Abstract
Background
Depression and anxiety are comorbidities of inflammatory bowel disease (IBD), and it is now recommended to screen IBD patients for these conditions. We screened patients using a novel computerized adaptive testing technology and compared the screening results to measures of disease activity.
Methods
Consecutive patients at our tertiary IBD clinic were asked to complete the validated CAT-MH survey (Adaptive Testing Technologies, Chicago, IL); we then reviewed disease and patient characteristics. Clinical remission status was determined based on clinical, laboratory, endoscopy, and imaging results. Statistical methods included Fisher exact test and Pearson chi-square tests to assess association. Univariable and multivariable analyses were performed.
Results
We included 134 patients, of which 34 (25.3%) screened positive for depression and 18 (13.4%) screened positive for anxiety. We identified 19 (55.9%) and 10 (55.5%) patients who were previously undiagnosed for depression and anxiety, respectively. Patients in clinical remission were less likely to screen positive for depression (odds ratio 0.19; 95% confidence interval 0.07–0.50) and for anxiety (odds ratio 0.30; 95% confidence interval 0.10–0.91). Compared to patients with negative C-reactive protein values, patients with positive C-reactive protein were more likely to also screen positive for depression (P = 0.025) and anxiety (P = 0.15).
Conclusions
We demonstrate the utility of a novel testing technology for screening patients with IBD for depression and anxiety. We found a large number of patients with previously undiagnosed anxiety or depression and a significant positive association between clinically active IBD and these mental health conditions. This work supports and informs recommendations for mental health screening in the IBD population.
Keywords: depression, anxiety, inflammatory bowel disease, mental health, comorbidities
INTRODUCTION
Depression and anxiety are observed at higher rates for patients with chronic diseases, including inflammatory bowel disease (IBD). These psychiatric comorbidities impact patients’ quality of life, their IBD treatment compliance, and morbidity.1–3 Addressing patient mental health can improve quality of life and disease outcomes.4 Updated clinical guidelines for ulcerative colitis (UC) and Crohn disease (CD) include that psychological conditions may impair social interaction or career progression, decrease health-related quality of life (HRQoL), and could contribute to disease progression and exacerbation.5,6 Further, these guidelines recommend the assessment and management of mental health conditions as part of the comprehensive care of patients with IBD, but do not elaborate on the operational aspects of performing such screening and treatment in busy clinical practices.
In this study, we used a novel adaptive testing technology to screen for major depressive disorder (MDD) and generalized anxiety disorder (GAD), and assessed risk factors associated with MDD and GAD.
METHODS
Survey Protocol
We enrolled consecutive patients in our tertiary IBD center in this study and used the Computerized Adaptive Testing-Mental Health technology (CAT-MH; Adaptive Testing Technologies, Chicago, IL), validated in previous studies.7,8 The CAT-MH is based on multidimensional item response theory (MIRT). IRT is a form of model-based measurement that estimates a person’s ability or impairment based on the most difficult or severe item endorsed, and the difficulty or severity of the item is a parameter that is estimated from calibration data. This contrasts with traditional mental health measurement that estimates ability/impairment as a simple unweighted count of the individual item scores, without regard to their varying difficulty or severity. MIRT extends traditional unidimensional IRT to complex traits such as depression and anxiety that are inherently multidimensional because the items are sampled from distinct subdomains such as mood, cognition, somatization, suicidality to name a few.9 Once the items are calibrated using an MIRT model, adaptive tests can be constructed to select an optimal small subset of items targeted directly to that person’s ability or impairment level, which is learned based on the person’s responses up to that point in the test administration.9,10 The net result is that we can dramatically increase the precision of measurement by extracting the information from large banks of items (the CAT-MH depression test has 389 items and the anxiety test has 437 items), while at the same time decreasing the burden of measurement by adaptively selecting a small subset of optimally selected items for that patient (on average 12 items for each construct measured).9 The CAT-MH is the only adaptive measurement system based on MIRT.9,10 Severity is measured on a 100 point scale with 5 points of precision. These scores have been thresholded into the categories of normal (<35), mild (35–65), moderate (66–75), and severe (>75) for both anxiety and depression screens.8,9
Using the CAT-MH we administered a brief suicide screener based on the Columbia-Suicide Severity Rating Scale (C-SSRS), a computerized adaptive diagnostic screener for MDD (the CAD-MDD),11 and adaptive tests for depression (CAT-DI)8 and anxiety (CAT-ANX).9 The C-SSRS yields a result of positive or negative, in which a positive result correlates to a 9-fold increase in the likelihood of a suicide attempt in the following 6 months.12 The MDD test produces a positive or negative diagnosis of MDD and the corresponding confidence level; this test has a sensitivity of 0.95 and a specificity of 0.87 for a structured clinical diagnostic interview (SCID for DSM-5), but reduces the time from an hour to less than a minute.11 The depression and anxiety tests report severity on a 100 point scale, and categorical severity classifications of none, mild, moderate, and severe. The test for anxiety also reports the probability of GAD. We characterized patients as positive for depression if they received a positive MDD screen, and we deemed patients positive for anxiety if their GAD probability was greater than or equal to 0.5.9
Patient Recruitment and Data Collection
This study was approved by the University of Chicago Institutional Review Board under IRB19-1256. We approached consecutive patients during their clinic appointments for consent and then administered the survey. The survey was delivered via text message (n = 133) or email (n = 1) to all participants. The patients were asked to take the survey while they remained in the clinic. Results of the CAT-MH survey were available immediately upon completion and were given to the senior author. If a patient screened positive for suicidal ideation or intent, positive for MDD, and/or scores in the moderate to severe categories for either anxiety or depression, the senior author was made aware, discussed the results with the patient and advised them regarding resources. Additionally, patients who screened positive for suicidal ideation or intent were counseled and referred to the emergency room if necessary.
We performed detailed chart review on recruited patients, reviewing demographic data, fecal calprotectin levels, and endoscopy reports within 6 months of the survey date, current and failed IBD medications, psychiatric medications, surgical history, disease classification, and CAT-MH survey results. We identified patients with a history of depression and/or anxiety based on a previous diagnosis by a psychiatric professional. Additionally, we classified patients as having a history of anxiety and/or depression if they previously been prescribed selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhbitor (SNRIs), tricyclics, or benzodiazepines for an associated mental health disorder. It is possible that a patient had a diagnosis of either depression or anxiety and it was not evident in their chart. We also reviewed past C-reactive protein (CRP) measures for all patients in order to evaluate for CRP reactivity. CRP measures ≥5 mg/L were considered positive and patients who did not have prior evidence of elevated CRP to rely on this measure of inflammatory activity were excluded in this part of the analysis.13
Patients were assessed as clinically active based on the clinic note of the date of the CAT-MH administration combined with the appointment-related laboratory, endoscopic, or radiologic assessments. All patient disease activity assignments were reviewed and confirmed by the senior author, who was blinded to the CAT-MH results at the time of disease activity assessment.
Statistical Analysis
Analysis was performed using SPSS Statistics (Version 23.0; IBM, Armonk, NY). Descriptive analyses were performed to assess the prevalence of psychiatric comorbidities prior to survey administration, to calculate the fraction of patients who screened positive for depression and/or anxiety, and to determine the population of patients that had previously been undiagnosed for either depression or anxiety. Categorical variables were assessed using chi-square and Fisher exact test, when appropriate. A binary logistic regression was conducted to further examine the associations between depression and anxiety and demographic and clinical characteristics. Covariates considered in the regression model were sex (male, female), IBD subtype (UC, CD), race (white, nonwhite, unknown), past surgeries related to IBD (yes, no), and disease activity (active, remission). Covariates were chosen based on hypothesized associations with mental illness and IBD or if they reached a threshold level of P = 0.2 in univariable analyses. The associations were reported as odds ratios (ORs) and 95% confidence intervals (CIs).
RESULTS
Our analysis included 134 patients of which 75 (55.9%) were women, 112 (83.5%) were Caucasian, and 84 (62.6%) had CD (Table 1). The median survey administration time was 3 minutes and 32 seconds. We report on the number of individuals who screened positive for depression and/or anxiety and the corresponding severity of the positive screen, on the proportion of patients who were previously undiagnosed with a psychiatric disorder relative to the proportion of patients who screened positive, on the risk factors that were associated with a positive diagnosis in our sample size, and on the correlation between a positive CRP level and the concurrence of positive diagnosis of anxiety and/or depression.
TABLE 1.
Variables Predicting Undiagnosed Patients
| Depression | Anxiety | |||
|---|---|---|---|---|
| Total Diagnosed | Previously Undiagnosed | Total Diagnosed | Previously Undiagnosed | |
| Sex, N (%) | ||||
| Female sex, 75 (55.9%) | 20/34 (59%) | 11/19 (58%) | 13/18 (72%) | 7/10 (70%) |
| Male sex, 59 (44.0%) | 14/34 (41%) | 8/19 (42%) | 5/18 (28%) | 3/10 (30%) |
| P | 0.90 | 1.00 | ||
| Race, N (%) | ||||
| White, 112 (83.5%) | 28/34 (82%) | 16/19 (84%) | 13/18 (72%) | 7/10 (70%) |
| Nonwhite, 12 (9.0%) | 3/34 (9%) | 3/19 (16%) | 2/18 (11%) | 3/10 (30%) |
| Not reported, 10 (7.5%) | 3/34 (9%) | 0/19 (0%) | 3/18 (17%) | 0/10 (0%) |
| P | 0.05* | 0.33 | ||
| Type of IBD, N (%) | ||||
| UC, 50 (37.3%) | 9/34 (26%) | 6/19 (32%) | 3/18 (17%) | 0/10 (0%) |
| CD, 84 (62.7%) | 25/34 (73%) | 13/19 (68%) | 15/18 (83%) | 10/10 (100%) |
| P | 0.70 | 0.07 | ||
*Significant if P < 0.05.
Previously Undiagnosed Depression/Anxiety
We identified 34 (25.3%) patients with depression, most of whom were in the mild category [30 mild (88.2%), 2 were moderate (5.9%), and 2 were severe (5.9%)]. We identified 18 (13.4%) patients with anxiety [6 with mild anxiety (33.3%), 10 with moderate anxiety (55.5%), and 2 with severe anxiety (11.1%)]. We found 11 patients (8.2%) with both depression and anxiety, 23 (17.2%) presented solely with depression, and 7 (5.2%) presented solely with anxiety (Table 2). Two (1.5%) of the 134 patients screened positive for suicidal ideation.
TABLE 2.
Number of Patients Categorized by Depression and Anxiety Results From CAT-MH Survey
| Anxiety Category | |||||
|---|---|---|---|---|---|
| n (%) | Normal | Mild | Moderate | Severe | Total |
| Depression category | |||||
| Normal | 93 (69.4%) | 3 (2.2%) | 3 (2.2%) | 1 (0.7%) | 100 (74.6%) |
| Mild | 21 (15.7%) | 3 (2.2%) | 6 (4.5%) | 0 | 30 (22.4%) |
| Moderate | 2 (1.5%) | 0 | 0 | 0 | 2 (1.5%) |
| Severe | 0 | 0 | 1 (0.7%) | 1 (0.7%) | 2 (1.5%) |
| Total | 116 (86.6%) | 6 (4.5%) | 10 (7.5%) | 2 (1.5%) | 134 (100%) |
Of the patients positive for depression, 19 (55.9%) did not have a previous lifetime diagnosis (17 mild, 1 moderate, and 1 severe). Of the 19 patients previously undiagnosed for depression, 16 (84.2%) were Caucasian (P = 0.05), 11 (57.9%) were women (P = 0.90), and 13 (68.4%) had CD (P = 0.70). Of the 18 patients positive for anxiety, 10 (55.5%) did not have a previous lifetime diagnosis (3 mild, 6 moderate, and 1 severe). Of the 10 patients with undiagnosed anxiety, 7 were Caucasian (70%) (P = 0.33), 7 were women (70%) (P = 1.00), and 10 (100%) had CD (P = 0.07) (Table 1).
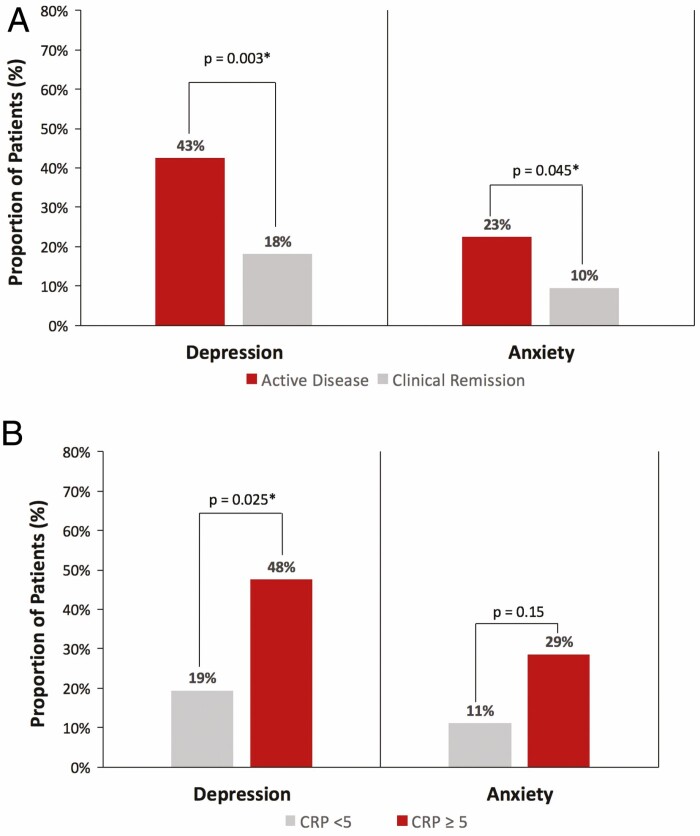
Factors Associated With Depression/Anxiety
Univariable analysis of 134 patients found that sex, race, type of IBD, smoking status, IBD-related surgical history, and number of discontinued medications were not statistically significant predictors for anxiety or depression (Table 3). Out of the 40 patients classified by the senior author as having active disease, 17 (42.5%) screened positive for depression whereas only 17 (18.1%) out of the 94 patients classified as being in remission screened positive for depression (P = 0.003). Similarly, 9 (22.5%) of the 40 patients with active disease screened positive for anxiety whereas 9.6% of the 94 patients with remission screened positive for anxiety (P = 0.045) (Fig. 1A).
TABLE 3.
Proportion of Patients Screening Positive for Depression or Anxiety by Hypothesized Risk Factors
| Positive for Depression | Positive for Anxiety | |
|---|---|---|
| N = 134 | n/N (%) | n/N (%) |
| Sex, N (%) | ||
| Female sex, 75 (55.9%) | 20/75 (26.7%) | 13/75 (17.3%) |
| Male sex, 59 (44.0%) | 14/59 (23.7%) | 5/59 (8.5%) |
| P | 0.70 | 0.14 |
| Race, N (%) | ||
| White, 112 (83.5%) | 28/112 (25.0%) | 13/112 (11.6%) |
| Nonwhite, 12 (9.0%) | 3/12 (25.0%) | 2/12 (16.7%) |
| Not reported, 10 (7.5%) | — | — |
| P | 1.00 | 0.64 |
| Type of IBD, N (%) | ||
| UC, 50 (37.3%) | 9/50 (18.0%) | 3/50 (6.0%) |
| CD, 84 (62.7%) | 25/84 (29.8%) | 15/84 (17.9%) |
| P | 0.13 | 0.07 |
| Smoking status, N (%) | ||
| Current or former, 30 (22.4%) | 10/30 (33.3%) | 5/30 (16.7%) |
| Never, 104 (77.6%) | 24/104 (23.1%) | 13/104 (12.5%) |
| P | 0.26 | 0.56 |
| Past surgeries related to IBD, N (%) | ||
| Yes, 57 (42.5%) | 19/57 (33.3%) | 7/57 (12.3%) |
| No, 77 (57.5%) | 15/77 (19.5%) | 11/77 (14.3%) |
| P | 0.07 | 0.74 |
| No. discontinued medications, N (%) | ||
| 0–2, 74 (55.2%) | 16/74 (21.6%) | 8/74 (10.8%) |
| 3+, 60 (44.8%) | 18/60 (30.0%) | 10/60 (16.7%) |
| P | 0.27 | 0.32 |
| Disease status, N (%) | ||
| Active, 40 (29.9%) | 17/40 (42.5%) | 9/40 (22.5%) |
| Clinical remission, 94 (70.1%) | 17/94 (18.1%) | 9/94 (9.6%) |
| P | 0.003* | 0.045* |
*Significant if P < 0.05.
FIGURE 1.
A, Proportion of patients with depression and anxiety based on clinically active disease. B, Proportion of patients with depression and anxiety based on CRP levels. *Significant if P < 0.05.
In the multivariable logistic regression model predicting depression and anxiety, IBD-related surgery was associated with an almost 3 times greater likelihood of screening positive for depression (OR = 2.79, 95% CI = 1.03–7.55). Patients with UC were 78% less likely to screen positive for anxiety (OR = 0.22, 95% CI = 0.06, 0.87). Moreover, patients in clinical remission were 81% less likely to screen positive for depression (OR = 0.19, 95% CI = 0.07, 0.50) and 70% less likely to screen positive for anxiety (OR = 0.30, 95% CI = 0.10, 0.91) (Table 4).
TABLE 4.
Multivariable Analysis for Factors Associated With Screening Positive for Depression and Anxiety
| Depression | Anxiety | |
|---|---|---|
| OR (95% CI) | OR (95% CI) | |
| Sex (male) | 0.95 (0.41–2.23) | 0.42 (0.13–1.32) |
| Race (white) | 0.99 (0.24–4.12) | 0.53 (0.09–3.03) |
| Type of IBD (UC) | 0.59 (0.21–1.61) | 0.22 (0.06–0.87)* |
| IBD-related surgery (yes) | 2.79 (1.03–7.55)* | — |
| Disease activity (clinical remission) | 0.19 (0.07–0.50)* | 0.30 (0.10–0.91)* |
*Significant at P < 0.05.
Correlation Between CRP, Disease Activity, and Depression/Anxiety
Since having clinically active disease was significantly associated with depression and anxiety, the association between objective measures of disease activity and depression and anxiety results were further explored. In all, 105 (78.35%) patients were reactive to CRP. Of the 105 patients, 57 (54.2%) patients had CRP measures taken within 6 months of their survey date. Median time between CRP measurement and CAT-MH administration was 2 days (interquartile range [IQR] = 70 days). Of these 57 patients, 21 (36.8%) had positive CRP measures (≥5 mg/L). Compared to patients with negative CRP values, patients with positive CRP were more likely to also screen positive for depression (P = 0.025) and anxiety (P = 0.15) (Fig. 1B).
DISCUSSION
In this study of patients with IBD at a tertiary center, we demonstrate for the first time the utility of a novel computerized adaptive testing technology and in using it, identified that a majority of these patients had previously undiagnosed depression, anxiety, or a combination of the 2. We also confirm previously reported correlations between clinically active disease and the presence of these mental health disorders.
Our study revealed that patients who are Caucasian, women, and/or have a diagnosis of CD are the most represented in the population of patients who were previously undiagnosed. These findings align with a comparable study on a population of patients with IBD in which the authors found that one-third of participants with depression and two-thirds with anxiety were previously undiagnosed.14
This study suggests that there are differences between races in patients who were previously undiagnosed with depression. This might be explained given the uneven distribution of races accounted for in our study. Other work suggests that there are differences between sexes with depression and anxiety, but not necessarily with race or IBD diagnosis.14,15 Given the significant proportion of patients that we identified as previously undiagnosed with a comorbid psychiatric disorder, we demonstrate the need for regular screening/inquiry by healthcare providers regarding mental health status, as well as a reliable network of mental health resources for patients with IBD. Recommendations regarding how to best mitigate the inconsistencies in mental health diagnoses and its bidirectional nature suggest that physicians become familiar both with appropriate mental health providers and SSRIs/SNRIs that could help treat their patients.16 Antidepressants may provide additional benefits to IBD course, and have been shown to effectively treat gastrointestinal symptoms in other disorders.17,18 The proportions of patients previously undiagnosed for anxiety and depression point to a gap in the care of patients with IBD and lack of consistent screening for psychiatric comorbidities. Without regular screening for these comorbidities, it remains unlikely that patients are receiving appropriate psychological or psychiatric treatment.
Our findings highlight a disparity in mental health screening of patients with IBD. Without proper screening mechanisms, patients remain undiagnosed (and therefore untreated) for comorbid mental health conditions. We suggest regular screening for patients with IBD, particularly those with active disease. Additionally, we recommend the incorporation of an IBD specific psychologist into clinic settings. Such a resource would help manage screening and assist in referring patients to appropriate psychologists and psychiatrists.
Given the need for regular mental health screenings in patients with IBD, our study demonstrated the utility and ease of using the CAT-MH. All patients received the same 4 modules screening for depression (CAT-DI), major depressive disorder (CAT-MDD), anxiety (CAT-ANX), and suicidality (C-SSRS) resulting in a median completion time of 3.5 minutes. The median completion time is comparable with other studies that used the CAT-DI and CAT-ANX.7
Further, this screening illustrated the positive association between clinically active disease status and the presence of depression and anxiety. The influence of clinically active disease upon mental health conditions was not surprising to us, given the detrimental effects IBD can have on HRQoL in many patients. Previous studies have, for instance, correlated decreased physical activity and sleep quality with active IBD.19 Additionally, recent research has indicated that active patients have a greater risk for depression and anxiety, presenting similar rates of depression and anxiety in an IBD population as found in this study.20 Untreated psychiatric comorbidities could worsen disease outcomes or lead to lower medication and appointment compliance in this subset of patients.2
Moreover, after adjusting for covariates, we found that patients with a history of IBD-related surgery were more likely to have depression. These results are consistent with previously reported work that showed that nondepressed patients with CD who underwent surgery were more likely to develop depression compared to patients who did not. This association was not seen for anxiety.21 We also found that patients with UC were less likely to screen positive for anxiety when compared to patients with CD. However, only 3 patients with UC screened positive for anxiety so it is unclear if this association could be attributed to our small sample size.
Despite our pretest hypotheses that factors such as number of previous surgeries and number of discontinued medications would correlate positively with depression and anxiety severity, we did not identify these factors as significant. We presumed that these variables could cause large amounts of stress and inconvenience upon patients, thus decreasing HRQoL and exacerbating mental health conditions.
Limitations of the study include small sample size and lack of biomarker results within 6 months of survey administration. Additionally, the senior author’s blinded determination of each patient’s disease status could have inadvertently been influenced by his previous knowledge of patients’ health histories. Though the CAT-MH has not previously been used in an IBD population which posed unique challenges and potential limitations in conceptualizing this study, this methodology however had been utilized in a primary care setting and among perinatal women.22,23
Previous studies validating use of the CAT-MH test in primary healthcare settings present lower rates of depression and anxiety than seen in the IBD population, and a compliance rate of 40% when surveys are administered via a patient portal.22,24 Our results therefore not only reinforce the utility of using the CAT-MH in a tertiary care center, but also highlight the heightened prevalence of depression and anxiety among patients with IBD. The CAT-MH is particularly well suited for the IBD population due to its increased precision, shorter administration times resulting in decreased patient burden, decreased need for clinician involvement, and feasibility of administration in and out of a clinical setting.10 Increased rates of mental health comorbidities in patients with IBD align with previous findings. Furthermore, findings of increased prevalence of depression and anxiety in patients with active disease are consistent with prior research.25
Given these findings, we propose that further research should explore the biological mechanisms and influence between disease activity and associated mental health conditions. The analysis of physiological markers inflammation, depression, and anxiety has been explored, and may be able to now be clinically correlated. For instance, exploring the avenue of serotonin synthesis, which primarily occurs in the gut, could provide insight into factors driving the seemingly interconnected relationship between IBD and depression and anxiety.26
CONCLUSIONS
We demonstrate the prevalence of previously undiagnosed psychiatric comorbidities in patients with IBD, as well as the positive association between clinically active disease status and the presence of depression and anxiety using a novel mental health adaptive testing technology. Many patients with IBD have undiagnosed mental health disorders and may be at risk for significantly impacted quality of life or other poor outcomes. Rapid and efficient screening tools such as the 1 studied here are needed in order to better apply current guidelines for the IBD population. In particular, our results suggest that physicians should consider patients with clinically active IBD at risk for depression and anxiety and treat or refer them accordingly.
ACKNOWLEDGMENTS
The authors would like to acknowledge 2 psychologists (Shona Vas, PhD, and Nancy J. Beckman, PhD) for recommending resources for this study.
Funding: This research is supported by generous gifts from the Gastro-Intestinal Research Foundation of Chicago, Jennifer Levine and Jeff Aeder, and Nicholas DiNardi and the Bigger Than Basketball organization.
Conflict of Interest: J.K., T.G.R., C.T., and V.R. have no relevant disclosures. David T. Rubin has no relevant disclosures, but has received grant support from Abbvie, Genentech/Roche, Janssen Pharmaceuticals, Prometheus Laboratories, Shire, and Takeda; and has served as a consultant for Abbvie, Abgenomics, Allergan Inc., Biomica, Boehringer Ingelheim Ltd., Bristol-Myers Squibb, Celgene Corp/Syneos, Check-cap, Dizal Pharmaceuticals, GalenPharma/Atlantica, Genentech/Roche, Gilead Sciences, GlaxoSmithKline Services, Ichnos Sciences S.A., InDex Pharmaceuticals, Janssen Pharmaceuticals, Lilly, Narrow River Mgmt, Pfizer, Prometheus Laboratories, Reistone, Shire, Takeda, and Techlab Inc. Robert Gibbons is a founder of Adaptive Testing Technologies which distributes the CAT-MH suite of tests and has served as an expert witness for the US Department of Justice, Merck, Glaxo-Smith-Kline, Pfizer, and Wyeth pharmaceuticals. The terms of these arrangements have been reviewed and approved by the University of Chicago in accordance with its conflict of interest policies.
Author Contribution: Study concept and design: D.T.R., V.R., and R.D.G. Analysis and interpretation of data: J.K., T.G.R., C.T., V.R., and R.D.G. Drafting of the manuscript: J.K., T.G.R., C.T., V.R., and D.T.R. Critical revision of the manuscript: J.K., T.G.R., C.T., V.R., R.D.G., and D.T.R.
DATA AVAILABILITY
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to information contained within that could compromise the privacy of research participants.
REFERENCES
- 1. Zhang CK, Hewett J, Hemming J, et al. The influence of depression on quality of life in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2013;19:1732–1739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nigro G, Angelini G, Grosso SB, et al. Psychiatric predictors of noncompliance in inflammatory bowel disease: psychiatry and compliance. J Clin Gastroenterol. 2001;32:66–68. [DOI] [PubMed] [Google Scholar]
- 3. Bernstein CN. Addressing mental health in persons with IBD. J Can Assoc Gastroenterol. 2018;1:97–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Katon WJ. Epidemiology and treatment of depression in patients with chronic medical illness. Dialogues Clin Neurosci. 2011;13:7–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rubin DT, Ananthakrishnan AN, Siegel CA, et al. ACG clinical guideline: ulcerative colitis in adults. Am J Gastroenterol. 2019;114:384–413. [DOI] [PubMed] [Google Scholar]
- 6. Lichtenstein GR, Loftus EV, Isaacs KL, et al. ACG clinical guideline: management of Crohn’s disease in adults. Am J Gastroenterol. 2018;113:481–517. [DOI] [PubMed] [Google Scholar]
- 7. Achtyes ED, Halstead S, Smart L, et al. Validation of computerized adaptive testing in an outpatient nonacademic setting: the VOCATIONS trial. Psychiatr Serv. 2015;66:1091–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gibbons RD, Weiss DJ, Pilkonis PA, et al. Development of a computerized adaptive test for depression. Arch Gen Psychiatry. 2012;69:1104–1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gibbons RD, Weiss DJ, Pilkonis PA, et al. Development of the CAT-ANX: a computerized adaptive test for anxiety. Am J Psychiatry. 2014;171:187–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gibbons RD, Weiss DJ, Frank E, et al. Computerized adaptive diagnosis and testing of mental health disorders. Annu Rev Clin Psychol. 2016;12:83–104. [DOI] [PubMed] [Google Scholar]
- 11. Gibbons RD, Hooker G, Finkelman MD, et al. The computerized adaptive diagnostic test for major depressive disorder (CAD-MDD): a screening tool for depression. J Clin Psychiatry. 2013;74:669–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mundt JC, Greist JH, Jefferson JW, et al. Prediction of suicidal behavior in clinical research by lifetime suicidal ideation and behavior ascertained by the electronic Columbia-Suicide Severity Rating Scale. J Clin Psychiatry. 2013;74:887–893. [DOI] [PubMed] [Google Scholar]
- 13. Franchimont D. C-reactive protein: informative or misleading marker of Crohn’s disease? Inflamm Bowel Dis. 2007;13:501–502. [DOI] [PubMed] [Google Scholar]
- 14. Lewis K, Marrie RA, Bernstein CN, et al. ; CIHR Team in Defining the Burden and Managing the Effects of Immune-Mediated Inflammatory Disease . The prevalence and risk factors of undiagnosed depression and anxiety disorders among patients with inflammatory bowel disease. Inflamm Bowel Dis. 2019;25:1674–1680. [DOI] [PubMed] [Google Scholar]
- 15. Altemus M, Sarvaiya N, Neill Epperson C. Sex differences in anxiety and depression clinical perspectives. Front Neuroendocrinol. 2014;35:320–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Keefer L, Kane SV. Considering the bidirectional pathways between depression and IBD: recommendations for comprehensive IBD care. Gastroenterol Hepatol (N Y). 2017;13:164–169. [PMC free article] [PubMed] [Google Scholar]
- 17. Weaver E, Szigethy E. Managing pain and psychosocial care in IBD: a primer for the practicing gastroenterologist. Curr Gastroenterol Rep. 2020;22:20. [DOI] [PubMed] [Google Scholar]
- 18. Macer BJ, Prady SL, Mikocka-Walus A. Antidepressants in inflammatory bowel disease: a systematic review. Inflamm Bowel Dis. 2017;23:534–550. [DOI] [PubMed] [Google Scholar]
- 19. Andersen M, Yvellez O, El Jurdi K, et al. Simplification of validated patient reported outcome instruments in inflammatory bowel disease.Crohns Colitis 360. 2019;1(3):otz043. [Google Scholar]
- 20. Byrne G, Rosenfeld G, Leung Y, et al. Prevalence of anxiety and depression in patients with inflammatory bowel disease. Can J Gastroenterol Hepatol. 2017;2017:6496727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ananthakrishnan AN, Gainer VS, Cai T, et al. Similar risk of depression and anxiety following surgery or hospitalization for Crohn’s disease and ulcerative colitis. Am J Gastroenterol. 2013;108:594–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Graham AK, Minc A, Staab E, et al. Validation of the computerized adaptive test for mental health in primary care. Ann Fam Med. 2019;17:23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kim JJ, Silver RK, Elue R, et al. The experience of depression, anxiety, and mania among perinatal women. Arch Womens Ment Health. 2016;19:883–890. [DOI] [PubMed] [Google Scholar]
- 24. Franco M, Staab EM, Zhu M, et al. Effectiveness of population-level depression screening via a patient portal: the Portal-depression study. Presented at Midwest Society of General Internal Medicine. 2020. [Google Scholar]
- 25. Neuendorf R, Harding A, Stello N, et al. Depression and anxiety in patients with inflammatory bowel disease: a systematic review. J Psychosom Res. 2016;87:70–80. [DOI] [PubMed] [Google Scholar]
- 26. Sofia MA, Ciorba MA, Meckel K, et al. Tryptophan metabolism through the Kynurenine pathway is associated with endoscopic inflammation in ulcerative colitis. Inflamm Bowel Dis. 2018;24:1471–1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to information contained within that could compromise the privacy of research participants.