Abstract
Background
The sacro-femoro-pubic (SFP) angle is a surrogate measurement for pelvic tilt obtained on anteroposterior (AP) pelvis radiographs. It is unknown whether the SFP angle can be measured reliably by senior surgeons and trainees alike.
Methods
We conducted an intrareader and interreader reliability study using preoperative AP pelvis radiographs. Using our hospital electronic database, we randomly selected 31 subjects undergoing primary total hip arthroplasty. An attending orthopedic surgeon and two orthopedic surgery residents performed two separate SFP angle measurements for each subject. Intrareader and interreader agreement were measured using intraclass correlation coefficients (ICC).
Results
Pairwise intrareader and interreader ICCs ranged from 0.91 to 0.99. Overall ICC was 0.94. Interreader ICCs between the attending surgeon and each orthopedic resident were 0.93 and 0.98, and the ICC between orthopedic residents was 0.91. Interreader mean differences for SFP angle measurements were 2.32 degrees or less: -2.03 (standard deviation: 2.23) and 0.29 (1.64) between the attending surgeon and each orthopedic resident, and 2.32 (2.44) between orthopedic residents.
Conclusion
SFP angle may be measured reliably on AP pelvis radiographs by senior clinicians and trainees. SFP angle measurement may prove helpful as an alternative to pelvic tilt measurements when lateral pelvic radiographs are not available.
Keywords: Pelvic tilt, Sacro-femoro-pubic (SFP) angle, Reliability, Reproducibility, Arthroplasty, Pelvis radiograph
Introduction
Dislocation after total hip arthroplasty (THA) is the most common cause of revision hip surgery [1]. Studies have observed a relationship between THA dislocation risk and conditions that lead to pathophysiologic pelvic orientation [[2], [3], [4]]. Pelvic orientation is often assessed by measuring pelvic tilt (PT) on lateral pelvis radiographs (Fig. 1) [2]. However, lateral pelvis radiographs are not routinely obtained before THA.
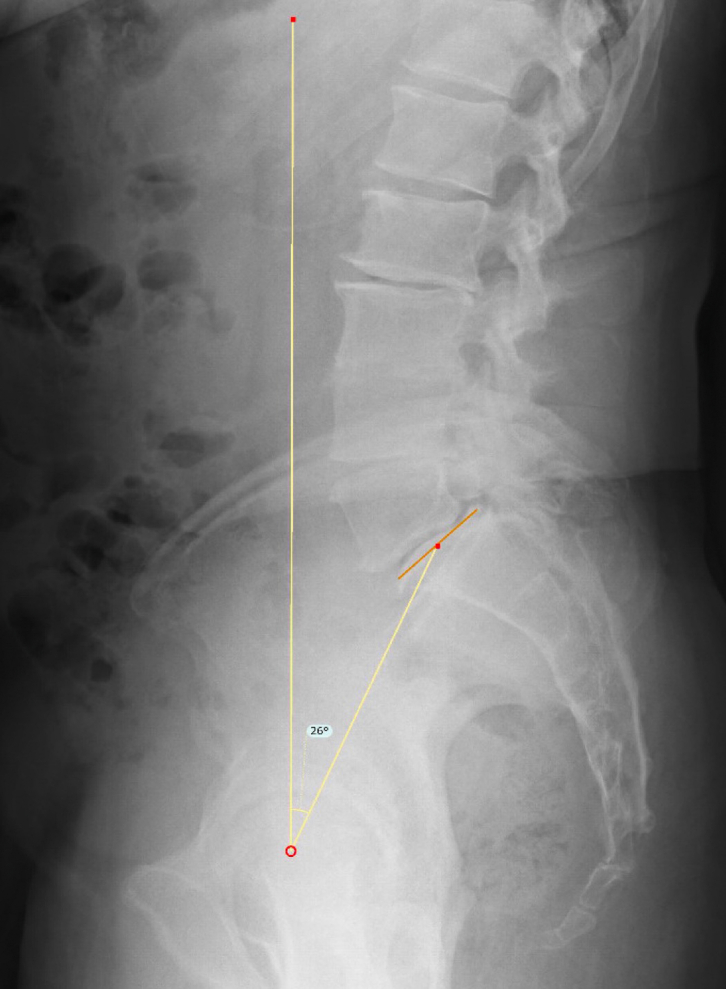
Figure 1.
Pelvic tilt measured on a standing lateral pelvis radiograph. The two arms of the angle include (1) a line drawn from the center of the superior endplate of the sacrum (S1) to the center of the femoral heads, and (2) another line drawn from the center of the femoral heads directly vertical (ie, perpendicular to the floor).
Blondel et al. [5] described a new parameter, the sacro-femoro-pubic (SFP) angle (Fig. 2) and analyzed for correlation with sagittal PT. The SFP angle is a surrogate for the PT measurement and can be measured on anteroposterior (AP) pelvis radiographs [Pelvic tilt can be estimated by using the following formula: PT = 75 – (SFP angle)] [5]. The SFP angle provides a helpful alternative for evaluating PT when lateral pelvis radiographs are not available. As AP pelvis radiographs are routinely obtained before THA, the SFP angle may be a welcome surrogate for surgeons who wish to measure a patient’s PT before undergoing THA. However, SFP angle is not commonly measured by orthopedic surgeons, and it is unknown if SFP angle can be measured reliably by surgeons of different experience levels.
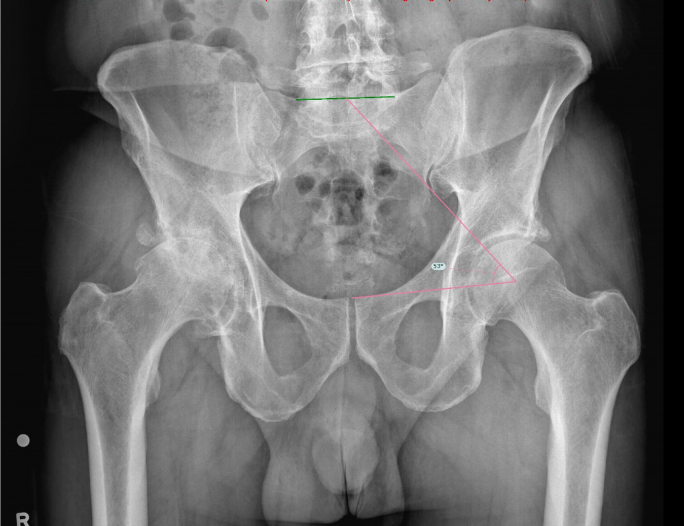
Figure 2.
SFP angle measured on a standing AP pelvis radiograph. The two arms of the angle include (1) a line drawn from the center of the superior endplate of the sacrum (S1) to the center of the femoral head, and (2) another line drawn from the center of the femoral head to the top of the pubic symphysis.
We conducted a study to investigate the intrareader and interreader reliability of SFP angle measurement on AP pelvis radiographs for orthopedists of different experience levels who were trained in the radiographic measurement technique. We hypothesized that the SFP angle measurement could be reproducibly measured by the same surgeon and reliably measured between surgeons with different levels of expertise.
Material and methods
Design and patient sample
The study design was an intrareader reproducibility and interreader reliability retrospective one. The patient sample inclusion criteron included patients who underwent primary THA at a single institution between 2008 and 2010. Patients were excluded if they did not have a preoperative AP pelvis radiograph. From this eligible population, we randomly selected 31 subjects for the study.
Data collection
If available, preoperative AP pelvis radiographs were identified from each subject’s medical record and visualized using Centricity Universal Viewer Zero Footprint (Version 6.0 SP7.0.4, GE Healthcare, Chicago, IL). An attending orthopedic surgeon trained two orthopedic residents on SFP angle measurement. The SFP angle is made between a line drawn from the center of the superior endplate of the sacrum to the center of the femoral head and another line drawn from the center of the femoral head to the top of the pubic symphysis (Fig. 2). Each reader then performed two separate SFP angle measurements for each subject, with readings 1-3 days apart. The readers were blinded to their own previous measurements and to the measurements of other readers.
Statistical analyses
Intrareader and interreader agreement were measured using intraclass correlation coefficients (ICCs). Statistical analyses were conducted using SAS software (Version 9.4; SAS Institute, Cary, NC). This study was approved by our hospital's institutional review board.
Results
Study population
Thirty subjects had preoperative AP pelvis radiographs available for reading, as 1 patient did not have an adequate preoperative AP pelvis radiograph available. The mean age of study subjects was 66 years (standard deviation [STD]: 8 years), and 81% of the patients were female.
SFP measurement reliability
The mean SFP angle was 62.4 degrees (STD: 8.0 degrees). Table 1 shows the intrareader and interreader mean differences for the SFP angle measurements. Mean differences were 2.32 degrees (STD: 2.44) or less. There was very good interreader agreement between the attending surgeon and resident 2 (mean difference: 0.29 [STD 1.64]), and there was less agreement between resident 1 and the other two readers (mean differences -2.03 [2.23] and 2.32 [2.44]).
Table 1.
Intrareader and interreader mean differences between SFP angle measurements.a
| Surgeon | Resident 1 | Resident 2 | |
|---|---|---|---|
| Surgeon | 0.003 (0.92) | -2.03 (2.23) | 0.29 (1.64) |
| Resident 1 | 0.19 (1.93) | 2.23 (2.44) | |
| Resident 2 | 0.07 (1.11) |
Mean difference reported as degrees (standard deviation).
Table 2 shows the intrareader and interreader ICCs. Intrareader reliability was generally excellent with ICCs ranging between 0.97 and 0.99. Interreader reliability was also excellent (ICC = 0.98 between the attending surgeon and resident 2, ICC = 0.93 between the attending surgeon and resident 1, and ICC = 0.91 between resident 1 and resident 2).
Table 2.
Intraclass correlation coefficients (ICCs) for SFP angle measurements.
| Surgeon | Resident 1 | Resident 2 | |
|---|---|---|---|
| Surgeon | 0.993 | 0.930 | 0.979 |
| Resident 1 | 0.971 | 0.913 | |
| Resident 2 | 0.990 |
Discussion
We investigated intrareader reproducibility and interreader reliability for SFP angle measurement on preoperative AP pelvis radiographs. We found excellent intrareader reproducibility and good interreader reliability. Our study aligns with previous literature that demonstrates SFP measurement reliability [6] and contributes further by demonstrating SFP measurement reliability between orthopedists of different experience levels. To our knowledge, this study is also the first to assess SFP measurement reliability for a population with known hip arthritis.
Prior investigations have found a mean PT of 13 degrees (STD: 6 degrees) in a group of asymptomatic individuals and a mean SFP angle of 59.2 degrees (STD: 8.9 degrees) [7]. To our knowledge, normal range for SFP has not been characterized in an arthritic population. Further study may help characterize normal SFP range in patients with hip arthritis.
The hip-spine relationship has garnered significant interest among arthroplasty surgeons in recent years. Studies have observed that abnormal pelvic orientation may affect clinical outcome after THA, such as dislocation risk [[2], [3], [4]]. Any preoperative clues regarding a patient’s disposition to these factors may be helpful in preventing suboptimal clinical outcomes after THA. Currently, the gold standard for assessment of abnormal pelvic orientation is the lateral pelvis radiograph, but lateral pelvis radiographs are not routinely obtained before THA in many clinical practices. Thus, the SFP angle as a surrogate measure for PT could be a useful tool for the arthroplasty surgeon with only an AP pelvis radiograph available preoperatively. This investigation assessed SFP measurement reliability in a population with known hip arthritis. Further studies might investigate correlations between SFP and clinical outcomes.
We acknowledge limitations in this study. The patient sample was small, and these results may not be the same in a larger population of patients. Radiographs were obtained from clinical practice and not a research protocol, introducing variability in images and patient positioning. In addition, we did not have lateral radiographs preoperatively, as this is not our institution’s standard clinical practice before hip replacement surgery, and therefore, we could not internally validate the correlation between SFP and PT. However, this correlation has been shown previously in the literature [5], and we assume it applies to our population as well. Those who read the radiographs in this study were all orthopedic surgeons, and this study was unable to determine if non-orthopaedic surgeons would be able to reliably measure SFP angles.
Conclusions
This study suggests SFP angle can be reliably and reproducibly measured by senior clinicians and trainees on AP pelvis radiographs of patients planning to undergo THA. The relationship between preoperative SFP angle and clinical outcome is unknown, and we will further investigate this relationship. Studies such as this one may serve as a model for teaching trainees to read images and document the reliability of their readings. Future work could help standardize measurement training and assess whether reliability holds for larger groups of readers.
Conflicts of interest
E. Losina is a paid consultant for Lilly/Pfizer and received research support from Samumed. A. F. Chen is a paid consultant for 3M, Avanos, bOne, Convatec, Ethicon, GLG, Guidepoint, Heraeus, IrriMax, PhagoMed, and Stryker; has stock or stock options in bOne, Graftworx, Hyalex, IrriMax, Joint Purification Systems, and Sonoran; received financial support from SLACK Incorporated and UpToDate; is in the editorial board of Journal of Arthroplasty, Annals of Joint, Clinical Orthopaedics and Related Research, Journal of Bone and Joint Infection, Knee Surgery, Sports Traumatology, Arthroscopy, Journal of Bone and Joint Surgery, and Journal of Orthopaedic Research; and is a board member in AAOS, AJRR, AAHKS, European Knee Association, International Congress for Joint Reconstruction, and Musculoskeletal Infection Society. J. N. Katz is the principal investigator of a cohort study of patients with osteoarthritis, funded by Samumed; is the deputy editor for Journal of Bone and Joint Surgery; and is a past president for and in the board of directors of Osteoarthritis Research Society, International. J. K. Lange received royalties from OnPoint Knee, Inc. and SLACK Inc. and is a AAHKS committee member.
Footnotes
One or more of the authors of this paper have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to https://doi.org/10.1016/j.artd.2021.08.015.
Funding
This work was supported by the National Institutes of Health (NIH T32AR055885, P30AR072577, and K24AR057827) and the Scholars in Medicine Office at Harvard Medical School. The funding sources did not play a role in this investigation.
Supplementary data
References
- 1.Bozic K.J., Kurtz S.M., Lau E., Ong K., Vail T.P., Berry D.J. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91(1):128. doi: 10.2106/JBJS.H.00155. [DOI] [PubMed] [Google Scholar]
- 2.Ike H., Dorr L.D., Trasolini N., Stefl M., McKnight B., Heckmann N. Spine-pelvis-hip relationship in the Functioning of a total hip replacement. J Bone Joint Surg Am. 2018;100(18):1606. doi: 10.2106/JBJS.17.00403. [DOI] [PubMed] [Google Scholar]
- 3.McKnight B.M., Trasolini N.A., Dorr L.D. Spinopelvic Motion and Impingement in total hip arthroplasty. J Arthroplasty. 2019;34(7S):S53. doi: 10.1016/j.arth.2019.01.033. [DOI] [PubMed] [Google Scholar]
- 4.Salib C.G., Reina N., Perry K.I., Taunton M.J., Berry D.J., Abdel M.P. Lumbar fusion involving the sacrum increases dislocation risk in primary total hip arthroplasty. Bone Jt J. 2019;101-B(2):198. doi: 10.1302/0301-620X.101B2.BJJ-2018-0754.R1. [DOI] [PubMed] [Google Scholar]
- 5.Blondel B., Schwab F., Patel A. Sacro-femoral-pubic angle: a coronal parameter to estimate pelvic tilt. Eur Spine J. 2012;21(4):719. doi: 10.1007/s00586-011-2061-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ragsdale M.I., Wong F.S., Boutin R.D., Meehan J.P. Pelvic tilt evaluation from Frontal radiographs: the Validity, Interobserver reliability and Intraobserver reproducibility of the sacro-femoral-pubic parameter. J Arthroplasty. 2017;32(5):1665. doi: 10.1016/j.arth.2016.11.026. [DOI] [PubMed] [Google Scholar]
- 7.Vialle R., Levassor N., Rillardon L., Templier A., Skalli W., Guigui P. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am. 2005;87(2):260. doi: 10.2106/JBJS.D.02043. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.