Abstract
Background:
The occipital transtentorial (OT) approach is well-established approach for pineal region tumors and can be of choice for the lesions located around the suboccipital part of tentorium such as the quadrigeminal plate, posterior part of thalamus, tentorial surface of cerebellum, splenial region, posterior falx, and lesions around the tentorial incisura. However, it is not very much extensively used in the above-mentioned locations other than the pineal region.
Methods:
Thirty-one patients of pineal region lesions were operated by OT approach, the role of conventional preoperative evaluation of the anatomy of the venous sinuses, deep venous system, and tentorial angle was investigated.
Results:
A variety of lesions were operated using this approach achieving gross and near total resection in majority of the cases (76.6%), with acceptable postoperative mean modified Rankin scales (1.8).
Conclusion:
The OT is a preferable approach for pineal region lesions for patients of all ages and can be tailored for achieving high resectability rates irrespective of the status of the deep venous system and tentorial angle, with reasonable postoperative surgical outcome.
Keywords: Deep venous system, Occipital transtentorial, Pineal region, Tentorial angle, Vein of Galen

INTRODUCTION
Pineal region can be described as pineal gland and adjacent area such as tentorial incisura, quadrigeminal plate, and posterior part of thalamus, tentorial surface of cerebellum, splenial region, posterior falx, and torcula.[18,21] The lesions of pineal region can be accessed by supracerebellar infratentorial (SCIT), occipital transtentorial (OT), or posterior interhemispheric approach (PIH). Conventionally, the OT approach is decided by many factors such as location of the lesion (supra or infratentorial), size of the lesion, and relation of the deep venous system, that is, vein of Galen (VOG) to the lesion (i.e. superior or inferior), and tentorial angle (mainly for lesions extending above the tentorial edge where the steepness of the tentorial angle limits the resection through the supracerebellar infra tentorial approach)[8] Although the SCIT approach provides a midline corridor and better orientation to midline structures, it has some disadvantages such as limited exposure, complications associated with sitting position, and sometimes ergonomic discomfort for the operating surgeon.[8] It has been also observed that the lesion resectability and postoperative neurological outcome may not be related to the surgical approach chosen.[6] Hence, the ease and comfort along with wider area of surgical exposure associated with OT makes it the procedure of choice for surgeons especially those having, familiarity, and experience with this approach.
This approach is relatively difficult as it deals with three big sinuses, namely, superior sagittal sinus (SSS), transverse sinus (TS), and straight sinus (SS) along with venous channels in the tentorium which may be present in some cases. Besides that, the cutting of the tentorium also has to be mastered. Moreover, if one learns to deal with these issues, it is the approach, which can address many lesions in the pineal region, and would provide wider exposure; main surgeon can get the help of assistant surgeons in vascular cases. However, it can be difficult and disorienting for some surgeons due to lateral/prone positioning, particularly in cases with aberrant and anomalous anatomy of venous sinuses. We are presenting our experience with this approach in pineal region lesions with special emphasis on location of veins in relation to lesion, cutting the tentorium, the tentorial angle, and the surgical outcome.
MATERIALS AND METHODS
All the of cases of pineal region lesions both benign and malignant as diagnosed by computed tomography (CT), magnetic resonance imaging (MRI) contrast, irrespective of age, and location of deep venous system were operated by OT approach. MR or CT Venogram was done to see occipital veins and TS dominance to decide the side of craniotomy, which was performed on the side with lesser number of occipital veins. The tentorial angle (n) [Figure 1] was measured on MRI sagittal cut by drawing a horizontal line along the floor of the fourth ventricle and a tangential line along the superior surface of cerebellum. The tentorium was labeled as steep if the tentorial angle was >60 degrees.
Figure 1:
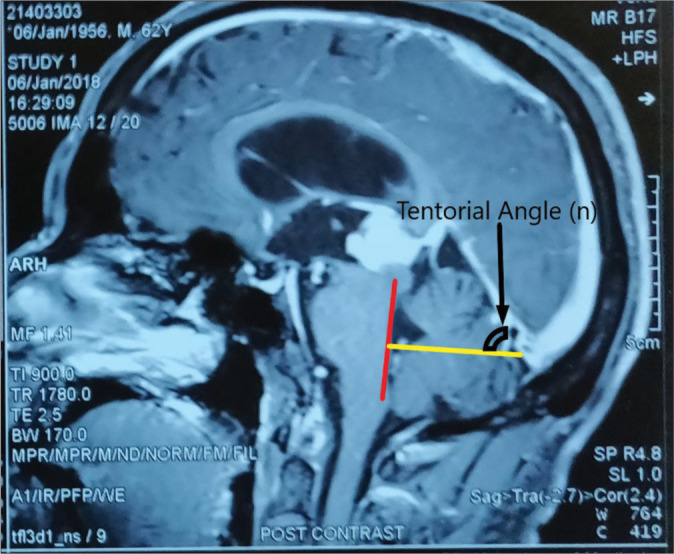
Measurement of tentorial angle (n). The floor of the fourth ventricle is marked by the line in red, extending inferiorly from just under the inferior colliculus. The new reference line, in yellow, is drawn perpendicular to this red line, extending through the torcula. The tentorial angle is measured against this yellow line.
Preoperative ventriculoperitoneal shunt was carried out in patients who presented with acute features of raised intracranial pressure. Patients were operated in prone or lateral position. In patients where prone position was used, after craniotomy, head was rotated to make the operative side dependent. Skin incision was U-shaped with vertical limb just lateral to midline [Figure 2a], one burr hole was made approximate 1.5–2 cm lateral to midline near torcula, another burr hole approximately 5 cm above it and making a parieto-occipital craniotomy of about 5 cm × 5 cm [Figure 2b]. Craniotomy is fashioned in such a way that TS, SSS, and falx should be visible. The dura was opened in a C-shaped fashion hinged on the SSS [Figure 2c]. Occipital lobe is retracted along the inferomedial aspect [Figure 3a]. SS is identified and tentorium is cut parallel to SS at least 1 cm away from posteroinferior and in the middle of cutting of the tent, angulate the microscope superomedial toward the spelnium and cut till the free edge and stay suture is taken on medial cut end of tentorium to keep tentorium retracted [Figure 3band c]. Any small vein encountered in suboccipital area is coagulated. After cutting the tent, both the venous systems with enveloped arachnoid and tumor are visible in the same field [Figure 3d]. Arachnoid dissection was done to dissect and expose tumor leaving the arachnoid enveloping the veins intact. Thereafter, tumor resection is done like any other tumor removal. After tumor removal, the suture taken to hold the cut tentorium is released and after achieving hemostasis, dura is closed.
Figure 2:
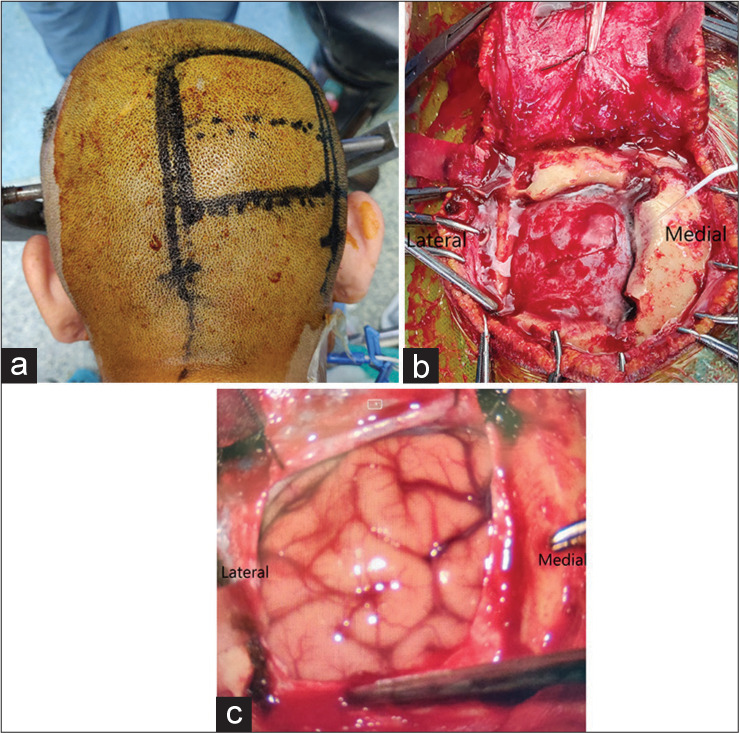
(a) Skin incision with a planned U-shaped flap. (b) Suboccipital craniotomy and removal of bone flap. (c) Occipital lobe as seen after durotomy.
Figure 3:
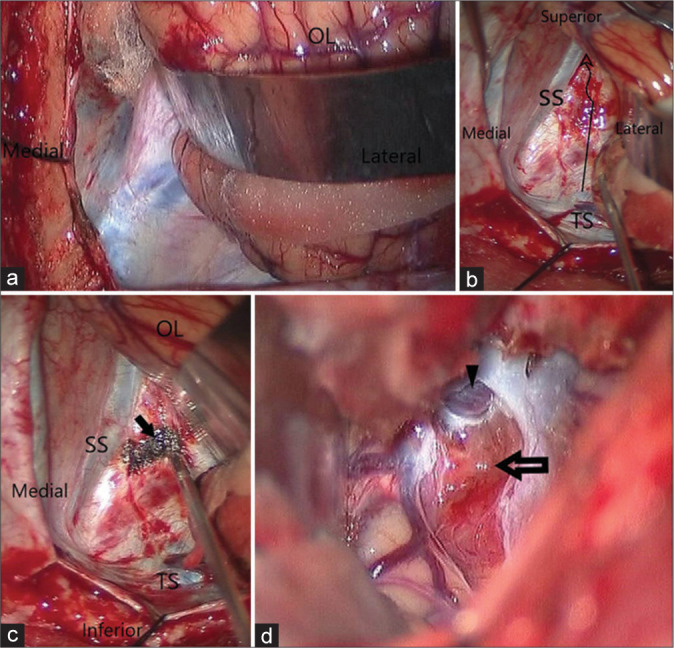
(a) Intraoperative view of tentorium cerebelli on retracting the occipital lobe (OL). (b) Method of cutting the tentorium cerebelli in antero superomedial direction. (c) Tentorium cauterised at the site of incision. (d) Intraoperative transtentorial view of pineal region lesion after incising the tentorium (arrow). Vein of galen with intact surrounding arachnoid can be seen (arrowhead). OL: Occipital lobe, SS: Straight sinus, TS: Transverse sinus.
For large tumors, falcotentorial, and posterior thalamic, PIH was combined with OT. The resection was defined as gross total, if the lesion was completely removed with no residual lesion detected on the postoperative CT scan, near total resection if more than 90% of the lesion was removed and subtotal resection if <90% of the lesion was removed. Assessment of surgical outcome was done in terms of anatomical accessibility, extent of tumor resection and histopathological diagnosis, and postoperative recovery evaluation was done by Modified Rankin Scale and the postoperative follow-up was done periodically after a week, 1 month, and 3 months.
RESULTS
Thirty-one patients, 15 females and 16 males, age group between 2 and 67 years (mean age 26.4 years) were operated by OT approach for lesions located in pineal region. The procedures were performed in prone and lateral positions because these were simple, safe, and significantly decreased the operative distance. This included one patient where surgery was abandoned due to excessive bleeding from sinuses during craniotomy. Hence, excluding this patient, the study was carried out in the remaining 30 subjects. In a patient with residual tumor who presented with regrowth, intact arachnoid around deep venous system was a good landmark to recognize neighboring structures and helped in tumor removal. There was no difficulty in retracting occipital lobe also.
In one girl child, tuberculomas were located on tentorial surface of cerebellum, but intact large suboccipital venous plexus while approaching from posterior suboccipital approach was the hindering factor to approach this lesion through posterior fossa approach, therefore removed through OT approach. One patient had multiple tuberculomas both supra and infratentorial suboccipital region. Posterior thalamic masses were approached after cutting tent, through suboccipital interhemispheric route.
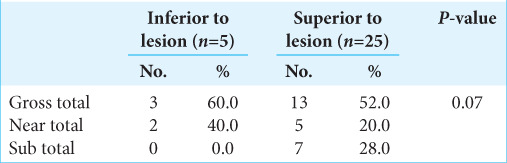
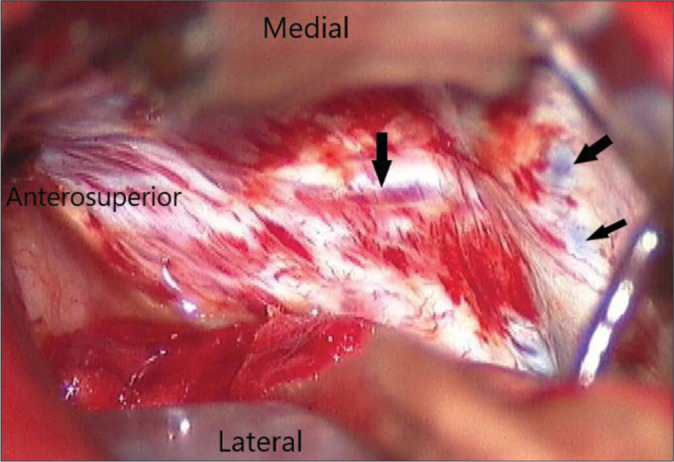
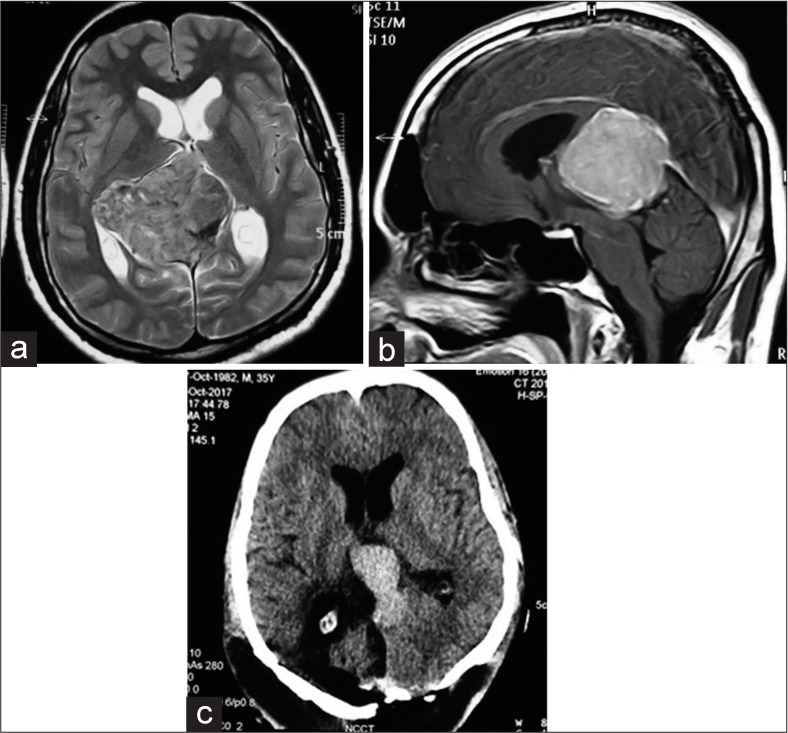
Location of lesion and pathological diagnosis is mentioned in [Table 1]. The location of the lesion was defined in relation to the deep venous system in all cases. The VOG was inferior to the lesion in 5 (16.7%) cases (three thalamic tuberculomas, one thalamic glioma, and one falcotentorial meningioma), whereas the VOG was superior to the lesion in rest of the 25 (83.3%) cases. In five cases, it was invading arachnoid, displacing lateral placed deep veins. Gross and near total resection was achieved in all five cases where the VOG was inferior in relation to the lesion and in 72% of cases where the VOG was superior to the lesion. Subtotal resection was done in remaining 28% of cases where the VOG was superiorly located to the lesion [Table 2]. The mean Modified Rankin scale score was 2.43 and 2.30 for inferiorly and superiorly placed VOG, respectively, showing comparable postoperative outcome. The results, however, were statistically insignificant (P = 0.88).
Table 1:
Anatomical diagnosis in study subjects (n=30).
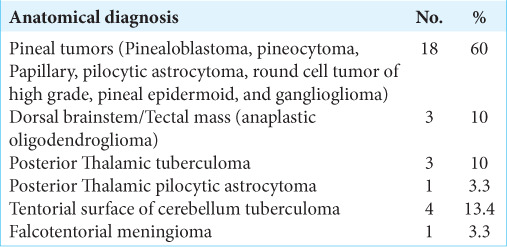
Table 2:
Association of deep venous system with extent of resection.
The mean angle between the tentorium and occipital surface of cerebellum (tentorial angle) was measured. The 51 degrees minimum and 83 degrees maximum tentorial angle was observed with a mean of 62.08 ± 7.17 degrees. All cases irrespective of the acuteness of tentorial angle and location of the deep venous system were operated by same approach.
Out of 30 study subjects, TS was found to be dominant on the right side in 13 (47.1%) cases and the left side in 17 (52.9 %) cases [Table 3]. However, dominance of the sinus was not the criterion to decide the side of craniotomy. The side of the craniotomy was decided by less number of occipital veins on that side. In one case, where the TS was hypoplastic on the left side but number of occipital veins was also less on the same side. Hence, we approached from the left side. However, operative findings during suboccipital exposure of tentorium revealed many big venous channels in the tentorium [Figure 4].
Table 3:
Side of transverse venous sinuses in study subjects (n=30).
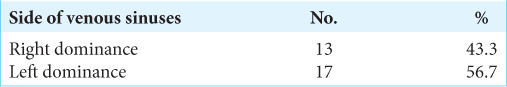
Figure 4:
Intraoperative view of tentorium cerebelli showing multiple venous channels (arrows).
Histopathological diagnosis of the lesions that were operated using this approach was five pineocytomas, three pinealoblastomas, five pilocytic astrocytomas, two pineal epidermoid, seven tuberculomas, three anaplastic oligodendrogliomas, one PNET, one ganglioglioma, one metastatic small cell carcinoma, one pineal parenchymal tumor, and one meningioma [Figures 5-9]. Gross total and near total resection was possible in 23 (76.6%) patients. Subtotal resection was done in 7 (23.4%) patients [Table 4].
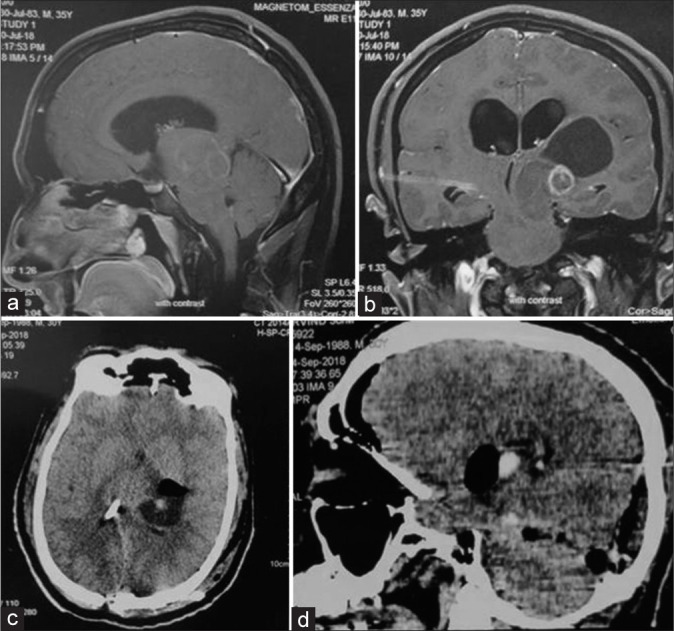
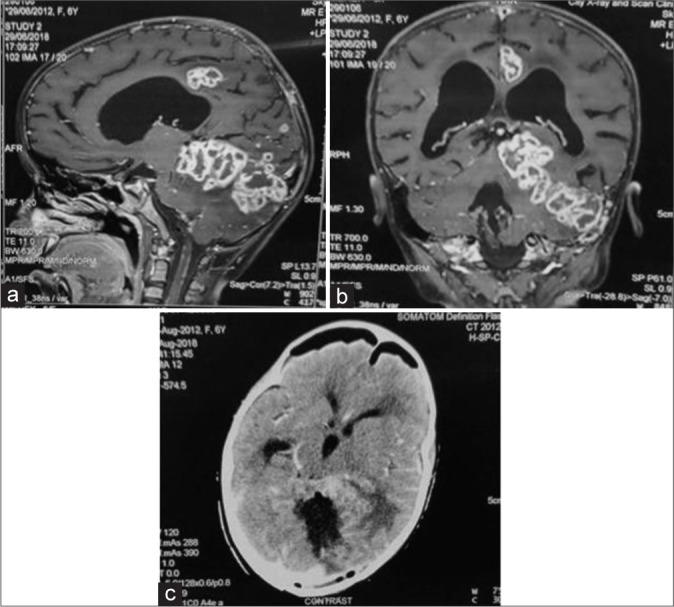
Figure 5:
(a) Preoperative images of falcotentorial meningioma with both supra and infratentorial extension, vein of Galen being inferior to the tumor. (b) Sagittal view. (c) Postoperative images of the same patient showing subtotal tumor removal.
Figure 9:
(a) A case of posterior thalamic pilocytic astrocytoma with both supra and infratentorial extension, with involvement of midbrain. (b) Coronal view. (c) Postoperative image of same patient showing gross total tumor removal, vp shunt tube is seen in situ. (d) Postoperative computed tomography scan in sagittal view of the same patient.
Table 4:
Extent of resection in study subjects (n = 30).
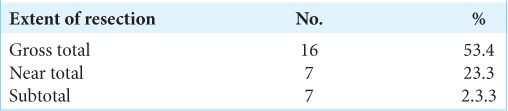
Figure 6:
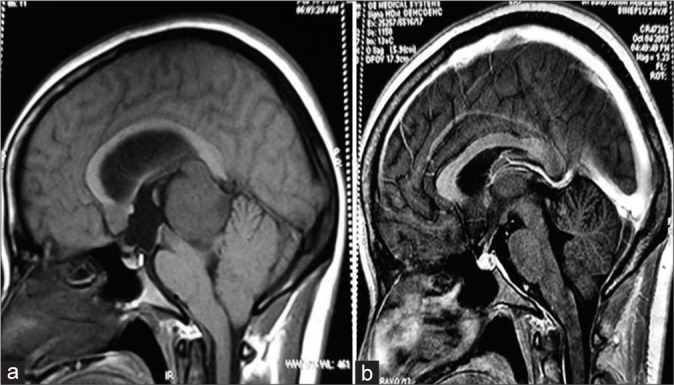
(a) Preoperative sagittal image showing pineal region mass (pineocytoma) located below the vein of Galen. (b) Postoperative image of same patient showing gross total tumor resection.
Figure 7:
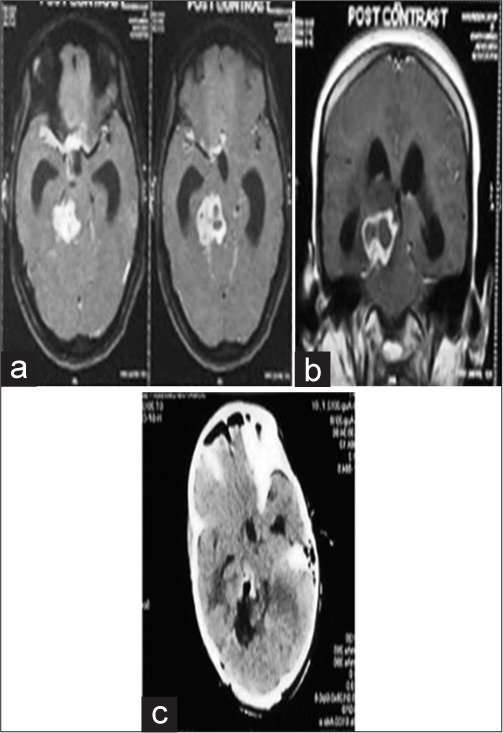
(a) Preoperative image of right thalamic tuberculoma extending both above and below the tentorium with involvement of midbrain. (b) Coronal view. (c) Postoperative image of same patient showing gross total tumor removal.
Figure 8:
(a) Preoperative image of multiple cerebellar tuberculomas with supra and infratentorial extension, vein of Galen is seen above the lesion. (b) Coronal view. (c) Postoperative image of same patient showing gross total tumor resection.
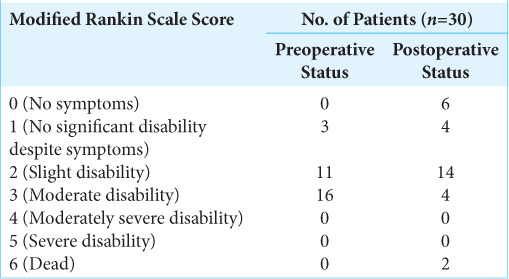
Few complications were encountered in the postoperative period. Superior gaze palsy was present preoperatively as well as postoperatively in two patients. Visual field defects in the form of homonymous hemianopia developed in two patients at the end of 1 week (P = 0.47). At the end of 1 and 3 months, however, only one patient had residual homonymous hemianopia (P = 0.98). The modified Rankin scale in the postoperative period for majority of the patients (14) was 2. The mean modified Rankin scale score was 1.8 which indicated slight postoperative disability. There were 2 postoperative mortalities due to uncontrolled postoperative seizure and acute hydrocephalus each [Table 5].
Table 5:
Preoperative and postoperative modified rankin scale in study subjects (n=30).
DISCUSSION
The pineal region can be the site of many central nervous system lesions, being responsible for 3–8% of the pediatric brain tumors and 0.4–1% of adult tumors.[14] The management options for pineal region tumors include either microsurgical resection or endoscopic resection with endoscopic third ventriculostomy (for concomitant management of hydrocephalus). Microsurgical approaches include the SCIT, OT, ¾ prone, OT with operated side down, combined suprainfratentorial trans-sinus, posterior transcallosal interhemispheric, and transcortical transventricular approaches. The infratentorial supracerebellar and the OT approaches are currently the most frequently used access ways to excise lesions of the pineal region.[2]
Historical perspective
The OT approach was described by Heppner in 1959 and popularized by Poppen. He was an American neurosurgeon, who operated a case of pinealoma using this approach in 1966 and published a series of 25 patients of pineal region lesions along with Marino in 1968.[16,17,20] Poppen is considered the pioneer of this approach; hence, the approach is commonly referred to as the Poppen’s approach. The original Poppen’s approach was, however, abandoned with due course of time as it was associated with drawbacks such as excessive occipital lobe retraction leading to increased postoperative homonymous hemianopia, surgeon’s discomfort (due to sitting position of the patient) as well as limited surgical exposure (mainly attributable to trephine craniotomy). Kenneth Jamieson, an Australian neurosurgeon, modified this approach in 1971 by approaching closer to the midline, and cutting the tentorium away from the SS.[7,20] Similarly, various modifications of the approach have been made by various authors down the line with variable results. Sano[19] used prone position in OT approach but it required significant occipital lobe retraction. Kobayashi et al.[9] used concorde position (head and shoulders elevated above waist) but it was uncomfortable for surgeon and assistant, Bloomfield et al.[3] suggested modified concorde position but was associated with similar surgeon’s discomfort.
Ausman et al. described a modified 3/4 prone, operated side down, occipitalparietal, transtentorial approach to the pineal region in which surgery was performed with the head placed in the threequarter prone position with the operated side down.[1] They utilized this position in 13 cases and found that it combined the advantages of all the previously described operations to the pineal region without the disadvantages. This position allowed excellent access to the pineal region and posterior third ventricle, comfort for the surgeon as well as the assistant, decreased risk of venous air embolism as compared to sitting position and minimum occipital lobe retraction (due to gravity assisted falling of the occipital lobe with cerebrospinal fluid [CSF] and ventricular drainage, without retraction). The steps in positioning are outlined in their paper. This position also allows easy access to the superior medullary velum and upper pons and midbrain. They operated a variety of pineal lesions using this position and approach and no postoperative homonymous hemianopia was found postoperatively in their cases. Similar good results were reported by Brotchi et al. who used this novel approach in their seven cases.[4] However, in our series, prone position was preferred due to its relative simplicity, ergonomic comfort, anatomic familiarity, and decreased risk of air embolism. With advances in technology and better understanding of the anatomy of the pineal region, the OT approach has stood the test of time and is still practiced by neurosurgeons all over the world with subtle modifications of the original Poppen’s approach.
The present series includes both pediatric and elderly patients with mean age of 26.47 years. The youngest patient in this series was 3 years old, and maximum of 67 years, with a mean age of 26.47 years. Maselli et al.[11] studied the efficacy of OT approach in 14 patients (nine males and five females) in the age group from 12 to 78 years with a mean age of 43.1 years. Similar to results obtained by Tanaka and Washiyama,[24] a wide variety of pineal region lesions as observed in histopathological analysis were operated with this approach in this series.
As suggested by Joaquim et al.,[8] the internal cerebral veins are usually elevated by the tumor and the VOG and its tributaries tightly cover the dorsal posterior portion of pineal region tumors. The tumor is approached through the opening between the VOG, ipsilateral basal vein.[8] This makes the preoperative assessment of venous architecture of paramount importance.
In this study, the VOG was found superiorly located with respect to the lesion in 25 (83.3%) cases, and inferiorly in 5 (16.7%) of cases. Gross and near total resection was achieved in all cases where the VOG was inferiorly located and in 72% of cases where the VOG was superiorly located in relation to the lesion. The subtotal resection happened due to infiltrative nature of the tumor and or unfavorable consistency of the tumor. In OT approach, the tumor and the venous system are visible in the same field on cutting the tentorium unlike infratentorial supra-cerebellar approach where venous system is visible or encountered after removing the tumor. This avoids the need of dissecting arachnoid encasing the veins. This may leave this area untouched and act as landmark to reach this site in recurrent surgery as was seen in one case in this study. The location of deep venous system had never been the limiting factor in removing the tumor in all the cases in this study which is in contrast to the conventional teaching, that is, if the deep venous system is superiorly placed in relation to lesion, SCIT and if below the lesion OT approach is indicated. We can preserve the precentral cerebellar vein in this approach which is sacrificed in other approaches; however, its sacrifice may not affect the outcome. This was in contrast with the observations made by Goto et al.[5] in 14 cases of falcotentorial meningiomas operated through OT approach; analyzing the influence of the anatomical relationship of the tumor to the VOG. They found unsatisfactory outcome in majority of cases with VOG located superior to the tumor, and satisfactory outcome in most cases of inferiorly placed VOG in relation to the tumor.
The lesions extending lateral to the midline with supratentorial extensions above the deep venous system, that is, those involving the lateral ventricle, posterior thalamus, or splenium of the corpus callosum require exposure to avoid undue retraction of brain which was achieved by this approach. In these cases combining PIH with OT may provide wider exposure. Lesions that extend dorsolateral to the brainstem, near the ambient cistern, and that extend inferiorly into the depths of the precentral cerebellar fissure near the fourth ventricular roof, inferior colliculus, and anterior vermis can also be exposed by the said approach as was also done in this series. Infiltration into surrounding structures was the limiting factor in complete tumor removal.
The parieto-occipital craniotomy is challenging as it requires exposure of SSS, TS, and SS. While cutting the bone, dura should be totally reflected from underlying bone to avoid injury to any of the sinus mentioned as was also the cause of abandoning a case in this series. Big tumors definitely require dural hitch sutures at SSS and TS level to avoid posttumor removal bleeding from hanging draining veins, which can be life threatening. Suzuki et al.[22] who applied 3D CT angiography to evaluate the deep venous system, emphasized the usefulness of preoperative assessment of variations in the deep venous system in the intraoperative navigation in OT approach.
Retraction of occipital lobe can be started first from the inferior side to locate the SS, SSS, TSs and starting the cutting of the tentorium 1–1.5 cm parallel to SS. In the middle of cutting of the tent, the microscope is angulated and the incision is preceded supero-medially toward the splenium and is completed till the free edge of tentorium cerebelli. These steps would help in keeping the trajectory toward deep venous system, as was done in all the cases in this series and was successful in all the cases. Our method differed from the original Poppen’s method where the tentorium was cut in a wedge shape with ligation of bridging veins; after a trephine craniotomy.[15] Cutting the tentorium may be a challenge in cases where multiple venous channels are present in the tentorium as was found in three cases in this series. One needs to understand this variation while cutting the tentorium. In these cases one need to change the course of cutting the tentorium which can be made safer by use of ICG.
There is paucity in the literature regarding extent of resection and functional outcome for various lesions requiring OT approach, most likely as a consequence of the relatively low frequency of the pineal region lesions, understanding the tentorial angulation, and technique of cutting the tent. OT approach requires retraction of occipital lobe and cutting of tentorium which can be performed in either lateral or prone position. Splitting the tentorium offers a panoramic supra- and infratentorial view of the tumor, the surrounding deep venous structures and the collicular plate of the midbrain; hence, the lesions with both supra and infratentorial extension can be resected by this approach.
Moreover, this position is better than sitting, that is, occipital approach is preferable if the tumor is vascular and in patients with associated comorbidities where sitting position is a relative contraindication. The OT is advocated in pineal region lesions mainly with steep tentorial angle, which limits the resection through the SCIT approach where excessive retraction or even resection of part of the upper cerebellar vermis may be necessary to reach the lesion.[8] Moreover, a steep tentorial angle can also be associated with occipital lobe damage. It can also be a confounding factor along with age and hard tumor consistency leading to increased operating time and may limit the resectability of the lesion.[10] Hence, the preoperative assessment of tentorial angle is important in guiding the surgeon about the anticipated intra operative difficulties in tumor resection and minimizing the complications.
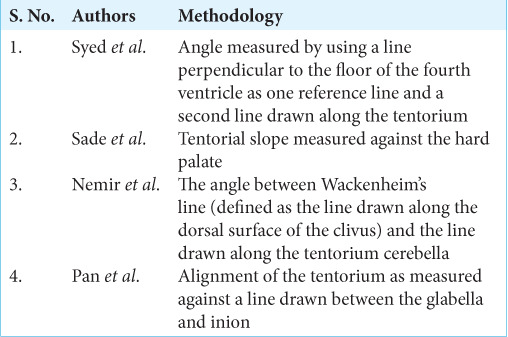
The tentorial angle was measured against a line joining the torcula to the plane of the fourth ventricle. The advantage of this method was its ability to accurately describe the slope of the tentorium, without underestimating it in case of a low lying torcula.[23] Various methods to measure the tentorial angle are mentioned in the literature, each having their own advantages and disadvantages [Table 6].[15] In the present series, the mean tentorial angle was 62.08 ± 7.17 with a minimum and maximum angle of 51° and 83°, respectively. Hence, cases having both shallow (<60 deg) and steep (>60 deg) tentorial angles were operated using OT approach in this study. A specific examination of the efficacy of the OT approach in patients with lesions arising from the precentral cerebellar fissure was done by Moshel[13] where Gross total and near total, subtotal resection 19 (86%) and 3 (14%) cases, respectively. Using this approach, gross total and near total resection was possible in 12 (71%) cases as observed in this study which is comparable with results obtained by Moshel. However, the reason for subtotal resection in 7 (23.3%) patients in the present study was poor plane between tumor and brainstem parenchyma, tumor adherence to VOG, and lesions infiltrating the tectal plate and midbrain. Similar factors for partial tumor resection were observed by Moshel.
Table 6:
Methods of measurement of tentorial alignment.
Few complications were encountered in the study. In one case, surgery was abandoned due to excessive bleeding from the SSS and torcula during craniotomy. Visual field defects in the form of homonymous hemianopia developed in two patients postoperatively and persisted at the end of 1 week. At the end of 1 and 3 months; however, only one patient had residual homonymous hemianopia. This was probably due to prolonged retraction followed by ischemic insult of the inferomedial surface of the occipital lobe and due to firm tumor consistency leading to increased operating time in these cases. However, the retraction associated deficits can be minimized by using multiple retractors, preoperative CSF diversion procedures (as used in the present series), intraoperative CSF drainage by ventricular puncture of the occipital horn and intermittent retraction.[1,12]
The postoperative surgical outcome as assessed by modified Rankin scale in majority of the patients (14) was 2. The mean modified Rankin scale score was 1.8 which indicated slight postoperative disability. Similar results were obtained by Maselli et al.[11] who obtained good to excellent functional outcomes as assessed by Karnofsky Performance Status scores.
Limitations
It is an institutional study which focuses on OT approach (mainly in prone or lateral positions) based on surgeon’s preference and hence it is imperative to consider established studies which advocate variation in position for the OT approach (i.e. three quarter prone position) for better and satisfactory surgical outcomes. Moreover, no comparative analysis is done among the various other surgical approaches for pineal region lesions in this series.
CONCLUSION
The pineal region masses occur in both extremes of age, that is, in pediatric and elderly population. The OT approach can be tailored to achieve high rates of resectability irrespective of the status of the deep venous system. The anatomical angles such as the tentorial angle have no correlation with tumor resectability and postoperative surgical outcome in the patients of pineal region mass operated by the OT approach.
The OT approach is a reasonably safe approach provided the craniotomy is made cautiously for the surgical management of pineal region lesions where high resectability rates can be achieved, with slight postoperative morbidity.
Footnotes
How to cite this article: Katyal A, Jadhav A, Katyal A, Jagetia A, Bodeliwala S, Singhal GD, et al. Occipital transtentorial approach for pineal region lesions: Addressing the controversies in conventional teaching. Surg Neurol Int 2021;12:503.
Contributor Information
Abhishek Katyal, Email: ak.neurosx.47@gmail.com.
Anil Jadhav, Email: aniljadhav7@gmail.com.
Aparna Katyal, Email: draparnakatyal@gmail.com.
Anita Jagetia, Email: anitajagetia@gmail.com.
Shaam Bodeliwala, Email: shaam.86@gmail.com.
Ghanshyam Das Singhal, Email: singhalgd@gmail.com.
Wajid Nazir, Email: dr_wajidnazir@rediffmail.com.
Vineeta Batra, Email: vvbatra9@gmail.com.
Arvind Kumar Srivastava, Email: aksrivastava2008@gmail.com.
Daljit Singh, Email: drdaljit@hotmail.com.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ausman JI, Malik GM, Dujovny M, Mann R. Three-quarter prone approach to the pineal-tentorial region. Surg Neurol. 1988;29:298–306. doi: 10.1016/0090-3019(88)90161-9. [DOI] [PubMed] [Google Scholar]
- 2.Azab WA, Nasim K, Salaheddin W. An overview of the current surgical options for pineal region tumours. Surg Neurol Int. 2014;5:39. doi: 10.4103/2152-7806.129430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bloomfield SM, Sonntag VK, Spetzler RF. Pineal region lesions. Barrow Neurol Inst Q. 1985;1:10–23. [Google Scholar]
- 4.Brotchi J, Levivier M, Raftopoulos C, Dewitte O, Pirotte B, Noterman J. Three-quarter prone approach to the pinealtentorial region. Report of seven cases. Acta Neurochir Suppl (Wien) 1991;53:144–7. doi: 10.1007/978-3-7091-9183-5_24. [DOI] [PubMed] [Google Scholar]
- 5.Goto T, Ohata K, Morino M, Takami T, Tsuyuguchi N, Nishio A, et al. Falcotentorial meningioma: Surgical outcome in 14 patients. J Neurosurg. 2006;104:47–53. doi: 10.3171/jns.2006.104.1.47. [DOI] [PubMed] [Google Scholar]
- 6.Isaac JA, Brian H, Jason B, Martin M, Richard GE. A single-institution experience with pineal region tumors: 50 tumors over 1 decade. Oper Neurosurg (Hagerstown) 2017;13:566–75. doi: 10.1093/ons/opx038. [DOI] [PubMed] [Google Scholar]
- 7.Jamieson KG. Excision of pineal tumors. J Neurosurg. 1971;35:550–3. doi: 10.3171/jns.1971.35.5.0550. [DOI] [PubMed] [Google Scholar]
- 8.Joaquim AF, dos Santos MJ, da Silva ÉG, Tedeschi H. Interhemispheric occipital transtentorial approach to the pineal region and dorsal midbrain. J Bras Neurocir. 2009;20:22–6. [Google Scholar]
- 9.Kobayashi S, Sugita K, Tanaka Y, Kyoshima K. Infratentorial approach to the pineal region in the prone position: Concorde position. Technical note. J Neurosurg. 1983;58:141–3. doi: 10.3171/jns.1983.58.1.0141. [DOI] [PubMed] [Google Scholar]
- 10.Li D, Zhang H, Jia W, Zhang L, Zhang J, Liu W, et al. Significance of the tentorial alignment in protecting the occipital lobe with the poppen approach for tentorial or pineal area meningiomas. World Neurosurg. 2017;108:453–9. doi: 10.1016/j.wneu.2017.08.013. [DOI] [PubMed] [Google Scholar]
- 11.Maselli G, Paulis D, Ricci A, Galzio R. Posterior cranial fossa tumours: Results and prognostic factors in a consecutive series of 14 operated patients by occipital transtentorial approach. Surg Neurol Int. 2012;3:85. doi: 10.4103/2152-7806.99911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Matsuo S, Baydin S, Güngör A, Middlebrooks EH, Komune N, Iihara K, et al. Prevention of postoperative visual field defect after the occipital transtentorial approach: Anatomical study. J Neurosurg. 2018;129:188–97. doi: 10.3171/2017.4.JNS162805. [DOI] [PubMed] [Google Scholar]
- 13.Moshel Y. A occipital transtentorial approach to the precentral cerebellar fissure and posterior incisural space. Neurosurgery. 2009;65:554–64. doi: 10.1227/01.NEU.0000350898.68212.AB. [DOI] [PubMed] [Google Scholar]
- 14.Mottolese C, Szathmari A, Beuriat PA. Incidence of pineal tumours. A review of the literature. Neurochirurgie. 2015;61:65–9. doi: 10.1016/j.neuchi.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 15.Nemir J, Njirić N, Ivanković D, Barl P, Domazet I, Radoš M, et al. Tentorial alignment and its relationship to cisternal dimensions of the pineal region: MRI anatomical study with surgical implications using the new clivotentorial method. Clin Neurol Neurosurg. 2018;172:99–10. doi: 10.1016/j.clineuro.2018.06.028. [DOI] [PubMed] [Google Scholar]
- 16.Poppen JL, Marino R. Pinealomas and tumors of the posterior portion of the third ventricle. J Neurosurg. 1968;28:357–64. doi: 10.3171/jns.1968.28.4.0357. [DOI] [PubMed] [Google Scholar]
- 17.Poppen JL. The right occipital approach to a pinealoma. J Neurosurg. 1966;25:706–10. doi: 10.3171/jns.1966.25.6.0706. [DOI] [PubMed] [Google Scholar]
- 18.Rhoton AL., Jr The tentorial incisura. Neurosurgery. 2000;47(Suppl 3):93–129. doi: 10.1097/00006123-200009001-00015. [DOI] [PubMed] [Google Scholar]
- 19.Sano K. Pineal region tumors: Problems in pathology and treatment. Clin Neurosurg. 1983;30:59–91. doi: 10.1093/neurosurgery/30.cn_suppl_1.59. [DOI] [PubMed] [Google Scholar]
- 20.Sharma M, Madhugiri V, Nanda A, James L. Poppen and surgery of the seat of the soul: A contemporary perspective. World Neurosurg. 2014;82:529–34. doi: 10.1016/j.wneu.2013.02.004. [DOI] [PubMed] [Google Scholar]
- 21.Simon E, Afif A, M’Baye M, Mertens P. Anatomy of the pineal region applied to its surgical approach. Neurochirurgie. 2015;61:70–6. doi: 10.1016/j.neuchi.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 22.Suzuki Y, Nakajima M, Ikeda H, Abe T. Three-dimensional computed tomography angiography of the galenic system for the occipital transtentorial approach. Neurol Med Chir (Tokyo) 2005;45:387–94. doi: 10.2176/nmc.45.387. [DOI] [PubMed] [Google Scholar]
- 23.Syed HR, Jean WC. A novel method to measure the tentorial angle and the implications on surgeries of the pineal region. World Neurosurg. 2018;111:e213–20. doi: 10.1016/j.wneu.2017.12.037. [DOI] [PubMed] [Google Scholar]
- 24.Tanaka R, Washiyama K. Occipital transtentorial approach to pineal region tumours. Oper Tech Neurosurg. 2009;6:215–21. [Google Scholar]


