Abstract
Background
Internet cognitive behavioural therapy (iCBT) for health anxiety has demonstrated efficacy but has not been evaluated during the COVID-19 pandemic. This study presents the first evaluation of the uptake and outcomes of iCBT for health anxiety during the COVID-19 pandemic.
Methods
THIS WAY UP is an Australian digital mental health service which delivers iCBT interventions to community members. We compared the uptake of THIS WAY UP’s iCBT course for health anxiety in an Australian adult sample who started the course before the pandemic (12th September 2019–11 th March 2020) to during the pandemic (12th March to 11th June 2020). The course was accessible to Australian adults over 18 years old, with no inclusion criteria. Outcomes included course registrations and commencements, lesson and course completion, and self-reported health anxiety (Short Health Anxiety Inventory), depression (Patient Health Questionnaire 9-item) and distress (Kessler-10).
Results
From March to June 2020, we observed significant increases in course registrations (N = 238 vs N = 1057); and course commencements (N = 126 vs. N = 778). Large, significant improvements in health anxiety (g = 0.89), and distress (K10: g = 0.91), and medium improvements in depression (g = 0.55) were found. Course completion during COVID was 30.5%.
Conclusions
iCBT improved health anxiety during the COVID-19 pandemic, and provides scalable intervention that can address increased demands for mental health services in the community.
Keywords: iCBT, Health anxiety, Internet intervention, Effectiveness, COVID-19
1. Introduction
The COVID-19 pandemic is one of the largest global health crises in living history. It has led to mass lockdowns, strict social distancing, travel restrictions, border closures, job losses and economic uncertainty. While these factors have increased fear, anxiety, and stress internationally (Wu et al., 2020), prolonged and repeated exposure to health-threatening information about COVID-19 has caused many to fear contracting and spreading COVID-19 and worry about their health and the health of loved ones (Asmundson and Taylor, 2020aaa, Newby et al., 2020). Frequent exposure to conversations, sensationalised mass media coverage, social media posts, and public health campaigns about the pandemic and personal hygiene practices may trigger and exacerbate health anxiety.
Prior to the pandemic, health anxiety was relatively common, affecting approximately 5.7% of the population during their lifetime (Sunderland, Newby, & Andrews, 2012), with estimates ranging from 2% to 13% (Weck, Richtberg, & Neng, 2014). Health anxiety is characterised by excessive and persistent worries about having or developing illnesses, the tendency to misinterpret benign bodily sensations as a sign of illness, body hypervigilance, and maladaptive behaviours including excessive checking, reassurance-seeking, internet searching about symptoms and illness, and avoidance of health-related stimuli (American Psychiatric Association, 2013). In some circumstances, anxiety about health, and particularly anxiety about COVID-19, can be helpful, as it motivates health protective behaviours such as hand-washing, mask wearing, uptake of vaccinations, and adherence to social distancing and self-isolation rules (Asmundson & Taylor, 2020b). However, when health anxiety becomes excessive, persistent, and out of proportion to the health threat, it can be problematic and debilitating. Excessive health anxiety causes distress and impairment in work, relationships, social roles, poor quality of life, and poor mental health and physical health (Bobevski et al., 2016, Sunderland et al., 2012). It also affects health care utilisation, leading to both over- and under-use of health care services. In most cases, people with health anxiety use more health services than people without health anxiety and those with well-defined medical conditions, including greater tests and investigations, primary care and specialist visits, emergency attendance and ambulance call-outs (e.g., Fink, Ørnbøl, & Christensen, 2010). However, health anxiety can also lead some individuals to avoid health care altogether due to the overwhelming fear of being diagnosed with or contracting illnesses (American Psychiatric Association, 2013).
Recent research has begun to uncover the extent of COVID-19 fear and general health anxiety during this pandemic (McKay et al., 2020, Taylor et al., 2020). Studies have shown that between one third to one half of survey respondents fear contracting COVID-19, one half are afraid that friends, family and loved ones will contract COVID-19, and one quarter report elevated health anxiety as a result of the pandemic (Newby & O’Moore, 2020). Some preliminary research suggests that women, people with pre-existing mental health conditions and chronic diseases, and those with a poorer health status are vulnerable to higher anxiety during COVID-19, and higher anxiety about health in general is associated with greater specific fears of COVID-19 (Jungmann and Witthöft, 2020, McKay et al., 2020, Mertens et al., 2020). Given the significant health threat posed by COVID-19, these fears and anxieties are likely to be adaptive, and proportionate to the threat posed. However, for some individuals, their anxiety may become so distressing, all-consuming, and debilitating that they might benefit from additional support, coping strategies, and treatment to help them better manage their anxiety. Evidence-based treatment strategies, such as those from cognitive behavioural therapy are potentially beneficial for those experiencing heightened and disabling health anxiety, even when it is not certain whether their anxiety is excessive or disproportionate to the threat of illness.
To our knowledge, no research has evaluated the uptake or outcomes of treatments for health anxiety during the COVID-19 pandemic. Digital interventions such as internet-delivered cognitive behavioural therapy (iCBT) have been shown to be effective in treating health anxiety prior to the pandemic, including in patients with DSM-IV hypochondriasis, and DSM-5 illness anxiety disorder and somatic symptom disorder. These randomised controlled trials involving more than 375 participants in total have shown that iCBT for health anxiety leads to large and clinically significant improvements in health anxiety (within-group effect sizes > 1.30), as well as comorbid anxiety and depression, psychological distress and quality of life in treatment-seeking samples, and outperforms a range of control groups, including waitlist, behavioural stress management, and psychoeducation controls (Hedman et al., 2014, Hedman et al., 2016, Newby et al., 2016). Furthermore, a recent RCT including 204 participants with illness anxiety disorder or somatic symptom disorder showed that iCBT for health anxiety was non-inferior to face-to-face CBT in reducing health anxiety symptom severity up to 12 months following treatment, but had lower societal costs to deliver it (Axelsson et al., 2020). iCBT also significantly improves health anxiety symptoms in unguided (i.e., self-help) and clinician-guided models of care in routine care settings, although treatment adherence and completion is typically lower in community and routine care settings compared to clinical trial settings (33% for self-guided iCBT, and 46% for guided iCBT) adherence in community/routine care (Newby, Haskelberg et al., 2020) vs. 60% under RCT conditions (Newby et al., 2018). Nevertheless, iCBT for health anxiety presents a potentially accessible, scalable treatment option. It allows individuals with health anxiety to access help without attending in-person appointments which may have been limited during lockdowns and travel restrictions, or too anxiety-inducing due to fears of contracting illnesses.
This study examined the uptake and outcomes of the THIS WAY UP iCBT for Health Anxiety course in an open (uncontrolled) evaluation during the early COVID-19 pandemic period in Australia (12th March–11th June 2020). Given the specific concerns about health-related anxiety in the COVID-19 context, we aimed to examine the clinical and demographic characteristics of this COVID-19 sample in terms of health anxiety symptom severity, depression symptom severity and psychological distress, and compare the program uptake and user characteristics in the six months prior to the spread of COVID-19 in Australia. The outcomes of the THIS WAY UP Health Anxiety program in the general community prior to COVID-19 have been previously demonstrated in an uncontrolled study of adults who underwent clinician-guided and unguided versions of the iCBT program (Newby et al., 2018). Specifically, we found large improvements in health anxiety severity, depression, and quality of life from pre to post-treatment in both clinician-guided and unguided groups (Newby, Haskelberg et al., 2020). Based on reports from online mental health providers and digital clinics showing substantial increases in service utilisation for general anxiety and depression during the COVID-19 pandemic (Mahoney, Li, Haskelberg, Millard, & Newby, 2021, Staples et al., 2020, Titov et al., 2020) and increases in the uptake of the THIS WAY UP OCD and Mindfulness courses (Li, Chen et al., 2020), we expected similar increases in uptake of the Health Anxiety Course during the COVID period. Consistent with previous studies, we hypothesised that the iCBT for health anxiety course would be associated with large effect size improvements in health anxiety and depression symptom severity with adherence rates of 30–45% during the COVID-19 period.
2. Methods
2.1. Setting
THIS WAY UP is a not-for-profit service providing iCBT programs for the treatment of depression, anxiety and related disorders in adults. The service is a joint initiative of St Vincent’s Hospital (Sydney, Australia) and the University of New South Wales (see thiswayup.org.au). The service offers 18 diagnosis-specific and transdiagnostic online courses for depression and anxiety disorders in clinician-guided or unguided/self-guided formats. Some examples include courses for health anxiety, generalised anxiety, panic disorder, mixed depression and anxiety, and obsessive compulsive disorder. There are multiple potential referral pathways to accessing the program. End-users might learn about the program from their health professional, such as a general practitioner, via social media or media promotions, insurance providers, or via word of mouth. The iCBT course for health anxiety was originally developed for people experiencing excessive and debilitating anxiety about health, such as those meeting diagnostic criteria for DSM-5 Illness Anxiety Disorder (formerly DSM-IV hypochondriasis). However, any adult 18 years or over could do the course if they wanted to. There were no specific eligibility criteria to apply.
Australian residents can complete THIS WAY UP programs either self-guided or guided by the user’s clinician (typically, the users’ general practitioner, psychologist, or other health professional). Individuals residing outside of Australia can complete THIS WAY UP programs in the clinician-guided format only. Current analyses were restricted to Australian users. THIS WAY UP programs usually cost $AUD59 to access, but in response to the COVID-19 pandemic and with the support of the St Vincent’s Hospital’s Inclusive Health Foundation, all THIS WAY UP courses were free to access between 25th March 2020 and 30th June 2020. After this period, free access continued for clinician-guided service users and remained free at time of this manuscript submission. The course fee for self-guided users was re-introduced on July 1st 2020. The service was promoted in a series of short national media engagements in April 2020.
2.2. Participants
Overall, a sample of 1295 individuals registered for the THIS WAY UP health anxiety course between 12th September 2019 and 11th June 2020. To register, individuals needed to be aged over 18 years. We split these groups into a pre-COVID sample (n = 238; 12th September 2019–11 th March 2020) and a during-COVID sample (n = 1057, 12th March to 11th June 2020). The cut-off date was chosen as the 11th March, which was the date the World Health Organisation confirmed the COVID-19 pandemic (with the 12th March being the first full day following this confirmation within the Australian time zone where the sample was recruited). Within a fortnight of this date, Australia had implemented severe containment measures including border closures, shutdown of non-essential services, and social distancing restrictions.
Of these 1295 registrants, a subset of individuals (126 in the pre-COVID sample and 778 in the during COVID sample) commenced their iCBT course and completed measures of clinical and demographic characteristics. The sample characteristics herein and the current estimates of iCBT outcomes are based on this sub-sample of course commencers as these individuals completed baseline study measures.
To access the health anxiety course, participants created an account at THIS WAY UP and provided their first name, age, gender, email address and postcode (optional). On average, participants were in the mid- to late 30s (M = 37.83, SD = 12.64, range = 18–81); the majority were female (n = 607, 67.1%) and engaged in the health anxiety course in the self-guided format (n = 804, 88.9%). We examined whether participants were living in major cities, or regional and rural Australia by their postcode and the Australian Statistical Geography Standards (Australian Bureau of Statistics, 2016). Of those who provided their postcode (70.9% from total commencers), most participants lived in major cities (n = 464/641, 72.4%) (see Table 1).
Table 1.
Participant demographic and baseline clinical characteristics in the pre- and during-COVID period.
| Pre-COVID (N = 126) |
During-COVID (N = 778) |
Pre- vs during-COVID comparison |
|||
|---|---|---|---|---|---|
| M (range) | SD | M (range) | SD | Statistic | |
| Age | 38.21 (18–74) | 12.72 | 37.76 (18–81) | 12.64 | t (902) = 0.36, p = .72 |
| SHAI | 34.69 (7–54) | 9.65 | 30.76 (0–54) | 11.13 | t (902) = 3.74, p < .001 |
| PHQ-9 | 9.41 (0–24) | 6.09 | 9.25 (0–27) | 5.95 | t (902) = 0.29, p = .78 |
| K-10 | 25.75 (10–42) | 7.25 | 25.24 (10–50) | 7.85 | t (902) = 0.68, p = .50 |
| n | % | n | % | Statistic | |
| Gender | |||||
| Female | 81 | 64.29 | 526 | 67.61 | χ2(2) = 0.56, p = .76 |
| Male | 39 | 30.95 | 220 | 28.27 | |
| Unspecified | 6 | 4.76 | 32 | 4.11 | |
| Rural statusa | |||||
| Major cities | 71 | 70.30 | 393 | 72.78 | χ2(1) = 0.26, p = .61 |
| Regional or remote | 30 | 29.70 | 147 | 27.22 | |
| Format | |||||
| Self-guided | 96 | 76.19 | 708 | 91.00 | χ2(1) = 24.18, p < .001 |
| Clinician-guided | 30 | 23.81 | 70 | 9.00 | |
| Clinically significant symptom severity | |||||
| SHAI > 18 | |||||
| Yes | 121 | 96.03 | 681 | 87.53 | χ2(1) = 7.83, p = .005 |
| No | 5 | 3.97 | 97 | 12.47 | |
| PHQ-9 > 10 | |||||
| Yes | 54 | 42.86 | 325 | 41.77 | χ2(1) = 0.05, p = .82 |
| No | 72 | 57.14 | 453 | 58.23 | |
| K-10 > 20 | |||||
| Yes | 98 | 77.78 | 591 | 75.96 | χ2(1) = 0.20, p = .66 |
| No | 28 | 22.22 | 187 | 24.04 | |
Note. M = Mean; SD = Standard Deviation; SHAI = Short Health Anxiety Inventory; PHQ-9 = Patient Health Questionnaire-9; K-10 = Kessler-10 Psychological Distress Scale; a=sample size for rural status based on optional provision of postcodes (npre-covid = 101, nduring-covid = 540)
This study was conducted as part of the routine quality assurance activities of THIS WAY UP and all self-report measures examined were required for the safe conduct of the health anxiety course. By agreeing to THIS WAY UP’s Terms of Use and Privacy Policy, all participants provided electronic informed consent that their pooled de-identified data could be collected, collated, analysed and published for quality assurance and research purposes (St Vincent’s Hospital Human Research Ethics Committee, 2020/ETH03027).
2.3. Intervention
The Health Anxiety program consists of six comic-based online lessons following the story of a fictional character who experiences health anxiety, and learns CBT skills with the help of a clinician (e.g., goal setting, thought monitoring and challenging, behavioural experiments, graded exposure) to manage their health anxiety. Each lesson teaches CBT skills, such as step-by-step guides on thought monitoring (lesson 3) and thought challenging techniques (lesson 4). After each lesson, the participant downloads the lesson homework which includes practical exercises, such as cognitive restructuring or graded exposure to complete prior to accessing the next lesson. CBT skills covered in the program include psychoeducation about the nature and maintenance of health anxiety; strategies to reduce worry, attentional hypervigilance and tolerate uncertainty; cognitive restructuring to shift unhelpful thoughts; behavioural experiments and graded exposure to reduce avoidance and maladaptive safety behaviours like excessive checking and reassurance-seeking; and relapse prevention (see Supplementary Table S1 and Newby et al., 2018 for more detail). Evidence supporting the efficacy and effectiveness of the course has been provided in one RCT of 86 participants with illness anxiety disorder or somatic symptom disorder (Newby et al., 2018) and one open trial involving 391 treatment-seeking adults from the general Australian community (Newby et al., 2018, Newby et al., 2020).
There is a five-day wait-period between lessons two to six to give participants time to practise the skills covered in the lessons. All participants are sent lesson reminder emails and some participants receive SMS reminders (if they opt in). Participants are given 90 days to complete the program and if completed within this timeframe, they gain an additional 12 months access to the program material. Participants are emailed referrals to crisis services if they score highly on self-reported measures of distress (Kessler-10 > 30; Kessler et al., 2002) and/or suicidal ideation (Patient Health Questionnaire 9-item, Q9 ≥ 1) (Kroenke, Spitzer, & Williams, 2001). Clinicians who supervise participants completing the program in a clinician-guided format also receive automated emails notifying them of their patient/client’s high score. Health professionals who ‘prescribed’ the iCBT course retained clinical responsibility for their patients for the duration of the program. Patients and their supervising clinicians were advised that THIS WAY UP courses are not recommended as stand-alone interventions for people who (1) were being treated with benzodiazepines or atypical anti-psychotics; (2) had an alcohol or substance use disorder; (3) had schizophrenia or bipolar affective disorder; or (4) were actively suicidal. The course information page encouraged these individuals to seek further clinical advice before enrolling in a self-guided online program. These recommendations were given because the efficacy of the course in people with these characteristics is unknown as they were excluded from the clinical trial evaluating the program. However, adhering to these recommendations was at the discretion of the service user and clinician and were not exclusion criteria.
2.4. Outcomes
The Short Health Anxiety Inventory (SHAI; Salkovskis, Rimes, Warwick, & Clark, 2002 ) is a validated 18-item self-report measure of health anxiety over the past week. Each item describes four health-related statements scored from 0 to 3 where participants are asked to select the statement most relevant to them (e.g., 0 = As a rule I am not afraid that I have a serious illness; 1 = I am sometimes afraid that I have a serious illness; 2 = I am often afraid that I have a serious illness; 3 = I am always afraid that I have a serious illness). Evidence supporting the internal consistency (α = 0.74–0.96), test-retest reliability (r = 0.87 over one week), and construct validity (including treatment sensitivity in both clinical and community samples) has been provided (Abramowitz et al., 2007, Alberts et al., 2013, Olatunji et al., 2011). A cut-off score of ≥18 was used as an indicator of clinically significant health anxiety (Alberts et al., 2013). Participants completed the SHAI before lessons 1, 4 and 6. Pre-treatment internal reliability in this study was α = 0.94.
The Patient Health Questionnaire-9 (PHQ-9; Kroenke et al., 2001 ) is a validated 9-item self-report measure of depression symptoms based on the DSM-IV criteria for major depressive disorder. Each item asks participants to rate the frequency of a symptom (e.g., little interest or pleasure in doing things) from 0 (not at all) to 3 (nearly every day). Evidence of internal consistency (α = 0.79), test-retest reliability (r = 0.84 over 48 h), convergent, divergent, criterion validity and treatment sensitivity has been provided (Beard et al., 2016, Kroenke et al., 2001). Participants completed the PHQ-9 before lesson 1, 4, and 6. Pre-treatment PHQ-9 internal consistency was α = 0.88.
The Kessler Psychological Distress Scale (K-10;Kessler et al., 2002) is a 10-item measure of psychological distress experienced by users over the past two weeks. Each item (e.g., About how often did you feel restless or fidgety?) is assessed on a 5-point scale from 1 (none of the time) to 5 (all of the time). A total score >20 indicates probable mental disorder(s) (Andrews & Slade, 2001). Evidence of internal consistency (α = 0.93), test re-test reliabilty (r = 0.80 over 1–2 weeks), convergent and discriminant validity, and treatment sensitivity has been reported (Furukawa et al., 2003, Slade et al., 2011, Sunderland et al., 2012). The psychometric properties of the instrument are stable across the adult lifespan (Sunderland, Hobbs, Anderson, & Andrews, 2012). Participants completed the K-10 prior to each lesson. Baseline internal consistency was α = 0.91.
2.5. Statistical analyses
All analyses were conducted in SPSS v 25. Counts of course registration, commencement and lesson completion estimated the uptake of the Health Anxiety course. Independent samples t-tests and χ2 tests were used to estimate group differences in demographic and clinical variables between the pre-COVID and during-COVID sample.
Intention-to-treat linear mixed models analyses with random intercepts for participants were conducted to estimate the effects of the Health Anxiety program on SHAI, PHQ-9, and K-10 total scores across time. Models were estimated using a restricted maximum likelihood estimator, time was treated as a categorical variable, and an identity covariance structure was specified to model the covariance structure of the random intercept. Linear mixed models make use of all available data including those with missing data, using maximum likelihood estimation to estimate model parameters. The relative fit of the residual covariance structure of the random effects was evaluated using the Bayesian information criterion. Specifying a first-order autoregressive structure for the residuals of the SHAI, PHQ-9 and K-10 provided the closest model fit. The fixed effects of gender, rural status, course format (self-guided vs. clinician guided), age and their interactions with time were then added to each of the models. Within-group Hedges’ g effect sizes were calculated between pre-and post-treatment and corrected for the correlation between repeated measurements (see Lakens, 2013 for formula to calculate Hedges g).
Among participants who completed the Health Anxiety program (and therefore had post-treatment data), clinically significant change was evaluated in two ways. First, health anxiety symptom severity was considered to have normalised if participants reported SHAI total scores <18 (Alberts et al., 2013, Newby et al., 2020). Second, based on Jacobson and Truax (1991), participants achieved clinically reliable change if their SHAI score reduced (reliable improvement) or increased (reliable deterioration) by ≥ 8 points from pre-to post-treatment (reliable change index calculated based on SHAI SD of 7.21 from Newby et al. (2018) and test-retest estimate of r = 0.87 from (Olatunji et al., 2011).
3. Results
3.1. Uptake of the health anxiety iCBT course associated with the COVID-19 pandemic
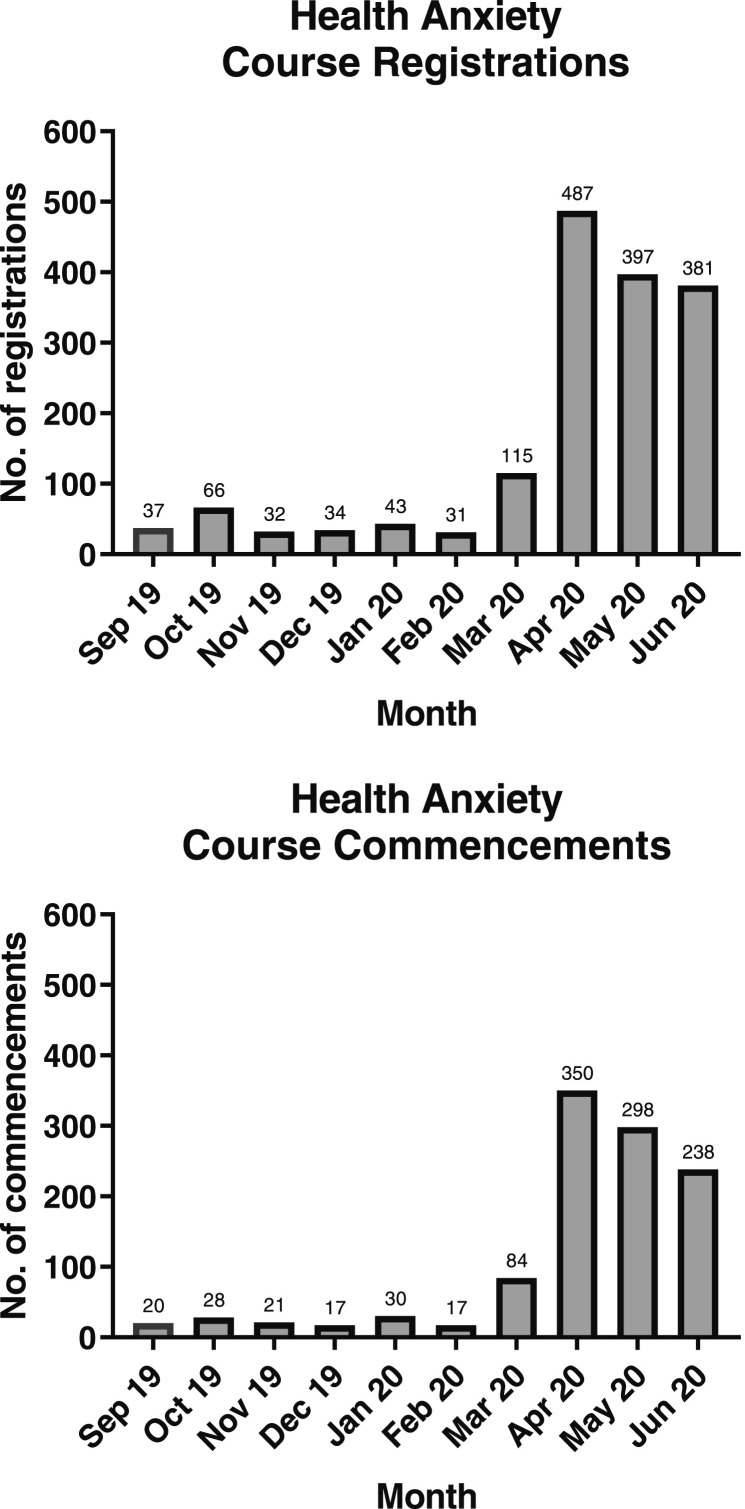
Fig. 1 provides the number of monthly course registrations and course commencements from September 2019 to June 2020. With March 2020 viewed as the transition from the pre-to during-COVID-19 pandemic period, we observed an average increase in monthly course registrations of 941.16% from the 6 months prior to the COVID-19 pandemic (September 2019 to February 2020; Mean number of registrations = 40.50 per month) to the first 3 full months of the COVID-19 pandemic (April to June 2020; Mean number of registrations = 421.67 per month). The average number of Health Anxiety course commencements per month increased by 1232.12% from the pre-COVID (M = 22.17 per month) to during-COVID period (M = 295.33 per month). A higher proportion of participants who registered for a course during the COVID pandemic started lesson one (70.04%), compared to those who registered in the pre-COVID period, where 54.74% of registrants commenced lesson one.
Fig. 1.
Course registrations and commencements by month for the THIS WAY UP Health Anxiety course.
3.2. Participant characteristics of the health anxiety course in the COVID-19 period
Table 1 provides the demographic and clinical characteristics of the participants who commenced their Health Anxiety iCBT course in each time period. There were no significant differences between the pre- and during-COVID samples in terms of age, gender or rurality, though, individuals in the COVID sample were more likely to commence a self-guided rather than clinician-guided course (see Table 1). Both the pre-COVID and during-COVID samples were characterised by high rates of probable disorder with >80% of patients reporting clinically significant health anxiety symptom severity (SHAI score ≥ 18), >40% reporting symptoms consistent with probable MDD (PHQ-9 ≥ 10), and >70% reporting clinically significant psychological distress (K10 ≥ 20). The COVID sample reported significantly lower health anxiety symptom severity compared to the pre-COVID users, although mean levels of depression and distress were comparable (see Table 1).
3.3. Adherence to the health anxiety iCBT course in the COVID-19 period
Table 2 provides a summary of lesson-by-lesson adherence for the clinician-guided vs. self-guided participants commencing the Health Anxiety course during the early months of the COVID-19 pandemic in Australia. The average number of lessons completed was 3.23 (SD = 2.11) with 30% completing all 6 lessons. There was no difference between clinician-guided and self-guided groups in course completion rates (χ 2(1) = 0.06, p = .82).
Table 2.
Lesson-by-lesson completion rates for clinician-guided and self-guided participants commencing the Health Anxiety iCBT during the COVID-19 pandemic in Australia.
| Lesson completion | Clinician-guided |
Self-guided |
||
|---|---|---|---|---|
| n | % | n | % | |
| Lesson 1 | 70 | 100 | 699 | 98.73 |
| Lesson 2 | 51 | 72.86 | 476 | 67.23 |
| Lesson 3 | 41 | 58.57 | 347 | 49.01 |
| Lesson 4 | 33 | 47.14 | 293 | 41.38 |
| Lesson 5 | 27 | 38.57 | 241 | 34.04 |
| Lesson 6 | 22 | 31.43 | 213 | 30.08 |
3.4. Program completers vs non-completers
On average, program completers were significantly older than non-completers (completers vs non-completers: M[SD] age = 40.87 [12.69] vs. 36.42 [12.38]), t (776) = −2.04, p = .04. Compared to non-completers, completers scored significantly lower on baseline self-reported measures of health anxiety (completers vs non-completers: M[SD] SHAI = 29.53 [10.53] vs. 31.30 [11.35]), t (776) = −2.04, p = .04; depression (completers vs non-completers: M[SD] PHQ-9 = 8.25 [5.86] vs. 9.68 [5.94]), t (776) = −3.11, p = .002); and psychological distress (completers vs non-completers: M[SD] K-10 = 23.40 [7.83] vs. 26.03 [7.73]), t (776) = −3.11, p < .001. Gender and rural status were not associated with completing the program (ps > 0.05; see Table 1).
3.5. Effectiveness of the health anxiety course during the COVID-19 pandemic
Table 3 shows the estimated marginal means and linear mixed model results for each outcome measure between pre-and post-treatment. The fixed effects of age, gender and the time by age interaction were significant and retained in the final model assessing SHAI outcomes. For analysis of depression outcomes (PHQ-9 as the outcome variable), the fixed effects of rural status and age were significant and retained in the model. For the psychological distress (K10) analysis, the fixed factor of age was also significant and retained in the final model. On average, participants experienced significant (p < .001) reductions on all outcome measures, with large effect size reductions in health anxiety symptom severity (SHAI; g = 0.89) and psychological distress (K10: g = 0.91). A medium effect size reduction in depression symptoms (PHQ-9: g = 0.55) was found.
Table 3.
Estimated marginal means and linear mixed models results and effect sizes for health anxiety, depression and psychological distress from pre-to post-treatment in the COVID-19 sample.
| Pre-treatment EMM (SD) | Post-treatment EMM (SD) | df for the time effect | F | r | Hedge’s g [95% CI] | |
|---|---|---|---|---|---|---|
| SHAIa | 29.15 (11.13) | 20.54 (10.18) | 463.52 | 36.23* | .731 | 0.89 [0.74; 1.04] |
| PHQ-9b | 9.54 (7.50) | 6.09 (5.74) | 323.80 | 73.59* | .680 | 0.55 [0.40; 0.70] |
| K-10c | 25.14 (7.78) | 19.40 (5.95) | 1114.51 | 75.83* | .652 | 0.91 [0.76; 1.06] |
Note. SHAI = Short Health Anxiety Inventory; PHQ-9 = Patient Health Questionnaire-9 Item; K-10 = Kessler Distress Scale-10 item; r = Pearson correlation between Lesson 1 and Lesson 6 scores for calculation of within-group effect sizes; EMM = estimated marginal mean; SD = standard deviation; *p < .001; a = Adjusted model with measurement occasion (time), age, gender and time by age interaction as fixed effects in the model; b = Adjusted model with measurement occasion (time), rural status and age as fixed effects in the model; c = Adjusted model with measurement occasion (time) and age as fixed effects in the model.
We calculated reliable improvement and deterioration in the sub-sample of patients who completed their post-treatment questionnaires to provide an index of pre-to-post symptom change (n = 235). In this sub-sample, 55.74% (n = 131/235) experienced reliable improvement and three participants (1.28%) experienced reliable deterioration in their health anxiety symptom severity. Lastly, we examined the proportion of patients whose symptom severity normalised (i.e., SHAI total < 18) at post-treatment. Of the 235 patients who completed post-treatment questionnaires, 34.04% scored below the SHAI threshold at post-treatment. Of these 235 individuals, 206 (87.66%) reported baseline SHAI scores ≥18 at pre-treatment; in this group, SHAI scores had normalised at post-treatment for 53 participants (25.73%).
4. Discussion
The COVID-19 pandemic has caused significant anxiety about health and fears of contracting COVID-19. For some people, health anxiety can be extremely disabling and distressing. To our knowledge, this study presents the first evaluation of the uptake and effectiveness of an internet cognitive behavioural therapy (iCBT) program for health anxiety, which had, prior to the pandemic, been shown to significantly reduce symptoms of health anxiety in treatment-seeking samples (Newby et al., 2016, Newby et al., 2018, Newby et al., 2020). Overall, in the months after the pandemic was declared by the World Health Organisation, as predicted, there were large increases in the numbers of people who registered for (941%) and started (1230%) the THIS WAY UP Health Anxiety iCBT Course, compared to before COVID-19. This corresponded to an average of 41 registrations per month prior to the pandemic, increasing by ten-fold to an average of 423 registrations per month in April to June 2020, during the first peak of the COVID-19 pandemic in Australia. Consistent with our previous evaluations of the Health Anxiety Course, conducted prior to the pandemic (Newby, Haskelberg et al., 2020), participants undertaking the iCBT course during the pandemic experienced significant improvements in health anxiety (Hedges’ g = 0.89), psychological distress (g = 0.91) and depression (g = 0.55). Fifty-five percent of course completers had clinically significant improvements, and 34% had scores below threshold for clinically significant levels of health anxiety on the Short Health Anxiety Inventory at the end of the program.
A comparison of the demographic and clinical profiles of participants who signed up to the Health Anxiety Course before and during COVID-19 revealed high rates of health anxiety, with >80% showing elevated health anxiety on the SHAI and > 40% reporting depression symptom severity consistent with a probable diagnosis of major depressive disorder. Unexpectedly, health anxiety scores were less severe in the sample who started the course during the pandemic, although the mean values of health anxiety on the SHAI were still very high (30.76) and in the clinical range (Alberts et al., 2013). There were no other demographic differences in the two cohorts. More participants signed up for the self-guided course option (91% versus 76% pre-COVID) than the clinician-guided option during the pandemic, which might have been due to the fact that face-to-face contact with psychologists and health providers were limited during the first few months of the pandemic in Australia due to strict nation-wide lockdowns.
The increases in uptake of the Health Anxiety course are consistent with the findings of other digital and remotely-accessed mental health service providers that have shown steep increases in service use and engagement with online therapy programs for depression and anxiety during COVID-19 (Mahoney et al., 2021, Mahoney, Li, Haskelberg, Millard, & Newby, 2021, Staples et al., 2020, Titov et al., 2020, Li et al., 2020a, Li et al., 2020b), in telephone calls to mental health and crisis support lines, telehealth consultations, and visits to mental health websites (Jayawardana and Gannon, 2021, Mahoney et al., 2021). Our results also highlight the demand for self-directed services, and the important role that scalable digital programs have in providing mental health support to address some of the mental health needs of the community in this pandemic.
One advantage of internet CBT for health anxiety is that it can be accessed even in strict lockdowns, or when people with health anxiety are unable or unwilling to travel to and attend in-person appointments due to concerns about contamination or contracting COVID-19. Our findings provide further evidence in support of some positive outcomes of iCBT for health anxiety and indicate that such programs can continue to improve health anxiety and comorbid depression and psychological distress under pandemic conditions. However, there is also room for improvement, given that 45% of program completers did not experience clinically significant improvements during the program. This proportion is higher than that observed in our evaluation of the health anxiety course prior to the pandemic where 30% of treatment completers did not report clinically significant improvement (Newby, Haskelberg et al., 2020). It is conceivable that the pandemic has attenuated the outcomes of the course to some extent. However, this possibility is speculative as no direct controlled comparisons have been conducted. Furthermore, the current outcomes of the Health Anxiety course are broadly consistent with the magnitude of symptom reduction and the rates of reliable change seen in other self-guided and clinician-guided iCBT courses for anxiety-related disorders that have been provided in community and routine care settings prior to the pandemic (Hobbs et al., 2017, Klein et al., 2011, Luu et al., 2020, Titov et al., 2017, Williams and Andrews, 2013). Nevertheless, a sizeable proportion of people do not substantially benefit from iCBT for their health anxiety and further research is needed to identify and address the factors that may contribute to this lack of response (e.g., treatment credibility, anxiety sensitivity (Hedman, Andersson, Lekander, & Ljotsson, 2015). Also, iCBT needs to be well-integrated within existing health care systems, perhaps within stepped and preventative models of care, so that additional treatment options can be considered when there is limited response to iCBT.
There are several factors which are likely to have contributed to the increase in course registrations. The course was made free to all users at the beginning of the pandemic, whereas it cost $AUD59 for 12 weeks access to the program prior to the pandemic. Making the program freely available may have reduced one barrier to signing up to the program. However, we also saw significant increases in uptake of THIS WAY UP online programs which were free before the pandemic, so the increased uptake may not be entirely explainable by the waived course fee (Li et al., 2020a, Mahoney et al., 2021, Mahoney et al., 2021). Additionally, the media promotion of THIS WAY UP and media focus on the mental health ramifications of COVID-19 likely contributed to increased course uptake. It is also possible that the high level of health anxiety and COVID-19 fear in the community, and the limited availability of clinician-based treatments (especially, face-to-face appointments) as the nation was in lockdown contributed to increased uptake of the program. Nonetheless our findings highlight the considerable need in the community for supports to manage anxiety about health, and the negative impacts of the pandemic on health anxiety in Australia, and globally.
Completion rates were lower than we expected in the COVID-19 pandemic cohort. Unexpectedly, there were no differences in completion rates in unguided (30%) and guided (31%) groups, whereas in our previous study (Newby, Haskelberg et al., 2020), we found higher completion rates in clinician-guided iCBT (46%) compared to unguided iCBT (33%). Although current completion rates are similar to those found in other evaluations of self-guided and clinician-guided iCBT (e.g., Grierson, Hobbs, & Mason, 2020, Li et al., 2020a, Li et al., 2020b, Mahoney et al., 2021, Mahoney, Li, Haskelberg, Millard, & Newby, 2021), rates of adherence are typically higher for guided iCBT (e.g., ~50–60%, Hobbs et al., 2017; Titov et al., 2017; Williams, O’Moore, Mason, & Andrews, 2014). It is unclear why completion was lower than expected in the guided Health Anxiety iCBT program in this study. The COVID-19 cohort had lower health anxiety, and lower symptom severity is associated with lower completion and engagement (Newby, Mewton, & Andrews, 2017). The waiver of the course fees may have also contributed to this finding. The addition of course fees has previously been associated with improved adherence (Hilvert-Bruce, Rossouw, Wong, Sunderland, & Andrews, 2012), and it is possible that some service users are more motivated to complete course lessons when they have paid to access them. The other possibility was that people were seeking help for COVID-19 fears, yet the program was designed for persistent, excessive fears of other diseases. Nevertheless, modest rates of course completion suggest that future research needs to develop effective strategies for improving adherence in iCBT, especially for self-guided courses which are highly scalable.
The Health Anxiety Course was originally designed to treat persistent, excessive and debilitating health anxiety, such as illness anxiety disorder and somatic symptom disorder. According to DSM-5 (American Psychiatric Association, 2013), to meet criteria for clinically significant health anxiety, a person needs to experience excessive preoccupation with illness fears for 6 months or longer, that is out of proportion to the health threat. During pandemics, some level of health anxiety is normal, adaptive, and useful in promoting proactive health behaviours (Asmundson and Taylor, 2020bbb, Faasse and Newby, 2020), and is likely to be transient, resolving once the health threat has passed, or the person learns how to adapt with and cope with their fears of the virus. Because we do not collect information on the reasons why people signed up to the course, or their clinical history, we do not know whether the increase in uptake of the Health Anxiety Course in the first few months of the pandemic was to gain supports and strategies to manage transient health anxiety, or to manage pre-existing clinical health anxiety that was exacerbated by the pandemic. Internet CBT has potential to be beneficial even if the anxiety appears proportional to the threat posed by COVID-19, provided the person is experiencing heightened or debilitating health anxiety. Normal, transient health anxiety may not require treatment as it will resolve once the threat has passed or eased. In addition, some of the treatment components in the Health Anxiety Course are likely to be useful (e.g., relaxation, challenging unhelpful cognitions about health and illness, limiting excessive internet searching about symptoms and body hypervigilance), but others may contradict the messaging of public health campaigns. For example, in the current pandemic, all citizens have been actively encouraged to seek testing for COVID-19 when they notice even mild symptoms of the disease. However, people with excessive health anxiety are often discouraged from repeatedly asking for multiple tests and investigations when they notice new signs and symptoms, especially after they have already received negative test results and medical reassurance. This is because repeated and excessive testing and investigations t can contribute to the maintenance of health anxiety by encouraging preoccupation and body hypervigilance. Future research efforts need to determine the most effective treatments and supports to help support people with transient health anxiety about COVID-19, whether tailored approaches are needed, and whether treatment is needed or not. One promising example of this is a brief 3-week self-guided online cognitive behavioural intervention for excessive and dysfunctional worry related to the COVID-19 pandemic, including worries about illness, death, economy, and family. In a Swedish sample, Wahlund and colleagues (Wahlund et al., 2020) found the program outperformed a waitlist control group in reducing anxiety 3 weeks post-baseline. These promising findings await replication in other countries and health care contexts.
4.1. Limitations
There was no control group, and it was possible that the improved health anxiety during COVID-19 was due to the easing of temporary health anxiety as individuals learned to adjust to their circumstances. We collect minimal information about service users, including their demographics, reasons for accessing support, treatment and clinical history, physical health status or comorbidities (including COVID-19 status). We only assessed health anxiety, not COVID-specific fears, and are limited by the lack of diagnostic interviews, and reliance on self-report data. Therefore, it is unknown whether participants met criteria for illness anxiety disorder or somatic symptom disorder, COVID-19 specific phobia, adjustment disorders, or other medical conditions. Although there were no exclusion criteria for enrolling in the Health Anxiety course, THIS WAY UP programs were not recommended for people experiencing psychosis, bipolar disorder or substance abuse disorders because the of the lack of evidence in those samples. It is unclear if current findings would generalise to these groups because it is unclear how many people with these disorders undertook the Health Anxiety course.
The THIS WAY UP digital mental health service administers measures of psychological symptoms at each lesson to track treatment progress, but the lack of follow-up assessments means we do not know whether treatment gains are maintained beyond the end of the program. The attrition and missing data are a limitation, which may have led to biased estimates of treatment effect. Finally, the questionnaires and cut-off scores to determine whether participants were reporting ‘clinical’ levels of health anxiety, depression and distress have not been specifically validated during the pandemic. Therefore, we may have under- or over-estimated the number of participants in the clinical range on these measures before and after the program finished.
5. Conclusions
There was a substantial increase in the demand and use of THIS WAY UP’s iCBT Health Anxiety course in the first four months of the COVID-19 pandemic in Australia. The THIS WAY UP internet-delivered CBT for health anxiety remains effective in pandemic conditions in reducing health anxiety, depression and distress. Internet CBT for health anxiety provides a potentially scalable, accessible tool to help manage health anxiety symptoms and demand for mental health care. Future research should explore how to improve engagement and outcomes of this iCBT program, and further evaluate the uptake, use and outcomes of iCBT for health anxiety throughout later stages of the pandemic.
Funding Source
A/Prof Newby is supported by the Medical Research Future Fund, Australia (Grant id: MRFF1145382).
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.janxdis.2021.102494.
Appendix A. Supplementary material
Supplementary material
.
References
- Abramowitz J.S., Deacon B.J., Valentiner D.P. The short health anxiety inventory: Psychometric properties and construct validity in a non-clinical sample. Cognitive Therapy and Research. 2007;31(6):871–883. doi: 10.1007/s10608-006-9058-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alberts N.M., Hadjistavropoulos H.D., Jones S.L., Sharpe D. The short health anxiety inventory: A systematic review and meta-analysis. Journal of Anxiety Disorders. 2013;27(1):68–78. doi: 10.1016/j.janxdis.2012.10.009. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . American Psychiatric Association; Arlington, VA: 2013. Diagnostic and statistical manual of mental disorders: DSM-5. [Google Scholar]
- Andrews G., Slade T. Interpreting scores on the Kessler psychological distress scale (K10) Australian and New Zealand Journal of Public Health. 2001;25(6):494–497. doi: 10.1111/j.1467-842X.2001.tb00310.x. [DOI] [PubMed] [Google Scholar]
- Asmundson G.J.G., Taylor S. Coronaphobia: Fear and the 2019-nCoV outbreak. Journal of Anxiety Disordes. 2020;70 doi: 10.1016/j.janxdis.2020.102196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asmundson G.J.G., Taylor S. How health anxiety influences responses to viral outbreaks like COVID-19: What all decision-makers, health authorities, and health care professionals need to know. Journal of Anxiety Disorders. 2020;71 doi: 10.1016/j.janxdis.2020.102211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Axelsson E., Andersson E., Ljótsson B., Björkander D., Hedman-Lagerlöf M., Hedman-Lagerlöf E. Effect of Internet vs face-to-face cognitive behavior therapy for health anxiety: A randomized noninferiority clinical trial. JAMA Psychiatry. 2020;77(9):915–924. doi: 10.1001/jamapsychiatry.2020.0940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beard C., Hsu K.J., Rifkin L.S., Busch A.B., Bjorgvinsson T. Validation of the PHQ-9 in a psychiatric sample. Journal of Affective Disorders. 2016;193:267–273. doi: 10.1016/j.jad.2015.12.075. [DOI] [PubMed] [Google Scholar]
- Bobevski I., Clarke D.M., Meadows G. Health anxiety and its relationship to disability and service use: Findings from a large epidemiological survey. Psychosomatic Medicine. 2016;78(1):13–25. doi: 10.1097/PSY.0000000000000252. [DOI] [PubMed] [Google Scholar]
- Faasse K., Newby J.M. Public perceptions of COVID-19 in Australia: Perceived risk, knowledge, health-protective behaviors, and vaccine intentions. Frontiers in Psychology. 2020;11 doi: 10.3389/fpsyg.2020.551004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fink P., Ørnbøl E., Christensen K.S. The outcome of health anxiety in primary care: A two-year follow-up study on health care costs and self-rated health. PLoS One. 2010;5(3) doi: 10.1371/journal.pone.0009873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furukawa T.A., Kessler R.C., Slade T., Andrews G. The performance of the K6 and K10 screening scales for psychological distress in the Australian National Survey of Mental Health and Well-Being. Psychological Medicine. 2003;33(2):357–362. doi: 10.1017/S0033291702006700. [DOI] [PubMed] [Google Scholar]
- Grierson A.B., Hobbs M.J., Mason E.C. Self-guided online cognitive behavioural therapy for insomnia: a naturalistic evaluation in patients with potential psychiatric comorbidities. Journal of Affective Disorders. 2020;266:305–310. doi: 10.1016/j.jad.2020.01.143. [DOI] [PubMed] [Google Scholar]
- Hedman E., Andersson E., Lekander M., Ljotsson B. Predictors in Internet-delivered cognitive behavior therapy and behavioral stress management for severe health anxiety. Behaviour Research and Therapy. 2015;64:49–55. doi: 10.1016/j.brat.2014.11.009. [DOI] [PubMed] [Google Scholar]
- Hedman E., Axelsson E., Andersson E., Lekander M., Ljótsson B. Exposure-based cognitive-behavioural therapy via the internet and as bibliotherapy for somatic symptom disorder and illness anxiety disorder: Randomised controlled trial. British Journal of Psychiatry. 2016;209(5):407–413. doi: 10.1192/bjp.bp.116.181396. [DOI] [PubMed] [Google Scholar]
- Hedman E., Axelsson E., Gorling A., Ritzman C., Ronnheden M., El Alaoui S.…Ljotsson B. Internet-delivered exposure-based cognitive-behavioural therapy and behavioural stress management for severe health anxiety: Randomised controlled trial. British Journal of Psychiatry. 2014;205(4):307–314. doi: 10.1192/bjp.bp.113.140913. [DOI] [PubMed] [Google Scholar]
- Hilvert-Bruce Z., Rossouw P.J., Wong N., Sunderland M., Andrews G. Adherence as a determinant of effectiveness of internet cognitive behavioural therapy for anxiety and depressive disorders. Behaviour Research and Therapy. 2012;50(7–8):463–468. doi: 10.1016/j.brat.2012.04.001. [DOI] [PubMed] [Google Scholar]
- Hobbs M.J., Mahoney A.E.J., Andrews G. Integrating iCBT for generalized anxiety disorder into routine clinical care: Treatment effects across the adult lifespan. Journal of Anxiety Disorders. 2017;51:47–54. doi: 10.1016/j.janxdis.2017.09.003. [DOI] [PubMed] [Google Scholar]
- Jacobson N.S., Truax P. Clinical significance: A statistical approach to defining meaningul change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59(1):12–19. doi: 10.1037/0022-006X.59.1.12. [DOI] [PubMed] [Google Scholar]
- Jayawardana D., Gannon B. Use of telehealth mental health services during the COVID-19 pandemic. Australian Health Review. 2021;45(4):442–446. doi: 10.1071/AH20325. [DOI] [PubMed] [Google Scholar]
- Jungmann S.M., Witthöft M. Health anxiety, cyberchondria, and coping in the current COVID-19 pandemic: Which factors are related to coronavirus anxiety? Journal of Anxiety Disorders. 2020;73 doi: 10.1016/j.janxdis.2020.102239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Andrews G., Colpe L.J., Hiripi E., Mroczek D.K., Normand S.L.T.…Zaslavsky A.M. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine. 2002;32(6):959–976. doi: 10.1017/S0033291702006074. [DOI] [PubMed] [Google Scholar]
- Klein B., Meyer D., Austin D.W., Kyrios M. Anxiety online-A virtual clinic: Preliminary outcomes following completion of five fully automated treatment programs for anxiety disorders and symptoms. Journal of Medical Internet Research. 2011;13(4):353–372. doi: 10.2196/jmir.1918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R., Williams J. The PHQ-9: Valdity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Frontiers in Psychology. 2013;4:863. doi: 10.3389/fpsyg.2013.00863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, I., Chen, A. Z., Newby, J. M., Kladnitski, N., Haskelberg, H., Millard, M., & Mahoney, A. E. J. (2020). The uptake and effectiveness of an online self-help mindfulness program during COVID-19. Manuscript submitted for publication.
- Li, I., Millard, M., Haskelberg, H., Hobbs, M. J., Luu, J., & Mahoney, A. E. J. (2020). COVID-19 related differences in the uptake and effects of internet-based cognitive behavioural therapy for symptoms of obsessive-compulsive disorder. Manuscript submitted for publication. [DOI] [PubMed]
- Luu J., Millard M., Newby J., Haskelberg H., Hobbs M.J., Mahoney A.E.J. Internet-based cognitive behavioural therapy for treating symptoms of obsessive compulsive disorder in routine care. Journal of Obsessive Compulsive and Related Disorders. 2020;26 doi: 10.1016/j.jocrd.2020.100561. [DOI] [Google Scholar]
- Mahoney A.E.J., Elders A., Li I., David C., Haskelberg H., Guiney H., Millard M. A tale of two countries: Increased uptake of digital mental health services during the COVID-19 pandemic in Australia and New Zealand. Internet Interventions. 2021;25 doi: 10.1016/j.invent.2021.100439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahoney A.E.J., Li I., Grierson A.B., Haskelberg H., Millard M., Mason E. Internet-based cognitive behaviour therapy for insomnia before and during the COVID-19 pandemic. Australian Psychologist. 2021:1–12. doi: 10.1080/00050067.2021.1979884. [DOI] [Google Scholar]
- Mahoney A.E.J., Li I., Haskelberg H., Millard M., Newby J.M. The uptake and effectiveness of online cognitive behaviour therapy for symptoms of anxiety and depression during COVID-19. Journal of Affective Disorders. 2021;292:197–203. doi: 10.1016/j.jad.2021.05.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay D., Yang H., Elhai J., Asmundson G.J.G. Anxiety regarding contracting COVID-19 related to interoceptive anxiety sensations: The moderating role of disgust propensity and sensitivity. Journal of Anxiety Disorders. 2020;73 doi: 10.1016/j.janxdis.2020.102233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mertens G., Gerritsen L., Duijndam S., Salemink E., Engelhard I.M. Fear of the coronavirus (COVID-19): Predictors in an online study conducted in March 2020. Journal of Anxiety Disorders. 2020;74 doi: 10.1016/j.janxdis.2020.102258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newby J.M., Haskelberg H., Hobbs M.J., Mahoney A.E.J., Mason E., Andrews G. The effectiveness of internet-delivered cognitive behavioural therapy for health anxiety in routine care. Journal of Anxiety Disorders. 2020;264:535–542. doi: 10.1016/j.jad.2019.11.087. [DOI] [PubMed] [Google Scholar]
- Newby J.M., Mahoney A.E.J., Mason E., Smith J., Uppal S., Andrews G. Pilot trial of a therapist-supported internet-delivered cognitive behavioural therapy program for health anxiety. Internet Interventions. 2016;6:71–79. doi: 10.1016/j.invent.2016.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newby J.M., Mewton L., Andrews G. Transdiagnostic versus disorder-specific internet cognitive behaviour therapy for depression and anxiety in primary care. Journal of Anxiety Disordersd. 2017;46:23–34. doi: 10.1016/j.janxdis.2016.06.002. [DOI] [PubMed] [Google Scholar]
- Newby J.M., O’Moore K., Tang S., Christensen H., Faasse K. Acute mental health responses during the COVID-19 pandemic in Australia. PLOS One. 2020;15(7) doi: 10.1371/journal.pone.0236562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newby J.M., Smith J., Uppal S., Mason E., Mahoney A.E.J., Andrews G. Internet-based cognitive behavioral therapy versus psychoeducation control for illness anxiety disorder and somatic symptom disorder: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2018;86(1):89–98. doi: 10.1037/ccp0000248. [DOI] [PubMed] [Google Scholar]
- Olatunji B.O., Etzel E.N., Tomarken A.J., Ciesielski B.G., Deacon B. The effects of safety behaviors on health anxiety: An experimental investigation. Behaviour Research and Therapy. 2011;49(11):719–728. doi: 10.1016/j.brat.2011.07.008. [DOI] [PubMed] [Google Scholar]
- Salkovskis P., Rimes K., Warwick H., Clark D. The health anxiety inventory: Development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychological Medicine. 2002;32(05):843–853. doi: 10.1017/S0033291702005822. [DOI] [PubMed] [Google Scholar]
- Slade T., Grove R., Burgess P. Kessler Psychological Distress Scale: Normative data from the 2007 Australian National Survey of Mental Health and Wellbeing. Australian and New Zealand Journal of Psychiatry. 2011;45(4):308–316. doi: 10.1080/00048670701261194. [DOI] [PubMed] [Google Scholar]
- Staples L., Nielssen O., Kayrouz R., Cross S., Karin E., Ryan K.…Titov N. Rapid report 2: Symptoms of anxiety and depression during the first 12 weeks of the Coronavirus (COVID-19) pandemic in Australia. Internet Interventions The Application of Information Technology in Mental and Behavioural Health. 2020;22 doi: 10.1016/j.invent.2020.100351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sunderland M., Hobbs M.J., Anderson T.M., Andrews G. Psychological distress across the lifespan: examining age-related item bias in the Kessler 6 Psychological Distress Scale. International Psychogeriatrics. 2012;24(2):231–242. doi: 10.1017/S1041610211001852. [DOI] [PubMed] [Google Scholar]
- Sunderland M., Newby J.M., Andrews G. Health anxiety in Australia: Prevalence, comorbidity, disability and service use. The British Journal of Psychiatry. 2012;202:56–61. doi: 10.1192/bjp.bp.111.103960. [DOI] [PubMed] [Google Scholar]
- Sunderland M., Wong N.R., Hilvert-Bruce Z., Andrews G. Investigating trajectories of change in psychological distress amongst patients with depression and generalised anxiety disorder treated with internet cognitive behavioural therapy. Behaviour Research and Therapy. 2012;50(6):374–380. doi: 10.1016/j.brat.2012.03.005. [DOI] [PubMed] [Google Scholar]
- Taylor S., Landry C.A., Paluszek M.M., Fergus T.A., McKay D., Asmundson G.J.G. Development and initial validation of the COVID Stress Scales. Journal of Anxiety Disorders. 2020;72 doi: 10.1016/j.janxdis.2020.102232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Titov N., Dear B.F., Staples L.G., Bennett-Levy J., Klein B., Rapee R.M.…Nielssen O.B. The first 30 months of the MindSpot Clinic: Evaluation of a national e-mental health service against project objectives. Australian and New Zealand Journal of Psychiatry. 2017;51(12):1227–1239. doi: 10.1177/0004867416671598. [DOI] [PubMed] [Google Scholar]
- Titov N., Staples L., Kayrouz R., Cross S., Karin E., Ryan K.…Nielssen O. Rapid report: Early demand, profiles and concerns of mental health users during the coronavirus (COVID-19) pandemic. Internet Interventions The Application of Information Technology in Mental and Behavioural Health. 2020;21 doi: 10.1016/j.invent.2020.100327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahlund T., Mataix-Cols D., Olofsdotter Lauri K., de Schipper E., Ljótsson B., Aspvall K., Andersson E. Brief online cognitive behavioural intervention for dysfunctional worry related to the COVID-19 pandemic: A randomised controlled trial. Psychotherapy and Psychosomatics. 2020;90:1–9. doi: 10.1159/000512843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weck F., Richtberg S., Neng J.M.B. Epidemiology of hypochondriasis and health anxiety: Comparison of different diagnostic criteria. Current Psychiatry Reviews. 2014;10(1):14–23. doi: 10.2174/1573400509666131119004444. [DOI] [Google Scholar]
- Williams A.D., Andrews G. The effectiveness of Internet cognitive behavioural therapy (iCBT) for depression in primary care: A quality assurance study. PLoS One. 2013;8(2) doi: 10.1371/journal.pone.0057447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams A.D., O’Moore K., Mason E., Andrews G. The effectiveness of internet cognitive behaviour therapy (iCBT) for social anxiety disorder across two routine practice pathways. Internet Interventions. 2014 doi: 10.1016/j.invent.2014.11.001. [DOI] [Google Scholar]
- Wu T., Jia X., Shi H., Niu J., Yin X., Xie J., Wang X. Prevalence of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis. Journal of Affective Disorders. 2020;281:91–98. doi: 10.1016/j.jad.2020.11.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material