Abstract
Background
Reverse total shoulder arthroplasty (RTSA) has become an increasingly popular surgery for patients with rotator cuff arthropathy, unreconstructible proximal humeral fracture, and end-stage glenohumeral arthritis. The increased annual volume of RTSAs has resulted in more postoperative complications and revision rates between 3.3% and 10.1%. Postoperative infection is one of the most common complications requiring revision surgery after primary RTSA. This study assesses patient-specific risk factors for development of early infection after primary RTSA in a single high-volume shoulder arthroplasty institution.
Methods
From 2014 to 2019, 902 consecutive primary RTSAs were performed for surgical treatment of rotator cuff arthropathy, glenohumeral arthritis, inflammatory arthropathy, and/or dislocation. Excluding proximal humeral or scapula fractures, 756 cases met the inclusion criteria and had a minimum of 3-month follow-up. All surgeries were performed using the same surgical technique and received similar antibiotic prophylaxis. Age, patient demographics, medical history, smoking history, and prior ipsilateral shoulder treatment and/or surgery were recorded. Multivariable logistic regression analysis was used to determine risk factors associated with development of postoperative shoulder infection.
Results
Thirty-five patients did not meet minimum follow-up criteria and were lost to follow-up. Overall, of 721, 22 patients (3%) developed a postoperative ipsilateral shoulder infection. Previous nonarthroplasty surgery and history of rheumatoid arthritis were significantly associated with the development of postoperative shoulder infection. Amongst 196 patients who had previous nonarthroplasty shoulder surgery, there were 12 postoperative shoulder infections (6%) compared with those without previous shoulder surgery (10 of 525, 2%) (P = .003). Among 58 patients with rheumatoid arthritis, there were 5 postoperative shoulder infections (9%) compared with patients without rheumatoid arthritis (17 of 663, 3%) (P = .010). Patient age, gender, smoking status, history of diabetes mellitus, history of cancer/immunosuppression, and prior cortisone injection did not demonstrate significant associations with the development of postoperative infection.
Conclusion
Prior nonarthroplasty shoulder surgery and/or rheumatoid arthritis are independently associated with the development of postoperative infection after primary RTSA. Patients who demonstrate these risk factors should be appropriately evaluated and preoperatively counseled before undergoing primary RTSA. Strong consideration should be given to avoid minimally invasive nonarthroplasty surgery as a temporizing measure to delay definitive RTSA.
Keywords: Reverse total shoulder arthroplasty, postoperative infection, complications, rheumatoid arthritis, risk factors, previous nonarthroplasty surgery, primary arthroplasty
Reverse total shoulder arthroplasty (RTSA) has become an increasingly used surgical treatment option not just for patients with rotator cuff arthropathy, or unreconstructible proximal humeral fracture, but also for patients with primary glenohumeral arthritis.2,4,15,17,19 The increased number of RTSAs performed in the United States each year has also resulted in an increased number of postoperative complications, with incidence of revision surgery ranging from 3.3% to 10.1%.2,3,19 The most common complications requiring revision surgery after primary RTSA are instability and infection.2,4,15,16
Deep and superficial site infections have potentially devastating consequences requiring antibiotics and potential need for debridement, revision, or possible resection surgery. Infection after reverse arthroplasty has been reported at rates between 3.8 and 12%.2,3,6,17,19,24 Primary RTSA has been associated with increased risk of infection vs. primary anatomic total shoulder arthroplasty across small sample size studies. However, the confounding effects of other patient variables such as past medical history, social history, sex, and prior treatment course on this risk of postoperative infection make etiology less clear.3,19,23
The purpose of this retrospective study was to assess patient-specific risk factors for development of early infection after primary RTSA in a single high-volume shoulder arthroplasty institution.
Methods
Between January 2014 and January 2019, the senior author performed 902 consecutive primary RTSAs for the surgical treatment of patients with rotator cuff tear arthropathy, primary glenohumeral arthritis, and/or proximal humeral fracture. During this time period, 756 cases met the inclusion criteria of primary RTSA for glenohumeral osteoarthritis, rotator cuff arthropathy, inflammatory arthropathy, and/or dislocation arthropathy (Fig. 1). Exclusion criteria included patients undergoing RTSA for proximal humerus fracture or other shoulder fractures (glenoid, scapula) and a minimum clinical follow-up of 3 months. Minimum duration was defined as 3 months, as acute perioperative infections can occur up to 3 months from date of index surgery.9
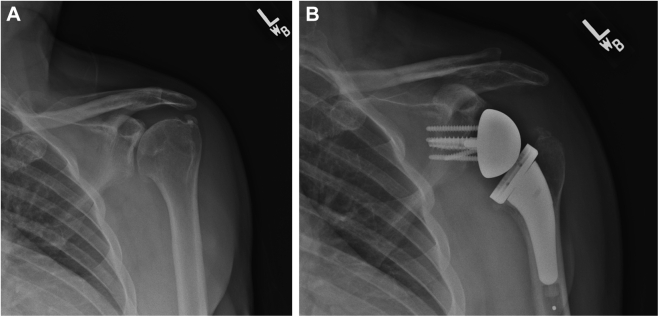
Figure 1.
66-year-old man with end-stage osteoarthritis underwent uneventful RTSA with glenoid bone grafting. (A) Preoperative. (B) Postoperative. RTSA, reverse total shoulder arthroplasty.
Electronic medical records were surveyed to collect patient demographics including age, gender, medical history, smoking history, shoulder laterality, and any treatment before primary RTSA—including any ipsilateral shoulder corticosteroid injection and/or soft-tissue (nonarthroplasty) shoulder surgery. All patients underwent the same surgical technique for primary RTSA using the same surgical approach, the same cementless humeral and glenoid components, and the same antibiotic prophylaxis with combined preoperative 3rd-generation cephalosporin and vancomycin antibiotics—both of which were continued for 24 hours postoperatively based on pharmacologic dosing guidelines.
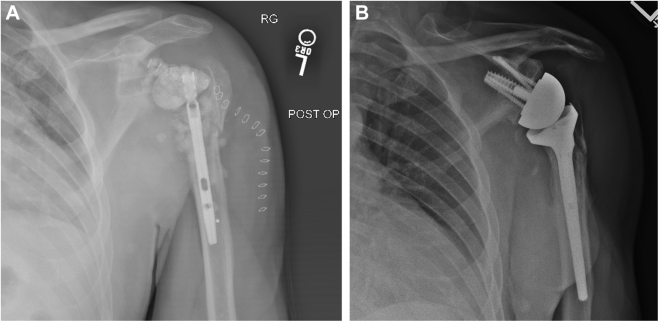
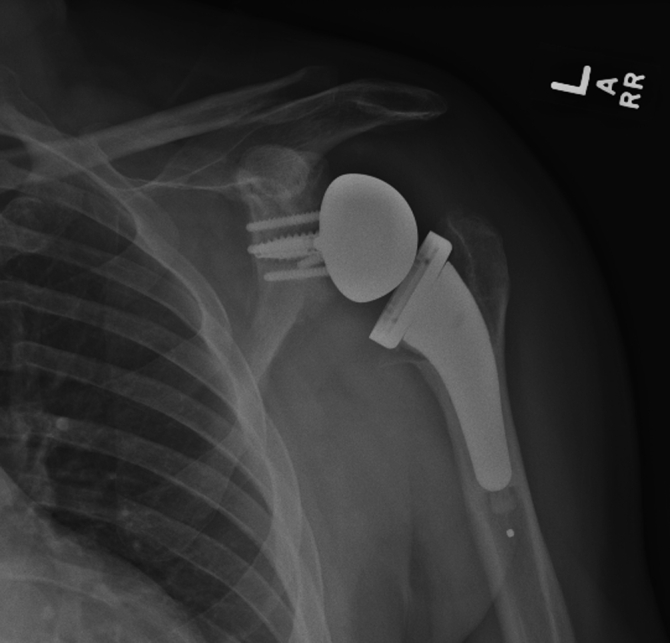
Institutional review board approval was obtained, and two independent investigators performed a retrospective chart review of all patients. Postoperative clinical course was followed across all patients for the incidence of either superficial or deep postoperative shoulder infection.9,12 Postoperative presentation of fevers, wound complications, erythema, induration, insidious shoulder pain, or radiographic progression of osteolysis were identified with high index of suspicion for infection (Fig. 2). If suspected, serum laboratory studies, computed tomography aspiration, and culture were performed. Prosthetic shoulder infection was ultimately diagnosed using major and minor criteria updated by the Musculoskeletal Infection Society in 2011.25 Any shoulders with equivocal but concerning criteria for periprosthetic joint infection were treated as infections with two-stage revision shoulder arthroplasty (Fig. 3).
Figure 2.
X-ray obtained at 2 years postoperatively shows proximal humeral bone resorption and prosthetic loosening.
Figure 3.
Two-stage revision was performed. First stage includes implant removal, antibiotic spacer placement, and IV antibiotics for 6 weeks. (A) Once infection is cleared, second stage is performed, which includes spacer removal and revision RTSA (B). RTSA, reverse total shoulder arthroplasty.
Patient characteristics and risk factors were summarized by mean and standard deviation or medians with interquartile range for continuous variables, while categorical variables by frequencies and percentage. Differences between those that developed infection vs. those that did not were compared by Student’s t-test or Mann-Whitney U test for continuous variables, while Pearson chi-square or Fisher’s exact test were used for categorical variables.
Multivariable logistic regression analysis was used to determine risk factors associated with development of shoulder infection. Backward step-by-step variable selection was implemented until final model was achieved, which was found to be parsimonious and had very good discriminative ability with c-statistics of 0.78. All analyses were performed with R, version 4.0.3 (http://www.r-project.org/) statistical software. P value < .05 was considered statistically significant.
Results
Detailed patient demographics are illustrated in Table I. There were 35 patients lost to follow-up with less than 3 months of follow-up. Overall, 22 of 721 patients (3%) developed a postoperative ipsilateral shoulder infection. Patient age, gender, smoking status, history of diabetes mellitus, and/or history of cancer/immunosuppression did not demonstrate significant associations with the development of postoperative infection.
Table I.
Cohort demographics.
| Patient demographics | Total (N = 721) | |
|---|---|---|
| Mean age (yr) | 70 | Range (39-92) |
| Mean follow-up (mo) | 18 | Range (1-76) |
| Gender | M 365 (51%) | F 356 (49%) |
| Comorbidities | Yes | No |
| Diabetes mellitus | 135 (19%) | 586 (81%) |
| Rheumatoid arthritis | 58 (8%) | 663 (92%) |
| Smoking | 37 (5%) | 684 (95%) |
| Cancer/Immunosuppression | 180 (25%) | 541 (75%) |
| Previous surgery | 196 (27%) | 525 (73%) |
| Corticosteroid injections | 510 (71%) | 211 (29%) |
Both previous nonarthroplasty surgery and history of rheumatoid arthritis were significantly associated with the development of postoperative shoulder infection. One hundred ninety-six patients (27%) in the overall study group reported a history of prior ipsilateral nonarthroplasty shoulder surgery. In this subgroup, there were 12 postoperative shoulder infections (12 of 196, 6%) compared with 10 infections in shoulders without previous surgery (10 of 525, 2%) (P = .004). Patients with previous surgery had 2.7 times higher odds of developing infection as compared those without previous surgery (odds ratio, 95% confidence interval = 2.67 [1.07, 6.76]).
Fifty-eight patients (8%) in the overall study group reported a medical history of rheumatoid arthritis. In this subgroup of 58 patients, 5 (9%) developed postoperative shoulder infections. This was statistically significant when compared with the 17 patients without rheumatoid arthritis who had a postoperative infection (17 of 663, 3%) (P = .009). Patients with rheumatoid arthritis had 3.5 times higher odds of developing infection as compared with patients without rheumatoid arthritis (odds ratio, 95% confidence interval = 3.45 [1.04, 9.09]).
There were 17 cases of infections in patients who had corticosteroid injections before primary RTSA (17 of 510, 3%). This did not demonstrate statistical significance when compared with the patients who did not have previous corticosteroid injections (5 of 211 or 2%, P = .521).
Discussion
Periprosthetic infection represents a potentially devastating complication after primary RTSA and often requires extensive treatment, including intravenous antibiotics, debridement, and/or revision arthroplasty. As such, it is important to identify preoperative risk factors that may increase infection risk and counsel patients accordingly. In this single-institution single-surgeon cohort, we identified an overall postoperative infection rate of 3%, which is consistent with rates reported across the peer-reviewed literature.2,3,6,17,19,24 However, our study demonstrated that prior nonarthroplasty shoulder surgery and/or rheumatoid arthritis are statistically significant independent risk factors contributing to early postoperative infection after RTSA.
Other studies have evaluated the association of comorbidities and postoperative RTSA infection. While little correlation has been shown comparing age, gender, hypertension, and/or cardiac disease with postoperative infection, some studies have found a higher risk of postoperative infection in patients with higher body mass index,18 diabetes,14 and/or smoking history.1,11 In our study, we did not identify an association with any medical comorbidity other than rheumatoid arthritis. Similarly, Cho et al6 performed a systematic review of RTSA in patients with rheumatoid arthritis and described complications in nearly 1 in 5 patients. Four infections were reported across 123 cases and were responsible for approximately 15% of overall adverse outcomes. Guery et al10 also presented 8 cases of infection after RTSA in patients with rheumatoid arthritis, who required the highest rates of revision surgery in their study population. Given these current findings, we would recommend a heightened index of suspicion of postoperative infection in patients with rheumatoid arthritis who complain of persistent unexplained shoulder pain postoperatively. The risk of infection in this patient population may be complicated by the management of their steroid use or disease-modifying antirheumatoid drugs. At our institution, we routinely involve rheumatologists in this decision-making process, which minimizes the bias of the surgeon regarding the discontinuation and resumption of these medications postoperatively.
Traditional orthopedic teaching preaches maximizing conservative management for large joint arthritis patients before definitive joint arthroplasty. Patients often undergo corticosteroid injection management and even arthroscopic debridement procedures before their final arthroplasty treatment. In the hip and knee literature, there are recent reports of increased postoperative infections associated with arthroplasty and prior corticosteroid injections .5,13,16,20 Furthermore, Werner et al21 evaluated 8420 patients with shoulder arthroplasty and found an increased incidence of infection in those who had received a corticosteroid injection within 3 months of surgery. In our study, we did not find a similar association between prior corticosteroid injection and postoperative infection; however, in comparison, our cohort is smaller and may be limited in power. Owing to the tertiary nature of the practice, we routinely encounter patients who had failed multiple cortisone injections before their presentation. We were unable to accurately identify the timing of their prior injections and, hence, unable to detect the impact of the corticosteroid injections on infection risk.
When evaluating the impact of prior non-arthroplasty surgery on infection risk, there are conflicting data in the literature. Frank et al8 prospectively evaluated 506 patients who underwent shoulder arthroplasty, 28% of whom had undergone previous procedures on the ipsilateral shoulder. The rate of minor complications was increased in the previous surgery group, but there was no difference between the two groups in major complications, including infection and revision surgery.8 Conversely, in a retrospective review of 464 RTSAs, Florschütz et al7 found that previously operated-on shoulders undergoing RTSA demonstrated a significantly higher infection rate compared than native shoulders. Moreover, Werthel et al22 evaluated 4577 patients who underwent anatomic, hemiarthroplasty, or reverse shoulder arthroplasty and found a significant increase in periprosthetic infections in those with a history of prior ipsilateral nonarthroplasty surgery. In our cohort, we similarly found a 3-fold higher risk of infection associated with history of shoulder surgery (6% vs. 2%) (Table II). This is consistent with the infection risk associated with prior shoulder surgery as reported by others, including Malik et al26 and Wright-Chisem et al.7,22,27 This statistically significant finding cautions against using nonarthroplasty surgery as a temporizing option before primary RTSA.
Table II.
Risk factors associated with development of postoperative shoulder infection.
| Demographic risk factors | Presence of infection |
P value | Post-hoc power | |
|---|---|---|---|---|
| Yes (N = 22) | No (N = 699) | |||
| Mean age (yr) | 66 | 70 | .047 | NA |
| Range (54-84) | Range (39-92) | |||
| Mean follow-up (mo) | 26 | 17 | .002 | NA |
| Range (1-64) | Range (3-76) | |||
| Gender | .709 | 6.8% | ||
| F | 10 (3%) | 346 (97%) | ||
| M | 12 (3%) | 353 (97%) | ||
| Diabetes mellitus | .947 | 5.3% | ||
| Yes | 4 (3%) | 131 (97%) | ||
| No | 18 (3%) | 568 (97%) | ||
| Rheumatoid arthritis | .010 | 28.6% | ||
| Yes | 5 (9%) | 53 (91%) | ||
| No | 17 (3%) | 646 (97%) | ||
| Smoking | .899 | 6.8% | ||
| Yes | 1 (3%) | 36 (97%) | ||
| No | 21 (3%) | 663 (97%) | ||
| Cancer/immunosuppression | .212 | 33.3% | ||
| Yes | 3 (2%) | 177 (98%) | ||
| No | 19 (4%) | 522 (96%) | ||
| Corticosteroid injections | .494 | 6.5% | ||
| Yes | 17 (3%) | 493 (97%) | ||
| No | 5 (2%) | 206 (98%) | ||
| Previous surgery | .003 | 67.3% | ||
| Yes | 12 (6%) | 184 (94%) | ||
| No | 10 (2%) | 515 (98%) | ||
Furthermore, when evaluating patients with previous nonarthroplasty procedures, it is advisable to include a full workup for subclinical infection before proceeding with primary RTSA—despite the benign clinical appearance of any scars or prior “minimally invasive” arthroscopic surgeries.
There are several limitations to this study. First, clinical follow-up is admittedly short term, and other associations with postoperative infection may develop with a longer-term follow-up. Second, as a retrospective cohort study, the study design was unable to capture all potential demographic or medical comorbid cofounders, including type of rheumatoid medications, overall health severity (Charlson comorbidity index), or nutritional impact to overall infection risk. Third, the incidence rate of shoulder infections in our study was very low. Therefore, the sample size for certain previously described infection risk factors (body mass index, diabetes, smoking, and so on) in our cohort may be too small to detect statistical significance. However, we reported an infection incidence rate similar to those published in other shoulder surgery literature. 2,3,19 Database studies with large enough sample sizes may be able to detect other significant risk factors; however, they may have other uncontrollable confounders across surgeons/institutions. The strengths of this study include an overall large consecutive sample size, uniform treatment by one surgeon using one technique and one implant, and prospectively collected postoperative data allowing for detailed retrospective evaluation.
Conclusion
Prior nonarthroplasty shoulder surgery and/or rheumatoid arthritis are independently associated with the development of postoperative infection after primary RTSA. Patients who demonstrate these risk factors should be appropriately evaluated and preoperatively counseled before undergoing primary RTSA. Furthermore, in light of the increased infection risk, strong consideration should be given by both physician and patient to avoiding minimally invasive nonarthroplasty shoulder surgery as a temporizing measure to delay definitive primary RTSA.
Disclaimers
Funding: No funding was disclosed by the author(s).
Conflict of interest: Sumant G. Krishnan discloses the following potential conflicts of interest of being a committee member in the Arthroscopy Association of North America; a committee member in American Shoulder and Elbow Surgeons; an editorial board member in the Journal of Bone and Joint Surgery; an editorial board member in the Journal of Shoulder and Elbow Surgery; an editorial board member in the Journal of American Academy of Orthopaedic Surgeons; recieved royalties from TAG Medical; recieved publishing royalties from Wolters Kluwer; a consultant in and recieved royalties from Wright Medical Technology, Inc.; a consultant in DJO Global.
The other authors, their immediate families, and any research foundation with which they are affiliated, have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Acknowledgments
The authors express their sincere appreciation and gratitude to Dr. Gerald O. Ogola of the Baylor Scott & White Research Institute, Dallas, TX, for his expertise in preparing the biostatistical analysis on this project. Investigation was performed at The Shoulder Center, Baylor University Medical Center, Dallas, TX, USA.
Footnotes
This study was approved by the Baylor Scott & White Research Institute IRB (study no. 017-084).
References
- 1.Althoff A.D., Reeves R.A., Traven S.A., Wilson J.M., Woolf S.K., Slone H.S. Smoking is associated with increased surgical complications following total shoulder arthroplasty: an analysis of 14,465 patients. J Shoulder Elbow Surg. 2020;29:491–496. doi: 10.1016/j.jse.2019.07.012. [DOI] [PubMed] [Google Scholar]
- 2.Black E.M., Roberts S.M., Siegel E., Yannopoulos P., Higgins L.D., Warner J.J.P. Failure after reverse total shoulder arthroplasty: what is the success of component revision? J Shoulder Elbow Surg. 2015;24:1908–1914. doi: 10.1016/j.jse.2015.05.029. [DOI] [PubMed] [Google Scholar]
- 3.Boileau P. Complications and revision of reverse total shoulder arthroplasty. Orthop Traumatol Surg Res. 2016;102:S33–S43. doi: 10.1016/j.otsr.2015.06.031. [DOI] [PubMed] [Google Scholar]
- 4.Botros M., Curry E.J., Yin J., Jawa A., Eichinger J.K., Li X. Reverse shoulder arthroplasty has higher perioperative implant complications and transfusion rates than total shoulder arthroplasty. JSES open access. 2019;3:108–112. doi: 10.1016/j.jses.2019.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cancienne J.M., Werner B.C., Luetkemeyer L.M., Browne J.A. Does timing of previous intra-articular steroid injection Affect the Post-Operative rate of infection in total knee arthroplasty? J Arthroplasty. 2015;30:1879–1882. doi: 10.1016/j.arth.2015.05.027. [DOI] [PubMed] [Google Scholar]
- 6.Cho C.-H., Kim D.-H., Song K.-S. Reverse shoulder arthroplasty in patients with rheumatoid arthritis: a systematic review. Clin Orthop Surg. 2017;9:325–331. doi: 10.4055/cios.2017.9.3.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Florschütz A.V., Lane P.D., Crosby L.A. Infection after primary anatomic versus primary reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2015;24:1296–1301. doi: 10.1016/j.jse.2014.12.036. [DOI] [PubMed] [Google Scholar]
- 8.Frank R.M., Lee S., Sumner S., Griffin J., Leroux T., Verma N.N. Shoulder arthroplasty outcomes after prior non-arthroplasty shoulder surgery. JB JS open access. 2018;3:e0055. doi: 10.2106/JBJS.OA.17.00055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Garrigues G.E., Zmistowski B., Cooper A.M., Green A., Hsu J., Ricchetti E. Proceedings from the 2018 International Consensus meeting on orthopedic infections: the definition of periprosthetic shoulder infection. J Shoulder Elbow Surg. 2019;28:S8–S12. doi: 10.1016/j.jse.2019.04.034. [DOI] [PubMed] [Google Scholar]
- 10.Guery J., Favard L., Sirveaux F., Oudet D., Mole D., Walch G. Reverse total shoulder arthroplasty. Survivorship analysis of eighty replacements followed for five to ten years. J Bone Joint Surg Am. 2006;88:1742–1747. doi: 10.2106/JBJS.E.00851. [DOI] [PubMed] [Google Scholar]
- 11.Hatta T., Werthel J.D., Wagner E.R., Itoi E., Steinmann S.P., Cofield R.H. Effect of smoking on complications following primary shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:1–6. doi: 10.1016/j.jse.2016.09.011. [DOI] [PubMed] [Google Scholar]
- 12.Nelson G.N., Davis D.E., Namdari S. Outcomes in the treatment of periprosthetic joint infection after shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg. 2016;25:1337–1345. doi: 10.1016/j.jse.2015.11.064. [DOI] [PubMed] [Google Scholar]
- 13.Papavasiliou A.V., Isaac D.L., Marimuthu R., Skyrme A., Armitage A. Infection in knee replacements after previous injection of intra-articular steroid. J Bone Jt Surg - Ser B. 2006;88:321–323. doi: 10.1302/0301-620X.88B3.17136. [DOI] [PubMed] [Google Scholar]
- 14.Rao A.J., Yeatts N.C., Reid R.T., Trofa D.P., Scarola G., Schiffern S.C. Is postoperative glucose variability associated with adverse outcomes following shoulder arthroplasty? J Shoulder Elbow Surg. 2021;30:616–624. doi: 10.1016/j.jse.2020.07.005. [DOI] [PubMed] [Google Scholar]
- 15.Scarlat M.M. Complications with reverse total shoulder arthroplasty and recent evolutions. Int Orthop. 2013 May;37:843–851. doi: 10.1007/s00264-013-1832-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schairer W.W., Nwachukwu B.U., Mayman D.J., Lyman S., Jerabek S.A. Preoperative hip injections increase the rate of periprosthetic infection after total hip arthroplasty. J Arthroplasty. 2016;31:166–169.e1. doi: 10.1016/j.arth.2016.04.008. [DOI] [PubMed] [Google Scholar]
- 17.Somerson J.S., Hsu J.E., Neradilek M.B., Matsen F.A., 3rd Analysis of 4063 complications of shoulder arthroplasty reported to the US Food and Drug Administration from 2012 to 2016. J Shoulder Elbow Surg. 2018;27:1978–1986. doi: 10.1016/j.jse.2018.03.025. [DOI] [PubMed] [Google Scholar]
- 18.Theodoulou A., Krishnan J., Aromataris E. Risk of complications in patients who are obese following upper limb arthroplasty: a systematic review and meta-analysis. Obes Res Clin Pract. 2020;14:9–26. doi: 10.1016/j.orcp.2020.01.001. [DOI] [PubMed] [Google Scholar]
- 19.Villacis D., Sivasundaram L., Pannell W.C., Heckmann N., Omid R., Hatch G.F.R., 3rd Complication rate and implant survival for reverse shoulder arthroplasty versus total shoulder arthroplasty: results during the initial 2 years. J Shoulder Elbow Surg. 2016;25:927–935. doi: 10.1016/j.jse.2015.10.012. [DOI] [PubMed] [Google Scholar]
- 20.Werner B.C., Cancienne J.M., Browne J.A. The timing of total hip arthroplasty after Intraarticular hip injection affects postoperative infection risk. J Arthroplasty. 2016;31:820–823. doi: 10.1016/j.arth.2015.08.032. [DOI] [PubMed] [Google Scholar]
- 21.Werner B.C., Cancienne J.M., Burrus M.T., Griffin J.W., Gwathmey F.W., Brockmeier S.F. The timing of elective shoulder surgery after shoulder injection affects postoperative infection risk in Medicare patients. J Shoulder Elbow Surg. 2016;25:390–397. doi: 10.1016/j.jse.2015.08.039. [DOI] [PubMed] [Google Scholar]
- 22.Werthel J.-D., Hatta T., Schoch B., Cofield R., Sperling J.W., Elhassan B.T. Is previous nonarthroplasty surgery a risk factor for periprosthetic infection in primary shoulder arthroplasty? J Shoulder Elbow Surg. 2017;26:635–640. doi: 10.1016/j.jse.2016.10.020. [DOI] [PubMed] [Google Scholar]
- 23.Zavala J.A., Clark J.C., Kissenberth M.J., Tolan S.J., Hawkins R.J. Management of deep infection after reverse total shoulder arthroplasty: a case series. J Shoulder Elbow Surg. 2012;21:1310–1315. doi: 10.1016/j.jse.2011.08.047. [DOI] [PubMed] [Google Scholar]
- 24.Zumstein M.A., Pinedo M., Old J., Boileau P. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg. 2011;20:146–157. doi: 10.1016/j.jse.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 25.Parvizi J., Zmistowski B., Berbari E.F., Bauer T.W., Springer B.D., Della Valle C.J., Garvin K.L., MontMA, Wongworawat M.D., Zalavras C.G. New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal infection Society. Clin Orthop Relat Res. 2011;469:2992–2994. doi: 10.1007/s11999-011-2102-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Malik A.T., Morris J., Bishop J.Y., Neviaser A.S., Khan S.N., Cvetanovich G.L. Undergoing an arthroscopic procedure prior to shoulder arthroplasty is associated with Greater risk of prosthetic joint infection. Arthroscopy. 2021;37:1748–1754.e1. doi: 10.1016/j.arthro.2021.01.013. [DOI] [PubMed] [Google Scholar]
- 27.Wright-Chisem J., Apostolakos J.M., Dines J.S., Dines D.M., Gulotta L.V., Taylor S.A., Werner B.C. The impact of prior ipsilateral arthroscopy on infection rates after shoulder arthroplasty. J Shoulder Elbow Surg. 2021;30:1596–1602. doi: 10.1016/j.jse.2020.09.019. [DOI] [PubMed] [Google Scholar]