Abstract
Objective:
To examine the extent to which the genetic and environmental etiology of suicide attempt and suicide death is shared versus unique.
Methods:
The authors used Swedish national registry data for a large cohort of twins, full siblings, and half siblings (N=1,314,990) born 1960-1990 and followed through 2015. They conducted twin-family modeling of suicide attempt and suicide death to estimate heritability for each outcome along with genetic and environmental correlations between them. They further assessed the relationship between suicide attempt by young people versus adults.
Results:
In bivariate models, suicide attempt and death were moderately heritable among both women (Aattempt=0.52 [95% confidence intervals 0.44, 0.56]; Adeath=0.45 [0.39, 0.59]) and men (Aattempt=0.41 [0.38, 0.49]; Adeath=0.44 [0.43, 0.44]). The outcomes were substantially, but incompletely, genetically correlated (rA=0.67 [0.55, 0.67] for women and rA=0.74 [0.63, 0.87] for men). Environmental correlations were weaker (rE=0.36 [0.29, 0.45] for women and rE=0.21 [0.19, 0.27] for men). Heritability of suicide attempt was stronger among people aged 10-24 (A=0.55-0.62) than among adults aged 25 and older (A=0.36-0.38), and the genetic correlation between attempt during youth versus adulthood was stronger for women (rA=0.79 [0.72, 0.79]) than for men (rA=0.39 [0.26, 0.47]).
Conclusions:
The genetic and environmental etiologies of suicide attempt and death are partially overlapping, exhibit modest sex differences, and shift across the life course. These differences must be considered when developing prevention efforts and risk prediction algorithms. Where feasible, suicide attempt and death should be considered separately rather than collapsed, including in the context of gene identification efforts.
Introduction
Suicidal behavior, which includes non-fatal suicide attempts and death by suicide, is a significant public health concern. Suicide accounts for approximately 800,000 deaths per year worldwide (1), and non-fatal attempts are estimated to be up to 30× more common than suicide deaths (2). A prior attempt is one of the most prominent predictors of future death by suicide (3, 4) and 4-7% of individuals with a history of self-harm die by suicide in the ensuing 5-9 years (5, 6). While suicide death is more common among men, women attempt more often (7). Furthermore, while attempts and suicide death share many predictors (8), there is some evidence of differential associations between risk factors with attempt versus death (9). For example, suicide attempts are more common among women and youth, while deaths are more common among men and adults (10). In addition, social isolation and anxiety disorders are associated with suicide attempts more strongly than with death (10). Clarification of common versus distinct contributions to etiology may improve the ability to assess risk and thereby inform prevention and intervention efforts.
Prior studies have revealed familial clustering and a modest to moderate heritable component to suicidal behavior (11–16), including recent efforts to identify specific genetic variants associated with risk (17–19). While many such studies limited their analyses to one outcome (e.g., suicide death), others have collapsed manifestations of suicidality (e.g., ideation, attempt, death) into one variable using inconsistent approaches (20–23). Results from such studies may be driven by only one contributing measure (e.g., ideation), potentially obscuring important differences in the genetic underpinnings of different suicidal outcomes. Twin/family studies with a single outcome of interest have reported heritability estimates of 0.17-0.55 for suicide attempt (24–26) and 0.43 for suicide death (27), though as noted previously (28) limited sample sizes contribute to widely varying heritability rates. Some analyses have been further complicated by sample selection, for example where participants are ascertained on the basis of a prior personal/family history of suicidal behavior (21, 29) or specific psychiatric disorder (17, 23, 30), precluding generalization to the overall population. Notably, Erlangsen et al. (31) found that adjusting for psychiatric comorbidity reduced the SNP-based heritability (h2SNP) of suicide attempt from 0.05 to 0.02. Based on findings from a recent study of suicide attempt within psychiatric disorders, h2SNP also varies as a function of the disorder in question, e.g., from h2SNP=0.03 within major depressive disorder to h2SNP=0.10 within schizophrenia (17). Recent support for classifying suicidal behavior as a distinct mental disorder (32) suggests that viewing suicidal behavior primarily through the lens of psychiatric illness has important limitations.
Efforts to directly compare the etiology of suicide attempt and death are difficult where longitudinal data on both outcomes are not available for a large, representative sample, e.g., when samples are selected as described above. Furthermore, the relatively low prevalence of attempts and, in particular, suicide deaths has impeded efforts to obtain reliable heritability estimates for these outcomes due to inadequate statistical power. In the near term, these constraints mean that molecular genetic studies are unlikely to be able to elucidate shared versus outcome-specific aspects of etiology. Accordingly, it is necessary to employ other methodologic approaches to this important area of research.
Here, we leverage national Swedish registry data, including the recent addition of primary care data, to evaluate the genetic relationship between suicide attempts and death by suicide. While prior reports have employed substantial samples sizes to study familial aggregation of suicidal behavior (11–13), the current study is, to our knowledge, the largest to date that applies formal twin/family modeling, particularly with a goal of estimating genetic and environmental correlations between suicide attempt and death. We previously demonstrated that these outcomes should be treated independently: A liability threshold model, in which attempt and death lie on the same continuum of risk and differ only as a function of severity, does not fit the data well (33).
We expand upon those efforts here, by conducting an extended twin-family model of liability to suicide attempt and death. Our use of nationwide registry data, with a high degree of completeness due to universal healthcare, which yields a representative and statistically powerful sample. Given previous evidence of sex differences in heritability for psychiatric and substance use outcomes (34–36), we also benefit from this large sample by modeling sources of variance separately by sex. The longitudinal nature of the data further enables us to test whether genetic and environmental influences on suicide attempt are stable or dynamic from youth (here, age 10-24) into adulthood (age 25 and older), which may be relevant given shifts in the heritability of both internalizing and externalizing symptoms across the life course (37).
Materials and Methods
Sample
We collected information on individuals from Swedish population-based mortality, inpatient, and outpatient registers (38) with national coverage linking each person’s unique personal identification number which, to preserve confidentiality, Statistics Sweden replaced with a serial number. We secured ethical approval from the Regional Ethical Review Board of Lund University (No. 2008/409, 2012/795, and 2016/679). We double entered all same sex twin pairs with known zygosity and birth years between 1960 and 1990 from the Swedish Twin Registry, and all Swedish-born same sex full- and half-sibling pairs born between 1960 and 1990, and within 5 years of each other, from the Swedish Multi-Generation Register. This cohort was selected to optimize data coverage across time and sample size. An individual could be included several times if he/she had several siblings or different types of siblings; note that this could result in narrowed confidence intervals, but did not substantively impact variance component estimates. Zygosity was assigned using standard self-report items, which, when validated against DNA markers, were 95% to 99% accurate.
Using the Swedish national census and population registers, we assessed cohabitation status for full- and half-sibling pairs as the proportion of possible years they lived in the same household until the oldest turned 16. Among monozygotic (MZ) and dizygotic (DZ) twins and full siblings, we only included pairs reared together for ≥80% of their possible years. Half siblings residing together for ≥80% of the possible years were classified as having been reared together. Those residing together for ≤20% of the possible years were classified as having been reared apart. See below for implications within the twin/family model.
Phenotypes
The following ICD codes were used to identify suicide attempts and deaths of both known and undetermined intent: ICD-8 codes E950-E959, E980-987, ICD-9 codes E950-E959, E980-987, ICD-10 codes X60-X84, Y10-Y34. Details are available through the World Health Organization (39). Distinctions between suicide death and non-fatal attempts, where necessary, were determined using the Cause of Death Register. Prior studies have provided support for the inclusion of events of undetermined intent (40, 41), with one reporting that excluding these cases would result in approximately 25% of true suicide attempts being misclassified (41). Suicide attempt and suicide death were treated as binary, and the registration for either outcome (i.e., the date that the ICD code was entered into the medical registry) could occur at any time during the follow-up period, which began when individuals turned 10 and ended in December 2015. Note that an individual could be registered for both suicide attempt and suicide death.
Statistical Analysis
We used classical bivariate twin/sibling modeling, which assumes three sources of liability to non-fatal suicide attempts and death by suicide: additive genetic (A), shared environment (C), and unique environment (E). The model assumes that MZ twins share 100% of their genes; DZ twins and full siblings share, on average, 50% of their genes; while half siblings share, on average, 25% of their genes. The model also assumes that the shared environment, which reflects family and community experiences, is equal between MZ twins, DZ twins, and full siblings, while for half siblings C equaled 1 for pairs reared together and 0 for pairs reared apart. Finally, the unique environment reflects experiences not shared by twins/siblings, random developmental effects, and random measurement error.
The model is based on the idea of an unobserved distribution of liability underlying each of the two binary outcomes, non-fatal suicide attempt and death by suicide. The correlation within each twin/sibling pair corresponds to the proportion of variance explained by the genes (A) and environment (C) they share. The bivariate model was built using the Cholesky decomposition where the first factor loads on both suicide attempts and death by suicide while the second loads only on the latter. Based on results from the univariate ACE models of suicide attempts and death by suicide, we restricted the bivariate model by setting the two C-paths to death by suicide to 0. All analyses were separated by gender. The OpenMx software (42, 43) was used to fit the models.
We conducted a sensitivity analysis in which events of undetermined intent were excluded to account for the possibility that these impacted estimates in the primary analysis. ICD-8 and ICD-9 codes corresponding to events of undetermined intent are E980-E987; for ICD-10, the codes are Y10-Y34. A total of N=18,436 suicide attempts and N=1063 suicide deaths were excluded in these analyses, corresponding to 42.4% and 25.6% of all attempts and deaths, respectively.
In a secondary analysis, we estimated the genetic and environmental correlations between suicide attempt during youth and adulthood, using the World Health Organization’s age range for “young people” – ages 10-24 (44). We selected this age range to capture neurodevelopment of the prefrontal cortex, which persists into the early 20’s (45, 46) and may be particularly relevant to impulsive behavior (47, 48), including suicidality (49). We imposed a restriction on the data to avoid misclassifying persistent suicidal behavior toward the end of the earlier developmental period as “adult”: Those with a suicide attempt at age 24 were censored for one year, such that additional attempts occurring during that year (into age 25) were not counted. Beyond that year-long censoring period, subsequent attempt registrations were classified as adult attempts. We identified N=916 individuals with an attempt at age 24 and within the subsequent year; of these, N=443 had an additional attempt at a later time and were coded as attempting as a young person and an adult, while the remaining N=473 were classified as attempting only as a young person. We lacked sufficient power to conduct a corresponding analysis of suicide death.
Results
Descriptive Statistics
Table 1 provides details on the number of pairs for each relative group (monozygotic or dizygotic twins, full siblings, and half siblings) that contributed to the analyses and corresponding descriptive statistics. The total sample size was N=1,314,990. There were N=21,664 women and N=21,854 men who attempted suicide; N=1048 women and N=3109 men died by suicide. Suicide attempts were more common among women (p<0.0001), while death by suicide was more common among men (p<0.0001). Individuals with half-siblings exhibited higher rates of both suicide attempts and deaths compared to twins or full-siblings.
Table 1.
Descriptive statistics for sibling pairs born in Sweden 1960-1990. Individuals may belong to more than one sibling pair.
| Women | Monozygotic twins | Dizygotic twins | Full siblings | Half siblings reared together | Half siblings reared apart | ||||||||||
| N Pairs | 3,186 | 2,570 | 275,668 | 9,828 | 19,166 | ||||||||||
| % Suicide attempt | 3.2% | 3.5% | 3.7% | 6.5% | 7.1% | ||||||||||
| % Suicide death | 0.2% | 0.2% | 0.2% | 0.4% | 0.4% | ||||||||||
|
| |||||||||||||||
| Median (Q1, Q3) age at suicidal event | Median | Q1 | Q3 | Median | Q1 | Q3 | Median | Q1 | Q3 | Median | Q1 | Q3 | Median | Q1 | Q3 |
| Suicide attempt | 24 | 19 | 32 | 26 | 20 | 35 | 23 | 18 | 31 | 22 | 17 | 30 | 22 | 17 | 32 |
| Suicide death | 39 | 35 | 42 | 26.5 | 20 | 33.5 | 30 | 23 | 39 | 27 | 23 | 34.5 | 28 | 23 | 38 |
|
| |||||||||||||||
| Tetrachoric correlations (95% CI) | |||||||||||||||
| SA between siblings | 0.57 | 0.49; 0.65 | 0.25 | 0.13; 0.27 | 0.28 | 0.27; 0.29 | 0.17 | 0.12; 0.21 | 0.12 | 0.09; 0.15 | |||||
| SD between siblings | n/a | n/a | n/a | n/a | 0.25 | 0.18; 0.32 | n/a | n/a | 0.17 | −0.03; 0.37 | |||||
| Within sibling SA and SD | 0.50 | 0.28; 0.73 | 0.47 | 0.21; 0.73 | 0.52 | 0.50; 0.54 | 0.45 | 0.36; 0.54 | 0.43 | 0.37; 0.50 | |||||
| Between sibling SA and SD | 0.33 | 0.04; 0.61 | 0.21 | −0.15; 0.57 | 0.16 | 0.12; 0.19 | 0.15 | 0.02; 0.27 | 0.01 | −0.09; 0.11 | |||||
|
| |||||||||||||||
| Men | Monozygotic twins | Dizygotic twins | Full siblings | Half siblings reared together | Half siblings reared apart | ||||||||||
| N Pairs | 2,646 | 2,294 | 310,569 | 10,138 | 21,430 | ||||||||||
| % Suicide attempt | 3.2% | 3.0% | 3.4% | 6.5% | 6.3% | ||||||||||
| % Suicide death | 0.3% | 0.4% | 0.5% | 0.9% | 0.9% | ||||||||||
|
| |||||||||||||||
| Median (Q1, Q3) age at suicidal event | Median | Q1 | Q3 | Median | Q1 | Q3 | Median | Q1 | Q3 | Median | Q1 | Q3 | Median | Q1 | Q3 |
| Suicide attempt | 28 | 22 | 35 | 28.5 | 23 | 35 | 26 | 20 | 34 | 26 | 20 | 33 | 26 | 20 | 35 |
| Suicide death | 31 | 26 | 36 | 29.5 | 26 | 39 | 29 | 23 | 37 | 29 | 24 | 38 | 29 | 23 | 37 |
|
| |||||||||||||||
| Tetrachoric correlations (95% CI) | |||||||||||||||
| SA between siblings | 0.41 | 0.30; 0.52 | 0.29 | 0.16; 0.43 | 0.30 | 0.29; 0.31 | 0.19 | 0.15; 0.24 | 0.12 | 0.09; 0.16 | |||||
| SD between siblings | 0.83 | 0.69; 0.96 | n/a | n/a | 0.20 | 0.17; 0.24 | 0.14 | −0.02; 0.30 | 0.12 | 0.01; 0.23 | |||||
| Within sibling SA and SD | 0.45 | 0.25; 0.66 | 0.60 | 0.43; 0.76 | 0.44 | 0.42; 0.45 | 0.36 | 0.29; 0.43 | 0.38 | 0.33; 0.43 | |||||
| Between sibling SA and SD | 0.23 | −0.04; 0.50 | 0.23 | −0.04; 0.51 | 0.15 | 0.13; 0.18 | 0.13 | 0.04; 0.22 | 0.09 | 0.02; 0.15 | |||||
SA=suicide attempt; SD=suicide death; CI=confidence intervals; n/a=cannot be estimated due to sample size).
Among individuals with a prior suicide attempt, 2.1% (N=457) of women and 3.9% (N=846) of men died by suicide during the observation period. Among those who died by suicide, 56.0% (N=581) of women and 72.6% (N=2,250) of men had no known prior attempt. The median (Q1, Q3) time interval between first attempt and suicide death was 4 years (1, 10) for women and 3 (1, 8) for men.
Tetrachoric correlations (used for binary data such as diagnostic status) within and across outcomes, both within individuals and across members of the sibling pairs, are reported in Table 1. In general, correlations were higher for full siblings (including monozygotic and dizygotic twin pairs) than for half siblings, although estimates were imprecise for some correlations. The low prevalence of suicide death prevented us from estimating sibling correlations for some groups. The correlation patterns suggest that genetic factors contribute to resemblance across siblings.
Univariate Twin and Family Models
We first fit standard ACE models for suicide attempt and suicide death separately, stratified by sex. Variance component estimates are presented in Table 2. Heritability estimates (A) were moderate for both outcomes. We observed low but significant contributions from shared environmental factors for suicide attempt but not death, though the latter could be a false negative finding in light of a relatively limited number of suicide deaths. We therefore elected to specify an ACE structure for attempt and an AE structure for suicide death in subsequent models.
Table 2.
Variance components (95% confidence intervals) from univariate and bivariate twin-family modeling results.
| Univariate Analyses | Bivariate Analyses | |||||||
|---|---|---|---|---|---|---|---|---|
| Suicide Attempt | Women Estimate | 95% CI | Men Estimate | 95% CI | Women Estimate | 95% CI | Men Estimate | 95% CI |
| A | 0.50 | 0.42; 0.54 | 0.41 | 0.32; 0.49 | 0.52 | 0.44; 0.56 | 0.41 | 0.38; 0.49 |
| C | 0.03 | 0.01; 0.03 | 0.09 | 0.06; 0.12 | 0.02 | 0.00; 0.06 | 0.09 | 0.09; 0.12 |
| E | 0.47 | 0.43; 0.51 | 0.50 | 0.45; 0.55 | 0.46 | 0.44; 0.46 | 0.50 | 0.50; 0.50 |
|
| ||||||||
| Suicide Death | ||||||||
| A | 0.47 | 0.36; 0.61 | 0.45 | 0.32; 0.53 | 0.45 | 0.39; 0.59 | 0.44 | 0.43; 0.44 |
| C | 0.01 | 0.00; 0.27 | 0.00 | 0.00; 0.06 | - | - | - | - |
| E | 0.52 | 0.39; 0.80 | 0.55 | 0.47; 0.63 | 0.55 | 0.42; 0.67 | 0.56 | 0.50; 0.57 |
A=additive genetic variance component (heritability); C=common/shared environment variance component; E=unshared environment variance component; HR=hazard ratio; CI=confidence intervals
Bivariate Twin and Family Models
Final parameter estimates from the bivariate model of suicide attempt and death by suicide are presented in the Figure, and variance components are presented in Table 2. We tested whether thresholds for both outcomes for each sibling group, plus genetic and shared environment path estimates could be equated across men and women, and they could not (ΔX2=4973.8, Δdf=15, p<0.0001). The genetic correlation between suicide attempt and death was rA=0.67 (0.55; 0.67) for women and rA=0.74 (0.63; 0.87) for men. The environmental correlation, attributable to environmental experiences not shared by siblings, was rE=0.36 (0.29; 0.45) for women and rE=0.21 (0.19; 0.27) for men.
Figure.
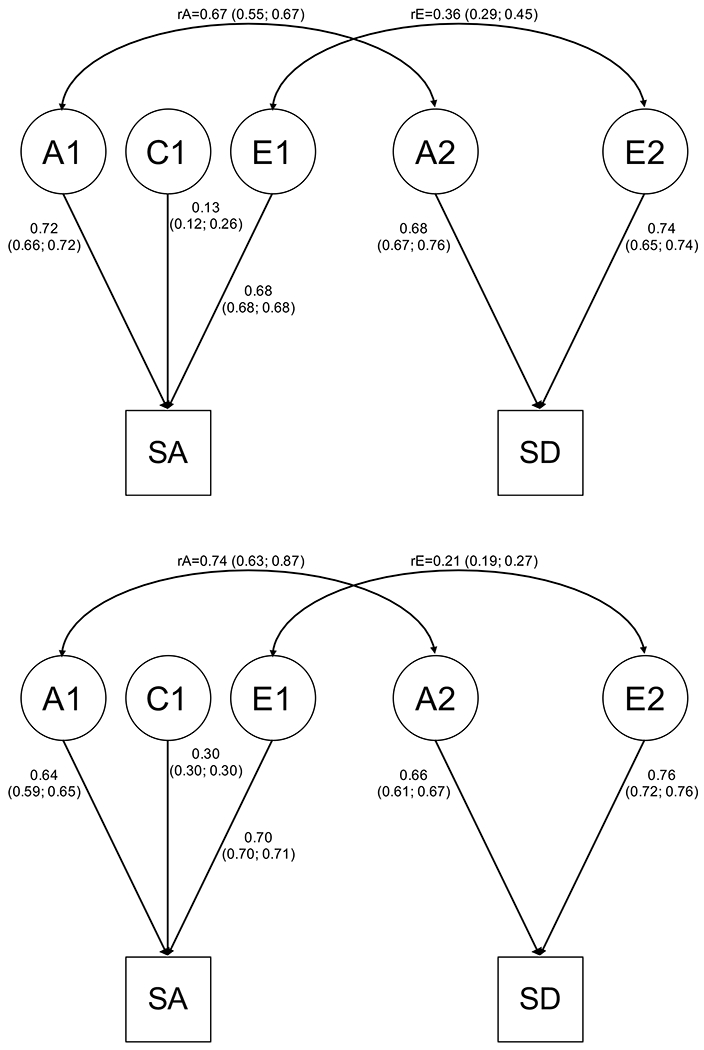
Parameter and correlation estimates (95% confidence intervals) from the bivariate twin-family model of non-fatal suicide attempt (SA) and suicide death (SD), for women (top panel) and men (bottom panel). The sources of variance are: additive genetic factors (A), common environmental factors (C; attempt only), and unique environmental factors (E).
Sensitivity Analysis
To determine whether parameter estimates were heavily influenced by attempts and deaths of undetermined intent, we conducted a sensitivity analysis excluding those registrations (N=18,436 suicide attempts and N=1063 suicide deaths). Among women, 15.0% of attempts and 12.5% of deaths were excluded; for men, 30.8% of attempts and 12.6% of deaths were excluded. Variance component estimates changed little for women and confidence intervals overlapped those in the primary analysis (Table 3). Similarly, rA and rE were comparable (rA=0.71 [0.71; 0.87]; rE=0.36 [0.34; 0.46]). For men, exclusion of these events resulted in a lower heritability estimate for suicide attempt, and confidence intervals did not overlap those from the primary analysis. Estimates for suicide death were less affected by the exclusion of these events. The genetic and environmental correlations across attempts and suicide death were modestly increased but with overlapping confidence intervals (rA=0.86 [0.86; 1.00]; rE=0.25 [0.2; −0.26]). Parameter estimates could not be equated across sex (ΔX2=9667.8, Δdf=15, p<0.0001).
Table 3.
Variance components (95% confidence intervals) from bivariate twin-family modeling results where events of undetermined intent were excluded from the analysis.
| Suicide Attempt | Women Estimate | 95% CI | Men Estimate | 95% CI |
| A | 0.55 | 0.55; 0.56 | 0.35 | 0.30; 0.35 |
| C | 0.00 | 0.00; 0.00 | 0.06 | 0.06; 0.06 |
| E | 0.44 | 0.42; 0.47 | 0.59 | 0.59; 0.62 |
|
| ||||
| Suicide Death | ||||
| A | 0.46 | 0.32; 0.61 | 0.44 | 0.44; 0.52 |
| C | - | - | - | - |
| E | 0.54 | 0.40; 0.68 | 0.56 | 0.48; 0.61 |
A=additive genetic variance component (heritability); C=common/shared environment variance component; E=unshared environment variance component; HR=hazard ratio; CI=confidence intervals
Secondary Analysis of Suicide Attempt as Young Person and/or Adult
We identified N=20,893 individuals with an attempt between ages 10-24, and N=22,625 individuals with an attempt after age 24. There were N=2752 individuals with attempts during both periods, of which 58% were women and 42% were men. Results of bivariate twin-family models are presented in Table 4. Heritability estimates were higher for attempt as a young person than as an adult for both sexes. The genetic correlation (rA) between non-fatal attempt as a young person and as an adult was higher among women than among men, and the Olkin-Pratt test for homogeneity of rA across sexes was significant (Q=28.2, df=1, p<0.0001). The shared environmental correlation (rC) between young and adult attempt was in opposite directions across sexes; however, C accounted for very little of the total variance, making substantive interpretation of these disparate estimates difficult.
Table 4.
Variance components (95% confidence intervals) from bivariate twin-family modeling results of suicide attempt among young people aged 10-24 and adults (age 25+).
| Young People | Women Estimate | 95% CI | Men Estimate | 95% CI |
| A | 0.62 | 0.59; 0.65 | 0.55 | 0.44; 0.65 |
| C | 0.01 | 0.00; 0.02 | 0.07 | 0.05; 0.07 |
| E | 0.37 | 0.35; 0.41 | 0.38 | 0.37; 0.42 |
|
| ||||
| Adults | ||||
| A | 0.36 | 0.30; 0.42 | 0.38 | 0.37; 0.44 |
| C | 0.09 | 0.09; 0.09 | 0.10 | 0.10; 0.10 |
| E | 0.55 | 0.52; 0.55 | 0.52 | 0.49; 0.55 |
|
| ||||
| Correlations between Young People and Adults | Correlation | 95% CI | Correlation | 95% CI |
| rA | 0.79 | 0.72; 0.79 | 0.39 | 0.26; 0.47 |
| rC | −0.88 | −1.00; 0.00 | 0.99 | 0.95; 1.00 |
| rE | 0.17 | 0.17; 0.17 | 0.22 | 0.16; 0.26 |
A=additive genetic variance component (heritability); C=common/shared environment variance component; E=unshared environment variance component; rA=genetic correlation; rC=common/shared environmental correlation; E=unshared environmental correlation; CI=confidence intervals
Discussion
Our primary research aim was to quantify the genetic relationship between suicide attempts and death by suicide using a representative national Swedish cohort. We found that attempts and suicide death were moderately heritable, with estimates from our twin-family approach (A=0.41-0.52) considerably higher than those from molecular genetic studies (h2SNP=0.03 for suicide attempt (17); h2SNP=0.16 for suicide death (19)), as is common across these different methodological approaches due in part to limited sample sizes and the inclusion of only common variants in the latter (50, 51). These outcomes are substantially genetically correlated (rA=0.67 for women and rA=0.74 for men), while the unique environmental correlation was more modest (rE=0.36 for women and rE=0.21 for men). Our findings support prior evidence that the etiologies of suicide attempt and suicide death are incompletely overlapping and may thus present distinct opportunities for prevention. In a secondary analysis, we found that the genetic factors contributing to risk of suicide attempt are potentially dynamic across the life course, underscoring the complex roles of biology and development in suicidality.
In conjunction with our prior study (33), which found that the genetic distinction between suicide attempt and death was not merely one of severity of liability, our results have implications for studies aimed at the identification of genetic risk variants for suicidal behavior. Genomewide association studies that collapse attempt and death are unable to distinguish whether implicated variants or genes have outcome-specific effects versus contribute to liability to both. This prevents dissection of differences in the biological etiologies of attempt and death, which may hinder prevention efforts. These complications could be extended to apply to suicidal ideation and non-suicidal self-injury: Prior evidence suggests these outcomes are at least partially etiologically distinct from suicide attempts and/or death (52–56), although a recent study revealed strong genetic and unique environmental correlations (rA=0.94 and rE=0.80) (57) in a sample of British twins. These outcomes have also been conceptualized as lying on a continuum of self-harm (20). Recent analytic advances that decompose genetic variance into that which is common across outcomes versus that which is outcome-specific (58–60) may avoid these shortfalls once genotyped samples of sufficient size are available.
In addition, our findings underscore the relevance of evaluating family history of suicidal behaviors. Stigma about suicidal behavior persists even among family members and medical personnel (61, 62), which may lead individuals to feel uncomfortable disclosing their own or their family members’ history. This is turn may prevent health care providers from fully appreciating patients’ risk, particularly if suicide attempts, which are more readily concealed from family members, are not disclosed. Clinicians should also be aware of both continuity of risk across the life course and the relevance of life stage-specific influences: i.e., the impact of environmental exposures experienced during adolescence may persist and be augmented by exposures experienced during adulthood.
We previously reported, in an extended adoption design in Sweden, evidence for substantial environmental transmission of suicide attempt liability from parents to offspring (33), while the current study found only a small contribution from the shared environment. These seemingly disparate findings are likely due in part to the different questions posed by these studies – parent-offspring “vertical” transmission of risk versus “horizontal” transmission between siblings close in age. Different, but potentially overlapping, aspects of the environment are captured across these methods. For example, the “shared environment” of the current study includes school/neighborhood-level exposures outside the home, while the “environment” of our previous study includes parenting behaviors that may differ across offspring (e.g., discipline, warmth). We have elsewhere shown, using empirical estimates of twin-twin and parent-child correlations for major dimensions of parenting, that the correlation in liability among twins for typical psychiatric phenotypes due to shared parenting would range from 2-4% (63), consistent with the findings of the current study.
The modest environmental correlations between suicide attempt and death, which reflect exposures not shared by family members, indicate that extrinsic factors differentially impact risk for these outcomes. One study found that most environmental factors examined, including low income and exposure to stressful legal, interpersonal, and work-related events, increased risk for both attempts and death (10). However, other factors had outcome-specific effects: A poor parental relationship during childhood was associated with suicide but not with serious attempts, while social isolation was associated with attempt and not death. Another study found that gun availability – i.e., access to a high lethality method – was related to suicide death but not attempt (9); gun ownership may also be a proxy for other risk factors such as adult antisocial behavior and exposure to violent crime (64). The dearth of studies that examine risk factors for both suicide attempt and death within the same sample – thereby enabling direct comparisons – precludes a nuanced interpretation of the modest environmental correlations we observed. This is a critical deficit in our understanding of the etiology of these outcomes, as it impacts risk prediction and prevention. Environmental exposures, in contrast to genetic variants, are potentially modifiable risk factors, but our findings reveal that environmental factors impacting risk for both suicide attempt and death represent only an incomplete portrait of prevention targets.
Our secondary analysis examining suicide attempt across young people and adults addresses research questions that have not, to our knowledge, been tested previously: To what extent do genetic factors differentially contribute to risk of suicide attempt across the life course, and is there incomplete overlap of genetic factors across time? We observed that the heritability of suicide attempt was considerably higher among young people, particularly for women (confidence intervals overlapped for men across time). This raises the possibility that temperament and/or psychopathology – that is, intrinsic factors of considerable heritability – may play a more prominent role among young people than adults. In contrast, the variance in liability accounted for by unique environmental factors during adulthood suggests that adverse life experiences are more potent risk factors for suicide attempt among adults. The shared environmental correlation (rC) estimates differed markedly across sexes. These factors accounted for little of the total variance in risk (C = 0.01-0.1) and the rC estimate was imprecise among women; substantive interpretation of the rC estimates is therefore not feasible.
Another key finding from the secondary analysis is the considerable sex difference in the genetic correlation between attempts among young people versus adults (rAwomen=0.79 [0.72, 0.79] and rAmen=0.39 [0.26, 0.47]). This indicates that, among women, continuity of risk across the life course is due largely to genetic factors whose impact persists across time. In contrast, for men, liability toward suicide attempt in adulthood is more strongly influenced by a qualitatively different facet of genetic influences than were relevant earlier in life. Similar to our findings on the genetic correlation between suicide attempt and death, the results of our secondary analysis have implications for gene-identification studies. The higher heritability of attempts among young people may facilitate genome-wide association studies (65) relative to studies among adults; however, restricting a GWAS study to only young people is not an ideal solution given the advantages of maximizing sample size. Instead, age at attempt could be included as a covariate along with an interaction term between age and genetic variant.
Limitations
There are several limitations to these analyses. First, we are reliant on ICD codes for suicide attempts and are therefore unable to detect attempts that did not require medical attention or were not otherwise reported to a health care provider, of which there may be a considerable number (7). Accordingly, our data likely captures more severe suicide attempts, which may be more closely related to suicide deaths than attempts overall. We are also reliant on the quality and consistency of the coding process (66, 67). We were able to identify only one study that obtained self-reports of self-harm in a sample for which institutional records (medical registrations) were also available (68), which found incomplete overlap between sources; however, the small sample precludes generalization to other studies. Prior evidence indicates that individuals hospitalized for self-harm may be less likely to complete a self-report survey (68), and the rate of refusal to participate is higher for non-anonymous surveys (69). These factors would likely lead to underestimation of suicide attempt prevalence as assessed via self-report. Such estimates vary widely, e.g. from 2.7-14% (69–71). The limitations of our use of registry records may therefore be offset by the reliability of these records.
Although these findings are representative of the Swedish population, they may not be generalizable to populations in other countries. Until relatively recently, Sweden’s annual suicide rate was consistently higher than that of the US, and became comparable at approximately 12 per 100,000 in 2007-2009. Since 2010, the US rate has increased while Sweden’s rate has remained stable (72). Our secondary analyses expose potentially important shifts in the etiology of suicide attempt across the life course, including those related to environmental exposures, which may differ markedly across countries and cultures. We also note that our selection of cohort, which maximized available registry data, did not include elderly individuals.
Consistent with other studies (41, 73), we included events of undetermined intent in our primary analyses. Our sensitivity analysis excluding those events resulted in shifts in estimates, particularly for suicide attempt among men. While some prior evidence suggests that events of undetermined intent include suicides that would otherwise be undetected (74, 75), the conservative approach is to regard the variance component and correlation estimates from our primary and sensitivity analyses as the bounds within which the “true” estimates fall.
Our models do not account for psychiatric disorders, which are genetically related to suicidal behavior (17). This limitation is offset by the insight provided by the current approach to the genetic and environmental influences on suicidal behavior in the general population. Indeed, the majority of those with registrations for suicide attempt (70.7%) or death (51.3%) did not have a prior registration for a major psychiatric disorder.
Although we demonstrated shifts in suicide attempt heritability, and a genetic correlation <1, across development, our analyses did not otherwise account for the potential effect of age. Given prior evidence of age, period, and cohort effects on suicidal behavior (76–78), additional research is warranted.
Conclusions
Suicide attempt and death are moderately heritable and are substantially–but not completely – genetically correlated. In conjunction with modest environmental correlations, our findings speak to partially distinct etiologies, raising the likelihood of incompletely overlapping opportunities for prevention and risk prediction. Furthermore, as demonstrated by our analysis of suicide attempt across young people and adults, both genetic and environmental influences on risk are temporally dynamic, particularly among men. Efforts to reduce risk of suicidal behavior must therefore consider sex differences and shifts across the life course, and gene identification efforts would benefit from distinguishing between suicide attempts versus death.
Acknowledgments:
This study was supported by NIH grants AA021399, AA023534, and AA027522; and by the Swedish Research Council as well as ALF funding from Region Skåne.
Footnotes
Disclosures: The authors have no competing interests to report.
References
- 1.World Health Organization: Suicide data. 2017. [Google Scholar]
- 2.Bachmann S Epidemiology of Suicide and the Psychiatric Perspective. Int J Env Res Public Health. 2018;15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bostwick JM, Pabbati C, Geske JR, McKean AJ. Suicide Attempt as a Risk Factor for Completed Suicide: Even More Lethal Than We Knew. Am J Psychiatry. 2016;173:1094–1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harris EC, Barraclough B. Suicide as an outcome for mental disorders. A meta-analysis. Br J Psychiatry. 1997;170:205–228. [DOI] [PubMed] [Google Scholar]
- 5.Carroll R, Metcalfe C, Gunnell D. Hospital presenting self-harm and risk of fatal and non-fatal repetition: systematic review and meta-analysis. PLoS One. 2014;9:e89944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Owens D, Horrocks J, House A. Fatal and non-fatal repetition of self-harm: Systematic review. Br J Psychiatry. 2002;181:193–199. [DOI] [PubMed] [Google Scholar]
- 7.Piscopo K, Lipari RN, Cooney J, Glasheen C: Suicidal Thoughts and Behavior among Adults: Results from the 2015 National Survey on Drug Use and Health. in NSDUH Data Review, Substance Abuse and Mental Health Service Association; 2016. [Google Scholar]
- 8.Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and suicidal behavior. Epidemiol Rev. 2008;30:133–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brent DA, Perper JA, Goldstein CE, Kolko DJ, Allan MJ, Allman CJ, Zelenak JP. Risk Factors for Adolescent Suicide: A Comparison of Adolescent Suicide Victims With Suicidal Inpatients. Arch Gen Psychiatry. 1988;45:581–588. [DOI] [PubMed] [Google Scholar]
- 10.Beautrais AL. Suicides and serious suicide attempts: two populations or one? Psychol Med. 2001;31:837–845. [DOI] [PubMed] [Google Scholar]
- 11.Tidemalm D, Runeson B, Waern M, Frisell T, Carlstrom E, Lichtenstein P, Langstrom N. Familial clustering of suicide risk: a total population study of 11.4 million individuals. Psychol Med. 2011;41:2527–2534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.von Borczyskowski A, Lindblad F, Vinnerljung B, Reintjes R, Hjern A. Familial factors and suicide: an adoption study in a Swedish National Cohort. Psychol Med. 2011;41:749–758. [DOI] [PubMed] [Google Scholar]
- 13.Runeson B, Asberg M. Family history of suicide among suicide victims. Am J Psychiatry. 2003;160:1525–1526. [DOI] [PubMed] [Google Scholar]
- 14.Voracek M, Loibl LM. Genetics of suicide: a systematic review of twin studies. Wien Klin Wochenschr. 2007;119:463–475. [DOI] [PubMed] [Google Scholar]
- 15.Petersen L, Sorensen TI, Kragh Andersen P, Mortensen PB, Hawton K. Genetic and familial environmental effects on suicide attempts: a study of Danish adoptees and their biological and adoptive siblings. J Affect Disord. 2014;155:273–277. [DOI] [PubMed] [Google Scholar]
- 16.O’Reilly LM, Kuja-Halkola R, Rickert ME, Class QA, Larsson H, Lichtenstein P, D’Onofrio BM. The intergenerational transmission of suicidal behavior: an offspring of siblings study. Transl Psychiatry. 2020;10:173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mullins N, Bigdeli TB, Borglum AD, Coleman JRI, Demontis D, Mehta D, Power RA, Ripke S, Stahl EA, Starnawska A, Anjorin A, M.R.C.Psych, Corvin A, Sanders AR, Forstner AJ, Reif A, Koller AC, Swiatkowska B, Baune BT, Muller-Myhsok B, Penninx B, Pato C, Zai C, Rujescu D, Hougaard DM, Quested D, Levinson DF, Binder EB, Byrne EM, Agerbo E, Dr.Med.Sc, Streit F, Mayoral F, Bellivier F, Degenhardt F, Breen G, Morken G, Turecki G, Rouleau GA, Grabe HJ, Volzke H, Jones I, Giegling I, Agartz I, Melle I, Lawrence J, M.R.C.Psych, Walters JTR, Strohmaier J, Shi J, Hauser J, Biernacka JM, Vincent JB, Kelsoe J, Strauss JS, Lissowska J, Pimm J, M.R.C.Psych, Smoller JW, Guzman-Parra J, Berger K, Scott LJ, Jones LA, Azevedo MH, Trzaskowski M, Kogevinas M, Rietschel M, Boks M, Ising M, Grigoroiu-Serbanescu M, Hamshere ML, Leboyer M, Frye M, Nothen MM, Alda M, Preisig M, Nordentoft M, Boehnke M, O’Donovan MC, Owen MJ, Pato MT, Renteria ME, Budde M, Dipl P, Weissman MM, Wray NR, Bass N, M.R.C.Psych, Craddock N, Smeland OB, Andreassen OA, Mors O, Gejman PV, Sklar P, McGrath P, Hoffmann P, McGuffin P, Lee PH, Mortensen PB, Kahn RS, Ophoff RA, Adolfsson R, Van der Auwera S, Djurovic S, Kloiber S, Heilmann-Heimbach S, Jamain S, Hamilton SP, McElroy SL, Lucae S, Cichon S, Schulze TG, Hansen T, Werge T, Air TM, Nimgaonkar V, Appadurai V, Cahn W, Milaneschi Y, Major Depressive Disorder Working Group of the Psychiatric Genomics C, Bipolar Disorder Working Group of the Psychiatric Genomics C, Schizophrenia Working Group of the Psychiatric Genomics C, Fanous AH, Kendler KS, McQuillin A, Lewis CM. GWAS of Suicide Attempt in Psychiatric Disorders and Association With Major Depression Polygenic Risk Scores. Am J Psychiatry. 2019;176:651–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stein MB, Ware EB, Mitchell C, Chen CY, Borja S, Cai T, Dempsey CL, Fullerton CS, Gelernter J, Heeringa SG, Jain S, Kessler RC, Naifeh JA, Nock MK, Ripke S, Sun X, Beckham JC, Kimbrel NA, Va Mid-Atlantic Mental Illness Research E, Clinical Center W, Ursano RJ, Smoller JW. Genomewide association studies of suicide attempts in US soldiers. Am J Med Genet B Neuropsychiatr Genet. 2017;174:786–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Docherty AR, Shabalin AA, DiBlasi E, Monson E, Mullins N, Adkins DE, Bacanu S-A, Bakian AV, Crowell S, Chen D, Darlington TM, Callor WB, Christensen ED, Gray D, Keeshin B, Klein M, Anderson JS, Jerominski L, Hayward C, Porteous DJ, McIntosh A, Li Q, Coon H. Genome-Wide Association Study of Suicide Death and Polygenic Prediction of Clinical Antecedents. Am J Psychiatry. 2020;177:917–927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Strawbridge RJ, Ward J, Ferguson A, Graham N, Shaw RJ, Cullen B, Pearsall R, Lyall LM, Johnston KJA, Niedzwiedz CL, Pell JP, Mackay D, Martin JL, Lyall DM, Bailey MES, Smith DJ. Identification of novel genome-wide associations for suicidality in UK Biobank, genetic correlation with psychiatric disorders and polygenic association with completed suicide. EBioMedicine. 2019;41:517–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roy A, Segal NL. Suicidal behavior in twins: a replication. J Affect Disord. 2001;66:71–74. [DOI] [PubMed] [Google Scholar]
- 22.Althoff RR, Hudziak JJ, Willemsen G, Hudziak V, Bartels M, Boomsma DI. Genetic and environmental contributions to self-reported thoughts of self-harm and suicide. Am J Med Genet B Neuropsychiatr Genet. 2012;159B:120–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schosser A, Butler AW, Ising M, Perroud N, Uher R, Ng MY, Cohen-Woods S, Craddock N, Owen MJ, Korszun A, Jones L, Jones I, Gill M, Rice JP, Maier W, Mors O, Rietschel M, Lucae S, Binder EB, Preisig M, Perry J, Tozzi F, Muglia P, Aitchison KJ, Breen G, Craig IW, Farmer AE, Muller-Myhsok B, McGuffin P, Lewis CM. Genomewide association scan of suicidal thoughts and behaviour in major depression. PLoS One. 2011;6:e20690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fu Q, Heath AC, Bucholz KK, Nelson EC, Glowinski AL, Goldberg J, Lyons MJ, Tsuang MT, Jacob T, True MR, Eisen SA. A twin study of genetic and environmental influences on suicidality in men. Psychol Med. 2002;32:11–24. [DOI] [PubMed] [Google Scholar]
- 25.Glowinski AL, Bucholz KK, Nelson EC, Fu Q, Madden PA, Reich W, Heath AC. Suicide attempts in an adolescent female twin sample. J Am Acad Child Adolesc Psychiatry. 2001;40:1300–1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Statham DJ, Heath AC, Madden PA, Bucholz KK, Bierut L, Dinwiddie SH, Slutske WS, Dunne MP, Martin NG. Suicidal behaviour: an epidemiological and genetic study. Psychol Med. 1998;28:839–855. [DOI] [PubMed] [Google Scholar]
- 27.McGuffin P, Marusic A, Farmer A. What can psychiatric genetics offer suicidology? Crisis. 2001;22:61–65. [DOI] [PubMed] [Google Scholar]
- 28.Pedersen NL, Fiske A. Genetic influences on suicide and nonfatal suicidal behavior: twin study findings. Eur Psychiatry. 2010;25:264–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mann JJ, Bortinger J, Oquendo MA, Currier D, Li S, Brent DA. Family history of suicidal behavior and mood disorders in probands with mood disorders. Am J Psychiatry. 2005;162:1672–1679. [DOI] [PubMed] [Google Scholar]
- 30.Levey DF, Polimanti R, Cheng Z, Zhou H, Nunez YZ, Jain S, He F, Sun X, Ursano RJ, Kessler RC, Smoller JW, Stein MB, Kranzler HR, Gelernter J. Genetic associations with suicide attempt severity and genetic overlap with major depression. Transl Psychiatry. 2019;9:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Erlangsen A, Appadurai V, Wang Y, Turecki G, Mors O, Werge T, Mortensen PB, Starnawska A, Borglum AD, Schork A, Nudel R, Baekvad-Hansen M, Bybjerg-Grauholm J, Hougaard DM, Thompson WK, Nordentoft M, Agerbo E. Genetics of suicide attempts in individuals with and without mental disorders: a population-based genome-wide association study. Mol Psychiatry. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sisti D, Mann JJ, Oquendo MA. Toward a Distinct Mental Disorder-Suicidal Behavior. JAMA Psychiatry. 2020. [DOI] [PubMed] [Google Scholar]
- 33.Kendler KS, Ohlsson H, Sundquist J, Sundquist K, Edwards AC. The Sources of Parent-Child Transmission of Risk for Suicide Attempt and Deaths by Suicide in Swedish National Samples. Am J Psychiatry. 2020;177:928–935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kendler KS, Ohlsson H, Lichtenstein P, Sundquist J, Sundquist K. The Genetic Epidemiology of Treated Major Depression in Sweden. Am J Psychiatry. 2018:appiajp201817111251. [DOI] [PubMed] [Google Scholar]
- 35.Kendler KS, PirouziFard M, Lonn S, Edwards AC, Maes HH, Lichtenstein P, Sundquist J, Sundquist K. A National Swedish Twin-Sibling Study of Alcohol Use Disorders. Twin Res Hum Genet. 2016;19:430–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Duncan LE, Ratanatharathorn A, Aiello AE, Almli LM, Amstadter AB, Ashley-Koch AE, Baker DG, Beckham JC, Bierut LJ, Bisson J, Bradley B, Chen CY, Dalvie S, Farrer LA, Galea S, Garrett ME, Gelernter JE, Guffanti G, Hauser MA, Johnson EO, Kessler RC, Kimbrel NA, King A, Koen N, Kranzler HR, Logue MW, Maihofer AX, Martin AR, Miller MW, Morey RA, Nugent NR, Rice JP, Ripke S, Roberts AL, Saccone NL, Smoller JW, Stein DJ, Stein MB, Sumner JA, Uddin M, Ursano RJ, Wildman DE, Yehuda R, Zhao H, Daly MJ, Liberzon I, Ressler KJ, Nievergelt CM, Koenen KC. Largest GWAS of PTSD (N=20 070) yields genetic overlap with schizophrenia and sex differences in heritability. Mol Psychiatry. 2018;23:666–673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bergen SE, Gardner CO, Kendler KS. Age-related changes in heritability of behavioral phenotypes over adolescence and young adulthood: a meta-analysis. Twin Res Hum Genet. 2007;10:423–433. [DOI] [PubMed] [Google Scholar]
- 38.Edwards AC, Ohlsson H, Sundquist J, Sundquist K, Kendler KS. Alcohol Use Disorder and Risk of Suicide in a Swedish Population-Based Cohort. Am J Psychiatry. 2020;177:627–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.World Health Organization: International Statistical Classification of Diseases and Related Health Problems 10th Revision. 2016. [Google Scholar]
- 40.Bakst SS, Braun T, Zucker I, Amitai Z, Shohat T. The accuracy of suicide statistics: are true suicide deaths misclassified? Soc Psychiatry Psychiatr Epidemiol. 2016;51:115–123. [DOI] [PubMed] [Google Scholar]
- 41.Simon GE, Johnson E, Lawrence JM, Rossom RC, Ahmedani B, Lynch FL, Beck A, Waitzfelder B, Ziebell R, Penfold RB, Shortreed SM. Predicting Suicide Attempts and Suicide Deaths Following Outpatient Visits Using Electronic Health Records. Am J Psychiatry. 2018:appiajp201817101167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Boker S, Neale M, Maes H, Wilde M, Spiegel M, Brick T, Estabrook R, Bates T, Mehta P, von Oertzen T, Gore R, Hunter M, Hackett D, Karch J, Brandmaier A, Pritikin J, Zahery M, Kirkpatrick R, Wang Y, Goodrich B, Driver C, Massachusetts Institute of Technology, Johnson S, Association for Computing Machinery, Kraft D, Wilhelm S, Medland S, Falk C, Keller M, Manjunath B, The Regents of the University of California, Ingber L, Shao Voon W, Palacios J, Yang J, Guennebaud G, Niesen J: OpenMx 2.18.1 User Guide. 2020. [Google Scholar]
- 43.Neale MC, Hunter MD, Pritikin JN, Zahery M, Brick TR, Kirkpatrick RM, Estabrook R, Bates TC, Maes HH, Boker SM. OpenMx 2.0: Extended Structural Equation and Statistical Modeling. Psychometrika. 2016;81:535–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.World Health Organization: Health for the World’s Adolescents. Geneva, Switzerland, World Health Organization; 2014. [Google Scholar]
- 45.Gogtay N, Giedd JN, Lusk L, Hayashi KM, Greenstein D, Vaituzis AC, Nugent TF 3rd, Herman DH, Clasen LS, Toga AW, Rapoport JL, Thompson PM. Dynamic mapping of human cortical development during childhood through early adulthood. Proc Natl Acad Sci U S A. 2004;101:8174–8179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wilke M, Krageloh-Mann I, Holland SK. Global and local development of gray and white matter volume in normal children and adolescents. Exp Brain Res. 2007;178:296–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brevet-Aeby C, Brunelin J, Iceta S, Padovan C, Poulet E. Prefrontal cortex and impulsivity: Interest of noninvasive brain stimulation. Neurosci Biobehav Rev. 2016;71:112–134. [DOI] [PubMed] [Google Scholar]
- 48.Merz EC, He X, Noble KG, Pediatric Imaging N, Genetics S. Anxiety, depression, impulsivity, and brain structure in children and adolescents. Neuroimage Clin. 2018;20:243–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mann JJ, Rizk MM. A Brain-Centric Model of Suicidal Behavior. Am J Psychiatry. 2020;177:902–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Manolio TA, Collins FS, Cox NJ, Goldstein DB, Hindorff LA, Hunter DJ, McCarthy MI, Ramos EM, Cardon LR, Chakravarti A, Cho JH, Guttmacher AE, Kong A, Kruglyak L, Mardis E, Rotimi CN, Slatkin M, Valle D, Whittemore AS, Boehnke M, Clark AG, Eichler EE, Gibson G, Haines JL, Mackay TF, McCarroll SA, Visscher PM. Finding the missing heritability of complex diseases. Nature. 2009;461:747–753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zuk O, Schaffner SF, Samocha K, Do R, Hechter E, Kathiresan S, Daly MJ, Neale BM, Sunyaev SR, Lander ES. Searching for missing heritability: designing rare variant association studies. Proc Natl Acad Sci U S A. 2014;111:E455–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Naifeh JA, Ursano RJ, Kessler RC, Zaslavsky AM, Nock MK, Dempsey CL, Bartolanzo D, Ng THH, Aliaga PA, Zuromski KL, Dinh HM, Fullerton CS, Kao TC, Mash HBH, Sampson NA, Wynn GH, Stein MB. Transition to suicide attempt from recent suicide ideation in U.S. Army soldiers: Results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). Depress Anxiety. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, Musacchio KM, Jaroszewski AC, Chang BP, Nock MK. Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychol Bull. 2017;143:187–232. [DOI] [PubMed] [Google Scholar]
- 54.Ribeiro JD, Franklin JC, Fox KR, Bentley KH, Kleiman EM, Chang BP, Nock MK. Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts, and death: a meta-analysis of longitudinal studies. Psychol Med. 2016;46:225–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nock MK. Why do People Hurt Themselves? New Insights Into the Nature and Functions of Self-Injury. Curr Dir Psychol Sci. 2009;18:78–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Taylor PJ, Jomar K, Dhingra K, Forrester R, Shahmalak U, Dickson JM. A meta-analysis of the prevalence of different functions of non-suicidal self-injury. J Affect Disord. 2018;227:759–769. [DOI] [PubMed] [Google Scholar]
- 57.Lim KX, Krebs G, Rimfeld K, Pingault JB, Rijsdijk FV. Investigating the genetic and environmental aetiologies of non-suicidal and suicidal self-harm: a twin study. Psychol Med. 2021:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Grotzinger AD, Rhemtulla M, de Vlaming R, Ritchie SJ, Mallard TT, Hill WD, Ip HF, Marioni RE, McIntosh AM, Deary IJ, Koellinger PD, Harden KP, Nivard MG, Tucker-Drob EM. Genomic structural equation modelling provides insights into the multivariate genetic architecture of complex traits. Nat Hum Behav. 2019;3:513–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Verhulst B, Maes HH, Neale MC. GW-SEM: A Statistical Package to Conduct Genome-Wide Structural Equation Modeling. Behav Genet. 2017;47:345–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Pritikin J: gwsem: Genome-Wide Structural Equation Modeling. https://cran.r-proiect.org/web/packages/gwsem/index.html2020.
- 61.Frey LM, Hans JD, Cerel J. Perceptions of Suicide Stigma. Crisis. 2016;37:95–103. [DOI] [PubMed] [Google Scholar]
- 62.Sudak H, Maxim K, Carpenter M. Suicide and Stigma: A Review of the Literature and Personal Reflections. Academic Psychiatry. 2008;32:136–142. [DOI] [PubMed] [Google Scholar]
- 63.Kendler KS, Myers J, Prescott CA. Parenting and adult mood, anxiety and substance use disorders in female twins: an epidemiological, multi-informant, retrospective study. Psychological Medicine. 2000;30:281–294. [DOI] [PubMed] [Google Scholar]
- 64.Gresham M, Demuth S. Who Owns a Handgun? An Analysis of the Correlates of Handgun Ownership in Young Adulthood. Crime & Delinquency. 2019;66:541–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Levinson DF, Mostafavi S, Milaneschi Y, Rivera M, Ripke S, Wray NR, Sullivan PF. Genetic studies of major depressive disorder: why are there no genome-wide association study findings and what can we do about it? Biol Psychiatry. 2014;76:510–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rhodes AE, Bethell J, Spence J, Links PS, Streiner DL, Jaakkimainen RL. Age-sex differences in medicinal self-poisonings: a population-based study of deliberate intent and medical severity. Soc Psychiatry Psychiatr Epidemiol. 2008;43:642–652. [DOI] [PubMed] [Google Scholar]
- 67.Crosby AE, Ortega L, Melanson C: Self-directed Violence Surveillance: Uniform Definitions and Recommended Data Elements, Version 1.0. Atlanta, GA, Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2011. [Google Scholar]
- 68.Mars B, Cornish R, Heron J, Boyd A, Crane C, Hawton K, Lewis G, Tilling K, Macleod J, Gunnell D. Using Data Linkage to Investigate Inconsistent Reporting of Self-Harm and Questionnaire Non-Response. Arch Suicide Res. 2016;20:113–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Safer DJ. Self-reported suicide attempts by adolescents. Ann Clin Psychiatry. 1997;9:263–269. [DOI] [PubMed] [Google Scholar]
- 70.Mars B, Heron J, Klonsky ED, Moran P, O’Connor RC, Tilling K, Wilkinson P, Gunnell D. What distinguishes adolescents with suicidal thoughts from those who have attempted suicide? A population-based birth cohort study. J Child Psychol Psychiatry. 2019;60:91–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Nock MK, Kessler RC. Prevalence of and risk factors for suicide attempts versus suicide gestures: analysis of the National Comorbidity Survey. J Abnorm Psychol. 2006;115:616–623. [DOI] [PubMed] [Google Scholar]
- 72.Organisation for Economic Co-operation and Developlment: Suicide Rates. [Google Scholar]
- 73.Fernandez de la Cruz L, Rydell M, Runeson B, D’Onofrio BM, Brander G, Ruck C, Lichtenstein P, Larsson H, Mataix-Cols D. Suicide in obsessive-compulsive disorder: a population-based study of 36 788 Swedish patients. Mol Psychiatry. 2017;22:1626–1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Chang SS, Sterne JA, Lu TH, Gunnell D. ‘Hidden’ suicides amongst deaths certified as undetermined intent, accident by pesticide poisoning and accident by suffocation in Taiwan. Soc Psychiatry Psychiatr Epidemiol. 2010;45:143–152. [DOI] [PubMed] [Google Scholar]
- 75.Lachaud J, Donnelly P, Henry D, Kornas K, Fitzpatrick T, Calzavara A, Bornbaum C, Rosella L. Characterising violent deaths of undetermined intent: a population-based study, 1999-2012. Inj Prev. 2018;24:424–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Galvao PVM, Silva H, Silva C. Temporal distribution of suicide mortality: A systematic review. J Affect Disord. 2018;228:132–142. [DOI] [PubMed] [Google Scholar]
- 77.Jukkala T, Stickley A, Makinen IH, Baburin A, Sparen P. Age, period and cohort effects on suicide mortality in Russia, 1956-2005. BMC Public Health. 2017;17:235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Allebeck P, Brandt L, Nordstrom P, Asgard U. Are suicide trends among the young reversing? Age, period and cohort analyses of suicide rates in Sweden. Acta Psychiatr Scand. 1996;93:43–48. [DOI] [PubMed] [Google Scholar]


