Abstract
We evaluated the effect of a nursing home safe resident handling intervention on the ergonomic exposures of nursing assistants. The healthcare version of the Postures, Activities, Tools and Handling (PATH) method was used by 12 observers to examine postures, manual handling, and resident handling pre-intervention and at three months, 12 months, 24 months, and 36 months post-intervention. There were marked downward trends in proportion of work time spent repositioning and transferring residents, and an increased use of handling equipment in transferring (Cochran–Armitage tests: all p-values <0.001). While resident handling, nursing assistants were also more likely post-intervention to be in neutral trunk postures, walking rather than standing still, working with both arms below 60°, and less likely to lift loads greater than 22.7 kg. Lateral transfer devices were infrequently observed in use for repositioning; additional training on the use of this equipment is recommended to increase the benefits from the intervention program.
Relevance to industry:
The study describes reductions in postural and manual handling loads of nursing assistants in nursing homes resulting from increased use of resident handling equipment following equipment installation with training and administrative support.
Keywords: Intervention effectiveness, Nursing home industry, Ergonomics tool, Exposure assessment, Injury risk
1. Introduction
High rates of back and other musculoskeletal disorders (MSDs) have been reported in healthcare workers in both nursing home and hospital settings. Much of this excess is thought to be due to manual handling (lifting, transferring, repositioning) of patients or residents (Collins et al., 2006; Fujimura et al., 1995; Lagerstrom et al., 1998; Smedley et al., 1995, 1997; Trinkoff et al., 2003). In 1998, the National Institute for Occupational Safety and Health (NIOSH) reported that, compared to all other female workers, Certified Nursing Assistants (CNAs) and Licensed Practical Nurses (LPNs) in nursing homes had more than twice the risk of developing work-related low back disorders (NIOSH, 1998). In 2009, nursing aides ranked second for occupations with the most reported work-related injuries and illnesses requiring days away from work and had the highest incidence rate of MSD cases per 10,000 full-time workers (BLS, 2010). A 2010 study reported that 20% of their surveyed sample of nurses experienced severe musculoskeletal symptoms in multiple body regions (Daraisah et al., 2010).
A 1998 review of 42 studies on low back pain among nursing jobs reported relationships between low-back pain and physical factors such as lifts, transfers, ‘save the patient’ situations, awkward work postures, static standing, and working as a nursing aide compared to a registered nurse (RN) (Lagerstrom et al., 1998). Studies of nurses in hospitals reported associations between MSDs and physically demanding tasks such as repositioning and transferring residents. Four of the 42 studies focused on nursing assistants in nursing homes; results indicated that on average, those with low back disorders performed more strenuous tasks and found resident handling more stressful than those who were free from pain.
A guide published by NIOSH, “Safe Lifting and Movement of Nursing Home Residents” (Collins et al., 2006), addressed the challenges of caregiver responsibilities, including manual resident handling in nursing homes. According to the NIOSH report,
“These conditions contributed to the 211,000 occupational injuries suffered by caregivers in 2003. … Due to the ongoing demand for skilled care services, musculoskeletal injuries to the back, shoulder, and upper extremities of caregivers are expected to increase.”
Intervention studies are useful for confirming causal relationships, demonstrating feasibility, and evaluating practicality. Many studies have evaluated ergonomics programs, especially for nurses, in hospital and laboratory settings. These interventions included different types of lifting techniques (Videman et al., 1989), the use of slings (Elford et al., 2000), ceiling-mounted lifts (Nelson et al., 2003a), and mechanical patient lifts (Engkvist, 2006). Results from these studies of nurses have shown smaller numbers of back injuries, less pain, fewer symptoms, and less absence from work due to musculoskeletal symptoms post-intervention.
These studies have assessed interventions for hospital nurses, primarily in laboratory settings; however, some physical exposures for nursing assistants in nursing homes, such as trunk flexion and heavy manual handling, can exceed those of nurses (Boyer, 2008). The majority of direct care in nursing homes, including resident handling, is performed by nursing assistants. Some injury reduction programs for nursing assistants have reported reductions in workers’ compensation claims and lost injury days (Collins et al., 2004; Nelson et al., 2006; Park, RM et al., 2009), OSHA 200 log incidents (Collins et al., 2004; Evanoff et al., 2003), self-reported injury rates (Collins et al., 2004), and claim costs (Nelson et al., 2006; Park, RM et al., 2009); and increased frequencies of perceived lift use (Evanoff et al., 2003).
A 2010 review examined studies of exercise interventions and multi-component patient handling interventions (MCPHI) in healthcare settings (Tullar et al., 2010). The authors defined a MCPHI as a program including injury reduction policies, the purchase of handling equipment, and ergonomic training covering safe patient handling and equipment usage. Although three of these studies were deemed quality evaluations of MCPHIs, only one studied a population of nursing assistants.
Ergonomic stressors of nursing assistants in nursing homes have been assessed through questionnaires, and work-related injuries have been examined by reviewing injury reports and workers’ compensation claims. These measures can be extremely useful; however, examining physical exposures using an observational method will provide objectivity to specific changes in postures and manual handling activities in a real-time nursing home work environment and confirm that exposure reduction is the mechanism by which injury rates have gone down. These types of measurements can be useful in developing strategies for preventing MSDs. The goal of this study was to evaluate a company-implemented multi-component Safe Resident Handling Program (SRHP) over a three year follow-up period in a sample of nursing homes by examining observed changes in resident handling activities, equipment use, and body postures among nursing assistants.
2. Methods
2.1. Background to the intervention process
In 2004, a large nursing home corporation instituted a SRHP to reduce exposure to back injuries related to resident handling. Mechanical devices, training, and protocols for use and maintenance were provided by a third-party firm, which offered the incentive that all equipment purchased would be reimbursed if injury rates were not reduced in one year.
In each center, prior to receiving equipment, RNs assessed each resident’s ability to support body weight. Next, the third-party trainers visited each facility to conduct orientation meetings with department heads and nurses. Equipment, based on the RNs resident assessments, was purchased by the corporation, to be received one week after these meetings, and representatives from the third-party company provided training on equipment use and maintenance to all clinical staff at this time.
Two weeks after the introduction of the equipment, follow-up visits were made by the third-party company to provide training and emphasize policies to the clinical nursing staff. Additional follow-up visits to provide more training, enforce policies, and ensure compliance took place after 4 weeks, 10 weeks, 20 weeks, 30 weeks, 40 weeks, and 50 weeks. All clinical staff had to demonstrate competency in using different types of equipment in order to remain in their jobs. In addition, staff development coordinators were trained to provide training to newly hired employees. Any injuries related to the SRHP were reported to supervisors; incident reports were filed and reported to the third-party company within 24 h of injury.
Nurses evaluated residents’ needs at baseline, and residents were also to be assessed upon admission, re-admission, when a significant change in health occurred, and in quarterly reviews. Assessments for safe patient handling indicated whether a resident was ambulatory, required a sit-stand lift, or required a total body lift of either 204-kilogram or 272-kilogram capacity (floor-based portable lifts). Assessment results were documented in care plans, aide sheets, and electronically. In addition, stickers were applied to residents’ nameplates to indicate the type of equipment to be used (if any), the size of the sling needed, and the number of staff required for turning and repositioning activities. Additional equipment was to be purchased to replace or augment existing equipment as needed over time.
2.2. Study design
At the initiation of this prospective study in 2006, eight centers in the company that had not yet enrolled in the SRHP were identified as eligible for baseline questionnaire surveys (eight centers) and ergonomic observations (four centers). Data were also collected there at 3-month, 12-month, and 24-month follow-up periods.
Subsequently, two facilities which had implemented the SRHP at least one year earlier permitted 12-month and 24-month data collection. Additionally, the nursing home corporation purchased several facilities in 2007 and implemented the SRHP later that year. Ergonomic observations were conducted at one of these newly purchased facilities at baseline, 3-month, 12-months, and 24-months. Last, 36-month data were collected in 2010 at five additional centers. All procedures were reviewed and approved by the University of Massachusetts Lowell Institutional Review Board. Prior to the SRHP all facilities involved in this study had some mechanical lifting equipment; however, device usage was inconsistent.
2.3. Ergonomic exposure assessment method
An adaptation of the method called “Postures, Activities, Tools, and Handling (PATH)” (Buchholz et al., 1996) was used to record the frequencies of ergonomic exposures. PATH is a direct observation work-sampling-based method developed for analysis of jobs without regular work cycles. Multiple ergonomic exposures are recorded in categorical form for a single moment in time, at a fixed time interval (in this case, 60 s); the data are used to estimate the percentage of observations that employees are exposed to each posture or activity. Clinical nursing work lacks short, repetitive work cycles, making the PATH method a useful choice for exposure assessment.
2.4. PATH template development
In order to obtain comparative data on a large number of healthcare job titles, the original PATH method was augmented in some areas and simplified in others. Customization for the jobs to be observed relied upon literature review of studies in nursing homes and hospitals (Myers et al., 2002; Nelson et al., 2003a; Smedley et al., 1995) and PATH observations by Rockefeller (2002) among nursing home workers in Washington.
The template, “Resident Handling,” was designed to record trunk, leg, and arm postures, manual material handling, resident handling, task information, and space constraints. The template included a mix of ordinal, nominal, and dichotomous variables.
Tasks were grouped into four mutually exclusive categories: ‘direct care,’ ‘medical care,’ ‘administrative,’ and ‘other care.’ Resident handling activity was coded when employees were repositioning (moving a resident (or body part) from one area to another on the same surface (e.g. boosting up in bed)); transferring (moving a resident from one surface to another (e.g. bed to wheelchair)); transporting (taking a resident from one place to another using equipment (e.g. wheelchair)); or assisting with ambulation (helping an ambulatory resident walk from one place to another). Resident handling equipment included total body lifts, sit-stand lifts, slings, slideboards, slipsheets and gait belts.
Manual material handling was only encoded if a load of more than 4.5 kg was being handled. The load weight categories were ‘less than 4.5 kg,’ ‘4.5–22.7 kg,’ and ‘greater than 22.7 kg.’
2.5. Data collection procedures
Twelve observers were trained to collect PATH data. Data collectors were professional ergonomists, graduate students in ergonomics, and undergraduate students in biology or kinesiology at the University of Massachusetts Lowell and the University of Connecticut; several of them had previous experience with its use in other settings. Training included review of the template and definitions, viewing video samples, discussion regarding the technique of posture coding, and evaluation of inter-rater agreement prior to field data collection.
Data were collected on six personal digital assistants (PDAs) equipped with touch screen technology, which facilitated field data collection via a stylus pen. The observation software used was InspectWrite™, marketed by Penfact Inc. (Boston MA). The PDAs were re-charged each day prior to field data collection and PATH data were downloaded into the authoring workstation at the close of each observation day.
Inter-rater reliability (IRR) was tested among pairs of observers who simultaneously observed a single subject. Agreement between paired observations was evaluated by raw percent agreement and kappa statistics (using SAS 9.1). Eighty percent agreement was considered adequate IRR for this study.
The modified PATH data collection protocol involved observation of clinical employees [nursing assistants (CNAs) and nurses (LPNs, and RNs)] in sessions lasting from one to eight hours based on employees’ schedules, preferences, and other external factors. Trained observers who had satisfied project criteria for IRR obtained informed consent from the targeted employees and recorded demographic characteristics for each employee recruited.
Because of the large amount of resident handling performed by nursing assistants, they were preferentially selectively recruited for ergonomic observations. RNs were rarely recruited once it became clear that they performed little resident handling. Individual workers were selected by convenience and followed exclusively for the duration of the observation period. Due to the sensitive nature of their work, some residents were not comfortable allowing researchers to observe tasks such as bathing and toileting. In these instances, missing observations were recorded as ‘not observed/not sure.’ As much as possible, follow-up observations were completed with the same individual workers who had volunteered to participate in previous data collection periods. Workers were paid an incentive for participation following each observation period.
2.6. Data management and analysis
Physical exposure data recorded on the PDAs were downloaded into the authoring workstation, cleaned, and documented in a standardized format. Each entry was identified by facility, department, and job code for data linkage; each individual employee was identified by ID number. Data were analyzed using SAS 9.2. Cochran–Armitage trend tests (Agresti, 2002) were computed (p-values and confidence limits) to determine the statistical significance of changes in ergonomic exposures over time.
An analysis of observations by time of day was performed to determine whether equipment use and resident handling activities were distributed similarly across data collection periods. Observations were grouped according to ‘heavy,’ ‘medium,’ and ‘light’ work for the analyses of resident handling activities and equipment use. The ‘heavy’ manual handling activities were observed between the hours of 7:00 am and 11:00 am, when most direct care of residents takes place, including bathing, dressing, repositioning, and transferring. The ‘light’ manual handling activities, including transporting residents in wheelchairs, were observed at mealtimes, between 11:00 am and 1:00 pm and again from 3:00 pm to 5:00 pm; toileting activities occurring between 1:00 pm and 3:00 pm represented a more intermediate level (‘medium’) of manual handling.
2.7. Healthcare workers questionnaire
All direct-care employees over the age of 18 were invited to complete the standardized questionnaire in each facility at each of the five data collection periods. Compensation of $20 was offered in exchange for each completed questionnaire returned with informed consent form.
The self-administered questionnaires included questions regarding current and recent health endpoints, psychosocial risk factors, workplace factors, demographics, brief medical history of selected conditions; health behaviors; health beliefs; acute injuries during the previous year; workplace physical assault during the past year; participation in sports or leisure activities; and responsibilities for family members and household work. Health endpoints of primary concern were musculoskeletal symptoms and current self-reported mental and physical health. Questions focusing on the frequency of lifting device use and reasons for not using devices were identified for analysis. At this point questionnaires were not cross-linked with the PATH observational data.
3. Results
Fifty-one observation periods of nursing assistants were completed at baseline, 56 at the 3-month follow-up, 100 at the 12-month follow up, 88 at the 24-month follow-up, and 58 at the 36-month follow up. In some instances nursing assistants were associated with more than one observation period per time period. These observation periods resulted in a total of 98,903 observation moments with more than 15,000 at each survey period. Demographic information on all of the workers observed is presented in Table 1.
Table 1.
Population demographics.
| Baseline | 3-Month | 12-Month | 24-Month | 36-Month | |
|---|---|---|---|---|---|
| Number of observation periods | 81 | 69 | 135 | 103 | 58 |
| Number of observation moments | 15,185 | 16,031 | 25,472 | 24,652 | 17,563 |
| Gender (% female) | 81% | 85% | 95% | 95% | 93% |
| Mean tenure (years)Job titles | 5.20 | 4.86 | 4.87 | 4.61 | 4.50 |
| Job titles | |||||
| GNA/CNA | 74% | 81% | 74% | 85% | 98% |
| CMA | 4% | 7% | 9% | 1% | 0% |
| LPN | 11% | 9% | 16% | 11% | 0% |
| RN | 5% | 3% | 1% | 3% | 2% |
| Other | 6% | 0% | 0% | 0% | 0% |
3.1. Baseline activities and ergonomic exposures
At baseline, nursing assistants were observed performing more resident handling activities (13.8% of total observations) than LPNs (2.4%) and RNs (0.3%). RNs were not discussed further in this study due to sparse data.
Baseline trunk postures while resident handling were compared among LPNs, nursing assistants, and nursing assistants while handling residents, and it was clear that nursing assistants work in more non-neutral trunk angles including flexion, laterally bent, and twisted postures (34% of observations) especially when handling residents (70% of resident handling observations) compared to LPNs (26% of observations). Nursing assistants were more often observed in static standing than LPNs, who were more likely to use dynamic leg actions (e.g. walking). Additionally, nursing assistants worked with at least one arm raised above 60° more often than did LPNs. Nursing assistants were also observed performing more manual handling of heavier loads (greater than 4.5 kg), both with a neutral and a flexed trunk, than were LPNs.
3.2. Resident handling and equipment use after SRHP implementation
At each data collection period, between 50 and 60% of observations were collected at times of the day when participants were performing ‘heavy’ work. At the 36-month follow-up, the proportion of resident handling activities decreased, and the proportion of resident handling observations in which equipment was used increased from 10% to 32%. The percentage of time that nursing assistants were observed handling residents decreased substantially two years after the program began, but by the end of three years the percentage of time had increased slightly (p < 0.001 test of overall trend) (Fig. 1). There was a substantial increase in the frequency of using resident handling equipment over the three-year follow-up (p < 0.001) (Fig. 2).
Fig. 1. Frequency of resident handling.* †.
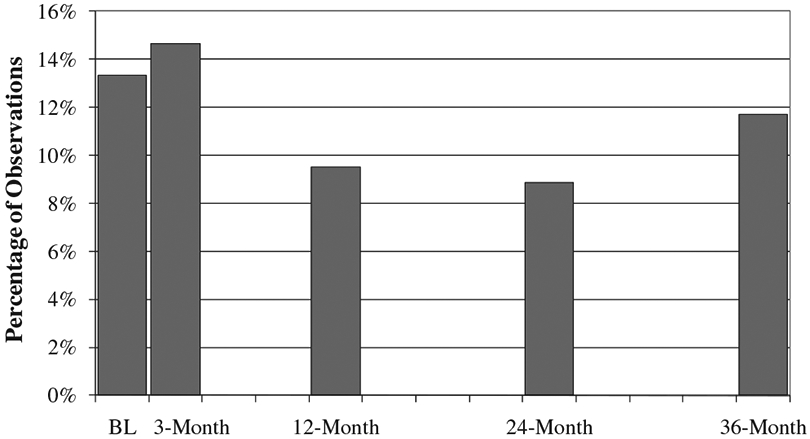
* Resident Handling Activities include Ambulation Assist, Reposition, Transfer and Transport
† p < 0.001 (Cochran-Armitage test of trend)
Fig. 2. Equipment use* while resident handling.†,††.
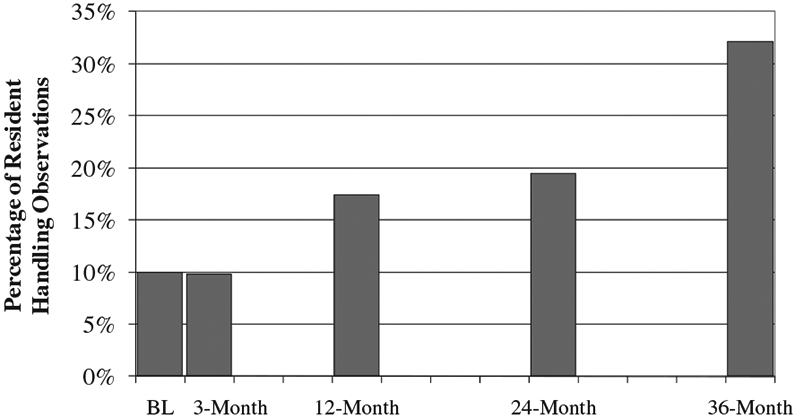
* Equipment includes Total Body Lifts, Sit-Stand Lifts, Slings, Slideboards, Slipsheets, and Gait-belts
† Resident Handling Activities include Ambulation Assist, Reposition, Transfer and Transport
†† p < 0.001 (Cochran-Armitage test of trend)
Within resident handling activities, repositioning and transferring were of particular interest because they require more physical effort than assisting with ambulation or transporting residents in wheelchairs, which also do not require the use of (or benefit from) handling equipment. The percentage of time observed repositioning decreased from 9.3% at baseline to 3.4% at the 36-month follow-up (p < 0.001), while the percentage of time observed transferring (manual or mechanically assisted) remained about the same for two years then increased after 36-months (Fig. 3).
Fig. 3.
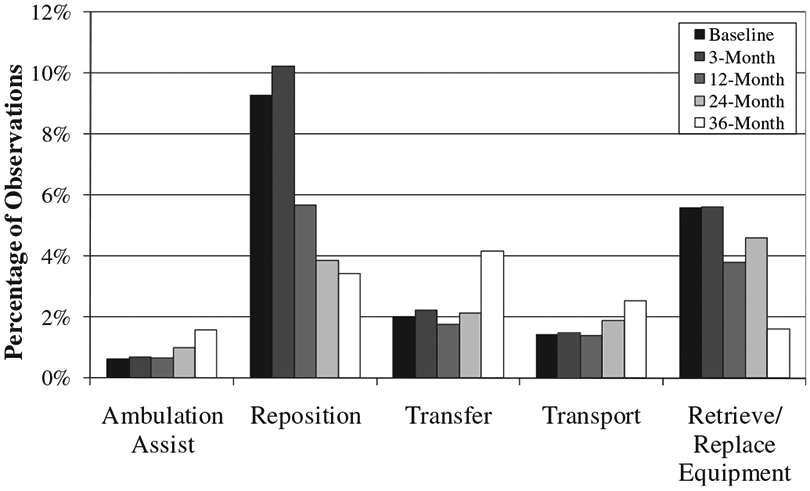
Frequency of resident handling activities.
The frequency with which aides were observed in the task ‘Retrieve/Replace Equipment’ was examined. The percentage of time spent performing this task decreased by the end of the 36-month follow-up (Fig. 3).
The extent of equipment usage while repositioning and transferring increased over time (both p-values <0.001); this trend was more pronounced for transfers (Fig. 4).
Fig. 4. Equipment use* while repositioning† and transferring.†.
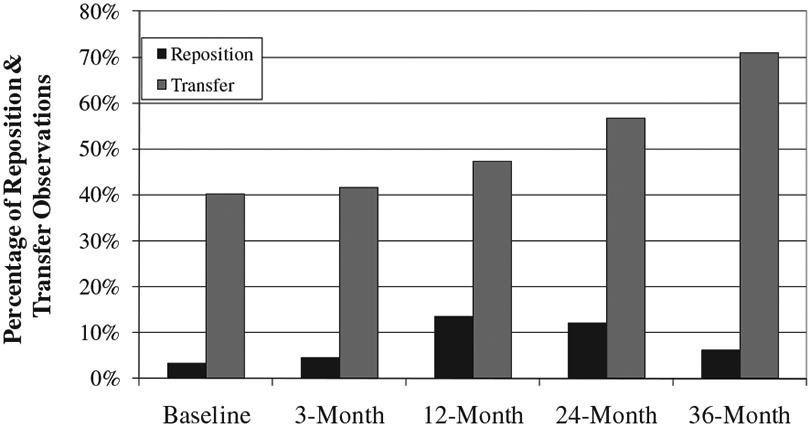
* Equipment includes Total Body Lifts, Sit-Stand Lifts, Slings, Slideboards, Slipsheets, and Gait-belts
† p < 0.001 (Cochran-Armitage test of trend)
At the 24-month follow-up, handling equipment was used for about 57% of transferring observations and about 12% of repositioning observations. At the same survey period questionnaire responses indicated that about two-thirds of the population ‘often’ or ‘always’ used patient lifting devices. The main reasons given for not using equipment every time were ‘device unavailable when needed (25%),’ ‘residents dislike them (14%),’ ‘I feel I don’t need them (14%),’ ‘not enough time (7%),’ ‘too much extra effort (5%),’ and ‘my co-workers don’t use them (4%)’ (responses not mutually exclusive). When asked to report additional reasons why lifting equipment was not always used, the most commonly reported answers included ‘some residents do not require lifts,’ ‘it is not part of my job,’ ‘there are not enough staff,’ and ‘someone else is using it.’
Weight in hands while repositioning and transferring was also examined (Fig. 5). Both while repositioning and transferring, the weight in hands category of 4.5–22.7 kg only decreased at 36 months. However there were observed decreases (p < 0.001) in the amount of time spent handling loads greater than 22.7 kg for both activities, (8.3%–1.8% of repositioning observations and 17%–2.6% of transferring observations). This corresponded to increases in the lowest weight category for both activities, though the increase was larger while transferring.
Fig. 5. Weight in hands while repositioning and transferring.
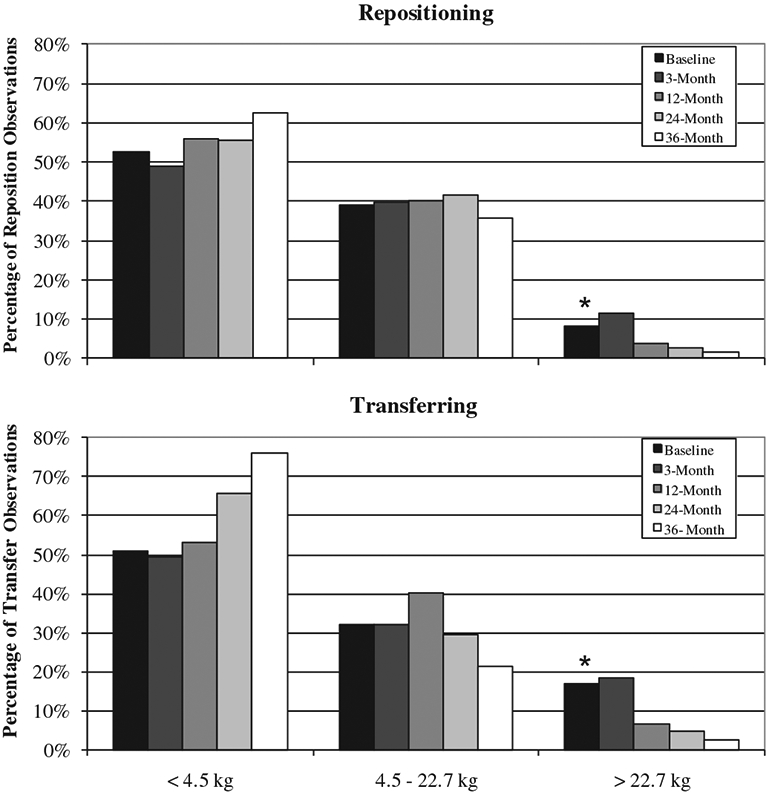
* p < 0.001 (Cochran-Armitage test of trend)
3.3. Changes in body postures after SRHP implementation
There were considerable differences across the five data collection periods in body postures while resident handling. By the 36-month follow-up, the observed occurrence of neutral trunk postures increased from 31% to 67% (p < 0.001), while moderate and severe flexion and lateral bent and twisted trunk postures all declined (Fig. 6).
Fig. 6. Changes in trunk posture while resident handling.*.
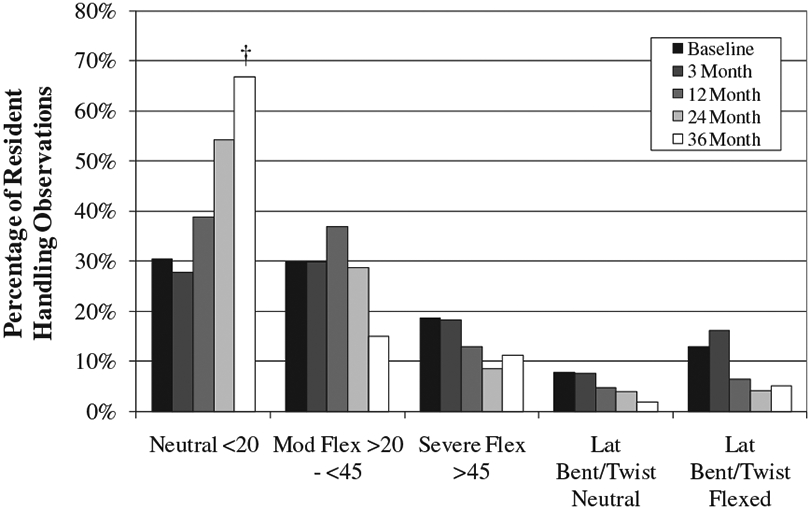
* Resident Handling Activities include Ambulation Assist, Reposition, Transfer and Transport
† p < 0.001 (Cochran-Armitage test of trend)
After 36 months, nursing assistants were observed handling residents with both arms below 60° about 75% of the time, compared to 38% at baseline, while the proportion of time spent working with one or both arms greater than 60° decreased (p < 0.001) (Fig. 7).
Fig. 7. Changes in arm angle while resident handling.*.
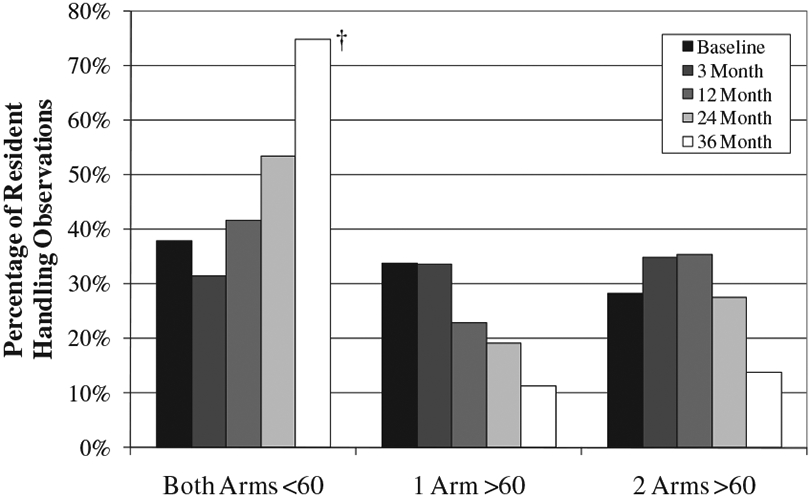
* Resident Handling Activities include Ambulation Assist, Reposition, Transfer and Transport
† p < 0.001 (Cochran-Armitage test of trend)
After 36 months, it was also observed that nursing assistants were standing still while resident handling 63% of the time compared to 81% of the time at baseline (p < 0.001). This corresponded to an increase in dynamic leg actions including walking (p < 0.001) (Fig. 8).
Fig. 8. Changes in leg action while resident handling.*.
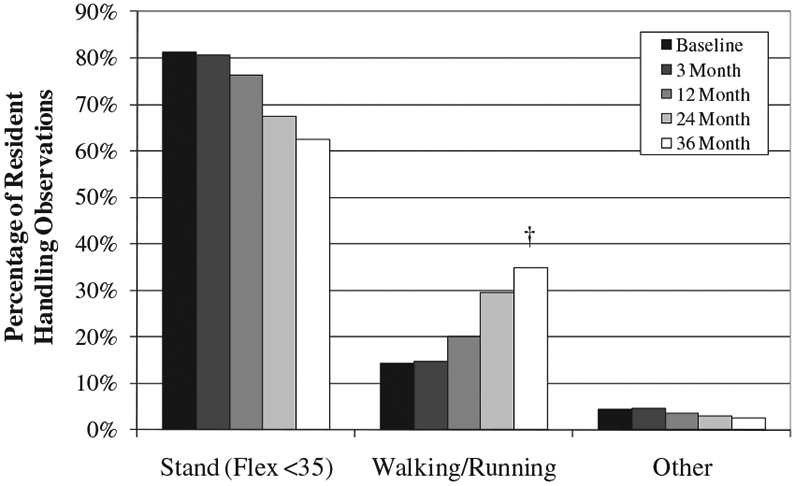
* Resident Handling Activities include Ambulation Assist, Reposition, Transfer and Transport
† p < 0.001 (Cochran-Armitage test of trend)
4. Discussion
Almost 99,000 observations from a convenience sample of nursing assistants were collected over three years to allow enough time for changes in exposures to occur. Observations were made in real-time workplace settings with a method that generates percentages of work time spent in pre-determined postures, tasks and activities. Many favorable trends were observed among nursing assistants over three years: equipment use increased; time spent handling residents decreased (specifically repositioning); and work was performed with more neutral trunk postures, fewer flexed, laterally bent, or twisted trunk postures, less static standing and more dynamic leg action, and more often with both arms below 60°. Because 50–60% of the observations at each data collection period were collected while nursing assistants performed ‘heavy’ work such as resident handling, bathing, dressing residents, and toileting, this suggests that changes in resident handling activities, equipment use, and postures were not related to the time of day the observations were made.
Nursing assistants were sometimes observed to walk while transferring residents in lifts. Once a resident was raised using a total body lift, a nursing assistant would usually walk while pushing the lift for a short time in order to position the resident over a wheelchair, commode, or bed. Without lifting equipment, a nursing assistant would typically transfer a resident while in a static standing or shallow squat position. Prolonged standing can increase the risk for lower limb symptoms such as poor circulation, swelling in the feet and legs, and joint damage. Additionally, nursing assistants’ trunk postures are most likely neutral while using lifts to transfer residents. The quantitative results indicate that the use of mechanical lifts reduced the need for nursing assistants to work in stressful body postures during resident handling.
Although the observational method used in this study does not output a total measure of mechanical load on the body, the postural analyses demonstrated increases in more favorable body postures while resident handling. Nursing assistants were also observed lifting loads less than 4.5 kg more frequently and loads greater than 22.7 kg less frequently. It is reasonable to assume that the effect of the SRHP on non-neutral postures and lifting led, in turn, to reduced loading on the body including lower forces on the lumbar spine and shoulders. Several laboratory studies have evaluated loading on the body resulting from patient handling tasks and have demonstrated reductions in biomechanical stress on the caregiver achieved by using mechanical lift devices (Garg, 1992a; Garg and Owen, 1992b; Nelson et al., 2003b; Zhuang et al., 1999).
A major finding of this study showed that after three years, nursing assistants used lifting equipment more than 50% of the time while transferring. It should be noted that not all residents require lifting equipment for transferring. However, handling equipment was used only about 12% of the time while repositioning after two years and 6% of the time after three. While this is an increase from about 3% at baseline, the results may indicate that there are some gaps in training at the centers. Because nursing assistants use equipment more often for transfers than repositions, they may feel that the use of equipment is more important for transferring than repositioning. However, handling equipment purchased for the SRHP included slideboards and slipsheets in addition to lifting equipment. These devices are inexpensive, available at the facilities, and are designed to help reduce stress on the body while repositioning.
Lateral repositions were reported to be the most frequent type of patient handling tasks in a recent study (Callison and Nussbaum, 2012). Fragala (2011) recognizes the lack of progress in reducing caregivers’ risk of injury while repositioning and then presents reduced workload related to repositioning patients using lateral transfer devices. Efforts have recently been made by the corporation to address the lack of equipment used for lateral repositions. Policies to increase the use of these devices were recently implemented; however this study had concluded prior to implementation, so our observational data did not capture the results of this new effort.
Results from the 24-month healthcare workers’ questionnaire indicated that two-thirds of nursing assistants use resident handling equipment often or always, while results from the observational assessment indicated that equipment was used for about 57% of transfers. The difference in self-reported and observed equipment use may have related to workers’ responses for reasons equipment was not used (availability of devices, residents’ dislike of equipment, perception that devices were not necessary, and lack of time). The difference may also be due to the necessity of using equipment on the basis of individual resident acuity.
In 1993, Fragala (Fragala, 1993) reported some reasons why patient lifts were not used in healthcare settings, such as additional time required, lack of accessibility, difficulty using devices, and residents' resistance to devices. These are similar to the major reasons nursing assistants reported for not using equipment in this study.
Retrieval of necessary equipment for handling residents has been reported as one reason contributing to the perceived increase in time for performing mechanically assisted lifting (Schoenfisch et al., 2011) However, in our study the amount of time spent retrieving and replacing equipment declined over time.
4.1. Limitations and strengths of this study
A limitation of this study is related to the convenience sample of ergonomic observations focused on nursing assistants. Due to facility access limitations and difficulties experienced in gaining consent from individuals within the study population, this selection process was the only method used in this study. The research team, however, made a concerted effort to recruit nursing employees across the full range of units, patient populations, and seniority levels in each facility. A random sample of individuals might have better ensured a representative population; however, the demographics of observed workers corresponded fairly well to the total study population. A large sample of observation moments was collected at each data collection period, which helped provide an extensive exposure profile for nursing assistants. Additionally, attempts to observe the same workers on the same shifts on follow-up visits were made, to standardize for any possible differences in work technique.
Another weakness is the possibility for the “Hawthorne effect,” which occurs when observed employees work differently simply because they are being observed. While this could not be ruled out, it is unlikely that it could explain away the exposure trends observed in this study. Overall, it was observed that resident handling equipment was used frequently at the study facilities, including by employees who were not under formal observation. At the same time, lifting equipment was not always used for every transfer, whether observed or not. In addition, the frequency of observed equipment usage while resident handling was actually lower than the nursing assistants’ self-reported usage during resident handling activities. This suggests that the Hawthorne effect probably did not play a significant role in the observed changes, because it would presumably have produced a bias in the direction of more usage, rather than less, and more so among workers whose activities were being recorded. In addition, it seems unlikely that workers could have known to adjust their body postures, or to do so intentionally, purely as an artifact of being observed.
The load weight categories of ‘4.5–22.7 kg’ and ‘greater than 22.7 kg’ are wide intervals for manual handling and may result in loss of sensitivity to real changes in weight in hands in the workplace. However, the way the categories were defined made it easier for observers to visually judge manual handling activities in a timely manner, since data were collected at 60 s intervals.
It is possible that some misclassification of exposures was made due to observer error. Observer error may result at the boundary lines of postures, such as that between moderate and severe flexion. However, observers were trained to underestimate postures in the case of boundary line uncertainty. Additionally, all observers attained a minimum of 80% agreement and kappa scores of at least 0.6 for IRR in all variable categories prior to collecting data for the study. PATH has been validated relative to direct instrumentation (Paquet et al., 2001), conditional upon adequate observer training and good inter-rater agreement (Park, JK et al., 2009). By ensuring high IRR for all observers, the amount of random and systematic error in the recording of observational data was limited and probably would not have affected internal comparisons.
5. Conclusions and recommendations
Many SRHP interventions in healthcare have focused on nurses in hospitals; fewer studies have examined the long-term care sector. Since nursing assistants perform the majority of resident handling in nursing homes, they stand to benefit the most from this type of intervention. This study demonstrated decreased time spent manually handling residents, increased neutral trunk postures while transferring and repositioning, decreased flexed, twisted, and laterally bent postures while transferring and repositioning, and decreased lifting of loads greater than 22.7 kg three years following the intervention.
Most SRHP intervention studies have reported findings based on questionnaire responses or administrative data such as injury rates and workers’ compensation claims. Future analyses examining injury rates and workers’ compensation claims at the centers should provide a more descriptive picture of the overall benefits from the increased use of resident handling equipment.
Analyses in this study also suggest the need for additional training in the centers on other types of handling equipment aside from total body lifts and sit-stand lifts. Slide boards and slipsheets are useful tools for eliminating stress on the body during lateral repositions. Considering that repositioning activities occur about twice as often as transferring activities, nursing assistants could benefit from increased usage of these devices.
Sustainability due to turnover of administrators and front line caregivers was identified as a barrier to the success of a similar SRHP in Washington State (Silverstein et al., 2003). Support for SRHPs is crucial to their success, and turnover rates can be very high in the nursing home industry. Part of the SRHP in this study included the training of staff development coordinators at each facility who could then provide training to newly-hired direct care employees to help reduce gaps in knowledge. In this study the ownership of the SRHP training was turned over from the third-party company to the individual nursing homes 36 months postintervention. The continued success of these programs will now depend on the efforts of individual centers, and future investigations are planned to evaluate further sustainability of the SRHP.
Several states have passed safe patient handling legislation in recent years. Although this is a step in the right direction, the laws are not comprehensive enough to adequately protect all healthcare workers. Some of these laws cover hospitals only, and most do not have a detailed plan for purchasing and maintaining handling equipment. Results from this intervention demonstrate benefits to nursing assistants in nursing homes in terms of reduced postural and manual handling loads resulting from increased use of handling equipment. Programs such as this SRHP have the potential to ensure maximum health and safety benefits to all healthcare workers.
Acknowledgments
This study was supported by Grant Number U19-OH008857 from the U.S. National Institute of Occupational Safety and Health (NIOSH). The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official views of NIOSH. We thank Donna LaBombard and Deborah Slack Katz for assistance with entry into the study sites and Susan Yuhas and Suzanne Nobrega for liaising with the centers. Jamie Tessler, Kendra Kincaid, Sam Agyem-Bediako, Brad Schugardt, XiaoLu Jing, Narendra Vaidya, Michelle LaBoda, Alex Neusner, and Priyadarshini Dasgupta assisted with the PATH worker observations.
References
- Agresti A, 2002. Categorical Data Analysis, second ed. Wiley, Hoboken. [Google Scholar]
- Boyer J, 2008. Ergonomic Exposures, Socioeconomic Status and Musculoskeletal Disorder Risk among Healthcare Workers. Doctoral dissertation. University of Massachusetts Lowell, Lowell, MA. [Google Scholar]
- Buchholz B, Paquet V, Punnett L, Lee D, Moir S, 1996. PATH: a work sampling-based approach to ergonomic job analysis for construction and other non-repetitive work. Appl. Ergon 27, 177–187. [DOI] [PubMed] [Google Scholar]
- Bureau of Labor Statistics [BLS], U.S. Dept. of Labor, 2010. Incidence Rates of Nonfatal Occupational Injuries and Illnesses by Case Type and Ownership, Selected Industries, 2009. Retrieved January 9, 2011 from: http://www.bls.gov/news.release/osh.t01.html. [Google Scholar]
- Callison MC, Nussbaum MA, 2012. Identification of physically demanding patienthandling tasks in an acute care hospital. Int. J. Ind. Ergon 42 (3), 261–267. [Google Scholar]
- Collins JW, Wolf L, Bell J, Evanoff B, 2004. An evaluation of a “best practices” musculoskeletal injury prevention program in nursing homes. Inj. Prev 10 (4), 206–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins JW, Nelson A, Sublet V, 2006. Safe Lifting and Movement of Nursing Home Residents. National Institute of Occupational Safety and Health (NIOSH), Cincinnati, OH. Publication No. 2006–117. [Google Scholar]
- Daraisah NM, Cronin SN, Davis LS, Shell RL, Karwowski W, 2010. Low back symptoms among hospital nurses, associations to individual factors and pain in multiple body regions. Int. J. Ind. Ergon 40 (1), 19–24. [Google Scholar]
- Elford W, Straker L, Strauss G, 2000. Patient handling with and without slings: an analysis of the risk of injury to the lumbar spine. Appl. Ergon 31, 185–200. [DOI] [PubMed] [Google Scholar]
- Engkvist IL, 2006. Evaluation of an intervention comprising a no lifting policy in Australian hospitals. Appl. Ergon 37 (2), 141–148. [DOI] [PubMed] [Google Scholar]
- Evanoff B, Wolf L, Aton E, Canos J, Collins J, 2003. Reduction in injury rates in nursing personnel through introduction of mechanical lifts in the workplace. Am. J. Ind. Med 44 (5), 451–57. [DOI] [PubMed] [Google Scholar]
- Fragala G, 1993. Injuries cut with lift use in ergonomics demonstration project. Provider 19 (10), 39–40. [PubMed] [Google Scholar]
- Fragala G, 2011. Facilitating repositioning in bed. AAOHN J. 59 (2), 63–68. [DOI] [PubMed] [Google Scholar]
- Fujimura T, Yasuda N, Ohara H, 1995. Work-related factors of low back pain among nursing aides in nursing homes for the elderly. Sangyo. Eiseigaku. Zasshi 37 (2), 89–98. [DOI] [PubMed] [Google Scholar]
- Garg A, 1992a. Occupational biomechanics and low-back pain. Occup. Med. State Art Rev 7 (4), 609–628. [PubMed] [Google Scholar]
- Garg A, Owen B, 1992b. Reducing back stress to nursing personnel: an ergonomic intervention in a nursing home. Ergonomics 35 (11), 1353–1375. [DOI] [PubMed] [Google Scholar]
- Lagerstrom M, Hansson T, Hagberg M, 1998. Work-related low-back problems in nursing. Scand. J. Work Environ. Health 24 (6), 449–464. [DOI] [PubMed] [Google Scholar]
- Myers D, Silverstein B, Nelson NA, 2002. Predictors of shoulder and back injuries in nursing home workers: a prospective study. Am. J. Ind. Med 41, 466–476. [DOI] [PubMed] [Google Scholar]
- National Institute for Occupational Safety and Health, 1998. Low Back Disorders. Retrieved March 21, 2007 from: http://www.cdc.gov/niosh/nrlowbck.html. [Google Scholar]
- Nelson A, Lloyd J, Menzel N, Gross C, 2003a. Preventing nurses’ back injuries. AAOHN J. 51 (3) [PubMed] [Google Scholar]
- Nelson A, Lloyd JD, Menzel N, Gross C, 2003b. Preventing nursing back injuries: redesigning patient handling tasks. AAOHN J. 51 (3), 126–134. [PubMed] [Google Scholar]
- Nelson A, Matz M, Chen F, Siddharthan K, Lloyd J, Fragala G, 2006. Development and evaluation of a multifaceted ergonomics program to prevent injuries associated with patient handling tasks. Int. J. Nurs. Stud 43 (6), 717–733. [DOI] [PubMed] [Google Scholar]
- Paquet V, Punnett L, Buchholz B, 2001. Validity of fixed-interval observations for postural assessment in construction work. Appl. Ergon 32 (3), 215–224. [DOI] [PubMed] [Google Scholar]
- Park JK, Boyer J, Tessler J, Casey J, Schemm L, Gore R, Punnett L, 2009a. Interrater reliability of PATH observations for assessment of ergonomic risk factors in hospital work. Ergonomics 52 (7), 820–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park RM, Bushnell PT, Bailer AJ, Collins JW, Stayner LT, 2009b. Impact of publicly sponsored interventions on musculoskeletal injury claims in nursing homes. Am. J. Ind. Med 52 (9), 683–697. [DOI] [PubMed] [Google Scholar]
- Rockefeller K, 2002. Ergonomics demonstration project: skilled nursing facility. Appl. Occup. Environ. Hyg 17 (7), 470–474. [DOI] [PubMed] [Google Scholar]
- Schoenfisch AL, Myers DJ, Pompeii LA, Lipscomb HJ, 2011. Implementation and adoption of mechanical patient lift equipment in the hospital setting: the importance of organizational and cultural factors. AJIM. 54, 946–954. [DOI] [PubMed] [Google Scholar]
- Silverstein B, Rockefeller K, Howard N, Kalat J, Pollisar N, 2003. Getting to Zero in Washington State Nursing Homes: Final Report on Intervention Effectiveness. SHARP Technical Report 61-05-2003. [Google Scholar]
- Smedley J, Egger P, Cooper C, Coggon D, 1995. Manual handling activities and risk of low back pain in nurses. Occup. Environ. Med 52, 160–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smedley J, Egger P, Cooper C, Coggon D, 1997. Prospective cohort study of predictors of incident low back pain in nurses. Br. Med. J 314, 1225–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trinkoff AM, Lipscomb JA, Geiger-Brown J, Storr CL, Brady BA, 2003. Perceived physical demands and reported musculoskeletal problems in registered nurses. Am. J. Prev. Med 24 (3), 270–275. [DOI] [PubMed] [Google Scholar]
- Tullar JM, Brewer S, Amick BC 3rd, Irvin E, Mahood Q, Pompeii LA, Wang A, Van Eerd D, Gimeno D, Evanoff B, 2010. Occupational safety and health interventions to reduce musculoskeletal symptoms in the health care sector. J. Occup. Rehabil 20 (2), 199–219. [DOI] [PubMed] [Google Scholar]
- Videman T, Rauhala H, Asp S, Lindström K, Cedercreutz G, Kämppi M, Tola S, Troup JD, 1989. Patient-handling skill, back injuries, and back pain: an intervention study in nursing. Spine 14 (2), 148–156. [DOI] [PubMed] [Google Scholar]
- Zhuang Z, Stobbe TJ, Hsiao H, Collins JW, Hobbs GR, 1999. Biomechanical evaluation of assistive devices for transferring residents. Appl. Ergon 30, 285–294. [DOI] [PubMed] [Google Scholar]


