Abstract
The management of forearm nonunion is challenging for orthopaedic surgeons because the forearm is a unique anatomical segment in which all the bones and structures involved embody a complex functional unit. Therefore, when treating such a complex condition, the surgeon must focus not only on bone healing but also on the restoration of the native anatomy in order to replicate the normal relationship between the bones and all the surrounding structures and thus the full function of the forearm, the elbow and the wrist.
Here we report the case of a 53-year-old patient with a left forearm deformity due to an atrophic nonunion of the ulna and a malunion of the radius, which was successfully managed with the use of the Masquelet technique associated with a corrective osteotomy of the radius, performed with the aid of a 3D model.
Keywords: Masquelet technique, Non-union(s), Bone defect(s), 3D printing, 3D model, Forearm
Introduction
Despite the improvement of fixation devices having minimised the incidence of nonunion of the forearm, this continues to represent a highly disabling condition for patients as well as a surgical challenge for orthopaedic surgeons [1].
Indeed, the radius and ulna constitute a functional unit whose integrity guarantees the correct function of the forearm, the elbow and the wrist. Thus, any healing problem affecting any of these bones affects not only the bone itself but it can also impair the function of any of the adjacent joints [2].
The aim of this paper is to present a complex case of ulnar diaphyseal bone defect as the outcome of an aseptic nonunion associated with a radial diaphyseal malunion, treated with the Masquelet technique and a corrective osteotomy performed with the aid of 3D technology.
Case report
A healthy 53-year-old man with a medical history of a left both bone forearm fracture following a road traffic accident in 2006, with a bifocal ulna fracture treated with a proximal and a distal LCP 3.5 plate (DePuy Synthes) and a diaphyseal radius fracture treated with a single LCP 3.5 plate (DePuy Synthes), came to our department with a left forearm deformity.
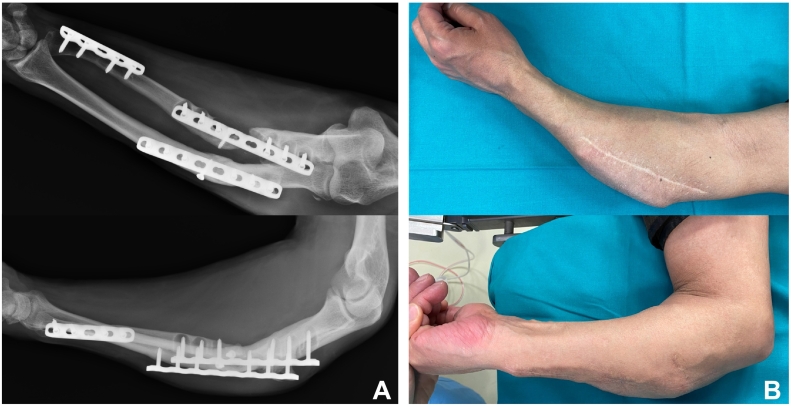
He had a clinically evident angular and rotational deformity of the forearm, limiting the full extension of the elbow and the pronation-supination of the forearm. X-rays highlighted an atrophic nonunion of the proximal diaphyseal ulna fracture and a malunion of the radius, with osteolysis around the screws of the proximal ulnar plate (Fig. 1). A three-step surgical revision was planned.
Fig. 1.
(A) Radiological and (B) clinical anterior-posterior and lateral views of the deformity showing an atrophic nonunion of the proximal ulnar shaft and a malunion of the proximal shaft of the radius.
The first step involved the removal of the implants using a single midline dorsal approach. Intra-operative samples were collected from both bones for microbiology, and later found to be negative. Concurrently, the patient was screened for low-grade infection, but blood parameters were in range. The forearm was immobilised in an above-elbow cast and X-rays and CT scan were obtained. The extent of the ulna bone defect was not able to be precisely evaluated due to the deformity of the radius, thus a 3D model (Medics) was obtained to plan the subsequent surgical step. A two-stage procedure according to the Masquelet technique was planned for the ulna, together with a corrective osteotomy of the radius with the aid of a custom-made 3D cutting guide.
Six weeks after the first operation, the patient underwent the second surgical step. Using a radial dorsal approach, the radius osteotomy was performed with aid of the guide, followed by the opening of the medullary canal and the osteosynthesis with a 6-hole LCP 3.5 mm compression plate (DePuy Synthes). Then, using an ulnar volar approach, the first stage of the Masquelet technique was performed. A debridement of the ulnar nonunion site with the removal of interposed fibrous tissue and devitalised bone was performed, together with the opening of the medullar canal on both ends. A bone defect of about six centimetres was measured and stabilised with a 12-hole LCP 3.5 mm plate (DePuy Synthes). The void was then filled with gentamicin loaded cement (PALACOS®R+G) to allow the development of the induced membrane.
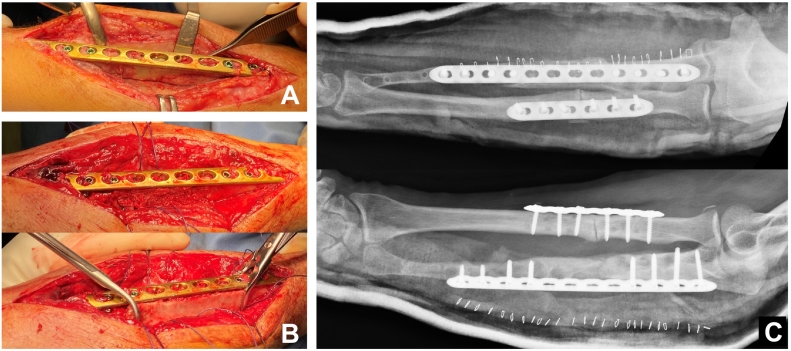
Twelve weeks later, the third surgical step was performed and the second Masquelet stage undertaken. Through the previously utilised volar incision, the ulna was approached, the induced membrane longitudinally opened and the cement spacer removed. The bone defect was filled with autologous cortico-cancellous bone graft harvested from the iliac crest and the 12-hole LCP plate was kept in place to stabilise the construct. Finally, the induced membrane was sutured over the construct (Fig. 2). The forearm was subsequently immobilised in an above-elbow back-slab for 4 weeks and then allowed to start progressive assisted mobilisation with load bearing restricted for 12 weeks.
Fig. 2.
(A) Intraoperative evidence of the formation of the induced membrane with cement spacer still in place; (B) cortico-cancellous bone grafting of the defect; (C) anterior-posterior and lateral post-operative X-ray control.
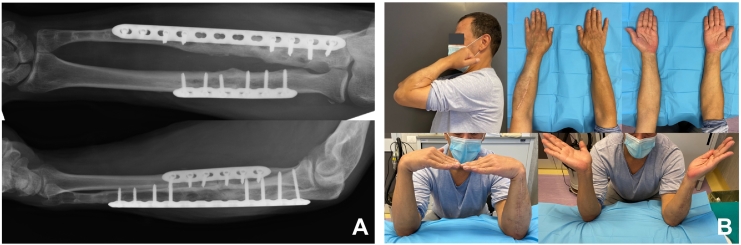
Six months after the third surgical step, the patient showed clinical and radiological healing of both bones with a complete ROM in pronation-supination of the forearm and flexion-extension of wrist and elbow (Fig. 3). The Quickdash score was 2.3% and the SF36 Physical functioning score was 90/100.
Fig. 3.
Follow-up at 6 months: (A) radiological healing of both bones with restoration of correct anatomic relationship between radius and ulna and adjacent joints; (B) full clinical recovery with complete ROM in pronation-supination of the forearm and flexion-extension of wrist and elbow.
Discussion
Management of forearm nonunions can be extremely challenging, as multiple issues must be considered and comprehensively addressed in order to effectively restore the anatomy of all the structures involved, which is the key for the functional recovery of this unique anatomical segment [2].
In this perspective, various treatment strategies have been proposed, such as bone transport, vascularised fibula flap, structural bone graft and the Masquelet induced membrane technique. The choice of treatment is determined by nonunion etiology, defect size and surgeon expertise [2], [3], [4].
In the case presented, the atrophic nature of the nonunion dictated the need for bone grafting. Thus, according to the large defect size of around six centimetres, a decision was made to perform the Masquelet technique. In literature, it is indeed reported that this technique is successfully applicable in large bone defects with healing rates of 83–100%, with the advantages of having a healing time independent of the defect size and without the need for microsurgical skills [5], [6]. These data are consistent with our case, in which the patient uneventfully progressed to bone healing in six months with a remarkably full functional recovery. Furthermore, in this specific case, the choice of the Masquelet technique allowed us to perform the treatment in stages, addressing each of the issues independently. In fact, during the second surgical step we were able to perform the correction of the radius malunion independently from the definitive treatment of the ulna, but concurrently creating the biological conditions for its subsequent healing with the induced membrane. In addition to this, the presence of the cement spacer gave extra mechanical stability to the construct, which may have aided the healing of the radius in the early post-operative period.
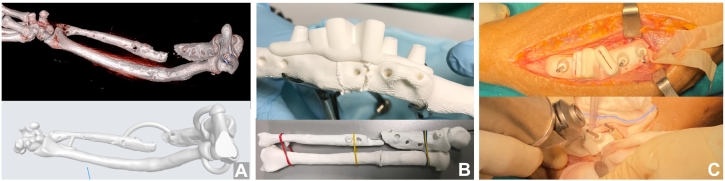
The complexity of the case, depicted by the association of the radial multiplanar deformity with the ulnar atrophic nonunion, made surgical planning exceptionally challenging. We decided therefore to avail of 3D printing technology, a powerful tool whose use is being increasingly applied in the deformity correction field with advantages both in the pre-operative and in the intra-operative phases [7]. Indeed, the use of a 3D model allowed us to better understand the deformity and to simulate the radius osteotomy with the aid of a 3D cutting guide in order to determine the precise wedge size. This permitted us to predict how the effects of the osteotomy would reflect on the ulnar bone defect and therefore on forearm functionality. Finally, the 3D cutting guide was used intra-operatively to maximise the precision of the osteotomy (Fig. 4). Unfortunately, in order to be able to apply the 3D technology, it was necessary to remove the implants, which implied the additional first surgical step. Nevertheless, the benefits gained by the use of a 3D model in such a complex deformity greatly outweighed the drawbacks caused by the additional surgical step.
Fig. 4.
Pre-operative planning and intra-operative use of the 3D printing technology: (A) CT 3D reconstruction and 3D preprint rendering of the forearm deformity; (B) simulation of the osteotomy with the 3D cutting guide on the 3D model and evaluation of its effects; (C) intra-operative utilisation of the 3D cutting guide.
In conclusion, the Masquelet technique represents an effective and reliable method for the treatment of large forearm defects. It could be considered above all in cases such as the one presented here, in which it allows us to comprehensively address multiple issues. In these circumstances, the use of 3D technology can be significantly useful both during the pre-operative and intra-operative phase.
Declaration of competing interest
All authors declare no conflict of interest.
No funding was received for the completion of this project.
References
- 1.Kloen P., Buijze G.A., Ring D. Management of forearm nonunions: current concepts. Strateg. Trauma Limb Reconstr. 2012;7:1–11. doi: 10.1007/s11751-011-0125-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dhar S.A., Dar T.A., Mir N.A. Management of Infected Nonunion of the forearm by the masquelet technique. Strateg. Trauma limb Reconstr. 2019;14:1–5. doi: 10.5005/jp-journals-10080-1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Micev A.J., Kalainov D.M., Soneru A.P. Masquelet technique for treatment of segmental bone loss in the upper extremity. J. Hand Surg. Am. 2015;40:593–598. doi: 10.1016/j.jhsa.2014.12.007. [DOI] [PubMed] [Google Scholar]
- 4.Giannoudis P.V., Harwood P.J., Tosounidis T., Kanakaris N.K. Restoration of long bone defects treated with the induced membrane technique: protocol and outcomes. Injury. 2016;47:S53–S61. doi: 10.1016/S0020-1383(16)30840-3. [DOI] [PubMed] [Google Scholar]
- 5.Mathieu L., Durand M., Collombet J.M., de Rousiers A., de l’Escalopier N., Masquelet A.C. Induced membrane technique: a critical literature analysis and proposal for a failure classification scheme. Eur J Trauma Emerg Surg. Oct 2020;47(5):1373–1380. doi: 10.1007/s00068-020-01540-9. [DOI] [PubMed] [Google Scholar]
- 6.Bourgeois M., Loisel F., Bertrand D., Nallet J., Gindraux F., Adam A. Management of forearm bone loss with induced membrane technique. Hand Surg. Rehabil. 2020;39:171–177. doi: 10.1016/j.hansur.2020.02.002. [DOI] [PubMed] [Google Scholar]
- 7.Raza M., Murphy D., Gelfer Y. The effect of three-dimensional (3D) printing on quantitative and qualitative outcomes in paediatric orthopaedic osteotomies: a systematic review. EFORT Open Rev. 2021;6:130–138. doi: 10.1302/2058-5241.6.200092. [DOI] [PMC free article] [PubMed] [Google Scholar]