Abstract
Objective:
Sexual and gender minority youth experience disparities in suicidal thoughts and behaviors, yet little is known about how to predict future attempts or transitions from suicidal thoughts to behaviors. Additionally, adaptive measurement of psychopathology is a promising approach that may help characterize risk in this population. The authors sought to examine the validity of the Computer Adaptive Test for Suicide Scale (CAT-SS) in predicting suicide attempts and in predicting the transition from suicide ideation to attempt.
Methods:
The CAT-SS was administered to participants of two ongoing cohort studies of sexual and gender minority adolescents and young adults (N=1,006). Survival analyses examined longitudinal associations between CAT-SS and time to suicide attempt. Analyses were conducted for the full sample and stratified by history of suicide ideation, with comparisons between adaptive and static measures of depressive symptoms.
Results:
The CAT-SS predicted future suicide attempts in the overall sample (HR = 1.34, 95% CI: 1.03–1.74). Social support reduced risk for attempts among youth without a history of ideation (HR = 0.66, 95% CI: 0.45–0.96). Among youth with a history of ideation, predictors of the transition from suicidal thoughts to suicide attempts included baseline CAT-SS score (HR = 1.51, 95% CIs: 1.06–2.15) and victimization (HR = 2.48, 95% CI: 1.10–5.59).
Conclusions:
Risk and protective factors for suicide attempts differed between youth with and without a history of suicidal thoughts. The CAT-SS demonstrated validity in predicting future risk for the sample overall and for youth with suicide ideation specifically.
Introduction
Youth suicide has increased in recent years and is a global health priority (1–3). Available evidence indicates that sexual and gender minority youth (SGMY) are more likely to consider, attempt, and die by suicide than heterosexual and cisgender youth (4–9). Due to a paucity of longitudinal research, little is known about why some SGMY attempt suicide whereas most do not (10,11). Despite persistence of these disparities, there are no well-established interventions tailored for this population (12,13). Prospective research is urgently needed in order to develop strategies to predict and prevent suicide attempts among SGMY (14,15).
Several recent advances inform future directions in establishing an evidence base for addressing suicidality among SGMY. First, developing methods for screening – the proactive identification of youth experiencing suicidality – is crucial (16,17). Correlates of suicidal behavior are more prevalent among SGMY, which may lead to different overall risk profiles (18–21). Novel electronically delivered health interventions to address SGM health disparities have demonstrated efficacy, feasibility, and acceptability (22,23). Evaluating available screening tools, particularly those that can be delivered electronically, in this population will inform efforts to identify SGMY at high risk and facilitate linkage to intervention.
Second, ascertaining factors that predict transitions from suicide ideation (SI) to behaviors can clarify targets for intervention (24,25). Predicting suicide attempts among youth is challenging, and this is especially the case for SGMY specifically (4,26). However, research in youth suicide risk screening indicates that a combination of mood and alcohol/substance use disorder symptoms is effective at identifying youth at risk, and may be informative in predicting SGMY risk (17). Additionally, the ability to identify within-person factors associated with transitions in risk can inform our understanding of the naturalistic course of suicidality, effectiveness of screening strategies, and individualization of interventions (27,28). To date, only three published studies have examined suicidality in SGMY longitudinally (29–31). Nevertheless, these studies were consistent in findings that attempt history and SI severity were better predictors than previously examined SGM-specific factors (e.g., child gender nonconformity). Thus, characterizing suicidality specifically is likely to aid in predicting risk transitions. Additionally, interpersonal factors such as SGM-related victimization and perceived social support are associated with retrospective reports of suicide attempt history and prospectively with changes in suicidal thoughts (29,32). As such, their role in suicide risk transitions should be explored further.
Third, computerized adaptive testing (CAT) provides advantages over standard approaches to mental health assessments (33,34). For instance, structured interviews have good predictive validity but are subject to clinical judgment and require administration by trained interviewers (35). Self-report measures can be administered in a wide range of settings but have modest predictive validity (36–38). Both methods often require the administration of a large number of items from static item banks and screening batteries. In contrast, CAT allows the number and sequencing of items to vary as a function of participants’ previous responses, facilitating personalized assessment with a high degree of accuracy for a range of mental health conditions including major depressive disorder (MDD) (39,40). The recently developed Computerized Adaptive Test for Suicide Scale (CAT-SS) has demonstrated convergent validity with structured clinical interviews, and may improve risk formulation (41).
The aims of this study were two-fold. First, we sought to identify risk and protective factors for transitions from suicidal thoughts to behavior among SGMY. Second, we examined the predictive validity of CAT-SS when controlling for other risk and protective factors.
METHODS
Sample
Data were drawn from two ongoing accelerated cohort studies of SGMY residing in Chicago, with both youth assigned male at birth (RADAR; current N = 1,153) and female at birth (FAB 400; current N = 488). The eligibility criteria and recruitment procedures of these studies have been described previously (42,43). Informed consent was obtained from all participants at the time of enrollment. All study procedures were IRB-approved. Participants in these studies (n=1,072; 65.3%) completed CAT measures at one visit between January 2018 and July 2018 (subsequently referred to as “baseline”). The majority of these participants completed at least one follow-up visit (n=1,006; 93.8%). The number of follow-up visits after CAT administration varied across participants (median = 3, range: 1–4 visits). Participants without follow-up data did not differ from the analytic sample in age, race/ethnicity, gender, or sexual orientation. Suicidality was measured at all follow-up visits conducted over 16.5±3.7 months (range = 6–24 months). Participants reported a mean±SD age of 20.7±3.2 years, with most identifying as cisgender (n=841; 83.6%) and with a non-monosexual sexual orientation (n=522; 51.9%). The racial/ethnic distribution was as follows: Black (n=354; 35.2%), Latinx (n=294; 29.2%), White (n=237; 23.6%), Other (n=121; 12.0%).
Measures
Suicidality.
Participants completed items from the Youth Risk Behavior Survey to assess suicidality. Suicide ideation was assessed using the question “During the past 6 months, did you ever seriously consider attempting suicide?” Attempts were assessed using the question “During the past 6 months, how many times did you actually attempt suicide?” Response options were measured on an ordinal frequency scale: 0 times, 1 time, 2 or 3 times, 4 or 5 times, and 6 or more times. These items have demonstrated good convergent and discriminant validity as well as test-retest reliability (44,45).
Computerized Adaptive Test – Suicide Scale (CAT-SS).
Participants completed the CAT-SS as a measure of recent suicide risk. The CAT-SS was developed using multidimensional item response theory methods in a sample of psychiatric patients and subsequently validated in a sample of emergency department patients. The item bank of 111 items was developed from an initial pool of 1,008 items assessing the domains of anxiety, depression, and mania (including 11 items directly assessing suicidal ideation). With an item bank that assesses multiple domains of impairment, participants completing the CAT-SS will receive prompts that can vary in how directly they inquire about suicidality. Examples of suicidality-specific items include “My life lacked meaning and purpose” and “Did you think about taking your own life?” With a mean of 10 adaptively administered items, the CAT-SS can accurately measure suicide risk in approximately 2 minutes. Scores range from 0 to 100, with higher scores indicating more severe suicide risk. The CAT-SS has demonstrated convergent validity with clinician-administered assessment of suicidality, the Columbia-Suicide Severity Rating Scale (41,46).
Computerized Adaptive Diagnostic Test for Major Depressive Disorder (CAD-MDD).
The CAD-MDD is a computerized adaptive test used to screen for the presence of MDD (39). Respondents are presented with questions drawn from an item bank of 88 items that map onto domains assessed in the diagnosis of MDD: negative affect, anhedonia, sleep disturbance, weight fluctuation, psychomotor changes, fatigue, negative self-perception, concentration impairment, and suicidality. The sensitivity and specificity of the CAD-MDD to detect MDD (based on a SCID DSM-5 structured clinical interview) are 0.95 and 0.87, respectively.
Computerized Adaptive Test – Depression Inventory (CAT-DI).
The CAT-DI provides an assessment of depression symptom severity on a 0 to 100 point scale (40). Items are drawn from an item bank of 389 items assessing domains of MDD. In prior studies, the CAT-DI has demonstrated convergent validity with clinician-administered structured diagnostic interviews with a sensitivity of 0.92 and specificity of 0.88, and convergent validity with the clinician-rated Hamilton Depression Rating scale of r=0.75.
Depressive Symptoms.
Depression was measured using Patient-Reported Outcomes Measurement Information System (PROMIS) Depression-Short Form 8A (47). This scale measures depressive symptoms in the past week (e.g., negative affect, worthlessness). Responses are rated on a 5-point Likert scale (1 = Never, 5 = Always). Measure reliability is high in both cohorts (RADAR: α = .95; FAB 400: α = .94) (48).
Alcohol Use.
The Alcohol Use Disorder Identification Test (AUDIT) is a 10-item tool that assesses alcohol consumption and related impairment (49). The AUDIT yields a summary score (range: 0–40), with higher scores indicating greater consumption and functional impairment. Consistent with prior studies of suicide risk in this age group, scores of 8 and above were classified as high-risk alcohol use (50,51). This measure has high reliability in these cohorts (RADAR: α = .81; FAB 400: α = .81) (48).
Sexual and Gender Minority-Based Victimization.
A 10-item measure was used to assess SGM-related victimization (52). Participants are asked to report on a 4-point scale (0 = Never, 3 = 3 or more times) how often they experienced verbal and physical threats and assaults in the past 6 months because they “are, or were thought to be, gay, lesbian, bisexual, or transgender.” Measurement reliability is high in these cohorts (RADAR: α = .86; FAB 400: α = .87) (48).
Social Support.
Participants completed the Multidimensional Scale of Perceived Social Support (MSPSS) (53). The measure assesses the extent to which participants receive support from family, friends, and significant others. Respondents rate agreement with items (e.g., “My family really tries to help me”) on a 7-point Likert scale (1 = Very Strongly Disagree, 7 = Very Strongly Agree). The total support subscale was used in the present study and has high reliability (RADAR: α = .88; FAB 400: α = .90) (48).
Statistical Analysis
Primary analyses examined the extent to which baseline characteristics and CAT-SS scores predicted suicide attempts in the overall sample and transitions from suicide ideation to subsequent attempt. Cox proportional hazards regression was used to examine time to suicide attempt at follow-up in the overall sample and in models stratified by baseline history of suicidal ideation. Associations between baseline factors and suicide attempts were examined in bivariate models (i.e., single predictor) and multivariate models (i.e., all predictors). A positive screen for depression on the CAD-MDD was included as a dichotomous variable (positive or negative screen). CAT-SS scores were divided by 10 to increase interpretability in terms of a unit change on a 10 point scale and analyzed as a continuous measure. We also conducted post hoc exploratory analyses to assess whether CAT-SS scores could be used to stratify participants into low and high risk groups. To test this, we used a log-rank test to determine if a score above 5 (50 on the original 100 point scale) distinguished participants with higher risk for attempt. For participants reporting multiple attempts, data were censored following the first attempt. Gender minority status, non-monosexual sexual orientation, and racial/ethnicity were examined as potential covariates but did not alter study findings. In sensitivity analyses, alternate models were examined with depressive symptoms measured with the CAT-DI and the PROMIS-8 (see supplemental tables). Analyses were conducted using Stata 16.
RESULTS
Baseline Characteristics
The characteristics of the overall sample, suicide ideators, and non-ideators at the time of CAT-SS administration are detailed in Table 1. At baseline, 258 participants (25.6%) reported a history of suicide ideation and 73 participants (7.3%) reported a history of suicide attempt. Suicide ideators were more likely to report being assigned female at birth, gender minority status, and non-monosexual sexual orientation and were less likely to report racial minority status. Ideators reported more frequent victimization, more severe depressive symptoms, and higher CAT-SS, as well as less social support.
Table 1.
Sample characteristics.
| Sample | Ideators | Non-Ideators | |||||
|---|---|---|---|---|---|---|---|
| N = 1,006 | n = 258 | n = 748 | |||||
| n | % | n | % | n | % | Group difference | |
| Assigned female at birth | 358 | 35.6 | 123 | 47.7 | 235 | 31.4 | 22.1*** |
| Gender minority | 165 | 16.4 | 66 | 25.6 | 99 | 13.2 | 21.3*** |
| Non-monosexual sexual orientation | 515 | 51.9 | 155 | 61.0 | 360 | 48.8 | 11.3** |
| Age (M±SD) | 20.7 ± 3.2 | 19.8 ± 2.7 | 21.0 ± 3.3 | 5.8* | |||
| Racial/ethnic minority | 769 | 76.4 | 184 | 71.3 | 585 | 78.2 | 5.1* |
| Black | 354 | 35.2 | 75 | 29.1 | 279 | 37.3 | |
| Latinx | 294 | 29.2 | 74 | 28.7 | 220 | 29.4 | |
| White | 237 | 23.6 | 74 | 28.7 | 163 | 21.8 | |
| Other | 121 | 12.0 | 35 | 13.6 | 86 | 11.5 | |
| Suicide plan | 143 | 14.2 | 127 | 49.2 | 16 | 2.1 | 348.8*** |
| Suicide attempt | 73 | 7.3 | 57 | 22.1 | 16 | 2.1 | 113.5*** |
| CAT-SS (M±SD)a | 2.4 ± 1.8 | 3.3 ± 2.0 | 2.0 ± 1.5 | 111.9*** | |||
| CAD-MDD positiveb | 315 | 31.3 | 133 | 51.6 | 182 | 24.3 | 66.1*** |
| CAT-DI (M±SD)c | 3.2 ± 2.2 | 4.3 ± 2.2 | 2.8 ± 2.0 | 100.6*** | |||
| PROMIS-8 (M±SD) d | 14.5 ± 7.4 | 18.6 ± 8.6 | 13.2 ± 6.3 | 116.4*** | |||
| Alcohol use (M±SD)e | 4.5 ± 4.3 | 5.5 ± 4.8 | 4.1 ± 4.0 | 18.9*** | |||
| Heavy alcohol usef | 183 | 18.2 | 66 | 25.6 | 117 | 15.6 | 12.7*** |
| Victimization (M±SD) g | 0.1 ± 0.3 | 0.2 ± 0.4 | 0.1 ± 0.2 | 35.5*** | |||
| Social Support (M±SD) h | 5.1 ± 1.3 | 4.8 ± 1.3 | 5.2 ± 1.3 | 11.1** | |||
Notes. Group difference statistics are from t-tests for continuous variables and Chi-square tests for categorical variables.
p < .10.
p < .05.
p < .01.
Computerized Adaptive Test – Suicide Scale (CAT-SS), range: 1–10, with higher scores indicating more severe suicidality.
Computerized Adaptive Diagnostic – Major Depressive Disorder.
Computerized Adaptive Test – Depression Inventory (CAT-DI), range: 1–10, with higher scores indicating more severe depressive symptoms.
Patient-Reported Outcomes Measurement Information System (PROMIS) Depression–Short Form 8A, range: 8–40, with higher scores indicating more severe depressive symptoms.
Alcohol Use Disorders Identification Test (AUDIT), range: 0–28, with higher scores indicating more severe alcohol use disorder symptoms.
Alcohol Use Disorders Identification Test (AUDIT) score above 7.
LGBT Victimization, range: 0–6, with higher scores indicating higher frequencies of victimization.
Multidimensional Scale of Perceived Social Support (MSPSS), range: 1–7, with higher scores indicating greater perceived social support.
Longitudinal Analysis
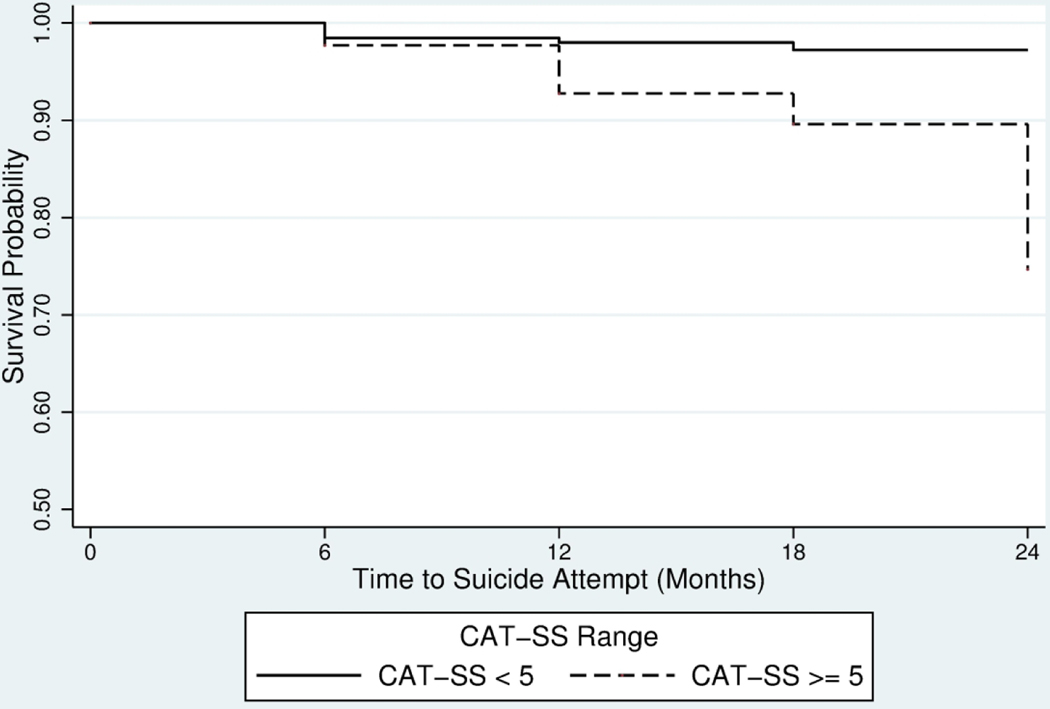
At follow-up, 32 participants reported at least one suicide attempt, with half of attempts occurring in the 6 months after CAT-SS administration. Bivariate associations between study variables and prospectively observed suicide attempts are detailed in Table 2. In the overall sample, all variables except alcohol predicted suicide attempts. Social support attenuated risk for suicide attempt among non-ideators whereas victimization increased risk for suicide attempt among ideators. A CAT-SS score of 5 and above was associated with time to suicide attempt (log-rank test χ2 = 14.94, p < .001; Figure 1). This relationship was attenuated in predicting the transition from suicide ideation to attempt (log-rank test χ2 = 2.86, p = .09; Figure 2).
Table 2.
Hazard ratios for bivariate associations of baseline characteristics with suicide attempt at follow-up.
| Sample | Ideators | Non-Ideators | ||||
|---|---|---|---|---|---|---|
| N = 1,006 | n = 258 | n = 748 | ||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| CAT-SSa | 1.32 | 1.10–1.57** | 1.20 | 0.96–1.51 | 1.13 | 0.81–1.56 |
| CAD-MDD positiveb | 1.91 | 0.95–3.84^ | 1.00 | 0.40–2.47 | 1.95 | 0.64–5.97 |
| CAT-DIc | 1.19 | 1.02–1.39* | 1.10 | 0.89–1.35 | 1.05 | 0.80–1.37 |
| PROMIS-8d | 1.05 | 1.01–1.09* | 1.02 | 0.97–1.07 | 1.04 | 0.97–1.12 |
| Heavy alcohol usee | 1.56 | 0.70–3.47 | 1.85 | 0.73–4.72 | 0.46 | 0.06–3.51 |
| Victimization | 2.67 | 1.41–5.04** | 2.29 | 1.11–4.72* | 1.67 | 0.27–10.53 |
| Social Support | 0.80 | 0.63–1.03^ | 1.03 | 0.73–1.46 | 0.66 | 0.45–0.95* |
Computerized Adaptive Test – Suicide Scale (CAT-SS), range: 1–10, with higher scores indicating more severe suicidality.
Computerized Adaptive Diagnostic – Major Depressive Disorder (CAD-MDD).
Computerized Adaptive Test – Depression Inventory (CAT-DI), range: 1–10, with higher scores indicating more severe depressive symptoms.
Patient-Reported Outcomes Measurement Information System (PROMIS) Depression–Short Form 8A, range: 8–40, with higher scores indicating more severe depressive symptoms.
Alcohol Use Disorders Identification Test (AUDIT) score above 7.
p < .10.
p < .05.
p < .01.
Figure 1.
Kaplan-Meier survival probabilities (time to first suicide attempt) in the overall sample (N=1,006).
Figure 2.
Kaplan-Meier survival probabilities (time to first suicide attempt) for suicide ideators (n=258).
In multivariate analyses, key predictors included CAT-SS score and victimization within the overall sample. Social support was a protective factor for suicide attempts among non-ideators. For suicide ideators, CAT-SS score and victimization predicted transition to suicide attempt. The CAT-SS predicted suicide attempts in the overall sample (HR = 1.34, 95% CI: 1.03–1.74, p < .05; see Table 3). For the CAT-SS, this represents a 34% increase in risk of a suicide attempt for each 10-point change. The CAT-SS also predicted suicide attempts among ideators (HR = 1.51, 95% CIs: 1.06–2.15, p < .05), which represents a 51% increase in risk of transition from suicide ideation to attempt for a 10-point change in score, or up to a five-fold increase in transition risk across the range of the scale. A positive screen for MDD on the CAD-MDD item was not associate with suicide attempts in the overall sample or among non-ideators. There was a modest association with suicide attempts among ideators (HR = 0.29, 95% CI: 0.07–1.18, p = .08). In sensitivity analyses, multivariate models were examined using alternate measures of depressive symptoms. The CAT-DI and PROMIS-8 were not associated with suicide attempts (see Supplemental Tables 1 and 2).
Table 3.
Hazard ratios for multivariate associations of baseline characteristics with suicide attempt at follow-up, with the CAD-MDD screen for depression.
| Sample | Ideators | Non-Ideators | ||||
|---|---|---|---|---|---|---|
| N = 1,006 | n = 258 | n = 748 | ||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| CAT-SSa | 1.34 | 1.03–1.74* | 1.51 | 1.06–2.15* | 0.91 | 0.57–1.45 |
| CAD-MDD positiveb | 0.71 | 0.25–1.98 | 0.29 | 0.07–1.18^ | 2.39 | 0.45–12.69 |
| Heavy alcohol usec | 1.21 | 0.54–2.75 | 1.53 | 0.59–3.99 | 0.45 | 0.06–3.47 |
| Victimization | 2.37 | 1.17–4.82* | 2.48 | 1.10–5.59* | 1.39 | 0.23–8.37 |
| Social Support | 0.87 | 0.67–1.14 | 1.12 | 0.78–1.62 | 0.66 | 0.45–0.96* |
Computerized Adaptive Test – Suicide Scale (CAT-SS), range: 1–10, with higher scores indicating more severe suicidality.
Computerized Adaptive Diagnostic – Major Depressive Disorder (CAD-MDD). Reference category is a negative screen.
Alcohol Use Disorders Identification Test (AUDIT) score above 7.
p < .10.
p < .05.
p < .01.
DISCUSSION
This study examined the predictive validity of the CAT-SS for future suicide attempts, for the transition from suicide ideation to attempts in a large sample of SGMY, and in combination with adaptive and static measures of depressive symptoms. Variables evaluated include self-report measures of risk and protective factors as well as a computer adaptive measure of suicidality, the CAT-SS. Three key findings emerged. First, predictors of suicide attempts differed between youth with and without a history of suicide ideation at baseline. Social support was associated with reduced risk among non-ideators whereas victimization predicted transition to attempts among ideators. Second, the CAT-SS demonstrated predictive validity as an individual predictor as well as in combination with other factors for suicide attempts and risk transitions in multivariate models. Third, the CAT-SS predicted suicide attempts regardless of the type of measure of depressive symptoms. Thus, the CAT-SS is a strong predictor of suicide attempts when examined alone or in combination with other risk and protective factors.
Several strengths in this study represent novel contributions to the literature. This study included a large sample and a prospective design. To date, only three studies have examined longitudinal predictors of attempts among SGMY. Stratifying by suicide ideation history revealed factors associated with both increased and reduced risk for attempts. Consistent with prior studies, heavy alcohol use was not a predictor of suicide attempts. Similarly, the predictive effects of depressive symptoms were reduced after accounting for other risk and protective factors. In ancillary analyses, the CAD-MDD was associated with a somewhat higher likelihood of attempting suicide in the overall sample when examined alone but a lower likelihood of transitioning from suicide ideation to attempt in multivariate models. This finding may be reflective of risk profile differences between youth with and without a history of suicide ideation. A positive CAD-MDD screen in the overall sample may be indicative of liability for any suicidality. Among youth with suicide ideation, a positive CAD-MDD screen may reflect particular impairments in domains that can reduce likelihood of engaging in suicidal behavior (e.g., fatigue, sluggishness, hypersomnia). Moreover, the predictive validity of the CAT-SS is encouraging. The CAT-SS appears to predict future suicide attempts, and beyond what is explained by having a history of SI. Additionally, the adaptive means of administration and large item bank allow for indirect assessment of suicidality. This aspect is a notable advantage as direct assessment could underestimate risk for individuals who may have risk that fluctuates over time and individuals who tend to underreport suicidal thoughts. CAT-SS assessments appear to improve the accuracy of the prediction of future suicide attempts, which opens the door to large-scale suicide prevention. Online health interventions for SGMY have demonstrated feasibility and efficacy (22,23). As such, the availability of computerized evidence-based assessment of suicidality can aid in reaching larger numbers of SGMY.
This study’s findings should be interpreted with its limitations in mind. First, the sample was drawn from two cohort studies based in Chicago. Future research should examine the extent to which these findings would replicate in more broadly representative samples. Second, the incidence of suicide attempts within this sample during the follow-up period may have limited statistical power to detect small effects. As hazard ratios were relatively modest (i.e., below 2), it is important to treat these findings as preliminary. Administration of the CAT-SS in large, high-risk samples would provide more definitive tests of the clinical utility of using adaptive assessment. Confidence intervals for some effects were wide (e.g., CAD-MDD, victimization), reflecting the relatively small number of attempts, and may become narrower in studies that include higher risk participants. Studies with longer follow-up periods may also reveal other relevant predictors of transitions from ideation to attempts. Third, we assessed most risk and protective factors using static self-report measures. Results of this and other studies have demonstrated the incremental utility of adaptive measures. Using CAT methods to characterize other mental health domains such as anxiety, posttraumatic stress symptoms, psychosis, and substance use may bolster prediction. Additionally, suicide attempts were measured using items from the YRBS surveys which may underestimate risk. Use of other validated measures would provide more comprehensive assessment of suicidal behavior as an outcome. Future research on the predictive validity of the CAT-SS could compare it with other standardized measures such as the clinician-administered C-SSRS (46). Future studies should explore more longitudinally intensive suicide assessments. The adaptive nature of the CAT-SS and the fact that all of the same questions are not repeatedly administered are advantages that could facilitate highly sensitive and precise ecological momentary assessments (e.g. daily or weekly assessments), which are now possible.
CONCLUSIONS
The results of this study represent important extensions of prior research and suggest directions for future work. This study is the first to conduct a prospective examination of transitions from suicide ideation to attempts among SGMY and demonstrates the predictive validity of the CAT-SS. Longitudinal risk and protective factors have been difficult to identify but results suggest that the salience of factors may differ for youth with a history of suicidal thoughts. Further, adaptive testing methods exhibit predictive validity and should be incorporated into screening and intervention efforts.
Supplementary Material
Highlights:
Authors examined the predictive validity of computer adaptive tests in 1,006 sexual and gender minority participants of two longitudinal cohort studies.
The Computer Adaptive Test for Suicide Scale (CAT-SS) predicted suicide attempts and the transition from suicide ideation to attempt.
Social support reduced risk for suicide attempts among youth without a history of ideation, and victimization predicted transition from suicide ideation to attempt.
These findings demonstrate that the CAT-SS has predictive validity in sexual and gender minority populations and for predicting transitions between suicidal thoughts and behaviors.
Acknowledgements:
Support for this project was provided in part by grants from the National Institute of Child Health and Human Development (R01-HD-086170), National Institute on Drug Abuse (U01-DA-036939), National Heart, Lung, and Blood Institute (R01-HL-137246), and National Institute of Mental Health (R01-MH-100155).
Footnotes
Disclosures: Dr. Gibbons is a founder of Adaptive Testing Technologies, which distributes the CAT-MH suite of computerized adaptive tests. The terms of this arrangement have been reviewed and approved by University of Chicago in accordance with its conflict of interest policies. The other authors report no financial relationships with commercial interests.
REFERENCES
- 1.Bridge JA: Suicide Trends Among Youths Aged 10 to 19 Years in the United States, 1996–2005. JAMA 300: 1025, 2008. [DOI] [PubMed] [Google Scholar]
- 2.Ruch DA, Sheftall AH, Schlagbaum P, et al. : Trends in Suicide Among Youth Aged 10 to 19 Years in the United States, 1975 to 2016. JAMA Netw Open 2: e193886, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Glenn CR, Kleiman EM, Kellerman J, et al. : Annual Research Review: A meta‐analytic review of worldwide suicide rates in adolescents. J Child Psychol Psychiatr 61: 294–308, 2020. [DOI] [PubMed] [Google Scholar]
- 4.Miranda-Mendizábal A, Castellví P, Parés-Badell O, et al. : Sexual orientation and suicidal behaviour in adolescents and young adults: systematic review and meta-analysis. Br J Psychiatry 211: 77–87, 2017. [DOI] [PubMed] [Google Scholar]
- 5.Ream GL: What’s Unique About Lesbian, Gay, Bisexual, and Transgender (LGBT) Youth and Young Adult Suicides? Findings From the National Violent Death Reporting System. Journal of Adolescent Health 64: 602–607, 2019. [DOI] [PubMed] [Google Scholar]
- 6.Valentine SE, Shipherd JC: A systematic review of social stress and mental health among transgender and gender non-conforming people in the United States. Clinical Psychology Review 66: 24–38, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Björkenstam C, Andersson G, Dalman C, et al. : Suicide in married couples in Sweden: Is the risk greater in same-sex couples? Eur J Epidemiol 31: 685–690, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.King CA, Grupp‐Phelan J, Brent D, et al. : Predicting 3‐month risk for adolescent suicide attempts among pediatric emergency department patients. J Child Psychol Psychiatr 60: 1055–1064, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Raifman J, Charlton BM, Arrington-Sanders R, et al. : Sexual Orientation and Suicide Attempt Disparities Among US Adolescents: 2009–2017. Pediatrics 145: e20191658, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haas AP, Eliason M, Mays VM, et al. : Suicide and Suicide Risk in Lesbian, Gay, Bisexual, and Transgender Populations: Review and Recommendations. Journal of Homosexuality 58: 10–51, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cha CB, Tezanos KM, Peros OM, et al. : Accounting for Diversity in Suicide Research: Sampling and Sample Reporting Practices in the United States. Suicide Life Threat Behav 48: 131–139, 2018. [DOI] [PubMed] [Google Scholar]
- 12.Coulter RWS, Egan JE, Kinsky S, et al. : Mental Health, Drug, and Violence Interventions for Sexual/Gender Minorities: A Systematic Review. Pediatrics 144: e20183367, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Glenn CR, Franklin JC, Nock MK: Evidence-based psychosocial treatments for self-injurious thoughts and behaviors in youth. Journal of Clinical Child & Adolescent Psychology 44: 1–29, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mustanski B: Future Directions in Research on Sexual Minority Adolescent Mental, Behavioral, and Sexual Health. Journal of Clinical Child & Adolescent Psychology 44: 204–219, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wolford-Clevenger C, Frantell K, Smith PN, et al. : Correlates of suicide ideation and behaviors among transgender people: A systematic review guided by ideation-to-action theory. Clinical Psychology Review 63: 93–105, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Babeva K, Hughes JL, Asarnow J: Emergency Department Screening for Suicide and Mental Health Risk. Curr Psychiatry Rep 18: 100, 2016. [DOI] [PubMed] [Google Scholar]
- 17.King CA, Arango A, Ewell Foster C: Emerging trends in adolescent suicide prevention research. Current Opinion in Psychology 22: 89–94, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.White Hughto JM, Reisner SL, Pachankis JE: Transgender stigma and health: A critical review of stigma determinants, mechanisms, and interventions. Social Science & Medicine 147: 222–231, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Salway T, Ross LE, Fehr CP, et al. : A Systematic Review and Meta-Analysis of Disparities in the Prevalence of Suicide Ideation and Attempt Among Bisexual Populations. Arch Sex Behav 48: 89–111, 2019. [DOI] [PubMed] [Google Scholar]
- 20.Talley AE, Gilbert PA, Mitchell J, et al. : Addressing gaps on risk and resilience factors for alcohol use outcomes in sexual and gender minority populations: Addressing gaps on risk and resilience factors. Drug and Alcohol Review 35: 484–493, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aromin RA: Substance Abuse Prevention, Assessment, and Treatment for Lesbian, Gay, Bisexual, and Transgender Youth. Pediatric Clinics of North America 63: 1057–1077, 2016. [DOI] [PubMed] [Google Scholar]
- 22.Pachankis JE, Williams SL, Behari K, et al. : Brief online interventions for LGBTQ young adult mental and behavioral health: A randomized controlled trial in a high-stigma, lowr-esource context. Journal of Consulting and Clinical Psychology 88: 429, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mustanski B, Parsons JT, Sullivan PS, et al. : Biomedical and behavioral outcomes of Keep It Up!: An eHealth HIV prevention program RCT. American Journal of Preventive Medicine 55: 151–158, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Klonsky ED, Qiu T, Saffer BY: Recent advances in differentiating suicide attempters from suicide ideators: Current Opinion in Psychiatry 30: 15–20, 2017. [DOI] [PubMed] [Google Scholar]
- 25.Mustanski B, Espelage DL: Why Are We Not Closing the Gap in Suicide Disparities for Sexual Minority Youth? Pediatrics 145: e20194002, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Franklin JC, Ribeiro JD, Fox KR, et al. : Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychological Bulletin 143: 187–232, 2017. [DOI] [PubMed] [Google Scholar]
- 27.Klonsky ED, May AM: the Three-Step Theory (3ST): A new theory of suicide rooted in the “Ideation-to-Action” framework. International Journal of Cognitive Therapy 8: 114–129, 2015. [Google Scholar]
- 28.Mars B, Heron J, Klonsky ED, et al. : Predictors of future suicide attempt among adolescents with suicidal thoughts or non-suicidal self-harm: A population-based birth cohort study. The Lancet Psychiatry 6: 327–337, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mustanski B, Liu RT: A Longitudinal Study of Predictors of Suicide Attempts Among Lesbian, Gay, Bisexual, and Transgender Youth. Arch Sex Behav 42: 437–448, 2013. [DOI] [PubMed] [Google Scholar]
- 30.Smith DM, Wang SB, Carter ML, et al. : Longitudinal predictors of self-injurious thoughts and behaviors in sexual and gender minority adolescents. Journal of Abnormal Psychology 129: 114–121, 2020. [DOI] [PubMed] [Google Scholar]
- 31.Berona J, Horwitz AG, Czyz EK, et al. : Predicting suicidal behavior among lesbian, gay, bisexual, and transgender youth receiving psychiatric emergency services. Journal of Psychiatric Research 122: 64–69, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baams L, Grossman AH, Russell ST: Minority stress and mechanisms of risk for depression and suicidal ideation among lesbian, gay, and bisexual youth. Developmental Psychology 51: 688–696, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gibbons RD, Weiss DJ, Frank E, et al. : Computerized Adaptive Diagnosis and Testing of Mental Health Disorders. Annu Rev Clin Psychol 12: 83–104, 2016. [DOI] [PubMed] [Google Scholar]
- 34.Gibbons RD, deGruy FV: Without Wasting a Word: Extreme Improvements in Efficiency and Accuracy Using Computerized Adaptive Testing for Mental Health Disorders (CAT-MH). Curr Psychiatry Rep 21: 67, 2019. [DOI] [PubMed] [Google Scholar]
- 35.Klonsky ED, May AM, Saffer BY: Suicide, Suicide Attempts, and Suicidal Ideation. Annu Rev Clin Psychol 12: 307–330, 2016. [DOI] [PubMed] [Google Scholar]
- 36.Huth-Bocks AC, Kerr DCR, Ivey AZ, et al. : Assessment of Psychiatrically Hospitalized Suicidal Adolescents. Journal of the American Academy of Child & Adolescent Psychiatry 46: 387–395, 2007. [DOI] [PubMed] [Google Scholar]
- 37.King CA, Jiang Q, Czyz EK, et al. : Suicidal ideation of psychiatrically hospitalized adolescents has one-year predictive validity for suicide attempts in girls only. J Abnorm Child Psychol 42: 467–477, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Large M, Myles N, Myles H, et al. : Suicide risk assessment among psychiatric inpatients: a systematic review and meta-analysis of high-risk categories. Psychol Med 48: 1119–1127, 2018. [DOI] [PubMed] [Google Scholar]
- 39.Gibbons RD, Hooker G, Finkelman MD, et al. : The CAD-MDD: A computerized adaptive diagnostic screening tool for depression. J Clin Psychiatry 74: 669–674, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gibbons RD, Weiss DJ, Pilkonis PA, et al. : Development of a computer adaptive test for depression. Arch Gen Psychiatry 69: 1104, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gibbons RD, Kupfer D, Frank E, et al. : Development of a Computerized Adaptive Test Suicide Scale—The CAT-SS. J Clin Psychiatry 78: 1376–1382, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mustanski B, Morgan E, Janulis P, et al. : Individual and network factors associated with racial disparities in HIV among young men who have sex with men: Results from the RADAR Cohort Study. J Acquir Immune Defic Syndr 80: 7, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Whitton SW, Dyar C, Mustanski B, et al. : Intimate partner violence experiences of sexual and gender minority adolescents and young adults assigned female at birth. Psychology of Women Quarterly 43: 232–249, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.May A, Klonsky ED: Validity of suicidality items from the Youth Risk Behavior Survey in a high school sample. Assessment 18: 379–381, 2011. [DOI] [PubMed] [Google Scholar]
- 45.Brener ND, Collins JL, Kann L, et al. : Reliability of the Youth Risk Behavior Survey Questionnaire. American Journal of Epidemiology 141: 575–580, 1995. [DOI] [PubMed] [Google Scholar]
- 46.Posner K, Brown GK, Stanley B, et al. : The Columbia-Suicide Severity Rating Scale: Initial validity and internal consistency findings from three multisite studies with adolescents and adults. AJP 168: 1266–1277, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pilkonis PA, Choi SW, Reise SP, et al. : Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS®): depression, anxiety, and anger. Assessment 18: 263–283, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Newcomb ME, Hill R, Buehler K, et al. : High burden of mental health problems, substance use, violence, and related psychosocial factors in transgender, non-binary, and gender diverse youth and young adults. Arch Sex Behav 49: 645–659, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Saunders JB, Aasland OG, Babor TF, et al. : Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption-II. Addiction 88: 791–804, 1993. [DOI] [PubMed] [Google Scholar]
- 50.King CA, Eisenberg D, Zheng K, et al. : Online suicide risk screening and intervention with college students: A pilot randomized controlled trial. Journal of Consulting and Clinical Psychology 83: 630–636, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kokotailo PK, Egan J, Gangnon R, et al. : Validity of the Alcohol Use Disorders Identification Test in college students. Alcoholism: Clinical and Experimental Research 28: 914–920, 2004. [DOI] [PubMed] [Google Scholar]
- 52.Mustanski B, Andrews R, Puckett JA: The effects of cumulative victimization on mental health among lesbian, gay, bisexual, and transgender adolescents and young adults. Am J Public Health 106: 527–533, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zimet GD, Powell SS, Farley GK, et al. : Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. Journal of Personality Assessment 55: 610–617, 1990. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.