Abstract
Purpose
This paper aims to evaluate the prevalence of REs in a clinic from Aguascalientes, Mexico by analysing clinical records from the local public health system. Refractive errors (REs) are quite common globally, but no data have been published regarding their frequency in clinics from Mexico. A priori, the frequency of ametropias should be high as admixture ancestry from this region is mainly European and Amerindian, the regions with high prevalence worldwide.
Methods
This cross-sectional study was conducted on 2195 subjects from records of public optometry services during the year 2018. Information obtained included age, gender, sphere, cylinder and axis. The prevalence of myopia, hyperopia and astigmatism was determined by gender and age groups in paediatric and adult patients. Chi-square testing was applied to determine significant differences in prevalence across age groups and gender. A p-value <0.05 was considered significant.
Results
In subjects under 18 years of age, the prevalence of emmetropia, astigmatism, myopia and hyperopia was 20.1%, 51.1%, 7.0% and 11.8%, respectively. In adults, emmetropia was present at a frequency of 20.1%, while 57.1% presented astigmatism, 12.4% hyperopia and 8.6% presented myopia. A significant association was observed between the presence of REs and age and gender.
Conclusions
In this first report of prevalence of REs from western Mexico, astigmatism was the most prevalent RE in children, adolescents and adults while the least common was myopia. Important differences were found in prevalence in comparison to national and international reports.
Keywords: Refractive errors, Prevalence, Mexico, Vision
Introduction
The prevalence of refractive errors (REs) worldwide differs across regions, with a higher prevalence of astigmatism in the Americas and Eastern Mediterranean among children and in the Americas and South-east Asia in adults according to a recent meta-analysis.1
Myopia is more prevalent in children from the Western Pacific and Europe as well as in adults from South-east Asia and Europe. Meanwhile, hyperopia is more frequent in American and European children as well as African and European adults.2, 3, 4, 5 These differences might be due to dissimilar genetic background and ambiental-related factors including some outdoor activities as suggested previously.6, 7, 8, 9, 10, 11
The settled population in the state of Aguascalientes, geographically located in the western region of Mexico, has genetic traits not fully shared with populations from other regions of Mexico and the world.12
Genetic background of Mexicans is diverse and varies by geographical region; patterns European ancestry is more prevalent in the north and west (66.7–95%), whereas Native American ancestry is more common in the centre and south-east (37–50%), with low African ancestry.7 A specific genetic analysis of Aguascalientes population found that maternal ancestry markers are 91% Amerindian, 5% European, 3% African and 1% Euroasian (6). Whereas paternal ancestry markers are 27% Amerindian, 54% European, 13% Euroasian, 1% Asian and 5% African.13
Because no reports exist on the prevalence of REs in the Aguascalientes population or in western Mexico and two previous studies of myopia prevalence in adolescents of two regions of Mexico (central and northern) have found extremely different prevalence of myopia (9.7% vs 44.9%, respectively) in individuals of similar age and gender,14, 15 we hypothesized that the prevalence of all RE might be dissimilar in population from Aguascalientes than in other Mexican geographical areas. Furthermore, to our knowledge no other reports exist about hyperopia and astigmatism prevalence in Mexican population by age groups. This study aims to determine the prevalence of REs in children and adults from Aguascalientes by analysing clinical records from the local public health system and comparing them with reports for regions worldwide.
Material and methods
Design and study population
A descriptive, transversal and retrospective study was carried out. A group of Optometrists performed an optometric test to evaluate the refractive status of both eyes in each patient. We analysed the data of all subjects who attended eye clinics of the public health system located in the state of Aguascalientes during 2018. These clinics provide health services to 60% of the global population of this small state located in western Mexico. We excluded cases of patients with a history of eye surgery or who were diagnosed with corneal ectasia during examination. The results are divided into two age groups: children and adolescents (<18 years) and adults (≥18 years). The ethics committee of the Autonomous University of Aguascalientes approved the study and informed consent of the participants in this research was obtained.
Diagnosis of refractive status
Visual acuity was evaluated using an Essilor CP550 optotype projector (Essilor Instruments, Chicago, IL, USA), and with phoropters ranged from –20.00 Diopter (D) to +20.00 D in sphere and a cylinder range from –0.25 to –6.00 D used to perform the skyascopy. The Optometrists performed an optometric test supported by a diagnostic kit (Welch Allyn Elite Retinoscope 3.5 V, Doral, USA). In paediatric patients since 1 year old the refractive evaluation was the gold standard test by cycloplegia at last 20 min. following instillation of cyclopentolate 1% and at the end of the subjective evaluation we perform MEM (Monocular Estimation Method) to promote relaxation of accommodation. For adult people we perform static retinoscopy the working distance was -2.00. The cut-off points for the diagnosis of REs were the following: myopia >0.50 D, hyperopia > +0.50 D; and the diagnosis for astigmatism was at least -0.75, likewise, the diagnosis of astigmatism was divided into five categories (simple myopic astigmatism [SMA], compound myopic astigmatism [CMA], simple hypermetropic astigmatism [SHA], compound hypermetropic astigmatism [CHA] and mixed astigmatism [MA]).16 Likewise, an evaluation of the binocular and ocular health status was carried out for all patients (data not shown).
Statistical analysis
Descriptive analysis was carried out with means and standard deviation (SD) calculated for the quantitative variables and proportions for the qualitative variables. To compare the prevalence of ametropias, categories by age subgroups were established in children and adolescents (1–5 years, 6–10 years, 11–14 years and 15–17 years), as well as in adults (18–30 years, 31–40 years, 41–50 years, 51–60 years, ≥61 years). The differences between age groups were tabulated for each according to the ametropias and were estimated through Chi-square testing. The analyses were performed with Stata software version 12.0 (StataCorp, College Station, Texas, USA) and the level of statistical significance was set at a p-value of <0.05.
Results
The total population evaluated included data from 2,195 subjects (4390 eyes) separated into individuals under 18 years (children and adolescents) and over 18 years (adults).
Data from 722 eyes of children and adolescents (52.4% female) were evaluated. The mean (SD) age was 9.7 (3.9) years. Table 1 presents the prevalence of REs in children and adolescents according to sex and different age groups. The prevalence of myopia, hyperopia and astigmatism in children under 18 years of age was 7.0%, 11.8% and 61.1%, respectively. The prevalence of eyes with normal refractive status in this infant-juvenile sample was 20.1%.
Table 1.
Proportion of ametropia in children and adolescents according to different sex and age groups.
| Refractive error |
Age groups (years) |
Total | p* | ||||
|---|---|---|---|---|---|---|---|
| 1–5 | 6–10 | 11–14 | 15–17 | ||||
| Boys | n | 62 | 146 | 96 | 40 | 344 | |
| Myopia | % | 6.5 | 5.5 | 3.1 | 22.5 | 7.0 | 0.001 |
| Hyperopia | % | 27.4 | 8.9 | 8.3 | 5.0 | 11.6 | <0.001 |
| Astigmatism | % | 46.8 | 64.4 | 51.0 | 57.5 | 56.7 | 0.064 |
| SMA | % | 6.5 | 21.2 | 21.9 | 30.0 | 19.8 | 0.018 |
| CMA | % | 3.2 | 16.4 | 9.4 | 12.5 | 11.6 | 0.045 |
| SHA | % | 3.2 | 8.2 | 5.2 | 0.0 | 5.5 | 0.171 |
| CHA | % | 29.0 | 12.3 | 5.2 | 7.5 | 12.8 | <0.001 |
| MA | % | 4.8 | 6.2 | 9.4 | 7.5 | 7.0 | 0.693 |
| Girls | n | 54 | 150 | 118 | 56 | 378 | |
| Myopia | % | 0.0 | 6.0 | 10.2 | 10.7 | 7.1 | 0.067 |
| Hyperopia | % | 27.8 | 14.0 | 5.9 | 3.6 | 11.9 | <0.001 |
| Astigmatism | % | 61.1 | 66.7 | 60.2 | 75.0 | 65.1 | 0.239 |
| SMA | % | 7.4 | 24.7 | 28.0 | 32.1 | 24.3 | 0.011 |
| CMA | % | 3.7 | 14.0 | 21.2 | 16.1 | 15.1 | 0.028 |
| SHA | % | 7.4 | 9.3 | 2.5 | 5.4 | 6.4 | 0.150 |
| CHA | % | 20.4 | 14.0 | 2.5 | 10.7 | 10.9 | 0.002 |
| MA | % | 22.2 | 4.7 | 5.9 | 10.7 | 8.5 | 0.001 |
| Total children | n | 116 | 296 | 214 | 96 | 722 | |
| Myopia | % | 3.5 | 5.7 | 7.0 | 15.6 | 7.1 | 0.003 |
| Hyperopia | % | 27.6 | 11.5 | 7.0 | 4.2 | 11.8 | <0.001 |
| Astigmatism & | % | 53.5 | 65.5 | 56.1 | 67.7 | 61.1 | 0.025 |
| SMA | % | 6.9 | 23.0 | 25.2 | 31.3 | 22.2 | <0.001 |
| CMA | % | 3.5 | 15.2 | 15.9 | 14.6 | 13.4 | 0.008 |
| SHA | % | 5.2 | 8.8 | 3.7 | 3.1 | 6.0 | 0.055 |
| CHA | % | 25.0 | 13.2 | 3.7 | 9.4 | 11.8 | <0.001 |
| MA | % | 12.9 | 5.4 | 7.5 | 9.4 | 7.8 | 0.072 |
Abbreviations: AMS, simple myopic astigmatism; AMC, composite myopic astigmatism; AHS, simple hypermetropic astigmatism; AHC, hypermetropic astigmatism compound; AM, mixed astigmatism. Chi-square test values are shown between age groups and statistical difference by gender p-value = 0.02 via Chi-square testing.
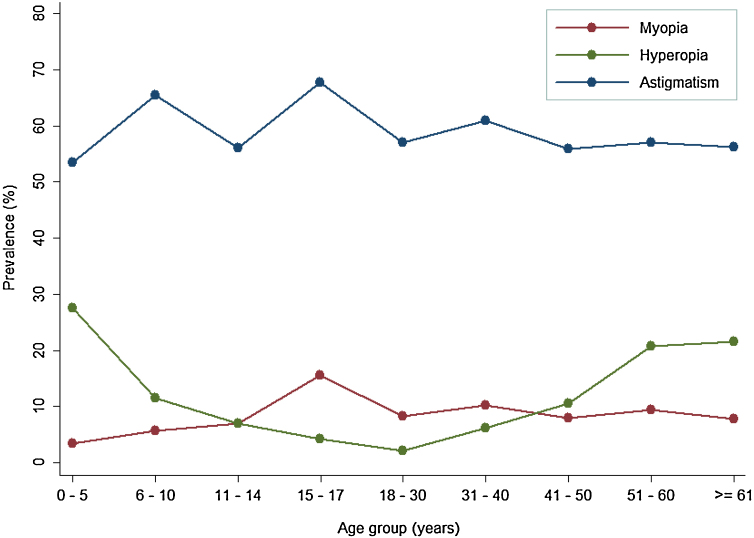
Hyperopia was more frequent in 1–5 year old children (27.6%, p < 0.001), whereas myopia was more common after 15 years old (p = 0.003; Table 1). On the other hand, astigmatism was the most frequent refractive disorder among all age groups for children (Table 1) and showed a significant difference in its distribution by gender. Within the categories of astigmatism, we found a higher percentage of SMA (22.2%) followed by CMA (13.4%) and CHA (11.8%) for the total infant-juvenile sample (Table 1, Graph 1).
Graph 1.
Refractive error prevalence according to age groups.
In the case of adults, data on 3668 eyes (60.6% of women) were analysed (mean age: 46.3 ± 16.7 years). The analysis revealed that 8.6% of adults presented myopia, 12.4% hyperopia and 57.1% had some type of astigmatism, whereas the prevalence of eyes with normal refractive status in adults was 21.9%.
During adulthood, hyperopia prevalence increased with age, rising from 2.2% in <30 years to 6.1% in the 31–40 age group and to 10.5% in the 41–50 age group. With this, prevalence doubled after 50 years in relation to the frequency of hyperopia in the 41–50 years age group (Table 2). On the other hand, hyperopia was significantly different (p < 0.05) among men and women (Table 2).
Table 2.
Proportion of ametropias in adults according to different sex and age groups.
| Refractive error |
Age groups (years) |
Total | p | |||||
|---|---|---|---|---|---|---|---|---|
| 18–30 | 31–40 | 41–50 | 51–60 | ≥ 61 | ||||
| Men | n | 408 | 182 | 250 | 242 | 364 | 1446 | |
| Myopia | % | 4.9 | 13.2 | 6.8 | 10.3 | 9.3 | 8.3 | 0.006 |
| Hyperopia | % | 2.2 | 4.4 | 9.2 | 15.3 | 13.7 | 8.8 | <0.001 |
| Astigmatism | % | 56.4 | 59.3 | 57.2 | 60.3 | 57.1 | 57.8 | 0.869 |
| SMA | % | 23.8 | 24.7 | 22.4 | 14.9 | 8.2 | 18.3 | <0.001 |
| CMA | % | 21.8 | 24.2 | 26.0 | 21.1 | 16.2 | 21.3 | 0.042 |
| SHA | % | 1.5 | 2.8 | 2.8 | 6.2 | 7.4 | 4.2 | <0.001 |
| CHA | % | 2.9 | 1.1 | 4.8 | 9.5 | 17.3 | 7.8 | <0.001 |
| MA | % | 6.4 | 6.6 | 1.2 | 8.7 | 8.0 | 6.3 | 0.005 |
| Women | n | 488 | 310 | 474 | 492 | 458 | 2222 | |
| Myopia | % | 11.1 | 8.4 | 8.4 | 9.2 | 6.6 | 8.8 | 0.182 |
| Hyperopia | % | 2.3 | 7.1 | 11.2 | 23.4 | 27.7 | 14.8 | <0.001 |
| Astigmatism | % | 57.6 | 61.9 | 55.3 | 55.3 | 55.5 | 56.8 | 0.320 |
| SMA | % | 25.2 | 28.4 | 17.9 | 10.2 | 9.0 | 17.4 | <0.001 |
| CMA | % | 27.3 | 18.7 | 20.0 | 16.9 | 12.0 | 19.1 | <0.001 |
| SHA | % | 1.8 | 4.8 | 4.0 | 4.5 | 6.8 | 4.3 | 0.007 |
| CHA | % | 1.0 | 3.2 | 5.7 | 13.4 | 21.0 | 9.2 | <0.001 |
| MA | % | 2.3 | 6.8 | 7.6 | 10.4 | 6.8 | 6.8 | <0.001 |
| Total adults | n | 896 | 492 | 724 | 734 | 822 | 3668 | |
| Myopia | % | 8.3 | 10.2 | 7.9 | 9.5 | 7.8 | 8.6 | 0.453 |
| Hyperopia & | % | 2.2 | 6.1 | 10.5 | 20.7 | 21.5 | 12.4 | <0.001 |
| Astigmatism | % | 57.0 | 61.0 | 55.9 | 57.0 | 56.2 | 57.1 | 0.449 |
| SMA | % | 24.6 | 27.0 | 19.5 | 11.7 | 8.6 | 17.8 | <0.001 |
| CMA | % | 24.8 | 20.7 | 22.1 | 18.3 | 13.9 | 20.0 | <0.001 |
| SHA | % | 1.7 | 4.1 | 3.6 | 5.0 | 7.1 | 4.3 | <0.001 |
| CHA | % | 1.9 | 2.4 | 5.4 | 12.1 | 19.3 | 8.6 | <0.001 |
| MA | % | 4.1 | 6.7 | 5.4 | 9.8 | 7.3 | 6.6 | <0.001 |
Abbreviations: AMS, simple myopic astigmatism; AMC, composite myopic astigmatism; AHS, simple hypermetropic astigmatism; AHC, hypermetropic astigmatism compound; AM, mixed astigmatism. * Chi-square test values are shown between age groups and statistical difference by gender p-value = 0.02 via Chi-square testing.
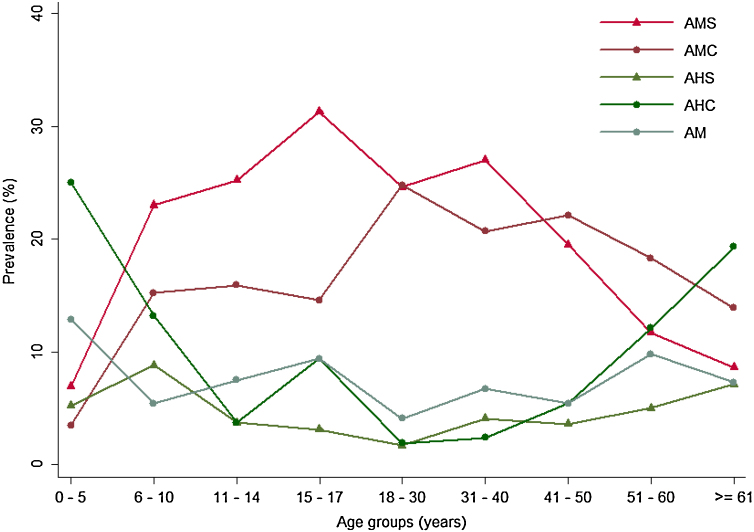
With respect to myopia, its prevalence remained stable across all age groups (from 7.8 to 10.2%; Table 2), whereas astigmatism was the most prevalent disorder across all age groups, reaching the highest prevalence in the 31–40 years age group (Table 2). By astigmatism type, the prevalence of SMA and CMA diminished as age increased; SMA began decreasing at 18 years of age, with the lowest prevalence after 60 years; CMA prevalence decreased after 50 years, also with the lowest prevalence after 60 years. In contrast, the prevalence of CHA in the 18–30 years age group was 1.9%, thereafter rising to 12.1% after 50 years and 19.3% after 60 years (Table 2, Graph 2).
Graph 2.
Astigmatism prevalence according to age groups.
Discussion
Several relevant findings were uncovered in terms of the prevalence of REs in patients from eye clinics of the public health system of Aguascalientes. The astigmatism most commonly occurring as a product of rotational asymmetries include one or both of the cornea surface, corneal astigmatism, likewise, those of the lens, internal astigmatism, and/or a tilt of the latter. Astigmatism gives rise to two planes of focus that may lie in front of, lie behind, or straddle the retinal plane, depending on whether it occurs alone or in combination with hyperopia or myopia.17 First, the prevalence of astigmatism in children and adolescents of our study was so much higher (61.5%) than that of Hashemi et al., who determined a prevalence of 14.3% in subjects ≤15 years old from a rural area of Iran1.18 In addition, our prevalence was higher than that reported by Marasini et al. (2014), who observed a 15.9% prevalence of astigmatism in children <10 years old in an eye clinic of New Zealand and 25–27% in subjects who were 10–20 years old who attended an eye clinic in the Maldives.19
In adults, the prevalence of astigmatism in our study (57.1%) was superior to what was reported by Hashemi et al. (32.2%) and Marasini et al. (8.66–24.54%) while also higher than that reported by Durkin et al. (31.1%) in a rural eye clinic from Australia.20 However, it was lower than the prevalence reported by Rodriguez and Romero (67.6%) from an eye clinic from Puerto Rico.21
With the analysis by gender, girls had a significantly higher prevalence of astigmatism than boys, but this difference was not significant by adulthood. The majority of previous reports did not establish differences in astigmatism prevalence by gender in children and adults11, 12, 13; only Rodriguez and Romero observed a higher prevalence of astigmatism in adult women versus men, a result that was not found in the present study.14
In our study, contrary to other reports, we did not observe significant differences in astigmatism frequency by age groups in children, adolescents and adults. For example, while Rodriguez and Romero, Durkin and Hashemi reported an increase of prevalence with age, Marasini described a higher prevalence below 30 years.11, 12, 13, 14Although the causes of these differences are unclear, they might be attributable to variations in the prevalence of risk factors for astigmatism, such as pterigium, the proportion of participants living in rural areas, nutritional status or distinct genetic backgrounds of participants in each study.22, 23, 24
In the present work, hyperopia frequency was greater in children below six years of age, then it diminished, reaching its nadir in individuals 18–30 years old. Afterwards, the prevalence increased to 10.5% at 40 years and more than 20% after 50 years old. The highest prevalence of hyperopia below six years might be explained by the small eye axial length and their subsequent reduction by increases of the axial length as the subject grew.25 Approaching the situation differently, the increase in hyperopia prevalence at 40 years and older might be the result of a reduction of the dioptric power of the crystalline lens associated with its increased axial thickness, as mentioned by Olsen in his study, when an imbalance occurs between the refractive components of the eye it is therefore more likely to be found in the relationship between axial length and the power of the lens,26 however, at this same age the accommodation changes begin causing a diminished capacity for lens accommodation or genuine longitudinal and cohort effects on refraction as described previously by Hashemi.27
The rising prevalence of hyperopia as age increases in adults has been reported previously in clinic-based studies of Hashemi, Durkin, and Rodriguez and Romero.11, 13, 14 Yet, the prevalence of this RE in adults was much lower in our study than in such studies across all age groups. This might be related to anatomic differences of the eye in our population in comparison with Iranian, Australian and Puerto Rican groups.17, 19, 20
We observed a higher hyperopia prevalence in women older than 50 years than among men, the same pattern reported by Durkin in women and men aged 40–49 years old and by Rodriguez and Romero.19, 20 It should be noted, though, that Hashemi et al. did not report gender differences in terms of hyperopia prevalence in adults.17
Studies as the Ehrlich et al. and Ingram and Barr, both show increase of the hyperopia as the infant grows older, as long as emmetropization is achieved. While we did not find clinic-based reports surrounding the prevalence of hyperopia in children, we did observe the same pattern of hyperopia prevalence in population-based studies, including the greatest prevalence for ages lower than six years old.28, 29, 30, 31
This prevalence is lower than that reported by Rodriguez and Romero in Puerto Rican adults for men (16.8%) and women (13.7%).14 Similarly, our myopia prevalence in adults was much lower than that reported in Australians (31.1%) and Iranians (28%) in clinics-based studies.11, 13 Thus, the prevalence of myopia in our study is contrary to the high prevalence of this RE in other populations.1
In the current work, the frequency of myopia in children and adolescents was higher (global: 7.8%; boys: 9.3%; girls: 6.6%) than that reported by Alemam et al. in an eye clinic from Saudi Arabia who found a frequency of 3.54% with no significant differences by gender (4.0% in boys and 3.1% in girls).30, 32 In contrast, Teophanous et al. reported a prevalence of myopia of 41.9% in patients 5–19 years old undergoing an ophthalmologic or optometric refraction examination through the Kaiser Permanente southern California health plan, especially being more common in subjects of Asian/Pacific Island origins than among whites.23 In fact, myopia is the most prevalent refractive disorder in paediatrics from East Asia with a prevalence of 70–90% in countries such as Hong Kong, China, Singapore and Taiwan.24
The prevalence of myopia in our population is low and similar to a report in Mexican school children from a rural community of Central Mexico where Garcia et al. determined a myopia prevalence of 9.7%.8 However, this was notably lower than the 44.9% prevalence reported by Villarreal in school children from northern Mexico,9 highlighting the geographical differences not only by race or country but also within a country. In consequence it would be valuable to determine the prevalence of RE by geographical areas since Mexico is a genetic diverse country.6, 7
The main limitation of this study is that it is based on data obtained in health system clinics, and may not reflect the population distribution. Likewise, that by including individuals who attended the clinic one could have a selection bias. However, we consider it valuable to communicate the results and clarify that it is a study based on clinical records, as other studies of similar design have reported in international literature.
In conclusion, According with our definition showed above of astigmatism and the way as we evaluated to the population studied, we assumed that the astigmatism was the most prevalent RE in children, adolescents and adults of Aguascalientes, specifically having one of the highest frequencies reported in clinic-based studies. In contrast, myopia was the least common RE in children, adolescents and adults and hyperopia lower than the reported in other populations. To the best of our knowledge, this is one of the most complete studies regarding the prevalence of RE in a population from western Mexico based on medical records from eye clinics of the public health system. As a consequence, it might serve as a reference when studying REs in Mexico and Latin America.
Disclosure
None of the authors has conflicts to declare with regards to this publication. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. The research was supported by the Universidad Autónoma de Aguascalientes, México. The views expressed are those of the authors and not necessarily those of the Department of Health in Aguascalientes.
Conflicts of interest
The authors have no conflicts of interest to declare.
References
- 1.Hashemi H., Fotouhi A., Yekta A., Pakzad R., Ostadimoghaddam H., Khabazkhoob M. Global and regional estimates of prevalence of refractive errors: Systematic review and meta-analysis. J Curr Ophthalmol. 2017;30:03–22. doi: 10.1016/j.joco.2017.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tarczy-Hornoch K. The epidemiology of early childhood hyperopia. Optom Vis Sci. 2007;84:115–123. doi: 10.1097/OPX.0b013e318031b674. [DOI] [PubMed] [Google Scholar]
- 3.Castagno V.D., Fassa A.G., Carret M.L.V., Vilela M.A.P., Meucci R.D. Hyperopia: A meta-analysis of prevalence and a review of associated factors among school-aged children. BMC Ophthalmol. 2014;14:163. doi: 10.1186/1471-2415-14-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mrugacz M., Gajecka M., Mrukwa-Kominek E., Witkowska K.J. Myopia: Risk factors, disease mechanisms, diagnostic modalities, and therapeutic options. J Ophthalmol. 2018;2018:1–4. doi: 10.1155/2018/7942379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holden B.A., Fricke T.R., Wilson D.A. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123:1036–1042. doi: 10.1016/j.ophtha.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 6.Shah R.L., Li Q., Zhao W. A genome-wide association study of corneal astigmatism: The CREAM Consortium. Mol Vis. 2018;124:127. [PMC free article] [PubMed] [Google Scholar]
- 7.Huang Y., Kee C.-S., Hocking P.M., Williams C., Yip S.P., Guggenheim J.A. A genome-wide association study for susceptibility to visual experience-induced myopia. IOVS. 2019;60:559–569. doi: 10.1167/iovs.18-25597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Simpson C.L., Wojciechowski R., Oexle K. Genome-wide meta-analysis of myopia and hyperopia provides evidence for replication of 11 loci. PLoS One. 2014;9:03–50. doi: 10.1371/journal.pone.0107110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saw S.-M., Hong C.-Y., Chia K.-S., Stone R.A., Tan D. Nearwork and myopia in young children. Lancet. 2001;357:390. doi: 10.1016/S0140-6736(05)71520-8. [DOI] [PubMed] [Google Scholar]
- 10.Rose K.A., Morgan I.G., Ip J. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology. 2008;115:1279–1285. doi: 10.1016/j.ophtha.2007.12.019. [DOI] [PubMed] [Google Scholar]
- 11.He M., Xiang F., Zeng Y. Effect of time spent outdoors at school on the development of myopia among children in China: A randomized clinical trial. Jama. 2015;314:1142–1248. doi: 10.1001/jama.2015.10803. [DOI] [PubMed] [Google Scholar]
- 12.Martínez‐Cortés G., Salazar-Flores J., Haro-Guerrero J. Maternal admixture and population structure in Mexican–Mestizos based on mtDNA haplogroups. Am J Phys Anthropol. 2013;151:526–1537. doi: 10.1002/ajpa.22293. [DOI] [PubMed] [Google Scholar]
- 13.Martinez-Cortes G., Salazar-Flores J., Fernandez-Rodriguez L.G. Admixture and population structure in Mexican-Mestizos based on paternal lineages. J Hum Genet. 2012;57:568–574. doi: 10.1038/jhg.2012.67. [DOI] [PubMed] [Google Scholar]
- 14.Garcia-Lievanos O., Sanchez-Gonzalez L., Espinosa-Cruz N., Hernandez-Flores L.A., Salmeron-Leal L., Torres-Rodriguez H.D. Myopia in schoolchildren in a rural community in the State of Mexico, Mexico. Clin Optom. 2016;8:53. doi: 10.2147/OPTO.S88353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Villarreal G.M., Ohlsson J., Cavazos H., Abrahamsson M., Mohamed J.H. Prevalence of myopia among 12-to 13-year-old schoolchildren in northern Mexico. Optom Vis Sci. 2003;80:369–373. doi: 10.1097/00006324-200305000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Grosvenor T.P. Primary Care Optometry. 5th ed. Butterworth-Heinemann Medical; Ed. St. Louis, Missouri: 2007. Cap 1. 03-75. [Google Scholar]
- 17.Harb E.N., Wildsoet C.F. Origins of refractive errors: Environmental and genetic factors. Annu Rev Vis Sci. 2019;5:47–72. doi: 10.1146/annurev-vision-091718-015027. [DOI] [PubMed] [Google Scholar]
- 18.Hashemi H., Rezvan F., Yekta A.A., Hashemi M., Norouzirad R., Khabazkhoob M. The prevalence of astigmatism and its determinants in a rural population of Iran: The “Nooravaran Salamat” mobile eye clinic experience. Middle East Afr J Ophthalmol. 2014;21:175–181. doi: 10.4103/0974-9233.129772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marasini S. Pattern of astigmatism in a clinical setting in Maldives. J Optometry. 2016;9:47–53. doi: 10.1016/j.optom.2015.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Durkin S.R., Tan E., Casson R., Selva D., Newland H. Romero who reported a prevalence of 20.6-39.1% in an Eye Clinic from Puerto Rico. Graefes Arch Clin Exp Ophthalmol. 2007;35:621–626. doi: 10.1111/j.1442-9071.2007.01555.x. [DOI] [PubMed] [Google Scholar]
- 21.Rodriguez N.M., Romero A.F. The prevalence of refractive conditions in Puerto Rican adults attending an eye clinic system. J Optom. 2014;7:161–167. doi: 10.1016/j.optom.2013.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Emerole C.G., Nneli R., Osim E. Astigmatism: Prevalence, distribution and determinants in Owerri, Nigeria. J Exp Clin Anat. 2013;12:87–91. [Google Scholar]
- 23.Ferguson D.A., Major G., Keldoulis T. Vision at work visual defect and the visual demand of tasks. Appl Ergon. 1974;5:84–93. doi: 10.1016/0003-6870(74)90084-2. [DOI] [PubMed] [Google Scholar]
- 24.Dirani M., Islam A., Shekar S.N., Baird P.N. Dominant genetic effects on corneal astigmatism: The genes in myopia (GEM) twin study. Invest Ophthalmol Vis Sci. 2008;49:1339–1344. doi: 10.1167/iovs.07-1011. [DOI] [PubMed] [Google Scholar]
- 25.Moore B., Lyons S.A., Walline J. A clinical review of hyperopia in young children. The Hyperopic Infants’ Study Group, THIS group. J Am Optom Assoc. 1999;70:215–224. [PubMed] [Google Scholar]
- 26.Olsen T., Arnarsson A., Sasaki H., Sasaki K., Jonasson F. On the ocular refractive components: The Reykjavik Eye Study. Acta Ophthalmol Scand. 2007;85:361–366. doi: 10.1111/j.1600-0420.2006.00847.x. [DOI] [PubMed] [Google Scholar]
- 27.Hashemi H., Iribarren R., Morgan I.G., Khabazkhoob M., Mohammad K., Fotouhi A. Increased hyperopia with ageing based on cycloplegic refractions in adults: The Tehran Eye Study. Br J Ophthalmol. 2010;94:20–30. doi: 10.1136/bjo.2009.160465. [DOI] [PubMed] [Google Scholar]
- 28.Hendler K., Mehravaran S., Lu X., Brown S.I., Mondino B.J., Coleman A.L. Refractive errors and amblyopia in the UCLA preschool vision program; first year results. Am J Ophthalmol. 2016;172:80–86. doi: 10.1016/j.ajo.2016.09.010. [DOI] [PubMed] [Google Scholar]
- 29.Schellini S.A., Durkin S.R., Hoyama E. Prevalence of refractive errors in a Brazilian population: The Botucatu eye study. Ophthalmic Epidemiol. 2009;16:90–97. doi: 10.1080/09286580902737524. [DOI] [PubMed] [Google Scholar]
- 30.Ehrlich D.L., Braddick O.J., Atkinson J. Infant emmetropization: Longitudinal changes in refraction components from nine to twenty months of age. Optom Vis Sci. 1997;74:822–843. doi: 10.1097/00006324-199710000-00022. [DOI] [PubMed] [Google Scholar]
- 31.Ingram R.M., Barr A. Changes in refraction between the ages of 1 and 3 1/2 years. Br J Ophthalmol. 1979;63:339–342. doi: 10.1136/bjo.63.5.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alemam Mohammed. Prevalence of myopia among children attending pediatrics ophthalmology clinic at Ohud hospital, Medina, Saudi Arabia. J Ophthalmol. 2018;2018:1–7. doi: 10.1155/2018/3708409. [DOI] [PMC free article] [PubMed] [Google Scholar]