Abstract
BACKGROUND:
Many students do not receive return to learn (RTL) services upon return to academics following a concussion.
METHODS:
Using a mixed-methods approach, we conducted a survey of RTL practices and experiences in Washington State schools between January 2015 and June 2015. We then held a statewide summit of RTL stakeholders and used a modified Delphi process to develop a consensus-based RTL implementation model and process.
RESULTS:
Survey participants included 83 educators, 57 school nurses, 14 administrators, and 30 parents, representing 144 schools in rural and urban areas. Unmet need domains and recommendations identified were (1) a current lack of school policies; (2) barriers to providing or receiving accommodations; (3) wide variability in communication patterns; and (4) recommendations shared by all stakeholder groups (including desire for readily available best practices, development of a formal school RTL policy for easy adoption and more training). Using stakeholder input from RTL summit participants and survey responses, we developed an RTL implementation model and checklist for RTL guideline adoption.
CONCLUSIONS:
Washington State children have unmet needs upon returning to public schools after concussion. The student-centered RTL model and checklist for implementing RTL guidelines can help schools provide timely RTL services following concussion.
Keywords: concussion, academic accommodations, traumatic brain injury (TBI), return to learn (RTL) services
There are between 1.1 and 1.9 million sports- and recreation-related concussions that occur annually among children aged 0–18 years in the United States,1 with many young athletes returning to play prior to getting cleared by a medical professional.2–6 The cost of traumatic brain injury (TBI) and concussion care is high, with care management estimated to be $76.5 billion in 2000 in the United States alone. However, this estimate does not capture the emotional, physical, or school impacts that often accompany concussion and TBI.7 Studies show thatmany students with more severe concussions and special education needs resulting from TBI do not receive adequate services in school.8,9 Whereas it is recognized that providing appropriate academic accommodations and school services to children with concussion is critical for supporting their recovery and development, and for increasing their capacity for higher education and work productivity,10–14 barriers to accessing school services such as lack of medical documentation and poor communication between medical professionals and schools are reported to hinder implementation of return to learn (RTL) services.15
Accommodations for students with recognized educational and medical needs, including concussion, may include either formally defined and temporary individualizedhealthcareplans,504plans,andindividualized education plans, or informal academic accommodations provided by individual educators.16–18 Current guidelines for accommodating students returning to school after concussion do not consider how school policies or teacher education on RTL practices might affect RTL guideline implementation or fidelity. The current guidelines also have not been evaluated.16–19 In addition, the development of these guidelines does not consistently include feedback or input from all key stakeholder groups about how policies and procedures might be implemented in schools or about how school policies might affect overall guideline implementation.15,17,19,20,21 Washington State was the first US state to pass a return to play law, known as the Zachary-Lystedt law, but has no RTL law or public school RTL policy. There is also little known about statewide RTL school policies or RTL needs in any of the states. To bridge this gap in knowledge, we examined RTL practices and experiences in Washington State public schools. We aimed to use this information to develop strategies that redress these needs and facilitate best practice guideline adoption for schools serving students with concussion.
METHODS
General Study Design
We used a mixed-methods approach to determine RTL needs. We conducted a statewide needs assessment using a survey of public school nurses, administrators, and teachers, as well as a survey of parents of children with concussion. The recruitment period for all survey data was February to May 2015. State needs assessment results were shared with the Washington State TBI council. We held a 1-day RTL summit in Seattle on January 22, 2016. Needs assessment results were used to guide development of summit contents and a RTL implementation model and checklist. The RTL model and RTL checklist were refined further using consensus from a modified Delphi process facilitated during the summit as well as from post-summit attendee feedback.22 The final model and checklist were agreed upon by stakeholders and attendees.
Statewide Needs Assessment
Schools.
Schools were selected for participation using a random sample of all public schools in Washington State; the Office of the Superintendent of Public Instruction for Washington State provided the list of schools. We excluded college programs and schools serving a special population such as inpatient facilities and schools for the deaf and hard of hearing. Because many cognitive symptoms do not become recognizable until a child with TBI reaches middle school and accommodations are more likely to be deemed necessary in grades 6–12 than in grades 5 and below, we surveyed schools that included students in grade 6 or higher; however, schools were not excluded if they also included students in grades K-5.20
The 1333 eligible public schools were divided into the following 8 groups based on their school-type designation: vocational schools, reengagement schools, tribal schools, alternative schools, K-12, elementary schools, middle schools, and high schools. They were labeled as either rural or urban within each school-type using the Washington State Department of Health designations of each school’s county. We randomly sampled schools in blocks of 10 from each school-type and rural/urban category, replacing those who declined to participate with the next school in that block, contacting a total of 254 schools by the end of the recruitment period. Using publicly available contact information, we contacted schools between February and May 2015, 208 of which were confirmed as eligible.
Administrators, teachers, and nurses.
Once a school agreed to participate, individual survey links were sent via e-mail to a school administrator, as well as to the school nurses and teachers. Due to a low survey response rate, we additionally disseminated the nurse and teacher surveys to registered school nurses and teachers statewide using the Washington State Office of the Superintendent of Public Instruction listserv. Teachers were asked demographic questions, but not asked to specify their school. School nurses and administrators were not asked demographic questions to protect respondent privacy.
Parents.
Parents of students in Washington State public schools who had experienced a concussion were recruited through the Brain Injury Alliance of Washington (BIAWA). Parents were sent an anonymous survey link through BIAWA’s Facebook page and listserv. Since the study focused on children who attended school (grades 6–12) following their concussion, we included only parents of children who were diagnosed with concussion prior to age 18years.
Study Materials and Survey Content
Surveys were developed based on questions included in prior studies of TBI in school aged children9,15,17,23–25 and based on input from interviews with 2 former teachers, a school nurse, and a district administrator in Washington State. Surveys asked questions aimed at assessing respondent knowledge, attitudes and beliefs as well as current practices and experience regarding students with concussion reentering school and any relevant policies in their corresponding public schools or districts.
Instrumentation
We used the National Institutes of Health funded online surveying platform designed for Health Insurance Portability and Accountability Act (HIPAA) compliant, institutional research called REDCap (Research Electronic Data Capture)26 to survey Washington State teachers, school nurses, school administrators, and parents of children with concussion. Databases were maintained at the Harborview Injury Prevention and Research Center and Seattle Children’s Research Institute.
Data Analysis
We used a mixed-methods approach to analyze survey data and assess the landscape of RTL guideline implementation practices and experiences in Washington State. Categorical and demographic survey questions were analyzed quantitatively while open-ended survey questions were analyzed using a qualitative content analysis. Two study coders independently reviewed the survey responses and identified thematic codes using an inductive approach.19 After coding was completed, investigators employed an iterative consensus-based process for theme development to facilitate interpretation of findings and model development.20 We identified 4 major domains and attributed themes within each domain to describe responses. Analysis was completed with Stata 13 and Dedoose software packages.27,28
RTL Summit
Participants.
The needs assessment results identified 6 major stakeholder groups with formal state and public school responsibilities for children with concussion and whose engagement would be critical for RTL guideline implementation in schools. Accordingly, invited stakeholder groups were parents, educators, state level policymakers, medical providers, social workers, and community organizations. We also contacted individuals who could represent multiple stakeholder groups (eg, a teacher who was also a parent of a child with concussion), with attention paid to representation from underserved populations (ie, Native American, Hispanics, and other disabilities). We invited a total of 59 individuals from the identified 6 major stakeholder groups. The summit was attended by 35 invitees with at least 1 person from each stakeholder group.
Summit agenda and process.
Before the summit, investigators reviewed and summarized existing RTL literature and results of the Washington State needs assessment. We sent participants the summary, as well as the Washington State Superintendents Association sample policy on student sports concussion and head injury, the Revised Code of Washington pertaining to student sports concussion, and an executive summary of the statewide RTL needs assessment. We asked participants to respond with questions and comments that were used to guide the summit agenda. Summit presenters reviewed and discussed the strengths and weaknesses of the RTL literature, discussed the completed Washington statewide needs assessment results, reviewed the neighboring Oregon RTL processes, and identified gaps in statute and formal policy pertaining to RTL.
Participants were then divided into 6 workgroups with at least 4 stakeholder groups represented in each workgroup where discussion was facilitated by a summit participant who was briefed on the process and goals prior to the discussion. By group, participants developed and ranked key components of RTL domains and implementation processes in order of relevance to implementation using a Delphi process.22 These domains were derived from the shared components of 2 of the most widely used RTL models, the REAP (Reduce Educate Accommodate Pace) Project29 and Brain 101,16 and included the prepared system, the coordinated care team, RTL protocols and program evaluation. Alongside each domain were pertinent questions raised by stakeholders and facilitators with respect to the RTL process during the pre-summit assessment.
Theme development.
At the end of the summit, facilitated workgroups developed group level consensus on ideal RTL guideline domains and preferred implementation components. Themes were identified by consensus among study investigators for use in the development of the RTL implementation model and checklist, as described below.
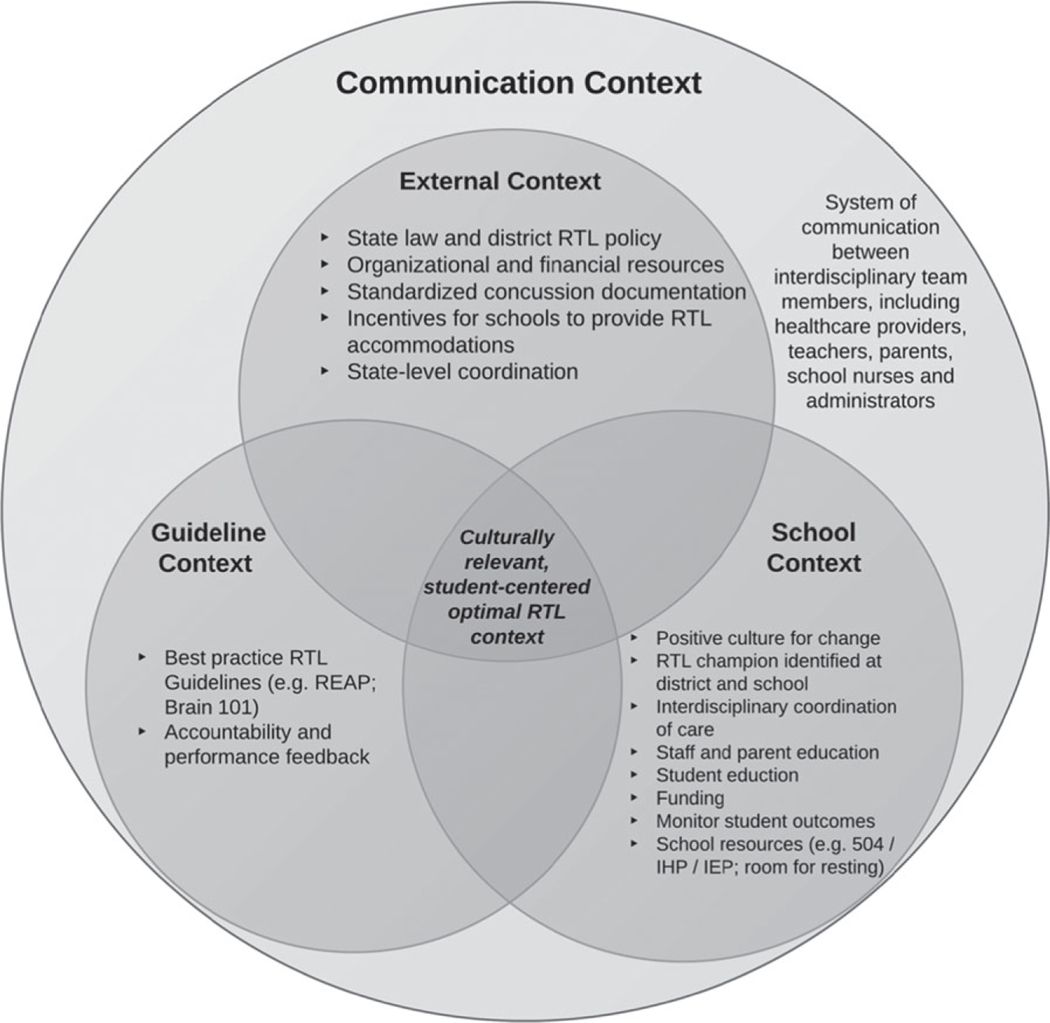
RTL Implementation Model Development
Using results from the needs assessment and summit findings, we adapted the Consolidated Model for Implementation Research (CFIR) developed by Damschroder et al30 to describe RTL specific external, guideline, school and communication contexts relevant to the development of an optimal RTL context. Following the Damschroder model, the external context refers to the state level policies, the school context refers to school capacity, the communication context refers to the systems of communication between interdisciplinary groups required to support RTL accommodations, and the guideline context refers to available RTL guidelines available for implementation.
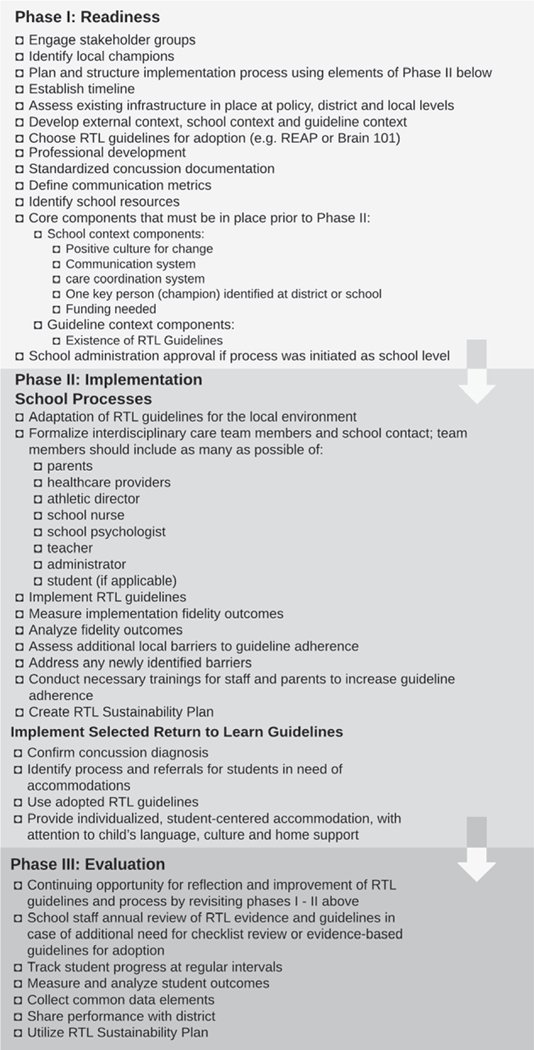
We then developed a 3-phase checklist that considers the optimal RTL context and could be used by schools to implement formal RTL policy. The checklist does not require full development of the external context because this aspect may lag behind school and guideline readiness. The model and checklist were further refined based on consensus from the core research group and summit participants at the summit and via e-mail after the summit. All stakeholders iteratively achieved final consensus regarding the final RTL implementation model and checklist.
RESULTS
Statewide RTL Needs Assessment
Participants.
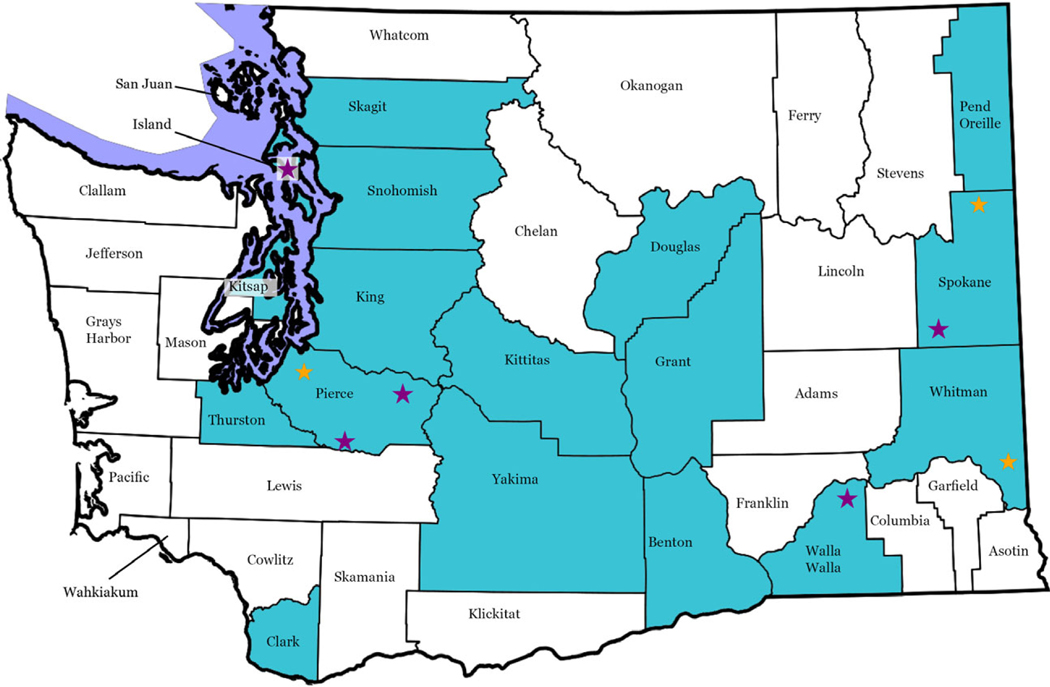
Survey participants included 83 educators, 57 school nurses, 14 administrators, and 30 parents from 17 (43.5%) counties, from 144 schools in rural and urban areas (Figure 1). Administrator and school nurses responded from 6 school-types: high schools, middle schools, elementary schools, vocational schools, reengagement schools, and tribal schools (Table 1).
Figure 1. Geographic Distribution of Study Participation and School- and District-Level Return to Learn (RTL) Policies.
Table 1.
Study Participant Demographics
| Respondents by School Type | Administrator (N=11) N (%) | Teacher (N=83) N (%) | School Nurse (N=57) N (%) |
|---|---|---|---|
|
| |||
| High School | 2 (14.3) | 11 (13.3) | 13 (22.8) |
| Middle School | 1 (7.1) | 7 (8.4) | 13 (22.8) |
| Elementary School | 2 (14.3) | 27 (32.5) | 9 (15.8) |
| Tribal School | 1 (7.1) | 4 (4.8) | 1 (1.8) |
| Reengagement Schools | 2 (14.3) | 12 (14.5) | 4 (7.0) |
| Vocational School | 3 (2.1) | 9 (10.8) | 0 (0) |
| OSPI | 0 (0.0) | 13 (15.7) | 0 (0.0) |
| District Level | 0 (0.0) | 0 (0.0) | 17 (29.8) |
|
| |||
| Demographics of children among participating parents (N = 21) | Children N (%) | ||
|
| |||
| White | 15 (71.4) | ||
| Private Insurance at time of injury | 18 (85.7) | ||
| TBI sustained | |||
| Prior to starting school | 1 (4.8) | ||
| K-5th grade | 7 (33.3) | ||
| 6th −8th grade | 1 (4.8) | ||
| 9th −12th grade | 12 (57.1) | ||
| Average Household Income | |||
| Below the FPL | 2 (9.5) | ||
| FPL-2xFPL | 2 (9.5) | ||
| 2xFPL or More | 17 (81.0) | ||
| Academic accommodations provided to support return to learn | |||
| No special services | 9 (42.9) | ||
| Informal Services | 6 (28.6) | ||
| 504 | 6 (28.6) | ||
| IEP | 0 (0.0) | ||
|
| |||
| Demographics of teachers (N = 83) | Teachers N (%) | ||
|
| |||
| Highest Level of Education Received | |||
| Bachelors | 28 (33.7) | ||
| Masters | 54 (65.1) | ||
| PhD | 1 (1.2) | ||
| Years Teaching | |||
| Less than 5 | 20 (24.1) | ||
| 5 to 10 | 11 (13.3) | ||
| 10 to 20 | 17 (20.5) | ||
| 20 or more | 35 (42.2) | ||
| Race | |||
| White | 76 (91.6) | ||
| American Indian | 1 (1.2) | ||
| Multiple Races | 6 (7.2) | ||
| Had formal TBI training | 25 (30.1) | ||
Domains
Responses from the open-ended needs assessment were categorized into 4 domains: (1) accommodation practices; (2) barriers to accommodation; (3) communication patterns; and (4) recommendations for improvement. Table 2 provides illustrative quotes representing themes within each domain.
Table 2.
Illustrative Quotes from the Needs Assessment Surveys
| Surveyed Group | Domain 1: Accommodations and School Policies | Domain 2: Barriers to accommodations | Domain 3: Communication patterns | Domain 4: Shared recommendations |
|---|---|---|---|---|
|
| ||||
| Parents | 1) “[The school should have] had a better process in place to know what to do and how to handle reentry.” 2) “The school at first was amazing, it’s now that we are 4 years into this I think they forget and her care is lessoned.” |
1) “They had no clue how to handle my son since he didn’t have a ‘visual’ impairment, like a cast or crutches. They thought he should be back to normal in 2 weeks.” 2) “The school refused to create an IEP [Individualized Healthcare Plan] at that time for my son because they said he needs to wait his turn on the IEP evaluation wait list.” 3) “Teachers thought [my child] was faking it.” |
“[The school should have] coordination and communication between school nurse, attendance office, counseling office and teachers.” | 1) “[Schools need] a flow chart with step by step guide.” 2) “ My son was weeks behind in school and had to drop 3 of his 6 classes while waiting for the accommodation plan to be put in place.” 3) “[Schools should] offer services immediately.” |
| Teachers | 1) “It would be nice to have a protocol for return to full classwork. I know in sports we have a gradual plan for returning kids back to practice then competition but there is no such plan for school.” 2) “State law needs to allow for flexible support for students with TBI’s.” |
“First, the teachers would have to know that we had TBI students in class. That kind of information gets socked away in the counselor’s office. Secondly, teachers would need to be informed on what we can do to better serve this group of children.” | 1) “[I would] request permission to speak with the doctor in order to be more attuned to expectations/possibilities and ideas for work-arounds where challenges.” 2)”More communication with family about how things are going at home, ie sleep and eating habits and mood swings as well as general overall well-being.” |
1) “Wouldn’t it be cool if the educational system had a consultant available?” 2) “Teachers don’t just need information, we need training. Someone needs to come in and coordinate the education of the teachers with what to expect, how to plan for & implement a classroom environment appropriate for a TBI student, as well as provide informational resources for future problems/concerns/situations that may arise.” |
| School Nurses | 1) “An easy-to-follow protocol for teachers. Coaches’ return-to-play protocol is understandable. Teachers don’t have guidance for cognitive ‘return to play’.” 2) “I would like to see a universal return to school policy/protocol that educators and health staff are trained on.” |
1) “The idea of resting and going slow is very difficult for staff to accept.” 2) “Concussions become opportunities for kids and sometimes, parents to brag. They don’t get the danger. Today a student told me, oh it is minor and implied that there was nothing to be concerned about although she had restrictions on activities. Her PCP didn’t write a note.” |
” Many times if the injury is not severe we as school nurses receive little information from the care provider. Many time we receive notes that say the student was seen in the ER, urgent care or clinic and that they may return to school on a specified date. The note may say that the student is not to participate in PE or sports for a specified period of time and that is it.” | “ A standard evaluation/tool/scoresheet to monitor and document progress when a student returns to school. This would be a tool that could be used to communicate with classroom teachers, and let them know at what level they can expect the student to perform on a given day.” |
| Administrators | 1) “We need access to doctors and current research on how to best meet the needs of students with TBI. 2) “[We need] uniform policy about how to service students with TBI, and training regarding the policy.” 3) “We don’t know what to do.” |
1) “Financial barriers (often extra support requires additional funding) [&] human resource barriers- not many people within the school are equipped or experienced in handling TBI.” 2) “The amount of content and growth they are expected to make each year. A serious concussion can set a good student back a full year.” |
1) “I would appreciate clearer direction from physicians regarding student limitations.” 2) “[Students] need a structured plan that is well communicated with an environment that supports their progressive recovery process.” |
1) “Have training for all teachers so that they all know the procedures and would have universal knowledge of the policy.” 2) “We require training and resources” |
Domain 1: school policies on accommodations.
Only 12% of schools reported a formal RTL policy. Most participating schools (67%) and districts (59%) had no formal RTL policy but described an informal process to support students transitioning back to school after concussion. Schools with formal policies were more likely to provide more formal accommodations specific to concussion (including extra time on tests even prior to student assessment and formal accommodations, extending homework deadlines, providing a note taker and requiring written clearance from a doctor prior to full RTL) if they had older students. Administrators at schools with no policy expressed “We don’t know what to do” (Table 2). Compared to schools with no RTL policies, schools with RTL policies were more likely to report providing an Individualized Health care Plan (0.0% and 26.7%, respectively),Individualized Education Program (0.0% and 20.0%, respectively) or 504 Plan (13.3% and 33.3%, respectively). Schools with a formal RTL policy were also more likely than schools without to report requiring written clearance from a physician before returning a student to their full academic load (6.7% and 40.0%, respectively), more likely to base accommodations on physician recommendation (33.3% and 66.7%, respectively), and more likely to hold a meeting between coordinated care team to discuss the student’s accommodations (0.0% and 46.7%, respectively).
Domain 2: barriers to accommodations.
Only 30% of teachers reported receiving concussion training and approximately half (N=42) reported having had a child with concussion in their classroom at some point in their career. Major thematic barriers to providing accommodation and recovery across stakeholder groups were: (1) invisibility of concussion as an injury; (2) time constraints; (3) lack of awareness, resources, and support for educators; and (4) lack of concussion knowledge. Invisibility of injury refers to the fact that in most cases, a child with concussion cannot be identified based on outward appearance; many parents indicated their child’s teacher “thought the child was faking it” because the injury could not be seen. Teachers and administrators both agreed that teachers did not have enough time to provide necessary 1-on-1 instruction with students recovering from a TBI. Teachers reported feeling unprepared to modify their curriculum to accommodate students with TBIs, due to a lack of knowledge of how TBI affects the individuals learning needs, school policy and lack of available curriculum adjustment tools.
Domain 3: communication patterns.
Across all groups represented in the needs assessment, there was a desire for more frequent meetings between individuals supporting the child’s return to school as well as more frequent communication with the child’s physician. Parents reported feeling responsible for the majority of the communication between the school and health care providers. Parents also reported not feeling listened to by school personnel when requesting or developing accommodation plans.
Domain 4: shared recommendations.
All surveyed groups agreed on the need for readily available best practices, development of an RTL policy for easy adoption and more training both for parents and for teachers (Table 3). Other recommendations included (1) need flexible accommodations immediately following concussion; (2) more staff time to support students with concussion; (3) expert resources to provide guidance for accommodations; and (4) providing environmental accommodations. The majority of participants agreed that implementing RTL policies and services was important and would provide additional support to all stakeholder groups involved in supporting a child with a concussion.
Table 3.
Shared Recommendations Between Surveyed Stakeholder Groups. RTL = Return to Learn
| Recommendations | Parents (N = 21) N (%) | Teachers (N = 83) N (%) | Nurses (N = 57) N (%) | Administrators (N = 11) N (%) |
|---|---|---|---|---|
|
| ||||
| More training | 7 (33.3) | 55 (66.3) | 16 (28.1) | 7 (50.0) |
| Have RTL school policy | 4 (19.0) | 8 (9.6) | 18 (31.6) | 5 (35.7) |
| More communication between transition team members | 10 (47.6) | 27 (32.5) | 15 (26.3) | 3 (21.4) |
| Have best practices available | 2 (9.5) | 26 (31.3) | 9 (15.8) | 2 (14.3) |
| Provide more staff time for one-on-one | - | 19 (22.9) | - | 1 (7.1) |
| Must have fast and flexible accommodations | 3 (14.3) | 6 (7.2) | - | - |
RTL Summit Participants
Of the 59 invited, 35 (58.3%) stakeholders attended, representing all targeted stakeholder groups and a total of 28 organizations. Participants included study investigators, pediatricians, rehabilitation medicine physicians, neuropsychologists, a representative of the School Nurses of Washington, the head of school nurses for Office of the Superintendent of Public Instruction, the Lead for the Disabilities Task Force on the Washington Student Achievement Council as well as many others (Appendix 1). All summit participants wanted to stay engaged in future efforts to address RTL needs for concussion, and to examine development of school policy for RTL after concussion.
RTL Implementation Model for Concussion
Following the development of the RTL model and implementation checklist, study investigators received input on the model and checklist from all RTL stakeholders who attended the summit plus an additional 10 newly recruited stakeholders from the Puget Sound Nurses Association. On the first round, 56 (80%) approved the model and checklist while 14 stakeholders recommended changes and or requested clarifications which were incorporated in the final products. The adapted and refined model highlights the optimal RTL context and the structural components needed to support RTL needs (Figure 2) while the checklist outlines specific steps for schools to expediently implement RTL guidelines (Figure 3) should a student with concussion be identified. The diagnosis of concussion would activate the chosen RTL guidelines.
Figure 2. Return to Learn Model for Concussion.
Figure 3. School Checklist for Implementation of Return to Learn Guidelines for Students Following Concussion.
Model Based Process for Implementing RTL Guidelines
Phase I: readiness.
Phase I starts with engaging major stakeholder groups and developing a plan and timeline for implementation and includes the current landscape and infrastructure that would support RTL guideline implementation using the above model as a guide. Identification of the RTL guidelines for adoption also occurs in this phase. The key RTL champion ensures that there is a positive culture for change in the schools, 1 key person is identified at the district or school, RTL costs are accounted for, and that a RTL guideline has been identified for implementation. Formalized concussion documentation, training plan, and communication metrics are developed. Schools identify local resources for students with concussion.
Phase II: RTL implementation process.
Adaptations of the RTL guidelines for the local environment should be considered. This process includes staff training, formalizing the multidisciplinary team, implementing RTL guidelines, and assessing guideline implementation fidelity. Barriers to implementation are identified and addressed. Students with concussion are identified. Individualized accommodations are initiated and periodically evaluated. Student achievement is periodically evaluated and need for discontinuation of RTL accommodations should be considered.
Phase III: continuous quality improvement.
New RTL evidence and new RTL guidelines should be examined annually by the school to determine need for revision of the checklist. Schools should measure student outcomes and share performance with their district.
DISCUSSION
The main findings of this study are that (1) few Washington State public schools have formal RTL policies for concussion; (2) there are numerous barriers to RTL implementation; and (3) there is uniform stakeholder support for the development and adoption of an RTL school policy and RTL state law. The student-centered RTL model and implementation checklist that resulted from this study support implementation of existing RTL guidelines, and provide a new school process for adopting these guidelines so that RTL accommodations for concussion can be activated and provided in a timely and structured manner.
In this report, we provide new information on the many barriers to RTL implementation in the Washington State public school system. Specifically, school personnel and parents both agreed that lack of multidisciplinary teams, lack of school capacity or a formal transition plan, lack of teacher training in concussion and lack of parent preparedness for advocating for their child with concussion were major barriers to RTL guideline implementation. While these findings align with previously described gaps by individual stakeholder groups, this study is the first to identify high priority barriers faced by all stakeholder groups attempting to implement RTL in Washington State public schools.4–6,10,15,27
We developed a conceptual model for RTL because conceptual models serve an important role in understanding complex issues influenced by multiple domains and in the development of recommendations.30,35 Thus, we were able to identify the optimal RTL context and developed a new model for RTL after concussion which contains the critical components of existing RTL guidelines and their relation to the factors affecting RTL guideline implementation. We considered multiple models for adaptation and selected the Damschroder model to adapt for RTL primarily because it allowed us to include and connect the contexts that are specifically relevant to the reintegration of the student into school after concussion.32 Stakeholders voiced lack of communication as a barrier to implementing RTL guidelines within each context; hence, this is shown as an overarching aspect of providing optimal RTL services.
The adapted RTL model allows schools to understand and evaluate their existing strengths prior to proceeding with implementation efforts. However, conceptual models, including the one we developed, do not uniformly translate to process improvement or successful implementation. This is evidenced by the fact that failure to implement evidence-based health services guidelines is a common and multifaceted problem. Within the educational system, RTL guideline adoption may be impacted by lack of formal school board policy, competing demands within the school system and/or a lack of awareness of best RTL practices.31–34 Consequently, we operationalized the model into a process and created a checklist that schools can use to demonstrate readiness, implement RTL guidelines, and evaluate RTL accommodations. The consensus-based RTL checklist has some distinct advantages. First, as recommended by the stakeholder group, the checklist leaves the choice of specific RTL guideline to the school. Second, the checklist accommodates the variability in school context by not specifying the cost coverage method, the key personnel position within the school structure, the individuals required on the coordinated care team, the method used to evaluate student progress or process of communication with health care providers and parents. The flexible checklist also allows schools to incorporate culturally relevant factors, and allows schools to develop local solutions to meet their specific RTL needs while providing all necessary elements of the RTL best practice checklist. Use of the model and checklist may allow schools to adopt structures and processes that facilitate successfully RTL guideline adoption even in the absence of district or state level policy.
There are currently 3 main RTL guidelines that have been developed and used: REAP, Brain 101, and Brain Steps.16,29,31 All of these are primarily consensus-based recommendations because data on the most effective RTL guidelines for concussion are scant. Despite this limitation, existing research suggests the importance of a designated and coordinated team to guide school transition and reintegration of students with concussion back to school and to ease the burden placed on school staff members, who may not have the time for coordinating these efforts.9,17,20 This recommendation is included in both the new RTL model and RTL checklist. The RTL model and checklist provide a systems-based approach for schools to facilitate implementation of the RTL guidelines.
We used a mixed-methods approach to examine RTL needs and to develop an RTL implementation process that schools can use to support children with concussion. Mixed-methods approaches are appealing because they maximize the strengths of qualitative and quantitative methods to address multifaceted, complex research questions that cannot be answered using only 1 method.33–35 In our study, the use of both qualitative and quantitative survey questions and the model development process involving multiple stakeholders allowed us to elicit both breadth and depth of perspectives and offer a holistic view of the barriers and facilitators of RTL services in Washington State as well as strategies for next steps. Had we only used a quantitative survey approach, we would have been able to quantify the magnitude of RTL needs, but would not have captured the rich detail about specific RTL concerns and recommendations that we obtained using open-ended survey questions and the consensus-driven, iterative model development process. Another strength of our methodology was that we could initiate stakeholder engagement to support RTL guideline adoption in Washington State; a key step in the implementation process (Figure 3: phase 1).
Limitations
This study has some limitations. First, this was a study in Washington State only and focused on the public school system. Hence, it is possible that there are some unique and specific RTL needs that we missed among students with concussion who attend private schools, and that the optimal RTL model may need to be adapted for private schools. We had a limited number of non-English speaking families which may have affected identification of themes, our understanding of their RTL barriers and, consequently, the development of the RTL model. We also did not examine specific school level RTL policies or student achievement, and are not able to determine the effect presence of school level policies on student outcomes. Despite these limitations, this study provides new information on unmet RTL needs and presents a new road map for schools to implement RTL services after concussion.
IMPLICATIONS FOR SCHOOL HEALTH
This study highlights the unmet needs of students with concussion upon returning to school and suggests potential strategies for improvement that have shared stakeholder support. We found that:
• Many parents felt unsupported by school personnel when navigating their child’s return to academics post-concussion.
Most schools do not have formalized RTL guidelines in place.
All surveyed stakeholder groups (parents, teachers, administrators, and school nurses) requested more training, school RTL guidelines, increased communication between team members and availability of best practices to support RTL transitions post-concussion.
Students and families are often unprepared to initiate RTL transitions and unaware of RTL best practices. This places the school in a unique position to offer the structure and support to families and students that will encourage successful RTL transition post-concussion. Schools can:
Adopt student-centered, culturally relevant RTL guidelines to proactively prepare for student concussion recovery.
Ensure students should not return to play prior to completed return to academics.
Utilize the model and implementation process developed to improve RTL transitions and outcomes for students with concussion.
Actively provide support for teachers when a student is transitioning back to academics post-concussion.
Engage parents actively when designing RTL accommodations for their child.
Human Subjects Approval Statement
Institutional Review Board exempt status #49218 was obtained from the University of Washington Human Subjects Division.
Acknowledgments
This study was funded by the Washington State Department of Health and Human Services Traumatic Brain Injury Council (Award to Dr. M.S.V.), Seattle Children’s Research Institute (SCRI) and the National Center for Advancing Translational Sciences of the National Institutes of Health (KL2TR000421 to Dr. M.M.). The funding sources had no involvement in the study design, data collection, analysis and interpretation of data; in the writing of the report; or in our decision to submit the paper for publication. Special thanks to Molly Fuentes, MD, Christina Schwien, MN, MPH, Sharon Ashman, PhD, Brian Ross, MA, and Mark Gudmastad for their support of this project. We would also like to thank Bud Bannan, MEd, Laura Bienen, David Breiger, PhD, Sara Chrisman, MD, MPH, David Coppel, PhD, Nora Coronado, MSW, MPH, Julie Dawning, MSP, CBIS, Matt Gillingham, Jessica Giordano, MA, Ann Glang, PhD, Kris Harper, BSN, Stanley Herring, MD, Will Hitchcock, Jeanne Hoffman, PhD, Emily Kroshus, ScD, MPH, Cari McCarty, PhD, Anne Messerly, Kristin White, MD, Laura Ploudre, MEd, Benjamin Rogers, Karen Starr, MEd, Elizabeth Stein, BA and Laura Widdice, MN for their engagement in the Return to Learn Summit.
Appendix 1.
Complete List of Summit Participant Organizations
Brain Injury Alliance of Washington
Center for Child Health
Center for Clinical and Translational Research
Center for Child Health, Behavior, and Development
Harborview Injury Prevention & Research Center
Issaquah School District
Kent-Meridian High School
Latino Center for Health
Lake Washington School Districts
Office of the Superintendent of Public Instruction
Renton School District
Safe Kids Washington
Shoreline School District
Steilacoom School District
Seattle Children’s Hospital Departments of Rehabilitation Psychology, Neuropsychology, Psychiatry, and Behavioral Health
School Nurses Association of Washington
Traumatic Brain Injury Model System
The Center on Brain Injury Research and Training
University of Oregon
University of Washington Sports Concussion Program
University of Washington School of Social Work and Departments of Pediatrics, Epidemiology, Anesthesiology, Psychiatry, and Behavioral Sciences, Adolescent Medicine, Rehabilitation Medicine, Developmental Pediatrics, Neurological Surgery, and Radiology
Vashon Partners in Education
Vashon Island School District
Virginia Mason Medical Center
Washington State Commission on Hispanic Affairs
Washington State Department of Health
Washington Student Achievement Council
Washington Traumatic Brain Injury Strategic Partnership Advisory Council
REFERENCES
- 1.Bryan MA, Rowhani-Rahbar A, Comstock RD, Rivara F. Sports and recreation-related concussions in US youth. Pediatrics. 2016;138(1):e20154635. DOI: 10.1542/peds.2015-4635. [DOI] [PubMed] [Google Scholar]
- 2.Kerr ZY, Register-Mihalik JK, Kroshus E, Baugh CM, Marshall SW. Motivations associated with nondisclosure of self-reported concussions in former collegiate athletes. Am J Sports Med. 2016;44:220–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kerr ZY, Register-Mihalik JK, Marshall SW, Evenson KR, Mihalik JP, Guskiewicz KM. Disclosure and non-disclosure of concussion and concussion symptoms in athletes: review and application of the socio-ecological framework. Brain Inj. 2014;28(8):1009–1021. [DOI] [PubMed] [Google Scholar]
- 4.Kay MC, Welch CE, McLeod TCV. Positive and negative factors that influence concussion reporting among secondary-school athletes. J Sport Rehabil. 2015;24(2):210–213. [DOI] [PubMed] [Google Scholar]
- 5.Asken BM, McCrea MA, Clugston JR, Snyder AR, Houck ZM, Bauer RM. “Playing through it”: delayed reporting and removal from athletic activity after concussion predicts prolonged recovery. J Athl Train. 2016;51(4):329–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Delahunty SE, Delahunt E, Condon B, Toomey D, Blake C. Prevalence of and attitudes about concussion in Irish schools’ rugby union players. J Sch Health. 2015;85(1): 17–26. [DOI] [PubMed] [Google Scholar]
- 7.. BrainAndSpinalCord.org. Brain Injury Cost. Available at: http://www.brainandspinalcord.org/cost-traumatic-brain-injury. Accessed June 14, 2016.
- 8.Ylvisaker M, Adelson PD, Braga LW, et al. Rehabilitation and ongoing support after pediatric TBI: twenty years of progress. J Head Trauma Rehabil. 2005;20(1):95–109. [DOI] [PubMed] [Google Scholar]
- 9.Glang A, Todis B, Sohlberg M, Reed PR. Helping parents negotiate the system. In: Singer GHS, Glang A, Williams JM, eds. Children with Acquired Brain Injury: Educating and Supporting Families. Baltimore, MD: Paul H Brookes; 1996. [Google Scholar]
- 10.Laxe S, Leon D, Salgado D, Zabaleta M. Description of functional outcome in pediatric traumatic brain injury after a comprehensive rehabilitation programme. Neurocirugia (Astur). 2015;26:84–89. [DOI] [PubMed] [Google Scholar]
- 11.Leonhard MJ, Wright DA, Fu R, Lehrfeld DP, Carlson KF.Urban/rural disparities in Oregon pediatric traumatic brain injury. Inj Epidemiol. 2015;2:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Su YS, Veeravagu A, Grant G. Neuroplasticity in traumaticbrain injury. In: Laskowitz D, Grant G, eds. Translational Research in Traumatic Brain Injury. Boca Raton, FL: CRC Press/Taylor and Francis Group; 2016:163–179. [Google Scholar]
- 13.Ransom DM, Vaughan CG, Pratson L, Sady MD, McGill CA, Gioia GA. Academic effects of concussion in children and adolescents. Pediatrics. 2015;135(6):1043–1050. [DOI] [PubMed] [Google Scholar]
- 14.Shaklai S, Peretz R, Spasser R, Simantov M, Groswasser Z. Long-term functional outcome after moderate-to-severe paediatric traumatic brain injury. Brain Inj. 2014;28(7): 915–921. [DOI] [PubMed] [Google Scholar]
- 15.Dettmer J, Ettel D, Glang A, McAvoy K. Building statewide infrastructure for effective educational services for students with TBI: promising practices and recommendations. J Head Trauma Rehabil. 2014;29(3):224–232. [DOI] [PubMed] [Google Scholar]
- 16.ORCAS Inc. Concussion Management - Brain 101: The Concussion Playbook. Policy and Resource Handbook. Eugene, OR: ORCAS Inc; 2011. Available at: http://orcas-sportsconc2.s3.amazonaws.com/files/A_CMTHandbook.pdf. Accessed January 18, 2015. [Google Scholar]
- 17.DeMatteo C, Stazyk K, Giglia L, et al. A balanced protocol for return to school for children and youth following concussive injury. Clin Pediatr. 2015;54(8):783–792. [DOI] [PubMed] [Google Scholar]
- 18.Baker JG, Rieger BP, McAvoy K, et al. Principles for return to learn after concussion. Int J Clin Pract. 2014;68(11): 1286–1288. [DOI] [PubMed] [Google Scholar]
- 19.Gioia GA. Medical-school partnership in guiding return to school following mild traumatic brain injury in youth. J Child Neurol. 2014;31(1):93–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Glang A, Tyler J, Pearson S, Todis B, Morvant M. Improving educational services for students with TBI through statewide consulting teams. NeuroRehabilitation. 2004;19(3):219–231. [PubMed] [Google Scholar]
- 21.Glang AE, Koester MC, Chesnutt JC, et al. The effectiveness of a web-based resource in improving postconcussion management in high schools. J Adolesc Health. 2015;56(1):91–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hsu CC, Sandford BA. The Delphi technique: making sense of consensus. Pract Assess Res Eval. 2007;12(1):1–8. [Google Scholar]
- 23.Arbogast KB, McGinley AD, Master CL, Grady MF, Robinson RL, Zonfrillo MR. Cognitive rest and school-based recommendations following pediatric concussion: the need for primary care support tools. Clin Pediatr. 2013;52(5):397–402. [DOI] [PubMed] [Google Scholar]
- 24.Halstead ME, McAvoy K, Devore CD, Carl R, Lee M, Logan K. Returning to learning following a concussion. Pediatrics. 2013;132(5):948–957. [DOI] [PubMed] [Google Scholar]
- 25.Majerske CW, Mihalik JP, Ren D, et al. Concussion in sports: post concussive activity levels, symptoms, and neurocognitive performance. J Athl Train. 2008;43(3):265–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) - a metadatadriven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dedoose. Web application for managing, analyzing, and presenting qualitative and mixed method research data. Los Angeles, CA: SocioCultural Research Consultant; 2016. Available at: www.dedoose.com. Accessed February 28, 2017. [Google Scholar]
- 28.StataCorp. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP; 2015. [Google Scholar]
- 29.McAvoy K. Rocky MHC REAP The Benefits of Good Concussion Management. Available at: http://www.concussiontreatment.com/images/REAP˙Program.pdf. Accessed January 15, 2015.
- 30.Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2): 105–112. [DOI] [PubMed] [Google Scholar]
- 31.Brown BE. BrainSTEPS: Students (K-12) with Concussion - Educational Impacts, Symptoms, Accomodations, Return to School Progression. Available at: http://www.pattan.net/Videos/Browse/Single/?code_name=brainsteps_students_k-12_with_concuss. Accessed January 3, 2015.
- 32.Damschroder LJ et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009;4:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Johnson BR, Onwuegbuzie A. Mixed methods research: a research paradigm whose time has come. Educ Res. 2004;33(7):14–26. [Google Scholar]
- 34.Johnson BR, Onwuegbuzie A, Turner LA. Toward a definition of mixed methods research. J Mix Methods Res. 2007;1(2): 112–133. [Google Scholar]
- 35.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. [DOI] [PubMed] [Google Scholar]