Abstract
Coronavirus disease 2019 (COVID-19) has resulted in a global pandemic, challenging both the medical and scientific community for the development of novel vaccines and a greater understanding of the effects of the SARS-CoV-2 virus. COVID-19 has been associated with a pronounced and out-of-control inflammatory response. Studies have sought to understand the effects of inflammatory response markers to prognosticate the disease. Herein, we aimed to review the evidence of 11 groups of systemic inflammatory markers for risk-stratifying patients and prognosticating outcomes related to COVID-19. Numerous studies have demonstrated the effectiveness of neutrophil to lymphocyte ratio (NLR) in prognosticating patient outcomes, including but not limited to severe disease, hospitalization, intensive care unit (ICU) admission, intubation, and death. A few markers outperformed NLR in predicting outcomes, including 1) systemic immune-inflammation index (SII), 2) prognostic nutritional index (PNI), 3) C-reactive protein (CRP) to albumin ratio (CAR) and high-sensitivity CAR (hsCAR), and 4) CRP to prealbumin ratio (CPAR) and high-sensitivity CPAR (hsCPAR). However, there are a limited number of studies comparing NLR with these markers, and such conclusions require larger validation studies. Overall, the evidence suggests that most of the studied markers are able to predict COVID-19 prognosis, however NLR seems to be the most robust marker.
Keywords: biomarkers, COVID-19, inflammation, inflammatory markers, prognosis, SARS-CoV-2
1 Introduction
Coronavirus disease 2019 (COVID-19) has emerged as a global challenge of the modern healthcare systems, resulting in more than 177 million confirmed cases and nearly 4 million deaths (1–3). Severe acute respiratory syndrome-coronavirus 2 (SARS-CoV-2) infection can involve various organs and produce a wide range of symptoms (4–9). Multiple organ involvement is thought to occur due to the almost universal distribution of angiotensin-converting enzyme 2 (ACE-2) that attaches to SARS-CoV-2 spike (S) protein receptor binding domain (RBD) and type 2 transmembrane serine proteases (TMPRSS2) that cleaves the S protein. It is thought that both these molecules may initiate immune evasion through various mechanisms (10–13).
It is well-documented that inflammatory mechanisms play a principal role in COVID-19-related organ dysfunction and mortality (14, 15). Patients with COVID-19 typically have higher inflammatory cytokines such as IL-6 and TNF-α compared with healthy individuals (16). Furthermore, patients with COVID-19 experience elevated levels of serologic indicators of inflammation, such as C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), lactate dehydrogenase (LDH), and procalcitonin (17, 18). These inflammatory cytokines may also alter the levels of various blood cell lineages and notably cause lymphocytopenia (18, 19). This hyperinflammation plays an important role in viral pathogenesis. However, it is also possible to use this proinflammatory response to risk-stratify COVID-19 patients at high risk of developing severe disease and respiratory complications (20).
Historically, markers of inflammation were used to successfully prognosticate patients with inflammatory diseases and, in particular, various types of cancers (21–25). Previous studies examined the role of inflammatory markers in other infectious diseases and demonstrated their ability to risk-stratify patients (26). Herein, we aimed to review the evidence for the effectiveness of systemic inflammatory markers in risk-stratifying patients and prognosticating outcomes related to COVID-19. The markers include neutrophil to lymphocyte ratio (NLR) and derived NLR (d-NLR), platelet to lymphocyte ratio (PLR), lymphocyte to monocyte ratio (LMR), lymphocyte to CRP ratio (LCR), fibrinogen to prealbumin ratio (FPR) and albumin to fibrinogen ratio (AFR), CRP to albumin ratio (CAR) and CRP to prealbumin ratio (CPAR), Glasgow prognostic score (GPS), modified GPS (mGPS), high-sensitivity mGPS (HS-mGPS), prognostic index (PI), prognostic nutritional index (PNI), systemic immune-inflammation index (SII), and interferon-alpha-inducible protein 27 (IFI27).
2 Inflammatory Markers
2.1 Neutrophil to Lymphocyte Ratio and Derived NLR
NLR is defined as the absolute neutrophil count (ANC)/absolute lymphocyte count (ALC) (27–29). d-NLR has a similar definition to NLR, calculated as ANC/(White blood cells (WBC) total count − ANC) (30). If we consider monocyte, basophil, and eosinophil levels as negligible (which are mostly not), the definition of these two markers would be equal. Earlier studies found links to higher NLR or d-NLR in chronic conditions with low-grade inflammatory nature, such as obesity, hypertension, diabetes mellitus, metabolic syndrome, atherosclerotic events of the heart and brain, and various cancers, although previous literature studied NLR more than d-NLR (27–29, 31–33). These underlying diseases are considered as risk factors for severe COVID-19 (2, 34, 35).
Since the beginning of the pandemic, studies have investigated the role of NLR in COVID-19 prognostication and its utility as a biomarker. NLR has been reported to prognosticate mortality, progression to severe disease, risk of intubation, risk of severe disease in intubated patients, days intubated, ICU admission, and longer intensive care unit (ICU) admission (30, 36–57). Two meta-analyses of n = 19 and n = 13 studies found significant associations between higher NLR and COVID-19 severity and mortality (58, 59). Furthermore, patients with higher NLR appear to have more comorbidities and, therefore, are more prone to severe COVID-19 (36). Even in patients with comorbidities, NLR might maintain its predictive ability for COVID-19 severity. For instance, NLR significantly predicted COVID-19 severity and survival in hospitalized patients with different types of cancers (60, 61). It has been suggested that each increased NLR unit resulted in an 8% higher mortality in COVID-19 patients (45).
A temporal analysis showed that on-admission NLR correlates well with the need for ICU and poor outcomes, and can be a potential risk-stratification tool. However, the clinical utility of NLR was lost in week 3 post-admission (62). The best predictive value of NLR can be achieved at its peak compared with its on-admission values (63). Concurrently, another study on the temporality of NLR found that day 7 measurement of NLR could significantly predict those requiring invasive mechanical ventilation and mortality, while measurement of day 1 NLR could not (64). In summary, on-admission NLR could predict COVID-19 prognosis. This predictive ability increases for a few days after admission, when NLR reaches its peak. However, NLR gradually loses its predictive ability as the patient recovers from COVID-19 and an associated reduction in inflammation. Finally, at week 3 post-admission, NLR loses its clinical utility to prognosticate severe COVID-19 outcomes.
Five studies proposed the ability of NLR to assist COVID-19 diagnosis (49, 65–68). They defined assisting COVID-19 diagnosis as significantly higher levels of NLR in individuals with COVID-19 compared with healthy controls. However, none of the studies mentioned how and due to what situations NLR can be integrated into COVID-19 diagnosis. Two other markers have been reported to be predictive for COVID-19 disease severity and mortality: granulocyte to lymphocyte ratio (69) and d-NLR (30, 70, 71).
2.1.1 NLR in Comparison With Other Markers
In Tables 1, 2, we compared NLR to other reported markers for COVID-19. We seperated the variables into those that have been reported for COVID-19 diagnosis and disease severity. Table 1 summarizes the studies comparing NLR to only LMR, PLR, and d-NLR. NLR had the highest predictive value compared with LMR, PLR, and d-NLR in most of the studies for severe COVID-19 parameters—disease severity, ICU admission, progression to acute respiratory distress syndrome (ARDS), need for mechanical ventilation, duration and expense of hospital stay, time to negative PCR, and mortality.
Table 1.
Studies comparing NLR to only PLR, LMR, and d-NLR among different measured variables.
| Study | Measured variable | Summary of findings |
|---|---|---|
| (49) | COVID-19 diagnosis | In intubated COVID-19 patients: higher NLR and PLR and lower LMR were observed compared with healthy individuals. |
| (65) | COVID-19 diagnosis | NLR, PLR, and MLR were all higher in COVID-19 patients [order of higher AUC: MLR (0.892) > PLR (0.748) > NLR (0.722)]. |
| (66) | COVID-19 diagnosis | Both NLR and PLR correlated (order of higher correlation: NLR > PLR). |
| (67) | COVID-19 diagnosis | Both NLR and PLR were higher is SARS-CoV-2 (+) patients [order of higher AUC: PLR (0.669) > NLR (0.615)]. |
| (30) | COVID-19 pneumonia | NLR correlated in the multivariate analysis, but d-NLR, LMR, and PLR did not. |
| (30) | Disease severity | NLR, d-NLR, and PLR correlated with disease severity (order of better prediction: NLR > d-NLR > PLR). LMR did not correlate. |
| (59) | Disease severity | In this meta-analysis, NLR correlated better than PLR (SMD: 2.80 vs. 1.82). |
| (72) | Disease severity | In patients with type 2 diabetes mellitus: both NLR and LMR correlated with disease severity (AUC: NLR = 0.730, p = 0.002; LMR = 0.322, p = 0.015). |
| (73) | Disease severity | NLR, d-NLR, and PLR correlated with disease severity [order of higher AUC: NLR (0.808) > d-NLR (0.803) > PLR (0.769)]. LMR did not correlate (AUC = 0.296). |
| (74) | Disease severity | NLR remained independently related in the logistic regression analysis. PLR only correlated in the univariate analysis. No correlation was observed for LMR. |
| (53) | Disease severity | NLR, PLR, and LMR could predict disease severity (order of higher AUC: NLR > LMR > PLR). |
| (65) | Progression to ARDS | NLR, PLR, and LMR predicted progression to ARDS. |
| (53) | ICU admission | Among patients with severe disease, NLR correlated with ICU admission, but LMR and PLR did not. |
| (75) | ICU admission | NLR, PLR, and LMR predicted ICU admission (order of better prediction: NLR > PLR > LMR). |
| (76) | Mechanical ventilation | NLR predicted the need for mechanical ventilation, but PLR did not. |
| (72) | Time to negative PCR | In patients with type 2 diabetes mellitus, NLR correlated (multivariate analysis), but LMR did not (univariate analysis). |
| (72) | Duration of hospital stay | In patients with type 2 diabetes mellitus, NLR independently correlated but LMR was not related in the univariate analysis. |
| (77) | In-hospital mortality | NLR and d-NLR correlated, but LMR and PLR did not. |
| (66) | Mortality | NLR correlated, but PLR did not. |
| (78) | All-cause mortality | NLR could predict this parameter, but PLR could not. |
| (72) | Hospital expenses | In patients with type 2 diabetes mellitus, NLR independently correlated but LMR did not correlate in the univariate analysis. |
NLR, neutrophil to lymphocyte ratio; PLR, platelet to lymphocyte ratio; LMR, lymphocyte to monocyte ratio; MLR, monocyte to lymphocyte ratio; d-NLR, derived-NLR; AUC, area under the curve; SMD, standardized mean difference; ARDS, acute respiratory distress syndrome; ICU, intensive care unit; PCR, polymerase chain reaction.
Table 2.
Studies comparing NLR with other biomarkers (studies involving discussed markers other than PLR, LMR, and d-NLR) among different measured variables.
| Study | Measured variable | Summary of findings |
|---|---|---|
| (68) | COVID-19 diagnosis | SII and NLR were higher in patients with SARS-CoV-2 diagnosis in the multivariate analysis (order of higher AUC: SII > NLR). PLR did not correlate. |
| (71) | Disease severity | Higher hsCAR, higher hsCPAR, and lower PNI correlated in the multivariate analysis, but d-NLR and SII only correlated in the univariate analysis. NLR, PLR, LMR, and AFR did not correlate. |
| (79) | Disease severity | Both CAR and NLR predicted disease severity in the multivariate analysis, but CAR had higher OR (OR = 17.65, p = 0.001 vs. OR = 1.51, p = 0.007). |
| (80) | Disease severity | In this meta-analysis, both NLR and LCR predicted disease severity [order of better prediction: NLR (SMD: 2.404) > LCR (SMD: −0.912)] |
| (61) | Mortality | In cancer patients: higher NLR, lower PNI, higher mGPS, and higher PI all predicted an increased mortality (p < 0.0001 for all), PLR did not. |
| (70) | Mortality | NLR, d-NLR, SII, and PNI all predicted mortality. |
| (81) | Mortality | NLR, d-NLR, and SII all predicted mortality in the univariate analysis; however, only SII was significant in the multivariate analysis. |
| (82) | Mortality | PNI independently predicted mortality in the multivariate analysis (AUC: 0.849). NLR and PLR significantly correlated in the univariate analysis. |
| (64) | Mortality, ICU admission, requiring invasive mechanical ventilation, and dialysis | Higher LCR on day 1 predicted an increased need for ICU admission and invasive mechanical ventilation. NLR could not predict any of the variables on day 1. Lower LCR on day 7 predicted increased mortality, while higher NLR correlated with requiring invasive mechanical ventilation and mortality. |
SII, systemic immune-inflammation index; NLR, neutrophil to lymphocyte ratio; PLR, platelet to lymphocyte ratio; AUC, area under the curve; hsCAR, high-sensitivity C-reactive protein to albumin ratio; hsCPAR, high-sensitivity C-reactive protein to prealbumin ratio; PNI, prognostic nutritional index; LMR, lymphocyte to monocyte ratio; d-NLR, derived-NLR; AFR, albumin to fibrinogen ratio; CAR, C-reactive protein to albumin ratio; OR, odds ratio; LCR, lymphocyte to C-reactive protein ratio; SMD, standardized mean difference; mGPS, modified Glasgow prognostic score; PI, prognostic index.
We first compared disease severity reported by seven studies (Table 1) (30, 53, 59, 71–74). One of these was a meta-analysis of 20 studies, 19 on NLR and 5 on PLR, that found a correlation between higher NLR and PLR with disease severity. However, the mean standardized difference (SMD) for NLR was higher than PLR (2.80 versus 1.82) (59). Five of the six remaining studies found NLR superior to d-NLR, PLR, and LMR (30, 53, 71–74). The other study found d-NLR to be the only predictive marker in the univariate but not multivariate analysis among these four. NLR, PLR, and LMR did not correlate with disease severity (71).
NLR, PLR, and LMR could predict ICU admission in hospitalized patients; however, NLR (AUC: 0.861) could predict ICU admission better than PLR (AUC: 0.715) and LMR (AUC: 0.705) (75). Sun et al. concluded similarly and stated that only NLR correlated with the risk of ICU admission, while LMR and PLR did not (53). NLR, monocyte to lymphocyte ratio (MLR), and PLR could all predict progression to ARDS (65). Higher NLR could predict the need for mechanical ventilation (p = 0.003), but PLR was similar between patients requiring ventilation and those not (p = 0.41) (76).
NLR outperformed in prognosticating mortality compared with PLR (61, 66, 77, 78) and LMR (77). Three studies comparing NLR and d-NLR found that both could predict mortality (70, 77, 81).
While NLR had a greater predictive power for severe COVID-19 parameters, it did not seem to correlate with COVID-19 diagnosis compared with PLR and LMR. The studies defined correlating with COVID-19 diagnosis as having significantly different levels in COVID-19 positive and negative patients. Five studies compared NLR, PLR, and LMR based on their diagnostic ability (Table 1) (49, 65–68). Lissoni et al. specifically compared intubated COVID-19 patients and healthy individuals. They concluded that lower LMR, higher NLR, and higher PLR were observed in intubated patients with COVID-19 compared with healthy controls (49). Among the remaining four studies, NLR correlated better than PLR in two studies (66, 68) and worse in two others (65, 67). Only one of these studies contained the MLR, the inverted LMR variable (65). In this study, MLR had the highest AUC to differentiate healthy individuals from COVID-19 patients (0.892), followed by PLR (0.748) and NLR (0.722) (65). Overall, NLR was not superior to LMR and PLR in assisting diagnosis, but data are insufficient on this part to determine the best marker.
Only nine studies compared NLR to markers other than PLR, LMR, and d-NLR (61, 64, 68, 70, 71, 79–82) (Table 2). These studies provide valuable evidence but are not sufficient for an extensive assessment. Five of these studies measured NLR and SII (61, 68, 70, 71, 81), two of them without the possibility to compare the predictive ability of NLR and SII (61, 70). These two studies—one of them in cancer patients—found that NLR, d-NLR, SII, PNI, and mGPS could predict COVID-19 mortality, but it was not possible to determine the best predictive marker in these studies (61, 70). SII was superior to NLR in all the other three remaining studies comparing NLR and SII (68, 71, 81); one study related COVID-19 diagnosis (68), one for disease severity (71), and one for mortality (81). SII was also superior to d-NLR, MLR, and PLR in predicting mortality, with a small hazard ratio (HR = 1.0001, p = 0.029) (81).
Xue et al. concluded that hsCAR, hsCPAR, and PNI predicted COVID-19 severity in the multivariate analysis, while d-NLR and SII only correlated in the univariate analysis. NLR, LMR, PLR, and AFR could not predict severe COVID-19 (71). This study concluded the superiority of hsCAR, hsCPAR, and PNI. PNI was superior to NLR in predicting mortality and CAR in predicting disease severity, each in one study (79, 82).
In the study of Lagunas-Rangel, NLR was superior to LCR in predicting disease severity (SMD: NLR = 2.404, LCR = −0.912), although both were significant predictors (P: NLR = 0.001, LCR < 0.001) (80).
Altogether, these data suggest that some markers might produce more promising results than NLR, such as SII, PNI, CAR and hsCAR, and CPAR and hsCPAR. However, these markers are less studied compared with NLR. Although this section contained some of the comparison of other variables, a detailed discussion on each marker follows.
2.2 Platelet to Lymphocyte Ratio
PLR could help in diagnosing COVID-19. Four studies found a significant difference in the PLR of patients with positive SARS-CoV-2 compared to healthy individuals (49, 65–67), while only one concluded against this (68).
Two meta-analyses confirmed the effectiveness of higher PLR on predicting COVID-19 severity (59, 83). Higher PLR also correlated with an increased risk of severe disease in intubated COVID-19 patients (49). This ability to predict disease severity seemed to be optimal at its peak. PLR at peak could predict disease severity in the multivariate regression analysis; however, PLR at admission did not correlate with disease severity in the univariate analysis (84). Two studies studied the ability of PLR to predict ICU admission, and they produced conflicting results on this matter (53, 75).
Although PLR could predict disease severity in most of the studies, it was not able to predict mortality (61, 66, 77, 78), one specifically in cancer patients (61). Similarly, another study concluded that PLR is only slightly prognostic in predicting mortality in the univariate analysis among hospitalized patients (p < 0.001), but not in the multivariate analysis (p = 0.154) (82).
Owing to all the strengths of PLR in predicting various COVID-19-related parameters, it is a potentially suitable marker to triage COVID-19 patients. However, it seems to lack potentials to predict mortality and have a lower ability than NLR to predict several parameters.
2.3 Lymphocyte to Monocyte Ratio
Unlike neutrophil and monocyte count, a decrease in lymphocyte count correlated to multiorgan injury in COVID-19 patients (85). This was shown by Kazancioglu et al recently. However, in their study, monocyte count only correlated to SARS-CoV-2 infection but not severity (69). These studies provide the hypothetical bases for the prognostic value of LMR in COVID-19, as well as NLR and PLR.
Two studies compared the effectiveness of LMR in COVID-19 diagnosis, both finding a significant relationship between LMR and testing positive for SARS-CoV-2. In one of them, MLR (AUC: 0.892) was the best predictor compared with NLR and PLR, and 0.23 was declared the best MLR cutoff point (65). In another, significantly lower LMR was observed in intubated COVID-19 patients compared with healthy controls (49).
LMR did not correlate with disease severity in most studies (30, 71, 73, 74) except two (53, 72). Liu et al. showed that higher LMR could only significantly predict disease severity in the univariate analysis and also did not correlate with a longer hospital stay, higher hospital costs, and longer time to negative PCR (72). LMR could prognosticate progression to ARDS (65).
In two studies examining the ability to predict ICU admission, LMR did not correlate in one (53), and correlated but was inferior to NLR and PLR in the other (75). Data are limited regarding the ability of LMR to predict COVID-19 mortality; however, a study concluded the ineffectiveness of LMR in prognosticating this parameter (77).
LMR might have limited benefits in prognosticating COVID-19 (86), but its abilities seem to be lower than NLR and PLR, especially in predicting disease severity, ICU admission, and mortality. However, we encourage future studies to pursue the ability of LMR to recognize SARS-CoV-2 positive patients, as it demonstrated promises.
2.4 Lymphocyte to C-Reactive Protein Ratio
A limited number of studies examined this marker. The most important article on this is perhaps a meta-analysis on the role of LCR in predicting disease severity. They found a significantly lower LCR in patients with severe disease (SMD = −0.912, p < 0.001); however, it was less predictive compared with NLR (SMD = 2.404, p = 0.001). They based their results on five studies for each marker (80).
Higher LCR on day 1 predicted the need for ICU admission (adjusted OR: 3.1, p = 0.003) and invasive mechanical ventilation (adjusted OR: 2.5, p = 0.009), but could not predict in-hospital mortality (p = 0.60) and requiring dialysis (p = 0.44). Nevertheless, lower LCR on day 7 only correlated with an increased in-hospital mortality risk (adjusted OR: 0.1, 95% CI = 0.01–0.30, p < 0.0001) but not with the other factors (64).
2.5 Fibrinogen to Prealbumin Ratio and Albumin to Fibrinogen Ratio
Similar to most of the discussed markers, studies demonstrate a prognostic role for FPR and AFR in some cancers and other diseases with inflammatory pathophysiology (87–89). Nevertheless, only a few articles studied them to determine COVID-19 disease severity.
Lower AFR correlated with severe COVID-19 in univariate analysis (p < 0.0001), but not multivariate analysis (p = 0.079) (71). However, fibrinogen to albumin ratio (FAR), remained significant in predicting disease severity in the multivariate analysis in another study (HR = 4.058, 95% CI = 1.246–13.222, p = 0.020) (90).
2.6 C-Reactive Protein to Albumin Ratio and C-Reactive Protein to Prealbumin Ratio
CAR could predict disease severity in two studies (79, 91): one comparing it with NLR and finding a higher OR for CAR (OR = 17.652, p = 0.001) than NLR (OR = 1.512, p = 0.007) (79). However, the other study did not find as large an OR for CAR (1.264, p = 0.037) (91).
hsCAR and hsCPAR differ from their counterparts as they utilize high-sensitivity CRP (92). Xue et al. found that on-admission hsCAR, hsCPAR, and PNI significantly correlated with severe COVID-19 in the multivariate analysis among several other markers (NLR, LMR, FPR, PLR, SII, AFR). Furthermore, among these markers, only hsCPAR and hsCAR correlated with hospital stay length (71). In the Oh et al. study, hsCAR could also predict in-hospital mortality in adults older than 65 years of age after adjusting for confounders (92).
Taken together, CAR and CPAR seemed promising in predicting disease severity, mortality, and length of hospital stay in all the studies, although we only identified four studies. Furthermore, a small study hailed prealbumin and CRP as potential markers to effectively triage patients in the early stages, and prealbumin seemed to be more effective (93).
2.7 Glasgow Prognostic Score, Modified GPS, and High-Sensitivity mGPS
GPS constitutes two main serum components, CRP and albumin levels, both having a potential of 0 or 1 score. CRP >10 mg/L and albumin <3.5 mg/dl receive one point each, and the score classifies the patients into three total scores of 0, 1, or 2. mGPS does not allocate a score to hypoalbuminemia without a rise in CRP to above 10 mg/L. hs-mGPS provides a similar classification to mGPS with a lower CRP threshold (>3 mg/L) (94, 95). These markers also have proven roles in predicting various cancers (94, 95).
In a study of 397 patients with COVID-19, no deaths occurred among 40 patients with hs-mGPS score of 0, while 10/263 (3.80%) and 24/94 (25.53%) of patients scoring 1 and 2 died, respectively (70). Concurrently, Dettorre et al. found that mGPS was able to foretell the overall survival of hospitalized cancer patients infected with COVID-19 (11.4%, 30.4%, and 50.6% for mGPS = 0 to mGPS = 2, respectively; p < 0.0001) (61). These two studies found promising results for mGPS and hs-mGPS and set the grounds for future research to better identify its effectiveness.
2.8 Prognostic Index
PI is similar to the GPS, only differing in the WBC component. WBC >11,000/µl and CRP >10 mg/L contribute to this scoring system of 0 to 2 (22).
We could only find one study discussing this marker in COVID-19. In that study, PI was able to predict the survival of cancer patients infected with COVID-19 (9.1%, 40%, and 50%, for scores of 0 to 2), similar to NLR, PNI, and mGPs. PI seemed superior to PLR in the study. Patients categorized in the poor-risk group (PI = 2) had 23 days median overall survival, while patients with favorable scores did not reach the required follow-up duration (all p-values less than 0.0001) (61).
2.9 Prognostic Nutritional Index
Onodera et al. proposed PNI as an immune-nutritional risk score for malnourished cancer patients undergoing for gastrointestinal surgery, formulizing it as serum albumin concentration (g/L) + 0.005 × total lymphocyte count (per mm3 of peripheral blood) (96, 97). This marker later demonstrated its effectiveness in prognosticating several types of cancer (98).
Three studies investigated the relationship between COVID-19 mortality and PNI, all showing significant correlations (61, 70, 82). Two studies were on hospitalized COVID-19 patients (70, 82) and another on patients with cancer (61). PNI also predicted disease severity better than other markers in the study of Xue et al., alongside hsCAR, and hsCPAR. Together, they were put into a nomogram that could predict disease severity well (C-index = 0.873) (71).
PNI successfully predicted disease severity and mortality in all the four studies examining it; therefore, it can be a suitable candidate for follow-up studies.
2.10 Systemic Immune-Inflammation Index
SII is defined as platelet count × NLR (99). SII remained a reliable predictor in most of the conducted studies on COVID-19 so far. Usul et al. found its superior predictive ability than NLR and PLR in COVID-19 diagnosis, as its values were significantly different in SARS-CoV-2-positive and -negative individuals. The proposed SII for helping in the COVID-19 diagnosis was 479.1 (68).
Xue et al. studied the relationship between several markers and disease severity. They found that SII could significantly predict disease severity in the univariate but not the multivariate analysis, inferior to hsCAR, hsCPAR, and PNI, but still better than several markers, such as NLR (71).
Two studies studied SII in predicting mortality, both finding significant correlations (70, 81). One of them found that SII was the only significant marker in the multivariate analysis, superior to NLR and d-NLR, but with a slight hazard ratio (HR = 1.0001, p = 0.029) (81).
2.11 Interferon-Alpha Inducible Protein 27
IFI27 is a part of the innate immune system highly induced by interferon (IFN)-α (100). High expression of IFI27 may also induce cell proliferation and invasion and reduce apoptosis, making it a possible oncogene (100, 102).
Type I IFN deficiency can be a marker of severe COVID-19 (103). Some of the IFN-stimulated genes (ISGs) like IFI27 were upregulated in patients with COVID-19 (104–107) and later downregulated in the recovery process (108, 109). IFI27 was overexpressed in various cell lineages of SARS-CoV-2-infected patients compared with healthy controls (110). In another study, IFI27 demonstrated a higher than two-fold upregulation in A549 and normal human bronchial epithelial (NHBE) cells infected with SARS-CoV-2 (111). Shaath et al. analyzed the bronchoalveolar lavage of 10 individuals. IFI27 was among the genes upregulated in the peripheral blood mononuclear cells (PBMC) of severe and mild COVID-19 patients, compared with two healthy controls (112).
IFI27 might also help distinguish COVID-19 from other acute respiratory illnesses and some viral diseases such as Ebola, SARS, MERS, and H1N1, as SARS-CoV-2, even at low loads, induced IFI27 more than other viruses (113, 114).
There is a lack of robust clinical evidence concerning IFI27-related prognostic value for COVID-19; however, ISGs and, particularly, IFI27 seem to be interesting for conducting further studies.
3 Conclusion
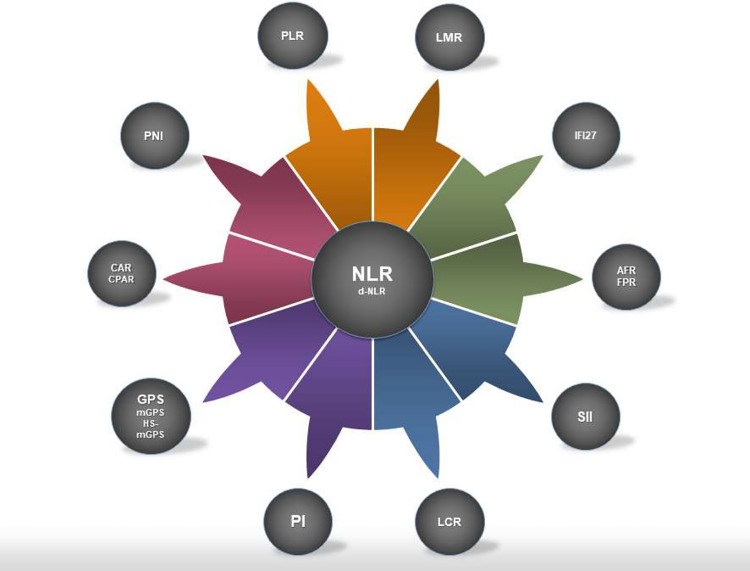
NLR seems to have the highest prognosticating potential among the biomarkers discussed in this study, because of its predictive value and availability for data across multiple studies, including meta-analyses. Therefore, this amplitude of evidence might increase its reliability to risk-stratify patients and help medical decision-making. Nevertheless, some other markers might also be promising, such as SII, PNI, CAR and hsCAR, and CPAR and hsCPAR, but other aspects of their prognostication need to be further studied (Figure 1). Careful comparisons require future meta-analyses.
Figure 1.
Systemic inflammation markers discussed in this study. NLR is illustrated in the middle as it was the most studied marker with strong prognosticating capabilities. However, some of the less studied markers reviewed in the study might have the potential to overtake the predictive value of NLR. NLR, neutrophil to lymphocyte ratio; d-NLR, derived NLR; PLR, platelet to lymphocyte ratio; LMR, lymphocyte to monocyte ratio; LCR, lymphocyte to C-reactive protein ratio; FPR, fibrinogen to prealbumin ratio; AFR, albumin to fibrinogen ratio; CAR, C-reactive protein to albumin ratio; CPAR, C-reactive protein to prealbumin ratio; GPS, Glasgow prognostic score; mGPS, modified GPS; hs-mGPS, high-sensitivity mGPS; PI, prognostic index; PNI, prognostic nutritional index; SII, systemic immune-inflammation index; IFI27, interferon-alpha inducible protein 27.
Several studies discussed the markers for specific subgroups, such as patients with underlying diabetes or cancer. Many of these conditions might be inflammatory in nature, and they might hypothetically alter the effectiveness of some markers.
The need for risk-stratifying COVID-19 patients also encouraged some researchers to design new markers for this purpose that should be examined in studies, such as COVID-19 severity-Iraqi index (CSI) measured by MLR × lactate dehydrogenase (LDH)/upper normal LDH value (115). Another study hypothesized combining functional and nutritional indices with the well-known CURB-65 pneumonia severity index (116).
Some of the presented markers may only require a complete blood count with differentials, a cheap and straightforward test. The other markers also require routine and widely available laboratory tests. Therefore, stratifying the risks of patients using these methods has the potential of being widely available.
Some important pitfalls and limitations exist that future research need to address. First, studies need to estimate the cost-effectiveness of triaging the patients with these biomarkers, as almost all of them seemed to be useful to various degrees. Second, there is a lack of sufficient evidence for many of these biomarkers. Some of these markers have the potential to be better prognosticators than NLR, but need further studies to confirm their abilities and provide sufficient evidence. Third, we encourage researchers to hypothesize novel biomarkers best-fitted to COVID-19 pathophysiology and test their hypotheses to understand their effectiveness. We also encourage future research on specific subgroups with certain underlying conditions, as the most suitable biomakers for those groups might differ from the overall population. At last, various COVID-19 variants are showing different specific outcomes of morbidity and mortality (117). Therefore, we suggest future researchers to update the findings related to systemic inflammatory markers specifically for emerging variants.
Author Contributions
AKa: conception, drafting of the initial manuscript, and revision of the final manuscript. PS: conception, drafting of the initial manuscript, and figure visualization. AKu: conception and careful revision of the manuscript draft. NR: conception and careful revision of the manuscript draft. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1. Lambert H, Gupte J, Fletcher H, Hammond L, Lowe N, Pelling M, et al. COVID-19 as a Global Challenge: Towards an Inclusive and Sustainable Future. Lancet Planet Health (2020) 4(8):e312–e4. doi: 10.1016/S2542-5196(20)30168-6 [DOI] [PubMed] [Google Scholar]
- 2. Mehraeen E, Karimi A, Barzegary A, Vahedi F, Afsahi AM, Dadras O, et al. Predictors of Mortality in Patients With COVID-19-a Systematic Review. Eur J Integr Med (2020) 40:101226. doi: 10.1016/j.eujim.2020.101226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. The World Health Organization . WHO Coronavirus Disease (COVID-19) Dashboard (2021). Available at: https://covid19.who.int/.
- 4. Shafi AMA, Shaikh SA, Shirke MM, Iddawela S, Harky A. Cardiac Manifestations in COVID-19 Patients—A Systematic Review. J Cardiac Surg (2020) 35(8):1988–2008. doi: 10.1111/jocs.14808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mehraeen E, Seyed Alinaghi SA, Nowroozi A, Dadras O, Alilou S, Shobeiri P, et al. A Systematic Review of ECG Findings in Patients With COVID-19. Indian Heart J (2020) 72(6):500–7. doi: 10.1016/j.ihj.2020.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Qiu Y, He J-S, Tan J-Y, Lin S-N, Mao R. Gastrointestinal and Liver Involvement in Patients With COVID-19 – Authors' Reply. Lancet Gastroenterol Hepatol (2020) 5(9):799–800. doi: 10.1016/S2468-1253(20)30240-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Thaweerat W. Current Evidence on Pancreatic Involvement in SARS-CoV-2 Infection. Pancreatology (2020) 20(5):1013–4. doi: 10.1016/j.pan.2020.05.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Momtazmanesh S, Shobeiri P, Hanaei S, Mahmoud-Elsayed H, Dalvi B, Rad EM. Cardiovascular Disease in COVID-19: A Systematic Review and Meta-Analysis of 10,898 Patients and Proposal of a Triage Risk Stratification Tool. Egypt Heart J (2020) 72(1):1–17. doi: 10.1186/s43044-020-00075-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Seyed ASA, Karimi A, Shobeiri P, Nowroozi A, Mehraeen E, Afsahi AM, et al. Psychological Symptoms of COVID-19 Epidemic: A Systematic Review of Current Evidence. Psihologija (2020) 54(2)173–92. doi: 10.2298/PSI200703035S [DOI] [Google Scholar]
- 10. SeyedAlinaghi S, Mehrtak M, MohsseniPour M, Mirzapour P, Barzegary A, Habibi P, et al. Genetic Susceptibility of COVID-19: A Systematic Review of Current Evidence. Eur J Med Res (2021) 26(1):46. doi: 10.1186/s40001-021-00516-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shang J, Wan Y, Luo C, Ye G, Geng Q, Auerbach A, et al. Cell Entry Mechanisms of SARS-CoV-2. Proc Natl Acad Sci (2020) 117(21):11727. doi: 10.1073/pnas.2003138117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mollica V, Rizzo A, Massari F. The Pivotal Role of TMPRSS2 in Coronavirus Disease 2019 and Prostate Cancer. Future Oncol (London England) (2020) 16(27):2029–33. doi: 10.2217/fon-2020-0571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Deng Q, Rasool RU, Russell RM, Natesan R, Asangani IA. Targeting Androgen Regulation of TMPRSS2 and ACE2 as a Therapeutic Strategy to Combat COVID-19. iScience (2021) 24(3):102254. doi: 10.1016/j.isci.2021.102254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Merad M, Martin JC. Pathological Inflammation in Patients With COVID-19: A Key Role for Monocytes and Macrophages. Nat Rev Immunol (2020) 20(6):355–62. doi: 10.1038/s41577-020-0331-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Vabret N, Samstein R, Fernandez N, Merad M. Advancing Scientific Knowledge in Times of Pandemics. Nat Rev Immunol (2020) 20(6):338. doi: 10.1038/s41577-020-0319-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Del Valle DM, Kim-Schulze S, Huang H-H, Beckmann ND, Nirenberg S, Wang B, et al. An Inflammatory Cytokine Signature Predicts COVID-19 Severity and Survival. Nat Med (2020) 26(10):1636–43. doi: 10.1038/s41591-020-1051-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ali N. Elevated Level of C-Reactive Protein May Be an Early Marker to Predict Risk for Severity of COVID-19. J Med Virol (2020) 92(11):2409–11. doi: 10.1002/jmv.26097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ghahramani S, Tabrizi R, Lankarani KB, Kashani SMA, Rezaei S, Zeidi N, et al. Laboratory Features of Severe vs.Non-Severe COVID-19 Patients Asian Populations: syst Rev meta-anal. Eur J Med Res (2020) 25(1):30. doi: 10.1186/s40001-020-00432-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tavakolpour S, Rakhshandehroo T, Wei EX, Rashidian M. Lymphopenia During the COVID-19 Infection: What It Shows and What Can Be Learned. Immunol Lett (2020) 225:31–2. doi: 10.1016/j.imlet.2020.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. RECOVERY Collaborative Group. Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, et al. Dexamethasone in Hospitalized Patients With Covid-19. New Engl J Med (2020) 384(8):693–704. doi: 10.1056/NEJMoa2021436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wang C, He W, Yuan Y, Zhang Y, Li K, Zou R, et al. Comparison of the Prognostic Value of Inflammation-Based Scores in Early Recurrent Hepatocellular Carcinoma After Hepatectomy. Liver Int Off J Int Assoc Study Liver (2020) 40(1):229–39. doi: 10.1111/liv.14281 [DOI] [PubMed] [Google Scholar]
- 22. Yamamoto M, Kobayashi T, Kuroda S, Hamaoka M, Okimoto S, Honmyo N, et al. Verification of Inflammation-Based Prognostic Marker as a Prognostic Indicator in Hepatocellular Carcinoma. Ann gastroenterol Surg (2019) 3(6):667–75. doi: 10.1002/ags3.12286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cui K, Ou Y, Shen Y, Li S, Sun Z. Clinical Value of Circulating Tumor Cells for the Diagnosis and Prognosis of Hepatocellular Carcinoma (HCC): A Systematic Review and Meta-Analysis. Medicine (2020) 99(40):e22242. doi: 10.1097/MD.0000000000022242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Tang M, Jia Z, Zhang J. The Prognostic Role of Prognostic Nutritional Index in Nasopharyngeal Carcinoma: A Systematic Review and Meta-Analysis. Int J Clin Oncol (2021) 26(1):66–77. doi: 10.1007/s10147-020-01791-x [DOI] [PubMed] [Google Scholar]
- 25. Sirin MC, Korkmaz S, Erturan I, Filiz B, Aridogan BC, Cetin ES, et al. Evaluation of Monocyte to HDL Cholesterol Ratio and Other Inflammatory Markers in Patients With Psoriasis. Anais brasileiros dermatol (2020) 95(5):575–82. doi: 10.1016/j.abd.2020.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Russell CD, Parajuli A, Gale HJ, Bulteel NS, Schuetz P, de Jager CPC, et al. The Utility of Peripheral Blood Leucocyte Ratios as Biomarkers in Infectious Diseases: A Systematic Review and Meta-Analysis. J Infect (2019) 78(5):339–48. doi: 10.1016/j.jinf.2019.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Templeton AJ, McNamara MG, Šeruga B, Vera-Badillo FE, Aneja P, Ocaña A, et al. Prognostic Role of Neutrophil-to-Lymphocyte Ratio in Solid Tumors: A Systematic Review and Meta-Analysis. JNCI: J National Cancer Institute (2014) 106:(6):dju124. doi: 10.1093/jnci/dju124 [DOI] [PubMed] [Google Scholar]
- 28. Tokgoz S, Kayrak M, Akpinar Z, Seyithanoğlu A, Güney F, Yürüten B, et al. Neutrophil Lymphocyte Ratio as a Predictor of Stroke. J Stroke Cerebrovascular Dis (2013) 22(7):1169–74. doi: 10.1016/j.jstrokecerebrovasdis.2013.01.011 [DOI] [PubMed] [Google Scholar]
- 29. Balta S, Celik T, Mikhailidis DP, Ozturk C, Demirkol S, Aparci M, et al. The Relation Between Atherosclerosis and the Neutrophil–Lymphocyte Ratio. Clin Appl Thrombosis/Hemostasis (2016) 22(5):405–11. doi: 10.1177/1076029615569568 [DOI] [PubMed] [Google Scholar]
- 30. Yang A-P, Liu J-P, Tao W-Q, Li H-M. The Diagnostic and Predictive Role of NLR, D-NLR and PLR in COVID-19 Patients. Int Immunopharmacol (2020) 84:106504. doi: 10.1016/j.intimp.2020.106504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Karaman M, Balta S, Ahmet AYS, Cakar M, Naharci I, Demirkol S, et al. The Comparative Effects of Valsartan and Amlodipine on vWf Levels and N/L Ratio in Patients With Newly Diagnosed Hypertension. Clin Exp Hypertens (2013) 35(7):516–22. doi: 10.3109/10641963.2012.758734 [DOI] [PubMed] [Google Scholar]
- 32. Balta S, Kurtoglu E, Kucuk U, Demirkol S, Ozturk C. Neutrophil–lymphocyte Ratio as an Important Assessment Tool. Expert Rev Cardiovascular Ther (2014) 12: (5):537–8. doi: 10.1586/14779072.2014.902309 [DOI] [PubMed] [Google Scholar]
- 33. Caputo D, Caricato M, Coppola A, La Vaccara V, Fiore M, Coppola R. Neutrophil to Lymphocyte Ratio (NLR) and Derived Neutrophil to Lymphocyte Ratio (D-NLR) Predict Non-Responders and Postoperative Complications in Patients Undergoing Radical Surgery After Neo-Adjuvant Radio-Chemotherapy for Rectal Adenocarcinoma. Cancer Invest (2016) 34(9):440–51. doi: 10.1080/07357907.2016.1229332 [DOI] [PubMed] [Google Scholar]
- 34. Zheng Z, Peng F, Xu B, Zhao J, Liu H, Peng J, et al. Risk Factors of Critical & Mortal COVID-19 Cases: A Systematic Literature Review and Meta-Analysis. J Infect (2020) 81(2):e16–25. doi: 10.1016/j.jinf.2020.04.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Meng Y, Lu W, Guo E, Liu J, Yang B, Wu P, et al. Cancer History is an Independent Risk Factor for Mortality in Hospitalized COVID-19 Patients: A Propensity Score-Matched Analysis. J Hematol Oncol (2020) 13(1):75. doi: 10.1186/s13045-020-00907-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tatum D, Taghavi S, Houghton A, Stover J, Toraih E, Duchesne JJS. Neutrophil-To-Lymphocyte Ratio and Outcomes in Louisiana Covid-19 Patients. Shock (2020) 54(5):652–8. doi: 10.1097/SHK.0000000000001585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Cheng B, Hu J, Zuo X, Chen J, Li X, Chen Y, et al. Predictors of Progression From Moderate to Severe Coronavirus Disease 2019: A Retrospective Cohort. Clin Microbiol Infect (2020) 26(10):1400–5. doi: 10.1016/j.cmi.2020.06.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Yan X, Li F, Wang X, Yan J, Zhu F, Tang S, et al. Neutrophil to Lymphocyte Ratio as Prognostic and Predictive Factor in Patients With Coronavirus Disease 2019: A Retrospective Cross-Sectional Study. J Medical Virol (2020) 92(11):2573–81. doi: 10.1002/jmv.26061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Asghar MS, Kazmi SJH, Khan NA, Akram M, Khan SA, Rasheed U, et al. Clinical Profiles, Characteristics, and Outcomes of the First 100 Admitted COVID-19 Patients in Pakistan: A Single-Center Retrospective Study in a Tertiary Care Hospital of Karachi. Cureus (2020) 12(6):e8712. doi: 10.7759/cureus.c34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Basbus L, Lapidus MI, Martingano I, Puga MC, Pollán JJM. Neutrophil to Lymphocyte Ratio as a Prognostic Marker in COVID-19. Medicina (Buenos Aires) (2020) 80:31–6. [PubMed] [Google Scholar]
- 41. Li H, Zhao M, Xu Y. Biochemical Analysis Between Common Type and Critical Type of COVID-19 and Clinical Value of Neutrophil/Lymphocyte Ratio. Nan Fang Yi Ke Da Xue Xue Bao (2020) 40(7):965–71. doi: 10.12122/j.issn.1673-4254.2020.07.08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ok F, Erdogan O, Durmus E, Carkci S, Canik A. Predictive Values of Blood Urea Nitrogen/Creatinine Ratio and Other Routine Blood Parameters on Disease Severity and Survival of COVID-19 Patients. J Medical Virol (2020) 93(2):786–93. doi: 10.1002/jmv.26300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Zhang B, Zhou X, Zhu C, Song Y, Feng F, Qiu Y, et al. Immune Phenotyping Based on the Neutrophil-to-Lymphocyte Ratio and IgG Level Predicts Disease Severity and Outcome for Patients With COVID-19. Front Mol Biosci (2020) 7:157. doi: 10.3389/fmolb.2020.00157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Zhang J-J, Cao Y-Y, Tan G, Dong X, Wang B-C, Lin J, et al. Clinical, Radiological, and Laboratory Characteristics and Risk Factors for Severity and Mortality of 289 Hospitalized COVID-19 Patients. Allergy (2020) 76(2):533–50. doi: 10.22541/au.159164076.65659447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Liu Y, Du X, Chen J, Jin Y, Peng L, Wang HH, et al. Neutrophil-To-Lymphocyte Ratio as an Independent Risk Factor for Mortality in Hospitalized Patients With COVID-19. J Infect (2020) 81(1):e6–12. doi: 10.1016/j.jinf.2020.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Liu Y-P, Li G-M, He J, Liu Y, Li M, Zhang R, et al. Combined Use of the Neutrophil-to-Lymphocyte Ratio and CRP to Predict 7-Day Disease Severity in 84 Hospitalized Patients With COVID-19 Pneumonia: A Retrospective Cohort Study. Ann Transl Med (2020) 8(10):635. doi: 10.21037/atm-20-2372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Xia X, Wen M, Zhan S, He J, Chen W. [An Increased Neutrophil/Lymphocyte Ratio Is an Early Warning Signal of Severe COVID-19]. Nan fang yi ke da xue xue bao = J South Med Univ (2020) 40(3):333–6. doi: 10.12122/j.issn.1673-4254.2020.03.06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Vafadar Moradi E, Teimouri A, Rezaee R, Morovatdar N, Foroughian M, Layegh P, et al. Increased Age, Neutrophil-to-Lymphocyte Ratio (NLR) and White Blood Cells Count Are Associated With Higher COVID-19 Mortality. Am J Emergency Med (2021) 40:11–4. doi: 10.1016/j.ajem.2020.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Lissoni P, Rovelli F, Monzon A, Privitera C, Messina G, Porro GJJIA. Evidence of Abnormally Low Lymphocyte-to-Monocyte Ratio in Covid-19-Induced Severe Acute Respiratory Syndrome. J Immunol Allergy (2020) 1(2):1–6. doi: 10.37191/Mapsci-2582-6549-1(2)-011 [DOI] [Google Scholar]
- 50. Fei M, Tong F, Tao X, Wang J. Value of Neutrophil-to-Lymphocyte Ratio in the Classification Diagnosis of Coronavirus Disease 2019. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue (2020) 32(5):554–8. doi: 10.3760/cma.j.cn121430-20200413-00506 [DOI] [PubMed] [Google Scholar]
- 51. Liu J, Liu Y, Xiang P, Pu L, Xiong H, Li C, et al. Neutrophil-To-Lymphocyte Ratio Predicts Critical Illness Patients With 2019 Coronavirus Disease in the Early Stage. J Transl Med (2020) 18:1–12. doi: 10.1186/s12967-020-02374-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Shang W, Dong J, Ren Y, Tian M, Li W, Hu J, et al. The Value of Clinical Parameters in Predicting the Severity of COVID-19. J Medical Virol (2020) 92(10):2188–92. doi: 10.1002/jmv.26031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Sun S, Cai X, Wang H, He G, Lin Y, Lu B, et al. Abnormalities of Peripheral Blood System in Patients With COVID-19 in Wenzhou, China. Clin Chimica Acta (2020) 507:174–80. doi: 10.1016/j.cca.2020.04.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Wang C, Deng R, Gou L, Fu Z, Zhang X, Shao F, et al. Preliminary Study to Identify Severe From Moderate Cases of COVID-19 Using Combined Hematology Parameters. Ann Transl Med (2020) 8(9):593. doi: 10.21037/atm-20-3391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Zha Q, Feng B, Li X, Zhou D, Kang Y, Qin HJLM. Study on Early Laboratory Warning of Severe COVID-19. Lab Med (2020) 35(06):557–60. [Google Scholar]
- 56. Chen F-F, Zhong M, Liu Y, Zhang Y, Zhang K, Su D-Z, et al. The Characteristics and Outcomes of 681 Severe Cases With COVID-19 in China. J Crit Care (2020) 60:32–7. doi: 10.1016/j.jcrc.2020.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Song H, Bai T, Shi J, Yang J. Predictive Value of Multiple Inflammatory Indexes on the Prognosis of Patients With Corona Virus Disease 2019. Pract J Cardiac Cereb Pneumal Vascular Dis (2020) 28(06):13–6. [Google Scholar]
- 58. Li X, Liu C, Mao Z, Xiao M, Wang L, Qi S, et al. Predictive Values of Neutrophil-to-Lymphocyte Ratio on Disease Severity and Mortality in COVID-19 Patients: A Systematic Review and Meta-Analysis. Crit Care (2020) 24(1):647. doi: 10.1186/s13054-020-03374-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Chan AS, Rout A. Use of Neutrophil-To-Lymphocyte and Platelet-To-Lymphocyte Ratios in COVID-19. J Clin Med Res (2020) 12(7):448–53. doi: 10.14740/jocmr4240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Ma J, Yin J, Qian Y, Wu Y. Clinical Characteristics and Prognosis in Cancer Patients With COVID-19: A Single Center's Retrospective Study. J Infect (2020) 81(2):318–56. doi: 10.1016/j.jinf.2020.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Dettorre G, Diamantis N, Loizidou A, Piccart M, Chester J, Jackson A, et al. 319o The Systemic Pro-Inflammatory Response Identifies Cancer Patients With Adverse Outcomes From SARS-CoV-2 Infection. Ann Oncol (2020) 31:S1366–S. doi: 10.1016/j.annonc.2020.10.313 [DOI] [Google Scholar]
- 62. Khourssaji M, Chapelle V, Evenepoel A, Belkhir L, Yombi JC, van Dievoet M-A, et al. A Biological Profile for Diagnosis and Outcome of COVID-19 Patients. Clin Chem Lab Med (CCLM) (2020) 58(12):2141–50. doi: 10.1515/cclm-2020-0626 [DOI] [PubMed] [Google Scholar]
- 63. Jimeno S, Ventura PS, Castellano JM, García-Adasme SI, Miranda M, Touza P, et al. Prognostic Implications of Neutrophil-Lymphocyte Ratio in COVID-19. Eur J Clin Invest (2021) 51(1):e13404. doi: 10.1111/eci.13404 [DOI] [PubMed] [Google Scholar]
- 64. Ullah W, Basyal B, Tariq S, Almas T, Saeed R, Roomi S, et al. Lymphocyte-To-C-Reactive Protein Ratio: A Novel Predictor of Adverse Outcomes in COVID-19. J Clin Med Res (2020) 12(7):415–22. doi: 10.14740/jocmr4227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Peng J, Qi D, Yuan G, Deng X, Mei Y, Feng L, et al. Diagnostic Value of Peripheral Hematologic Markers for Coronavirus Disease 2019 (COVID-19): A Multicenter, Cross-Sectional Study. J Clin Lab Anal (2020) 34(10):e23475. doi: 10.1002/jcla.23475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Eslamijouybari M, Heydari K, Maleki I, Moosazadeh M, Hedayatizadeh-Omran A, Vahedi L, et al. Neutrophil-To-Lymphocyte and Platelet-To-Lymphocyte Ratios in COVID-19 Patients and Control Group and Relationship With Disease Prognosis. Caspian J Intern Med (2020) 11(Suppl 1):531–5. doi: 10.22088/cjim.11.0.531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Seyit M, Avci E, Nar R, Senol H, Yilmaz A, Ozen M, et al. Neutrophil to Lymphocyte Ratio, Lymphocyte to Monocyte Ratio and Platelet to Lymphocyte Ratio to Predict the Severity of COVID-19. Am J Emergency Med (2021) 40:110–4. doi: 10.1016/j.ajem.2020.11.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Usul E, Şan İ, Bekgöz B, Şahin A. Role of Hematological Parameters in COVID-19 Patients in the Emergency Room. Biomarkers Med (2020) 14(13):1207–15. doi: 10.2217/bmm-2020-0317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Kazancioglu S, Yilmaz FM, Bastug A, Sakallı A, Ozbay BO, Buyuktarakci C, et al. Lymphocyte Subset Alteration and Monocyte CD4 Expression Reduction in Patients With Severe COVID-19. Viral Immunol (2020) 34(5):342–51. doi: 10.1089/vim.2020.0166 [DOI] [PubMed] [Google Scholar]
- 70. Doganci S, Ince M, Ors N, Yildirim A, Sir E, Karabacak K, et al. A New COVID-19 Prediction Scoring Model for in-Hospital Mortality: Experiences From Turkey, Single Center Retrospective Cohort Analysis. Eur Rev Med Pharmacol Sci (2020) 24(19):10247–57. doi: 10.26355/eurrev_202010_23249 [DOI] [PubMed] [Google Scholar]
- 71. Xue G, Gan X, Wu Z, Xie D, Xiong Y, Hua L, et al. Novel Serological Biomarkers for Inflammation in Predicting Disease Severity in Patients With COVID-19. International Immunopharmacology. Int Immunopharmacol (2020) 89(Pt A):107065. doi: 10.1016/j.intimp.2020.107065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Liu G, Zhang S, Hu H, Liu T, Huang J. The Role of Neutrophil-Lymphocyte Ratio and Lymphocyte–Monocyte Ratio in the Prognosis of Type 2 Diabetics With COVID-19. Scottish Med J (2020) 65(4):154–60. doi: 10.1177/0036933020953516 [DOI] [PubMed] [Google Scholar]
- 73. Noor A, Akhtar F, Tashfeen S, Anwar N, Saleem B, Khan SA, et al. Neutrophil-To-Lymphocyte Ratio, Derived Neutrophil-to-Lymphocyte Ratio, Platelet-to-Lymphocyte Ratio and Lymphocyte-to-Monocyte Ratio as Risk Factors in Critically Ill Covid-19 Patients, a Single Centered Study. J Ayub Med Coll Abbottabad (2020) 32(4-sup):S595–601. [PubMed] [Google Scholar]
- 74. Huang S, Huang M, Li X, Zhang T, Lu H. Significance of Neutrophil-to-Lymphocyte Ratio, Platelet-to-Lymphocyte Ratio for Predicting Clinical Outcomes in COVID-19. Medrxiv (2020). doi: 10.1101/2020.05.04.20090431 [DOI]
- 75. Bastug A, Bodur H, Erdogan S, Gokcinar D, Kazancioglu S, Kosovali BD, et al. Clinical and Laboratory Features of COVID-19: Predictors of Severe Prognosis. Int Immunopharmacol (2020) 88:106950. doi: 10.1016/j.intimp.2020.106950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Nair PR, Maitra S, Ray BR, Anand RK, Baidya DK, Subramaniam R. Neutrophil-To-Lymphocyte Ratio and Platelet-To-Lymphocyte Ratio as Predictors of the Early Requirement of Mechanical Ventilation in COVID-19 Patients. Indian J Crit Care Med (2020) 24(11):1143–4. doi: 10.5005/jp-journals-10071-23663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Panagiotis P, Angelo Z, Valentina S, Giulia M, Giacomo De R, Rosa MP, et al. Laboratory Test Alterations in Patients With COVID-19 and non COVID-19 Interstitial Pneumonia: A Preliminary Report. J Infect Developing Countries (2020) 14(07):685–90. doi: 10.3855/jidc.12879 [DOI] [PubMed] [Google Scholar]
- 78. Wang X, Li X, Shang Y, Wang J, Zhang X, Su D, et al. Ratios of Neutrophil-to-Lymphocyte and Platelet-to-Lymphocyte Predict All-Cause Mortality in Inpatients With Coronavirus Disease 2019 (COVID-19): A Retrospective Cohort Study in a Single Medical Centre. Epidemiol Infect (2020) 148:e211. doi: 10.1017/S0950268820002071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Wang X, Xu Y, Huang H, Jiang D, Zhou C, Liao H, et al. Increased Pretreatment C-Reactive Protein-to-Albumin Ratio Predicts Severe Coronavirus Disease 2019. Researchsquare (2020). doi: 10.21203/rs.3.rs-31723/v2 [DOI]
- 80. Lagunas-Rangel FA. Neutrophil-To-Lymphocyte Ratio and Lymphocyte-to-C-Reactive Protein Ratio in Patients With Severe Coronavirus Disease 2019 (COVID-19): A Meta-Analysis. J Med Virol (2020) 92(10):1733–4. doi: 10.1002/jmv.25819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Fois AG, Paliogiannis P, Scano V, Cau S, Babudieri S, Perra R, et al. The Systemic Inflammation Index on Admission Predicts In-Hospital Mortality in COVID-19 Patients. Molecules (2020) 25(23):5725. doi: 10.3390/molecules25235725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Wang R, He M, Yin W, Liao X, Wang B, Jin X, et al. The Prognostic Nutritional Index Is Associated With Mortality of COVID-19 Patients in Wuhan, China. J Clin Lab Anal (2020) 34(10):e23566. doi: 10.1002/jcla.23566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Simadibrata DM, Pandhita BAW, Ananta ME, Tango T. Platelet-To-Lymphocyte Ratio, a Novel Biomarker to Predict the Severity of COVID-19 Patients: A Systematic Review and Meta-Analysis. J Intensive Care Soc (2020), 1751143720969587. doi: 10.1177/1751143720969587 [DOI] [PMC free article] [PubMed]
- 84. Qu R, Ling Y, Zhang Y-H-Z, Wei L-Y, Chen X, Li X-M, et al. Platelet-To-Lymphocyte Ratio Is Associated With Prognosis in Patients With Coronavirus Disease-19. J Med Virol (2020) 92(9):1533–41. doi: 10.1002/jmv.25767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Zheng Y, Huang Z, Ying G, Zhang X, Ye W, Hu Z, et al. Comparative Study of the Lymphocyte Change Between COVID-19 and non-COVID-19 Pneumonia Cases Suggesting Uncontrolled Inflammation Might Not be the Main Reason of Tissue Injury. Medrxiv (2020). doi: 10.1101/2020.02.19.20024885 [DOI]
- 86. Rizo-Téllez SA, Méndez-García LA, Flores-Rebollo C, Alba-Flores F, Alcántara-Suárez R, Manjarrez-Reyna AN, et al. The Neutrophil-To-Monocyte Ratio and Lymphocyte-To-Neutrophil Ratio at Admission Predict In-Hospital Mortality in Mexican Patients With Severe SARS-CoV-2 Infection (Covid-19). Microorganisms (2020) 8(10). doi: 10.3390/microorganisms8101560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Sun D-W, An L, Lv G-Y. Albumin-Fibrinogen Ratio and Fibrinogen-Prealbumin Ratio as Promising Prognostic Markers for Cancers: An Updated Meta-Analysis. World J Surg Oncol (2020) 18(1):9. doi: 10.1186/s12957-020-1786-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Yue W, Liu Y, Ding W, Jiang W, Huang J, Zhang J, et al. The Predictive Value of the Prealbumin-to-Fibrinogen Ratio in Patients With Acute Pancreatitis. Int J Clin Pract (2015) 69(10):1121–8. doi: 10.1111/ijcp.12682 [DOI] [PubMed] [Google Scholar]
- 89. Shufei Z, Lei S, Jinying Z, Min Y, Jun L, Heyuan D. Prealbumin to Fibrinogen Ratio is Closely Associated With Diabetic Peripheral Neuropathy. Endocr Connections (2020) 9(8):858–63. doi: 10.1530/EC-20-0316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Bi X, Su Z, Yan H, Du J, Wang J, Chen L, et al. Prediction of Severe Illness Due to COVID-19 Based on an Analysis of Initial Fibrinogen to Albumin Ratio and Platelet Count. Platelets (2020) 31(5):674–9. doi: 10.1080/09537104.2020.1760230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Karakoyun I, Colak A, Turken M, Altin Z, Arslan FD, Iyilikci V, et al. Diagnostic Utility of C-Reactive Protein to Albumin Ratio as an Early Warning Sign in Hospitalized Severe COVID-19 Patients. Int Immunopharmacol (2021) 91:107285. doi: 10.1016/j.intimp.2020.107285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Oh J, Kim SH, Park KN, Oh SH, Kim YM, Kim HJ, et al. High-Sensitivity C-Reactive Protein/Albumin Ratio as a Predictor of in-Hospital Mortality in Older Adults Admitted to the Emergency Department. Clin Exp Emerg Med (2017) 4(1):19–24. doi: 10.15441/ceem.16.158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Guo X-L, Zhang Y, Zeng Y-H, Zhao F-Y, Liu W-P, Xiao L, et al. Serum Prealbumin Deserves More Significance in the Early Triage of COVID-19 Patients. Clin Chem Lab Med (CCLM) (2020) 58(10):e209–e11. doi: 10.1515/cclm-2020-0663 [DOI] [PubMed] [Google Scholar]
- 94. Zheng C, Liu S, Feng J, Zhao X. Prognostic Value of Inflammation Biomarkers for Survival of Patients With Neuroblastoma. Cancer Manag Res (2020) 12:2415–25. doi: 10.2147/CMAR.S245622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Fang E, Wang X, Feng J, Zhao X. The Prognostic Role of Glasgow Prognostic Score and C-Reactive Protein to Albumin Ratio for Sarcoma: A System Review and Meta-Analysis. Dis Markers (2020) 2020:8736509. doi: 10.1155/2020/8736509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Onodera T, Goseki N, Kosaki G. Prognostic Nutritional Index in Gastrointestinal Surgery of Malnourished Cancer Patients. Nihon Geka Gakkai Zasshi (1984) 85(9):1001. [PubMed] [Google Scholar]
- 97. Jiang N, Deng J-Y, Ding X-W, Ke B, Liu N, Zhang R-P, et al. Prognostic Nutritional Index Predicts Postoperative Complications and Long-Term Outcomes of Gastric Cancer. World J Gastroenterol (2014) 20(30):10537. doi: 10.3748/wjg.v20.i30.10537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Sun K, Chen S, Xu J, Li G, He Y. The Prognostic Significance of the Prognostic Nutritional Index in Cancer: A Systematic Review and Meta-Analysis. J Cancer Res Clin Oncol (2014) 140(9):1537–49. doi: 10.1007/s00432-014-1714-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Hu B, Yang XR, Xu Y, Sun YF, Sun C, Guo W, et al. Systemic Immune-Inflammation Index Predicts Prognosis of Patients After Curative Resection for Hepatocellular Carcinoma. Clin Cancer Res an Off J Am Assoc Cancer Res (2014) 20(23):6212–22. doi: 10.1158/1078-0432.CCR-14-0442 [DOI] [PubMed] [Google Scholar]
- 100. Chiang K-C, Huang S-T, Wu R-C, Huang S-C, Yeh T-S, Chen M-H, et al. Interferon α-Inducible Protein 27 is an Oncogene and Highly Expressed in Cholangiocarcinoma Patients With Poor Survival. Cancer Manag Res (2019) 11:1893–905. doi: 10.2147/CMAR.S196485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Suomela S, Cao L, Bowcock A, Saarialho-Kere U. Interferon Alpha-Inducible Protein 27 (IFI27) Is Upregulated in Psoriatic Skin and Certain Epithelial Cancers. J Invest Dermatol (2004) 122(3):717–21. doi: 10.1111/j.0022-202X.2004.22322.x [DOI] [PubMed] [Google Scholar]
- 102. Wang H, Qiu X, Lin S, Chen X, Wang T, Liao T. Knockdown of IFI27 Inhibits Cell Proliferation and Invasion in Oral Squamous Cell Carcinoma. World J Surg Oncol (2018) 16(1):64. doi: 10.1186/s12957-018-1371-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Hadjadj J, Yatim N, Barnabei L, Corneau A, Boussier J, Smith N, et al. Impaired Type I Interferon Activity and Inflammatory Responses in Severe COVID-19 Patients. Science (2020) 369(6504):718. doi: 10.1126/science.abc6027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Wilk AJ, Rustagi A, Zhao NQ, Roque J, Martínez-Colón GJ, McKechnie JL, et al. A Single-Cell Atlas of the Peripheral Immune Response in Patients With Severe COVID-19. Nat Med (2020) 26(7):1070–6. doi: 10.1038/s41591-020-0944-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Zhang N, Zhao YD, Wang XM. CXCL10 an Important Chemokine Associated With Cytokine Storm in COVID-19 Infected Patients. Eur Rev Med Pharmacol Sci (2020) 24(13):7497–505. doi: 10.26355/eurrev_202007_21922 [DOI] [PubMed] [Google Scholar]
- 106. Al Heialy S, Hachim MY, Senok A, Gaudet M, Abou Tayoun A, Hamoudi R, et al. Regulation of Angiotensin- Converting Enzyme 2 in Obesity: Implications for COVID-19. Front Physiol (2020) 11:555039–. doi: 10.3389/fphys.2020.555039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Patterson BK, Seethamraju H, Dhody K, Corley MJ, Kazempour K, Lalezari JP, et al. Disruption of the CCL5/RANTES-CCR5 Pathway Restores Immune Homeostasis and Reduces Plasma Viral Load in Critical COVID-19. medRxiv (2020). doi: 10.1101/2020.05.02.20084673 2020.05.02.20084673 [DOI]
- 108. Zheng H-Y, Xu M, Yang C-X, Tian R-R, Zhang M, Li J-J, et al. Longitudinal Transcriptome Analyses Show Robust T Cell Immunity During Recovery From COVID-19. Signal Transduction Targeted Ther (2020) 5(1):294. doi: 10.1038/s41392-020-00457-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Trouillet-Assant S, Viel S, Gaymard A, Pons S, Richard J-C, Perret M, et al. Type I IFN Immunoprofiling in COVID-19 Patients. J Allergy Clin Immunol (2020) 146(1):206–8.e2. doi: 10.1016/j.jaci.2020.04.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Huang L, Shi Y, Gong B, Jiang L, Liu X, Yang J, et al. Blood Single Cell Immune Profiling Reveals the Interferon-MAPK Pathway Mediated Adaptive Immune Response for COVID-19. Medrxiv (2020). doi: 10.1101/2020.03.15.20033472 [DOI]
- 111. Loganathan T, Ramachandran S, Shankaran P, Nagarajan DJP. Host Transcriptome-Guided Drug Repurposing for COVID-19 Treatment: A Meta-Analysis Based Approach. PeerJ (2020) 8:e9357. doi: 10.7717/peerj.9357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Shaath H, Vishnubalaji R, Elkord E, Alajez NM. Single-Cell Transcriptome Analysis Highlights a Role for Neutrophils and Inflammatory Macrophages in the Pathogenesis of Severe COVID-19. Cells (2020) 9(11). doi: 10.3390/cells9112374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Mick E, Kamm J, Pisco AO, Ratnasiri K, Babik JM, Castañeda CS, et al. Upper Airway Gene Expression Differentiates COVID-19 From Other Acute Respiratory Illnesses and Reveals Suppression of Innate Immune Responses by SARS-CoV-2. Nat Commun (2020) 11(1):5854. doi: 10.1038/s41467-020-19587-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Alsamman AM, Zayed H. The Transcriptomic Profiling of COVID-19 Compared to SARS, MERS, Ebola, and H1N1. PLoS One (2020) 15(12):e0243270. doi: 10.1371/journal.pone.0243270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Hammadi AA, Al Jubouri AM, Ahmed G, Hayyawi AH, Kareem K, Gorial FI, et al. A New Hematological Prognostic Index For Covid-19 Severity. Medrxiv (2021). doi: 10.1101/2021.02.11.21251285 [DOI]
- 116. Lidoriki I, Frountzas M, Schizas D. Could Nutritional and Functional Status Serve as Prognostic Factors for COVID-19 in the Elderly? Med Hypotheses (2020) 144:109946. doi: 10.1016/j.mehy.2020.109946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. SeyedAlinaghi S, Mirzapour P, Dadras O, Pashaei Z, Karimi A, MohsseniPour M, et al. Characterization of SARS-CoV-2 Different Variants and Related Morbidity and Mortality: A Systematic Review. Eur J Med Res (2021) 26(1):51. doi: 10.1186/s40001-021-00524-8 [DOI] [PMC free article] [PubMed] [Google Scholar]