Abstract
Objective.
The goal of this effort to investigate if experienced breachers, professionals with a career history of exposure to repeated low-level blasts, exhibited postural instability.
Methods.
Postural data were examined using traditional tests of means and compared to normative data.
Results.
Breachers had significantly lower NeuroCom Sensory Organization Test (SOT) visual scores (within normative limits), prolonged Limits of Stability (LOS) test reaction time (30% of breachers and 7% of controls testing abnormal), and slower LOS movement velocity (21% of breachers and 0% of controls testing abnormal) compared to controls.
Conclusion.
Our LOS test findings are like those previously reported for students in the military breacher training course and seem to indicate that while acute effects of blasts on sensory control of balance fade away, effects on postural LOS persist over time.
Keywords: breacher, blast, balance, posture, limits of stability
INTRODUCTION.
Blast-induced mild traumatic brain injury (mTBI) is often considered the signature injury of modern armed conflicts such as the wars in Iraq and Afghanistan, accounting for 78% of all combat injuries.1 This injury rate may be an underestimate as it is based on hostile action and ICD-9-coded diagnosable conditions, and there is a growing body of literature that repeated low-level blast exposure from service members’ use of their weapons and tactics might adversely impact on health and operational readiness in the absence of a medically diagnosable injury.2–7 This possibility is of particular concern for the purpose of generating motor action to compensate for the destabilizing effect of gravity and to resist external perturbations. The military operational and medical communities as service members are exposed to sub-concussive low-level blasts far more frequently during training and deployment relative to concussive events.8
Assessing the impact of low-level blast on service member’s health is difficult due to the transient nature of its effects. Most of the research on the acute effects of repeated low-level blast exposure has been performed using military and civilian law enforcement dynamic entry populations (“breachers”). Breachers are routinely exposed to low-level blasts during training and operations as they use explosives to gain entry to or to breach secured structures. Studies involving breacher training environments reported that trainees and instructors can experience a transient symptom cluster, like blast-induced mTBI, often referred to as “breacher’s brain.” The symptom cluster is characterized by, but not limited to, headache, fatigue, dizziness, imbalance, and cognitive difficulties.4,7 Studies have also reported acute changes in neuroimaging, serum biomarker levels, and neurocognitive performance resulting from repetitive low-level blast exposure.9–16
With dizziness and imbalance being common complaints among breachers, studies evaluated how repetitive low-level blast exposure adversely acutely affects balance.17–20 Baker et al. reported postural control deficits as indicated by the Balance Error Scoring System (BESS). However, there were inconsistencies in their findings, such as BESS abnormalities were reported in both instructors and trainees at the start of the training course (i.e., pre-exposure), which persisted post-exposure for students.17 It should be noted that the BESS, is subjective, where the evaluator grades the participant’s performance on 20 second long tasks of quiet stance and has to count the number of errors by the participant (e.g. opening eyes, moving hands from hips, moving hips more than 30 degrees in abduction). Such subjectivity has been reported to affect the reliability and validity of the BESS.21–23 For this reason, other methods to assess balance that rely on objective tools (e.g., force plate) are preferable.24
Two types of balance deficits have been found in force plate studies: problems with sensory control of posture and problems with limits of stability.18–20 These are distinct, yet complementary, aspects of postural control.
Sensory control of posture, often referred to as sensory integration, is the ability to combine sensory information relevant to postural control (vision, vestibular and proprioception signaling muscle stretch and joint angle) for the purpose of generating motor action to compensate for the destabilizing effect of gravity and to resist external perturbations. Standardized tests known as the modified Clinical Tests of Sensory Integration and Balance (mCTSIB) and the Sensory Organization Test (SOT) can illuminate if there are potential problems with the sensory control of posture. It should be noted that the SOT is a more powerful assessment tool compared to the mCTSIB as it can reveal not only whether there are sensory problems, but also what sensory system (e.g., visual, vestibular, somatosensory) is functioning abnormally.
Difficulties with limits of stability are often reported alongside sensory integration issues. Limits of stability refer to our ability to purposefully move our center of gravity toward the edges of our base of support without taking a step or reaching for support to prevent a fall. The Limits of Stability (LOS) test can illuminate potential problems with limits of stability.
St. Onge et al.20 used the CTSIB and LOS test to determine if trainees and instructors involved in a breacher training course exhibited balance deficits following course completion. The result indicated that both groups had sensory integration (i.e., mCTSIB) and limits of stability (LOS test) issues when the post-course assessments where compared to the pre-course or baseline evaluation. Carr et al.19 also reported that participants in an advanced breacher course (both trainee and instructor) exhibited balance related sensory integration difficulties at the end of the course indicated by the CTSIB. Combined, these two studies provide evidence of the acute effects of repetitive low-level blasts exposure.
In contrast to the studies, Littlefield et al. reported no significant findings on the SOT when comparing a group of breaching instructors during a 2-year training period versus a group of engineers who served as controls.18 The lack of significant findings group-wise may have been a result of several methodological limitations. First, the data were not collected immediately following blast exposure, but rather at an undefined time after exposure when subjects could make the time available in their schedules for the 2-hour round trip travel to the clinic site for assessments. Assessments may have occurred days or weeks after blast exposure. Given the transient nature of breacher’s brain, it is feasible that the effects were no longer observable as the post-exposure assessments occurred outside of an acute window. Additionally, data for the second and third-time point SOT assessments were missing for half of the group that resulted in underpowered analyses. It should be noted that the baseline assessment indicated that the SOT vestibular scores for a few participants were significantly lower than normative data. It is feasible that some of the participants may have exhibited baseline vestibular orientated balance issues similar to those reported in acute and chronic blast-related mTBI.25–27
This current effort was the first to investigate the long-term, vice acute, effects of repetitive low-level blast exposure on balance in experienced breacher. We utilized the SOT and the LOS tests to assess balance in a well-characterized cohort of active-duty military or civilian law enforcement breachers and healthy age- and gender-matched controls. We hypothesized that the breacher group would score more poorly on SOT vestibular scores, as well as on several measures of the LOS test.
METHODS
Participants
A total of 20 active or prior active-duty military or civilian law enforcement breachers (14 military and 6 law enforcement; 39.7 ± 8.3 years old) were recruited into the study. The breachers group must have had at least 4 years of experience in the breaching profession and have been actively involved in breacher training or operations. As an alternate inclusion criterion, breachers must have been exposed to 400 breaching blasts or more within a career to be enrolled in the study.
A total of 14 controls (10 military and 4 law enforcement; 38.9 ± 7.8 years old) were recruited and matched by operational experience. The control group must have had at least 4 years of experience in the military or civilian law enforcement profession, be actively involved in military or civilian law enforcement training or operations, and could not have been exposed to more than 40 individual blasts over a career. A history of moderate to severe brain injury with loss of consciousness greater than 5 minutes, diagnosis of central nervous system disorder, cardiac, respiratory, or other medical conditions affecting cerebral metabolism were all considered criteria for exclusion from the study.
The protocol was reviewed and approved by Institutional Review Boards at the National Institute of Health (NIH) and the Naval Medical Research Center (NMRC) and was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments. Informed consent was provided by all participants and all procedures were performed on-site at the NIH Clinical Center.
Procedures
Demographic information and clinical history were collected from the participants. Self-reported symptomology was obtained via a clinical interview. A variety of neurophysiological and behavioral measurements were collected in this study and specific findings related to those measures have been reported elsewhere.28,29 The focus of the current report is objective assessments of balance.
A NeuroCom Smart Balance Master (previously Natus Medical Inc., Seattle, WA) was used for the SOT and LOS tests. Details and visual graphics depicting these tests can be found in the literature.30 The NeuroCom Smart Balance Master has been reported to demonstrate high test-retest reliability, supporting its use in assessing static and dynamic postural stability.31
The SOT is a test of quiet stance that is commonly used to assess the sensory control of posture.30–32 It consists of six conditions: (1) eyes open, no sway reference; (2) eyes closed, no sway reference; (3) eyes open, visual/surround sway reference; (4) eyes open, support surface sway reference; (5) eyes closed, support surface sway reference; and (6) eyes open, support surface and visual/surround sway reference. Sway reference refers to the displacement of the platform and/or the visual surround, which is initiated by the sway of the participant and registered as a change in the center of force on the platform in the sagittal plane. Higher scores reflect less body sway (i.e., better balance), with a maximum score of 100 indicating perfect balance and a score of 0 representing a fall. Three 20-second trials are completed per condition and averaged. SOT metrics are based on an equilibrium score (average of 3 trials), which compares the patient’s maximal anteroposterior sway during each trial to the theoretical sway stability limit of 12.5 degrees. Using the average equilibrium score for each condition, a composite score (CS) is calculated, as well as ratio pairs representing somatosensory (SOM), vestibular (VES), visual (VIS), visual preference (PREF) ratio scores. Our variables of interest included the CS as well as all ratios representing each sensory system.
The LOS is a test of dynamic postural control that is commonly used to assess postural limits of stability.30–32 Participants stand in a designated foot position roughly hip-width apart on a fixed force plate. Participants are asked to transfer their center of gravity (COG) toward eight targets spaced at 45-degree angular intervals around the body’s COG, as represented on a computer monitor placed at eye level. Participants are asked to begin shifting in the forward (12:00) position and to move sequentially in a clockwise manner, covering each of the 8 directions. During the leaning motion, participants are asked to maintain a straight posture and keep their feet planted on the floor, only moving at their ankles, like an inverted pendulum. LOS metrics of interest were composite scores (average of all 8 directions) on the following variables: endpoint excursion (distance traveled by the COG to reach the target at the first attempt, as a percentage of theoretical LOS), maximal excursion (distance traveled by the COG to reach the target over the entire trial duration – 8 seconds, as a percentage of theoretical LOS), movement velocity (MV; the average speed of the COG movement, in degrees/second) and reaction time (RT; the time between the signal to move and the initiation of the movement). Figure 1 shows and illustration of the test setup and representative data for a breacher participant.
Figure 1. Representative LOS test report.
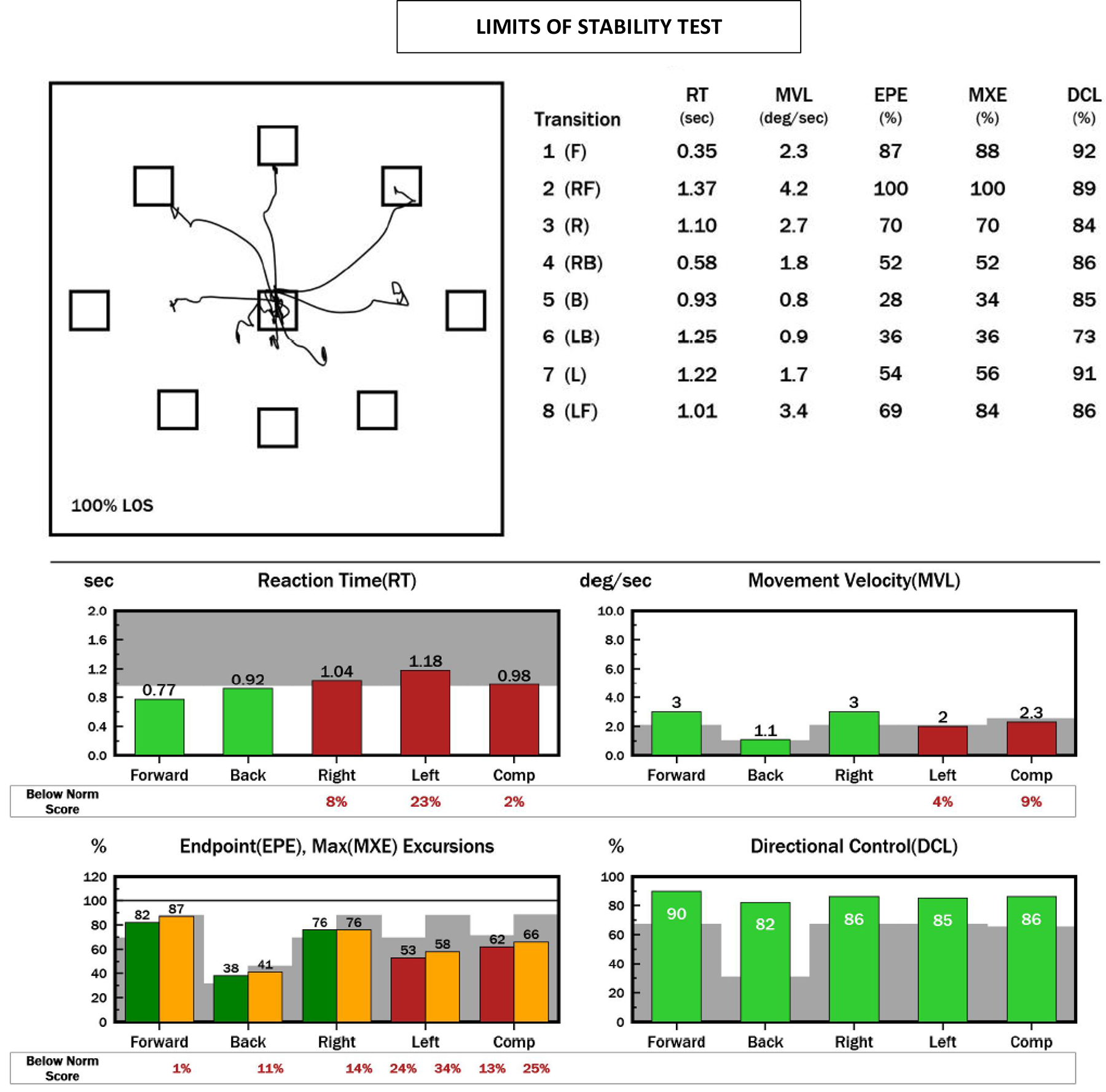
NeuroCom report of the LOS test for a Breacher participant. In this test the patient is required to purposefully lean his body toward targets displayed in 8 directions at 100% of his theoretical limits of stability. The top left plot shows this patient’s center of gravity tracings during the leaning task. During testing, the patient starts in the center box and leans toward each target in a clockwise manner. Ideally, the tracing should look like a star, with 8 lines radiating from the center to each target. The top right are scores on each LOS parameter for each target. Bottom bar plots represent this participant’s scores on the forward, back, right, left directions and composite scores (all directions). Red and yellow bars represent abnormal scores and green bars represent normal scores. Gray shading represents abnormal area that is 2 standard deviations from normative mean values. The numbers underneath abnormal bars represent how much (percentage) that particular score was below normal. This participant scored abnormal on the composite scores for reaction time, movement velocity, endpoint and maximum excursions. Note: F=forward, RF=right forward, R=right, RB=right backwards, B=backwards, LB=left backwards, L=left, LF=left forwards, in reference to the 8 target placements.
SOT and LOS metrics were compared to the NeuroCom age-referenced normative data set and were classified as clinically “abnormal” if greater than 2 standard deviations (SD) from the normative mean (dataset provided by the NeuroCom manufacturer).32
Statistical analysis
All analyses were performed in JASP (version 0.11.1.0). Percentages of clinically abnormal balance scores and self-reported symptomology were compared using Pearson’s chi-squared tests. The assumption of normality of all data was statistically verified with the Shapiro-Wilk test. The assumption of homoscedasticity was verified via visual inspection of Bland-Altman plots. Not all data met the assumption of normality and homoscedasticity and non-parametric tests were used where appropriate. We performed traditional comparisons of means (Independent t-tests or Mann-Whitney U tests; alpha = 0.05). The between-subject effects were reported using Cohen’s d and Rank Biserial Correlations (rrb) where appropriate. Cohen’s d was interpreted using the following criteria for group differences: small effect (d = 0.2), medium effect (d = 0.5), and large effect (d =0.8).31 Rank Biserial Correlations were interpreted using the following criteria for group differences: small effect (0.1 < rrb < .03), medium effect (.03 < rrb < 0.5), and large effect (0.5 < rrb <1.0).33 The effect size is one of the most important indicators of clinical significance. It reflects the magnitude of the difference in outcomes between groups; a greater effect size indicates a larger difference between experimental and control groups.
RESULTS
No significant differences were observed between groups for age, ethnicity, service, duration of service, or prevalence of history of concussion. Career breachers reported an average of 4,628 (100 – 34,800) breaching blast exposures over a career, while controls reported an average of 3 (0 – 35) exposures. Eighteen of twenty career breachers reported exposure to blast within the past year, while none of the controls reported exposure the prior year. Sample demographics and clinical characteristics are displayed in Table 1 with breachers having a higher proportion of individuals reporting memory problems, ringing in ears, concentration problems, and irritability.
Table 1.
Demographics and clinical characteristics.
| Variable | BRCH (% yes) | CTRL (% yes) | p |
|---|---|---|---|
| Right-handed | 90 | 85.7 | 0.703 |
| Experience with large arms (10 exp) | 50 | 21.4 | 0.092 |
| Experience with artillery | 30 | 7.1 | 0.105 |
| Experience with small explosives | 25 | 57.1 | 0.058 |
| Experience with non-breaching large explosives | 40 | 7.1 | 0.033 |
| Back Issues | 60 | 36 | 0.163 |
| Change in Appetite | 5 | 0 | 0.396 |
| Head Injury, Concussion, LOC | 70 | 43 | 0.113 |
| Avoiding Reminding Stressful Activities | 0 | 7 | 0.225 |
| Headaches | 15 | 14 | 0.954 |
| Memory Problems | 65 | 29 | 0.037 |
| Ringing in Ears | 65 | 29 | 0.037 |
| Difficulty Decision Making | 0 | 7 | 0.225 |
| Diminished Hearing | 55 | 29 | 0.127 |
| Concentration Problems | 55 | 14 | 0.016 |
| Discharge From Ears | 5 | 0 | 0.396 |
| Change in Taste or Smell | 15 | 0 | 0.129 |
| Pain in Ear | 5 | 0 | 0.396 |
| Difficulty with Sleep | 50 | 36 | 0.409 |
| ENT Problems | 30 | 14 | 0.288 |
| Sleepwalking, Nightmares | 15 | 0 | 0.129 |
| Light-headedness | 10 | 0 | 0.223 |
| Dizziness, Vertigo | 10 | 14 | 0.703 |
| Eye Trouble | 20 | 7 | 0.298 |
| Balance Problems | 5 | 7 | 0.794 |
| Sensitivity to Light, Noise | 30 | 7 | 0.105 |
| Coordination Problems | 5 | 7 | 0.794 |
| Fatigue | 20 | 7 | 0.298 |
| Motion Sickness | 10 | 14 | 0.703 |
| Irritability | 55 | 14 | 0.016 |
| Gastrointestinal/Nausea | 5 | 0 | 0.396 |
| Repeated Disturbing Imagery | 5 | 0 | 0.396 |
| Physical Reaction | 0 | 7 | 0.225 |
| Depression | 15 | 7 | 0.484 |
| Anxiety | 20 | 7 | 0.298 |
| Stress | 15 | 14 | 0.954 |
Sensory Control of Posture
Figure 2 illustrates the percentages of abnormal scores on the SOT for each group, as compared to the NeuroCom normative database. Only 10% of the breacher group showed abnormal vestibular scores and 5% showed other SOT abnormalities, whereas controls showed 0% abnormal vestibular scores and 7 % with abnormal SOM scores. Table 2 includes the results of the group-wise comparisons for the SOT. The Mann-Whitney U tests revealed between-group differences for the SOT VIS score with a small effect size. No other differences were observed for the SOT.
Figure 2. Percentage of abnormal Sensory Organization and Limits of Stability test scores.
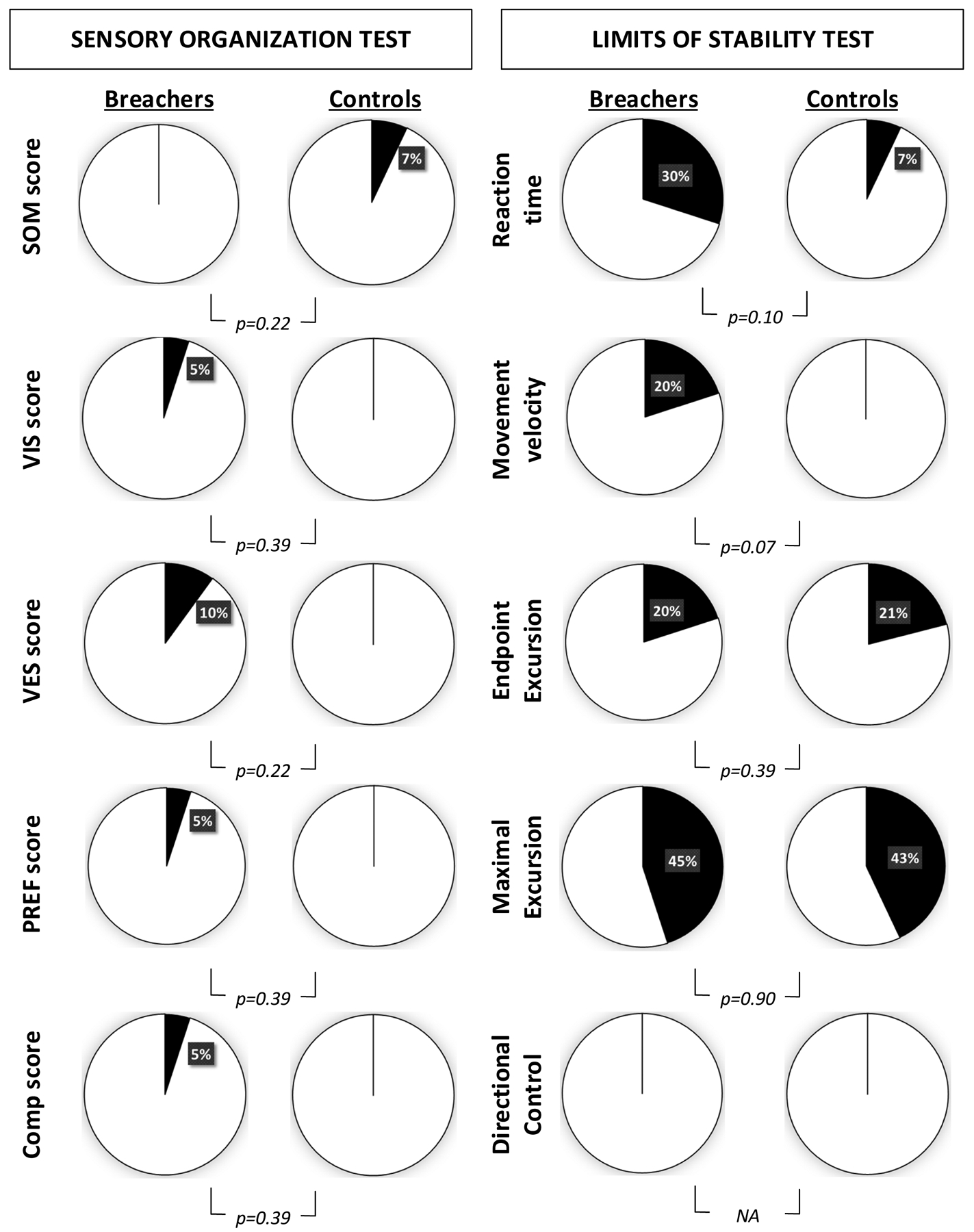
Pie charts show percentage of abnormal scores (black on the charts) of Breachers and controls under each test. Scores were considered abnormal if they were more than 2 standard deviations away from the mean of the NeuroCom normative database. Chi-square p values are presented for each comparison and there no significant differences between groups on the percentages of abnormal scores.
Table 2.
Mean (standard deviation) and p-values of dynamic posturography variables.
| Postural Stability Outcomes | Breacher (n = 20) | Control (n = 14) | Test | Traditional Comparisons | ||
|---|---|---|---|---|---|---|
| Statistic | p | Effect Size | ||||
| Sensory Organization Test | ||||||
| COMP score | 82.05 (5.84) | 83.00 (4.11) | Mann-Whitney | 143.5 | 0.916 | 0.025 |
| SOM score | 96.95 (2.31) | 94.71 (8.15) | Mann-Whitney | 130 | 0.736 | −0.071 |
| VIS score | 91.20 (8.69) | 95.64 (3.69) | t-test | 199 | 0.082 | 0.421 |
| VES score | 72.60 (12.11) | 73.86 (6.94) | Mann-Whitney | 120.5 | 0.505 | −0.139 |
| PREF score | 103.25 (6.03) | 106.57 (7.69) | Mann-Whitney | 184.5 | 0.123 | 0.318 |
| Limits of Stability Test | ||||||
| Reaction time (ms) | 0.83 (.27) | 0.66 (.19) | t-test | −2.052 | 0.048 | −0.715 |
| Movement Velocity (deg/s) | 4.19 (1.81) | 5.40 (1.30) | t-test | 2.148 | 0.039 | 0.749 |
| End Point Excursion (%) | 74.75 (11.02) | 79.71 (10.44) | Mann-Whitney | 182 | 0.146 | 0.300 |
| Maximum Excursion (%) | 84.00 (12.07) | 87.857 (8.07) | Mann-Whitney | 160.5 | 0.483 | 0.146 |
| Directional Control (%) | 81.30 (4.03) | 82.14 (3.01) | t-test | 0.663 | 0.512 | 0.231 |
Note. SOM: somatosensory (condition 2/condition 1), VIS: visual (condition 4/condition 1), VEST: vestibular (condition 5/condition 1), PREF: (condition 3+ condition 6)/(condition 2+ condition 5).
Postural Limits of Stability
Figure 2 illustrates the percentages of abnormal scores LOS scores that were proportionally more abnormal for breachers compared to controls on RT and MV, although differences were not statistically significant. Notice how both groups showed similar percentages of abnormal excursions, with 20–21% of abnormalities on endpoint excursion and remarkably almost half each group (43–45%) showing abnormal maximal excursions. Table 2 includes the results of the group-wise comparisons for the LOS tests. The Independent t-tests for the LOS test revealed between-group differences for RT and MV, with medium-to-large effect sizes.
DISCUSSION
This study examined the chronic effects of breaching blasts on the postural stability of a group of breachers with at least 4 years of experience or exposure to a minimum of 400 breaching blasts. Our results showed balance problems with postural limits of stability but not sensory control of balance. Compared to a healthy, matched cohort, the breacher cohort had significantly reduced LOS RT and MV, with 30% of breacher scores being abnormal on RT and 20% abnormal on MV.
Sensory Control of Posture
Although breachers scored statistically worse than their matched peers on the SOT VIS, the majority of breachers were clinically normal; with only one participant (5%) considered to be clinically abnormal (i.e., > 2 SDs from norms). This participant did not endorse any subjective balance-related symptoms (e.g., light-headedness, dizziness) but a history of head trauma, difficulty sleeping, and ENT problems. This participant’s abnormal score could have been a consequence of head trauma rather than repetitive long-term blast exposures. Overall, these results seem to indicate no long-term issues from repetitive low-level blast exposure regarding visual control of posture.
Contrary to our hypothesis, we found no vestibular SOT problems in the majority (90%) of the breacher cohort. It is important to remember that SOT VES scores are not diagnostic and do not reveal potential damage to the vestibular system but rather they reveal balance problems when using vestibular information for postural control.34 Breachers were thoroughly examined in a separate clinic in this outpatient study with specific vestibular testing and found to have no vestibular abnormalities as a group.29 A closer examination of the two individuals (10%) with clinically abnormal SOT VES scores showed one individual also scored abnormally for SOT VIS and the other had a history of prior head trauma symptomology (e.g., memory problems, ringing in ears, etc.). Overall, our results agree with Littlefield et al.18, who reported no group-wise differences between breachers and controls on the SOT vestibular scores in acute and subacute post-blast exposures but did report some individuals with abnormal VES SOT scores. In conclusion, our negative findings seem to provide no evidence of long-term problems of vestibular control of posture following repetitive blast exposures.
Postural Limits of Stability
LOS RT was prolonged for breachers compared to controls and was abnormal in 30% of the breacher group compared to only 7% of the control group. Breachers may have had altered RT due to their prior history of head trauma (70% of breachers versus 43% of controls). The only other study that tested LOS in breachers was St. Onge et al.20, who reported other LOS parameters to be affected but not RT. This study only assessed the acute effects of blast exposures, where our study examined chronic effects. This distinction is important as some research has indicated that delays in the postural reaction happen as a chronic, rather than acute, effect of repetitive low-level blast exposure.21 Regardless, both of our studies indicate that the LOS test elicits performance deficits, supporting previous research involving individuals with chronic TBI.35
Breachers delayed RT may have resulted from slight auditory and cognitive issues (55% of the breachers endorsed problems concentrating, 65% ringing in the ears, and 55% diminished hearing).29 The LOS test indirectly tests cognitive functioning through postural tasks that involve attention, processing speed, and decision making. Acute blast exposure adversely affects procedural RT;7 however, there is limited research on if it impacts cognitive functioning longitudinally. A companion study involving the same participants was only able to report trends.28
LOS MV scores were lower for breachers compared to controls. This finding agrees with St. Onge et al.’s study, which also found slow LOS leaning movements among breachers in acute stages post-blast.20 Together, these findings seem to indicate LOS MV problems emerge acutely and persist chronically in breachers. In our study, 21% of the breacher cohort scored abnormally in contrast to 0% of the control group. These results are similar to those reported for chronic TBI34 for percentages of the group affected, but, for scoring, our participants performed slightly better than reported for a TBI sample (our study = average 4.19 degrees/second ± 1.8 versus Row’s TBI cohort = 3.7 degrees/second ± 1.6). While it is difficult to separate the effects of chronic repetitive blasts from prior head trauma in our study, LOS MV appears to distinguish chronic blast exposure as the control group had no abnormalities compared to the blast group.
Regarding all other LOS parameters, our investigation detected no differences between groups. However, that is not to say there were no abnormalities. Almost half of both cohorts indicated abnormal maximal excursions (breachers = 45% versus controls 43%), which turned out to be the most frequent balance abnormality in this study. It seems reasonable that prior head injury endorsed by both groups may be a cause. Reduced LOS excursions are not uncommon in chronic TBI,35 or movement disorders36,37 or even part of the aging process.38 Clinical implications of such impairments are difficulty performing tasks that require bending over, reaching, or transferring postures (e.g., sit-to-stand, gait initiation). However, it is hard to conceive that such a high-functioning group of individuals would experience those problems while still being able to perform their duties, which are physically demanding. Most of the breachers in our study reported no balance issues on the clinical questionnaire. If challenges exist, they are subtle, and only an in-depth questionnaire or investigation would show.
Limitations and future directions
One of the main limitations of this study was the lack of pre-exposure baseline data, making it difficult to separate the consequences of repetitive blast exposure versus prior head trauma. An ideal study design would be one where breachers are followed over time and assessed before their career starts. Such monitoring would be consistent with U.S. policy – Public Law 116–92 stipulates blast exposure monitoring for U.S. military personnel. Nevertheless, we believe having a control group helped overcome this limitation to some extent. Another limitation was the small sample size. Future research should focus on associations between these balance deficits and the number of blast exposures experienced by these individuals.
CONCLUSION
As most of the literature has focused on acute post-blast balance problems in breachers, the main finding of this study is that some of these problems can be long-lasting and persist for years. Our study provides evidence that chronic exposure to repetitive low-level blasts is associated with impaired postural limits of stability but not the sensory organization in breachers. The LOS problems detected by this study were prolonged RT and decreased MV with 30% and 21% of breachers testing abnormally, respectively. Abnormally reduced limits of stability excursions were also found, but not exclusively in the breacher group. Future studies with larger samples are needed to confirm these findings as individuals with a history of low-level blast exposures may experience subtle yet persistent, long-term balance deficits that could adversely affect their activities of daily living. We suggest breachers undergo an objective balance assessment that includes a limit of stability test before their career starts and are followed over time. Ideally, such an assessment should be coupled with a balance questionnaire to assess subjective balance complaints. Such monitoring would be consistent with U.S. policy – Public Law 116–92 stipulates blast exposure monitoring for U.S. military personnel.
Funding Sources.
This work was supported/funded by the Joint Program Committee- 5 Development of Exposure Standards to Repeated Blast Exposure program, work unit #603115HP-3730-001-A1118, Office of Naval Research (ONR) award #N00014-18-1-2440 with supplemental funding to the ONR award provided by Cohen Veterans Bioscience, imaging resources from the Center for Neuroscience and Regenerative Medicine, and the Clinical Neurosciences Program of the National Institute of Neurological Disorders and Stroke, Project # 1ZIANS002977-21, to Dr. Wassermann.
Footnotes
Conflict of Interest. No competing financial interests exist.
Ethical Considerations & Disclosures(s). The protocol was reviewed and approved by Institutional Review Boards at the National Institute of Health (NIH) and the Naval Medical Research Center (NMRC). Informed consent was provided by all participants and all procedures were performed on-site at the NIH Clinical Center.
Publisher's Disclaimer: Disclaimers. The authors alone are responsible for the content and writing of the paper. The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense or the US Government. Approved for public release; distribution is unlimited. FH and ML are military service members and CZ, EW, SA and WC are employees of the US Government. This work was prepared as part of their official duties. Title 17 U.S.C. § 105 provides that “Copyright protection under this title is not available for any work of the United States Government.” Title 17 U.S.C. § 101 defines a US Government work as a work prepared by a military service member or employee of the US Government as part of that person’s official duties.
REFERENCES
- 1.Owens BD, Kragh JFJ, Wenke JC, Macaitis J, Wade CE, Holcomb JB. Combat Wounds in Operation Iraqi Freedom and Operation Enduring Freedom. J Trauma Acute Care Surg. 2008;64(2):295–299. doi: 10.1097/TA.0b013e318163b875 [DOI] [PubMed] [Google Scholar]
- 2.Luethcke CA, Bryan CJ, Morrow CE, Isler WC. Comparison of Concussive Symptoms, Cognitive Performance, and Psychological Symptoms Between Acute Blast-Versus Nonblast-Induced Mild Traumatic Brain Injury. J Int Neuropsychol Soc. 2011;17(1):36–45. doi: 10.1017/S1355617710001207 [DOI] [PubMed] [Google Scholar]
- 3.Carr W, Stone JR, Walilko T, et al. Repeated Low-Level Blast Exposure: A Descriptive Human Subjects Study. Mil Med. 2016;181(suppl_5):28–39. doi: 10.7205/MILMED-D-15-00137 [DOI] [PubMed] [Google Scholar]
- 4.Tate CM, Wang KKW, Eonta S, et al. Serum Brain Biomarker Level, Neurocognitive Performance, and Self-Reported Symptom Changes in Soldiers Repeatedly Exposed to Low-Level Blast: A Breacher Pilot Study. J Neurotrauma. 2013;30(19):1620–1630. doi: 10.1089/neu.2012.2683 [DOI] [PubMed] [Google Scholar]
- 5.Lange R, Pancholi S, Brickell T, et al. Neuropsychological Outcome from Blast versus Non-blast: Mild Traumatic Brain Injury in US Military Service Members. J Int Neuropsychol Soc JINS. 2012;18:595–605. doi: 10.1017/S1355617712000239 [DOI] [PubMed] [Google Scholar]
- 6.Haran FJ, Handy JD, Servatius RJ, Rhea CK, Tsao JW. Acute neurocognitive deficits in active duty service members following subconcussive blast exposure. Appl Neuropsychol Adult. 2019;0(0):1–13. doi: 10.1080/23279095.2019.1630627 [DOI] [PubMed] [Google Scholar]
- 7.LaValle CR, Carr WS, Egnoto MJ, et al. Neurocognitive Performance Deficits Related to Immediate and Acute Blast Overpressure Exposure. Front Neurol. 2019;10. doi: 10.3389/fneur.2019.00949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA. Mild Traumatic Brain Injury in U.S. Soldiers Returning from Iraq. N Engl J Med. 2008;358(5):453–463. doi: 10.1056/NEJMoa072972 [DOI] [PubMed] [Google Scholar]
- 9.Wang Z, Wilson CM, Mendelev N, et al. Acute and Chronic Molecular Signatures and Associated Symptoms of Blast Exposure in Military Breachers. J Neurotrauma. 2019;37(10):1221–1232. doi: 10.1089/neu.2019.6742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gill J, Motamedi V, Osier N, et al. Moderate blast exposure results in increased IL-6 and TNFα in peripheral blood. Brain Behav Immun. 2017;65:90–94. doi: 10.1016/j.bbi.2017.02.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eonta SE, Kamimori GH, Wang KKW, et al. Case Study of a Breacher: Investigation of Neurotrauma Biomarker Levels, Self-reported Symptoms, and Functional MRI Analysis Before and After Exposure to Measured Low-Level Blast. Mil Med. 2020;185(3–4):e513–e517. doi: 10.1093/milmed/usz185 [DOI] [PubMed] [Google Scholar]
- 12.Tschiffely AE, Statz JK, Edwards KA, et al. Assessing a Blast-Related Biomarker in an Operational Community: Glial Fibrillary Acidic Protein in Experienced Breachers. J Neurotrauma. 2019;37(8):1091–1096. doi: 10.1089/neu.2019.6512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Polejaeva E, Carr W, Wassermann E, Dell K. How do you Characterize “Breacher’s Brain”? J Int Neuropsychol Soc. 2019;Final Program Forty Seventh Annual Meeting International Neuropsychological Society(25):i–422. [Google Scholar]
- 14.Carr W, Polejaeva E, Grome A, et al. Relation of Repeated Low-Level Blast Exposure With Symptomology Similar to Concussion. J Head Trauma Rehabil. 2015;30(1):47–55. doi: 10.1097/HTR.0000000000000064 [DOI] [PubMed] [Google Scholar]
- 15.Carr W, Taylor M, LoPresti ML, et al. Symptomology observed in humans following acute exposure to explosive blast. J Neurotrauma. 2015;32:A–109. [Google Scholar]
- 16.Stone JR, Tustison NJ, Wassermann EM, et al. Neuroimaging correlates of repetitive blast exposure in experienced military breachers. In: Journal of Neurotrauma. Vol 30. Mary Ann Liebert, Inc 140 Huguenot Street, 3rd FL, New Rochelle, NY 10801 USA; 2013:A120–A121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baker AJ, Topolovec-Vranic J, Michalak A, et al. Controlled Blast Exposure during Forced Explosive Entry Training and Mild Traumatic Brain Injury. J Trauma Acute Care Surg. 2011;71(5):S472. doi: 10.1097/TA.0b013e318232e7da [DOI] [PubMed] [Google Scholar]
- 18.Littlefield PD, Pinto RL, Burrows HL, Brungart DS. The Vestibular Effects of Repeated Low-Level Blasts. J Neurotrauma. 2015;33(1):71–81. doi: 10.1089/neu.2014.3824 [DOI] [PubMed] [Google Scholar]
- 19.Carr W, Yarnell AM, Ong R, et al. Ubiquitin Carboxy-Terminal Hydrolase-L1 as a Serum Neurotrauma Biomarker for Exposure to Occupational Low-Level Blast. Front Neurol. 2015;6. doi: 10.3389/fneur.2015.00049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.St Onge P, McIlwain DS, Hill ME, Walilko TJ, Bardolf LB. Marine Corps Breacher Training Study: auditory and vestibular findings. US Army Med Dep J. Published online 2011. [PubMed] [Google Scholar]
- 21.Rhea CK, Kuznetsov NA, Wright WG, Haran FJ, Ross SE, Duckworth JL. Assessments for Quantifying Neuromotor Functioning After Repetitive Blast Exposure. In: Pre-Clinical and Clinical Methods in Brain Trauma Research. Springer; 2018:283–305. [Google Scholar]
- 22.Finnoff JT, Peterson VJ, Hollman JH, Smith J. Intrarater and Interrater Reliability of the Balance Error Scoring System (BESS). PM&R. 2009;1(1):50–54. doi: 10.1016/j.pmrj.2008.06.002 [DOI] [PubMed] [Google Scholar]
- 23.Chang JO, Levy SS, Seay SW, Goble DJ. An Alternative to the Balance Error Scoring System: Using a Low-Cost Balance Board to Improve the Validity/Reliability of Sports-Related Concussion Balance Testing. Clin J Sport Med. 2014;24(3):256–262. doi: 10.1097/JSM.0000000000000016 [DOI] [PubMed] [Google Scholar]
- 24.Mancini M, Horak FB. The relevance of clinical balance assessment tools to differentiate balance deficits. Eur J Phys Rehabil Med. 2010;46(2):239–248. [PMC free article] [PubMed] [Google Scholar]
- 25.Haran FJ, Slaboda JC, King LA, Wright WG, Houlihan D, Norris JN. Sensitivity of the Balance Error Scoring System and the Sensory Organization Test in the Combat Environment. J Neurotrauma. 2015;33(7):705–711. doi: 10.1089/neu.2015.4060 [DOI] [PubMed] [Google Scholar]
- 26.Scherer MR, Burrows H, Pinto R, et al. Evidence of Central and Peripheral Vestibular Pathology in Blast-Related Traumatic Brain Injury. Otol Neurotol. 2011;32(4):571–580. doi: 10.1097/MAO.0b013e318210b8fa [DOI] [PubMed] [Google Scholar]
- 27.Hoffer ME, Balaban C, Gottshall K, Balough BJ, Maddox MR, Penta JR. Blast exposure: vestibular consequences and associated characteristics. Otol Neurotol. 2010;31(2):232–236. [DOI] [PubMed] [Google Scholar]
- 28.Stone JR, Avants BB, Tustison NJ, et al. Functional and Structural Neuroimaging Correlates of Repetitive Low-Level Blast Exposure in Career Breachers. J Neurotrauma. Published online September 14, 2020. doi: 10.1089/neu.2020.7141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Modica Claire M., Johnson BR, Zalewski C, et al. Hearing loss and irritability reporting without vestibular differences in explosive breaching professionals. Frontiers in Neurology. (accepted for publication November 2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nashner LM. Computerized dynamic posturography. In: Jacobson GP, Newman CW, Kartush JM, editors. Handbook of Balance Function Testing. San Diego: Singular Publishing Group; 1993. [Google Scholar]
- 31.Thompson M NeuroCom – Clinical Interpretations Guide. NeuroCom International Inc.; 2009. [Google Scholar]
- 32.Pickerill Marie L., and Harter Rod A.. Validity and reliability of limits-of-stability testing: a comparison of 2 postural stability evaluation devices. J Ath Train. 2011;46(6): 600–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cohen J Statistical Power Analysis. Curr Dir Psychol Sci. 1992;1(3). doi: 10.1111/1467-8721.ep10768783 [DOI] [Google Scholar]
- 34.Jacobson GP. Handbook of Balance Function Testing. Mosby Elsevier Health Science; 1993. [Google Scholar]
- 35.Row J, Chan L, Damiano D, Shenouda C, Collins J, Zampieri C. Balance Assessment in Traumatic Brain Injury: A Comparison of the Sensory Organization and Limits of Stability Tests. J Neurotrauma. 2019;36(16):2435–2442. doi: 10.1089/neu.2018.5755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mancini M, Zampieri C, Carlson-Kuhta P, Horak FB, Chiari L. Stance posture changes in early Parkinson’s disease are detectable with a wearable inertial device. Gait Posture. 2008;(28):S30. [Google Scholar]
- 37.Ondo W, Warrior D, Overby A, et al. Computerized Posturography Analysis of Progressive Supranuclear Palsy: A Case-Control Comparison With Parkinson’s Disease and Healthy Controls. Arch Neurol. 2000;57(10). doi: 10.1001/archneur.57.10.1464 [DOI] [PubMed] [Google Scholar]
- 38.Melzer I, Benjuya N, Kaplanski J. Postural stability in the elderly: a comparison between fallers and non-fallers. Age Ageing. 2004;33(6):602–607. doi: 10.1093/ageing/afh218 [DOI] [PubMed] [Google Scholar]


