomechanical studies showed more changes consistent with stress shielding in the stainless steel group than in the titanium group. This is similar to the findings in the distal femur studies. In clinical studies of tibial nailing, the rate of interlocking screw breakage was higher in the stainless steel group compared with titanium.[30] As in the femoral scenario, the authors postulated that this is likely related to the increased amount of interfragmentary strain seen with titanium implants.
The major limitation of our study is the limited amount and quality of the data in the available literature. Of 37 identified manuscripts, there were only 12 comparative clinical studies that included both types of implants, and of those, only 1 was a prospective controlled trial. Retrospective studies and studies with low power are more prone to bias and type II or beta errors. Though this paucity of high-quality studies limits the ability of this review to make generalizable conclusions, it highlights the importance of performing studies to look at this question on a larger scale. Certainly with the data available it is clear that titanium implants provide clinical outcomes similar to, and in some circumstances superior to, their stainless steel counterparts. Another limitation of our review is that we were unable to identify comparative studies that examined other potential benefits of one material over the other such as cost, availability, or imaging compatibility. In the era of surgical cost-containment, implant cost is a critical factor for the operating surgeon to consider.
The heterogenous nature of the data did not allow for combining the results or performing quantitative measurements on pooled results. For examples, even in the distal radius, there was wide variability across the studies in type of surgical approach and plate position. Studies also used different primary and secondary endpoints as determinants of function that further complicate the potential for pooling or combining the results of each study. While most of the studies included mechanical properties of materials as well as complication rates, pain, and postsurgical functional outcomes, a broader variety of measures should be utilized to confidently select the appropriate plate material in a given scenario.[42] Lastly, as previously stated, the number, type, and composition of screws used in a plate are also very important as this may result in a construct that is too stiff, and lead to delayed or nonunion. This data was not consistently available in any of the studies we identified. Lastly, fracture healing is a complex interaction of biology and mechanics and the mechanical aspect includes not only the type of metal but the implant itself, locking versus nonlocking screw fixation, and pattern and dispersion of screws. Thus, we cannot expand our conclusions past a very limited assessment of specific implant composition and types for specific areas from what is available in the literature.
5. Conclusion
The results of this review support the use of titanium implants in certain clinical fracture scenarios. In clinical studies of fracture fixation in the distal femur and tibia, titanium implants had a lower rate of failure, and a lower rate of complications than stainless steel. In the use of IM nails for tibial shaft fractures, there is strong evidence that the rate of locking screw breakage is lower for nails and screws composed of titanium, as opposed to stainless steel. In other areas such as the clavicle, distal radius, ankle, and foot, comparative studies between the implants composed of the 2 materials are equivocal. Prior issues with the difficulty of removing titanium implants have diminished with the improved handling characteristics of modern titanium alloys. Larger, prospective, comparative studies are needed in these areas to clarify and define potential clinically relevant differences.
References
- 1.Marcomini JB, Baptista CA, Pascon JP, et al. Investigation of a fatigue failure in a stainless steel femoral plate. J Mech Behav Biomed Mater. 2014;38:52–58. [DOI] [PubMed] [Google Scholar]
- 2.Uhthoff HK, Poitras P, Backman DS. Internal plate fixation of fractures: short history and recent developments. J Orthop Sci. 2006;11:118–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lujan TJ, Henderson CE, Madey SM, et al. Locked plating of distal femur fractures leads to inconsistent and asymmetric callus formation. J Orthop Trauma. 2010;24:156–162. [DOI] [PubMed] [Google Scholar]
- 4.Chen YQ, Dai KR, Qiu SJ, et al. Bone remodelling after internal fixation with different stiffness plates: ultrastructural investigation. Chin Med J. 1994;107:766–770. [PubMed] [Google Scholar]
- 5.Disegi JA. Titanium alloys for fracture fixation implants. Injury. 2000;31 suppl 4:14–17. [DOI] [PubMed] [Google Scholar]
- 6.Goswami T, Markert RJ, Anderson CG, et al. Biomechanical evaluation of a pre-contoured clavicle plate. J Shoulder Elbow Surg. 2008;17:815–818. [DOI] [PubMed] [Google Scholar]
- 7.Jain R, Podworny N, Hearn T, et al. A biomechanical evaluation of different plates for fixation of canine radial osteotomies. J Trauma. 1998;44:193–197. [DOI] [PubMed] [Google Scholar]
- 8.Sinicropi SM, Su BW, Raia FJ, et al. The effects of implant composition on extensor tenosynovitis in a canine distal radius fracture model. J Hand Surg Am. 2005;30:300–307. [DOI] [PubMed] [Google Scholar]
- 9.Cohen MS, Turner TM, Urban RM. Effects of implant material and plate design on tendon function and morphology. Clin Orthop Relat Res. 2006;445:81–90. [DOI] [PubMed] [Google Scholar]
- 10.Nazzal A, Lozano-Calderón S, Jupiter JB, et al. A histologic analysis of the effects of stainless steel and titanium implants adjacent to tendons: an experimental rabbit study. J Hand Surg Am. 2006;31:1123–1130. [DOI] [PubMed] [Google Scholar]
- 11.Marshall T, Momaya A, Eberhardt A, et al. Biomechanical comparison of volar fixed-angle locking plates for ao c3 distal radius fractures: titanium versus stainless steel with compression. J Hand Surg Am. 2015;40:2032–2038. [DOI] [PubMed] [Google Scholar]
- 12.Osada D, Viegas SF, Shah MA, et al. Comparison of different distal radius dorsal and volar fracture fixation plates: a biomechanical study. J Hand Surg Am. 2003;28:94–104. [DOI] [PubMed] [Google Scholar]
- 13.Rozental TD, Beredjiklian PK, Bozentka DJ. Functional outcome and complications following two types of dorsal plating for unstable fractures of the distal part of the radius. J Bone Joint Surg Am. 2003;85-A:1956–1960. [DOI] [PubMed] [Google Scholar]
- 14.Shakir S, Naran S, Neral M, et al. Titanium versus stainless-steel plating in the surgical treatment of distal radius fractures: a randomized trial. J Hand Microsurg. 2016;8:155–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Souer JS, Ring D, Matschke S, et al. Comparison of functional outcome after volar plate fixation with 2.4-mm titanium versus 3.5-mm stainless-steel plate for extra-articular fracture of distal radius. J Hand Surg Am. 2010;35:398–405. [DOI] [PubMed] [Google Scholar]
- 16.Damron TA, Jebson PJ, Rao VK, et al. Biomechanical analysis of dorsal plate fixation in proximal phalangeal fractures. Ann Plast Surg. 1994;32:270–275. [DOI] [PubMed] [Google Scholar]
- 17.Gok K, Inal S, Gok A, et al. Comparison of effects of different screw materials in the triangle fixation of femoral neck fractures. J Mater Sci Mater Med. 2017;28:81. [DOI] [PubMed] [Google Scholar]
- 18.Taheri NS, Blicblau AS, Singh M. Comparative study of two materials for dynamic hip screw during fall and gait loading: titanium alloy and stainless steel. J Orthop Sci. 2011;16:805–813. [DOI] [PubMed] [Google Scholar]
- 19.Gabarre S, Albareda J, Gracia L, et al. Influence of gap size, screw configuration, and nail materials in the stability of anterograde reamed intramedullary nail in femoral transverse fractures. Injury. 2017;48 suppl 6:S40–S46. [DOI] [PubMed] [Google Scholar]
- 20.Gabarre S, Albareda J, Gracia L, et al. Influence of screw combination and nail materials in the stability of anterograde reamed intramedullary nail in distal femoral fractures. Injury. 2017;48 suppl 6:S47–S53. [DOI] [PubMed] [Google Scholar]
- 21.Chantarapanich N, Sitthiseripratip K, Mahaisavariya B, et al. Biomechanical performance of retrograde nail for supracondylar fractures stabilization. Med Biol Eng Comput. 2016;54:939–952. [DOI] [PubMed] [Google Scholar]
- 22.Karaarslan AA, Karakaşlı A, Aycan H, et al. Biomechanical comparison of three-point bending resistance of titanium and stainless steel locking screws in intramedullary nails. Eklem Hastalik Cerrahisi. 2015;26:145–150. [DOI] [PubMed] [Google Scholar]
- 23.Beingessner D, Moon E, Barei D, et al. Biomechanical analysis of the less invasive stabilization system for mechanically unstable fractures of the distal femur: comparison of titanium versus stainless steel and bicortical versus unicortical fixation. J Trauma. 2011;71:620–624. [DOI] [PubMed] [Google Scholar]
- 24.Kandemir U, Augat P, Konowalczyk S, et al. Type of fixation at the shaft, and position of plate modify biomechanics of distal femur plate osteosynthesis. J Orthop Trauma. 2017;31:e241–e246. [DOI] [PubMed] [Google Scholar]
- 25.Uhthoff HK, Bardos DI, Liskova-Kiar M. The advantages of titanium alloy over stainless steel plates for the internal fixation of fractures. An experimental study in dogs. J Bone Joint Surg Br. 1981;63-B:427–484. [DOI] [PubMed] [Google Scholar]
- 26.Uhthoff HK, Finnegan M. The effects of metal plates on post-traumatic remodelling and bone mass. J Bone Joint Surg Br. 1983;65:66–71. [DOI] [PubMed] [Google Scholar]
- 27.Seligson D, Mehta S, Mishra AK, et al. In vivo study of stainless steel and Ti-13Nb-13Zr bone plates in a sheep model. Clin Orthop Relat Res. 1997;213–223. [PubMed] [Google Scholar]
- 28.Rodriguez EK, Boulton C, Weaver MJ, et al. Predictive factors of distal femoral fracture nonunion after lateral locked plating: a retrospective multicenter case-control study of 283 fractures. Injury. 2014;45:554–559. [DOI] [PubMed] [Google Scholar]
- 29.Husain A, Pollak AN, Moehring HD, et al. Removal of intramedullary nails from the femur: a review of 45 cases. J Orthop Trauma. 1996;10:560–562. [DOI] [PubMed] [Google Scholar]
- 30.Schemitsch EH, Bhandari M, Guyatt G, et al. Prognostic factors for predicting outcomes after intramedullary nailing of the tibia. J Bone Joint Surg Am. 2012;94:1786–1793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Seyhan M, Guler O, Mahirogullari M, et al. Complications during removal of stainless steel versus titanium nails used for intramedullary nailing of diaphyseal fractures of the tibia. Ann Med Surg (Lond). 2018;26:38–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Popkov AV, Gorbach EN, Kononovich NA, et al. Bioactivity and osteointegration of hydroxyapatite-coated stainless steel and titanium wires used for intramedullary osteosynthesis. Strategies Trauma Limb Reconstr. 2017;12:107–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Suzuki T, Smith WR, Stahel PF, et al. Technical problems and complications in the removal of the less invasive stabilization system. J Orthop Trauma. 2010;24:369–373. [DOI] [PubMed] [Google Scholar]
- 34.Holzach P, Matter P. The comparison of steel and titanium dynamic compression plates used for internal fixation of 256 fractures of the tibia. Injury. 1978;10:120–123. [DOI] [PubMed] [Google Scholar]
- 35.Beumer A, Campo MM, Niesing R, et al. Screw fixation of the syndesmosis: a cadaver model comparing stainless steel and titanium screws and three and four cortical fixation. Injury. 2005;36:60–64. [DOI] [PubMed] [Google Scholar]
- 36.Ozkaya U, Parmaksizoglu AS, Gul M, et al. Minimally invasive treatment of distal tibial fractures with locking and non-locking plates. Foot Ankle Int. 2009;30:1161–1167. [DOI] [PubMed] [Google Scholar]
- 37.Reese K, Litsky A, Kaeding C, et al. Cannulated screw fixation of Jones fractures: a clinical and biomechanical study. Am J Sports Med. 2004;32:1736–1742. [DOI] [PubMed] [Google Scholar]
- 38.DeVries JG, Cuttica DJ, Hyer CF. Cannulated screw fixation of Jones fifth metatarsal fractures: a comparison of titanium and stainless steel screw fixation. J Foot Ankle Surg. 2011;50:207–212. [DOI] [PubMed] [Google Scholar]
- 39.Hunt KJ, Ellington JK, Anderson RB, et al. Locked versus nonlocked plate fixation for hallux MTP arthrodesis. Foot Ankle Int. 2011;32:704–709. [DOI] [PubMed] [Google Scholar]
- 40.Jain R, Podworny N, Hearn T, et al. Effect of stainless steel and titanium low-contact dynamic compression plate application on the vascularity and mechanical properties of cortical bone after fracture. J Orthop Trauma. 1997;11:490–495. [DOI] [PubMed] [Google Scholar]
- 41.Gautier E, Perren SM, Cordey J. Strain distribution in plated and unplated sheep tibia an in vivo experiment. Injury. 2000;31 suppl 3:C37–C44. [DOI] [PubMed] [Google Scholar]
- 42.Arens S, Schlegel U, Printzen G, et al. Influence of materials for fixation implants on local infection. An experimental study of steel versus titanium DCP in rabbits. J Bone Joint Surg Br. 1996;78:647–651. [PubMed] [Google Scholar]