Abstract
Manual resident handling (RH) tasks increase risk of musculoskeletal disorders (MSDs) for clinical staff in nursing homes. To reduce the incidence and cost of MSDs, a large healthcare corporation instituted a Safe Resident Handling Program (SRHP) comprising purchase of mechanical lifting equipment, worker training, and detailed usage/maintenance protocols. The program was initially administered by a third-party company; after three years, program responsibility shifted to individual centers.
Workers’ compensation claim rates were compared before and after SRHP implementation. Claims and FTEs were classified as “pre-SRHP,” “first post period” (up to 3 years post-SRHP), or “second post period” (4–6 years post-SRHP), based on claim date relative to implementation date for each center.
Complete data were available for 136 nursing homes with average annual employment of 18,571 full-time equivalents. Over the 8-year period, 22,445 claims were recorded. At each time period, the majority of RH claims affected the back (36% low, 15% other) and upper extremity (26%). Workers’ compensation claims were reduced by 11% during the first post period and 14% during the second post period. RH-related claims were reduced by 32% and 38%, respectively. After six years, the rate for all claims had decreased in 72% of centers, and RH claim rates decreased in 82%. Relative risk for post-/pre-SRHP injury rates increased for centers with less developed wellness programs, unionized centers, and centers with higher LPN turnover pre-SRHP. Injury reduction among these nursing home workers is plausibly attributable to the introduction of mechanical lifting equipment within the context of this multi-faceted SRHP.
Keywords: Intervention studies, Safe resident handling program, Healthcare ergonomics, Musculoskeletal disorders, Workers’ compensation claims
1. Introduction
According to the Bureau of Labor Statistics (BLS) in 2014, the incidence rate of non-fatal occupational injuries and illnesses for nursing care facilities was 7.1/100 full-time workers (total recordable cases); the rate for cases involving days away from work, job transfer, or restriction was 4.3/100 (U.S. Department of Labor, 2015a). In contrast, the rates for construction workers were 3.6/100 for total recordable cases and 2.0/100 for cases involving days away from work, job transfer, or restriction (U.S. Department of Labor, 2015a). Compared to all occupations, nursing assistants suffered the second-highest number of lost-time musculoskeletal disorder (MSD) cases in 2014 (U.S. Department of Labor, 2015b). In that job group, 54% of lost-time incidents were classified as MSDs, compared to 26% among construction workers (U.S. Department of Labor, 2015b).
In nursing homes, caregivers perform heavy lifting, transferring, and repositioning of residents, a task which often exceeds the lifting capacity of most nursing staff (Collins et al., 2004). Several factors contribute to the difficulty of resident transfers, including residents’ weight, combativeness, and tendency to fall or lose balance (Collins et al., 2006). Resident or patient handling has been identified as one of the main causes of back injury among nursing personnel (Trinkoff et al., 2003; Smedley et al., 1997); in addition to the lifting itself, this activity often involves non-neutral postures, such as trunk flexion and rotation, and sudden movements (Engkvist et al., 1998). Upper extremity pain in nursing personnel has also been associated with physical demands such as lifting, stooping, and other awkward postures (Trinkoff et al., 2003). The rising rate of obesity in the United States (Centers for Disease Control and Prevention (CDC), 2007) – affecting nursing home residents as well – raises concerns about further increases in risk of injury for workers that handle these residents (Lapane and Resnik, 2006).
Mechanical lifting equipment has produced significant reductions in biomechanical loading during patient handling in laboratory trials (Zhuang et al., 1999; Elford et al., 2000; Nelson et al., 2003). In addition, safe handling programs – including training programs for proper use and maintenance of the equipment – have shown benefits for worker health in hospitals (Trinkoff et al., 2003; Engkvist, 2006; Li et al., 2004; Evanoff et al., 2003; Lipscomb et al., 2012; Hunter et al., 2010; Black et al., 2011; Schoenfisch et al., 2013) and nursing homes (Collins et al., 2004; Evanoff et al., 2003; Park et al., 2009; Nelson et al., 2006; Engst et al., 2005; Garg, 1999; Restrepo et al., 2013). The nursing home studies, in particular, have reported reductions in a variety of outcome measures: injury rates (Evanoff et al., 2003; Nelson et al., 2006; Garg, 1999); resident handling (RH) injury rates (Collins et al., 2004); claims for repositioning injuries (Garg, 1999); lost workday injuries (Collins et al., 2004; Evanoff et al., 2003; Nelson et al., 2006; Garg, 1999); OSHA 200 log incidents (Collins et al., 2004; Evanoff et al., 2003); self-reported injury rates (Collins et al., 2004); and workers’ compensation (WC) claim costs (Collins et al., 2004; Park et al., 2009; Nelson et al., 2006; Engst et al., 2005; Garg, 1999; Restrepo et al., 2013).
Most nursing home studies included only a few facilities. One study (Park et al., 2009) covered 887 nursing homes in the state of Ohio; however, the interventions varied from center to center and only 10.6% of employers purchased equipment as part of their intervention programs. Typical post-intervention follow-up periods for nursing home studies have been around two years (Collins et al., 2004; Evanoff et al., 2003; Park et al., 2009; Garg, 1999), however one study of six nursing homes (and one hospital) had follow-up periods that ranged from three to five years, but the sample was small and interventions and pre-and post-intervention periods were not uniform (Garg and Kapellusch, 2012). Analysis of longer pre- and post-intervention periods in a larger sample would better describe long-term sustainability and diminish the likelihood that any apparent benefits are artifacts of short-term changes in injury reporting. This paper details the findings of an eight-year prospective intervention study of a multi-component safe resident handling program (SRHP) in a chain of more than 200 nursing homes. The primary goal was to assess whether rates of injury among nursing home staff were reduced in the six years following SRHP implementation.
2. Methods
2.1. Program and study design
A large nursing home corporation instituted a SRHP to reduce the incidence and cost of musculoskeletal problems among the clinical nursing staff. This program entailed purchase and installation of mechanical resident handling aids as well as staff training in the use of the devices and detailed protocols for equipment maintenance, sling laundering, and battery recharging. The program was implemented in March, 2004, by a risk management company specializing in SRHPs.
The implementation process for each center began with a department head meeting (DHM), to inform staff of their roles in the changes necessary for an effective program. During the same visit, the risk management company provided education on resident assessment for equipment needs to the clinical nursing staff. Immediately following the DHM, each resident was assessed to determine whether they were ambulatory or would require mobility assistance from floor-based portable sit-stand lifts or total body lifts of 204-kg or 272-kg capacity. Residents were also assessed upon admission and readmission, following significant changes in health, and in quarterly reviews. Documentation for each resident indicated the type of equipment and number of staff required for handling tasks. Equipment was then purchased to accommodate each center’s needs.
The risk management company provided initial training on equipment use, maintenance, and program policies, then made follow-up visits after 2 weeks, 4 weeks, 10 weeks, 20 weeks, 30 weeks, 40 weeks, and 50 weeks. Six follow-up visits were made in the program’s second year, and 4 were made in the third year. Hands-on training at follow-up visits varied, and included skills check-off, equipment demonstrations during peak resident transfer times, train-the-trainer sessions, resident/family council meetings, reinforcing policies and procedures, and investigating program-related injuries. Clinical staff were required to demonstrate competency in the use of handling equipment at each visit.
At the end of three years, management of the SRHP was passed from the risk management company to representatives at individual centers. Typically nurse educators were identified as SRHP trainers in the centers. No information from the corporation indicates that there was any form of standardization across centers for program maintenance or compliance.
For each center, the time period beginning on January 1, 2003, until the initial DHM was defined as pre-SRHP. The time period starting on the DHM and ending three years later was considered the first post period. The three years following program hand-off were categorized as the second post period.
2.2. Study population and data sources
Initially, all centers owned or jointly managed by the corporation from 2003 through 2006 were selected to take part in the study. Several inclusion criteria were applied: (1) The center had to be a skilled nursing facility (SNF), as opposed to an assisted-living facility. (2) The date of the initial DHM had to be recorded.(3) Data on WC claims and annual average workforce size (number of full-time equivalents (FTEs)) had to be available for the entire eight-year study period.
A total of 165 skilled nursing facilities were owned or operated by the company. WC data were not available from West Virginia, so 23 centers were excluded from analysis. Three centers closed during the study period, and three other centers had discrepancies in the number of FTEs. Thus 136 centers in 11 states met all criteria for inclusion.
Descriptive data received annually for each center from January 1, 2003, to December 31, 2010, included facility name, address, business unit number, location code, type(s) of service, workforce size (beginning January 1, 2004), and number of beds. These data were compiled and the unique business unit number and location code for each center were used to match data files by center across years.
2.3. Data management and analysis
2.3.1. Workers’ compensation data
WC claims for all employees were received from the corporation for the time period January 1, 2003 to December 31, 2010. Each claim record included the center name and number, date of incident, description of the cause, nature of the injury, body part (s) injured, and associated medical costs. Job titles of claimants were not available in all years.
WC claims within each center were designated with regard to the center’s implementation dates as pre-SRHP, first post period, or second post period. The numbers of all claims pre-SRHP, first post period, and second post period were summed by time period and center, and also aggregated corporate-wide.
The subset of claims associated with RH was identified using the ‘cause of injury’ field. Four causes were coded: “Resident Handling - Helping Into/Out of Bed,” “Resident Handling - Helping Chair/Toilet,” “Resident Handling - Into/Out of Bath,” and “Resident Handling - Not Otherwise Classified (NOC).” A post hoc quality check of WC claims by cause of injury and accident description (free text) was performed to quantify misclassified RH claims.
2.3.2. Workforce data
To determine injury rates, the number of claims was divided by the number of FTE staff members for each center and each year of the study. FTE data were available from the company beginning in 2004. FTE counts were examined and found to be relatively stable throughout the study period, so FTE data for 2004 were assumed to apply to 2003. For the year in which the SRHP began in each center, the FTE denominator was apportioned pro-rata by the numbers of days in the year before and after the DHM date.
WC claims came from all employees (e.g. clinical staff, housekeeping, maintenance, dietary, rehabilitation, recreation, administrative, social workers), whereas FTE data were provided only for clinical employees until 2007. To convert the numbers of clinical FTEs into all FTEs for the years 2004 through 2007, a correction factor was used. Head-count files for each center were reviewed to compute the ratio of clinical staff to all employees for 2008 and 2009, and these two ratios were averaged. This value was used to estimate the correction factor for computing all FTEs from clinical FTEs for 2003 through 2007 for each center.
Several centers had large differences in FTE estimates for two or more years of the study. To examine discrepancies, centers with a coefficient of variation (C.V.) greater than 10% for FTE estimates from 2004 to 2010 were identified. Annual ratios of the number of FTEs to the number of skilled beds were computed to determine whether variability in staff counts could be explained by changes in the numbers of skilled beds (e.g., if increases in beds may have resulted in hiring additional staff). Centers for which the C.V. was greater than 10%, even after accounting for the annual numbers of skilled beds, were categorized as having discrepancies in the number of FTEs and excluded from the analyses.
Using workforce rosters supplied by the corporation, mean employee age and the gender ratio of employees were calculated for each center.
2.3.3. Workers’ compensation rates
For each center, annual pre-SRHP rates of WC claims were computed using the number of claims pre-SRHP and the number of FTEs for each full or partial (pro-rated) year prior to implementation. Rates of claims in the first post and second post periods were similarly computed as the number of claims over the number of FTEs for each full or partial year in the time period. The relative risk (RR) and 95% confidence intervals for post-SRHP claims were computed separately for the first and second three-year follow-up periods, using the pre-SRHP claim rate as the reference value. RR’s were computed for claims in all SNF’s combined as well as for each center.
2.3.4. Multivariate regression modeling
The SAS Genmod procedure was used to model the natural log of the RR of WC claim rate for post-/pre-SRHP against wellness program status, unionization and average licensed practical nurse (LPN) turnover pre-SRHP. Regression coefficients and 95% confidence intervals were reported for multivariable models.
3. Results
Over the eight years of observation, the annual average total number of workers (all job titles) was 18,571 FTEs, of which 11,603 (62%) were direct care clinical staff: Registered Nurses (RNs), LPNs, Nursing Assistants (NAs), and Certified Medicine Aides (CMAs). Distributions of the workforce age, gender, ethnicity, seniority, and hours worked per week were extremely similar among the centers and consistent over time. For all jobs, the mean age was about 41 years and the population was 85% female.
3.1. All Workers’ compensation claims
A total of 22,454 claims were recorded: 7,321 pre-SRHP, 8,204 in the first post period and 6,929 in the second post period. The annualized rate per 100 FTEs was 0.1653 pre-SRHP and 0.1474 post-SRHP, for an overall RR of 0.892 (Table 1A). In the second post period the annualized claim rate dropped slightly more to 0.1420 (RR = 0.859).
Table 1.
Pooled WC claims, full-time equivalent (FTE) worker-years of follow-up, claim rates per 100 FTEs, and relative risks for (A) all employees and all claims and (B) clinical employees and resident handling-related claims: 136 skilled nursing facilities, eastern United States, 2003–2010.
| Number of claims | Claim rate | Relative risk compared to pre-SRHP | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre | First post period | Second post period | Pre | First post period | Second post period | RR first post period | Confidence Interval | RR second post period | Confidence Interval | |
| A. All-employee FTE-yrs | 44296.1 | 55666.9 | 48806.9 | 44296.1 | 55666.9 | 48806.9 | ||||
| Type of incident | ||||||||||
| All claims | 7321 | 8204 | 6929 | 16.53 | 14.74 | 14.20 | 0.892 | (0.864, 0.920) | 0.859 | (0.830, 0.887) |
| Back claims | 1921 | 1827 | 1394 | 4.34 | 3.28 | 2.86 | 0.757 | (0.709, 0.807) | 0.659 | (0.614, 0.706) |
| Falls on same level | 1070 | 1575 | 1419 | 2.42 | 2.83 | 2.91 | 1.171 | (1.083, 1.267) | 1.204 | (1.111, 1.304) |
| Material handling: manual | 652 | 586 | 353 | 1.47 | 1.05 | 0.72 | 0.715 | (0.639, 0.801) | 0.491 | (0.430, 0.560) |
| Needlestick | 297 | 374 | 325 | 0.67 | 0.67 | 0.67 | 1.002 | (0.858, 1.171) | 0.993 | (0.846, 1.166) |
| Aggression | 654 | 726 | 637 | 1.48 | 1.30 | 1.31 | 0.883 | (0.794, 0.983) | 0.884 | (0.791, 0.987) |
| Struck by/against object | 913 | 1206 | 1050 | 2.17 | 2.17 | 2.15 | 1.051 | (0.964, 1.147) | 1.044 | (0.954, 1.142) |
| B. Clinical FTE-yrs | 27428.5 | 34757.1 | 30765.9 | 27428.5 | 34757.1 | 30765.9 | ||||
| Type of incident | ||||||||||
| Resident handling (any) | 2551 | 2200 | 1765 | 9.30 | 6.33 | 5.74 | 0.681 | (0.643.0.721) | 0.617 | (0.580, 0.655) |
| NOC | 1275 | 1089 | 945 | 4.65 | 3.13 | 3.07 | 0.674 | (0.622, 0.731) | 0.661 | (0.607, 0.719) |
| Help into/out of bed | 427 | 310 | 236 | 1.56 | 0.89 | 0.77 | 0.573 | (0.493, 0.664) | 0.493 | (0.418, 0.578) |
| Help chair, toilet, etc. | 608 | 456 | 274 | 2.22 | 1.31 | 0.89 | 0.592 | (0.523, 0.669) | 0.402 | (0.347, 0.464) |
| Help into/out of bath | 11 | 24 | 29 | 0.04 | 0.07 | 0.09 | 1.722 | (0.812, 3.894) | 2.350 | (1.140, 5.214) |
| Help move in bed | 230 | 321 | 281 | 0.84 | 0.92 | 0.91 | 1.101 | (0.927, 1.310) | 1.089 | (0.912, 1.302) |
The mean of center-level RR’s for the first post period was 0.92 and the median was 0.87. There were reductions in injury rates in 95 centers (70%) (Fig. 1A). The mean RR for the second post period was 0.95 (median = 0.75), and 98 centers (72%) had claim rates lower than pre-SRHP (Fig. 1B).
Fig. 1.
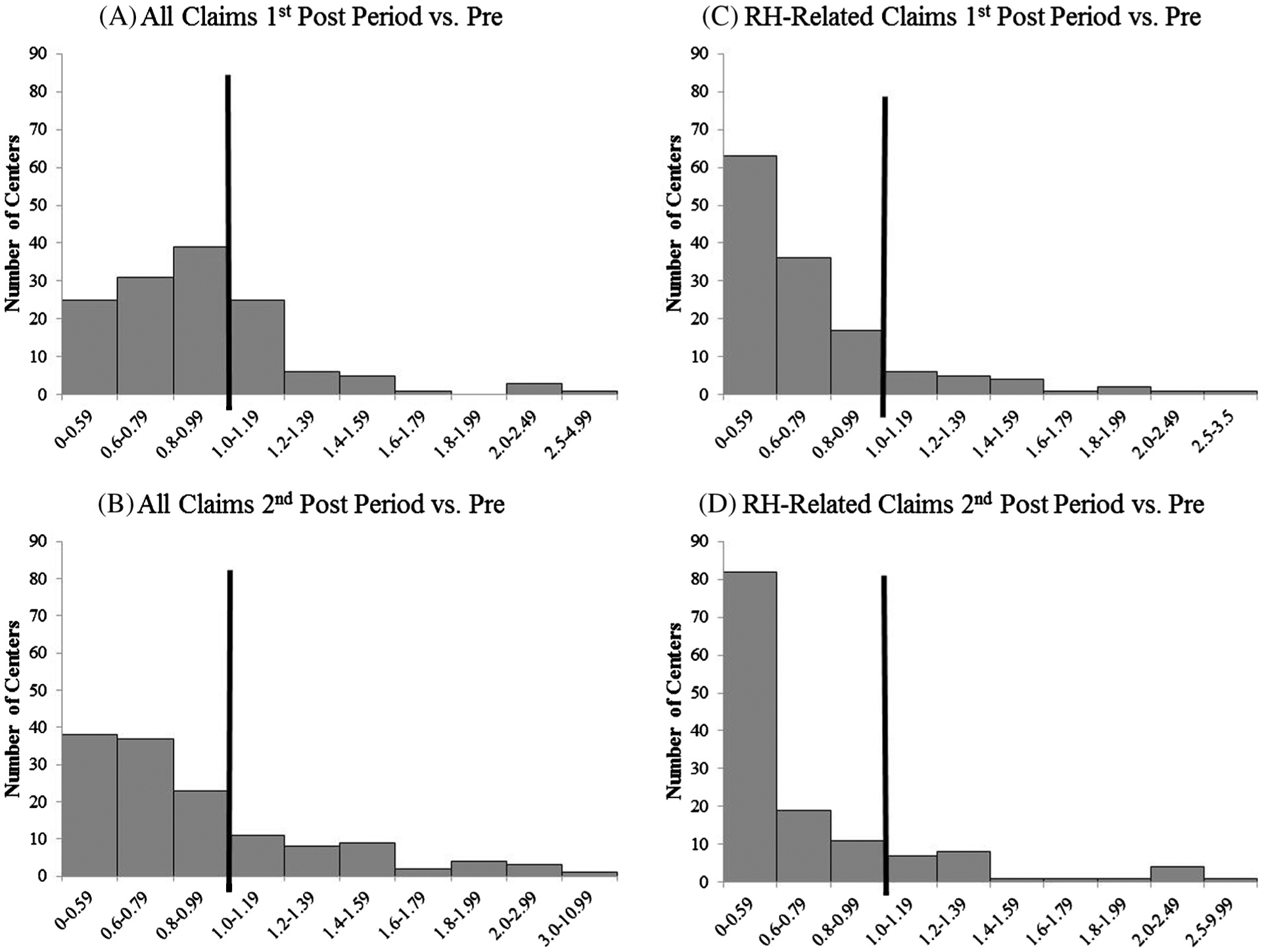
Distribution of workers’ compensation claim rates by center (n = 136): (A) all claims first post period vs. pre-SRHP; (B) all claims second post period vs. pre-SRHP; (C) resident handling-related claims first post period vs. pre-SRHP; and (D) resident handling-related claims second post period vs. pre-SRHP.
A total of 81 centers with classified wellness programs were included in a multivariate analysis of the natural log of RR for post-/pre-SRHP for WC claims. RR for post-/pre-SRHP injury rates increased as the level of wellness program development decreased, and among unionized compared to non-unionized centers (Table 2). Higher average LPN turnover pre-SRHP also increased post-/pre-SRHP RRs for WC claims (Table 2). Although the only significant relationship with post-/pre-SRHP injury rate ratios was average LPN turnover, the addition of wellness program level and unionization improved the model fit.
Table 2.
Multivariate modeling of WC claim RR (post-SRHP/Pre-SRHP): GENMOD linear regression coefficient (95% confidence interval).
| Model A | Model B | Model C | ||
|---|---|---|---|---|
| Wellness = nonea | n = 47 (58%) | 0.195 (−0.056, 0.445) | 0.218 (−0.031, 0.467) | 0.207 (−0.038, 0.451) |
| Wellness = somea | n = 25 (31%) | 0.084 (−0.188, 0.356) | 0.119 (−0.154, 0.391) | 0.090 (−0.179, 0.360) |
| Avg. LPN turnover (pre-SRHP) | x1 = 25 SD = 9.5 | 0.008 (0.002, 0.016) | 0.009 (0.001, 0.017) | |
| Unionizedb | n = 11 (14%) | 0.144 (−0.016, 0.304) | ||
| Intercept | −0.295 (−0.523, −0.067) | −0.515 (−0.827, −0.203) | −0.578 (−0.892, −0.264) |
vs. Wellness = well-developed.
vs. Non-unionized.
3.2. Resident handling claims
RH claims were more than one-third of all claims before the SRHP and only about one-fourth of the total after the program began (Table 1B). A total of 6,516 RH claims were recorded: 2,551 pre-SRHP, 2,200 in the first post period, and 1,765 in the second post period. The corporate-wide rate of RH incidents decreased in both follow-up periods, with RRs of 0.681 and 0.617.
The majority of RH claims affected the lower back (36%) and upper extremity (26%) (Table 3); distribution by body part was stable over time. Eighteen percent of the RH claims affected “other” body parts, including the neck and chest.
Table 3.
Body part(s) affected in all resident handling claims from 136 skilled nursing facilities: number and percentage of claims, 2003–2010.
| All RH claims | All RH: “Sprain or Strain” | All RH: “Pain NOC” | |
|---|---|---|---|
| Lower Back | 36.3% (n = 2367) | 42.2% (n = 2106) | 26.8% (n = 202) |
| Back, Other | 15.0% (n = 978) | 14.6% (n = 728) | 25.5% (n = 192) |
| Upper Extremity | 25.6% (n = 1667) | 25.0% (n = 1249) | 18.2% (n = 137) |
| Lower Extremity | 4.7% (n = 303) | 3.7% (n = 186) | 3.5% (n = 26) |
| Other | 18.4% (n = 1200) | 14.6% (n = 727) | 26.1% (n = 197) |
The percentage of strains and sprains increased from 67% of RH claims pre-SRHP to 80% in the first post period and 87% in the second post period. There was a drop in incidents classified as “Pain – NOC” from 21% of RH-related injuries to 9% to 1% over the three follow-up periods. The proportions of other injury types remained stable over time.
Comparing the two largest categories of incident type with regard to body part(s) affected, the back represented the largest percentage of each group. Sprain/strains involved the low back in 42% and back/other in 15% of cases; pain NOC involved the low back in 27% and back/other in 25% (Table 3). Additionally, the upper extremity was affected in 25% of sprains/strains and 18% of pain NOC incidents.
Among all centers, the mean RR of first post period to pre-SRHP for RH claims was 0.71 and the median was 0.63. There were reductions in injury rates in 116 centers (85%) (Fig. 1C). The mean RR of second post period to pre-SRHP claims related to RH was 0.72 and the median was 0.54. For this time period, claim rates were reduced in 112 centers (82%) (Fig. 1D).
3.2.1. Misclassification of resident handling claims
RH claims with cause incorrectly categorized were identified (Table 4). Across three time periods 4.2%, 2.8%, and 3.4% of all claims not coded RH were misclassified in this manner, and therefore missing from these analyses. Across the same time periods, less than 2% of a random sample of RH-related claims were misclassified by cause, most of which should have been categorized as ‘resident/employee aggression.’
Table 4.
Misclassified resident handling claims: number and percentage of each category.
| Cause of Injury | Pre | 1st post period | 2nd post period |
|---|---|---|---|
| Carpal tunnel syndrome/tenosynovitis/white finger | 24.3% (n = 9) | 17.2% (n = 5) | 0% (n = 0) |
| Caught in/under/between | 10.3% (n = 14) | 5.8% (n = 8) | 12.8% (n = 1) |
| Falls on same level | 2.5% (n = 36) | 2.6% (n = 42) | 2.2% (n = 35) |
| Lifting, lowering - manual handling | 0% (n = 0) | 28.6% (n = 2) | 3.2% (n = 4) |
| Material handling - manual | 13.3% (n = 120) | 1.9% (n = 11) | 5.1% (n = 20) |
| Material handling - mechanical | 0% (n = 0) | 16.7% (n = 1) | 60.9% (n = 14) |
| Miscellaneous - NOC | 1% (n = 2) | 0.7% (n = 1) | 1.0% (n = 1) |
| Multiple complaints | 18.4% (n = 9) | 0% (n = 0) | 0% (n = 0) |
| Pushing, pulling - manual handling | 0% (n = 0) | 0% (n = 0) | 11.8% (n = 11) |
| Repetitive motion | 5.9% (n = 1) | 4.8% (n = 1) | 13.3% (n = 4) |
| Slip or trip (not fall) | 1.4% (n = 1) | 0.6% (n = 1) | 2.0% (n = 5) |
| Struck by/against objects | 5.8% (n = 68) | 7.4% (n = 91) | 6.8% (n = 81) |
| Struck by/against other persons | 4.2% (n = 4) | 10.3% (n = 8) | 11.5% (n = 7) |
4. Discussion
4.1. Injury rates
In this eight-year study of one company’s experience with a SRHP, the rates of all WC claims and RH-related WC claims were reduced substantially within three years of beginning the program. Claims experience further improved up to six years after SRHP implementation, despite the transition in program ownership, suggesting long-term program sustainability.
Additionally, there was a drop in rates of claims related to aggression. This could potentially be at least partially attributed to the SRHP, since physical contact during stressful transferring situations was reduced.
Of the 136 centers included in these analyses, 70% experienced an overall decrease in their rate of WC claims and over 80% had lower claim rates specifically for resident handling incidents. Although mean RRs for all claims and RH-related claims were slightly higher in the second than the first follow-up period, the median RRs were lower in the later time period, when a larger number of centers had reductions in claims. The decreases in claims rates are consistent with separate observations of reduced ergonomic exposures in a subset of these centers (Kurowski et al., 2012) and resulted in an overall cost-savings for the corporation (Lahiri et al., 2013).
These results are not explained by any identifiable changes in resident or worker characteristics over the course of the study period. The general population is becoming more obese, so to the extent that this increases the physical workload of nursing home employees, an increase rather than a decrease in rates would have been expected. Gender is often a covariate of MSD rates, and in the nursing home sector exposures might be associated with employee gender. Female residents often do not allow male nursing aides to assist with bathing, dressing, or toileting tasks, which can add to female nursing aides’ workload. On the other hand, male nursing aides are often recruited by female co-workers for assistance with handling residents, especially those who are obese. In this study, women consistently represented 91% of the clinical workforce and 85% of all employees. Therefore, while gender might explain between-worker differences, it could not have any explanatory power for center-level injury rates in this study.
Training is widely reported to be an essential component for safe handling programs (Thomas and Thomas, 2014; Hodgson et al., 2013; Massachusetts Department of Public Health Occupational Health Surveillance Program, 2014). Studies have reported mixed results on the effects of training combined with handling devices on injury outcomes (Thomas and Thomas, 2014). However, for this study it is possible that in the first three years post-SRHP the frequently scheduled trainings prompted a change in safety culture helping to increase employee awareness of lifting policies and procedures for proper use of equipment. Since we do not have any information about how individual centers ran their SRHPs during the extended follow-up period (years 4–6), it is difficult to draw conclusions about the effect training may have had on program sustainability.
Results from the regression analysis helped in understanding some factors explaining RR for post-vs. pre-SRHP injury rates. The RR was higher for centers with less-developed wellness programs. Regardless of which covariates were included in the models, centers with no wellness programs tended to have RR’s around 0.2 and centers with somewhat-developed wellness programs had RR’s of around 0.1 (well-developed wellness programs = reference group), indicating a dose-response relationship. Perhaps employees at centers with better general health and wellness awareness also more strictly adhered to SRHP policies and procedures.
There was also a higher RR for unionized centers. It is unclear why unionization might raise the risk of post-vs. pre-SRHP injury rates. It is possible that employees at unionized centers may be more aware of procedures for reporting injuries, and may have more encouragement to report. It is also possible that unionization occurred in response to injury rates and workplace safety issues.
Higher average LPN turnover pre-SRHP also affected the RR for post-vs. pre-SRHP injury rates. Perhaps the instability in this job title affected implementation during the pre-period, resulting in less effective implementation in the post-SRHP period.
4.2. Study strengths and weaknesses
The data in this study were obtained from 136 nursing homes in 11 states and covered an eight-year time period, which allowed for a substantial observation period both before and after SRHP implementation in each center. The large study population, long observation period, and highly consistent program design and implementation across so many workplaces provide statistical stability and generalizability and strengthen the likelihood that the results are due to true injury reduction rather than short-term reporting changes or other artifacts.
There are some potential limitations to this study. Underreporting of occupational injuries has been recognized as a problem for accurately estimating WC rates (Azaroff et al., 2002; Siddharthan et al., 2006; Fan et al., 2006). It is possible there were unreported injuries in this population, although this issue would presumably have been present before the SRHP as well, thus diluting the actual rates of injuries at all time periods. However, we cannot rule out that reporting might have been further depressed by management or coworker discouragement of claim filing after the program began. This could have created an artificially lower rate of WC claims, especially in RH incidents.
This study did not have a control group, since all centers received the same intervention. In general, work disability rates (total recordable cases) have been decreasing nation-wide (Massachusetts Department of Public Health Occupational Health Surveillance Program, 2014), so the lack of a concurrent comparison group makes it more difficult to determine whether our results can be attributed to the SRHP. However, one set of internal reference values is provided by claims for other types of injuries not likely affected by the SRHP. Needlesticks and struck by/against injuries remained steady across the eight-year time period. In contrast, the major reductions were seen in manual handling claims, and resident handling in particular.
Our analysis of all WC claims necessitated the assumption that claims unrelated to RH either remained constant or increased over time, and therefore that any reductions in injury rates could be attributed to the SRHP, either directly or indirectly. As noted above, this assumption seems to be justified. The justification for examining all claims, in addition to RH-related claims, is that there might be relevant incidents not identified as RH in the “cause of injury” field. For example, a worker might trip over or strike a body part against the handling equipment. The total number of claims actually increased in the first follow-up period, primarily due to more falls on the same level; however, a review of free text fields where available did not support the interpretation that these incidents involved the RH equipment.
Because job title was not included in the WC claim report, there was no way to distinguish between claims filed by clinical nursing staff and those from other employees, such as housekeeping and maintenance staff. RH claims rates were based on the numbers of clinical FTEs for each time period. It is possible, though unlikely, that some of the claims were to non-direct care employees in these analyses. If this occurred, the denominators of workers at risk would have been underestimated so the rates would have been overestimated, but probably with a very small effect on the total numbers. Any such errors would also have been equally likely both before and after the SRHP.
In the process of a separate analysis of WC claims in this same population, we identified RH claims that had been incorrectly categorized as well as a smaller percentage of claims that had been misclassified as RH-related. However, if we had the ability to recode misclassification in both directions for this dataset, the ‘pre’ rates of WC claims would have been even higher.
4.3. Conclusions and recommendations
The elderly population in the U.S. will continue to increase, creating a growing need for long-term care services. Nursing home workers will likely continue to face high injury risks. Thus it is very important to identify and disseminate effective ways to reduce those risks.
Traditionally, nursing staff have been trained in manual patient handling techniques. However, these techniques have not been effective in decreasing work-related injuries (Bureau of Labor Statistics [BLS], 2012). Back belts have also been used, but again this strategy lacks evidence to support effectiveness in reducing work-related MSDs (Nelson et al., 2003; Nelson and Baptiste, 2004; Ergonomics Technical Advisory Group, 2001). Meanwhile, evidence continues to accumulate to show that the use of mechanical lifting equipment has resulted in lower injury rates and insurance premiums, as well as fewer lost workdays and musculoskeletal symptoms.
In 2004, OSHA released ergonomics guidelines for nursing homes to reduce the number and severity of work-related MSDs (Occupational Safety and Health Administration (OSHA), 2004). One specific recommendation is that manual lifting of residents should be minimized in all cases and eliminated where feasible. In 2004, the American Nurses Association (ANA) developed a campaign called “Handle with Care,” which supports safe practices for patient handling. This campaign is currently working on a profession-wide effort to prevent MSDs through increased education and training, and increased use of patient-handling equipment (de Castro, 2004).
Nevertheless, some workers are still not using lifting equipment all of the time (Nelson et al., 2006). In 1993, Fragala discussed barriers to using lifting equipment such as extra time required, difficulty using devices, and residents’ resistance to devices (Fragala, 1993). Other obstacles include lack of training and respondents who do not perceive a need to use equipment (Evanoff et al., 2003); device inaccessibility (Koppelaar et al., 2011; Kurowski et al., 2016); inconsistent management support of programs (Koppelaar et al., 2011); and staffing issues and work environment culture (Schoenfisch et al., 2011). More research should be done to understand and address these barriers.
Nursing aides may struggle with maneuvering lifting devices into and around rooms due to space constraints. This can make RH tasks more difficult if workers have to assume awkward postures in order to gain access to residents and equipment. Many nursing homes face issues regarding size and layout, so other types of lifting equipment, such as ceiling-mounted lifts could be investigated to determine differences in cost and feasibility. Nelson reported reduced internal loading on the body when ceiling lifts were used for transferring patients compared to mobile handling equipment (Nelson et al., 2003). Although many research studies show the effectiveness of no-lift policies in healthcare, the concept of introducing mechanical lifting equipment has been slow to be accepted in the United States. Many challenges exist including providing proper equipment in every facility, getting staff to change manual patient-handling practices, and providing management with proper training so they can provide support to the nursing staff.
Overall, the findings of this study support that reduction of injuries among nursing home staff is plausibly attributed to the introduction of sufficient mechanical lifting equipment for all residents who need it, along with training in its use, regular battery charging, and other program features that are essential for effectiveness. Since the majority of WC claims unrelated to RH remained constant over time, we believe that the implementation of the SRHP has had a substantial impact on the WC claim rates in the participating nursing homes. The maintenance of lower claim rates for a six-year period after the program began is very encouraging with regard to long-term sustainability. At the same time, RH claims were not eliminated, so continued efforts are needed to identify persisting reasons for injury while resident handling and how to reduce those injuries.
Acknowledgements
We thank Donna LaBombard, Annmarie Reiner, and Suzanne Nobrega for assistance in data acquisition. This study was supported by Grant Number U19-OH008857 from the U.S. National Institute of Occupational Safety and Health (NIOSH). The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official views of NIOSH.
References
- Azaroff LS, Levenstein C, Wegman DH, 2002. Occupational injury and illness surveillance: conceptual filters explain underreporting. Am. J. Public Health 92 (9), 1421–1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black TR, Shah SM, Busch AJ, Metcalfe J, Lim HJ, 2011. Effect of transfer, lifting, and repositioning (TLR) injury prevention program on musculoskeletal injury among direct care workers. J. Occupational Environ. Hygiene 8 (4), 226–235. [DOI] [PubMed] [Google Scholar]
- Bureau of Labor Statistics [BLS], 2012. U.S. Dept. of Labor, Workplace injuries and illnesses – 2010. Retrieved September 4, 2012 from <http://www.bls.gov/news.release/archives/osh_10202011.pdf>. [Google Scholar]
- Centers for Disease Control and Prevention (CDC), 2007. National Center for Health Statistics. Health, United States. Chartbook on Trends in the Health of Americans <http://www.cdc.gov/nchs/data/hus/hus07.pdf#17> (accessed April 17, 2008). [Google Scholar]
- Collins JW, Wolf L, Bell J, Evanoff B, 2004. An evaluation of a “Best practices” musculoskeletal injury prevention program in nursing homes. Injury Prevention 10, 204–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins JW, Nelson A, Sublet V, 2006. Safe Lifting and Movement of Nursing Home Residents, DHHS (NIOSH) Publication No. 2006–117 National Institute for Occupational Safety and Health, Cincinnati, OH. [Google Scholar]
- de Castro AB, 2004. Handle With Care®: The American Nurses Association’s Campaign to Address Work-Related Musculoskeletal Disorders. Online J. Issues Nursing 9 (3) <www.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Volume92004/No3Sept04/HandleWithCare.aspx>. [PubMed] [Google Scholar]
- Elford W, Straker L, Strauss G, 2000. Patient handling with and without slings: an analysis of the risk of injury to the lumbar spine. Appl. Ergonomics 31, 185–200. [DOI] [PubMed] [Google Scholar]
- Engkvist IL, 2006. Evaluation of an intervention comprising a No-Lifting policy in Australian hospitals. Appl. Ergonomics 37, 141–148. [DOI] [PubMed] [Google Scholar]
- Engkvist IL, Hagberg M, Hjelm EW, Menckel E, Ekenvall L, 1998. The accident process preceding overexertion back injuries in nursing personnel. Scand. J. Work Environ. Health 24 (5), 367–375. [DOI] [PubMed] [Google Scholar]
- Engst C, Chokkar R, Miller A, Tate RB, Yassi A, 2005. Effectiveness of overhead lifting devices in reducing the risk of injury to care staff in extended care facilities. Ergonomics 48 (2), 187–199. [DOI] [PubMed] [Google Scholar]
- Ergonomics Technical Advisory Group, 2001. Patient Care Ergonomics Resource Guide: Safe Patient Handling and Movement. Patient Safety Center of Inquiry, Veterans Health Administration and Department of Defense, Tampa, FL: <http://www.visn8.med.va.gov/patientsafetycenter> (retrieved August 10, 2010 from). [Google Scholar]
- Evanoff B, Wolf L, Aton E, Canos J, Collins J, 2003. Reduction in injury rates in nursing personnel through introduction of mechanical lifts in the workplace. Am. J. Ind. Med 44, 451–457. [DOI] [PubMed] [Google Scholar]
- Fan ZJ, Bonauto DK, Foley MP, Silverstein BA, 2006. Underreporting of work-related injury or illness to workers’ compensation: individual and industry factors. J Occupational Environ. Med 48 (9), 914–922. [DOI] [PubMed] [Google Scholar]
- Fragala G, 1993. Injuries cut with lift use in ergonomics demonstration project. Provider 19 (10), 39–40. [PubMed] [Google Scholar]
- Garg A, 1999. Long-Term Effectiveness of a “zero-lift” Program in Seven Nursing Homes and One Hospital. U.S. Department of Health and Human Services, National Institute for Occupational Safety and Health, Contract Report No. U60/CCU512089–02. [Google Scholar]
- Garg A, Kapellusch JM, 2012. Long-term efficacy of an ergonomics program that includes patient-handling devices on reducing musculoskeletal injuries to nursing personnel. Hum. Factors 54 (4), 608–625. [DOI] [PubMed] [Google Scholar]
- Hodgson MJ, Matz MW, Nelson A, 2013. Patient handling in the Veterans Health Administration: facilitating change in the health care industry. J. Occup. Environ. Med 55 (10), 1230–1237. [DOI] [PubMed] [Google Scholar]
- Hunter B, Branson M, Davenport D, 2010. Saving costs, saving health care providers’ backs, and creating a safe patient environment. Nursing Economic$ 28 (2), 130–134. [PubMed] [Google Scholar]
- Koppelaar E, Knibbe JJ, Miedema HS, Burdorf A, 2011. Individual and organizational determinants of use of ergonomic devices in healthcare. Occup. Environ. Med 68 (9), 659–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurowski A, Boyer J, Fulmer S, Gore R, Punnett L, 2012. Changes in ergonomic exposures of nursing assistants after the introduction of a safe resident handling program in nursing homes. Int. J. Ind. Ergon 42, 525–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurowski A, Gore R, Mpolla N, Punnett L, 2016. Use of resident handling equipment by nursing aides in long-term care: associations with work organziation and individual level characteristics. Am. J. SPHM 6 (1), 16–24. [PMC free article] [PubMed] [Google Scholar]
- Lahiri S, Latif S, Punnett L ProCare Research Team, 2013. An economic analysis of a safe resident handling program in nursing homes. Am. J. Ind. Med 56, 469–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lapane KL, Resnik L, 2006. Weighing the relevant issues: obesity in nursing homes. J. Aging Soc. Policy 18 (2), 1–9. [DOI] [PubMed] [Google Scholar]
- Li J, Wolf L, Evanoff B, 2004. Use of mechanical patient lifts decreased musculoskeletal symptoms and injuries among health care workers. Injury Prevention 10 (4), 212–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipscomb HJ, Schoenfisch AL, Myers DJ, Pompeii LA, Dement JM, 2012. Evaluation of direct workers’ compensation costs for musculoskeletal injuries surrounding interventions to reduce patient lifting. Occup. Environ. Med 69 (5), 367–372. [DOI] [PubMed] [Google Scholar]
- Massachusetts Department of Public Health Occupational Health Surveillance Program, 2014. Moving into the Future: Promoting Safe Patient Handling for Worker and Patient Safety in Massachusetts Hospitals. Report of the Massachusetts Hospital Ergonomics Task Force. [Google Scholar]
- Nelson A, Baptiste A, 2004. Evidence-based practices for safe patient handling and movement. Online J. Issues Nursing 9 (3) <http://www.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Volume92004/No3Sept04/EvidenceBasedPractices.aspx>. [PubMed] [Google Scholar]
- Nelson A, Lloyd J, Menzel N, Gross C, 2003. Preventing nurses’ back injuries: redesigning patient handling tasks. Am. Assoc. Occupational Health Nurses J 51 (3), 126–134. [PubMed] [Google Scholar]
- Nelson A, Matz M, Chen F, Siddharthan K, Lloyd J, Fragala G, 2006. Development and evaluation of a multifaceted ergonomics program to prevent injuries associated with patient handling tasks. Int. J. Nurs. Stud 43 (6), 717–733. [DOI] [PubMed] [Google Scholar]
- Occupational Safety and Health Administration (OSHA), 2004. Ergonomics: Guidelines for nursing Homes Retrieved January 15, 2011 from <www.osha.gov/ergonomics/guidelines/nursinghome/final_nh_guidelines.pdf>.
- Park RM, Bushnell PT, Bailer AJ, Collins JW, Stayner LT, 2009. Impact of publicly sponsored interventions on musculoskeletal injury claims in nursing homes. Am. J. Ind. Med 52 (9), 683–697. [DOI] [PubMed] [Google Scholar]
- Restrepo TE, Schmid FA, Gucer PW, Shuford HL, Shyong CJ, McDiarmid MA, 2013. Safe lifting programs at long-term care facilities and their impact on workers’ compensation costs. J. Occup. Environ. Med 55 (1), 27–35. [DOI] [PubMed] [Google Scholar]
- Schoenfisch AL, Myers DJ, Pompeii LA, Lipscpmb HJ, 2011. Implementation and adoption of mechanical patient lift equipment in the hospital setting: the importance of organizational and cultural factors. Am. J. Ind. Med 54, 946–954. [DOI] [PubMed] [Google Scholar]
- Schoenfisch AL, Lipscpmb HJ, Pompeii LA, Myers DJ, Dement JM, 2013. Musculoskeletal injuries among hospital patient care staff before and after implementation of patient lift and transfer equipment. Scand. J. Work Environ. Health 39 (1), 27–36. [DOI] [PubMed] [Google Scholar]
- Siddharthan K, Hodgson M, Rosenberg D, Haiduven D, Nelson A, 2006. Underreporting of work-related musculoskeletal disorders in the Veterans Administration. Int. J. Health Care Qual. Assurance Incorporating Leadership Health Services 19 (6–7), 463–476. [DOI] [PubMed] [Google Scholar]
- Smedley J, Egger P, Cooper C, Coggon D, 1997. Prospective cohort study of predictors of incident low back pain in nurses. Br. Med. J 314, 1225–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas DR, Thomas YLN, 2014. Interventions to reduce injuries when transferring patients: a critical appraisal of reviews and a realist synthesis. Int. J. Nurs. Stud 51, 1381–1394. [DOI] [PubMed] [Google Scholar]
- Trinkoff AM, Lipscomb JA, Geiger-Brown J, Storr CL, Brady BA, 2003. Perceived physical demands and reported musculoskeletal problems in registered nurses. Am. J. Prev. Med 24 (3), 270–275. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Labor, 2015a. Bureau of Labor Statistics [BLS]. U.S. Dept. of Labor. Incidence Rates of Nonfatal Occupational Injuries and Illnesses by Case type and Ownership, Selected Industries, 2014 Retrieved October 14, 2016 from <http://www.bls.gov/news.release/osh.t01.htm>. [Google Scholar]
- U.S. Department of Labor, 2015. Bureau of Labor Statistics [BLS]. U.S. Dept. of Labor, Nonfatal Occupational Injuries and Illnesses Requiring Days Away from Work, 2014 Retrieved October 14, 2016 from <http://www.bls.gov/news.release/pdf/osh2.pdf>. [Google Scholar]
- Zhuang Z, Stobbe TJ, Hsiao H, Collins JW, Hobbs GR, 1999. Biomechanical evaluation of assistive devices for transferring residents. Appl. Ergonomics 30, 285–294. [DOI] [PubMed] [Google Scholar]


