Graphical abstract
Keywords: SARS-CoV-2, Serology, Antibodies, COVID-19, IgA
To the editor
Serum antibodies are an important pillar of the immune response to the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. With earlier data, we have shown that SARS-CoV-2 IgG and IgA antibody responses are both, gender dependent and characterized by a declining antibody concentration early on1. We can now show that antibodies, especially against spike protein (S), remain detectable for more than one year in most persons after PCR confirmed mild to moderate COVID-19, despite the fact that a relevant decline can be observed. We here present the extended longitudinal profile of IgG and IgA against S and of IgG against nucleocapsid protein (N) for more than one year (the cohort was initiated during the first infection wave in Switzerland in March 2020).
The study includes outpatients with a history of positive SARS-CoV-2 PCR, i.e. a mild to moderate disease course. The total cohort comprises 278 individuals (12.0–91.2 years, median = 51.2, IQR = 25.8; 59.5% females), of which 53 (24.8–91.2 years, median = 55.8, IQR = 13.9; 41% females) were followed for 14 months (supplementary Table 1). The study is registered in the Swiss COVID-19 database (https://swissethics.ch/covid-19/approved-projects; K2) and was approved by the regional ethics committee (ID2020–00,941). PCR analysis of stool and nasopharyngeal swabs were performed together with blood draws every week in a first month and then after another four weeks in the second month; this course was repeated if patients consented. All SARS-CoV-2 ELISA (anti-S IgG and IgA, Euroimmun, Lübeck, Germany; anti-N IgG, Epitope Diagnostics, San Diego, USA) were run on an automated DSX ELISA processor (Dynex Technologies) according to the recommendations of the manufacturers. We defined an OD ratio of 11 (anti-S IgG) or 9 (anti-S IgA) as the upper threshold of the dynamic range, since the assays saturate above these points2. Statistical definitions, analysis and visualizations were based on or performed with software R using the implemented statistical tests and the packages “tidyverse” and “ggplot2”3.
During the initial 4 months after a positive PCR result, 94.2% of participants showed quantifiable evidence of seroconversion, while 5.8% did not (Fig. 1 A–C). Upon their first visit (median 6 weeks after positive PCR; 95% CI 0.43 weeks) 11.9% (33 / 278), 21.6% (60 / 278) and 24.5% (68 / 278) had not developed measurable anti-S IgG, anti-S IgA or anti-N IgG, respectively. Furthermore, 66.9% of participants displayed quantifiable antibody concentrations for all three entities evaluated. Remarkably, all long-term sub cohort participants presented at least one quantifiable antibody entity at all time points until their last visit, while only 49% showed quantifiable antibody concentrations in all three entities. Note that study participants with no initially detectable antibodies against SARS-CoV-2 (5.8%) did not participate in the long-term sub cohort.
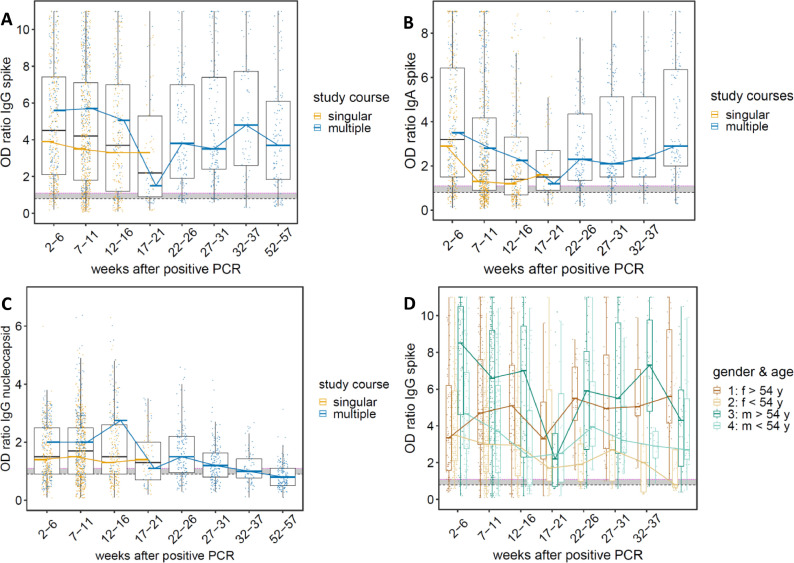
Fig. 1.
Overall dynamic changes in anti-SARS-CoV-2 antibody levels (IgG and IgA) over time. Results were grouped according to the time after positive PCR diagnosis: 2–6 weeks (n = 408, 21.3%), 7–11 weeks (n = 690, 36.0%), 12–16 weeks (n = 257, 13.4%), 17–21 weeks (n = 73, 3.8%), 22–26 weeks (n = 143, 7.5%), 27–31 weeks (n = 156, 8.1%), 32–37 weeks (n = 72, 3.8%) and 52–57 weeks (n = 119, 6.2%). Horizontal bold lines indicate median values; boxes indicate quartiles 1 and 3; whiskers indicate 1.5 * IQR confidence intervals; dotted magenta line indicate optical density (OD) ratio at 1.1 (positive cut-off); dotted black line indicate OD ratio at 0.8 for anti-S antibodies, 0.9 for anti-N IgG (values below are considered negative); gray shaded region in-between OD ratio 0.8/0.9–1.1 contains borderline results. Black line represents all individuals, independent of the number of study courses. Yellow dots and line represent individuals performing a singular study course (1–5 longitudinal blood draws) and blue dots and line represent individuals with multiple study courses (1–15 longitudinal blood draws). Each point represents a single measurement. (A) anti-spike (S) IgG; (B) anti-S IgA; (C) anti-nucleocapsid (N) IgG; (D) Gender and age specific dynamic changes in anti-S IgG antibody levels over time. 1 = female individuals with age higher than 54 years; 2 = female individuals with age lower than 54 years; 3 = male individuals with age higher than 54 years; 4 = male individuals with age lower than 54 years.
The statistically significant gender-associated difference in the antibody concentrations observed earlier persist for the first 3 months; thereafter, gender-associated differences are no longer observed1. In addition, a significant (p < 2.1e–08) age dependent difference in antibody concentrations becomes apparent at weeks 22 to 26 (Fig. 1D). Individuals younger than 54 years of age tend to show lower antibody concentrations than their older counterparts; this was also observed in other studies4.
While antibody concentrations may have complex kinetics5, we categorized the anti-S antibody longitudinal courses based on the slope of the robust regression line (Fig. 2 ). We identified two statistically distinctive patterns of antibody dynamics for anti-S IgG and IgA: declining antibody concentrations (decrease of anti-S IgG levels, average slope: −0.045 (±0.037) OD ratio/week, n = 47; decrease of anti-S IgA levels, average slope: −0.032 (±0.052) OD ratio/week, n = 19) and increasing antibody concentrations (increase of anti-S IgG levels, average slope: +0.029 (±0.020) OD ratio/week, n = 6; increase of anti-S IgA levels, average slope: +0.053 (±0.066) OD ratio/week, n = 34).
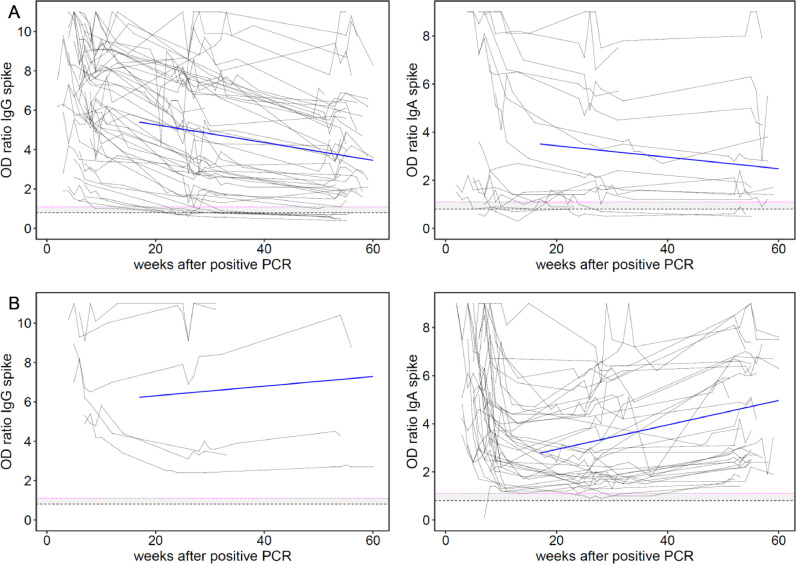
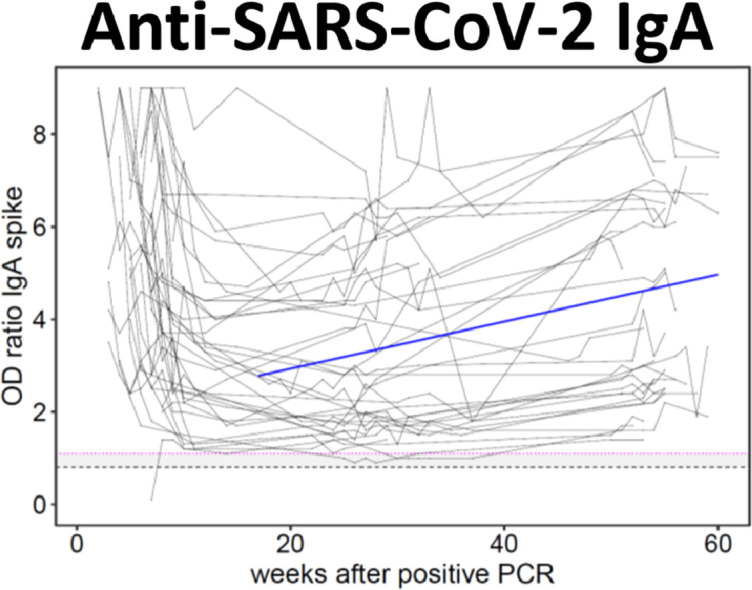
Fig. 2.
Longitudinal courses of individual anti-SARS-CoV-2 antibody levels (IgG and IgA) over time. Individual longitudinal anti-spike IgG and anti-spike IgA courses were analyzed utilizing robust regression (period week 17–57) using an MM estimator, which is an M-estimation with Turkey's biweight initialized by a specific S-estimator. The corresponding slopes were categorized according to the following properties of their individual course: Declining antibody concentrations were defined by a negative slope value (slope < 0 OD ratio/week); increasing antibody concentrations were defined by a positive slope value (slope > 0 OD ratio/week). Blue line represents an illustrative line indicating the averaged present slope calculated by the robust regression of data from week 17 to 57; dotted magenta line indicate optical density (OD) ratio at 1.1 (positive cut-off); dotted black line indicate OD ratio of 0.8 (values below are considered negative); gray shaded region in-between OD ratio 0.8–1.1 contains borderline results. Each point represents a single measurement. (A) anti-spike IgG (n = 47, 89%) and IgA (n = 19, 36%) antibody levels with declining tendency. (B) anti-spike IgG (n = 6, 11%) and IgA (n = 34, 64%) antibody levels with increasing tendency.
The majority (89%) of the long-term sub cohort showed declining anti-S IgG antibody concentrations, while a small subgroup (11%) showed increasing antibody concentrations over time (Fig. 2B). An even higher proportion of increasing antibody concentrations was observed with the individual courses of anti-S IgA antibodies (36% declining and 64% increasing antibody concentrations). As there are substantially more individual anti-S IgA increases than decreases, this might indicate an underlying mechanism of IgA stimulation. The detection of SARS-CoV-2 material in some stool samples early during the observation period might be hinting at such a stimulatory exposure (supplementary Table 2). Considering all results of our observation, one might therefore conclude that IgA antibodies might provide a more persistent and more stable defense against SARS-CoV-2 than IgG6 , 7.
According to the current understanding, one would have to expect a continuous decrease in antibody concentration - in the absence of the antigen - after an initial increase5. Our current data, however, describe a secondary increase in anti-spike IgG in a few and in IgA in many more patients. If this increase was due to re-infection, a much steeper increase (i.e. a booster response) could be expected to be observed, at least temporarily8. In addition, nasopharyngeal swabs and stool samples for PCR testing were taken at every visit, but none of them were found to be positive in any of the individuals within the long-term sub-cohort; obviously, this observation does not allow to rule out a potential re-infection or re-exposure during the observation period with certainty. However, it seems at least to rule out persistence of a high viral load in the nasopharynx and the gut within this group. But even non-detectable persistence of virus particles might have provided sufficient antigen to induce the observed response, preventing waning of antibodies. This would be compatible with findings of coronavirus particles in the small bowel of covalescent study participants or durable antigen presentation on follicular dendritic cells9 , 10. The observed IgA antibody increase over time might indicate a state of chronic infection5 and may help to understand how our immune system copes with this virus.
Funding
This work was supported by the Center for Laboratory Medicine, the Swiss Federal Laboratories for Materials Science and Technology St. Gallen (Empa) and the Canton of St. Gallen.
Declaration of Competing Interest
The authors declare that they have no competing interests.
Acknowledgments
We thank all the participants who agreed to participate in this study as well as the physicians, nurses and members from Polipraxis in St. Gallen, Praxis Seidenbaum in Trübbach and the outpatient clinic of the Center for Laboratory Medicine in St. Gallen, Switzerland.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jinf.2021.11.001.
Appendix. Supplementary materials
References
- 1.Korte W., Buljan M., Rösslein M., Wick P., Golubov V., Jentsch J., et al. SARS-CoV-2 IgG and IgA antibody response is gender dependent; and IgG antibodies rapidly decline early on. J Infect. 2021;82(1):e11–ee4. doi: 10.1016/j.jinf.2020.08.032. JanPubMed PMID: 32853597. Pubmed Central PMCID: PMC7445467. Epub 2020/08/28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Manisty C., Treibel T.A., Jensen M., Semper A., Joy G., Gupta R.K., et al. Time series analysis and mechanistic modelling of heterogeneity and sero-reversion in antibody responses to mild SARS‑CoV-2 infection. EBioMedicine. 2021;65 doi: 10.1016/j.ebiom.2021.103259. MarPubMed PMID: 33662833. Pubmed Central PMCID: PMC7920816. Epub 2021/03/05. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wickham M.A.H., Bryan J., Chang W., McGowan L.D.A., François R., Grolemund G., et al. Welcome to the tidyverse. J Open Source Softw. 2019;4(43):1686. [Google Scholar]
- 4.Laing E.D., Epsi N.J., Richard S.A., Samuels E.C., Wang W., Vassell R., et al. medRxiv; 2021. SARS-CoV-2 antibodies remain detectable 12 months after infection and antibody magnitude is associated with age and COVID-19 severity. 2021.04.27.21256207. [Google Scholar]
- 5.Amanna I.J., Slifka M.K. Mechanisms that determine plasma cell lifespan and the duration of humoral immunity. Immunol Rev. 2010;236(1):125–138. doi: 10.1111/j.1600-065X.2010.00912.x. JulPubMed PMID: 20636813. Pubmed Central PMCID: PMC7165522. Epub 2010/07/20. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dispinseri S., Secchi M., Pirillo M.F., Tolazzi M., Borghi M., Brigatti C., et al. Neutralizing antibody responses to SARS-CoV-2 in symptomatic COVID-19 is persistent and critical for survival. Nat Commun. 2021;12(1):2670. doi: 10.1038/s41467-021-22958-8. 2021/05/11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sterlin D., Mathian A., Miyara M., Mohr A., Anna F., Claër L., et al. IgA dominates the early neutralizing antibody response to SARS-CoV-2. Sci Transl Med. 2021;13(577):eabd2223. doi: 10.1126/scitranslmed.abd2223. Jan 20PubMed PMID: 33288662. Pubmed Central PMCID: PMC7857408. Epub 2020/12/09. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brehm T.T., Pfefferle S., von Possel R., Kobbe R., Nörz D., Schmiedel S., et al. SARS-CoV-2 reinfection in a healthcare worker despite the presence of detectable neutralizing antibodies. Viruses. 2021;13(4):661. doi: 10.3390/v13040661. PubMed PMID. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gaebler C., Wang Z., Lorenzi J.C.C., Muecksch F., Finkin S., Tokuyama M., et al. Evolution of antibody immunity to SARS-CoV-2. Nature. 2021;591(7851):639–644. doi: 10.1038/s41586-021-03207-w. MarPubMed PMID: 33461210. Epub 2021/01/19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sui Y., Li J., Zhang R., Prabhu S.K., Andersen H., Venzon D., et al. Protection against SARS-CoV-2 infection by a mucosal vaccine in rhesus macaques. JCI Insight. 2021;6(10) doi: 10.1172/jci.insight.148494. PubMed PMID: 33908897. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.