Abstract
Background:
Despite mainly benign, exophytic subcutaneous cranial masses present with a myriad of differential diagnosis possibilities, ranging from simple, superficial lesions to complex lesions involving the central nervous system. Although the gold standard imaging modality for the diagnosis of these lesions is magnetic resonance imaging, Doppler Ultrasonography can be a useful, inexpensive, and available tool for evaluation of lesions that could potentially be safely treated in the primary care setting, and lesions that would demand advanced neurosurgical care.
Case Description:
This patient presented with a complex exophytic plasmocytoma that was first diagnosed and erroneously approached as a subcutaneous lipoma with surgical resection in an outpatient surgical setting. This interpretive approach resulted in the failure of the procedure due to significant hemorrhage. The patient was immediately referred to neurosurgical care and transferred to our center. Admission doppler ultrasound imaging revealed absence of the frontal bone, the enriched and profuse vascularization, allowing further and proper diagnostic approach and treatment.
Conclusion:
Ultrasound could be a reliable, fast, and simple imaging method aiding practitioners to perform a better workup for patients with exophytic subcutaneous cranial masses.
Keywords: Forehead subcutaneous mass, Plasmacytoma, Ultrasound in neurosurgery

INTRODUCTION
The term exophytic tumor is used to define masses that expand to the skin’s external surface. Soft subcutaneous tumor differentials are dermoid cysts, hemangiomas, lipomas, epidermal inclusion cysts, and osteomas.[6] Forehead lipomas are soft slow-growing solitary masses, often diagnosed clinically and promptly treated with ambulatorial resection for esthetic purposes, since most of these tumors are non-painful.[5] Meningiomas, hemangiopericytomas, and plasmacytomas can be found from any intracranial or spinal dural surface, being the first one of the most common primary central nervous system tumors in adults, of which 53.2% are non-malignant.[3]
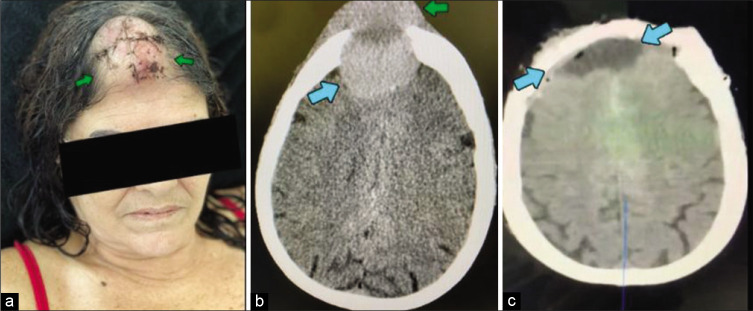
In certain locations and histological subtypes, these CNS tumors might equally present as soft slow-growing, solitary forehead masses, with no otherwise neurological deficits [Figure 1].[2] The gold standard modality for radiological diagnosis is magnetic resonance imaging and the diagnostic approach of these lesions often involves computerized tomography scans prior to craniotomy and neurosurgical resection. However, both intracranial exophytic lesions and these forehead tumors often present to the surgery department with a previous diagnosis of a benign subcutaneous mass with no other malignancy signs. This scenario might lead to inadvertent resection attempts in primary care consults, leading to significant and potentially fatal complications.
Figure 1:
Patient’s incision aspect after first approach (a) without prior imaging. Preoperative CT scan (b) showing intracranial (blue arrow) and extracranial (green arrow) components of the tumor. Postoperative imaging (c) showing no residual intra or extracranial lesions after evacuation (blue arrows).
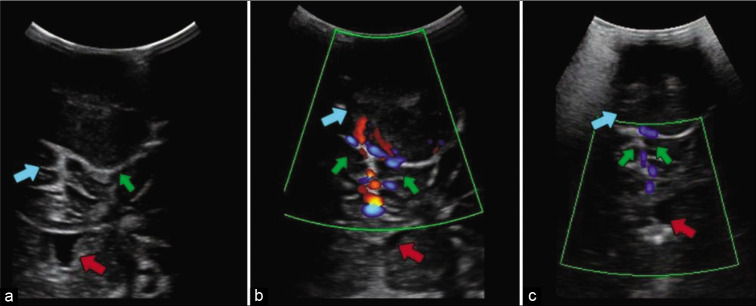
Recently in low-income and middle-income contexts, intraoperative ultrasound is shown to be a cost-effective and widely available tool for both diagnostic and neuronavigation/ surgical planning purposes, allowing multiple derivations of both intraoperative and preoperative usages.[4] In this context, the doppler ultrasonography might be a cost-effectively and widely available alternative in establishing differential diagnosis between a large subcutaneous lesion and an intracranial exophytic lesion demanding specialized neurosurgical care [Figure 2].[1]
Figure 2:
Ultrasound image (a) showing the exophytic lesion (green arrow) in direct contact with the cerebral parenchyma (blue arrow). Bone erosion created a window in the frontal bone through which even the lateral ventricles (red arrow) are visible. Doppler ultrasound performed before embolization (b) showing vascularity of the tumor (green arrows) and after embolization (c) showing reduced blood flow (green arrows). In these images, the lesion (green arrow and blue arrows, a and b image respectively) and the lateral ventricles (red arrows) surrounded by brain parenchyma are still seen.
Footnotes
How to cite this article: Perret C, Bertani R, Barbosa MM, Batista S, Koester SW, Maria PS, et al. Hemorrhage due to attempted excision of a frontal exophytic lesion: A cautionary tale. Surg Neurol Int 2021;12:512.
Contributor Information
Caio Perret, Email: perretcaio@gmail.com.
Raphael Bertani, Email: contato@rbertani.com.
Mauricio Mendes Barbosa, Email: mmbarbosafilho@gmail.com.
Savio Batista, Email: saviobatista360@gmail.com.
Stefan W. Koester, Email: stefanwkoester@gmail.com.
Paulo Santa Maria, Email: paulo.stmaria.rj@gmail.com.
Hugo Schiavini, Email: hcschiavini@yahoo.com.br.
Declaration of patients consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no Conflict of Interest.
REFERENCES
- 1.Abdi A, Armijo E, Seif D, Kang T. Man with a forehead mass: Detection of a forehead pseudoaneurysm with bedside ultrasonography. Case Rep Emerg Med. 2014;2014:647175. doi: 10.1155/2014/647175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brown JM, Cherry AP. Subcutaneous meningioma. Med J Aust. 1971;2:1072–3. doi: 10.5694/j.1326-5377.1971.tb92710.x. [DOI] [PubMed] [Google Scholar]
- 3.Buerki RA, Horbinski CM, Kruser T, Horowitz PM, James CD, Lukas RV. An overview of meningiomas. Future Oncol. 2018;14:2161–77. doi: 10.2217/fon-2018-0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kaale AJ, Rutabasibwa N, Mchome LL, Lillehei KO, Honce JM, Kahamba J, et al. The use of intraoperative neurosurgical ultrasound for surgical navigation in low-and middle-income countries: The initial experience in Tanzania. J Neurosurg. 2020;134:630–7. doi: 10.3171/2019.12.JNS192851. [DOI] [PubMed] [Google Scholar]
- 5.Neches SK, Parcells AL, Feintisch AM, Granick MS. Submuscular lipoma of the forehead. Eplasty. 2015;15:ic17. [PMC free article] [PubMed] [Google Scholar]
- 6.Sewell LD, Adams DC, Marks VJ. Subcutaneous forehead nodules: Attention to the button osteoma and frontalis-associated lipoma. Dermatol Surg. 2008;34:791–8. doi: 10.1111/j.1524-4725.2008.34148.x. [DOI] [PubMed] [Google Scholar]