Abstract
Short-acting β2-agonist (SABA) use is known to be lower in Korean patients with asthma than in those from other countries, while the rate of asthma exacerbations in Korea is higher than in other countries. Thus, an epidemiologic study on SABA use and the relationship between SABA overuse and treatment outcomes in asthma is needed in Korea. We performed a cross-sectional study using the National Health Insurance Service-National Sample Cohort 2002–2012 database. We evaluated the trend of annual SABA use and overuse (prescription of 3 or more SABA canisters/year) and the impact of SABA overuse on mortality. During the study period, the proportion of asthmatic patients who used SABA was approximately 8%–11%, with no significant change in trend. The mean annual SABA use in asthmatic patients was 0.15–0.22 canisters/patient/year and 1.93–2.05 canisters/patient/year in those who used SABA in 12 months. SABA overuse was observed in about 2%–4% of asthmatic patients during the study period. SABA overuse generally tended to increase as the age of patients increased, with triple peaks in the late 20s (3.3%), late 40s (3.1%), and late 70s (3.6%). SABA overuse was associated with mortality (adjusted odds ratio, 1.72; 95% confidence interval, 1.61–1.84). The rate of SABA use was very low in Korean asthmatic patients between 2002–2012. SABA overuse was found in 2%–4% of patients in Korea. SABA overuse was associated with an increased risk of mortality.
Keywords: Asthma, SABA, population, epidemiology, treatment outcome, cross-sectional studies, prescription, mortality, asthma exacerbation
INTRODUCTION
Asthma is a serious global health problem associated with increased health-related cost and mortality,1 and short-acting β2-agonist (SABA) overuse is a major contributor to these burdens.1,2,3,4,5,6 Consequently, SABA is no longer recommended to be used alone as a treatment option in the Global Initiative for Asthma due to safety issues.1 For these reasons, there has been great interest in estimating the nationwide burden of SABA overuse in many countries. However, although some studies have addressed this issue in a few countries,7,8,9 there is still a lack of data about the burden of overuse in many countries, including Korea.10
In Korea, SABA use was reported to be much lower than in other countries,11 while the rate of acute exacerbations of asthma is higher than in other countries at similar socioeconomic levels.12,13 Therefore, whereas the main issue in other countries is the overuse of SABA,7,8,9 low SABA use seems to be problematic in Korea. Consequently, not only SABA overuse but also low SABA use needs to be evaluated in Korea.
Therefore, in this study, we aimed to evaluate the real-world use of SABA in Korea, including overuse in asthma. We also evaluated whether SABA overuse is associated with increased mortality.
MATERIALS AND METHODS
Study population
We performed a cross-sectional study of asthmatic patients ≥ 10 years of age using the National Health Insurance Service-National Sample Cohort (NHIS-NSC) database 2002–2012, which includes a 2.2% representative sample of Korean citizens.13 This study was approved by the Institutional Review Board (IRB) of Hanyang University Hospital (IRB No. HYUH 2020-07-026).
Definitions
Persistent asthma was defined according to the followings: 1) International Statistical Classification of Diseases and Related Health Problems (ICD)-10 codes J45–46 (asthma) and 2) ≥1 claim for a prescription of asthma-related medications for a year.14,15,16 SABA was defined as a metered-dose inhaler of salbutamol sulfate. SABA overuse was defined as a prescription of ≥ 3 SABA canisters (200 doses/canister) per year.9 Incident asthma was defined when a patient met the diagnostic criteria for asthma for the first time in the last 3 years of washout. Because the NHIS-NSC database provided data from 2002, patients with incident asthma were evaluated from 2005 to 2012. Asthma-related mortality was determined when the cause of death was classified as asthma (ICD-10 codes J45–J46).
Main outcomes
The main outcome was the trend of SABA prescription patterns in asthmatic patients. The secondary outcome was to elucidate whether SABA overuse is associated with increased mortality in asthmatic patients.
Statistical analysis
Categorical variables are presented as frequency (%), and continuous variables as mean ± standard deviation. To estimate the odds ratio (OR) and 95% confidence interval (CI) of SABA overuse for overall mortality and asthma-related mortality in patients with asthma, we performed logistic regression analysis. P values < 0.05 were considered statistically significant. All statistical analyses were performed using SAS 9.4 (SAS Institute, Cary, NC, USA).
RESULTS
Population
There were 153,481 patients with asthma from 2002 to 2012 (Table 1), with the age- and sex-adjusted prevalence of asthma ranging from 2.7% in 2002 to 5.1% in 2012 (Supplementary Table S1). The overall patients with asthma were in the following age groups in years: 17.2% were 10–19, 7.9% were 20–29, 15.4% were 30–39, 15.2% were 40–49, 15.3% were 50–59, 29.0% were aged >60. By sex, 40.2% were male and 59.8% were female. The proportion of patients who used asthma-related medications were as follows: inhaled corticosteroid (ICS), 27.5%; long-acting β2-agonist (LABA), 14.3%; leukotriene receptor antagonist, 36.6%; theophylline, 51.9%; ICS/LABA, 14.3%; and oral corticosteroid (OCS), 53.9%. The characteristics of patients with incident asthma are also summarized in Table 1.
Table 1. Characteristics of patients with asthma.
| Variables | Total (n = 153,481) | Patients with incident asthma (n = 78,869) | |
|---|---|---|---|
| Age group (yr) | |||
| 11–19 | 26,445 (17.2) | 7,144 (9.1) | |
| 20–29 | 12,118 (7.9) | 8,265 (10.5) | |
| 30–39 | 23,567 (15.4) | 14,474 (18.4) | |
| 40–49 | 23,323 (15.2) | 13,331 (16.9) | |
| 50–59 | 23,495 (15.3) | 13,509 (17.1) | |
| ≥ 60 | 44,533 (29.0) | 22,146 (28.1) | |
| Sex | |||
| Male | 61,723 (40.2) | 31,600 (40.1) | |
| Female | 91,758 (59.8) | 47,269 (59.9) | |
| Type of insurance | |||
| Self-employed health insurance | 57,377 (37.4) | 27,437 (34.8) | |
| Employee health insurance | 92,008 (60.0) | 48,413 (61.4) | |
| Medical aid | 4,096 (2.7) | 3,019 (3.8) | |
| Asthma medication* | |||
| ICS | 42,204 (27.5) | 17,555 (22.3) | |
| LABA | 21,991 (14.3) | 8,482 (10.8) | |
| LTRA | 56,090 (36.6) | 28,216 (35.8) | |
| Theophylline | 79,660 (51.9) | 37,033 (47.0) | |
| ICS/LABA | 21,920 (14.3) | 8,456 (10.7) | |
| LAMA | 2,032 (1.3) | 682 (0.9) | |
| OCS | 82,685 (53.9) | 38,615 (49.0) | |
| CCI | |||
| 0–1 | 125,215 (81.6) | 63,878 (81.0) | |
| 2 or more | 28,266 (18.4) | 14,991 (19.0) | |
Data are presented as frequency (%).
ICS, inhaled corticosteroid; LABA, long-acting β2 agonist; LTRA, leukotriene receptor antagonist; LAMA, long-acting muscarinic antagonist; OCS, oral corticosteroid; CCI, Charlson Comorbidities Index.
*Drugs prescribed at least once between 2002 and 2012 were included.
SABA use in the overall population
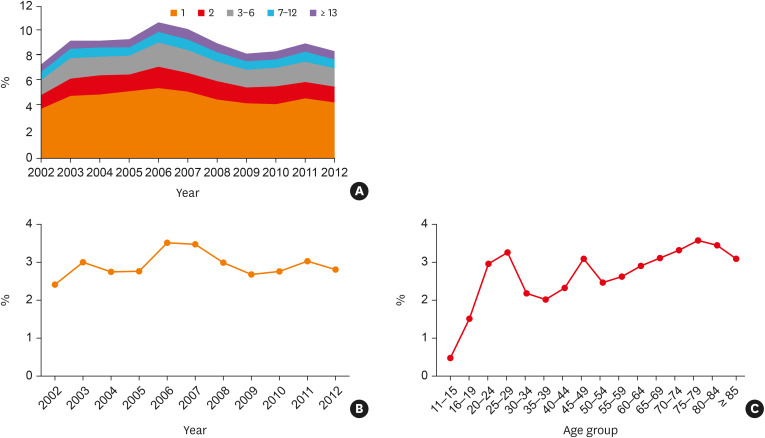
The proportion of asthmatic patients who used SABA during the study period was relatively stable, ranging from 7.4% to 10.8% (Fig. 1). The number of SABA canisters among the asthma population between 2002 and 2012 is summarized in Supplementary Table S1. In overall patients with asthma, the mean number of yearly SABA canisters ranged from 0.15 ± 0.65 to 0.22 ± 0.76. It ranged from 1.93 ± 1.27 to 2.07 ± 1.32 among the patients who used SABA. The rate of yearly SABA overuse was relatively stable, ranging from 2.4% to 3.5%.
Fig. 1. The trend of yearly SABA use in overall asthmatic patients between 2002 and 2012. (A) Percentage of patient groups categorized by the number of prescribed SABA canisters per year. (B) Percentage of patients with SABA overuse. (C) Percentage of SABA overuse according to age group among the total patients with asthma. SABA overuse was defined as a prescription of at least 3 SABA canisters (200 doses/canister) per year.
SABA, short-acting β2 agonist.
As shown in Supplementary Fig. S1A, the proportion of SABA use in patients who did not use ICS tended to decrease during the study period. In contrast, in patients who used ICS, SABA use gradually increased. (Supplementary Fig. S1B). Whereas the proportion of SABA overuse tended to decrease in patients who did not use ICS, it tended to increase in patients who used ICS during the study period (Supplementary Fig. S1A and B).
SABA overuse in the overall population
SABA overuse was observed in 2.4%–3.5% of asthmatic patients. The proportion of SABA overuse in asthmatic patients was relatively stable, ranging from 2.4% to 3.5% (Fig. 1B). Among the patients who used SABA, the proportion of SABA overuse was relatively stable, ranging from 29.4% to 33.4% (Supplementary Fig. S2A).
By age group, SABA overuse sharply increased from less than 0.5% in patients in their early teens and peaked in those in their late 20s (3.3%). Thereafter, it decreased to 2.0% in the late 30s and increased to 3.1% in the late 40s. In patients ≥ 50 years, SABA overuse gradually increased from 2.6% in the late 50s to 3.6% in the late 70s, and thereafter, it decreased (Fig. 1C). Among the subjects who used SABA, SABA overuse sharply increased from less than 15% in patients in their early teens and double-peaked at the late 20s (34.6%) and late forties (37.2%). In patients ≥ 50 years, SABA overuse was relatively stable, ranging from about 32.0% and 35.7% (Supplementary Fig. S2B).
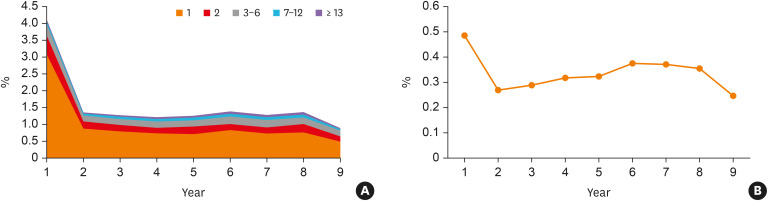
SABA use in patients with incident asthma
Fig. 2A shows that 4.1% of patients with incident asthma used at least one SABA in the first year of asthma diagnosis. It abruptly decreased to 1.4% from year 2, and thereafter, it remained stable. SABA overuse was observed in about 0.5% of patients with asthma in the first year of asthma diagnosis. It was decreased to 0.27% in the second year and thereafter tended to increase (Fig. 2B). The proportion of SABA overuse by year among patients with incident asthma who used SABA gradually increased from 11.8% in 2004 to 27.7% in 2012 (Supplementary Fig. S3).
Fig. 2. The trend of yearly SABA use in patients with incident asthma. (A) Percentage of subgroup patient groups categorized by the number of SABA canisters per year in patients with incident asthma after initial diagnosis. (B) Percentage of patients with SABA overuse in patients with incident asthma after initial diagnosis.
SABA, short-acting β2-agonist.
Association of SABA overuse and all-cause and asthma-related mortality
As shown in Table 2, patients who used 1–2 canisters of SABA/year (adjusted OR for overall mortality, 1.48; 95% CI, 1.40–1.56 and adjusted OR for asthma-related mortality, 2.13; 95% CI, 1.81–2.51) and SABA overusers (≥ 3 canisters/year) (adjusted OR for overall mortality, 1.72; 95% CI, 1.61–1.84 and adjusted OR for asthma-related mortality, 3.25; 95% CI, 2.72–3.89) were more likely to die compared to those who did not use SABA.
Table 2. Adjusted odds ratio and 95% CI of SABA use for all-cause mortality and healthcare use for asthma exacerbation according to SABA use.
| Variables | Mortality* | ||
|---|---|---|---|
| All-cause | Asthma-related | ||
| SABA use | |||
| 0/yr | Reference | Reference | |
| 1–2/yr | 1.48 (1.40–1.56) | 2.13 (1.81–2.51) | |
| ≥ 3/yr | 1.72 (1.61–1.84) | 3.25 (2.72–3.89) | |
Data are presented as a ratio (95% CI).
CI, confidence interval; SABA, short-acting β2 agonist; LTRA, leukotriene receptor antagonist; ICS, inhaled corticosteroid; LABA, long-acting β2 agonist; LAMA, long-acting muscarinic antagonist; CCI, Charlson Comorbidities Index; OCS, oral corticosteroid.
*Adjusted for age, sex, type of insurance, and treatment level (LTRA or ICS only vs. ICS/LABA vs. ICS/LABA/LAMA), CCI (0–1 vs. 2 or more), and any OCS use.
DISCUSSION
During the study period (2002–2012), about 8%–11% of asthmatic patients used SABA, without significant changes in trend. SABA overuse was observed in about 2%–4% of asthmatic patients. SABA overuse tended to increase as the age of asthmatic patients increased. While the proportion of SABA overuse among asthmatic patients was low, SABA overuse was associated with a significantly increased risk of mortality.
In this study, the mean number of annual SABA canisters in patients who used SABA was about 2, which is higher than in Germany (mean, 1.6) and lower than in the UK (mean, 4.2).9 However, a distinctive feature in Korean asthmatics was that the rates of SABA use and SABA overuse were lower compared to other countries. A previous study performed in Michigan, USA revealed that three-quarters of asthmatic patients used SABA.6 In comparison, as reported in our study and a previous study, about 10% of Korean asthmatic patients used SABA (only SABA canisters were counted in our study).17 Regarding SABA overuse, although SABA overuse ranged from 9% to 38% of asthmatic patients in European countries,9 SABA overuse was found in only 2%–4% of Korean asthmatics based on similar study design and definition of SABA overuse. These results are very surprising considering that the exacerbation rate of asthmatic patients is higher in Korea than in other countries in East Asia at similar socioeconomic levels.12 We should emphasize that these results do not inform us whether the SABA use in Korea is appropriate. On the contrary, these results may raise concerns that extremely low SABA use may be linked to insufficient symptom relief. In addition, since extremely low SABA use may have resulted in a poor asthma action plan, it might increase the need for health care use.18 We also would like to emphasize the absence of an action plan on how to increase the prescription rate and how to make patients use SABA properly is also a big problem in Korea. Thus, future studies are needed on whether not only SABA overuse but also extremely low SABA use can contribute to poor treatment outcomes in Korean asthmatic patients.
There are several possible explanations for the low SABA use in Korean asthmatic patients. First, in Korea, SABA is regarded as an “emergency medication” not as a rescue medication. In Korea, there has been a stigma that SABA can increase mortality, and thus it should not be used if possible. Although SABA is useful to relieve acute respiratory symptoms of asthma and its proper use can prevent further deterioration of asthma exacerbation, many Korean patients tend to use SABA not for preventing exacerbations, but only after the occurrence of acute exacerbation. Secondly, the availability of SABA is very limited in Korea compared to other countries.9 For example, SABA is easily available as an over-the-counter drug in many Western countries.19 However, patients in Korea should receive a prescription for SABA by physicians. Thirdly, after ICS/LABA was introduced to the market in the early 2000s, advertisements driven by the pharmaceutical companies skewed these asthma medications as a controller. Thus, more and more patients are using ICS/LABA, whereas the use of ICS monotherapy decreased over time in Korea.11 Finally, very high prescription rate of OCS in the Qualitative Assessment of Asthma Management by Health Insurance Review and Assessment Service suggests that OCS may have been used as reliever medication without the use of SABA in Korea.20
Previous studies showed a linear trend between SABA overuse and age.7,8 In line with these findings, the rate of SABA overuse generally tends to increase as age increased in our study. However, in contrast to the findings in the previous study, a relatively higher rate of SABA overuse was observed in Korean asthmatic patients in their late 20s and late 40s. The reasons for this phenomenon are not easy to explain; however, a relatively higher workload and the stress of daily life might be one plausible explanation.21 When SABA use was compared to the use of ICS in Korean asthmatic patients, it tended to increase in patients who used ICS. This is positive, considering the very low SABA use in Korea. However, there is a concern that SABA overuse tends to increase in patients who have used ICS. As shown in other studies,1,2,3,6 SABA overuse was significantly associated with increased mortality and health care use in this study. When it comes to SABA overuse in patients with incident asthma, SABA overuse was very low in patients with incident asthma (< 0.5%). This result suggests that SABA overuse seems to be problematic in patients with longstanding asthma. We cautiously suggest that appropriate patient education, which emphasizes the side effects of SABA overuse as well as the importance of proper SABA use, is urgently needed in Korea.
There are some limitations to this study. First, as we used nationwide sample data between 2002 and 2013, we could not analyze more recent data. Secondly, due to the limitation of the NHIS-NHS dataset, we did not have data on body mass index, smoking history, and pulmonary function, which may be linked to the severity of asthma. Thirdly, due to the cross-sectional design, we could not evaluate the impact of SABA use on treatment outcomes other than mortality. Finally, we could not evaluate the association between low SABA use and treatment outcomes, because the NHIS-NHS dataset did not provide the data on the reasons why SABA was not used.
To conclude, between 2002 and 2012, SABA use was as low as 8%–11% in Korean asthmatic patients. SABA overuse was observed in about 2%–4% of asthmatic patients, and it was significantly associated with increased mortality.
ACKNOWLEDGMENTS
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HC19C0318), and by the Bio & Medical Technology Development Program of the National Research Foundation (NRF) funded by the Korean government (MSIT) (No. 2019M3E5D1A01069363). We thank the Biostatistical Consulting and Research Lab, Hanyang University for assistance with statistical analysis.
Footnotes
Disclosure: There are no financial or other issues that might lead to conflict of interest.
SUPPLEMENTARY MATERIALS
Yearly SABA use
Trend in SABA use according to ICS use between 2002 and 2012. (A) Percentage of patients groups categorized by the number of prescribed SABA canisters per year in patients who did not use ICS. (B) Percentage of patients groups categorized by the number of prescribed SABA canisters per year in patients who used ICS. SABA, short-acting β2-agonist; ICS, inhaled corticosteroid.
Trend in SABA overuse among the patients with asthma who used SABA between 2002 and 2012. (A) Percentage of patients with SABA overuse among the patients with asthma who used SABA. (B) Percentage of SABA overuse according to age group among the patients with asthma who used SABA.
Trend in SABA overuse among the patients with incident asthma who have used SABA between 2004 and 2012.
References
- 1.Nwaru BI, Ekström M, Hasvold P, Wiklund F, Telg G, Janson C. Overuse of short-acting β2-agonists in asthma is associated with increased risk of exacerbation and mortality: a nationwide cohort study of the global SABINA programme. Eur Respir J. 2020;55:1901872. doi: 10.1183/13993003.01872-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Suissa S, Ernst P, Boivin JF, Horwitz RI, Habbick B, Cockroft D, et al. A cohort analysis of excess mortality in asthma and the use of inhaled beta-agonists. Am J Respir Crit Care Med. 1994;149:604–610. doi: 10.1164/ajrccm.149.3.8118625. [DOI] [PubMed] [Google Scholar]
- 3.Anis AH, Lynd LD, Wang XH, King G, Spinelli JJ, Fitzgerald M, et al. Double trouble: impact of inappropriate use of asthma medication on the use of health care resources. CMAJ. 2001;164:625–631. [PMC free article] [PubMed] [Google Scholar]
- 4.Schatz M, Zeiger RS, Vollmer WM, Mosen D, Apter AJ, Stibolt TB, et al. Validation of a beta-agonist long-term asthma control scale derived from computerized pharmacy data. J Allergy Clin Immunol. 2006;117:995–1000. doi: 10.1016/j.jaci.2006.01.053. [DOI] [PubMed] [Google Scholar]
- 5.Patel M, Pilcher J, Reddel HK, Pritchard A, Corin A, Helm C, et al. Metrics of salbutamol use as predictors of future adverse outcomes in asthma. Clin Exp Allergy. 2013;43:1144–1151. doi: 10.1111/cea.12166. [DOI] [PubMed] [Google Scholar]
- 6.Paris J, Peterson EL, Wells K, Pladevall M, Burchard EG, Choudhry S, et al. Relationship between recent short-acting beta-agonist use and subsequent asthma exacerbations. Ann Allergy Asthma Immunol. 2008;101:482–487. doi: 10.1016/S1081-1206(10)60286-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sadatsafavi M, Tavakoli H, Lynd L, FitzGerald JM. Has asthma medication use caught up with the evidence?: a 12-year population-based study of trends. Chest. 2017;151:612–618. doi: 10.1016/j.chest.2016.10.028. [DOI] [PubMed] [Google Scholar]
- 8.Tavakoli H, Mark FitzGerald J, Lynd LD, Sadatsafavi M. Predictors of inappropriate and excessive use of reliever medications in asthma: a 16-year population-based study. BMC Pulm Med. 2018;18:33. doi: 10.1186/s12890-018-0598-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Janson C, Menzies-Gow A, Nan C, Nuevo J, Papi A, Quint JK, et al. SABINA: an overview of short-acting β2-agonist use in asthma in European countries. Adv Ther. 2020;37:1124–1135. doi: 10.1007/s12325-020-01233-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cabrera CS, Nan C, Lindarck N, Beekman MJ, Arnetorp S, van der Valk RJ. SABINA: global programme to evaluate prescriptions and clinical outcomes related to short-acting β2-agonist use in asthma. Eur Respir J. 2020;55:1901858. doi: 10.1183/13993003.01858-2019. [DOI] [PubMed] [Google Scholar]
- 11.Lee E, Kim A, Ye YM, Choi SE, Park HS. Increasing prevalence and mortality of asthma with age in Korea, 2002–2015: a nationwide, population-based study. Allergy Asthma Immunol Res. 2020;12:467–484. doi: 10.4168/aair.2020.12.3.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thompson PJ, Salvi S, Lin J, Cho YJ, Eng P, Abdul Manap R, et al. Insights, attitudes and perceptions about asthma and its treatment: findings from a multinational survey of patients from 8 Asia-Pacific countries and Hong Kong. Respirology. 2013;18:957–967. doi: 10.1111/resp.12137. [DOI] [PubMed] [Google Scholar]
- 13.Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017;46:e15. doi: 10.1093/ije/dyv319. [DOI] [PubMed] [Google Scholar]
- 14.Lee H, Ryu J, Chung SJ, Park DW, Sohn JW, Yoon HJ, et al. Coexisting COPD increases mortality in patients with corticosteroid-dependent asthma: a nationwide population-based study. Allergy Asthma Immunol Res. 2020;12:821–831. doi: 10.4168/aair.2020.12.5.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Choi JY, Yoon HK, Lee JH, Yoo KH, Kim BY, Bae HW, et al. Nationwide use of inhaled corticosteroids by South Korean asthma patients: an examination of the Health Insurance Review and Service database. J Thorac Dis. 2018;10:5405–5413. doi: 10.21037/jtd.2018.08.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee H, Ryu J, Nam E, Chung SJ, Yeo Y, Park DW, et al. Increased mortality in patients with corticosteroid-dependent asthma: a nationwide population-based study. Eur Respir J. 2019;54:1900804. doi: 10.1183/13993003.00804-2019. [DOI] [PubMed] [Google Scholar]
- 17.Choi JY, Yoon HK, Lee JH, Yoo KH, Kim BY, Bae HW, et al. Current status of asthma care in South Korea: nationwide the Health Insurance Review and Assessment Service database. J Thorac Dis. 2017;9:3208–3214. doi: 10.21037/jtd.2017.08.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goto T, Camargo CA, Jr, Gimenez-Zapiola C, Pallin DJ, Shapiro NI, Ferro TJ, et al. Comparing ran-out status of inhaled short-acting beta-agonists in emergency department patients with acute asthma: 1996–1998 versus 2015–2017. J Allergy Clin Immunol Pract. 2018;6:1999–2005.e3. doi: 10.1016/j.jaip.2018.04.001. [DOI] [PubMed] [Google Scholar]
- 19.Azzi EA, Kritikos V, Peters MJ, Price DB, Srour P, Cvetkovski B, et al. Understanding reliever overuse in patients purchasing over-the-counter short-acting beta2 agonists: an Australian community pharmacy-based survey. BMJ Open. 2019;9:e028995. doi: 10.1136/bmjopen-2019-028995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim SR, Lee YC, Sung MJ, Bae HW. Current epidemiological data on asthma management in South Korea from qualitative assessment of asthma management by Health Insurance Review and Assessment Service (HIRA) Tuberc Respir Dis (Seoul) 2017;80:221–225. doi: 10.4046/trd.2017.80.3.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seoul Mental Health Welfare Center. Seoul Mental Health Statistics [Internet] Seoul: Seoul Mental Health Welfare Center; 2015. [cited 2020 Jul 24]. Available from: http://seoulmentalhealth.kr. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Yearly SABA use
Trend in SABA use according to ICS use between 2002 and 2012. (A) Percentage of patients groups categorized by the number of prescribed SABA canisters per year in patients who did not use ICS. (B) Percentage of patients groups categorized by the number of prescribed SABA canisters per year in patients who used ICS. SABA, short-acting β2-agonist; ICS, inhaled corticosteroid.
Trend in SABA overuse among the patients with asthma who used SABA between 2002 and 2012. (A) Percentage of patients with SABA overuse among the patients with asthma who used SABA. (B) Percentage of SABA overuse according to age group among the patients with asthma who used SABA.
Trend in SABA overuse among the patients with incident asthma who have used SABA between 2004 and 2012.