Abstract
Background
Public health measures to contain the spread of COVID-19 have resulted in adverse effects, including high level of psychological distress, anxiety, and depression.
Aims
This study explored adolescent psychopathological profiles at age 17, and their role in predicting the impact of the COVID-19 pandemic at age 19.
Methods
The analyses used a sample of 904 participants (mean age = 19.17 years) from the Millennium Cohort Study (MCS) sweep 7 who completed the mental health questions from January 2018 to March 2019 (mean age = 17.18 years) and the COVID-19 Survey in May 2020. Adolescent psychopathological profiles were identified by means of latent class analysis.
Results
Four psychopathological profiles were identified: “low-symptom class” (60.17% of participants), “high-symptom class” (23.01% of participants), “substance/behavioural addictions class” (12.03% of participants), and “emotion-dysregulation class” (4.79% of participants). Adolescents in the high-symptom and emotional-dysregulation classes had the worst outcome during the lockdown. Specifically, they experienced more stress, conflict and loneliness, and lower levels of perceived social support than adolescents in the other psychopathological classes. Adolescents in the emotional-dysregulation class also consumed more alcohol and had worse financial situation during the lockdown compared to pre- lockdown period.
Conclusion
Adolescent psychopathological profiles predicted mental health impacts of the COVID-19 outbreak.
Keywords: Millennium Cohort Study, Psychopathological profiles, Adolescent, COVID-19
1. Introduction
On 23rd March 2020, the UK Prime Minister announced the “Stay at home” statement which required that “Everyone must stay at home to help stop the spread of coronavirus”. People were allowed to leave their home for the following specific reasons: “shopping for basic necessities, as infrequently as possible; one form of exercise a day - for example a run, walk, or cycle - alone or with members of your household; any medical need, to provide care or to help a vulnerable person; and travelling to and from work, but only where this is absolutely necessary and cannot be done from home.” (UK Government, 2020). The lockdown was slightly eased on May 10 and it was only on July 4 (the so-called “Super Saturday”) that the hospitality industry (i.e., pubs and restaurants) and hair salons were allowed to open. These restrictions have caused unprecedented disruptions in the way people live, work, study, and socialise.
While the full impact of the self-isolation/social distancing is unclear, the World Health Organisation (2020) has warned that this measure may result in people becoming more anxious, angry, stressed, and withdrawn. Indeed, studies are beginning to highlight the negative consequences of this measure on people's mental health (Fegert et al., 2020). Among the earliest studies that have examined the impact of the COVID-19 pandemic on mental health were conducted in China. For example, in a study that involved adults from 194 cities in China, approximately half (53.8%) of the participants rated the psychological impact of the pandemic as moderate or severe (Wang et al., 2020); 16.5% and 28.8% were reported to have moderate to severe depressive and anxiety symptoms, respectively. In another online survey in China (Huang and Zhao, 2020), the prevalence of sleep problems, generalised anxiety and depressive symptoms were reported to be 35.1%, 20.1%, and 18.2%, respectively.
Studies conducted in other countries such as in the USA (Liu et al., 2020), Spain (Gómez-Salgado et al., 2020), Brazil (Goularte et al., 2020; Passos et al., 2020), Hong Kong (Choi et al., 2020), Portugal and Brazil (Passos et al., 2020), Canada (Nwachukwu et al., 2020), Australia (Newby et al., 2020) and the UK (Lee et al., 2020) have similarly showed high level of psychological distress among adults in the general population. Elevated levels of mental health problems (e.g., anxiety, depression) and poor sleep quality have also been reported among studies involving children, adolescents and young people (Cao et al., 2020; McElroy et al., 2020; Orgilés et al., 2020; Morgül et al., 2020).
Factors which have been reported to increase the person's likelihood to experience poor mental health during the pandemic include (a) sociodemographic factors (e.g., females, low socio-economic status, low educational attainment, ethnicity, low annual income) (Goularte et al., 2020; Smith et al., 2020; Zhu et al., 2020), (b) occupational factors (e.g., frontline workers) (Huang and Zhao, 2020; Zhu et al., 2020), (c) pre-existing or history of mental health such as anxiety and depression, and loneliness (Liu et al., 2020; Goularte et al., 2020; Smith et al., 2020), (d) high exposure to COVID-19 (Cao et al., 2020; Newby et al., 2020) and longer period of social distancing (Goularte et al., 2020), and (e) pre-existing emotion regulation difficulties (Breaux et al., 2021; Machado et al., 2020). By contrast, engaging in preventative health measures (e.g., hand hygiene, wearing a mask) have been associated with lower level of distress (Newby et al., 2020). Sociodemographic factors such as living in urban areas, having a stable family income stability, and living with parents were associated with low level of anxiety (Cao et al., 2020). Other sociodemographic factors such as age has been inconsistent. While some studies found older compared to younger adolescents have higher levels of anxiety (Ahmed et al., 2020; McElroy et al., 2020), other studies have reported the opposite finding (Huang and Zhao, 2020; Smith et al., 2020).
While informative, findings of the above studies were conducted using cross-sectional design. As such it is not possible to derive any definitive conclusions about whether the pandemic caused greater mental health problems among individuals during the COVID-19 outbreak in the absence of pre-pandemic data. Studies with longitudinal design that enable comparing levels of mental health problems before and during the pandemic, and factors that determine that changes are lacking. From a developmental perspective, understanding the antecedents of psychopathology should be considered in order to better contextualize adjustment and symptom development in response to new challenges and environmental demands later in life (Thapar and Riglin, 2020). Unfortunately, most studies have focused on adults, thus, overlooking the influence of distal factors on current mental health. Moreover, studies that examined the psychological wellbeing of adolescents during the pandemic are lacking. Adolescence is a developmental stage for the development of social skills and a sense of identity which happen during social connections and peer interactions (Orben et al., 2020); the need for peer social approval and peer influence is of heightened importance in adolescence (Orben et al., 2020; Foulkes et al., 2018; Knoll et al., 2015). School closure and social distancing mean that adolescents have no or little opportunity to see their friends and peers, which could lead to educational setbacks and setbacks in their social and emotional skills. Furthermore, prior psychopathology may interact with risk factors leading to poorer adjustment to COVID lockdown and restrictions.
Therefore, the main aim of this study was to identify psychopathological profile of adolescents at age 17, and to examine its role in predicting the outcome of the COVID-19 pandemic at age 19. In line with our recent study (Essau and de la Torre-Luque, 2019), we expected to identify three psychopathological profiles (i.e., high emotional symptoms, high behavioural symptoms, high emotional-behavioural symptoms) which could predict the impact of the pandemic. Adolescents with high emotional-behavioural symptoms profile were hypothesized to have the highest level of psychological distress during the pandemic. Moreover, the presence of potential psychopathology factors (e.g., emotion dysregulation symptoms, such as self-harm or suicidal behaviour) would put the adolescents to have the worse psychological adjustment to COVID lockdown and restrictions. Adolescents with high emotional symptoms profile were hypothesized to have a high level of emotional problems during the pandemic, whereas those with high behavioural symptoms were hypothesized to have high level of substance consumption.
2. Method
2.1. Study design and participants
The sample for this study was drawn from the Millennium Cohort Study (MCS; Connelly and Platt, 2014) which is a nationally-representative birth cohort study among British millennials (i.e., toddlers born in the XXIst century). The aims of the MCS are to understand the developmental patterns of physical and mental health throughout the childhood and adolescence, and to identify protective and risk factors. The MCS cohort members were recruited using a stratified clustering strategy to ensure adequate representation of ethnic minorities across the UK administrative areas. The MCS collects data from parents, teachers and cohort members in the seven follow-up waves.
In May 2020, the University of London, the UK Institute of Education and the University College London (UCL) Centre for Longitudinal Studies launched a survey to study the impact of COVID-19 on participants who are followed in five longitudinal studies in the UK (i.e., the Millennium Cohort Study, Next Steps, 1970 British Cohort Study, and 1958 National Child Development Study). This recent survey included questions on physical and mental health symptoms (Brown et al., 2020; University of London et al., 2020) and data on the impact of the national lockdown to contain the spread of COVID-19.
Our study used data from the MCS sweep 7 survey and the COVID-19 Survey administered to MCS cohort members. More concretely, we used data from an initial sample of 10,533 UK citizens (50.20% males) who were surveyed at the MCS sweep 7. The participants were 17.18 years old on average (SD = 0.34) and were mostly White Caucasian (84.40% of participants). In the MCS sweep 7, a subsample of 2860 participants responded to the questions on mental health (54.51% women; 96.7% White Caucasian; m = 17.18 years, sd = 0.32); these responses were used to identify psychopathology profile (see below).
In the COVID-19 Survey, a total of 2536 MCS participants were surveyed (70.62% women, 88.25% White Caucasian; m = 19.17 years old, sd = 0.33). A sample of 904 participants (70.80% women, 97.56% White Caucasian; m = 19.17 years old, sd = 0.32) completed the mental health questions at both the MCS sweep 7 and the COVID-19 Survey. This sample was used in the present study (see in the Data analysis section).
2.2. Data collection and procedures
We used data on time-invariant, proximal and distal factors on the impact of the COVID-19 outbreak on adolescent's mental health. First, time-invariant data (sex and ethnicity) and adolescent's mental health (distal factors) data were used. These data were collected at the MCS sweep 7 survey when the participant was 17 years old. The adolescent mental health data consisted of a list of problematic behaviours and mental health symptoms. All the items were self-reported and included: heavy drinking behaviour (having engaged in 10 or more episodes of at least 5 drinks at a time in the last year), regular smoking (having smoked more than 5 cigarettes a week in last year), cannabis use (cannabis use in last year, with three responses categories: no use; sporadic [i.e., less than 10 times of cannabis use in last year]; and regular use [i.e., 10 times or more]); use of other drugs (at least once during the last year); having been arrested by a police officer and taken to a police station in last year; problematic video gaming (5 or more hours playing games using media devices on a normal week day); gambling (having spent money on either fruit machines, betting at a betting shop or online gambling in last month); poor sleep quality (based on the self-rated sleep quality over the past year); self-harm (having hurt themselves on purpose during the last year by: self-bruising, burning, pulling out their hair or cutting, or taking overdose of tablets); and suicide attempt (having hurt themselves on purpose to end life). Additionally, clinical mental health difficulties were measured using the Strength and Difficulties Questionnaire (SDQ; Goodman et al., 1998). More concretely, a SDQ total score greater than the 75th percentile was regarded as having mental health difficulties. The SDQ is a 25-item screening questionnaire to measure adolescent's strength and difficulties; each item can be scored on a 3-point Likert scale. Five dimensions (emotional symptoms, conduct problems, hyperactivity, peer problems and pro-social behaviour) can be derived from the SDQ as well as a total score. The total scores were obtained by adding all the SDQ subscales except for the pro-social behaviour subscale, with higher scores, indicating greater difficulties. The Cronbach Alpha of the total SDQ score in the present study was 0.80.
Second, the proximal factors to determine the influence of COVID-19 lockdown on mental health were taken from the COVID-19 Survey. For this purpose the following self-reported items were analyzed: having outdoor spaces in house; financial situation during the COVID-19 lockdown; and changes from the pre-lockdown in the household member composition, conflict level (whether the participant thinks that the number of conflict had increased), stress level (whether the participant had been feeling higher amount of stress), sleep time (less sleep time), smoking (number of cigarettes a day), and alcohol drinking (number of drinks a day). Finally, social support and loneliness feelings during the lockdown were also considered. The availability of social support was measured using a 3-item version of the Social Provisions Scale (Cutrona and Russell, 1983), which can be rated on a 3-point Likert scale. Psychometric properties of this scale in the COVID-19 MCS sample was satisfactory (α = 0.69). Loneliness was measured by the 3-item UCLA Loneliness Scale (Russell, 1996). The scale measures the frequency of current loneliness and related feelings on a 3-point scale. The Cronbach Alpha of the UCLA scale in the present study was 0.87.
The mental health impact of the COVID-19 pandemic was measured using four questionnaires: (a) K6 Kessler Distress Scale (Kessler et al., 2003) was used to measure the presence of psychological symptoms in the last 30 days. It contains six items which were rated on a 5-point Likert scale. The psychometric properties of the K6 in the present study was adequate (α = 0.87). (b) Warwick-Edinburgh Mental Wellbeing Scale (WEMWBS; Stewart-Brown et al., 2009) was used to measure mental wellbeing over the past two weeks. It contains seven items, which can be rated on a 5-point Likert scale. The psychometric properties of the WEMWBS was good, with Cronbach Alpha being 0.83. (c) Patient Health Questionnaire (PHQ-2; Kroenke et al., 2003) was used to measure the frequency of two depressive symptoms (i.e., depressed mood and anhedonia) over the past 2 weeks. Each item was to be rated from 0 (“not at all”) to 3 (“nearly every day”). (d) Generalised Anxiety Disorder Scale (GAD-2; Kroenke et al., 2007) was used to measure the frequency of two anxiety symptoms (i.e., “not being able to stop or control worrying” and “not being able to stop or control worrying”) over the past 2 weeks. Each item was to be rated from 0 (“not at all”) to 3 (“nearly every day”). Further details of the PHQ-2 and GAD-2 have been described elsewhere (Brown et al., 2020).
2.3. Data analysis
Attrition analysis (based on t-test for continuous variables, and χ2 test for dichotomous/categorical variables) was conducted to examine the way in which drop-out samples could affect the results by taking into account the drop-out rate at each follow-up assessments. In order to prevent from inflated type I error due to large sample size (Lin Jr. et al., 2013), meaningful between-group differences were considered as a sign of drop-out impact (i.e., those with at least medium effect size: Cohen's d ≥ 0.50 or Cramer's V ≥ 0.30).
Latent class analysis (LCA; Lanza and Cooper, 2016) was used to identify adolescent psychopathological profiles based on problematic behaviours and psychological symptoms collected on the MCS sweep 7 survey. This method allows modeling latent variable solutions with increasingly finite number of groups (adolescent psychopathological profiles) which were formed from the response of the same set of items. No covariates were used in latent class enumeration to prevent class overestimation (Lubke and Luningham, 2017; Vermunt, 2010). To select the model with an optimal class enumeration, two indexes were used: the Akaike's information criterion (AIC) and the sample-adjusted Bayesian information criterion (SABIC). The lower the AIC and SABIC, the better the model fit. Additionally, mean of posterior probabilities of belonging to each class should be greater than 0.70.
To determine the impact of the COVID-19 lockdown on adolescent's mental health, linear regression (K6 and WEMWBS scores) and generalised linear regression (PHQ-2 and GAD-2 scores, under gamma distribution) were used. Time-invariant, proximal factors (those studied during the lockdown) and the adolescent psychopathology profile (as a distal factor) were included as covariates. Regression models were weighted using the MCS weights. Multiple imputation procedures were used to estimate missing data on proximal factors, under a cut-off of 10 iterations to reach convergence for the solution with imputed values. The random forest algorithm was used to impute data. The adjusted R 2 (based on the Kullback-Leibler divergence method for generalised linear regression models) was used to estimate an effect size.
All the analyses were conducted by means of R x64 3.0.1 (poLCA, mice, effsize and psych packages).
3. Results
Table 1 displays the descriptive statistics of the samples in MCS Sweep 7 and in the COVID Survey. The attrition analysis revealed significant differences between samples who dropped out of the study and those who did not drop out. However, effect size of such differences was not meaningful (i.e., between-group differences did not reach a medium effect size: d < 0.50 or Cramer's V < 0.30), discarding potential effects of the drop-out rate on the analyses.
Table 1.
Descriptive statistics and attrition analyses.
| Initial sample (N = 10,533) | Sample used in the profile analysis (n = 2860) | Sample used in the COVID analysis (n = 904) | Attrition analysis |
||||
|---|---|---|---|---|---|---|---|
| Profile |
COVID sample |
||||||
| t / χ2 | ES | t / χ2 | ES | ||||
| Sex (% female) | 50.2 | 54.51 | 70.8 | 28.89⁎⁎ | 0.05 | 0.01 | 0 |
| Ethnicity (% non-White Caucasian) | 15.6 | 3.3 | 2.44 | 430.12⁎⁎ | 0.20 | 103.10⁎⁎ | 0.07 |
| Baseline age (years) | 17.18 (0.34) | 17.18 (0.32) | 17.17 (0.32) | 1.05 | 0.02 | −1.12 | −0.05 |
| Distal factors | |||||||
| Heavy drinking (% yes) | 16.05 | 15.82 | 20.10⁎⁎ | 0.03 | |||
| Regular smoking (% yes) | 6.71 | 4.98 | 0.12 | 0 | |||
| Cannabis use | 131.78⁎⁎ | 0.08 | |||||
| No use | 64.2 | 66.04 | |||||
| Sporadic | 28.92 | 29.54 | |||||
| Regular | 6.89 | 4.42 | |||||
| Other drugs (% yes) | 6.29 | 4.31 | 13.86⁎⁎ | 0.03 | |||
| Being arrested (% yes) | 1.57 | 0.55 | 0.32 | 0.01 | |||
| Problematic video gaming (% yes) | 16.64 | 10.95 | 0.02 | 0 | |||
| Gambling (% yes) | 16.61 | 12.83 | 17.26⁎⁎ | 0.03 | |||
| Sleep quality (% bad) | 33.46 | 33.74 | 6.52⁎ | 0.02 | |||
| Self-harm (% yes) | 28.5 | 33.74 | 24 | 0.03 | |||
| Suicide attempt (% yes) | 8.53 | 8.85 | 9.96⁎⁎ | 0.02 | |||
| Mental health difficulties1 (% over 75th percentile) | 26.22 | 25.66 | 0.1 | 0 | |||
| Proximal factors | |||||||
| Outdoor spaces in house (% no) | 3.44 | 0.52 | 0.01 | ||||
| Change in household members (% yes) | 29.24 | 6.25⁎ | 0.02 | ||||
| Financial management (% worse management) | 26.75 | 0.01 | 0 | ||||
| Change in conflict level (% more conflict around) | 23.19 | 2.52 | 0.01 | ||||
| Change in perceived stress (% more feelings of stress) | 44.1 | 1.3 | 0.01 | ||||
| Change in sleep time2 | 1.34 (0.83) | −0.13 | −0.01 | ||||
| Change in smoking pattern3 | −0.5 (3.67) | 1.93 | 0.23 | ||||
| Change in drinking pattern4 | 0.08 (0.27) | −1.32 | −0.07 | ||||
| Social provisions5 | 8.41 (1.02) | 0.02 | 0 | ||||
| Loneliness6 | 7.14 (2.26) | −0.88 | −0.04 | ||||
| Mental wellbeing7 | 22.99 (4.82) | 0.95 | 0.04 | ||||
| Mental distress8 | 8.62 (5.03) | −1.61 | −0.07 | ||||
| Anxiety symptoms9 | 3.94 (1.81) | −1.58 | −0.07 | ||||
| Depressive symptoms10 | 3.98 (1.69) | −1.7 | −0.07 | ||||
Note. Percentage of cases are displayed for dichotomous and categorical variables. Mean and standard deviation (between brackets) are displayed for continuous variables. Attrition analysis involves comparing the variables of interest between: 1) the sample of profile analysis (n = 2860) and the sample dropped out (n = 7673) from the initial sample (Profile attrition analysis); 2) the sample used in the COVID impact analysis (n = 904) with the sample dropped out (n = 1956) from the psychopathology profile analysis (COVID sample attrition analysis). The t -based tests (continuous variables) and χ2 tests (dichotomous/categorical variables) were used as contrast test statistics. Effect size (ES) estimates were the Cohen's d for continuous variables and Cramer's V for non-continuous ones.
The distal factor data were collected when participants were 17 years old (in 2018). The proximal factor data were collected on May 2020 (in times of the COVID-19 pandemic) when the participants were 19 years old.
Derived from the Strength and Difficulties Questionnaire total scores.
Differences between sleep hours before and during the COVID-19 lockdown.
Difference in the number of cigarettes smoked per day before and during the COVID-19 lockdown.
Difference in the number of alcohol drinks before and during the COVID-19 lockdown.
Measured using the Social Provisions Scale.
Measured using the UCLA Loneliness Scale.
Measured using the Warwick-Edinburgh Mental Health and Wellbeing Scale.
Measured using the Kessler K6 Scale.
Measured using the 2-item Generalised Anxiety Disorder Scale.
Measured using the 2-item Patient Health Questionnaire.
p < .05.
p < .01.
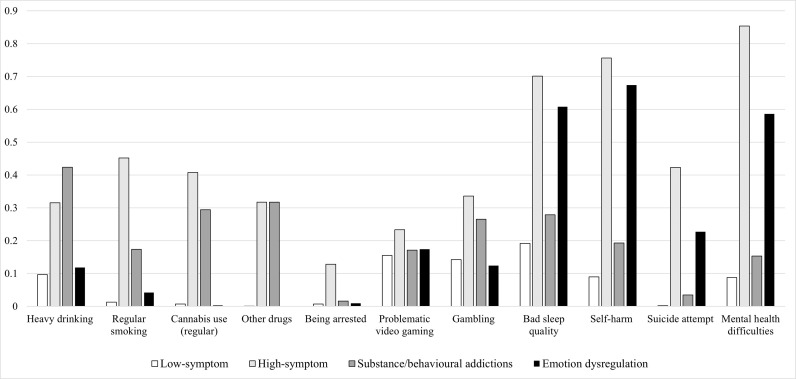
Analysis conducted to identify the adolescent psychopathological profile revealed that the 4-class model fitted better to data (see Table 2 ), as shown by its low AIC and SABIC (AIC = 26,059.55; SABIC = 26,201.392). Mean of posterior probabilities of being classified into each of the four profiles were between 0.79 and 0.86. Fig. 1 depicts the distribution of specific behaviours or symptoms across the four psychopathological profiles. The first profile (called “low-symptom class”; n = 1721, 60.17% of sample) consisted of adolescents with low levels of psychological symptoms. The second profile (called “high-symptom class”; n = 658, 23.01% of sample) consisted of adolescents with the highest risk of showing almost all the psychological symptoms and problematic behaviours. The third profile (called “substance/behavioural addictions class”; n = 344, 12.03% of sample) comprised adolescents at high risk of substance use (i.e., the highest probability of heavy drinking and drug use) and behavioural addictions (high level of gambling). Finally, the fourth profile (called “emotion-dysregulation class”; n = 137, 4.79% of sample) consisted of adolescents who reported having bad sleep quality and mental health difficulties, and symptoms indicative of poor emotion regulation (e.g., self-harm behaviour and attempted suicide).
Table 2.
Fit indexes for adolescent psychopathology profile solutions.
| Number of classes in the model |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
| LLiK | −13,819.20 | −13,279.47 | −13,052.76 | −12,978.77 | −12,954.45 | −12,924.59 | −12,906.24 | −12,889.16 | −12,885.11 | −12,860.57 |
| G2 | 2903.18 | 1823.73 | 1370.31 | 1222.34 | 1173.70 | 1113.97 | 1077.27 | 1043.11 | 1035.00 | 985.92 |
| AIC | 27,662.39 | 26,608.94 | 26,181.52 | 26,059.55 | 26,036.91 | 26,003.18 | 25,992.49 | 25,984.32 | 26,002.21 | 25,979.13 |
| SABIC | 27,695.77 | 26,678.47 | 26,287.21 | 26,201.39 | 26,214.91 | 26,217.34 | 26,242.80 | 26,270.79 | 26,324.83 | 26,337.91 |
Note. LLik = log-likelihood convergence value; G2 = conditional χ2 test statistic; AIC = Akaike information criterion; SABIC = Sample-adjusted Bayesian information criterion.
Fig. 1.
Adolescent psychopathological profile and the impact of COVID-19 outbreak.
Note. The symptoms are displayed on the X axis and the probability to show the symptom on the Y axis.
Each bar corresponds to each adolescent psychopathology class. The Mental health difficulties symptom was operationalised as showing a score over the 75th percentile on the Strength and Difficulties Questionnaire.
For the regression analyses, a total of 4206 values (10.07% of values in analysis) was imputed by means of multiple imputation procedures. Adolescents in the high-symptom and emotional-dysregulation classes were mostly women and had higher probability of experiencing higher amount of stress, conflict and loneliness, and lower levels of perceived social support (social provisions) than adolescents in the other psychopathological classes (Table 3 ). Adolescents in the emotional-dysregulation class also reported higher levels of alcohol consumption and had worse financial situation during than before the lockdown.
Table 3.
Descriptive statistics according to psychopathology profiles.
| Adolescent psychopathology class |
Contrast test |
ES |
||||
|---|---|---|---|---|---|---|
| Low-symptom | High-symptom | Substance/behavioural addictions | Emotion-dysregulation | |||
| n | 555 | 226 | 84 | 39 | ||
| Sex (% female) | 67.57 | 82.3 | 58.33 | 76.92 | 24.28⁎⁎ | 0.05 |
| Ethnicity (% non-White Caucasian) | 2.08 | 3.76 | 5.71 | 5.46 | 0.14 | 0.02 |
| Baseline age (years) | 17.17 (0.32) | 17.16 (0.32) | 17.23 (0.31) | 17.18 (0.35) | 1.06 | 0 |
| Proximal factors | ||||||
| Outdoor spaces in house (% no) | 3.07 | 3.98 | 2.38 | 7.69 | 2.83 | 0.01 |
| Change in household members (% yes) | 29.96 | 30.09 | 25 | 23.08 | 1.66 | 0.01 |
| Financial management (% worse management) | 22.74 | 30.8 | 28.57 | 56.41 | 24.07⁎⁎ | 0.03 |
| Change in conflict level (% more conflict around) | 19.75 | 32.59 | 15.85 | 33.33 | 19.52⁎⁎ | 0.03 |
| Change in perceived stress (% more feelings of stress) | 39.31 | 54.02 | 43.37 | 56.41 | 16.49⁎⁎ | 0.03 |
| Change in sleep time1 | 1.34 (0.84) | 1.37 (0.8) | 1.33 (0.84) | 1.32 (0.81) | 0 | 0 |
| Change in smoking pattern2 | −1.23 (2.58) | 0.11 (3.45) | −0.78 (5.08) | 0.91 (3.9) | 4 | 0.03 |
| Change in drinking pattern3 | 0.06 (0.24) | 0.1 (0.3) | 0.11 (0.31) | 0.18 (0.39) | 7.48⁎ | 0.01 |
| Social provisions4 | 8.59 (0.84) | 7.99 (1.23) | 8.63 (0.79) | 7.87 (1.38) | 23.47⁎⁎ | 0.03 |
| Loneliness5 | 6.66 (2.07) | 8.27 (2.32) | 6.73 (2.11) | 8.32 (2.17) | 33.78⁎⁎ | 0.04 |
Note. Sample in COVID-19 impact analysis was used (n = 904). Percentage of cases are displayed for dichotomous and categorical variables. Mean and standard deviation (between brackets) are displayed for continuous variables. The F -based test (continuous variables) and χ2 test (dichotomous/categorical variables) were used as contrast test statistics. Effect size (ES) estimates were the η2partial for continuous variables and Cramer's V for non-continuous ones.
The proximal factor data were collected in May 2020 (i.e., during the COVID-19 pandemic).
Difference in the length of sleep (in hours) before and during the COVID-19 lockdown.
Difference in the number of cigarettes smoked perday before and during the COVID-19 lockdown.
Difference in the number alcohol drinks before and during the COVID-19 lockdown.
Measured using the Social Provisions Scale.
Measured using the UCLA Loneliness Scale.
p < .05.
p < .01.
The regression models with the covariates explained a significant proportion of outcome variance (R 2 adj = 0.50, for mental distress; R 2 adj = 0.46, for mental wellbeing; R 2 adj = 0.35, for anxious symptoms; R 2 adj = 0.42, for depressive symptoms). Predictive coefficients of time-invariant, proximal and distal factors on lockdown-related mental health outcomes are displayed in Table 4 . Six covariates with significant loading (p < .05 for all the covariates) were found to explain the mental health outcomes: sex, social support, loneliness, changes in perceived stress and conflict levels, and psychopathological class membership. These findings showed that worse outcomes (i.e., higher mental distress, higher anxious and depressive symptom levels, and lower mental wellbeing) were associated with being woman, having lower social support (not involved in anxious symptom prediction), and experienced higher levels of stress, conflict, and loneliness. Moreover, being a member of the high-symptom class or the emotion-dysregulation class was associated with the worse mental health outcomes (in comparison to the low-symptom class) during the lockdown. However, the emotion-dysregulation class membership was not related to higher levels of depressive symptoms. Finally, increasing level of cigarette smoking during the lockdown was also associated with high psychological distress (B = 0.54, SE = 0.15; t = 3.50, p < .01).
Table 4.
Regression coefficients to explain COVID-19 impact on mental health outcomes.
| Mental distress |
Mental wellbeing |
Anxiety symptoms |
Depressive symptoms |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | t | B | SE | T | B | SE | t | B | SE | t | |
| (Intercept) | 5.31 | 0.26 | 20.76⁎⁎ | 25.28 | 0.26 | 98.29⁎⁎ | 1.03 | 0.03 | 36.75⁎⁎ | 1.14 | 0.02 | 46.81⁎⁎ |
| Sex (ref.: male) | ||||||||||||
| Female | 1.71 | 0.26 | 6.64⁎⁎ | −1.16 | 0.26 | −4.47⁎⁎ | 0.19 | 0.03 | 6.89⁎⁎ | 0.11 | 0.02 | 4.39⁎⁎ |
| Ethnic group (ref.: White Caucasian) | ||||||||||||
| Non-White Caucasian | −0.56 | 0.90 | −0.62 | 0.29 | 0.90 | 0.32 | 0.04 | 0.10 | 0.43 | −0.09 | 0.09 | −1.00 |
| Number of members in household | −0.01 | 0.14 | −0.08 | 0.09 | 0.14 | 0.63 | 0.01 | 0.02 | 0.52 | 0.01 | 0.01 | 1.05 |
| Outdoor spaces at home (ref.: yes) | 1.04 | 0.76 | 1.38 | 0.36 | 0.76 | 0.48 | 0.10 | 0.08 | 1.24 | 0.05 | 0.07 | 0.73 |
| Change in household composition | 0.18 | 0.26 | 0.68 | −0.12 | 0.26 | −0.48 | −0.01 | 0.03 | −0.25 | −0.03 | 0.02 | −1.12 |
| Financial management (ref.: similar or better management) | 0.31 | 0.26 | 1.18 | −0.08 | 0.27 | −0.29 | 0.01 | 0.03 | 0.30 | 0.00 | 0.03 | 0.19 |
| Change in sleep time1 | −0.07 | 0.11 | −0.65 | −0.05 | 0.11 | −0.42 | −0.01 | 0.01 | −1.15 | 0.00 | 0.01 | −0.31 |
| Social support2 | −0.50 | 0.15 | −3.27⁎⁎ | 0.92 | 0.15 | 5.93⁎⁎ | −0.01 | 0.02 | −0.77 | −0.03 | 0.01 | −2.11⁎ |
| Loneliness3 | 2.09 | 0.14 | 14.44⁎⁎ | −1.91 | 0.15 | −13.18⁎⁎ | 0.13 | 0.02 | 8.38⁎⁎ | 0.18 | 0.01 | 13.02⁎⁎ |
| Change in smoking pattern4 | 0.54 | 0.15 | 3.50⁎⁎ | −0.26 | 0.16 | −1.69 | 0.03 | 0.02 | 1.53 | 0.01 | 0.01 | 0.52 |
| Change in drinking pattern5 | 0.08 | 0.12 | 0.71 | −0.01 | 0.12 | −0.08 | 0.00 | 0.01 | 0.10 | 0.01 | 0.01 | 0.52 |
| Change in perceived stress (ref.: no more feelings of stress) | 2.12 | 0.24 | 8.66⁎⁎ | −1.79 | 0.25 | −7.30⁎⁎ | 0.22 | 0.03 | 8.11⁎⁎ | 0.16 | 0.02 | 6.85⁎⁎ |
| Change in conflict level (ref.: no more conflict around) | 0.94 | 0.29 | 3.28⁎⁎ | −1.03 | 0.29 | −3.60⁎⁎ | 0.10 | 0.03 | 3.32⁎⁎ | 0.12 | 0.03 | 4.35⁎⁎ |
| Adolescent psychopathology class (ref.: low-symptom class) | ||||||||||||
| High-symptom | 2.05 | 0.29 | 6.98⁎⁎ | −1.30 | 0.30 | −4.40⁎⁎ | 0.17 | 0.03 | 5.24⁎⁎ | 0.16 | 0.03 | 5.67⁎⁎ |
| Substance/behavioural addictions | 0.28 | 0.41 | 0.68 | 0.09 | 0.41 | 0.23 | −0.07 | 0.04 | −1.68 | −0.04 | 0.04 | −0.92 |
| Emotion-dysregulation | 2.14 | 0.62 | 3.49⁎⁎ | −1.97 | 0.62 | −3.18⁎⁎ | 0.17 | 0.07 | 2.46⁎ | 0.09 | 0.06 | 1.46 |
Note. Mental distress was measured using the Kessler K6 Scale. Mental wellbeing was measured using the Warwick-Edinburgh Mental Health and Wellbeing Scale (WEMHWS). Anxiety symptoms was measured using the 2-item Generalised Anxiety Disorder Scale (GAD-2). Depressive symptoms were measured using the 2-item Patient Health Questionnaire (PHQ-2). Linear regression was used to model mental distress (K6 score) and mental wellbeing (WEMHWS score) solutions. Generalised linear regression (under gamma distribution) was used to model anxious symptoms (GAD-2 score) and depressive symptoms (PHQ-2 score) solutions. All the regressions models were weighted using specific loading to ensure representativeness across the UK.
B = Regression loading. SE = Standard error of B. t = Contrast test.
Difference the duration of sleep (in hours) before and during the COVID-19 lockdown.
Measured using the Social Provisions Scale.
Measured using the UCLA Loneliness Scale.
Difference in the of number of cigarettes smoked per day before and during the COVID-19 lockdown.
Difference in the number of alcohol drinks before and during the COVID-19 lockdown.
p < .05.
p < .01.
4. Discussion
The present study adds to knowledge by examining the role of adolescent psychopathological profile at age 17 years in predicting the outcome of the COVID-19 pandemic at age 19 years. To our knowledge this study is the first to have examined the impact of existing or history of psychopathological symptoms on the mental health consequences of the lockdown. Data of 904 adolescents who participated in the MCS sweep 7 survey (mean age = 17.18 years) and the COVID-19 Survey (mean age = 19.17 years) who completed the mental health questions were analyzed.
The novelty of our finding was the identification of specific psychopathological profiles which predicted the mental health impact of COVID-19 pandemic. First, based on the MCS sweep 7 survey, four psychopathological profiles could be identified: “low-symptom class” (60.17% of participants), “high-symptom class” (23.01% of participants) “substance/behavioural addictions class” (12.03% of participants), and “emotion-dysregulation class” (4.79% of participants). The finding that 23% of the adolescents belonged to the “high-symptom class” is in agreement with the prevalence of mental disorders among adolescents as reported in numerous studies (Kessler et al., 2012; Merikangas et al., 2009; Shen et al., 2018). Furthermore, in line with findings of several studies, about 50% of mental disorders emerge in mid- to late-adolescence (Jones, 2013; Kessler et al., 2007).
Second, adolescents in the emotional-dysregulation class reported experiencing higher level of stress, conflict, and loneliness, and lower levels of perceived social support than adolescents in the other psychopathological classes; these adolescents also reported higher levels of alcohol consumption and had worse financial situation during than before the lockdown. These findings suggested that adolescents in the emotional-dysregulation class may have important deficits in coping with emotional distress. Ineffective coping in adolescence (e.g., they often engaged in self-harm behaviour) may reinforce the perceived inability to cope with the emotional demands of stressful situations, leading to worse psychological adjustment during the COVID-19 lockdown (Hatkevich et al., 2019; Rajappa et al., 2012). Adolescent's consumption of more alcohol during the lockdown compared to pre-lockdown period, maybe regarded as another ineffective strategy to cope with the psychological distress associated with the lockdown. Furthermore, the increasing pattern of cigarette smoking during the lockdown was also associated with psychological distress. This finding is in agreement with a recent statement by Clay and Parker (2020) who suggested that stress (e.g., uncertainty related to the pandemic and social distancing) and having trait impulsivity (i.e., act without adequate reflection) are important factors for alcohol use and misuse.
By contrast, some problematic behaviours (e.g., video gaming or betting) may buffer the impact of the COVID-19 lockdown on the emotional status which could explain why individuals in the substance/behavioural addictions profile showed a better mental health outcome. Several studies have reported an increase in at-home gambling, video gaming and internet use during the COVID-19 lockdown as people use these activities to cope with psychological distress associated with the lockdown (Håkansson, 2020; Lemenager et al., 2021). Furthermore, individuals with a history of behavioural problems (e.g., members of the Substance/behavioural addictions class) may be at higher risk of engaging at-home gambling and problematic internet use and video gaming during the COVID-19 lockdown (Jovic et al., 2020).
Third, adolescents in the high-symptom class had the worst mental health outcome during the lockdown. Interestingly, participants in the emotional-dysregulation class also showed poorer mental health outcome. Specifically, adolescents from both psychopathology classes similarly experienced more stress, conflict and loneliness, and lower levels of perceived social support than adolescents in the other psychopathological classes. This finding supports previous studies that showed the negative impact of the lockdown on children, adolescents and adults such as feelings of loneliness, anxiety and depression (Lei et al., 2020; Wang et al., 2020). However, individuals with a mental health history are likely to be disproportionately affected, and that those with ongoing symptoms are likely to show a worsening of symptoms (Chatterjee et al., 2020; Mazza et al., 2020). It can be argued that fear of contracting the virus (Holmes et al., 2020), the experience of physical distancing, and uncertainty about the future (Galea et al., 2020) could be particularly stressful to adolescents who have pre-existing mental health problems. The inability or limited access to mental health services and social supports may have further exacerbated mental health problems (Liu et al., 2020).
Fourth, most of the adolescents in the high-symptom or emotional-dysregulation classes were females. This finding supports previous studies which reported significantly more females than males are negatively affected by the COVID-19 pandemic (Goularte et al., 2020; Smith et al., 2020; Zhu et al., 2020). However, it should be noted that females generally showed higher prevalence of mental health difficulties (Essau et al., 2010) and poorer sleep quality (Fatima et al., 2016) and had higher rates of suicidal behaviours (Miranda-Mendizabal et al., 2019). While it is beyond the scope of this paper to examine factors associated with female's higher prevalence in mental health difficulties, previous studies have reported female's higher prevalence, compared to males, to be associated with numerous biological, social and psychological factors (Nolen-Hoeksema, 2001).
5. Strengths and limitations
A major strength of the study was the inclusion of a wide range of emotional and behavioural symptoms, and substance use and behavioural addictions which were used to identify four distinct psychopathological profiles in predicting the outcome of the pandemic. The study also covers a wide range of the proximal factors to determine the influence of the COVID-19 lockdown on adolescent's mental health. By integrating time-invariant, proximal and distal factors we can conceptually articulate combination of factors from a developmental perspective. The interaction of factors at different time may provide a wider and more naturalistic picture of the impact of the pandemic on adolescents. Adolescents with a history of mental health problems are particularly vulnerable to have the worse mental health outcomes as a result of the preventative measures to contain the spread of COVID-19 (Guessoum et al., 2020). For that reason, phenotype characterisation should become a priority for health care provision during and after the pandemic (Jefsen et al., 2020). The large sample size was based on nationally representative cohort with a longitudinal research design, with a wide range of sociodemographic and clinical data. However, the study also has several limitations. The data was based on participants' self-report which raise questions about reporting biases. Furthermore, as is common in longitudinal studies, missing data is inevitable problem. The male participants were largely underrepresented in this study although the male sample was large enough for the analyses to test the study hypotheses.
Overall, by identifying patterns of psychopathological profiles, the present study shed light into factors at age 17 years which predicted the outcomes of COVID-19 pandemic when the adolescents are 19 years. The adolescent psychopathological profiles may constitute modifiable factors which could form key targets for preventing the negative impact of the pandemic on adolescents.
Author statement
Both authors contributed to this manuscript. Prof Essau conceptualized the research questions, did the literature review, and the discussion. Dr. de la Torre-Luque tested the hypotheses, undertook the statistical analyses and interpreted the findings.
Funding
The Millennium Cohort Study is funded by the Economic and Social Research Council (ESRC) through grants awarded to the Centre for Longitudinal Studies (CLS). The most recent CLS award was ESRC grant reference number: ES/M001660/1.
Ethical statement
Ethical approval was not required for this study as the analysis involved secondary analysis of publicly available data.
Data availability
University of London, Institute of Education, Centre for Longitudinal Studies owns the copyright for the Millennium Cohort Study (MCS) data used in this study (2020). Millennium Cohort Study: Seventh Survey, 2018. [data collection]. UK Data Service. SN: 8682, https://doi.org/10.5255/UKDA-SN-8682-1
Declaration of Competing Interest
Both authors declare no conflicts of interest.
Acknowledgements
We are grateful to the Centre for Longitudinal Studies (CLS), UCL Social Research Institute, for the use of these data and to the UK Data Service for making them available. Neither CLS nor the UK Data Service bear any responsibility for the analysis or interpretation of these data.
References
- Breaux R., Dvorsky M.R., Marsh N.P., Green C.D., Cash A.R., Shroff D.M., Buchen N., Langberg J.M., Becker S.P. Prospective impact of COVID-19 on mental health functioning in adolescents with and without ADHD: protective role of emotion regulation abilities. J. Child Psychol. Psychiatry. 2021 doi: 10.1111/jcpp.13382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown M., Goodman A., Peters A., Ploubidis G.B., Sanchez A., Silverwood R., Smith K. 2020. COVID-19 Survey in Five National Longitudinal Studies: Wave 1 User Guide. London. [Google Scholar]
- Chatterjee S.S., Barikar C.M., Mukherjee A. Impact of COVID-19 pandemic on pre-existing mental health problems. Asian J. Psychiatry. 2020;51:102,071. doi: 10.1016/j.ajp.2020.102071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi E., Hui B., Wan E. Depression and Anxiety in Hong Kong during COVID-19. Int J Environ Res Public Health. 2020;17(10):3740. doi: 10.3390/ijerph17103740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clay J.M., Parker M.O. Alcohol use and misuse during the COVID-19 pandemic: A potential public health crisis? The Lancet Public Health. 2020;5:E259. doi: 10.1016/S2468-2667(20)30088-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connelly R., Platt L. Cohort profile: UK Millennium Cohort Study (mcs) Int. J. Epidemiol. 2014;43:1719–1725. doi: 10.1093/ije/dyu001. [DOI] [PubMed] [Google Scholar]
- Cutrona C.E., Russell D.W. In: Advances in Personal Relationships. Jones W.H., Perlman D., editors. Jessica Kingsley Publishers; London: 1983. The provisions of social relationships and adaptation to stress; pp. 37–67. [Google Scholar]
- Essau C.A., de la Torre-Luque A. Comorbidity profile of mental disorders among adolescents: A latent class analysis. Psychiatry Research. 2019;278:228–234. doi: 10.1016/j.psychres.2019.06.007. [DOI] [PubMed] [Google Scholar]
- Essau C.A., Lewinsohn P.M., Seeley John R., Sasagawa S. Gender differences in the developmental course of depression. Journal of Affective Disorders. 2010;127:185–190. doi: 10.1016/j.jad.2010.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fatima Y., Doi S.A., Najman J.M., Mamun A.A. Exploring gender difference in sleep quality of young adults: findings from a large population study. Clinical medicine & research. 2016;14(3–4):138–144. doi: 10.3121/cmr.2016.1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fegert J.M., Vitiello B., Plener P.L., Clemens V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc. Psychiatry. Ment. Health. 2020;14:1–11. doi: 10.1186/s13034-020-00329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foulkes L., Leung J.T., Fuhrmann D., Knoll L.J., Blakemore S.-J. Age differences in the prosocial influence effect. Dev Sci. 2018;2018:21e12666. doi: 10.1111/desc.12666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S., Merchant R.M., Lurie N. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMAIntern. Med. 2020 doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- Gómez-Salgado J., Andrés-Villas M., Domínguez-Salas S., Díaz-Milanés D., Carlos Ruiz-Frutos C. Related health factors of psychological distress during the COVID-19 pandemic in Spain. Int. J. Environ. Res. Public Health. 2020;17:3947. doi: 10.3390/ijerph17113947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman R., Meltzer H., Bailey V. The strengths and difficulties questionnaire: A pilot study on the validity of the self-report version. Eur. Child Adolesc. Psychiatry. 1998 doi: 10.1007/s007870050057. [DOI] [PubMed] [Google Scholar]
- Goularte J.F., Serafim S.D., Colombo R., Hogg B., Caldieraro M.A., Rosa A.R. COVID-19 and mental health in Brazil: Psychiatric symptoms in the general population. J Psychiatr Res. 2020;132:32–37. doi: 10.1016/j.jpsychires.2020.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guessoum S.B., Lachal J., Radjack R., Carretier E., Minassian S., Benoit L., Moro M.R. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020;291:113,264. doi: 10.1016/j.psychres.2020.113264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Håkansson A. Changes in gambling ehaviour during the COVID-19 pandemic—A web survey study in Sweden. Int. J. Environ. Res. Public Health. 2020 doi: 10.3390/ijerph17114013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatkevich C., Penner F., Sharp C. Difficulties in emotion regulation and suicide ideation and attempt in adolescent inpatients. Psychiatry Res. 2019 doi: 10.1016/j.psychres.2018.11.038. [DOI] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Silver R.C., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., Worthman C.M., Yardley L., Cowan K., Cope C., Hotopf M., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30168-1. 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Zhao N. Generalised anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry research. 2020;288:112,954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jefsen O.H., Rohde C., Norremark B., Ostergaard S.D. COVID-19 pandemic-related psychopathology in children and adolescents with mental illness. J. Child Psychol. Psychiatry. 2020 doi: 10.1111/jcpp.13292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones P. Adult mental health disorders and their age at onset. Br. J. Psychiatry. 2013;202(s54):s5e10. doi: 10.1192/bjp.bp.112.119164. [DOI] [PubMed] [Google Scholar]
- Jovic J., Pantovic-Stefanovic M., Mitkovic-Voncina M., Dunjic-Kostic B., Mihajlovic G., Milovanovic S., Ivkovic M., Fiorillo A., Latas M. Internet use during coronavirus disease of 2019 pandemic: Psychiatric history and sociodemographics as predictors. Indian J. Psychiatry. 2020 doi: 10.4103/psychiatry.IndianJPsychiatry_1036_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Barker P.R., Colpe L.J., Epstein J.F., Gfroerer J.C., Hiripi E., Howes M.J., Normand S.L.T., Manderscheid R.W., Walters E.E., Zaslavsky A.M. Screening for serious mental illness in the general population. Arch. Gen. Psychiatry. 2003 doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Amminger G.P., Aguilar-Gaxiola S., et al. Age of onset of mental disorders: A review of recent literature. Curr Opin Psychiatry. 2007;20:359. doi: 10.1097/YCO.0b013e32816ebc8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Avenevoli S., Costello E.J., Georgiades K., Green J.G., Gruber M.J., He J., Koretz D., McLaughlin K.A., Petukhova M., Sampson N.A., Zaslavsky A.M., Merikangas K.R. Prevalence, persistence, and sociodemographic correlates of DSM-IV disorders in the national comorbidity survey replication adolescent supplement. Arch. Gen. Psychiatry. 2012;69:372–380. doi: 10.1001/archgenpsychiatry.2011.160.Prevalence. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knoll L.J., Magis-Weinberg L., Speekenbrink M., Blakemore S.-J. Social influence on risk perception during adolescence. Psychol Sci. 2015;26:583–592. doi: 10.1177/0956797615569578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The patient health questionnaire-2: Validity of a two-item depression screener. Med. Care. 2003 doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W., Monahan P.O., Löwe B. Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Ann. Intern. Med. doi. 2007 doi: 10.7326/0003-4819-146-5-200,703,060-00004. [DOI] [PubMed] [Google Scholar]
- Lanza S.T., Cooper B.R. Latent class analysis for developmental research. Child Dev. Perspect. 2016;10:59–64. doi: 10.1111/cdep.12163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lei L., Huang X., Zhang S., Yang J., Yang L., Xu M. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in Southwestern China. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2020;26 doi: 10.12659/MSM.924609. e924609–1–e924609–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemenager T., Neissner M., Koopmann A., Reinhard I., Georgiadou E., Müller A., Kiefer F., Hillemacher T. Covid-19 lockdown restrictions and online media consumption in germany. Int. J. Environ. Res. Public Health. 2021 doi: 10.3390/ijerph18010014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin M., Jr., Shmueli G., Lin M. Too big to fail: large samples and the p -value problem. Inf. Syst. Res. 2013;7047:1–12. doi: 10.1287/isre.2013.0480. [DOI] [Google Scholar]
- Liu C.H., Stevens C., Conrad R.C., Hahm H.C. Evidence for elevated psychiatric distress, poor sleep, and quality of life concerns during the COVID-19 pandemic among U.S. young adults with suspected and reported psychiatric diagnoses. Psychiatry Research. 2020 doi: 10.1016/j.psychres.2020.113345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubke G.H., Luningham J. Fitting latent variable mixture models. Behav. Res. Ther. 2017;98:91–102. doi: 10.1016/j.brat.2017.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Machado P.P.P., Pinto-Bastos A., Ramos R., Rodrigues T.F., Louro E., Gonçalves S., Brandão I., Vaz A. Impact of COVID-19 lockdown measures on a cohort of eating disorders patients. J. Eat. Disord. 2020;8:57. doi: 10.1186/s40337-020-00340-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazza C., Ricci E., Biondi S., Colasanti M., Ferracuti S., Napoli C., Roma P. A nationwide survey of psychological distress among italian people during the COVID19 pandemic: immediate psychological responses and associated factors. Int. J. Environ. Res. Public Health. 2020;17:3165. doi: 10.3390/ijerph17093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McElroy E., Patalay P., Moltrecht B., Shevlin M., Shum A., Creswell C., Waite P. Demographic and health factors associated with pandemic anxiety in the context of COVID-19. British Journal of Health Psychology. 2020 doi: 10.1111/bjhp.12470. [DOI] [PubMed] [Google Scholar]
- Merikangas K.R., Avenevoli S., Costello E.J., Koretz D., Kessler R.C. National comorbidity survey replication adolescent supplement (NCS-A): I. Background and Measures. J. Am. Acad. Child Adolesc. Psychiatry. 2009;48:367–379. doi: 10.1097/CHI.0b013e31819996f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda-Mendizabal A., Castellví P., Parés-Badell O., et al. Gender differences in suicidal ehaviour in adolescents and young adults: systematic review and meta-analysis of longitudinal studies. International journal of public health. 2019;64(2):265–283. doi: 10.1007/s00038-018-1196-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgül E., Kallitsoglou A., Essau C.A. Psychological effects of the COVID-19 lockdown on children and families in the UK. Revista de Psicología Clínica con Niños y Adolescentes. J. Child and Adolesc. Clin. Psychol. 2020;7:42–48. [Google Scholar]
- Newby J.M., O’Moore K., Tang S., Christensen H., Faasse K. Acute mental health responses during the COVID-19 pandemic in Australia. PLoS ONE. 2020;15(7) doi: 10.1371/journal.pone.0236562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Gender differences in depression. Current directions. Psychological Science. 2001;10:173–176. [Google Scholar]
- Nwachukwu I., Nkire N., Shalaby R., Hrabok M., Vuong W., Gusnowski A., Surood S., Urichuk L., Greenshaw A.J., Agyapong V. COVID-19 Pandemic: Age-Related Differences in Measures of Stress, Anxiety and Depression in Canada. Int J Environ. Res. Public Health. 2020;17(17):6366. doi: 10.3390/ijerph17176366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orben A., Tomova L., Blakemore S.-J. The effects of social deprivation on adolescent development and mental health. The Lancet Child and Adolescent Health. 2020;4(8):634–640. doi: 10.1016/S2352-4642(20)30186-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orgilés M., Morales A., Delvecchio R., Mazzeschi C., Espada J.P. 2020. Immediate psychological effects of the COVID-19 quarantine in youth from Italy and Spain.https://psyarxiv.com/5bpfz Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Passos L., Prazeres F., Teixeira A., Martins C. Impact on mental health due to COVID-19 pandemic: cross-sectional study in Portugal and Brazil. Int. J. Environ. Res. Public Health. 2020;17(18):6794. doi: 10.3390/ijerph17186794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajappa K., Gallagher M., Miranda R. Emotion dysregulation and vulnerability to suicidal ideation and attempts. Cognit. Ther. Res. 2012 doi: 10.1007/s10608-011-9419-2. [DOI] [Google Scholar]
- Russell D.W. UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. J. Pers. Assess. 1996;66:20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- Shen Y.M., Chan B.S.M., Liu J.B., Zhou Y.Y., Cui X.L., He Y.Q., Fang Y., Xiang Y.T., Luo X.R. The prevalence of psychiatric disorders among students aged 6– 16 years old in central Hunan, China. BMC Psychiatry. 2018;18:1–9. doi: 10.1186/s12888-018-1823-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart-Brown S., Tennant A., Tennant R., Platt S., Parkinson J., Weich S. Internal construct validity of the Warwick-Edinburgh Mental Well-Being Scale (WEMWBS): A Rasch analysis using data from the Scottish Health Education Population Survey. Health Qual. Life Outcomes. 2009;7:1–8. doi: 10.1186/1477-7525-7-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thapar A., Riglin L. The importance of a developmental perspective in Psychiatry: what do recent genetic-epidemiological findings show? Mol. Psychiatry. 2020;25:1631–1639. doi: 10.1038/s41380-020-0648-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- University College London, UCL Institute of Education, Centre for Longitudinal Studies . 2nd. UK Data Service; 2020. COVID-19 Survey in Five National Longitudinal Cohort Studies: Millennium Cohort Study, Next Steps, 1970 British Cohort Study and 1958 National Child Development Study, 2020. [data collection] SN: 8658. [DOI] [Google Scholar]
- Vermunt J.K. Latent class modeling with covariates: Two improved three-step approaches. Polit. Anal. 2010;18:450–469. doi: 10.1093/pan/mpq025. [DOI] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization [WHO] 2020. WHO Coronavirus Disease (COVID-19) Dashboard.https://covid19.who.int/ Available online at: (accessed December 5, 2020) [Google Scholar]
- Zhu Z., Liu Q., Jiang X., Manandhar U., Luo Z., Zheng X., Li Y., Xie J., Zhang B. The psychological status of people affected by the COVID-19 outbreak in China. Journal of Psychiatric Research. 2020;129:1–7. doi: 10.1016/j.jpsychires.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
University of London, Institute of Education, Centre for Longitudinal Studies owns the copyright for the Millennium Cohort Study (MCS) data used in this study (2020). Millennium Cohort Study: Seventh Survey, 2018. [data collection]. UK Data Service. SN: 8682, https://doi.org/10.5255/UKDA-SN-8682-1