Abstract
Background
Although being the historical gold standard for rotator cuff repair, open transosseous (TO) repair was largely replaced by anchor-based methods with the advent of arthroscopic surgery owing to their comparative ease of use. However, suture anchors are at risk of dislodgement, especially among older patients, who have more osteopenic bone or those presenting large tears. Considering the ever-increasing active life expectancy and associated increased quality of life expectations by older generations, the need to offer safe and efficient surgical treatments to these patients imposes itself. Arthroscopic TO repairs would combine the best of both worlds and be well adapted to these populations. The primary objective of this study was to evaluate the functional outcome and complication rate of the TO arthroscopic repair technique when using a 2-mm braided suture tape. The secondary objective of this study was to assess functional outcome of TO repair in older patients and patients with >3-cm tears.
Methods
One hundred thirty-seven consecutive patients with full-thickness rotator cuff tear who underwent arthroscopic TO (anchorless) rotator cuff repair between January 2011 and December 2013 were reviewed. The surgery was performed by a single surgeon with a reusable curved suture passer and 2-mm braided tape suture. Follow-up was 3 to 5 years (mean = 50 months). All patients underwent preoperative and postoperative functional assessments (American Shoulder and Elbow Surgeons and Quick Dash) and were questioned with their overall satisfaction.
Results
Thirty-eight (28%) of the 137 patients were 65 years and older, and 62 (45%) had a large or massive tear. One patient (0.7%) had early retear at the suture-tendon interface after trauma 3 weeks postoperatively. The average Quick Dash score improved by 55.6 points and the average American Shoulder and Elbow Surgeons score improved by 69.7 points 3.5 and 6.3 times their minimal clinically important differences, respectively. There was no significant difference in final functional outcomes between patients 65 years and older and younger patients or between patients with large and massive (>3 cm) and smaller tears (≤3 cm). Mean operative time was 68 min ± 16.
Conclusions
Arthroscopic TO repair using a 2-mm tape material has achieved significant mid-term functional improvement, with results statistically unaffected by larger tear size (>3 cm) or older age (≥65 years).
Keywords: Rotator cuff repair, Transosseous, Shoulder arthroscopy, 2-mm tape suture
The open transosseous (TO) technique of rotator cuff tears has been the historical gold standard for rotator cuff repair, offering the best healing environment for the repaired tendons (compression in a large vascularized footprint area).22,30 It has more recently been overtaken by arthroscopic anchor-assisted technique, with studies describing comparable clinical results, equal or lower complication rates, and an overall improvement of patient satisfaction.8 Despite their popularity, anchors present the unfortunately poorly quantified risk of pullout4 which increases with larger tear and in elderly populations (>65 years),9,11,21 two significantly overlapping populations16 historically considered poorer surgical candidates.19,20 However, increasingly active older individuals trigger the need for orthopedic care that will restore and support their high functioning lifestyles.
Combining arthroscopy with the TO technique would theoretically combine the best of both worlds.24 So far, it has not garnered many followers owing to a lack of intuitive instrumentation and the fear of TO suture cutting through bone,18 resulting in perioperative failures. Despite this issue, biomechanical studies have compared the initial strength and cyclic load of the TO technique to the suture anchors technique, finding similar results, and some even found the TO repair to be superior.25,26,29 However, some clinical studies on arthroscopic TO repair have reported perioperative bone complications (tunnel failure) with the use of modern No 2 wire sutures, a problem more likely to occur when operating on weaker osteoporotic bone. To overcome that obstacle, some authors have advocated for tunnel augmentation with small cylindrical implants.5,15 Other authors advocate the use of a wider suture, such as a 2-mm tape, instead of the thinner No 2 wire to prevent bone cutting.6 Such a tape would provide equal force but less pressure at the contact area, thanks to a wider contact surface with the bone and soft tissue, as well as optimal viscoelastic properties.28
The primary purpose of this study was to evaluate the functional outcome and complication rate of the TO arthroscopic repair technique when using a 2-mm braided suture tape.
The secondary objectives were to assess functional outcome of TO repair in older patients and patients with >3-cm tears.
Materials and methods
During a 36-month period, between January 2011 and December 2013, there were 206 consecutive arthroscopic TO repairs with a 2-mm tape by the same senior surgeon, in a private facility.
Inclusion criteria were that all patients had preoperative documented radiologic imaging (by ultrasound or magnetic resonance imaging) of full-thickness rotator cuff tear involving the supraspinatus, infraspinatus, or both. Each patient was evaluated preoperatively by the same surgeon, who completed the history, a physical examination, and a functional assessment using the American Shoulder and Elbow Surgeons (ASES) score and QuickDASH.
Exclusion criteria were previous shoulder fracture, presence of arthritis or osteoarthritis, previous infection, subscapularis tear Lafosse class III, IV or V, recent chemotherapy or radiotherapy, and chronic steroid use. Using these criteria, the authors excluded 37 patients of the 206 initial patients, for a final cohort of 169 patients for our study.
Of these 169 patients, the research team was able to reach 137 (81%) for follow-up questionnaires and assessment, all of them having a postoperative period of more than 3 years.
Surgical technique
All patients were operated in a beach chair position, under regional interscalene block alone (no general anesthesia). A pressure pump and an articulated arm holder (Tenet Spyder, Smith and Nephew Inc. Fort Worth, TX, USA) were used for all cases.
After routine glenohumeral diagnostic arthroscopy, a bursectomy, cuff debridement and acromioplasty were performed for all patients. Subscapularis repair and long biceps tenotomy or tenodesis were done as needed, using 5.5-mm PEEK suture anchors. Supraspinatus and infraspinatus inspection and palpation were completed to assess tear size and mobilization pattern, in preparation for a repair. Marginal convergence repair using No 2 sutures (Ultrabraid, Smith and Nephew Inc. Fort Worth, TX, USA or Fiberwire, Arthrex Inc. Naples, FL, USA) was performed as needed for L-shape or U-shaped tears, before final tendon to bone repair. The greater tuberosity was abraded with the shaver until bleeding bone was reached, while taking precautions not to damage cortex integrity.
Bone tunnels in the greater tuberosity were created as follows:
-
1.
The superior greater tuberosity was penetrated with a 4-mm manual straight awl, directed 45 degrees obliquely, close to the articular cartilage, at 1, 2, or 3 sites depending on the number of tunnels needed.
-
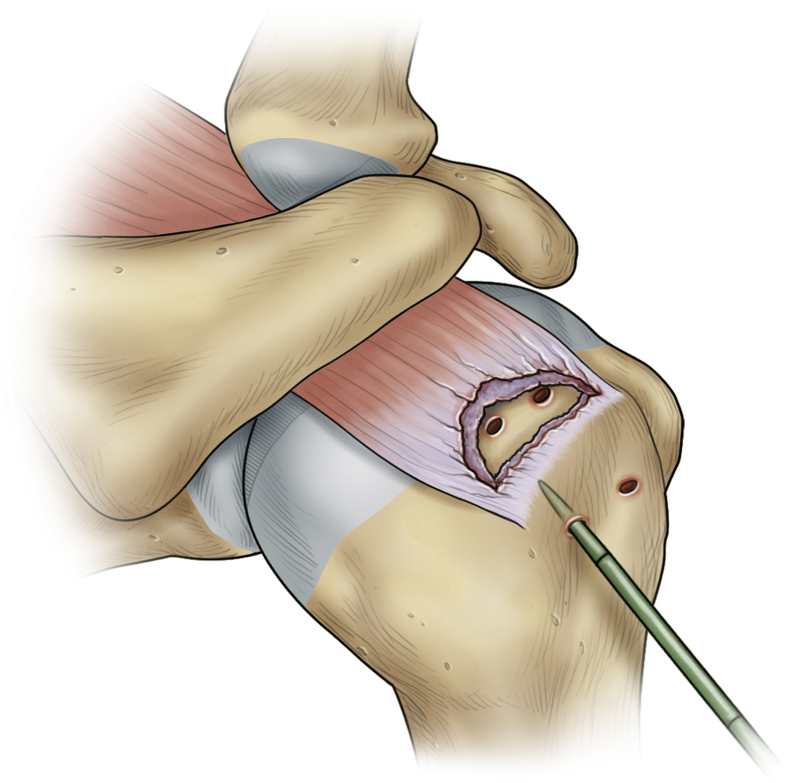
2.
The straight awl was used to perforate the lateral humeral cortex 10 to 15 mm lower than the apex of the greater tuberosity (Fig. 1).
-
3.
A curved manual reusable sharp awl was introduced in the distal hole to connect with the corresponding superior hole.
Figure 1.
The straight awl perforating the lateral humeral cortex.
Tendon repair was performed as follows:
-
1.
A similarly curved fenestrated awl was used to transport the loaded 2 mm tape (Arthrex Inc. Naples, FL) through the bone tunnel from the distal entry to the superior exit.
-
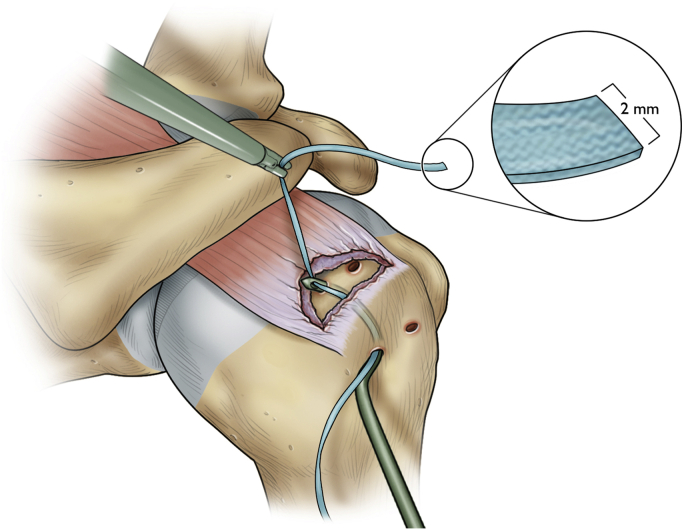
2.
The suture was grasped at the superior (subacromial) exit hole and pulled through (Fig. 2).
-
3.
The solidity of the bone tunnel was manually assessed by pulling strongly on the tape loop.
-
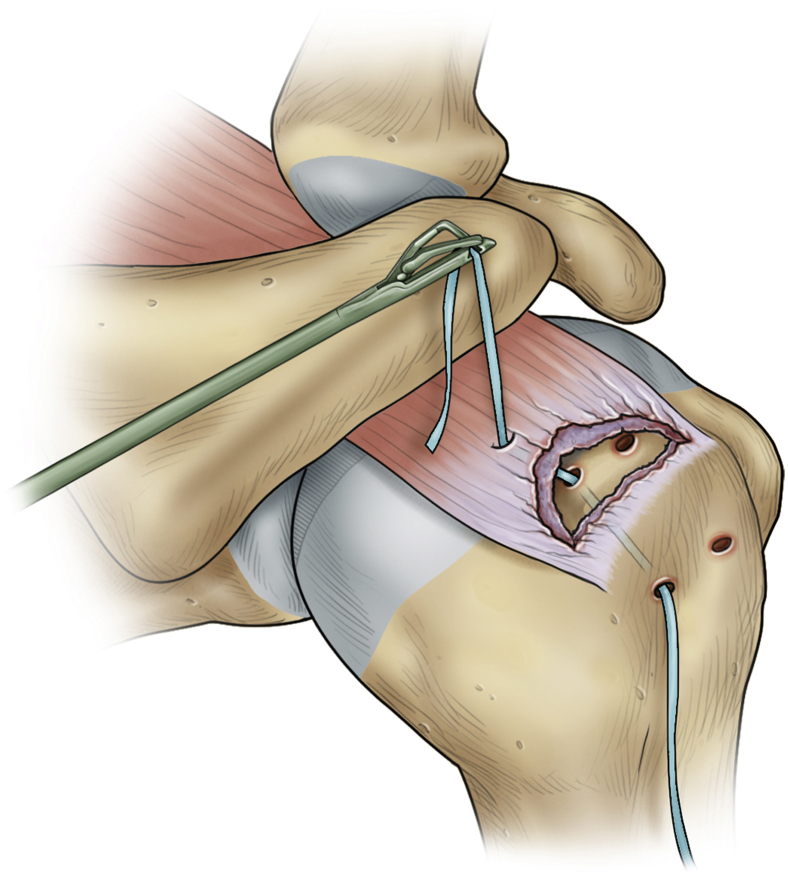
4.
Passing the tape through the tendon stump was achieved with a commercial passing device (Viper or Scorpion, Arthrex Inc. Naples, FL, USA) (Fig. 3).
-
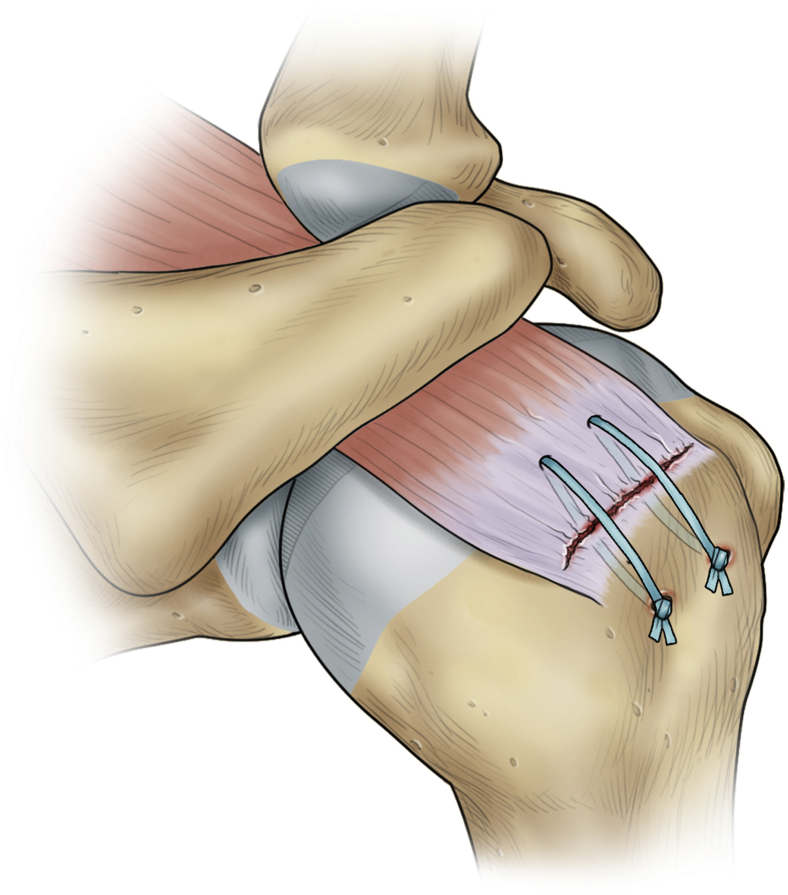
5.
A regular arthroscopic knot-tying technique was used. During the final tie, migration and compression on the footprint could be observed, and the knot was carefully placed within the distal humeral hole (Fig. 4). If more than one tunnel was used, all sutures had to be passed before tying.
-
6.
Releasing the arm holder, passive mobilization was assessed to confirm the solidity of the repair, as well as the absence of knot impingement in the subacromial space.
Figure 2.
2-mm tape suture being pulled through.
Figure 3.
Passing the tape through the tendon stump.
Figure 4.
Knot placed within the distal humeral hole.
Postoperatively, a short (1-2 weeks) sling immobilization was prescribed, with rapid pendulum exercises to be started as tolerated. However, in cases of large or massive tears, six weeks of sling immobilization was recommended. Physiotherapy with a progressive strengthening program was started for all patients at 12 weeks postoperatively.
Postoperative visits were scheduled at 2 weeks, 2 months, 4 months, and 6 months for all patients. All patients were discharged 6 to 9 months postoperatively.
Postoperative outcome evaluation
More than three years after completion of the clinical series, all charts were reviewed to verify inclusion and exclusion criteria and validate data completeness. An independent clinical research assistant, trained for functional outcome assessments, questioned all patients by telephone, using the ASES and QuickDASH scales, and completed the data with specific questions related to overall patient satisfaction. This research assistant was blinded to the preoperative clinical and radiologic information, the operative findings and postoperative physical examinations.
The complications considered were perioperative tunnel failure, surgical site infection, neurovascular compromise, stiffness, and further revision surgery.
Statistical analysis
The preoperative vs. postoperative outcome score results (ASES and QuickDASH) were compared with a paired Student t-test. A P value < .05 was considered statistically significant. The authors specifically compared results as per patient age and perioperative size of the tear, using the age of 65 years as a cutoff to determine groups. “Large (3-4 cm) and massive (>4 cm) tears” were compared with “small (<1.5 cm) and medium (1.5-3 cm) size tears,” using 3 cm as the cutoff value. For these analyses, with unequal sample sizes and non-normal distributions, the authors used the Mann-Whitney U test, with a P value <.05 considered to be significant. Results are given as values (95% confidence interval).
Results
Patient population
Of the initial cohort of 169 patients, 137 (81%) were available for follow-up questionnaires and assessment. They all had a postoperative follow-up of 3 years or more. Mean follow-up was 50 months. Of the 137 patients, 93 were men (68%) and 44 women (32%). The mean age was 59.0 years, ranging from 32 to 80. One hundred thirty-one (96%) patients had surgery for primary tears, and 6 (4%) were revisions.
All were contacted by phone for questioning by the independent research assistant. Demographic features of the study sample are summarized in Table I, as well as operative observations and procedures.
Table I.
Intraoperative findings and additional procedures performed.
| Characteristic | Value (percentage) |
|---|---|
| Patients, No | 137 |
| Age, average (range) | 59 (32-80) |
| Sex, male-female No | 93-44 |
| Primary vs. revision | |
| Primary | 131 |
| Revision | 6 |
| Number of 2-mm tapes per case | |
| 1 | 73 (53.3%) |
| 2 | 60 (43.8) |
| 3 | 4 (2.9%) |
| Number of patients with marginal convergence suture | 87 (63.5%) |
| Biceps tenotomy or tenodesis | 33 (24.1%) |
| Synovectomy | 4 (2.9%) |
| Capsule release | 6 (4.4%) |
| Subscapular tear | 16 (11.7%) |
| Suprastinatus-infraspinatus tear size | |
| <1 cm | 16 (11.5%) |
| 1-3 cm | 59 (43.5%) |
| >3 cm | 62 (45%) |
All 137 tears were of full thickness, involving the supraspinatus and/or infraspinatus tendons. All tears were amenable to complete anatomic repair (no partial repairs were performed). Ten patients presented a class I or II superior subscapularis tear, and 33 patients had a significant long biceps tear or intra-articular partial dislocation. Subscapularis repairs and/or long biceps tenodesis were performed using 5.5-mm PEEK suture anchors (Twinfix, Smith and Nephew, Fort Worth, TX, USA).
The mean operating time was 68 minutes (36.6-99.4).
Functional outcome
Table II summarizes the functional outcome results for the entire cohort. Overall, there was a marked and significant (P < .05) difference between the preoperative and the postoperative values for both ASES and QuickDASH scores. Table III, Table IV present the functional results as per tear size and age, respectively. For the group presenting large and massive tears (>3 cm), there was an average postoperative ASES score of 90.9 points, which is slightly less than the one observed for the group presenting small and medium sized tears (93.0 points). This difference was statistically significant, P = .029. However, there was no statistically significant difference in postoperative vs. preoperative improvement for both ASES and QuickDASH scores when comparing the large and massive tear group vs. the small and medium tear group (P = .68 and 0.59). The same was true for the older patient group (≥65 years) vs. the younger group (<65 years), with no significant differences in their postoperative functional results or postoperative vs. preoperative improvement (for both ASES and QuickDASH).
Table II.
Preoperative vs. postoperative functional results for the total sample (n = 137).
| Characteristic | Before surgery | After surgery | Improvement | P value |
|---|---|---|---|---|
| ASES value | 22.4 | 92.1 | 69.7 (67.4-72.6) | <.001 |
| (mean; 95% CI) | (0-50.0) | (70.2-100) | ||
| QuickDASH value | 59.0 | 3.4 | 55.6 (52.3-58.9) | <.001 |
| (mean; 95% CI) | (19.4-100) | (0-16.3) |
ASES, American Shoulder and Elbow Surgeons; CI, confidence interval.
Table III.
Preoperative vs. postoperative functional results, as per size of tear.
| Size of tear | ASES |
QuickDASH |
||||
|---|---|---|---|---|---|---|
| ≤3 cm (n = 75) |
>3cm (n = 62) |
P value | ≤3 cm (n = 75) |
>3cm (n = 62) |
P value | |
| (mean; 95% CI) | (mean; 95% CI) | (mean; 95% CI) | (mean; 95% CI) | |||
| Before surgery | 23.5; | 20.9; | .15 | 58.8; | 59.8; | .71 |
| 0-50.1 | 0-49.1 | 19.7-97.8 | 18.4-100 | |||
| After surgery | 93.0; | 90.93; | .029 | 3.7; | 3.1; | .34 |
| 70.4-100 | 70.0-100 | 0-18.1 | 0-13.9 | |||
| Improvement | 69.51 | 70.0 | .68 | 55.1 | 56.7 | .59 |
ASES, American Shoulder and Elbow Surgeons; CI, confidence interval.
Table IV.
Preoperative and postoperative functional results as per age at surgery.
| Patient age (years) | ASES |
QuickDASH |
||||
|---|---|---|---|---|---|---|
| <65 (n = 99) |
≥65 (n = 38) |
P value | <65 (n = 99) |
≥65 (n = 38) |
P value | |
| (mean; 95% CI) | (mean; 95% CI) | (mean; 95% CI) | (mean; 95% CI) | |||
| Before surgery | 22.5; | 21.2; | .34 | 58.8; | 60.3; | .21 |
| 0-49.7 | 0-50.1 | 18.3-99.4 | 20.4-100 | |||
| After surgery | 91.2; | 94.1; | .54 | 3.7; | 2.7; | .75 |
| 67.8-100 | 76.6-100 | 0-16.7 | 0-15.5 | |||
| Improvement | 68.7 | 72.9 | .16 | 55.1 | 57.7 | .59 |
ASES, American Shoulder and Elbow Surgeons; CI, confidence interval.
For the patients undergoing revision surgery (n = 6), the mean preoperative ASES score was 21.1 points (0-53.05), and the mean postoperative score was 88.0 points (53.90-100), with a mean improvement of 66.9 points. Their mean preoperative QuickDASH score was 51.1 points (0-100), and the mean postoperative score was 3.4 points (0-11.83), with an average improvement of 47.7 points. The results for patients undergoing revision surgery were not significantly different from the ones obtained for the repair of primary tears.
In addition to the ASES and QuickDASH questionnaires, patients were asked to rate their overall satisfaction with their final results at the time of the follow-up phone call, using a scale ranging from poor, fair, good, or excellent. One hundred ten (80%) reported “excellent,” 19 (14%) reported “good,” 8 (6%) reported “fair,” and 0 reported “poor.” To the question “would you do the surgery again if you were in the same situation?” 128 patients (94%) answered yes.
Complications
There were no perioperative complications. No bone cut-out (tunnel failure) occurred during the final suturing and neither was there any tendon-to-tape tear.
In the early postoperative period, there was one case (0.7%) of need for revision at week 3 postoperatively. It was linked to an unplanned traumatic event in which the patient had to dive in the water and pull a heavy charge with the operated arm (to rescue an adult). At revision surgery, the retear was observed at the tendon-tape interface, with the bone tunnels and knots intact. A revision TO repair was performed. There were no other complications within the cohort for the study period.
Discussion
The authors found that functional outcomes at three to five years postoperatively were on par with those from the suture anchor techniques and conventional braided polyethylene suture TO repairs. Our data show that apart from one early (3 weeks) traumatic event at the suture-tendon interface, none of the patients required short- or mid-term revision surgery. Although many patients in the present cohort were in the 65 years and over group and presented markedly soft bone (osteopenia) during surgery, none experienced perioperative tunnel failure.
Functional outcome
Pain symptoms affect patient function the most because they are the most disruptive to daily life and the ASES and QuickDASH were designed and validated to evaluate pain and function related to daily activities.1 The minimal clinical important difference of the ASES for arthroscopic rotator cuff repair is 11.1,7 while the QuickDASH minimal clinically important difference (MCID) is 15.9.13 In our study, all patients (100%) achieved ASES MCID, with the average improvement being 6.3 times the value, while 136 patients (99.3%) achieved the QuickDASH MCID, with the average improvement being 3.5 times the value. Both outcome scores reflect the effectiveness of the surgical procedure to address the pain symptoms and to restore daily function in our sample. This is also echoed by the overall high subjective satisfaction expressed by the patients of our cohort. Our data demonstrated a significant improvement in postoperative vs. preoperative function, for the entire cohort, regardless of the age or the severity (size) of the tear. These highly favorable outcomes after arthroscopic TO rotator cuff repair match those reported by other authors,12,23 adding weight to the clinical validity of arthroscopic TO repair. Similar findings were also reported previously in comparable outcome studies where suture anchors had been used.3,10 More recently, Sandow and Schutz27 described satisfactory functional and anatomical results with a TO repair in an osteoporotic cohort of 15. Similarly, Arican et al2 described satisfactory clinical outcomes at >2 years in 70 patients treated with TO repair. In a larger randomized controlled trial of 69 patients, Randelli et al24 described comparable radiologic and functional results at >3 years between arthroscopic anchor-based and TO repair, while the latter was associated with significantly less postoperative pain.
The results of our subanalyses fail to show statistically significant difference in functional outcomes in older patients (>65 years) and larger tears (>3 cm), as shown in Table III, Table IV, despite the higher expected rate of retear or nonhealing for these groups.1 Of interest, there is an increasing body of evidence in the literature claiming that anatomic integrity does not affect clinical outcome,14,17,22 which could apply to our group. Full integrity of the repaired tendon or not, our results suggest the efficiency of surgical treatment in patients some could consider poor candidates for surgery.
Study limitations
The authors underline as a limitation to our study its scope was restricted to clinical results, with no postoperative radiological imaging addressing the tendon healing or the integrity of the bone. This prevents the present study from claiming effective healing in patients, instead focusing on clinical results. However, in the setting of private care with patients paying out of pocket, additional imaging would only have been reasonable with a need for revision surgery.
Another limitation of our study lies in the absence of a control group of patients, operated with suture anchors instead of TO, which prevents this study from comparing TO repair directly to anchor-based repair, and the lack of bone density assessment to quantify the osteoporosis of the patients.
The patient sample was not representative of the general patient population, as there was a disproportionately large number of older patients with larger tears, suggesting that a selection bias would underscore clinical efficiency.
Furthermore, TO repairs require a learning curve, which implies that results with this technique would vary as per the surgeon’s proficiency.
Conclusion
Arthroscopic TO repair using a 2-mm tape material has achieved significant midterm functional improvement in this group of patients, with results statistically unaffected by larger tear size (>3 cm) or older age (≥65 years), suggesting that this surgery presents great benefits for the aging population desiring to prolong their functionality and activity.
In our study, the adjunct of a 2-mm tape did not require tunnel augmenting implantable devices. The main remaining obstacle to the widespread use of the TO technique among the orthopedic surgeon community lies in the need for an intuitive and user-friendly surgical device that allows for quick, easy, and fast bone tunnel formation and suture transport.
Disclaimers
Funding: No funding was disclosed by the author(s).
Conflicts of interest: The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Acknowledgments
The authors wish to thank Mrs. Gabrielle Lapointe and Ms Kathleen Beaumont for research assistance.
Footnotes
The research ethics committee granted approval for this study.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jseint.2021.06.001.
Supplementary data
References
- 1.Angst F., Schwyzer H.-K., Aeschlimann A., Simmen B.R., Goldhahn J. Measures of adult shoulder function. Arthritis Care Res (Hoboken) 2011;63:S174–S188. doi: 10.1002/acr.20630. [DOI] [PubMed] [Google Scholar]
- 2.Arican M., Turhan Y., Karaduman Z.O., Ayanoğlu T. Clinical and functional outcomes of a novel transosseous device to treat rotator cuff tears: a minimum 2-year follow-up. J Orthop Surg (Hong Kong) 2019;27 doi: 10.1177/2309499019875172. [DOI] [PubMed] [Google Scholar]
- 3.Bennett W.F. Arthroscopic repair of massive rotator cuff Tears: a prospective cohort with 2- to 4-year follow-up. J Arthrosc Relat Surg. 2003;19:380–390. doi: 10.1053/jars.2003.50131. [DOI] [PubMed] [Google Scholar]
- 4.Benson E.C., MacDermid J.C., Drosdowech D.S., Athwal G.S. The incidence of early metallic suture anchor pullout after arthroscopic rotator cuff repair. Arthroscopy. 2010;26:310–315. doi: 10.1016/j.arthro.2009.08.015. [DOI] [PubMed] [Google Scholar]
- 5.Black E.M., Lin A., Srikumaran U., Jain N., Freehil M.T. Arthroscopic transosseous rotator cuff repair: Technical Note, outcomes, and complications. Orthopedics. 2015;38:352–358. doi: 10.3928/01477447-20150504-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chillemi C., Mantovani M., Osimani M., Castagna A. Arthroscopic transosseous rotator cuff repair: the eight-shape technique. Eur J Orthop Surg Traumatol. 2017;27:399–404. doi: 10.1007/s00590-017-1906-z. [DOI] [PubMed] [Google Scholar]
- 7.Cvetanovich G.L., Gowd A.K., Liu J.N., Nwachukwu B.U., Cabarcas B.C., Cole B.J. Establishing clinically significant outcome after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2019;28:939–948. doi: 10.1016/j.jse.2018.10.013. [DOI] [PubMed] [Google Scholar]
- 8.Day M., Westermann R., Duchman K., Gao Y., Pugely A., Bollier M. Rotator cuff Repair: open versus arthroscopic. Arthrosc J Arthrosc Relat Surg. 2018;34:1130–1136. doi: 10.1016/j.arthro.2017.10.027. [DOI] [PubMed] [Google Scholar]
- 9.Denard P.J., Burkhart S.S. Techniques for managing poor quality tissue and bone during arthroscopic rotator cuff repair. Arthroscopy. 2011;27:1409–1421. doi: 10.1016/j.arthro.2011.05.015. [DOI] [PubMed] [Google Scholar]
- 10.Denard P.J., Jiwani A.Z., Lädermann A., Burkhart S.S. Long-term outcome of arthroscopic massive rotator cuff Repair: the importance of double-row fixation. J Arthrosc Relat Surg. 2012;28:909–915. doi: 10.1016/j.arthro.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 11.Djurasovic M., Marra G., Arroyo J.S., Pollock R.G., Flatow E.L., Bigliani L.U. Revision rotator cuff repair: Factors influencing results. J Bone Joint Surg Am. 2001;83:1849–1855. doi: 10.2106/00004623-200112000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Flanagin B.A., Garofalo R., Lo E.Y., Feher L., Castagna A., Qin H. Midterm clinical outcomes following arthroscopic transosseous rotator cuff repair. Int J Shoulder Surg. 2016;10:3–9. doi: 10.4103/0973-6042.174511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Franchignoni F., Vercelli S., Giordano A., Sartorio F., Bravini E., Ferriero G. Minimal clinically important difference of the disabilities of the arm, shoulder and hand outcome measure (DASH) and its shortened version (QuickDASH) J Orthop Sports Phys Ther. 2014;44:30–39. doi: 10.2519/jospt.2014.4893. [DOI] [PubMed] [Google Scholar]
- 14.Galatz L.M., Ball C.M., Teefey S.A., Middleton W.D., Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Jt Surg. 2004;86-A:219–224. doi: 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Garrigues G.E., Lazarus M.D. Arthroscopic bone tunnel augmentation for rotator cuff repair. Orthopedics. 2012;35:392–397. doi: 10.3928/01477447-20120426-04. [DOI] [PubMed] [Google Scholar]
- 16.Gumina S., Carbone S., Campagna V., Candela V., Sacchetti F.M., Giannicola G. The impact of aging on rotator cuff tear size. Musculoskelet Surg. 2013;97:69–72. doi: 10.1007/s12306-013-0263-2. [DOI] [PubMed] [Google Scholar]
- 17.Klepps S., Bishop J., Lin J., Cahlon O., Strauss A., Hayes P. Prospective evaluation of the effect of rotator cuff integrity on the outcome of open rotator cuff repairs. Am J Sports Med. 2004;32:1716–1722. doi: 10.1177/0363546504265262. [DOI] [PubMed] [Google Scholar]
- 18.Leger St-Jean B., Ménard J., Hinse S., Petit Y., Rouleau D.M., Beauchamp M. Braided tape suture provides superior bone pull-through strength than wire suture in greater tuberosity of the humerus. J Orthop. 2015;12:S14–S17. doi: 10.1016/j.jor.2015.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Matthews T.J., Hand G.C., Rees J.L., Athanasou N.A., Carr A.J. Pathology of the torn rotator cuff tendon. Reduction in potential for repair as tear size increases. J Bone Joint Surg Br. 2006;88:489–495. doi: 10.1302/0301-620X.88B4.16845. [DOI] [PubMed] [Google Scholar]
- 20.Matthews T.J., Smith S.R., Peach C.A., Rees J.L., Urban J.P., Carr A.J. In vivo measurement of tissue metabolism in tendons of the rotator cuff: implications for surgical management. J Bone Joint Surg Br. 2007;89:633–638. doi: 10.1302/0301-620X.89B5.18905. [DOI] [PubMed] [Google Scholar]
- 21.Park J.G., Cho N.S., Song J.H., Baek J.H., Jeong H.Y., Rhee Y.G. Rotator cuff repair in patients over 75 Years of age: clinical outcome and repair integrity. Clin Orthop Surg. 2016;8:420–427. doi: 10.4055/cios.2016.8.4.420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Park M.C., Cadet E.R., Levine W.N., Bigliani L.U., Ahmad C.S. Tendon-to-Bone pressure distributions at a repaired rotator cuff footprint using transosseous suture and suture anchor fixation techniques. Am J Sports Med. 2005;33:1154–1159. doi: 10.1177/0363546504273053. [DOI] [PubMed] [Google Scholar]
- 23.Plachel F., Traweger A., Vasvary I., Schanda J.E., Resch H., Moroder P. Long-term results after arthroscopic transosseous rotator cuff repair. J Shoulder Elbow Surg. 2019;28:706–714. doi: 10.1016/j.jse.2018.09.003. [DOI] [PubMed] [Google Scholar]
- 24.Randelli P., Stoppani C.A., Zaolino C., Menon A., Randelli F., Cabitza P. Advantages of arthroscopic rotator cuff repair with a transosseous suture technique: a Prospective randomized controlled trial. Am J Sports Med. 2017;45:2000–2009. doi: 10.1177/0363546517695789. [DOI] [PubMed] [Google Scholar]
- 25.Redler L.H., Byram I.R., Luchetti T.J., Tsui Y.L., Moen T.C., Gardner T.R. Influence of rotator cuff tear size and repair technique on the creation and management of dog ear deformities in a transosseous- equivalent rotator cuff repair model. Orthop J Sport Med. 2014;2 doi: 10.1177/2325967114529257. 2325967114529257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rouleau D.M., Canet F., Beauchamp M. Biomechanical study comparing 3 fixation methods for rotator cuff massive tear: transosseous No. 2 suture, transosseous braided tape, and double-row b. J Orthop Sci. 2016;21:732–738. doi: 10.1016/j.jos.2016.07.001. [DOI] [PubMed] [Google Scholar]
- 27.Sandow M.J., Schutz C.R. Arthroscopic rotator cuff repair using a transosseous knotless anchor (ATOK) J Shoulder Elbow Surg. 2020;29:527–533. doi: 10.1016/j.jse.2019.07.017. [DOI] [PubMed] [Google Scholar]
- 28.Taha M.E., Schneider K., Clarke E.C., O'Briain D.E., Smith M.M., Cunningham G. A biomechanical comparison of different suture materials used for arthroscopic shoulder procedures. Arthroscopy. 2020;36:708–713. doi: 10.1016/j.arthro.2019.08.048. [DOI] [PubMed] [Google Scholar]
- 29.Urch E., Lin C.C., Itami Y., Patel N.A., McGarry M.H., Limpisvasti O. Improved rotator cuff footprint contact characteristics with an augmented repair construct using lateral edge fixation. Am J Sports Med. 2020;48:444–449. doi: 10.1177/0363546519888182. [DOI] [PubMed] [Google Scholar]
- 30.Urita A., Funakoshi T., Horie T., Nishida M., Iwasaki N. Difference in vascular patterns between transosseous-equivalent and transosseous rotator cuff repair. J Shoulder Elbow Surg. 2017;26:149–156. doi: 10.1016/j.jse.2016.06.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.