Background:
The purpose of the present study was to estimate the effect of preoperative fracture tilt and to scrutinize the effect of anterior tilt on the risk of treatment failure in patients with Garden Type-I and II femoral neck fractures that are treated with internal fixation.
Methods:
A retrospective multicenter study was performed on a consecutive series of patients ≥60 years of age who had undergone primary internal fixation for the treatment of Garden Type-I and II femoral neck fractures. The study included 1,505 patients with a minimum follow-up of 2 years. Radiographic assessments encompassed preoperative and postoperative tilt, implant inclination, and treatment failure. Data on reoperation and mortality were collected. The risk of treatment failure was assessed with use of Cox proportional hazard regression analysis.
Results:
The study comprised 1,505 patients (71% female) with a median age of 81 years (range, 60 to 108 years). Overall, 234 patients (16%) were classified as having a treatment failure and 251 patients (17%) underwent reoperation. A preoperative anterior tilt of >10° and a posterior tilt of >20° were predictors of treatment failure and reoperation, respectively. Treatment failure occurred in 74 (25%) of 301 patients with a posterior tilt of >20° and in 17 (43%) of 40 patients with an anterior tilt of >10°.
Conclusions:
This multicenter cohort study identified a subgroup of patients with Garden Type-I and II femoral neck fractures with an anterior tilt of >10° as having high treatment failure rates and major reoperation rates comparable with those associated with displaced femoral neck fractures. A preoperative posterior tilt of >20° increases the risk of treatment failure, and the potential benefit of arthroplasty in this subgroup of patients remains to be further investigated.
Level of Evidence:
Prognostic Level III. See Instructions to Authors for a complete description of levels of evidence.
Garden Type-I and II femoral neck fractures are classified on the basis of anteroposterior radiographs and are routinely treated with closed reduction and internal fixation1,2. However, the outcomes following this procedure have been questioned because of a high reported reoperation rate of 8% to 21%2. Several small to medium-sized studies have investigated radiographic risk factors to identify patients with an increased risk of treatment failure. Those studies demonstrated an increased risk in patients with a posterior tilt3-11. Recently, a study from our institution demonstrated that an anterior tilt of >10° was associated with a high rate of treatment failure7. Alternative procedures for subsets of patients with Garden Type-I and II femoral neck fractures and a high risk of failure include hemiarthroplasty and total hip arthroplasty.
The purpose of the present large multicenter cohort study was to assess the effect of preoperative fracture tilt on the risk of treatment failure and reoperation in patients with Garden Type-I and II femoral neck fractures that were treated with closed reduction and internal fixation. The null hypothesis was that fracture tilt would not increase the risk of treatment failure and reoperation.
Materials and Methods
Settings and Location
This retrospective multicenter study included patients who had been managed with closed reduction and internal fixation for the treatment of Garden Type-I or II femoral neck fractures between January 2003 and October 2018 at 3 hospitals in Sweden: Umeå University Hospital (2003 to 2018), Danderyd University Hospital (2010 to 2018), and Skellefteå Hospital (2004 to 2018). Umeå University Hospital is a tertiary university hospital with a catchment area for emergency care of about 160,000 inhabitants. Danderyd University Hospital is a third-level regional emergency teaching hospital affiliated with the Karolinska Institute and has a catchment area of approximately 500,000 inhabitants. Skellefteå Hospital is a primary hospital with a catchment area for emergency care of approximately 80,000 inhabitants.
Ethics
The study was conducted according to the Helsinki Declaration’s ethical principles and was approved by the Swedish Ethical Review Authority (entry number 2019-06449).
Patients and Data Collection
We included a consecutive series of all patients ≥60 years of age with a nonpathological Garden Type-I or II femoral neck fracture that had been treated with closed reduction and internal fixation with screws or pins (Fig. 1). We included 384 patients who had been included in a previous study from our department7. Patients who were missing a preoperative lateral radiograph or who had insufficient radiographs were excluded. Follow-up evaluations were performed until November 2020 or death, whichever occurred first. Patient characteristics and follow-up data were collected retrospectively from in-hospital medical records at the time of admission. The data that were collected included age, sex, American Society of Anesthesiologists (ASA) classification, cognitive impairment (yes/no), use of a walking aid (yes/no), admission from sheltered housing (yes/no), surgical treatment, reoperation, and date of death.
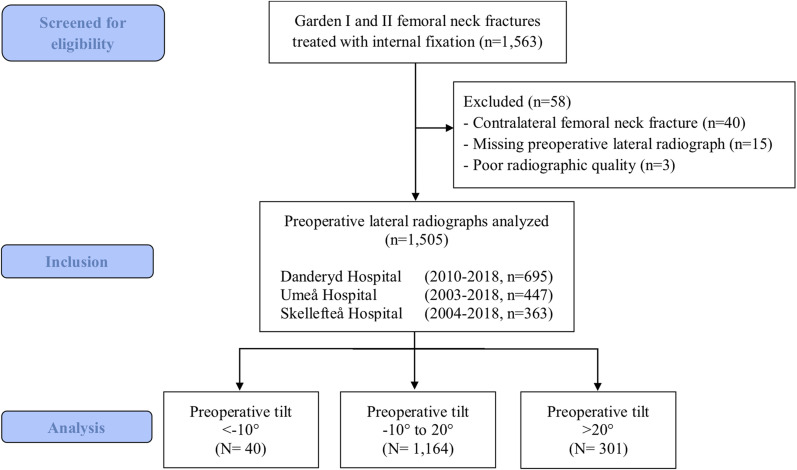
Fig. 1.
Patient flowchart.
Radiographic Assessment
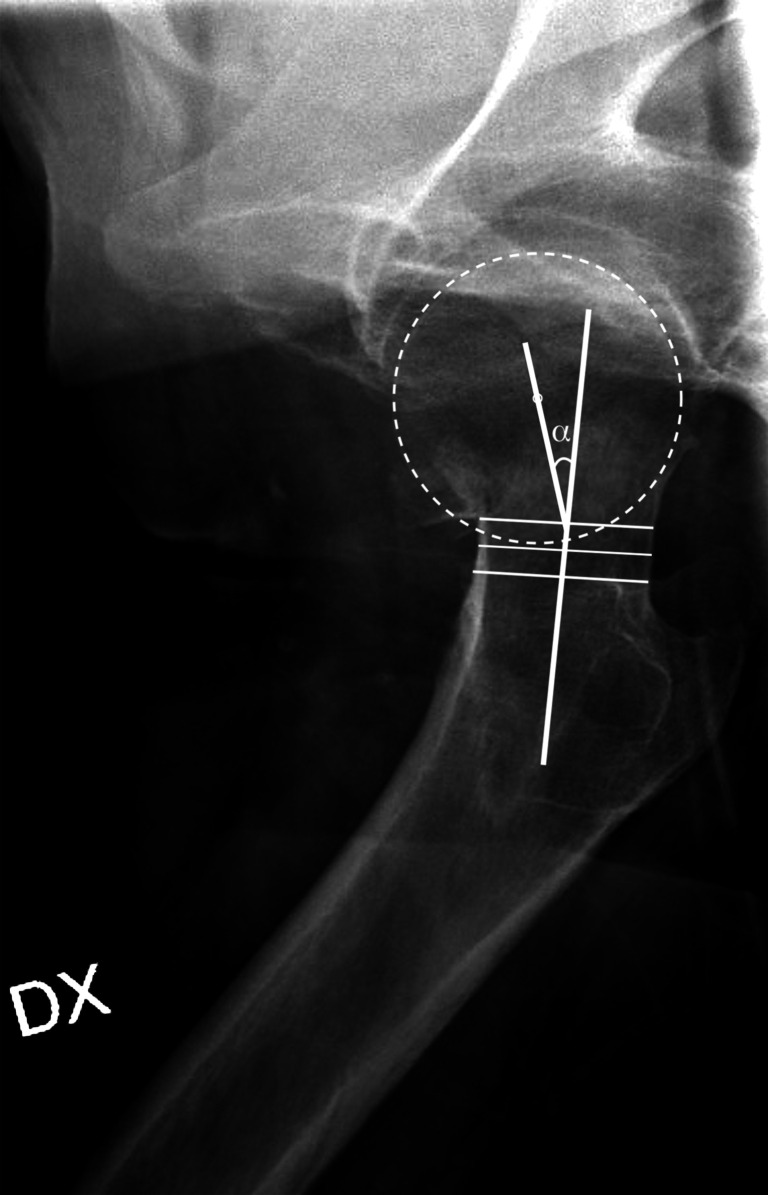
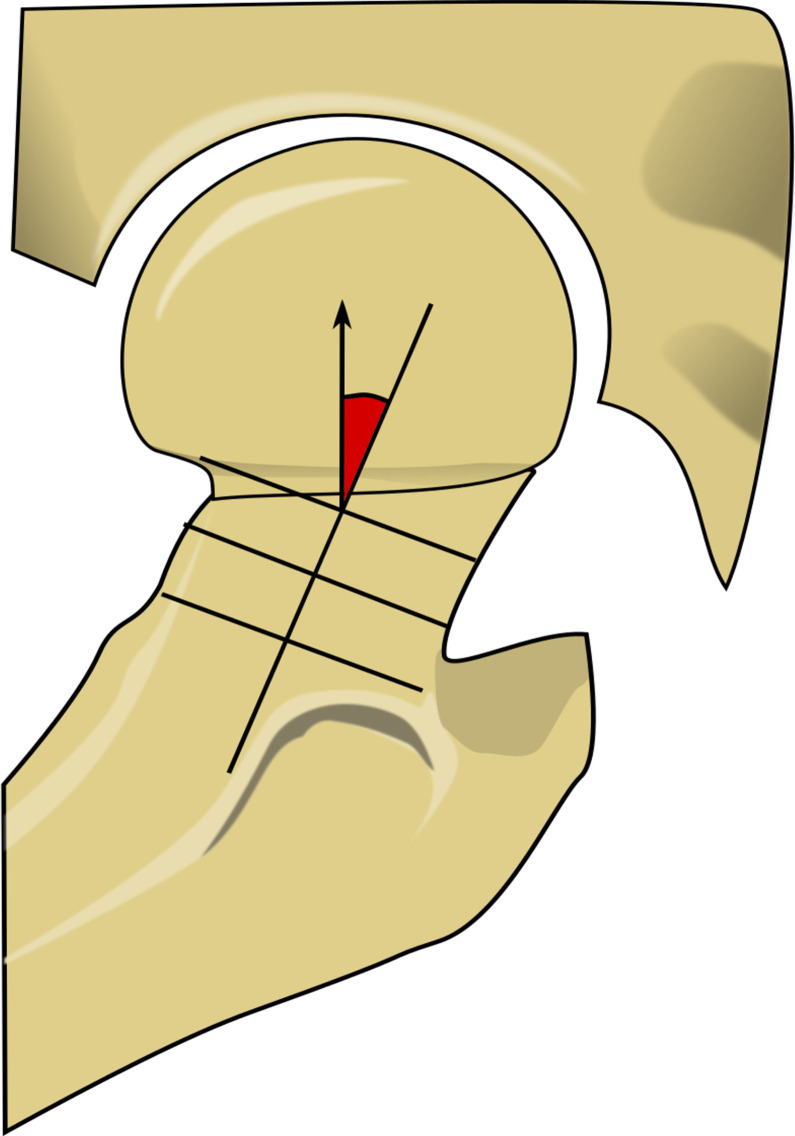
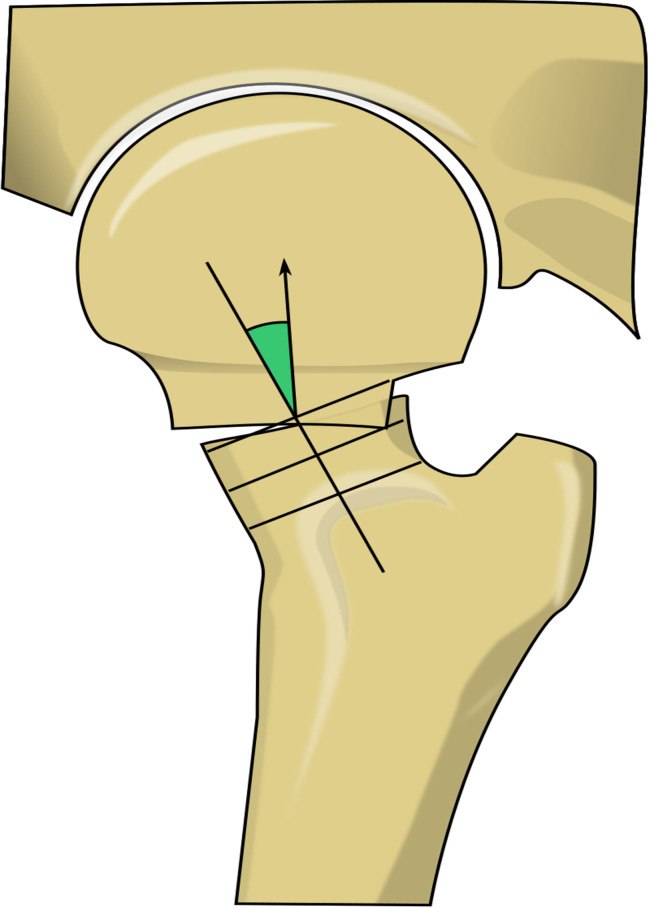
Garden Type-I and II femoral neck fractures were identified on anteroposterior radiographs. The tilt of the femoral head was measured on standardized preoperative and postoperative lateral radiographs of the hip according to the method described by Palm et al. (Figs. 2, 3-A, and 3-B)6. If a postoperative lateral radiograph was missing, the postoperative tilt was assessed on the basis of intraoperative C-arm image documentation. The implant inclination of the inferior pin or screw was measured on the postoperative anteroposterior pelvic radiograph, or on the intraoperative image if a postoperative lateral radiograph was missing. Measurements were made by 2 raters (P.S., J.S.) who were not blinded. Interobserver reliability was assessed with the use of the preoperative radiographs for 50 randomly selected patients. Images were digitally acquired using a picture archiving and communication system (PACS) (Impax; Agfa).
Fig. 2.
Lateral radiograph showing a femoral neck fracture with an anterior tilt.
Fig. 3-A.
Illustration of a lateral radiograph depicting a femoral neck fracture with an anterior tilt.
Fig. 3-B.
Illustration of a lateral radiograph depicting a femoral neck fracture with a posterior tilt.
Internal Fixation
Internal fixation was carried out identically at the participating hospitals. The patient was positioned on a fracture table. Internal fixation was performed with 2 pins (Hansson Pin system; Swemac) (Fig. 4), as routinely used at Skellefteå Hospital and Umeå University Hospital, or with 2 or 3 cannulated screws (Olmed; DePuy/Johnson & Johnson), as are routinely used at Danderyd University Hospital. Perioperative antibiotic prophylaxis and thromboprophylaxis were routinely administered. A physiotherapist supervised the mobilization, which was intended to start on the first postoperative day.
Fig. 4.
Anteroposterior depicting internal fixation with 2 Hansson pins.
Outcome Measurements
The main outcome measure was treatment failure, which was defined as a composite variable consisting of any nonunion, fixation failure, osteonecrosis, or posttraumatic osteoarthritis (defined as radiographic signs of osteoarthritis in combination with clinical symptoms involving hip joint pain). The secondary outcomes was major reoperation, defined as hip resection hip resection arthroplasty, hip arthroplasty, or repeat osteosynthesis due to subsequent fractures around the implants. Minor reoperation was defined as the removal of osteosynthesis implants, adjustment of pins or screws, or a DAIR (surgical debridement, antibiotics, and implant retention) procedure due to deep postoperative infection.
Statistical Analysis
Cox proportional hazard regression was used to identify risk factors for treatment failure and for major reoperation. The assumption of proportional hazards was assessed with use of Schoenfeld residuals. In additional to the exposure variable (fracture tilt), the variables of age, sex, ASA classification, cognitive impairment, and residence in sheltered housing were selected as covariates indicating patient fragility. Surgical factors such as implant inclination and postoperative tilt were also included as covariates.
Continuous variables, including preoperative and postoperative tilt, implant inclination, and age, were tested for nonlinearity by means of analysis of variance (ANOVA) and, if significant, were modeled with use of restricted cubic splines. The number of knots, which determines flexibility of the spline, was chosen with use of the Bayesian information criterion. Competing risk analysis was investigated with use of cause-specific Cox proportional hazard regression12. We also performed an unadjusted relative risk calculation. Interobserver reliability between the 2 raters who measured the preoperative fracture tilt was analyzed with use of the interclass correlation coefficient. We used SPSS (version 26.0, SPSS Statistics for Macintosh; IBM) and R (version 4.0.3) in combination with the rms package (version 6.1-0) for the survival analysis and risk regression (R version 2020.12.08) for competing risk analysis.
Source of Funding
The study was funded by grants from the ALF (regional agreement on medical training and clinical research) between the Västerbotten County Council and Umeå University.
Results
Patients and Descriptive Data
Of 1,563 patients accessed, 1,505 (96%) were included in the study (Fig. 1). The majority of the patients were female (71%), and the median age was 81 years (range, 60 to 108 years) (Fig. 1, Table I). The mean duration of follow-up was 3.2 years (range, 2 to 17 years). The 1-year mortality rate was 22%, and the 2-year mortality rate was 34%.
TABLE I.
Patient Characteristics (N = 1,505)
| Age* (yr) | 81 ± 9 |
| Female sex† | 1,071 (71%) |
| ASA classification‡ | |
| 1-2† | 568 (38%) |
| 3-5† | 937 (62%) |
| Cognitive impairment† | 539 (36%) |
| Sheltered housing† | 429 (29%) |
| Preoperative tilt* | 11° ±12° |
| Missing† | 0 |
| Postoperative tilt* | 4° ± 8° |
| Missing† | 27 (2%) |
| Implant inclination* | 137° ± 7° |
| ≤125°† | 64 (4%) |
| >125°† | 1,407 (93%) |
| Missing† | 34 (2%) |
The values are given as the mean and standard deviation.
The values are given as the number of patients, with the percentage in parentheses.
ASA = American Society of Anesthesiologists.
Treatment Failure
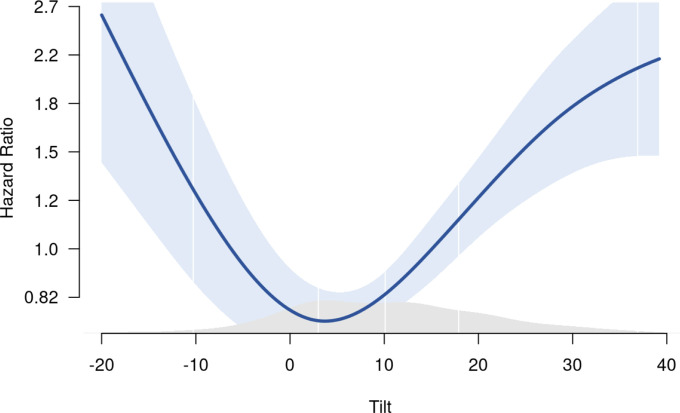
Overall, 234 patients (16%) were classified as having treatment failure (Table II). The relative risk of treatment failure was 3.5 (95% confidence interval [CI], 2.3 to 5.1) in patients with a preoperative anterior tilt of >10° and 2.0 (95% CI, 1.6 to 2.6) in those with a posterior tilt of >20° as compared with those with a preoperative tilt between −10° and 20°, respectively. The hazard ratio of treatment failure was significant in patients with an anterior tilt of >10° and a posterior tilt of >20° (Fig. 5, Table III). Competing risk regression confirmed that significant predictors of mortality were age, sex, ASA category, sheltered living, and cognitive impairment. Neither tilt nor the operative variables (implant inclination and postoperative tilt) significantly affected mortality. The interobserver reliability of preoperative tilt as estimated with the interclass correlation coefficient was excellent (0.98) between the 2 raters.
Fig. 5.
Graph showing the risk of treatment failure as a function of tilt in degrees. Anterior tilt corresponds with negative values on the x axis. The values are adjusted for sex, American Society of Anesthesiologists (ASA) classification, sheltered housing, implant inclination, cognitive impairment, and postoperative fracture tilt. The light blue area corresponds to the 95% CI.
TABLE II.
Treatment Failures and Reoperations*
| <−10° (N = 40) | −10° to 20° (N = 1,164) | >20° (N = 301) | All Patients (N = 1,505) | |
|---|---|---|---|---|
| Age† (yr) | 83 ± 7 | 80 ± 9 | 81 ± 9 | 81 ± 9 |
| Female sex‡ | 33 (83%) | 847 (73%) | 191 (63%) | 1,071 (71%) |
| Failure‡ | 17 (43%) | 143 (12%) | 74 (25%) | 234 (16%) |
| Osteonecrosis | 10 | 80 | 25 | 115 (8%) |
| Nonunion | 4 | 27 | 25 | 56 (4%) |
| Fixation failure | 3 | 23 | 21 | 47 (3%) |
| Posttraumatic arthritis | 0 | 13 | 3 | 16 (1%) |
| Reoperation‡ | 14 (35%) | 172 (15%) | 65 (22%) | 251 (17%) |
| Total arthroplasty | 7 | 72 | 31 | 110 (7%) |
| Removal of osteosynthesis | 1 | 52 | 16 | 69 (5%) |
| Hemiarthroplasty | 6 | 22 | 16 | 44 (3%) |
| Periprosthetic fracture | 0 | 11 | 1 | 12 (1%) |
| Adjustment of osteosynthesis | 0 | 9 | 0 | 9 (0.5%) |
| Girdlestone procedure | 0 | 5 | 1 | 6 (0.4%) |
| DAIR§ | 0 | 1 | 0 | 1 (0.06%) |
In the header row, negative values indicate anterior tilt.
The values are given as the mean and the standard deviation.
The values are given as the number of patients, with or without the percentage in parentheses.
DAIR = debridement, antibiotics, and implant retention.
TABLE III.
Cox Proportional Hazard Model for Covariates Associated with Treatment Failure (N = 1,505)*
| Variable | Crude HR† (95% CI, 2.5%-97.5%) | Adjusted HR† (95% CI, 2.5%-97.5%) |
|---|---|---|
| Age (per 10 yr) | 1.2 (1.0-1.4) | 1.3 (1.1-1.5) |
| Sex | ||
| Male (reference) | 1.0 | 1.0 |
| Female | 1.3 (1.0-1.8) | 1.4 (1.0-2.0) |
| ASA classification‡ | ||
| 1-2 (reference) | 1.0 | 1.0 |
| 3-5 | 1.0 (0.8-1.3) | 0.9 (0.7-1.3) |
| Sheltered housing | ||
| No (reference) | 1.0 | 1.0 |
| Yes | 0.6 (0.4-0.9) | 0.7 (0.4-1.0) |
| Cognitive impairment | ||
| No (reference) | 1.0 | 1.0 |
| Yes | 0.8 (0.6-1.0) | 0.8 (0.6-1.2) |
| Implant inclination (per 10°) | 0.8 (0.7-1.0) | 0.9 (0.7-1.1) |
| Preoperative tilt§ | ||
| −20° | 2.2 (1.2-4.1) | 4.0 (2.2-7.3) |
| −10° | 1.6 (1.1-2.4) | 1.9 (1.3-2.7) |
| 0° | 1.2 (1.0-1.4) | 0.9 (0.8-1.1) |
| 10° (reference) | 1.0 | 1.0 |
| 20° | 1.2 (1.1-1.3) | 1.8 (1.5-2.2) |
| 30° | 1.8 (1.5-2.2) | 2.3 (1.8-3.0) |
| 40° | 2.7 (1.9-3.7) | 2.7 (1.8-4.0) |
| Postoperative tilt (per 1°) | 1.0 (1.0-1.0) | 1.0 (1.0-1.0) |
| Hospital | ||
| Danderyd (reference) | 1.0 | 1.0 |
| Umeå University | 0.8 (0.6-1.1) | 0.9 (0.6-1.3) |
| Skellefteå | 1.3 (1.0-1.7) | 1.3 (1.0-1.8) |
Adjusted for age, sex, ASA classification, sheltered housing, cognitive impairment, implant inclination, postoperative tilt, and hospital.
HR = hazard ratio.
ASA = American Society of Anesthesiologists.
Negative values indicate anterior tilt.
Reoperations
A total of 251 (17%) of the 1,505 patients underwent any reoperation, including minor procedures, during the study period (Table II). A total of 149 (64%) of the 234 patients who were identified as having a treatment failure underwent a major reoperation in the first 2 years after internal fixation. In addition, 54 patients with a treatment failure (including 24 with osteonecrosis, 12 with nonunion, 12 with fixation failure, and 6 with posttraumatic arthritis) did not undergo a major reoperation because of their general health status or because they died while awaiting surgery. Covariates associated with major reoperation according to the Cox proportional hazard model are presented in Table IV.
TABLE IV.
Cox Proportional Hazard Model for Covariates Associated with Major Reoperation (N = 1,505)*
| Variable | Crude HR† (95% CI, 2.5%-97.5%) | Adjusted HR† (95% CI, 2.5%-97.5%) |
|---|---|---|
| Age (per 10 yr) | 1.0 (0.8-1.1) | 1.1 (0.9-1.3) |
| Sex | ||
| Male (reference) | 1.0 | 1.0 |
| Female | 1.3 (0.9-1.8) | 1.2 (0.8-1.8) |
| ASA classification‡ | ||
| 1-2 (reference) | 1.0 | 1.0 |
| 3-5 | 0.7 (0.5-1.0) | 0.8 (0.6-1.1) |
| Sheltered housing | ||
| No (reference) | 1.0 | 1.0 |
| Yes | 0.3 (0.2-0.5) | 0.4 (0.2-0.8) |
| Cognitive impairment | ||
| No (reference) | 1.0 | 1.0 |
| Yes | 0.4 (0.3-0.6) | 0.6 (0.4-1.0) |
| Implant inclination (per 10°) | 0.9 (0.7-1.1) | 0.9 (0.7-1.1) |
| Preoperative tilt§ | ||
| −20° | 2.2 (1.1-4.5) | 3.3 (1.7-6.3) |
| −10° | 1.7 (1.1-2.6) | 1.7 (1.2-2.6) |
| 0° | 1.2 (1.0-1.5) | 0.9 (0.8-1.2) |
| 10° (reference) | 1.0 | 1.0 |
| 20° | 1.1 (1.0-1.3) | 1.6 (1.2-2.0) |
| 30° | 1.5 (1.1-2.0) | 1.8 (1.3-2.6) |
| 40° | 2.0 (1.3-3.1) | 2.0 (1.2-3.4) |
| Postoperative tilt (per 1°) | 0.9 (0.7-1.1) | 0.9 (0.7-1.2) |
| Hospital | ||
| Danderyd (reference) | 1.0 | 1.0 |
| Umeå University | 1.0 (0.7-1.4) | 1.1 (0.8-1.7) |
| Skellefteå | 1.0 (0.7-1.5) | 1.1 (0.7-1.6) |
Adjusted for age, sex, ASA classification, sheltered housing, cognitive impairment, implant inclination, postoperative tilt and hospital.
HR = hazard ratio.
ASA = American Society of Anesthesiologists.
Negative values indicate anterior tilt.
Discussion
The main finding of this large multicenter cohort study was the identification of a subgroup of elderly patients with Garden Type-I and II femoral neck fractures with an anterior tilt of >10°, who had failure rates comparable with those for displaced femoral neck fractures7,13. This study also confirmed that a preoperative posterior tilt of >20° increases the risk of treatment failure necessitating major reoperation.
The finding that an anterior tilt >10° is a risk factor for treatment failure was first reported in a peer-reviewed study from our institution7. Previously, anterior tilt had only been proposed as a risk factor for femoral neck fractures in a book on internal fixation by Manninger et al.13. Patients with this finding represent just 2% to 3% of all patients with Garden Type-I and II femoral neck fractures, but this small group has a high rate of treatment failure and major reoperations. A prospective randomized controlled trial (RCT) comparing hip arthroplasty and internal fixation in this subgroup of patients is not feasible because of their rarity. On the basis of the high rate of failure for those with a preoperative anterior tilt >10°, we recommend that this subgroup of elderly patients be treated with primary hip arthroplasty.
Many studies have reported an association between preoperative posterior tilt and treatment failure3-10. One-fifth of our patients had a preoperative posterior tilt of >20°, representing a relatively large proportion of Garden Type-I and II femoral neck fractures. The wide range of reoperation rates reported in the literature (10% to 56%) might be due to differences between the studies in terms of the categorization of measurements, the definition of outcomes, sample size, and the duration of follow-up. In our previous study7, we found a similar failure rate as that reported by Dolatowski et al.4. The increased risk of treatment failure raises the question whether hip arthroplasty has an advantage over internal fixation14. In a recent RCT comparing hemiarthroplasty with internal fixation for the treatment of Garden Type-I and II femoral neck fractures, Dolatowski et al. performed a post hoc analysis of patients assigned to internal fixation and found that patients with a preoperative posterior tilt of >20° had a higher risk of healing complications than those with a tilt of ≤20°15. A large nationwide register-based RCT, including all Garden Type-I and II femoral neck fractures, was recently started in Sweden to further disentangle the benefit of hip arthroplasty in this group of patients16. To highlight the different prognosis depending on fracture tilt, a modification with the addition of an anterior tilt of >10° and a posterior tilt of >20° could be added as a complement to AO/OTA classification.
The rates of treatment failure and reoperation in the present study are lower in patients with an anterior tilt of ≤10° and a posterior tilt of ≤20°. This group of patients and the benefit of arthroplasty in elderly patients with a Garden type-I and II femoral neck fracture are under investigation in 2 large RCTs16,17. A pronounced tilt might cause a predisposition to increased instability due to comminution of the femoral calcar with a risk of disrupted healing tendency and for redisplacement11,18. Vascular disruption of the retinacular arteries and venous drainage of the femoral neck and head might contribute to the higher failure rate in patients with a more pronounced tilt18,19. Internal fixation failure necessitating the need for salvage hip arthroplasty is a severe complication in older patients because of the inferior outcomes compared with those of primary hip arthroplasty20,21.
Consistent with previous results4,6, perioperative reduction of the fracture tilt did not influence the risk of treatment failure in the present study. In a recent study of patients undergoing osteosynthesis for a Garden Type-I or II or Garden Type-III or IV femoral neck fracture, Nyholm et al. concluded that femoral head cartilage perforation, varus implant positions (≤125°), and insufficient reduction were the only surgical factors influencing the risk of reoperation5. In the present study, we did not find that varus positioning of the implant, as indicated by implant inclination, influenced the risk of treatment failure.
Our study has a number of limitations. First, the retrospective cohort study design, with the lack of any patient-reported outcomes and scheduled follow-up evaluations, could obscure unidentified treatment failures. Approximately one-fourth (29%) of the patients lived in sheltered housing. Such patients have a lower risk of reoperation and tend to have a lower risk of treatment failure. These findings are most likely due to the fact that patients living in sheltered housing have a high mortality rate and are unfit to seek health-care services actively. This fragile group might reduce the identification of failure and mask the breadth of issues related to internal fixation of Garden Type-I and II femoral neck fractures.
Second, we could not analyze the effect of potentially influential factors that were not recorded in the medical files, such as smoking and osteoporosis. Third, patients with missing or poor-quality radiographs were excluded from the present analysis.
The strengths of the present study include the multicenter design and the inclusion of the largest sample size of Garden Type-I and II femoral neck fractures to be reported to date. The large sample allowed us to identify and confirm anterior tilt as a major risk factor for treatment failure. The use of the unique Swedish personal identity number made it possible to collect data by reviewing our in-hospital medical databases. In addition, the inclusion of all health-care services in the catchment area ensured completeness of data. We assessed interobserver reliability to validate the radiographic outcomes and found excellent agreement, consistent with the findings of previous studies on the reliability of posterior tilt measurements. The minimum detectable change has previously been reported to be 1422. Moreover, lateral radiographs have been shown to accurately assess posterior tilt as compared with computed tomography models in patients with Garden Type-I and II femoral neck fractures23. The statistical methods analyzing fracture tilt as a continuous variable strengthened the study.
In summary, we identified a subgroup of elderly patients with Garden Type-I and II femoral neck fractures with an anterior tilt of >10° as having high rates of treatment failure and major reoperation, comparable with those associated with displaced femoral neck fractures. Primary arthroplasty should be considered for this subgroup of elderly patients. This study also confirmed that a preoperative tilt of >20° increases the risk of treatment failure necessitating reoperation.
Footnotes
Investigation performed at the Department of Orthopaedics, Umeå University Hospital, Umeå, Sweden
Disclosure: The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A330).
References
- 1.Kjærvik C, Stensland E, Byhring HS, Gjertsen JE, Dybvik E, Søreide O. Hip fracture treatment in Norway: deviation from evidence-based treatment guidelines: data from the Norwegian Hip Fracture Register, 2014 to 2018. Bone Jt Open. 2020. Oct 14;1(10):644-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oñativia IJ, Slullitel PA, Diaz Dilernia F, Gonzales Viezcas JM, Vietto V, Ramkumar PN, Buttaro MA, Piuzzi NS. Outcomes of nondisplaced intracapsular femoral neck fractures with internal screw fixation in elderly patients: a systematic review. Hip Int. 2018. Jan;28(1):18-28. [DOI] [PubMed] [Google Scholar]
- 3.Clement ND, Green K, Murray N, Duckworth AD, McQueen MM, Court-Brown CM. Undisplaced intracapsular hip fractures in the elderly: predicting fixation failure and mortality. A prospective study of 162 patients. J Orthop Sci. 2013. Jul;18(4):578-85. [DOI] [PubMed] [Google Scholar]
- 4.Dolatowski FC, Adampour M, Frihagen F, Stavem K, Erik Utvåg S, Hoelsbrekken SE. Preoperative posterior tilt of at least 20° increased the risk of fixation failure in Garden-I and -II femoral neck fractures. Acta Orthop. 2016. Jun;87(3):252-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nyholm AM, Palm H, Sandholdt H, Troelsen A, Gromov K; Danish Fracture Database Collaborators. Osteosynthesis with parallel implants in the treatment of femoral neck fractures: minimal effect of implant position on risk of reoperation. J Bone Joint Surg Am. 2018. Oct 3;100(19):1682-90. [DOI] [PubMed] [Google Scholar]
- 6.Palm H, Gosvig K, Krasheninnikoff M, Jacobsen S, Gebuhr P. A new measurement for posterior tilt predicts reoperation in undisplaced femoral neck fractures: 113 consecutive patients treated by internal fixation and followed for 1 year. Acta Orthop. 2009. Jun;80(3):303-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sjöholm P, Otten V, Wolf O, Gordon M, Karsten G, Sköldenberg O, Mukka S. Posterior and anterior tilt increases the risk of failure after internal fixation of Garden I and II femoral neck fracture. Acta Orthop. 2019. Dec;90(6):537-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lapidus LJ, Charalampidis A, Rundgren J, Enocson A. Internal fixation of Garden I and II femoral neck fractures: posterior tilt did not influence the reoperation rate in 382 consecutive hips followed for a minimum of 5 years. J Orthop Trauma. 2013. Jul;27(7):386-90 [DOI] [PubMed] [Google Scholar]
- 9.van der List JP, El Saddy S, Vos SJ, Temmerman OPP. Role of preoperative posterior tilt on the outcomes of internal fixation of non-displaced femoral neck fractures: A systematic review and meta-analysis. Injury. 2021. Mar;52(3):316-23. [DOI] [PubMed] [Google Scholar]
- 10.Okike K Udogwu UN Isaac M Sprague S Swiontkowski MF Bhandari M Slobogean GP; FAITH Investigators. Not All Garden-I and II Femoral Neck Fractures in the Elderly Should Be Fixed: Effect of Posterior Tilt on Rates of Subsequent Arthroplasty. J Bone Joint Surg Am. 2019. Oct 16;101(20):1852-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garden RS. Stability and union in subcapital fractures of the femur. J Bone Joint Surg Br. 1964. Nov;46:630-47. [PubMed] [Google Scholar]
- 12.Gerds TA, Scheike TH, Andersen PK. Absolute risk regression for competing risks: interpretation, link functions, and prediction. Stat Med. 2012. Dec 20;31(29):3921-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Manninger J, Bosch U, Cserháti P, Fekete K, Kazár G, editors. Internal fixation of femoral neck fractures: an atlas. Springer; 2007. [Google Scholar]
- 14.Ma HH, Chou TA, Tsai SW, Chen CF, Wu PK, Chen WM. Outcomes of internal fixation versus hemiarthroplasty for elderly patients with an undisplaced femoral neck fracture: a systematic review and meta-analysis. J Orthop Surg Res. 2019. Oct 11;14(1):320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dolatowski FC, Frihagen F, Bartels S, Opland V, Šaltytė Benth J, Talsnes O, Hoelsbrekken SE, Utvåg SE. Screw Fixation Versus Hemiarthroplasty for Nondisplaced Femoral Neck Fractures in Elderly Patients: A Multicenter Randomized Controlled Trial. J Bone Joint Surg Am. 2019. Jan 16;101(2):136-44. [DOI] [PubMed] [Google Scholar]
- 16.Wolf O, Sjöholm P, Hailer NP, Möller M, Mukka S. Study protocol: HipSTHeR - a register-based randomised controlled trial - hip screws or (total) hip replacement for undisplaced femoral neck fractures in older patients. BMC Geriatr. 2020. Jan 21;20(1):19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Viberg B, Kold S, Brink O, Larsen MS, Hare KB, Palm H; SENSE collaborators. Is arthroplaSty bEtter than interNal fixation for undiSplaced femoral nEck fracture? A national pragmatic RCT: the SENSE trial. BMJ Open. 2020. Oct 10;10(10):e038442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lazaro LE, Klinger CE, Sculco PK, Helfet DL, Lorich DG. The terminal branches of the medial femoral circumflex artery: the arterial supply of the femoral head. Bone Joint J. 2015. Sep;97-B(9):1204-13. [DOI] [PubMed] [Google Scholar]
- 19.Gojda J, Bartoníček J. The retinacula of Weitbrecht in the adult hip. Surg Radiol Anat. 2012. Jan;34(1):31-8. [DOI] [PubMed] [Google Scholar]
- 20.Blomfeldt R, Törnkvist H, Ponzer S, Söderqvist A, Tidermark J. Displaced femoral neck fracture: comparison of primary total hip replacement with secondary replacement after failed internal fixation: a 2-year follow-up of 84 patients. Acta Orthop. 2006. Aug;77(4):638-43. [DOI] [PubMed] [Google Scholar]
- 21.Frihagen F, Madsen JE, Aksnes E, Bakken HN, Maehlum T, Walløe A, Nordsletten L. Comparison of re-operation rates following primary and secondary hemiarthroplasty of the hip. Injury. 2007. Jul;38(7):815-9. [DOI] [PubMed] [Google Scholar]
- 22.Dolatowski FC, Hoelsbrekken SE. Eight orthopedic surgeons achieved moderate to excellent reliability measuring the preoperative posterior tilt angle in 50 Garden-I and Garden-II femoral neck fractures. J Orthop Surg Res. 2017. Sep 19;12(1):133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Temmesfeld MJ, Dolatowski FC, Borthne A, Utvåg SE, Hoelsbrekken SE. Cross-Table Lateral Radiographs Accurately Predict Displacement in Valgus-Impacted Femoral Neck Fractures. JB JS Open Access. 2019. Feb 27;4(1):e0037. [DOI] [PMC free article] [PubMed] [Google Scholar]